Abstract
Histone deacetylase inhibitors (HDACis) are a significant category of pharmaceuticals that have developed in the past two decades to treat multiple myeloma. Four drugs in this category have received approval from the U.S. Food and Drug Administration (FDA) for use: Panobinonstat (though canceled by the FDA in 2022), Vorinostat, Belinostat and Romidepsin. The efficacy of this group of drugs is attributed to the disruption of many processes involved in tumor growth through the inhibition of histone deacetylase, and this mode of action leads to significant anti-multiple myeloma (MM) activity. In MM, inhibition of histone deacetylase has many downstream consequences, including suppression of NF-κB signaling and HSP90, upregulation of cell cycle regulators (p21, p53), and downregulation of antiapoptotic proteins including Bcl-2. Furthermore, HDACis have a variety of direct and indirect oxidative effects on cellular DNA. HDAC inhibitors enhance normal immune function, thereby decreasing the proliferation of malignant plasma cells and promoting autophagy. The various biological effects of inhibiting histone deacetylase have a combined or additional impact when used alongside other chemotherapeutic and targeted drugs for multiple myeloma. This helps to decrease resistance to treatment. Combination treatment regimens that include HDACis have become an essential part of the therapy for multiple myeloma. These regimens incorporate drugs from other important classes of anti-myeloma agents, such as immunomodulatory drugs (IMiDs), conventional chemotherapy, monoclonal antibodies, and proteasome inhibitors. This review provides a comprehensive evaluation of the clinical efficacy and safety data pertaining to the currently approved histone deacetylase inhibitors, as well as an explanation of the crucial function of histone deacetylase in multiple myeloma and the characteristics of the different histone deacetylase inhibitors. Moreover, it provides a concise overview of the most recent developments in the use of histone deacetylase inhibitors for treating multiple myeloma, as well as potential future uses in treatment.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) is a hematologic malignancy defined by the development of aberrant clonal plasma cells in the bone marrow, which can cause severe bone lesions, renal damage, anemia, and hypercalcemia [1]. MM is most prevalent in industrialized countries, particularly in Australia, Western Europe, and the United States, where it has the greatest prevalence [2]. It is the second most common hematologic malignancy in the United States, accounting for around 1.8% of all cancers and approximately 10% of hematologic malignancies [3]. In 2022, according to the American Cancer Society, about 34,470 new MM cases will be diagnosed in the United States, with an estimated 12,640 deaths [4]. MM is a neoplasm of older adults, with the median age of diagnosis in the United States being 69, and the median age of death is 75. Globally, men are around 1.5 times more likely than women [5]. Although recent therapies have led to a significant increase in the illness's 5-year survival rate, which now exceeds 5 years, and have improved the quality of life for patients, it is important to note that the condition is still incurable [6].
The notable enhancements in results have been correlated with the extensive utilization of autologous stem cell transplantation (ASCT) as a customary practice for eligible patients [7], along with the advancement and authorization of many innovative medications and treatment plans for managing MM [8]. In the past twenty years, various new types of drugs have been developed, including proteasome inhibitors, immunomodulatory drugs, monoclonal antibodies (mAbs), antibody–drug conjugates (ADC), bispecific T-cell engagers (BiTE), chimeric antigen-T-cell therapy (CAR-T), peptide-drug conjugates, selective inhibitors of nuclear export, and small-molecule targeted therapies [9]. With the introduction of these new treatments, treatment paradigms for MM patients have evolved as well, by employing more intricate methods, such as the use of triple therapy as opposed to dual therapy, and the increased implementation of continuous or long-term treatment, patient results can be improved. Nevertheless, the effectiveness of these treatments is frequently compromised by the emergence of resistance and the occurrence of relapse, thereby emphasising a significant deficiency in the therapy continuum [10,11,12]. Hence, the significance of novel therapeutic approaches for multiple myeloma cannot be overstated.
Over the last two decades, histone deacetylases (HDACs) have emerged as important therapeutic targets in cancers, particularly multiple myeloma [13, 14]. HDACis have gained significant interest as they target HDAC, which have been identified as crucial in the development of new therapy approaches for this specific condition. The fact that HDACis reduce multiple myeloma cell survival and proliferation through different mechanisms has contributed to their effectiveness. As it turns out, many HDACis have been used and evaluated in both preclinical and clinical contexts. Significantly, the FDA has granted approval to four HDACis: Vorinostat, Romidepsin, Panobinostat, and Belinostat. These HDACis are mostly utilized in clinics for hematologic tumors with less severe side effects [15]. These drugs' clinical data will be summarized later in this study.
This review provides a comprehensive analysis of the crucial role of HDACis in MM, as well as the clinical evaluation of different HDACis. It focuses on the many consequences of inhibiting histone deacetylation in MM and examines the justification for using HDACis in conjunction with medications or immunotherapies that target other pathways, with the goal of enhancing their effectiveness. Furthermore, it examines the mechanisms behind resistance to histone deacetylation inhibition and explores potential strategies to overcome this resistance through combination treatment.
In the end, it offers an in-depth review of the clinical effectiveness and safety data for treatments based on HDACis in various treatment scenarios for MM, highlighting the significance of these drugs as the primary form of treatment for MM.
Rationale for targeting HDACs in MM
Based on homology to yeast HDAC, subcellular localization, and noncellular enzymatic activity, the 18 HDAC isoforms in humans are divided into four groups, classes I (HDAC1, HDAC2, HDAC3, HDAC8), Class IIa (HDAC4, HDAC5, HDAC7, HDAC9), Class IIb (HDAC 6, DAC10), Class III (SIRT1-SIRT7), and Class IV (HDAC11) (Fig. 1a) [16,17,18,19]. Class I, II, and IV HDACs possess a deacetylase domain that relies on the presence of Zn2+, while class III HDACs contain a deacetylase domain that depends on the presence of NAD+. Class I members exhibit widespread expression, with nuclear localization being the predominant pattern. They also have an N-terminal catalytic domain and are made up of about 400 amino acids. Their catalytic domain is formed by two neighboring histidine residues, two aspartic acid residues, and a tyrosine residue centered on a Zn2+ ions [20, 21]. Class II members exhibit enhanced specificity in expression and possess the ability to actively transport between the nucleus and the cytoplasm. Class IIa HDACs consist of 600–1200 amino acids and possess an N-terminal regulatory domain that enables interactions with tissue-specific transcription factors and corepressors [22, 23]. In the C-terminal region of Class IIb HDACs, there is another catalytic domain and a ubiquitin-binding zinc finger domain, respectively [24, 25]. The sirtuin deacetylase family (SIRT1-7) belongs to class III, however they are not functionally linked to HDAC; their deacetylase activity is based on NAD+ rather than Zn2+-dependent enzymes [26]. HDAC11, the sole member of the class IV HDAC family, is mostly found in the nucleus. The majority of its amino acid sequence is dedicated to its catalytic domain [27].
HDAC biology
HDACs have a crucial function in controlling gene expression by altering the acetylation state of histones, which are proteins involved in the packaging and organization of DNA in the cell nucleus [28, 29]. In the context of MM, HDACs have been associated with several facets of the disease (Fig. 1b), including cell cycle regulation [30], apoptosis resistance [31], and interactions with the tumor microenvironment (Proliferation, differentiation, inflammation, metastasis, angiogenesis) [32,33,34]. Notably, endothelial cells play a crucial role in the process of angiogenesis, which involves the development of new blood vessels. This process is essential for the growth and dissemination of tumors. In the microenvironment of MM, these cells undergo alterations in their properties and concurrently promote angiogenesis, thereby expediting the advancement of the disease and the development of medication resistance. HDACis have become a prominent inhibitory factor in this process by compromising the activities of endothelial cells and affecting the blood supply network of the tumor [35, 36]. Their mechanism of action involves the inhibition of HDACs, which induces alterations in gene expression in endothelial cells, ultimately leading to anti-angiogenic effects [37]. The integration of endothelial cell targeting and angiogenesis in the treatment of MM is a promising approach to overcome drug resistance and improve therapeutic results.
HDACs, as a whole, facilitate the elimination of acetylation from lysine residues in target proteins [30, 38]. They play a critical role in regulating cell function, not only by removing acetyl groups from lysine residues on core histones, leading to tighter chromatin and reduced gene expression [14], but also by deacetylating non-histone proteins such as the tumor suppressor p53 [39,40,41], STAT3 [42], HSP90 [43], and NF-κB [44]. This action significantly affects these proteins' function, interactions, and stability, influencing various cellular activities [45] (Fig. 2). In MM, this regulation becomes particularly important. The constant activation of the NF-κB pathway [46] and other cancer-promoting mechanisms leads to fast cell growth and a supportive environment in the bone marrow [47]. This creates a cycle that helps MM cells survive and multiply. HDACis can break this cycle. They change the acetylation pattern of both histone and non-histone proteins, which impacts chromatin structure, gene activity, and critical signaling pathways, such as NF-κB, PI3K/AKT/mTOR, and MAPK [48, 49]. As we mentioned before, by also affecting the tumor environment and promoting cell death and cell cycle arrest, HDACis show strong potential against MM. Their ability to target both epigenetic and non-epigenetic factors highlights their promise in MM treatment, especially when used alongside other therapies [30]. Moreover, autophagy, an essential cellular mechanism responsible for the degradation and recycling of impaired organelles and proteins, assumes a multifaceted and ambivalent role in the pathology of MM [40, 50, 51]. This process facilitates cellular survival under conditions of stress by provisioning vital nutrients and energy, thereby contributing to the development of drug resistance. Conversely, aberrant or excessive autophagy may precipitate cellular demise, potentially amplifying the efficacy of anti-cancer therapeutics [52] (Fig. 2). HDACis are observed to modulate autophagy within MM cells through a bifurcated mechanism: initiating protective autophagy that favors cellular survival or provoking cytotoxic autophagy, culminating in cellular mortality [53, 54]. This comprehensive approach aims to disrupt the key cellular processes that MM cells rely on to survive and grow. In conclusion, factors such as autophagy, drug resistance, and endothelial cells are interrelated factors that influence the efficacy of MM treatment [55], especially in the context of HDAC inhibition. Understanding the complex interplay between these factors can help guide the development of new treatment strategies and improve outcomes for patients with MM.
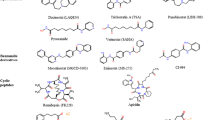
HDAC inhibitors
A range of HDACis have been investigated in the context of malignancies. HDACis are categorized into six types based on their chemical structure. Short-chain fatty acid, hydroxamic acid, benzamide, cyclic peptide, mercaptoketone, sirtuin inhibitors, and other compounds [56, 57] (Table 1). Non-selective HDACis have the ability to inhibit various HDAC isoforms. However, previous research has shown that the primary focus of clinically important HDACis are HDAC 1, 2, 3, and 6. These findings indicate that the primary mechanism behind the anti-tumor properties of non-selective HDACis is the inhibition of class I and class IIb HDAC enzymes [58]. Clinical development of HDACis continues benefiting a growing number of patients with RRMM. Among them, Panobinostat (LBH589) is a strong non-selective oral pan-histone deacetylase inhibitor with efficacy in myeloma patients [59]. Panobinostat was approved by the FDA in 2015 to treat RRMM based on promising preclinical and clinical research. However, it was withdrawn in the United States in March 2022 (Fig. 3). As clinical studies progress, an increasing number of HDACis are becoming viable options for treating RRMM. For instance, Qusinostat, Gavinostat and Rocilinostat employed exclusively in the management of solid tumors and refractory leukemia, demonstrate potential efficacy in the treatment of RRMM [60, 61].
Mechanisms of action of HDACis
HDACis work in several ways to prevent myeloma cell survival and growth. Cancer cells, particularly MM cells, exhibit cell cycle disruption, resulting in accelerated cell proliferation. Non-selective HDACis or class I HDACis cause G0/G1 cell cycle arrest by upregulating cell cycle regulators, such as p21 (WAF1) [62, 63] and p53 [64, 65], or downregulation of antiapoptotic proteins such as Bcl-2 [66]. HDACis facilitate the restoration of regular immunological function, leading to a reduction in the excessive growth of malignant plasma cells. Furthermore, HDACis exert various direct and indirect effects on cellular DNA, resulting in oxidative damage [67]. They induce mitotic delays by bypassing the spindle assembly checkpoint. In our recent exploration, we uncovered the reciprocal relationships between the epigenetic machinery and the non-coding genome in the control of gene expression. This involved delving into the fascinating connections between HDAC6-induced lncRNA and its prospective sponge miRNA in the context of MM [68]. Simultaneously, as discussed in Section "HDAC biology", Heat-shock protein 90 (HSP90), a cellular chaperone essential for proteins involved in intracellular signaling (Her2/neu, Raf, ERK, NF-κB), is likewise inhibited by HDACis [69, 70]. For instance, the protein Hsp90, which acts as a molecular chaperone, is affected by the process of deacetylation carried out by HDAC6. Various pieces of evidence indicate that inhibiting both HDAC6 and Hsp90 at the same time leads to enhanced anti-tumor effects on various cancer cell lines. This emphasizes the advantages of creating a single compound that can target multiple molecules simultaneously [71]. As such, dual-targeting strategies against histone deacetylase are designed to enhance therapeutic efficacy while minimizing the side effects associated with broad-spectrum HDAC inhibition.
Synergy with and resistance to HDAC Inhibition
Suppressing histone deacetylase has several effects that result in increased efficacy when combined with other chemotherapeutic and targeted therapies in MM, either via synergy or addition. Previous studies have shown that either panobinostat or vorinostat anticancer effects were increased in preclinical trials in patients with RRMM when combined with proteasome inhibitors such as bortezomib [72,73,74,75,76]. Both of them exhibit a synergistic impact in restraining cell proliferation and enhancing programmed cell death in MM cells [77]. The investigation further revealed that the co-administration of tubacin, a selective inhibitor of HDAC6, with bortezomib elicited a comparable outcome, concomitant with a notable augmentation in polyubiquitinated proteins [78]. In addition, the synergistic effect of panobinostat and romidepsin combined with proteasome inhibitors was also found in the MM cell mouse xenograft models in vivo [79, 80].
The strategy of combining therapies to overcome resistance to HDACis has been demonstrated to occur through multiple mechanisms [72]. The concurrent suppression of the proteasome and aggresome pathways is the most extensively studied manifestation of synergy between proteasome inhibitors and HDACis [81, 82] (Fig. 4). The convergence of bortezomib, a proteasome-targeting agent, with an HDAC6 inhibitor, specifically directed at aggregates within tumor cells, engenders heightened accumulation of polyubiquitinated proteins, consequently inducing increased cellular stress and death [81, 82]. In particular, proteasome inhibition promotes aggregation formation, which is dependent on HDAC6 interactions with tubulin and dynein complexes. Furthermore, both proteasome inhibitors (bortezomib) and HDAC6 inhibitors (tubacin or panobinostat) enhance tubulin hyperacetylation and polyubiquitinated protein synthesis, which increases cellular stress responses and leads to autophagy and apoptosis. This is partly determined by caspase activity [81, 82]. The potential overcoming of resistance mechanisms in multiple myeloma may be achieved through the synergistic combination of HDAC inhibitors with other active agents possessing diverse mechanisms of action within the context of MM, or by incorporating novel targeted agents specifically designed to address resistance pathways, allowing the persistent use of histone deacetylase inhibition as the mainstay of the entire course of treatment.
Aggresome pathway and synergy with proteasome inhibitors. Ubiquitin targets unfolded and/or misfolded proteins for destruction via the proteasome and aggresome pathways. Inhibiting proteasome pathways with inhibitors like bortezomib or carfilzomib results in the formation of ubiquitin protein aggregates, which are subsequently shuttled to the lysosome and destroyed via the aggresome pathway. Protein aggregates migrate across microtubules utilizing the dynein motor protein in the aggregation process. HDAC-6 promotes protein aggregate/microtubule complexes. If histone deacetylase (HDAC) is inhibited (together with proteasome inhibitors) at this moment, ubiquitin protein aggregates would develop further, resulting to apoptosis. If histone deacetylase (HDAC) is inhibited (together with proteasome inhibitors) at this moment, ubiquitin protein aggregates would develop further, resulting to apoptosis. Figure created with BioRender.com
Clinical outcomes of HDACis in MM
Numerous studies have established the applicability of histone deacetylation inhibitors in the treatment of MM during the course of more than a decade of continuous development of HDACis. Since the FDA approved some nonselective HDACis for the treatment of MM, a growing number of HDACis have become the cornerstone of overall MM treatment and are now or are being studied as an option for induction, consolidation, and maintenance therapy, as well as a single agent or in multiple highly effective combination regimens in RRMM. Here, we summarized clinical trials involving HDACis used alone, combined with dexamethasone, immunomodulatory drugs (IMiDs), traditional chemotherapy, and novel targeted agents. It is worth noting that recent advancements in the development of HDAC inhibitors for cancer treatment are geared towards specificity and improved outcomes. Innovations include the development of class I HDAC inhibitors [83], targeting enzymes frequently overexpressed in tumors to reduce growth and offer better therapeutic options. CN133, a promising HDAC inhibitor, showcases high selectivity for class I HDACs and improved penetration into prostate tissue, hinting at enhanced efficacy in prostate cancer treatment, particularly in combination therapies [84]. Additionally, research into HDAC10 targeting has led to the creation of specific inhibitors, like Tubastatin A and its analogues, aiming for precise action against HDAC10, which is linked to poor prognosis in neuroblastoma [85]. These efforts represent a move towards more targeted cancer therapies with the potential for fewer side effects in treating MM.
Monotherapy in MM
Wolf et al. [86] conducted a Phase II research (NCT00445068) with 38 patients with RRMM. The study used a dose of Panobinostat at 20 mg, administered three times a week, on a weekly basis within 21-day cycles. Prior to this, patients had undergone a minimum of two therapy regimens, which involved the use of an IMiD (thalidomide or lenalidomide) and bortezomib. The overall activity was deemed to be low, as seen by one partial reaction and one minimum response. Both of these responses exhibited excellent durability, lasting for 19 and 28 months, respectively. However, the trial was ended owing to insufficient efficacy. More than 80% of patients had gastrointestinal adverse events (AEs), with the bulk of these occurrences classified as grade 1–2. The most common grade 3–4 occurrences were related to blood disorders, including neutropenia, thrombocytopenia, and anaemia. Additionally, 26% of the patients reported experiencing fatigue. A Phase Ia/II dose-escalation study of oral Panobinostat was conducted on 176 patients with hematologic malignancies, including 12 with RRMM, as part of another clinical trial (NCT00621244) [87]. The doses of Panobinostat ranged from 20 to 80 mg in two different dose-escalation regimens, either administered three times per week or once every two weeks. In Phase II, the prescribed dosage for MM was 40 mg administered on a weekly basis. The maximum acceptable dose, on the other hand, was Panobinostat 60 mg given every two weeks. Coincidentally, one RRMM patient responded somewhat like adverse events, particularly gastrointestinal and hematologic AEs, were similar with those found in earlier studies. This trial confirmed overall safety and guided dosage for further monotherapy and combo treatment. In addition to Panobinostat, Vorinostat (NCT00045006), ITF2357 (NCT00792506), Entinostat (NCT00015925), Tacedinaline (NCT00005624), Domatinostat (NCT01344707) and Romidepsin (NCT00066638) were also used in monotherapy clinical trials. In summary, while Panobinostat has shown some efficacy as a monotherapy in treating MM, its clinical benefits are more pronounced and better supported when used in combination with other therapies. The management of multiple myeloma remains complex, requiring a multidisciplinary approach to optimize patient outcomes (Table 2).
Doublet combination therapy with dexamethasone
The preclinical research demonstrated the synergistic effects of HDACis in combination with bortezomib and dexamethasone in MM cell lines. Additionally, the safety data from monotherapy provided a foundation for conducting combination studies (Table 2). These trials ultimately resulted in the accelerated approval of the treatment regimen [82]. In a phase II study (NCT01720875) [88], 16 MM patients, previously treated once, received a regimen of bortezomib, dexamethasone, and vorinostat, showing an 81.3% overall response rate with 100% clinical benefit. Despite a median progression-free survival of 11.9 months and maintenance treatment with vorinostat, 75% of the participants required dose adjustments or discontinued treatment due to side effects. The findings reveal that, although toxicity and dosage reductions were challenges, this combination therapy is effective in treating relapsed myeloma. This success underscores the importance of continuing to refine HDAC inhibitor-based combinations, aiming to improve both their tolerability and efficacy for myeloma treatment. Between July 2012 and August 2015, a study (NCT01583283) enrolled 38 patients to test ricolinostat [89]. Yee et al. found ricolinostat to be mostly safe, with the best dose determined as 160 mg once daily for 21 days in a 28 day cycle, combined with two other medications. The most common side effects were mild to moderate fatigue and diarrhea. The drug effectively inhibited its target enzyme without significantly affecting other enzymes, and its effectiveness wasn’t compromised when taken with the other medications. In early assessments, 55% of patients showed a positive response to the treatment, suggesting ricolinostat could be a promising option for patients with RRMM. The studies (NCT01502085 and NCT00642954) explored a new combination therapy of vorinostat, lenalidomide, and dexamethasone for treating MM, based on promising lab research. It was a phase I trial involving patients with RRMM, aiming to find the highest dose patients could tolerate without severe side effects. The maximum dose tested was well-tolerated, with drug-related adverse events in 90% of patients and serious ones in 45%. About 47% of participants showed a partial or better response to the treatment, indicating the combination's potential effectiveness with manageable side effects [90, 91]. In a study (NCT01023308) conducted between January 2010 and February 2012 involving 768 patients with RRMM, participants were divided into two groups: one received a combination of panobinostat, bortezomib, and dexamethasone (387 patients), and the other received a placebo with bortezomib and dexamethasone (381 patients). The panobinostat group showed a significantly longer median progression-free survival of nearly 12 months compared to 8 months in the placebo group. Although overall survival rates were not conclusive, the panobinostat group had a slightly higher median overall survival at the time of analysis. The study also found a higher rate of complete or near complete response in the panobinostat group compared to the placebo group, though overall response rates (ORR) were similar. The panobinostat group experienced more serious adverse events and grade 3–4 laboratory abnormalities. The findings suggest panobinostat could be beneficial for treating this patient population, but longer follow-up is needed to assess the impact on overall survival [92]. Furthermore, more and more clinical trials show that Doublet combination therapy with dexamethasone can improve the efficacy of treatment in RRMM [93,94,95,96,97].
Combination therapy with IMiDs
Due to encouraging preclinical anti-MM action, the effectiveness of HDACis has been investigated in combination with other treatments, such as IMiDs (Table 2). Specifically, panobinostat has been used in combination with lenalidomide and dexamethasone. The Phase I clinical trial (NCT01440582) demonstrates the safety and efficacy of combining VRd (Bortezomib plus lenalidomide and dexamethasone) with a 10 mg dose of panobinostat in newly diagnosed multiple myeloma patients who are eligible for transplantation. In early testing, the lowest dose did not cause serious side effects, while a higher dose did in two patients, indicating it was too strong. Therefore, the study established the lower dose as the safest and most tolerable for patients. This combination therapy shows promise for treating newly diagnosed multiple myeloma in patients eligible for a transplant, but more extensive research is needed to confirm these findings [94]. Between July 2012 and August 2015, a study (NCT01583283) enrolled 38 patients to assess the safety and efficacy of ricolinostat in treating MM. The study identified a recommended dose of ricolinostat at 160 mg daily for future research, following two cases of significant adverse effects at a higher dosage. Common side effects included fatigue and diarrhea, but the drug demonstrated a promising ability to selectively inhibit HDAC6 without significantly impacting HDAC1, suggesting it could enhance treatments with lenalidomide and dexamethasone. Preliminary results showed a 55% response rate among participants, indicating that ricolinostat could be a safe and effective option for RRMM [89]. Moreover, the Phase I/II clinical trial (NCT01502085), and the Phase I clinical trial (NCT02569320) demonstrate that vorinostat, and AR-42 have the potential to synergize with lenalidomide and dexamethasone, hence improving their effectiveness in RRMM [89, 90, 98].
Combination therapy with conventional chemotherapy
In the 1980s, the primary therapeutic choices for MM were induction therapy utilizing alkylating agents such anthracyclines and steroids, as well as high-dose chemotherapy followed by autologous stem cell transplantation. As previously stated, the introduction of advanced medicines, including proteasome inhibitors, immunomodulatory drugs, monoclonal antibodies, and histone deacetylase inhibitors, has led to a notable enhancement in prognosis through the use of a new therapy strategy. Multiple treatment protocols including these innovative medications in different combinations have been formulated and assessed in clinical trials. Annually, the outcomes of these novel therapeutic regimens are disseminated through publication. In the context of this multifaceted contemporary landscape, conventional chemotherapeutic agents persist in retaining prominence, particularly when integrated with emerging therapeutic modalities [99]. We reviewed clinical trials of HDACis in combination with conventional chemotherapy, among them, we found only two ( NCT00744354 and NCT01394354) and were unable to track the results.
Combination therapy with novel targeted agents
As elucidated in Section “Synergy with and resistance to HDAC Inhibition”, proteasome inhibitors exhibit synergistic effects, concurrently impeding cellular proliferation and augmenting apoptosis in MM cells [77]. We found that Bortezomib, Carfilzomib, and Ixazomib were predominantly used in clinical trials (Table 2). Bortezomib is a specific and reversible inhibitor of proteasomes. It works by directly attaching to the β1 and β5 subunits of the catalytic 20S complex, hence preventing chymotrypsin-like activity85. Treatment with bortezomib enhances the bone marrow microenvironment by stimulating the development of osteoblasts and decreasing the activity of osteoclasts that depend on the receptor activator of NF-κB (RANKL). This effect is achieved through the activation of NF-κB, p38, and AP-1 pathways, and is influenced by the dosage of bortezomib [100]. The Phase I clinical trial study (NCT00858234) revealed that the most predominant adverse events were thrombocytopenia, leukopenia, neutropenia, diarrhea, nausea, decreased appetite, and vomiting [101]. Another Phase II clinical trial study (NCT01720875) showed that despite observed toxicity and dose reductions, which demonstrated that the combination of vorinostat, bortezomib, and dexamethasone was effective and had good response rates in relapsed myeloma, suggesting further optimization of HDAC inhibitor-based combination therapy for myeloid Tumor to improve tolerance and enhance efficacy [88]. However, the findings from the Phase III clinical trial study (NCT01023308) revealed that panobinostat was linked to a marginal improvement in overall survival when juxtaposed with the combination of bortezomib and dexamethasone placebo. Optimized regimens have the potential to prolong therapeutic duration and enhance patient outcomes; however, additional trials are requisite to corroborate these observations [102]. Carfilzomib is a second-generation drug that inhibits proteasomes and is mostly used for patients with multiple myeloma who have not responded to previous treatments or have experienced a relapse. Carfilzomib inhibits chymotrypsin-like activity by attaching to the catalytic 20S proteasome. Unlike bortezomib, this interaction is permanent and more specific, which accounts for certain side effects that are absent in bortezomib therapy. The usual route of administration for carfilzomib is intravenous, with a frequency of twice per week for a period of three weeks. The recommended dose is 27 mg/m2. Carfilzomib's molecular mode of action is similar to that of bortezomib, which includes inducing apoptosis and improving bone injury. Carfilzomib side effects may include hypertension, cardiotoxicity, thrombocytopenia, hypocalcemia, and gastrointestinal problems [103,104,105]. Ixazomib is an innovative proteasome inhibitor used orally at a dosage of 4 mg once per week. It functions by obstructing the enzyme in MM cells, impeding their capacity to proliferate and endure [106], nevertheless, only one clinical trial (NCT02057640) has been completed so far, but no definite results can be obtained. Common adverse effects of ixazomib encompass thrombocytopenia, edoema in the lower extremities, peripheral neuropathy (resulting in weakness, numbness, and pain in the hands and feet), gastrointestinal disturbances such as diarrhoea, constipation, nausea, vomiting, and back pain [107].
The clinical safety of HDAC inhibitors in MM
There is an overexpression of HDAC in cancer cells, and the use of HDACis has been shown to enhance the outcomes of individuals who have been diagnosed with haematological malignancies include T-cell lymphomas and multiple myeloma. Five drugs were previously approved in different national jurisdictions, namely belinostat, chidamide, romidepsin, vorinostat and Panobinostat. It is worth noting that Secura Bio, Inc. requested the withdrawal of FDA approval for Panobinostat in 2021, citing the impracticality of conducting necessary postmarketing trials. Subsequently, in March 2022, the FDA withdrew panobinostat from the US market [108]. However, despite its removal from the US market, panobinostat continues to be employed in Europe as a viable treatment option for patients whose diseases have advanced after undergoing standard therapies. These drugs have been linked to a variety of severe and/or significant side responses, including myelosuppression, diarrhea, hepatic effects and various cardiac effects [109]. In this section, we have selected the most important side effects for review (Table 2, Fig. 5a).
a HDAC inhibitors have been linked to a variety of severe and/or significant side responses; b Distribution of grade 3/4 toxicities in clinical trials (Table 2) of histone deacetylase inhibitors. Figure created with BioRender.com
Myelosuppression
From Fig. 5b, we can see five medication clinical studies revealed 3 common side effects including thrombocytopenia, neutropenia and anemia. Thrombocytopenia is common and can result in bleeding, although neutropenia is frequently a sign of infection. These side effects may be sufficiently serious to necessitate the transfusions of blood and/or the administration of granulocyte colony-stimulating agents. To reduce the clinical effects, blood counts should be checked on a frequent basis and dose modifications done as needed; nonetheless, if toxicities of grade 3 or 4 return after reducing the dosage, treatment should be discontinued. In the aggregate, the majority of clinical trials have demonstrated myelosuppression as a noteworthy side effect, warranting careful consideration.
Cardiac effects
The ether-a-go-go (hERG) channel in humans is responsible for controlling the duration of ventricular repolarization, which is visually represented as the QT interval on the surface electrocardiogram (ECG). Drugs that inhibit or reduce the function or expression of hERG channels lead to an elongation of the QT interval. Torsades de pointes (TdP), a potentially fatal ventricular tachyarrhythmia, can occur when the QTc interval is extended due to excessive duration or the presence of risk factors. Schiattarella et al. [114] discovered that HDACis elicit typical albeit insignificant cardiac side effects, mostly manifesting as ECG abnormalities such as ST-T abnormalities and QT prolongation. This conclusion was drawn after analysing 62 trials with a collective patient population of 3268 individuals. The most common electrocardiographic abnormalities seen in patients treated with romidepsin (25.3%) and panobinostat (22.3%) were ST depression and/or T wave inversion, which accounted for 14.5% of the patients. QTc prolongation was observed in 4.4% of the total 3268 individuals. This percentage was lower than the rates reported for belinostat (12.2%), panobinostat (4.3%), vorinostat (3.4%), and romidepsin (3.3%). Ventricular tachycardia was observed in 0.6% (21/3268) of the entire study group, with the majority of cases occurring after the administration of romidepsin (19/944, 2.0%) or panobinostat (2/1047, 0.2%). Treated persons exhibited atrial fibrillation, whereas 13 individuals (0.4%) reported experiencing atrial fibrillation. This was mostly detected in vorinostat (8/888) and belinostat (2/221) patients. [109].
Gastrointestinal effects
From Fig. 5b, It is readily apparent that gastrointestinal side effects are also one of the main side effects. A comprehensive analysis of clinical studies has indicated that the use of antiemetic and antidiarrheal medications, together with fluid and electrolyte supplements, may be necessary to manage symptoms of nausea, vomiting, and diarrhoea following therapy with any of the five treatments (Belinostat, Panobinostat, Romidepsin, Vorinostat, Chidamide). Panobinostat has the potential to induce severe diarrhoea (grade 3 or 4) in 25% of people on therapy, which may necessitate a decrease in dosage or complete cessation of the treatment.
Hepatic effects
Complications arising from therapeutic interventions with romidepsin, panobinostat, belinostat, and chidamide have been systematically documented, frequently manifesting as elevated blood transaminases and/or bilirubin levels. Notably, vorinostat has not been correlated with any hepatic side effects. Despite a comprehensive literature search yielding no reports of clinically significant hepatotoxicity associated with these agents, a pivotal event in a belinostat clinical study, marked by a treatment-related fatality linked to hepatic failure, prompted the FDA to modify the approved label for belinostat. The revised label underscores the potential for fatal toxicity and advocates for pre-treatment and cyclical liver function test monitoring, it is particularly important. In the event of discernible hepatic impairment, a judicious course of action involves either dose adjustment or discontinuation, contingent upon the severity of the observed hepatotoxicity [109].
Agent‐specific adverse effects
Table 3 concisely summarizes distinct extra adverse effects linked to various HDACis that set them apart from the wider class. The infections observed with belinostat and romidepsin are most likely caused by neutropenia, while cases of hemorrhage associated with panobinostat and pericardial effusion after chidamide therapy are coupled with thrombocytopenia created by these drugs. Increased levels of creatine phosphokinase in conjunction with chidamide and the presence of cardiac ischemia with panobinostat may indicate the potential of these particular drugs to cause harm to the myocardium.
Tumor lysis syndrome, a phenomenon that often occurs in the early stages of treatment and is frequently associated with belinostat and romidepsin, is commonly seen in patients with advanced-stage disease and/or high levels of hematological tumor burden. This syndrome is a metabolic disorder that can be life-threatening. It is characterized by high levels of uric acid, potassium, and phosphate, and low levels of calcium. This condition not only causes gastrointestinal symptoms like nausea and vomiting, but also leads to serious complications such as acute uric acid nephropathy, acute kidney failure, seizures, cardiac arrhythmias, and even death.
However, the clarification of prothrombotic and hyperglycemic effects associated with vorinostat poses challenges, as these phenomena may be attributed to factors such as the investigational drug itself, the characteristics of the patient population under scrutiny, or concurrent therapeutic interventions.
HDACis are a hopeful treatment for MM, aiming to correct cancer-specific gene patterns. Yet, their effectiveness is complicated by the fact that MM patients differ greatly in their genetic makeup, leading to varied responses to these drugs. This variation highlights the need for identifying markers that can predict who will benefit most from these treatments. Additionally, the side effects of HDAC inhibitors can vary from mild to severe, making it crucial to manage these carefully to ensure patients truly benefit from the treatment. Looking ahead, research is zeroing in on finding these predictive markers, creating drug combinations that work better and have fewer side effects, understanding why some patients develop resistance, and paying closer attention to how treatments impact patients' quality of life. This approach aims to make HDACis treatment more personalized, maximizing benefits while reducing drawbacks for MM patients.
Challenges in the combined use of HDACis and immunotherapy
Immunological evasion in cancer is a critical process that involves the expression of immunological checkpoints, including PD-1, PD-L1, and CTLA-4. Inhibiting these checkpoints is an effective approach for treating cancer. Multiple studies demonstrate that STAT3 is involved in directly or indirectly controlling these immunological checkpoint molecules [115,116,117,118]. Notably, HDAC6 emerges as a significant regulator of the STAT3 pathway [119,120,121]. Lienlaf et al. provided evidence that HDAC6 plays a role in the body's defence against tumours in melanoma by affecting the STAT3-PD-L1 pathway [121], this discovery was further supported by Keremu et al. in their study on osteosarcomas [120]. Elevated production of HDAC6 leads to the phosphorylation of STAT3 and its translocation into the nucleus, without causing any changes in acetylation of its co-protein PP2A. Phosphorylated STAT3 and HDAC6 coexist in the nucleus and target the PD-L1 promoter, resulting in the activation of transcription and the enhancement of PD-L1 gene expression [19, 121, 122] (Fig. 6). Notably, preclinical studies indicate that a combination of HDAC6 inhibitor and PD-L1 antibody enhances γδ T cell antitumor functions [123]. This underscores the potential of targeting the HDAC6 inhibition-PD-1/PD-L1 pathway as a novel approach to augment cancer immunotherapy. The concurrent use of pan-HDACis and cytokine-induced killer (CIK) cell treatment [124], which has demonstrated efficacy in preclinical multiple myeloma models [125, 126], provides additional validation for this idea. The presence of specific HDAC6 inhibitors such as ACY-1215, tubastatin A, and ricolinostat presents a potential opportunity for their use, either alone or in conjunction with CIK cell therapy, in medical environments. This offers a hopeful pathway for the treatment of cancer.
Mechanistic illustration of HDAC6 in STAT3-PD-L1 pathway: When HDAC6 levels are high, STAT3 accumulates in a phosphorylated form, reducing the interaction between STAT3 and PP2A. After entering the nucleus, pSTAT3 and HDAC6 bind to the PD-L1 promoter, promoting PD-L1 expression. Figure created with BioRender.com
The combined use of HDACis and immunotherapy holds promise for enhancing cancer treatment outcomes, but it also presents several challenges. (1) Limited understanding of mechanisms: The mechanisms through which HDACis interact with the immune system and modulate responses to immunotherapy are not fully understood. Better insights into these mechanisms are crucial for optimizing combination therapies. (2) Dose-dependent effects: The effects of HDACis can be dose-dependent, and finding the right balance is critical. High doses of HDACis may have immunosuppressive effects, counteracting the desired immune activation promoted by immunotherapy. (3) Off-target effects: HDACis can affect various cellular processes beyond histone acetylation, potentially leading to off-target effects [127]. Understanding and minimizing these off-target effects is important to avoid unintended consequences on immune cells and overall treatment efficacy. (4) Patient heterogeneity: Patient responses to HDACis and immunotherapy can vary significantly. Identifying biomarkers to predict which patients are more likely to benefit from the combination is a challenge. Personalized medicine approaches may be essential for optimizing treatment strategies. (5) Toxicity and side effects: HDACis can be associated with toxicities and side effects, including hematological toxicity and fatigue. Combining these agents with immunotherapy may exacerbate these issues, and managing the overall toxicity profile is crucial for patient safety and adherence. (6) Resistance development: Tumor cells can develop resistance to HDACis and immunotherapy. Understanding the mechanisms of resistance and developing strategies to overcome or prevent resistance is essential for long-term treatment success. (7) Optimal sequence and timing: Determining the optimal sequence and timing of HDACis and immunotherapy is challenging. The order in which these treatments are administered can impact their effectiveness, and finding the right schedule is critical for maximizing therapeutic benefits. (8) Synergistic vs. antagonistic effects: Achieving synergistic effects between HDACis and immunotherapy is the goal, but there is a risk of antagonistic interactions. Careful preclinical and clinical studies are needed to assess the compatibility of these treatments and avoid potential counteractive effects. (9) Clinical trial design: Designing clinical trials to effectively evaluate the safety and efficacy of combined HDACis and immunotherapy is challenging. Robust study designs, appropriate patient selection, and relevant endpoints are necessary to draw meaningful conclusions. (10) Regulatory hurdles: Regulatory approval for combination therapies can be complex. Coordinating the approval process for two or more agents may require additional evidence of safety and efficacy, and navigating regulatory pathways is a significant challenge. Addressing these challenges will require collaborative efforts from researchers, clinicians, and regulatory authorities to advance the understanding and implementation of combined HDACis and immunotherapy for cancer treatment. Ongoing research and clinical trials are essential to further elucidate the complexities and refine treatment strategies.
Conclusions and future directions
In the past decade, the landscape of MM treatment has undergone significant transformation, largely due to advancements in HDACis, immunomodulatory drugs, and other novel therapies. The incorporation of HDACis into the therapeutic arsenal has expanded the spectrum of effective treatment options, leading to increased patient longevity and improved quality of life. Presently, a wide array of potent therapy regimens that leverage HDACis as a backbone is available, indicating a pivotal shift in MM management strategies. Moreover, ongoing research is exploring innovative approaches, such as the integration of HDACis with monoclonal antibodies, targeted medicines, and cellular immunotherapy, aiming to further enhance treatment efficacy and patient outcomes.
A notable area of progress involves the synergistic combination of HDACis with anti-CD38 monoclonal antibodies, such as daratumumab, which received FDA approval in November 2015. For example, the combination of daratumumab with bortezomib and dexamethasone improved progression-free survival in patients with RRMM compared to just bortezomib and dexamethasone [128]. Panobinostat, MS-275, and ACY1215 enhance CD38 expression, thereby increasing daratumumab's anti-myeloma effectiveness [129, 130]. In general, it has shown promising results in vitro, underscoring the potential for HDACis to improve the efficacy of established therapies in both initial and relapse settings. Despite these advancements, the specific molecular mechanisms underlying the enhanced anti-tumor activity of these combination therapies remain to be fully elucidated. Furthermore, the development of isoform and/or class-selective HDACis presents a promising avenue to mitigate the adverse effects commonly associated with non-selective HDACis, while maintaining robust anti-tumor efficacy.
The ongoing challenge of addressing toxicity, resistance mechanisms, and the absence of reliable biomarkers for predicting HDACis response underscores the need for continued research. Efforts to identify predictive markers, understand the molecular basis of HDACis action, and explore novel therapeutic combinations are essential for optimizing MM treatment. As research progresses, it is anticipated that the targeted application of HDACis, either as monotherapies or in combination with other agents, will significantly advance the treatment paradigm for MM, offering patients more personalized and effective treatment options [131, 132]. This integration of novel HDACis-based therapies into MM treatment regimens not only reflects the current progress but also sets the stage for future advancements that promise to further improve patient survival and quality of life.
Availability of data and materials
Not applicable.
Abbreviations
- HDACs:
-
Histone deacetylases
- HDACis:
-
Histone deacetylase inhibitors
- MM:
-
Multiple myeloma
- IMiDs:
-
Immunomodulatory drugs
- ASCT:
-
Autologous stem cell transplantation
- mAbs:
-
Monoclonal antibodies
- ADC:
-
Antibody–drug conjugates
- BiTE:
-
Bispecific T-cell engagers
- CAR-T:
-
Chimeric antigen-T-cell therapy
- FDA:
-
The United States Food and Drug Administration
- RRMM:
-
Relapsed/refractory multiple myeloma
- CTCL:
-
Cutaneous T-cell lymphoma
- CMML:
-
Chronic myelomonocytic leukemia
- HIV:
-
Human immunodeficiency virus
- AIDS:
-
Acquired immunodeficiency syndrome
- DLBCL:
-
Diffuse large B-cell lymphoma
- PTCL:
-
Peripheral T-cell lymphoma
- NSCC:
-
Non-small cell lung carcinoma
- HCC:
-
Hepatocellular carcinoma
- ATLL:
-
Adult T-cell leukemia-lymphoma
- hERG:
-
The human ether-a-go-go
- ECG:
-
Electrocardiogram
- tdP:
-
Torsades de pointes
- CIK:
-
Cytokine-induced killer
References
Cowan AJ, Green DJ, Kwok M, Lee S, Coffey DG, Holmberg LA, Tuazon S, Gopal AK, Libby EN. Diagnosis and management of multiple myeloma: a review. JAMA. 2022;327(5):464–77.
Padala SA, Barsouk A, Barsouk A, Rawla P, Vakiti A, Kolhe R, Kota V, Ajebo GH. Epidemiology, staging, and management of multiple myeloma. Med Sci. 2021;9(1):3.
Rajkumar SV. Multiple myeloma: 2022 update on diagnosis, risk stratification, and management. Am J Hematol. 2022;97(8):1086–107.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33.
Cowan AJ, Allen C, Barac A, Basaleem H, Bensenor I, Curado MP, Foreman K, Gupta R, Harvey J, Hosgood HD, et al. Global burden of multiple myeloma: a systematic analysis for the global burden of disease study 2016. JAMA Oncol. 2018;4(9):1221–7.
Abramson HN. Immunotherapy of multiple myeloma: promise and challenges. Immunotargets Ther. 2021;10:343–71.
Al Hamed R, Bazarbachi AH, Malard F, Harousseau JL, Mohty M. Current status of autologous stem cell transplantation for multiple myeloma. Blood Cancer J. 2019;9(4):44.
Mikhael J, Ismaila N, Cheung MC, Costello C, Dhodapkar MV, Kumar S, Lacy M, Lipe B, Little RF, Nikonova A, et al. Treatment of multiple myeloma: ASCO and CCO joint clinical practice guideline. J Clin Oncol. 2019;37(14):1228–63.
Soekojo CY, Chng WJ. Treatment horizon in multiple myeloma. Eur J Haematol. 2022;109(5):425–40.
Zhang X, Zhang H, Lan H, Wu J, Xiao Y. CAR-T cell therapy in multiple myeloma: current limitations and potential strategies. Front Immunol. 2023;14:1101495.
Holstein SA, Grant SJ, Wildes TM. Chimeric antigen receptor T-cell and bispecific antibody therapy in multiple myeloma: moving into the future. J Clin Oncol. 2023;41(27):4416–29.
Tanenbaum B, Miett T, Patel SA. The emerging therapeutic landscape of relapsed/refractory multiple myeloma. Ann Hematol. 2023;102(1):1–11.
Cengiz Seval G, Beksac M. A comparative safety review of histone deacetylase inhibitors for the treatment of myeloma. Expert Opin Drug Saf. 2019;18(7):563–71.
Harada T, Hideshima T, Anderson KC. Histone deacetylase inhibitors in multiple myeloma: from bench to bedside. Int J Hematol. 2016;104(3):300–9.
Yoon S, Eom GH. HDAC and HDAC inhibitor: from cancer to cardiovascular diseases. Chonnam Med J. 2016;52(1):1–11.
Wang P, Wang Z, Liu J. Role of HDACs in normal and malignant hematopoiesis. Mol Cancer. 2020;19(1):5.
Dasko M, de Pascual-Teresa B, Ortin I, Ramos A. HDAC inhibitors: innovative strategies for their design and applications. Molecules. 2022;27(3):715.
Fan W, Zhang L, Jiang Q, Song W, Yan F, Zhang L. Histone deacetylase inhibitor based prodrugs. Eur J Med Chem. 2020;203: 112628.
Pu J, Sharma A, Hou J, Schmidt-Wolf IG. Histone deacetylase 6: at the interface of cancer and neurodegeneration. Epigenomics. 2023;15:1195–203.
Patel P, Wahan SK, Vishakha S, Kurmi BD, Gupta GD, Rajak H, Asati V. Recent progress in histone deacetylase (HDAC) 1 inhibitors as anticancer agent. Curr Cancer Drug Targets. 2022;23(1):47–70.
Porter NJ, Christianson DW. Structure, mechanism, and inhibition of the zinc-dependent histone deacetylases. Curr Opin Struct Biol. 2019;59:9–18.
Di Giorgio E, Brancolini C. Regulation of class IIa HDAC activities: it is not only matter of subcellular localization. Epigenomics. 2016;8(2):251–69.
Liu L, Dong L, Bourguet E, Fairlie DP. Targeting class IIa HDACs: insights from phenotypes and inhibitors. Curr Med Chem. 2021;28(42):8628–72.
Kee HJ, Kim I, Jeong MH. Zinc-dependent histone deacetylases: potential therapeutic targets for arterial hypertension. Biochem Pharmacol. 2022;202: 115111.
Cheng F, Zheng B, Wang J, Zhao G, Yao Z, Niu Z, He W. Histone deacetylase 10, a potential epigenetic target for therapy. Biosci Rep. 2021;41(6):BSR20210462.
Rajabi N, Galleano I, Madsen AS, Olsen CA. Targeting sirtuins: substrate specificity and inhibitor design. Prog Mol Biol Transl Sci. 2018;154:25–69.
Chen H, Xie C, Chen Q, Zhuang S. HDAC11, an emerging therapeutic target for metabolic disorders. Front Endocrinol. 2022;13: 989305.
Ropero S, Esteller M. The role of histone deacetylases (HDACs) in human cancer. Mol Oncol. 2007;1(1):19–25.
Falkenberg KJ, Johnstone RW. Histone deacetylases and their inhibitors in cancer, neurological diseases and immune disorders. Nat Rev Drug Discov. 2014;13(9):673–91.
Ramaiah MJ, Tangutur AD, Manyam RR. Epigenetic modulation and understanding of HDAC inhibitors in cancer therapy. Life Sci. 2021;277: 119504.
Patra S, Panigrahi DP, Praharaj PP, Bhol CS, Mahapatra KK, Mishra SR, Behera BP, Jena M, Bhutia SK. Dysregulation of histone deacetylases in carcinogenesis and tumor progression: a possible link to apoptosis and autophagy. Cell Mol Life Sci. 2019;76(17):3263–82.
Lin Y, Jing X, Chen Z, Pan X, Xu D, Yu X, Zhong F, Zhao L, Yang C, Wang B, et al. Histone deacetylase-mediated tumor microenvironment characteristics and synergistic immunotherapy in gastric cancer. Theranostics. 2023;13(13):4574–600.
Aventaggiato M, Vernucci E, Barreca F, Russo MA, Tafani M. Sirtuins’ control of autophagy and mitophagy in cancer. Pharmacol Ther. 2021;221: 107748.
Ell B, Kang Y. Transcriptional control of cancer metastasis. Trends Cell Biol. 2013;23(12):603–11.
Li M, van Esch B, Wagenaar GTM, Garssen J, Folkerts G, Henricks PAJ. Pro- and anti-inflammatory effects of short chain fatty acids on immune and endothelial cells. Eur J Pharmacol. 2018;831:52–9.
Cross D, Drury R, Hill J, Pollard AJ. Epigenetics in sepsis: understanding its role in endothelial dysfunction, immunosuppression, and potential therapeutics. Front Immunol. 2019;10:1363.
Xue X, Zhang Y, Liao Y, Sun D, Li L, Liu Y, Wang Y, Jiang W, Zhang J, Luan Y, et al. Design, synthesis and biological evaluation of dual HDAC and VEGFR inhibitors as multitargeted anticancer agents. Invest New Drugs. 2022;40(1):10–20.
Witt O, Deubzer HE, Milde T, Oehme I. HDAC family: what are the cancer relevant targets? Cancer Lett. 2009;277(1):8–21.
Kuo YH, Qi J, Cook GJ. Regain control of p53: Targeting leukemia stem cells by isoform-specific HDAC inhibition. Exp Hematol. 2016;44(5):315–21.
Mrakovcic M, Bohner L, Hanisch M, Frohlich LF. Epigenetic targeting of autophagy via HDAC inhibition in tumor cells: role of p53. Int J Mol Sci. 2018;19(12):3952.
Wagner T, Brand P, Heinzel T, Kramer OH. Histone deacetylase 2 controls p53 and is a critical factor in tumorigenesis. Biochim Biophys Acta. 2014;1846(2):524–38.
Chen J, Zhao KN, Vitetta L. Effects of intestinal microbial(-)elaborated butyrate on oncogenic signaling pathways. Nutrients. 2019;11(5):1026.
Chae HY, Park SY, Jha S, Gupta SK, Kim M, Ha E, Seo YH. Design, synthesis, and biological evalution of bifunctional inhibitors against Hsp90-HDAC6 interplay. Eur J Med Chem. 2022;240: 114582.
Leus NG, Zwinderman MR, Dekker FJ. Histone deacetylase 3 (HDAC 3) as emerging drug target in NF-kappaB-mediated inflammation. Curr Opin Chem Biol. 2016;33:160–8.
Zhao C, Dong H, Xu Q, Zhang Y. Histone deacetylase (HDAC) inhibitors in cancer: a patent review (2017-present). Expert Opin Ther Pat. 2020;30(4):263–74.
Vrabel D, Pour L, Sevcikova S. The impact of NF-kappaB signaling on pathogenesis and current treatment strategies in multiple myeloma. Blood Rev. 2019;34:56–66.
Wong AH, Shin EM, Tergaonkar V, Chng WJ. Targeting NF-kappaB signaling for multiple myeloma. Cancers. 2020;12(8):2203.
Hu J, Hu WX. Targeting signaling pathways in multiple myeloma: pathogenesis and implication for treatments. Cancer Lett. 2018;414:214–21.
Ramakrishnan V, Kumar S. PI3K/AKT/mTOR pathway in multiple myeloma: from basic biology to clinical promise. Leuk Lymphoma. 2018;59(11):2524–34.
Al-Odat OS, Guirguis DA, Schmalbach NK, Yao G, Budak-Alpdogan T, Jonnalagadda SC, Pandey MK. Autophagy and apoptosis: current challenges of treatment and drug resistance in multiple myeloma. Int J Mol Sci. 2022;24(1):644.
Hamedi KR, Harmon KA, Goodwin RL, Arce S. Autophagy and the bone marrow microenvironment: a review of protective factors in the development and maintenance of multiple myeloma. Front Immunol. 2022;13: 889954.
Mo H, Zhang R, Chen Y, Li S, Wang Y, Zou W, Lin Q, Zhao DG, Du Y, Zhang K, et al. Synthesis and anticancer activity of novel histone deacetylase inhibitors that inhibit autophagy and induce apoptosis. Eur J Med Chem. 2022;243: 114705.
Koeneke E, Witt O, Oehme I. HDAC family members intertwined in the regulation of autophagy: a druggable vulnerability in aggressive tumor entities. Cells. 2015;4(2):135–68.
Zhang J, Zhong Q. Histone deacetylase inhibitors and cell death. Cell Mol Life Sci. 2014;71(20):3885–901.
Desantis V, Saltarella I, Lamanuzzi A, Mariggio MA, Racanelli V, Vacca A, Frassanito MA. Autophagy: a new mechanism of prosurvival and drug resistance in multiple myeloma. Transl Oncol. 2018;11(6):1350–7.
Eckschlager T, Plch J, Stiborova M, Hrabeta J. Histone deacetylase inhibitors as anticancer drugs. Int J Mol Sci. 2017;18(7):1414.
McClure JJ, Li X, Chou CJ. Advances and challenges of HDAC inhibitors in cancer therapeutics. Adv Cancer Res. 2018;138:183–211.
Ho TCS, Chan AHY, Ganesan A. Thirty years of HDAC inhibitors: 2020 insight and hindsight. J Med Chem. 2020;63(21):12460–84.
Eleutherakis-Papaiakovou E, Kanellias N, Kastritis E, Gavriatopoulou M, Terpos E, Dimopoulos MA. Efficacy of panobinostat for the treatment of multiple myeloma. J Oncol. 2020;2020:7131802.
Ashjian E, Redic K. Multiple myeloma: updates for pharmacists in the treatment of relapsed and refractory disease. J Oncol Pharm Pract. 2016;22(2):289–302.
Ganai SA. Histone deacetylase inhibitor givinostat: the small-molecule with promising activity against therapeutically challenging haematological malignancies. J Chemother. 2016;28(4):247–54.
Hideshima T, Chauhan D, Podar K, Schlossman RL, Richardson P, Anderson KC. Novel therapies targeting the myeloma cell and its bone marrow microenvironment. Semin Oncol. 2001;28(6):607–12.
Ocio EM, San Miguel JF. The DAC system and associations with multiple myeloma. Invest New Drugs. 2010;28(Suppl 1):S28-35.
Teoh PJ, Chng WJ. p53 abnormalities and potential therapeutic targeting in multiple myeloma. Biomed Res Int. 2014;2014: 717919.
John L, Krauth MT, Podar K, Raab MS. Pathway-directed therapy in multiple myeloma. Cancers. 2021;13(7):1668.
Liu T, Wu Z, He Y, Xiao Y, Xia C. Single and dual target inhibitors based on Bcl-2: promising anti-tumor agents for cancer therapy. Eur J Med Chem. 2020;201: 112446.
Kumar V, Kundu S, Singh A, Singh S. Understanding the role of histone deacetylase and their inhibitors in neurodegenerative disorders: current targets and future perspective. Curr Neuropharmacol. 2022;20(1):158–78.
Pu J, Liu T, Sharma A, Schmidt-Wolf IGH. Balancing the interplay of histone deacetylases and non-coding genomes: a step closer to understand the landscape of cancer treatment. BMC Med Genomics. 2023;16(1):295.
Lane AA, Chabner BA. Histone deacetylase inhibitors in cancer therapy. J Clin Oncol. 2009;27(32):5459–68.
Al-Janadi A, Chandana SR, Conley BA. Histone deacetylation : an attractive target for cancer therapy? Drugs R D. 2008;9(6):369–83.
Bonanni D, Citarella A, Moi D, Pinzi L, Bergamini E, Rastelli G. Dual targeting strategies on histone deacetylase 6 (HDAC6) and heat shock protein 90 (Hsp90). Curr Med Chem. 2022;29(9):1474–502.
Hideshima T, Richardson PG, Anderson KC. Mechanism of action of proteasome inhibitors and deacetylase inhibitors and the biological basis of synergy in multiple myeloma. Mol Cancer Ther. 2011;10(11):2034–42.
San-Miguel JF, Einsele H, Moreau P. The role of panobinostat plus bortezomib and dexamethasone in treating relapsed or relapsed and refractory multiple myeloma: a european perspective. Adv Ther. 2016;33(11):1896–920.
Richardson PG, Laubach JP, Lonial S. Correction to: Panobinostat: a novel pan-deacetylase inhibitor for the treatment of relapsed or relapsed and refractory multiple myeloma. Expert Rev Anticancer Ther. 2015;15(9):1121.
Tzogani K, Hennik PV, Walsh I, De Graeff P, Folin A, Sjoberg J, Salmonson T, Bergh J, Laane E, Ludwig H, et al. EMA Review of Panobinostat (Farydak) for the treatment of adult patients with relapsed and/or refractory multiple myeloma. Oncologist. 2018;23(7):870.
Chhabra S. Novel proteasome inhibitors and histone deacetylase inhibitors: progress in myeloma therapeutics. Pharmaceuticals. 2017;10(2):40.
Afifi S, Michael A, Azimi M, Rodriguez M, Lendvai N, Landgren O. Role of histone deacetylase inhibitors in relapsed refractory multiple myeloma: a focus on vorinostat and panobinostat. Pharmacotherapy. 2015;35(12):1173–88.
Simms-Waldrip T, Rodriguez-Gonzalez A, Lin T, Ikeda AK, Fu C, Sakamoto KM. The aggresome pathway as a target for therapy in hematologic malignancies. Mol Genet Metab. 2008;94(3):283–6.
Kikuchi J, Wada T, Shimizu R, Izumi T, Akutsu M, Mitsunaga K, Noborio-Hatano K, Nobuyoshi M, Ozawa K, Kano Y, et al. Histone deacetylases are critical targets of bortezomib-induced cytotoxicity in multiple myeloma. Blood. 2010;116(3):406–17.
Ocio EM, Vilanova D, Atadja P, Maiso P, Crusoe E, Fernandez-Lazaro D, Garayoa M, San-Segundo L, Hernandez-Iglesias T, de Alava E, et al. In vitro and in vivo rationale for the triple combination of panobinostat (LBH589) and dexamethasone with either bortezomib or lenalidomide in multiple myeloma. Haematologica. 2010;95(5):794–803.
Haney SL, Allen C, Varney ML, Dykstra KM, Falcone ER, Colligan SH, Hu Q, Aldridge AM, Wright DL, Wiemer AJ, et al. Novel tropolones induce the unfolded protein response pathway and apoptosis in multiple myeloma cells. Oncotarget. 2017;8(44):76085–98.
Catley L, Weisberg E, Kiziltepe T, Tai YT, Hideshima T, Neri P, Tassone P, Atadja P, Chauhan D, Munshi NC, et al. Aggresome induction by proteasome inhibitor bortezomib and alpha-tubulin hyperacetylation by tubulin deacetylase (TDAC) inhibitor LBH589 are synergistic in myeloma cells. Blood. 2006;108(10):3441–9.
West AC, Johnstone RW. New and emerging HDAC inhibitors for cancer treatment. J Clin Invest. 2014;124(1):30–9.
Chen Z, Yang X, Chen Z, Li M, Wang W, Yang R, Wang Z, Ma Y, Xu Y, Ao S, et al. A new histone deacetylase inhibitor remodels the tumor microenvironment by deletion of polymorphonuclear myeloid-derived suppressor cells and sensitizes prostate cancer to immunotherapy. BMC Med. 2023;21(1):402.
Pojani E, Barlocco D. Selective inhibitors of histone deacetylase 10 (HDAC-10). Curr Med Chem. 2022;29(13):2306–21.
Wolf JL, Siegel D, Goldschmidt H, Hazell K, Bourquelot PM, Bengoudifa BR, Matous J, Vij R, de Magalhaes-Silverman M, Abonour R, et al. Phase II trial of the pan-deacetylase inhibitor panobinostat as a single agent in advanced relapsed/refractory multiple myeloma. Leuk Lymphoma. 2012;53(9):1820–3.
DeAngelo DJ, Spencer A, Bhalla KN, Prince HM, Fischer T, Kindler T, Giles FJ, Scott JW, Parker K, Liu A, et al. Phase Ia/II, two-arm, open-label, dose-escalation study of oral panobinostat administered via two dosing schedules in patients with advanced hematologic malignancies. Leukemia. 2013;27(8):1628–36.
Brown S, Pawlyn C, Tillotson AL, Sherratt D, Flanagan L, Low E, Morgan GJ, Williams C, Kaiser M, Davies FE, et al. Bortezomib, vorinostat, and dexamethasone combination therapy in relapsed myeloma: results of the phase 2 MUK four trial. Clin Lymphoma Myeloma Leuk. 2021;21(3):154-161 e153.
Yee AJ, Bensinger WI, Supko JG, Voorhees PM, Berdeja JG, Richardson PG, Libby EN, Wallace EE, Birrer NE, Burke JN, et al. Ricolinostat plus lenalidomide, and dexamethasone in relapsed or refractory multiple myeloma: a multicentre phase 1b trial. Lancet Oncol. 2016;17(11):1569–78.
Durie BG, Harousseau JL, Miguel JS, Blade J, Barlogie B, Anderson K, Gertz M, Dimopoulos M, Westin J, Sonneveld P, et al. International uniform response criteria for multiple myeloma. Leukemia. 2006;20(9):1467–73.
Siegel DS, Richardson P, Dimopoulos M, Moreau P, Mitsiades C, Weber D, Houp J, Gause C, Vuocolo S, Eid J, et al. Vorinostat in combination with lenalidomide and dexamethasone in patients with relapsed or refractory multiple myeloma. Blood Cancer J. 2014;4(2): e182.
San-Miguel JF, Hungria VT, Yoon SS, Beksac M, Dimopoulos MA, Elghandour A, Jedrzejczak WW, Gunther A, Nakorn TN, Siritanaratkul N, et al. Panobinostat plus bortezomib and dexamethasone versus placebo plus bortezomib and dexamethasone in patients with relapsed or relapsed and refractory multiple myeloma: a multicentre, randomised, double-blind phase 3 trial. Lancet Oncol. 2014;15(11):1195–206.
Suzuki K, Sunami K, Matsumoto M, Maki A, Shimada F, Suzuki K, Shimizu K. Phase II, multicenter, single-arm, open-label study to evaluate the efficacy and safety of panobinostat in combination with bortezomib and dexamethasone in japanese patients with relapsed or relapsed-and-refractory multiple myeloma. Acta Haematol. 2021;144(3):264–74.
Manasanch EE, Shah JJ, Lee HC, Weber DM, Thomas SK, Amini B, Feng L, Berkova Z, Hildebrandt M, Orlowski RZ. Bortezomib, lenalidomide, and dexamethasone with panobinostat for front-line treatment of patients with multiple myeloma who are eligible for transplantation: a phase 1 trial. Lancet Haematol. 2018;5(12):e628–40.
Laubach JP, Schjesvold F, Mariz M, Dimopoulos MA, Lech-Maranda E, Spicka I, Hungria VTM, Shelekhova T, Abdo A, Jacobasch L, et al. Efficacy and safety of oral panobinostat plus subcutaneous bortezomib and oral dexamethasone in patients with relapsed or relapsed and refractory multiple myeloma (PANORAMA 3): an open-label, randomised, phase 2 study. Lancet Oncol. 2021;22(1):142–54.
Richardson PG, Schlossman RL, Alsina M, Weber DM, Coutre SE, Gasparetto C, Mukhopadhyay S, Ondovik MS, Khan M, Paley CS, et al. PANORAMA 2: panobinostat in combination with bortezomib and dexamethasone in patients with relapsed and bortezomib-refractory myeloma. Blood. 2013;122(14):2331–7.
Siegel DS, Dimopoulos M, Jagannath S, Goldschmidt H, Durrant S, Kaufman JL, Leleu X, Nagler A, Offner F, Graef T, et al. VANTAGE 095: an international, multicenter, open-label study of vorinostat (MK-0683) in combination with bortezomib in patients with relapsed and refractory multiple myeloma. Clin Lymphoma Myeloma Leuk. 2016;16(6):329-334 e321.
Cheng H, Xie Z, Jones WP, Wei XT, Liu Z, Wang D, Kulp SK, Wang J, Coss CC, Chen CS, et al. Preclinical Pharmacokinetics Study of R- and S-enantiomers of the histone deacetylase inhibitor, AR-42 (NSC 731438). Rodents AAPS J. 2016;18(3):737–45.
Gentile M, Morabito F, Martino M, Vigna E, Martino EA, Mendicino F, Martinelli G, Cerchione C. Chemotherapy-based regimens in multiple myeloma in 2020. Panminerva Med. 2021;63(1):7–12.
Ding K, Jiang W, Jia H, Lei M. Synergistically anti-multiple myeloma effects: flavonoid, non-flavonoid polyphenols, and bortezomib. Biomolecules. 2022;12(11):1647.
Ogawa Y, Ogura M, Tobinai K, Ando K, Suzuki T, Watanabe T, Ohmachi K, Uchida T, Hanson ME, Tanaka Y, et al. A phase I study of vorinostat combined with bortezomib in Japanese patients with relapsed or refractory multiple myeloma. Int J Hematol. 2016;103(1):25–33.
San-Miguel JF, Hungria VT, Yoon SS, Beksac M, Dimopoulos MA, Elghandour A, Jedrzejczak WW, Gunther A, Nakorn TN, Siritanaratkul N, et al. Overall survival of patients with relapsed multiple myeloma treated with panobinostat or placebo plus bortezomib and dexamethasone (the PANORAMA 1 trial): a randomised, placebo-controlled, phase 3 trial. Lancet Haematol. 2016;3(11):e506–15.
Kaufman JL, Mina R, Jakubowiak AJ, Zimmerman TL, Wolf JJ, Lewis C, Gleason C, Sharp C, Martin T, Heffner LT, et al. Combining carfilzomib and panobinostat to treat relapsed/refractory multiple myeloma: results of a Multiple Myeloma Research Consortium Phase I Study. Blood Cancer J. 2019;9(1):3.
Berdeja JG, Hart LL, Mace JR, Arrowsmith ER, Essell JH, Owera RS, Hainsworth JD, Flinn IW. Phase I/II study of the combination of panobinostat and carfilzomib in patients with relapsed/refractory multiple myeloma. Haematologica. 2015;100(5):670–6.
Berdeja JG, Gregory TK, Faber EA, Hart LL, Mace JR, Arrowsmith ER, Flinn IW, Matous JV. A phase I/II study of the combination of panobinostat and carfilzomib in patients with relapsed or relapsed/refractory multiple myeloma: final analysis of second dose-expansion cohort. Am J Hematol. 2021;96(4):428–35.
Richardson PG, Zweegman S, O’Donnell EK, Laubach JP, Raje N, Voorhees P, Ferrari RH, Skacel T, Kumar SK, Lonial S. Ixazomib for the treatment of multiple myeloma. Expert Opin Pharmacother. 2018;19(17):1949–68.
Kristinsson SY, Anderson WF, Landgren O. Improved long-term survival in multiple myeloma up to the age of 80 years. Leukemia. 2014;28(6):1346–8.
Pan D, Mouhieddine TH, Upadhyay R, Casasanta N, Lee A, Zubizarreta N, Moshier E, Richter J. Outcomes with panobinostat in heavily pretreated multiple myeloma patients. Semin Oncol. 2023;50(1–2):40–8.
Shah RR. Safety and tolerability of histone deacetylase (HDAC) inhibitors in oncology. Drug Saf. 2019;42(2):235–45.
Moreau P, Facon T, Touzeau C, Benboubker L, Delain M, Badamo-Dotzis J, Phelps C, Doty C, Smit H, Fourneau N, et al. Quisinostat, bortezomib, and dexamethasone combination therapy for relapsed multiple myeloma. Leuk Lymphoma. 2016;57(7):1546–59.
Dimopoulos M, Siegel DS, Lonial S, Qi J, Hajek R, Facon T, Rosinol L, Williams C, Blacklock H, Goldschmidt H, et al. Vorinostat or placebo in combination with bortezomib in patients with multiple myeloma (VANTAGE 088): a multicentre, randomised, double-blind study. Lancet Oncol. 2013;14(11):1129–40.
San-Miguel JF, Richardson PG, Gunther A, Sezer O, Siegel D, Blade J, LeBlanc R, Sutherland H, Sopala M, Mishra KK, et al. Phase Ib study of panobinostat and bortezomib in relapsed or relapsed and refractory multiple myeloma. J Clin Oncol. 2013;31(29):3696–703.
Chari A, Cho HJ, Dhadwal A, Morgan G, La L, Zarychta K, Catamero D, Florendo E, Stevens N, Verina D, et al. A phase 2 study of panobinostat with lenalidomide and weekly dexamethasone in myeloma. Blood Adv. 2017;1(19):1575–83.
Schiattarella GG, Sannino A, Toscano E, Cattaneo F, Trimarco B, Esposito G, Perrino C. Cardiovascular effects of histone deacetylase inhibitors epigenetic therapies: systematic review of 62 studies and new hypotheses for future research. Int J Cardiol. 2016;219:396–403.
Zou S, Tong Q, Liu B, Huang W, Tian Y, Fu X. Targeting STAT3 in cancer immunotherapy. Mol Cancer. 2020;19(1):145.
Kuo IY, Yang YE, Yang PS, Tsai YJ, Tzeng HT, Cheng HC, Kuo WT, Su WC, Chang CP, Wang YC. Converged Rab37/IL-6 trafficking and STAT3/PD-1 transcription axes elicit an immunosuppressive lung tumor microenvironment. Theranostics. 2021;11(14):7029–44.
Shen M, Xu Z, Xu W, Jiang K, Zhang F, Ding Q, Xu Z, Chen Y. Inhibition of ATM reverses EMT and decreases metastatic potential of cisplatin-resistant lung cancer cells through JAK/STAT3/PD-L1 pathway. J Exp Clin Cancer Res. 2019;38(1):149.
Herrmann A, Lahtz C, Nagao T, Song JY, Chan WC, Lee H, Yue C, Look T, Mulfarth R, Li W, et al. CTLA4 Promotes Tyk2-STAT3-dependent B-cell oncogenicity. Cancer Res. 2017;77(18):5118–28.
Cosenza M, Civallero M, Marcheselli L, Sacchi S, Pozzi S. Citarinostat and momelotinib co-target HDAC6 and JAK2/STAT3 in lymphoid malignant cell lines: a potential new therapeutic combination. Apoptosis. 2020;25(5–6):370–87.
Keremu A, Aimaiti A, Liang Z, Zou X. Role of the HDAC6/STAT3 pathway in regulating PD-L1 expression in osteosarcoma cell lines. Cancer Chemother Pharmacol. 2019;83(2):255–64.
Lienlaf M, Perez-Villarroel P, Knox T, Pabon M, Sahakian E, Powers J, Woan KV, Lee C, Cheng F, Deng S, et al. Essential role of HDAC6 in the regulation of PD-L1 in melanoma. Mol Oncol. 2016;10(5):735–50.
Li T, Zhang C, Hassan S, Liu X, Song F, Chen K, Zhang W, Yang J. Histone deacetylase 6 in cancer. J Hematol Oncol. 2018;11(1):111.
Ou L, Wang H, Huang H, Zhou Z, Lin Q, Guo Y, Mitchell T, Huang AC, Karakousis G, Schuchter L, et al. Preclinical platforms to study therapeutic efficacy of human gammadelta T cells. Clin Transl Med. 2022;12(6): e814.
Sharma A, Schmidt-Wolf IGH. 30 years of CIK cell therapy: recapitulating the key breakthroughs and future perspective. J Exp Clin Cancer Res. 2021;40(1):388.
Stephan D, Weiher H, Schmidt-Wolf IGH. CIK cells and HDAC inhibitors in multiple myeloma. Int J Mol Sci. 2017;18(5):945.
Pu J, Sharma A, Liu T, Hou J, Schmidt-Wolf IG. Synergistic integration of histone deacetylase inhibitors apparently enhances the cytokine-induced killer cell efficiency in multiple myeloma via the NKG2D pathway. Clin Transl Immunol. 2024;13(3): e1500.
Lin A, Giuliano CJ, Palladino A, John KM, Abramowicz C, Yuan ML, Sausville EL, Lukow DA, Liu L, Chait AR, et al. Off-target toxicity is a common mechanism of action of cancer drugs undergoing clinical trials. Sci Transl Med. 2019;11(509):eaaw8412.
Palumbo A, Chanan-Khan A, Weisel K, Nooka AK, Masszi T, Beksac M, Spicka I, Hungria V, Munder M, Mateos MV, et al. Daratumumab, bortezomib, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375(8):754–66.
Garcia-Guerrero E, Gogishvili T, Danhof S, Schreder M, Pallaud C, Perez-Simon JA, Einsele H, Hudecek M. Panobinostat induces CD38 upregulation and augments the antimyeloma efficacy of daratumumab. Blood. 2017;129(25):3386–8.
Bat-Erdene A, Nakamura S, Oda A, Iwasa M, Teramachi J, Ashtar M, Harada T, Miki H, Tenshin H, Hiasa M, et al. Class 1 HDAC and HDAC6 inhibition inversely regulates CD38 induction in myeloma cells via interferon-alpha and ATRA. Br J Haematol. 2019;185(5):969–74.
Abdulkadyrov KM, Salogub GN, Khuazheva NK, Sherman ML, Laadem A, Barger R, Knight R, Srinivasan S, Terpos E. Sotatercept in patients with osteolytic lesions of multiple myeloma. Br J Haematol. 2014;165(6):814–23.
Garcia-Guerrero E, Gotz R, Doose S, Sauer M, Rodriguez-Gil A, Nerreter T, Kortum KM, Perez-Simon JA, Einsele H, Hudecek M, et al. Upregulation of CD38 expression on multiple myeloma cells by novel HDAC6 inhibitors is a class effect and augments the efficacy of daratumumab. Leukemia. 2021;35(1):201–14.
Acknowledgements
We acknowledge the China Scholarship Council (CSC) for its financial support to JJP and TL.
Funding
This study was supported by Top Talent Support Program for Young and Middle-aged People of Wuxi Health Committee (HB2023080), Wuxi Medical Development Discipline Project (FZXK2021008) and The "Three" strategic linkeln team of Wuxi Maternal and Child Health Care Hospital (LY2023004).
Author information
Authors and Affiliations
Contributions
JJP, TL, XZW, AS, IGHS-W, JH and LPJ contributed to conceive, design and revision of the manuscript sections. JJP wrote the manuscript. JJP and TL designed figures and created Tables. JJP, AS, IGHS-W, JH and LPJ supervised the manuscript by providing critical feedbacks and revisions. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pu, J., Liu, T., Wang, X. et al. Exploring the role of histone deacetylase and histone deacetylase inhibitors in the context of multiple myeloma: mechanisms, therapeutic implications, and future perspectives. Exp Hematol Oncol 13, 45 (2024). https://doi.org/10.1186/s40164-024-00507-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40164-024-00507-5