Abstract
Background
The use of central venous pressure (CVP) measurements among (intensive care unit) ICU patients with severe coma has been questioned. This study aimed to investigate the application value of CVP in this population.
Methods
Data stored in the ICU Collaborative Research Database (eICU-CRD) and Medical Information Mart for Intensive Care III (MIMIC-III) database were reviewed. Critically ill patients with a Glasgow Coma Scale (GCS) score of 3–8 were included. The primary outcome was the in-hospital mortality rate. The statistical approaches used included multivariable Cox regression, propensity score matching (PSM), inverse probability treatment weighting (IPTW), stabilized IPTW, and restricted cubic splines (RCS) to ensure the robustness of our findings.
Results
In total, 7386 patients were included in the study. Early CVP measurement was independently associated with in-hospital mortality [hazard ratio, 0.63; p < 0.001] in patients with severe-to-moderate coma. This result was robust in the PSM, sIPTW, and IPTW cohorts. For all patients with CVP measurements, the RCS curves showed that the risk of in-hospital mortality increased as the initial CVP time was delayed. In addition, early CVP measurement was significantly associated with lower ICU mortality, 28-day mortality, and 365-day mortality and a significantly higher number of ventilator-free days.
Conclusion
Early CVP measurement could improve clinical outcomes in critically ill patients with severe coma
Similar content being viewed by others
Background
Central venous pressure (CVP) is the pressure recorded in the superior vena cava or the right atrium and, to a lesser extent, the left ventricular preload [1], reflecting venous return and right ventricular function [2]. Thus, CVP measurements could help in fluid management [3]. However, the CVP can also be influenced by thoracic, pericardial and abdominal pressures, complicating its understanding. Recently, several studies have found that the CVP cannot predict fluid responsiveness and only higher or lower CVP values may have negative or positive predictive values [4,5,6]. Therefore, the application of CVP measurement has been questioned. Some researchers have suggested that although there could be some limitations to using the CVP to assist fluid resuscitation, it would be better to fully understand and address these limitations, rather than abandoning them completely [3, 7]. The CVP levels still provide significant information about patient's cardiocirculatory status.
Many clinical studies have reported that higher CVP values may be associated with patients’ poor outcomes in different conditions, such as patients undergoing cardiac surgery [11], early Fontan failure [10], acute kidney injury (AKI) [8, 9], patients undergoing cardiopulmonary bypass surgery [9], and critically ill patients [2]. A controlled lower CVP can also reduce blood loss during hepatectomy [12]. Meanwhile, CVP measurement has been reported to shorten the time to be medically fit for discharge and benefit the clinical outcomes for patients with acute respiratory distress syndrome or sepsis [13,14,15]. Some researchers have suggested using the CVP as a stopping rule for fluid infusion [3, 7]. However, to our knowledge, the value of CVP measurements in patients with coma remains unclear. Fluid administration could increase cardiac output; however, it could also increase the risk of hydrostatic pressure or edema formation. Theoretically, this situation could be more complicated in critically ill comatose patients, and CVP may be beneficial in these conditions.
Therefore, the purposes of this study were to investigate 1) the association between early CVP measurement and patients’ outcomes and 2) the association between initial CVP time and all-cause mortality of intensive care unit (ICU) patients with severe coma.
Methods
Study design and population
Data were collected from patients in the ICU Collaborative Research Database (eICU-CRD) [16] and the Medical Information Mart for Intensive Care III (MIMIC-III) [17]. Patient characteristics available in both databases included demographic information, vital signs, laboratory test results, diagnoses, medical histories, treatments and so on. Detailed information on these two databases can be found in PhysioNet [18].
Patients with severe coma were identified using the Glasgow Coma Scale (GCS). The GCS was first published in 1975 and is the most widely applied outcome measure in clinical settings and researches on brain injury [19, 20]. Currently, the GCS is recommended by lots of countries to use as a measurement for primary outcome. A severe coma is defined as a score of 3–8 [21]. We only collected the GCS scores before sedative drug use on the first day for each patient. For patients with multi-ICU admissions, we only include the first admission. Patients aged < 18 years or ≥ 90 years were excluded. An early CVP measurement was defined as a CVP measurement in the first 24 h after first ICU admission. According to early CVP, the entire cohort was divided into CVP and non-CVP groups. The initial CVP time and CVP values were also collected. All comorbidities were identified based on recorded ICD-9 or APACHE components. We only collected the first value within 24 h of ICU admission for vital signs and laboratory test results.
In clinical practice, there may be many reasons for coma development. Due to the nature of retrospective research, we cannot accurately determine the direct cause of coma in patients. Therefore, we collected the primary diagnoses of patients and classified them according to ICD-9 for different diseases, such as circulatory disease and injury disease.
Study outcome
All-cause in-hospital mortality rate was set as the primary outcome. The secondary outcomes included 28-day mortality; 365-day mortality; ICU mortality; MV-free days; vasopressor-free days within 28 days after ICU admission; intravenous fluid (IVF) volumes (ml) of the first, second, and third days after ICU admission; and incidences of AKI within 2 days and 7 days after ICU admission [22].
Statistics analysis
Continuous variables are illustrated as mean ± standard deviation (SD). Categorical variables are presented as total number and percentage. The Chi-square test was applied to compare proportions, and the T-test or Wilcoxon rank-sum test was used for continuous variables. Early CVP was analyzed as a categorical variable for the primary analysis in the whole cohort, and the CVP value was analyzed as a continuous variable in the CVP group. Multivariable Cox regression was used for all outcomes to adjust for confounders that may affect the outcomes. Variables with a P value of < 0.2 in the univariable analysis were enrolled in the multivariable analysis.
We used several sensitivity analyses to ensure the consistency of the findings, including propensity score matching (PSM), inverse probability treatment weighting (IPTW), and stabilized IPTW (sIPTW). Patients’ propensity score was assessed using a multivariable logistic analysis to minimize the covariate imbalance between the CVP and non-CVP groups. To compare secondary outcomes, the standardized mean differences and statistical significance of parameters between the CVP and non-CVP groups in the PSM cohort were calculated using the Chi-square test or t-test. We also used restricted cubic spline (RCS) curves based on multivariable Cox regression to evaluate the relationship between the initial CVP time or value and the primary outcome. All statistical analyses were performed using R software.
Results
Baseline information
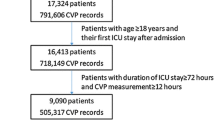
A total of 26,2391 ICU admissions were reviewed from the eICU-CRD and MIMIC-III databases. After exclusion, 7386 patients were included in the final analysis, including 1861 patients with CVP and 5525 patients without CVP (Fig. 1). The mean GCS was 5.46 ± 1.99. The mean age of the entire cohort was 62.82 ± 16.70 years, and 3170 (42.9%) patients were female. The total in-hospital and ICU mortality rates were 41.0% (3031/7386) and 33.2% (2455/7386), respectively. Patients in the CVP group had more comorbidities, larger CCI, higher SOFA scores, lower GCS scores, lower vital signs, and greater use of sedative drugs, vasopressor drugs, and MV than those in the non-CVP group. The details of the original and PSM cohorts are presented in Table 1. In the CVP group, the initial CVP time was 5.21 ± 5.79 h and mean initial CVP value was 12.15 ± 8.79 cmH2O. Information on the missing values is demonstrated in Additional file 1: Table S1.
Primary outcome and sensitivity analysis
CVP was conducted in 18.7% of the non-surviving patients and 29.7% of the surviving patients. After adjustment for primary diagnosis, age, sex, GCS, ethnicity, unit type, AF, malignant tumor, renal disease, stroke, liver disease, CHF, CAD, COPD, MAP, temperature, heart rate, lactate, hemoglobin, platelet count, bicarbonate, BUN, WBC count, potassium, chloride, sedative use, vasopressor use, MV use, SOFA score, CCI, and database type, early CVP was significantly associated with lower all-cause in-hospital mortality in the whole cohort (hazard ratio [HR] 0.63; 95% confidence intervals [CI] 0.55–0.71; P < 0.001), and remained robust in the PSM cohort (HR, 0.58; 95% CI 0.51–0.66; P < 0.001), IPTW cohort (HR 0.65; 95% CI 0.56–0.75; P < 0.001), and sIPTW cohort (HR 0.64; 95% CI 0.55–0.74; P < 0.001) (Table 2). The full results of the different multivariate models are shown in Additional file 1: Tables S2-S5.
The initial CVP time (hours) and value (cmH2O) after ICU admission were both associated with in-hospital mortality in the CVP group, with HRs of 1.02 (95% CI 1.01–1.03; P = 0.034) and 1.02 (95% CI 1.01–1.02; P < 0.001), respectively. In general, the RCS curve shows that with the delay in the initial CVP time, the risk of all-cause mortality in hospital increases (Fig. 2).
Restricted cubic spline (RCS) curves of associations between initial central venous pressure (CVP) time and all-cause in-hospital mortality. Results were adjusted for primary diagnoses, Glasgow Coma scale, unit, congestive heart failure, atrial fibrillation, coronary artery disease, stroke, heart rate, temperature, white blood cell count, hemoglobin, sodium, bicarbonate, chloride, blood urea nitrogen, lactate, sedative use, vasopressor use, mechanical ventilation use, SOFA scale, and days in ICU. RCS regression models were conducted with 3 knots at the 10th, 50th, and 90th percentiles of initial CVP time. The red lines represent the 95% confidence intervals for the spline model
Secondary outcomes
Compared with patients without CVP measurement, those with CVP have a lower ICU mortality (44.4% vs. 27.8%; P < 0.001), lower 28-day mortality (in MIMIC-III only, 37.8% vs. 20.6%; P < 0.001), lower 365-day mortality (in MIMIC-III only, 50.9% vs. 30.8%; P < 0.001), and a more significant number of vasopressor-free days (in MIMIC-III only, 16.95 ± 13.31 days vs. 21.15 ± 11.00 days; P < 0.001) (Table 3). However, patients in the CVP group as have a higher 2-day (69.5% vs. 75.5%, P = 0.001) and a higher 7-day (77.3% vs. 81.2%, P = 0.018) AKI rates. Moreover, no association was found between the number of MV-free days (20.79 ± 9.86 vs. 21.22 ± 9.80; P = 0.272). Compared to patient without CVP, patients in the CVP group have a higher IVF volume on day 1 (3100.88 ± 3163.26 ml vs. 4167.19 ± 3838.39 ml; P < 0.001) and lower IVF volumes on day 2 (2274.16 ± 2405.90 ml vs. 2058.66 ± 2357.80 ml; P = 0.045) and day 3 (2178.88 ± 2492.15 ml vs. 1647.62 ± 2097.16 ml; P < 0.001).
Discussion
The goal of current study was to investigate the application value of CVP in patients with severe coma in the ICU. We found that early CVP was independently associated with lower all-cause in-hospital mortality in severe coma patients (GCS score 3–8). We also found the association of the initial CVP time and in-hospital mortality was presented as a “U-shape” in the RCS curve. As the initial CVP time increases, the risk of all-cause in-hospital mortality increases.
Because of the standardization of advances in technologies, such as MVs, in ICU management, more and more comatose patients are surviving life-threatening diseases. However, the high mortality rate and cost for this type of patient are still among the most severe clinical and social problems [23, 24]. Any efforts that could increase the chances of reasonable functional outcomes in patients with coma are of utmost clinical and ethical significance [25].
This is the first study to investigate the association between the early CVP and clinical outcomes in patients with severe coma. The current study was a post hoc analysis. The data included in this study were from the eICU and MIMIC-III databases, which contain ICU patients across more than 200 different hospitals in the USA, with varying CVP practices. Our analysis leverages the availability of time-stamped demographic information, comorbidities, vital signs, laboratory results, etc., to investigate whether CVP could benefit patients with severe coma. The results of the study were highly consistent across different sensitivity analyses.
Conflicting evidence on the application of the CVP has been reported in previous studies. Eskesen et al. found that the application value of the CVP measurement is low in a re-analysis of 1148 patient data sets [5]. They reported that only in certain extreme cases, such as higher or lower, does CVP measurement demonstrate some of its value in liquid management. Marik et al. conducted a meta-analysis and reported that only 57% of patients were fluid responders, and the correlation between CVP level and stroke volume index was not strong; thus, the use of the CVP for fluid resuscitation should be abandoned in widespread practice due to insufficient evidence. However, many studies have reported the association between the CVP levels and patients’ clinical outcomes with various conditions. For example, Chen et al. found in a meta-analysis that a higher CVP value was associated with higher mortality (odds ratio [OR] 1.65) and a greater risk of AKI (OR, 2.09). Quail et al. found that a higher CVP is associated with a higher risk of early Fontan failure after total cavopulmonary connections [10]. Liu et al. also found that a controlled lower CVP could reduce blood loss during hepatectomy and recommended the promotion of CVP use in clinical settings [12].
Despite the conflicting evidence reported and the value of the CVP being questioned, some clinicians still recommend the use of the CVP in clinical settings [3, 7]. One recommendation is to use CVP as a stop symbol in liquid management. Weil and Henning first proposed this approach and suggested that fluid administration could be stop as the CVP increased by 5 cmH2O or more [26]. However, Hamzaoui et al. reported that changes in the stroke volume could not be reflected by the CVP levels. Therefore, the CVP levels could not represent as a criterion for predicting fluid responsiveness [6].
Whatever the approach to CVP application, some evidence also indicates that CVP use is associated with a better clinical outcome in some patients [14, 15]. Chen et al. reported the association between the CVP using and lower 28-day mortality in septic patients [14]. Tang et al. reported that the CVP could improve the clinical outcomes of patients with acute respiratory distress syndrome [15]. However, both studies were from a single-center database; thus, the generalization of the results could be hindered. In these multicenter studies, we found that severe comas patients with CVP suing have a lower in-hospital mortality than those without CVP. Moreover, we found that with the delay in the initial CVP time, the risk of in-hospital mortality is increasing. In the secondary outcomes, we found that CVP was also associated with ICU mortality, 28-day mortality, 365-day mortality, and more days without vasopressor drugs. We believe that these results confirm the application value of CVP in comatose patients.
The detailed influence of the CVP on therapeutic interventions was difficult to explore due to the retrospective design. Previous studies reported that the trigger caused by CVP, such as fluid therapy, could lower lactate levels of patients, thus could improve outcomes [14, 15]. Semler et al. found that different fluid management based on initial CVP values could influence outcomes of acute respiratory distress syndrome patients, and conservative fluid administration could lower the mortality of patients with a low initial CVP [27]. Wang et al. found that patients who have a peak CVP value more than 12 mmHg also have worse organ function, higher SOFA score and longer hospital stay [2]. These results indicate that CVP could positively impact the latter management of patients. In the current study, we found that the IVF was significantly different between patients with and -out CVP. Generally, IVF volumes in patients with CVP were higher on day 1 and lower on day 3 compared to those in the non-CVP group. Most patients (62.1%) with CVP had an initial CVP value of ≤ 12 mmH2O. It is difficult to investigate whether the difference in the IVF on the first day was influenced by the CVP. However, relatively free fluid management may be safe when the levels maintaining as low as possible [3]. Fluid management is a double-edged sword. Correction of intravascular hypovolemia is critical for preventing and managing AKI, but excessive fluid administration could also increases the risk of AKI [28, 29]. In the current study, we also discovered that the 2-day and 7-day AKI was higher in patients with CVP, which is different from that in previous studies. The causal relationship between the increased risk of AKI and the CVP requires further research and evaluation.
Limitations
Our study had some limitations. First, although the GCS has been used for more than 40 years and is the most widespread measurement in brain injury studies [20], using the GCS score of 3–8 to define severe coma in patients in the ICU could still introduce patient selection bias. Meanwhile, all data in this study were extracted using a structured query language, which may also cause misclassification of patients. Second, considering that the significant covariate imbalance between the CVP and non-CVP groups may influence the explanation of the results, we used a PSM approach to minimize the differences and performed several sensitivity analyses. However, covariate imbalance was still observed for some variables. Third, although we included patients from two large databases from more than 200 hospitals to improve the generalization of the results, the retrospective design may still introduce some analysis bias. Fourth, because CVP values are generally measured and read manually, measurement and reading errors cannot be avoided. Finally, CVP-related management changes are complex in clinical practice. The nature of post hoc analysis of the current study should not be ignored. Although we found a robust association between CVP and the primary outcome, the causal relationship of this condition remains unclear and should be investigated in further studies.
Conclusion
In critically ill patients with severe coma (GCS score 3–8), early CVP measurements is independently associated with lower in-hospital mortality. Among patients with CVP measurements, in-hospital mortality increased with a delayed initial CVP measurement.
Data availability
MIMIC III and eICU-CRD databases are available to researchers through credentialed access on the PhysioNet.
Abbreviations
- AKI:
-
Acute kidney injury
- CVP:
-
Central venous pressure
- GCS:
-
Glasgow Coma Scale
- HR:
-
Hazard ratio (HR)
- eICU-CRD/eICU:
-
ICU Collaborative Research Database
- IVF:
-
Intravenous fluid
- IPTW:
-
Inverse probability treatment weighting
- MIMIC-III:
-
Medical Information Mart for Intensive Care III
- OR:
-
Odds ratio
- PSM:
-
Propensity score matching
- RCS:
-
Restricted cubic splines
- sIPTW:
-
Stabilized IPTW
- SD:
-
Standard deviation
References
Hughes RE, Magovern GJ. The relationship between right atrial pressure and blood volume. AMA Arch Surg. 1959;79:238–43.
Wang X, Chen H, Liu D, Zhang Q, Su L. The correlation between CVP-derived parameters and the prognosis of critically ill patients. J Crit Care. 2017;40:257–64.
De Backer D, Vincent J-L. Should we measure the central venous pressure to guide fluid management? Ten answers to 10 questions. Crit Care. 2018;22:43.
Marik PE, Cavallazzi R. Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med. 2013;41:1774–81.
Eskesen TG, Wetterslev M, Perner A. Systematic review including re-analyses of 1148 individual data sets of central venous pressure as a predictor of fluid responsiveness. Intensive Care Med. 2016;42:324–32.
Hamzaoui O, Gouëzel C, Jozwiak M, Millereux M, Sztrymf B, Prat D, Jacobs F, Monnet X, Trouiller P, Teboul J-L. Increase in central venous pressure during passive leg raising cannot detect preload unresponsiveness. Crit Care Med. 2020;48:e684–9.
Pinsky MR, Kellum JA, Bellomo R. Central venous pressure is a stopping rule, not a target of fluid resuscitation. Crit Care Resusc. 2014;16:245–6.
Chen C-Y, Zhou Y, Wang P, Qi E-Y, Gu W-J. Elevated central venous pressure is associated with increased mortality and acute kidney injury in critically ill patients: a meta-analysis. Crit Care. 2020;24:80.
Yang Y, Ma J, Zhao L. High central venous pressure is associated with acute kidney injury and mortality in patients underwent cardiopulmonary bypass surgery. J Crit Care. 2018;48:211–5.
Quail MA, Chan I, Sarna S, Hughes M, Muthurangu V. A preoperative estimate of central venous pressure is associated with early fontan failure. J Thorac Cardiovasc Surg. 2021;161:1426–34.
Schiefenhövel F, Trauzeddel RF, Sander M, Heringlake M, Groesdonk HV, Grubitzsch H, Kruppa J, Berger C, Treskatsch S, Balzer F. High central venous pressure after cardiac surgery might depict hemodynamic deterioration associated with increased morbidity and mortality. JCM. 2021;10:3945.
Junrungsee S, Suwannikom K, Tiyaprasertkul W, Lapisatepun W, Chotirosniramit A, Sandhu T, Chandacham K, Jirapongcharoenlap T, Lapisatepun W, Ko-Iam W. Efficacy and safety of infrahepatic inferior vena cava clamping under controlled central venous pressure for reducing blood loss during hepatectomy: a randomized controlled trial. J Hepatobiliary Pancreat Sci. 2021;28:604–16.
Venn R, Steele A, Richardson P, Poloniecki J, Grounds M, Newman P. Randomized controlled trial to investigate influence of the fluid challenge on duration of hospital stay and perioperative morbidity in patients with hip fractures. Br J Anaesth. 2002;88:65–71.
Chen H, Zhu Z, Zhao C, Guo Y, Chen D, Wei Y, Jin J. Central venous pressure measurement is associated with improved outcomes in septic patients: an analysis of the MIMIC-III database. Crit Care. 2020;24:433.
Tang R, Peng J, Wang D. Central venous pressure measurement is associated with improved outcomes in patients with or at risk for acute respiratory distress syndrome: an analysis of the medical information mart for intensive care IV database. Front Med (Lausanne). 2022;9: 858838.
Pollard TJ, Johnson AEW, Raffa JD, Celi LA, Mark RG, Badawi O. The eICU collaborative research database, a freely available multi-center database for critical care research. Sci Data. 2018;5: 180178.
Johnson AEW, Pollard TJ, Shen L, Lehman L-WH, Feng M, Ghassemi M, Moody B, Szolovits P, Celi LA, Mark RG. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3: 160035.
Goldberger AL, Amaral LA, Glass L, Hausdorff JM, Ivanov PC, Mark RG, Mietus JE, Moody GB, Peng CK, Stanley HE. PhysioBank, PhysioToolkit, and PhysioNet: components of a new research resource for complex physiologic signals. Circulation. 2000;101:E215-220.
McMillan T, Wilson L, Ponsford J, Levin H, Teasdale G, Bond M. The glasgow outcome scale - 40 years of application and refinement. Nat Rev Neurol. 2016;12:477–85.
Teasdale G, Maas A, Lecky F, Manley G, Stocchetti N, Murray G. The glasgow coma scale at 40 years: standing the test of time. The Lancet Neurology. 2014;13:844–54.
Mehta R, trainee GP, Chinthapalli K, Consultant neurologist. Glasgow coma scale explained. BMJ. 2019;365: l1296.
Kellum JA, Lameire N, KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care. 2013;17:204.
Luce JM. Chronic disorders of consciousness following coma: part two: ethical, legal, and social issues. Chest. 2013;144:1388–93.
Vasilevskis EE, Chandrasekhar R, Holtze CH, Graves J, Speroff T, Girard TD, Patel MB, Hughes CG, Cao A, Pandharipande PP, et al. The cost of ICU delirium and coma in the intensive care unit patient. Med Care. 2018;56:890–7.
Claassen J. Coma science: intensive care as the new frontier. Intensive Care Med. 2020;46:97–101.
Weil MH, Henning RJ. New concepts in the diagnosis and fluid treatment of circulatory shock. Thirteenth annual Becton, Dickinson and Company Oscar Schwidetsky memorial lecture. Anesth Analg. 1979;58:124–32.
Semler MW, Wheeler AP, Thompson BT, Bernard GR, Wiedemann HP, Rice TW, National Institutes of Health National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network. Impact of initial central venous pressure on outcomes of conservative versus liberal fluid management in acute respiratory distress syndrome. Crit Care Med. 2016;44:782–9.
Ostermann M, Liu K, Kashani K. Fluid Management in acute kidney injury. Chest. 2019;156:594–603.
Vanmassenhove J, Kielstein J, Jörres A, Biesen WV. Management of patients at risk of acute kidney injury. Lancet. 2017;389:2139–51.
Acknowledgements
None.
Funding
Natural Science Foundation of China (81771233, 82171290); Research and Promotion Program of Appropriate Techniques for Intervention of Chinese High-risk Stroke People (GN-2020R0007); BTH Coordinated Development-Beijing Science and Technology Planning Project (Z181100009618035); Beijing Municipal Administration of Hospitals' Ascent Plan (DFL20190501); Beijing Natural Science Foundation (19L2013; 22G10396).
Author information
Authors and Affiliations
Contributions
AH. L. and CZ. D. conceived and designed the study. X.T. collected the data. X.T. and X.F. conceived of the project, analyzed the data, and wrote the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Consent for publication
The MIMIC-IV database was built by the Massachusetts Institute of Technology and was approved to waive the documentation of informed consent by the Institutional Review Boards of Beth Israel Deaconess Medical Center. The eICU-CRD study was exempt from institutional review board approval due to the retrospective design, lack of direct patient intervention, and the security schema, for which the re-identification risk was certified as meeting safe harbor standards by an independent privacy expert (Privacert, Cambridge, MA) (Health Insurance Portability and Accountability Act Certification no. 1031219-2). To access the database, X. T. completed the Collaborative Institutional Training Initiative course named “Data or Specimens Only Research” and obtained the certification (certification number: 43334826). There was no requirement for individual informed consent to extract data from the MIMIC-III and eICU-CRD databases because both databases’ information was publicly available, and all patient data were deidentified.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Missing value for included variables in this study. Table S2. Full multivariate model assessing the impact of central venous pressure on in hospital mortality in the original cohort. Table S3. Full multivariate model assessing the impact of central venous pressure on in hospital mortality in the PSM cohort. Table S4. Full multivariate model assessing the impact of central venous pressure on in hospital mortality in the IPTW cohort. Table S5. Full multivariate model assessing the impact of central venous pressure on in hospital mortality in the sIPTW cohort.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tong, X., Feng, X., Duan, C. et al. Association between central venous pressure measurement and outcomes in critically ill patients with severe coma. Eur J Med Res 28, 35 (2023). https://doi.org/10.1186/s40001-022-00981-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-022-00981-9