Abstract
Background
Interleukin-6 receptor antagonists (IL-6RAs) and steroids are emerging immunomodulatory therapies for severe and critical coronavirus disease (COVID-19). In this preliminary report, we aim to describe the epidemiology, clinical characteristics, and outcomes of adult critically ill COVID-19 patients, requiring invasive mechanical ventilation (iMV), and receiving IL-6RA and steroids therapy over the last 11 months.
Materials and methods
International, multicenter, cohort study derived from Viral Infection and Respiratory Illness University Study registry and conducted through Discovery Network, Society of Critical Care Medicine. Data were collected between March 01, 2020, and January 10, 2021.
Results
Of 860 patients who met eligibility criteria, 589 received steroids, 170 IL-6RAs, and 101 combinations. Patients who received IL-6RAs were younger (median age of 57.5 years vs. 61.1 and 61.8 years in the steroids and combination groups, respectively). The median C-reactive protein level was > 75 mg/L, indicating a hyperinflammatory phenotype. The median daily steroid dose was 7.5 mg dexamethasone or equivalent (interquartile range: 6–14 mg); 80.8% and 19.2% received low-dose and high-dose steroids, respectively. Of the patients who received IL-6RAs, the majority received one dose of tocilizumab and sarilumab (dose range of 600–800 mg for tocilizumab and 200–400 mg for sarilumab). Regarding the timing of administration, we observed that steroid and IL-6RA administration on day 0 of ICU admission was only 55.6% and 39.5%, respectively. By day 28, when compared with steroid use alone, IL-6RA use was associated with an adjusted incidence rate ratio (aIRR) of 1.12 (95% confidence interval [CI] 0.88, 1.4) for ventilator-free days, while combination therapy was associated with an aIRR of 0.83 (95% CI 0.6, 1.14). IL-6RA use was associated with an adjusted odds ratio (aOR) of 0.68 (95% CI 0.44, 1.07) for the 28-day mortality rate, while combination therapy was associated with an aOR of 1.07 (95% CI 0.67, 1.70). Liver dysfunction was higher in IL-6RA group (p = 0.04), while the bacteremia rate did not differ among groups.
Conclusions
Discordance was observed between the registry utilization patterns (i.e., timing of steroids and IL-6RA administration) and new evidence from the recent randomized controlled trials and guideline recommendations. These data will help us to identify areas of improvement in prescribing patterns and enhance our understanding of IL-6RA safety with different steroid regimens. Further studies are needed to evaluate the drivers of hospital-level variation and their impact on clinical outcomes.
Trial registration ClinicalTrials.gov: NCT04486521. Registered on July 2020
Similar content being viewed by others
Background
Severe and critical coronavirus disease 2019 (COVID-19) can manifest as respiratory failure with elevated inflammatory markers, resulting in exaggerated cytokine release, for which interleukin-6 receptor antagonists (IL-6RAs) are approved as treatment [1,2,3]. Interest in IL-6RAs and corticosteroids has increased recently due to their potential role as immunomodulators [4,5,6,7]. In view of the results from International Randomized, Embedded, Multi-factorial, Adaptive Platform trial for Community-Acquired Pneumonia (REMAP-CAP) and Randomized Evaluation of COVID-19 Therapy (RECOVERY), guidelines by National Institutes of Health and Infectious Disease Society of America conditionally suggest tocilizumab in combination with steroids (low-dose dexamethasone, 6 mg daily for 10 days) for intensive care unit (ICU) patients exhibiting rapid respiratory failure progression or high inflammatory markers [8,9,10,11]. On July 6, 2021, the World Health Organization (WHO) rapid evidence appraisal for COVID-19 therapies (REACT) working group developed a prospective meta-analysis of IL-6RAs in patients hospitalized for COVID-19 and showed that 28-day all-cause mortality rate was lower among patients who received IL-6RAs compared with those who received usual care or placebo [12]. The lower mortality rate was more marked among patients who received concomitant steroids and did not require invasive mechanical ventilation (iMV) at randomization. As such, WHO Living guideline recommends IL-6RAs (tocilizumab or sarilumab) in combination with steroids for patients with severe or critical COVID-19 [13]. Moreover, the Bayesian reanalysis of RECOVERY trial showed that hospitalized COVID-19 patients on non-invasive ventilation (NIV), and high-flow nasal cannula (HFNC) have a high probability of a clinically meaningful outcome benefit from tocilizumab [14]. Therefore, the immunomodulatory effect of IL6-RAs appears to be most beneficial in combination with steroids and when administered in the early phase of critical care trajectory.
A retrospective observational study from Viral Infection and Respiratory Illness Universal Study (VIRUS) registry during March–November 2020 identified a large hospital-level variation and geographic disparity in the use of repurposed medications for the management of COVID-19 [15]. Herein, we aimed to reflect on our experience over the past 11 months and to describe the epidemiology, clinical characteristics, and outcomes of critically ill adult COVID-19 patients requiring iMV and receiving IL-6RA and steroid therapy. This will help to identify areas of improvement in prescribing patterns to enhance adherence to the recent guideline recommendations, and subsequently the outcomes in this subgroup of patients.
Materials and methods
Study design and data source
Data for this study were derived from VIRUS registry, an international, multicenter, observational study conducted through Discovery Network, Society of Critical Care Medicine (SCCM), and included 168 hospitals across 16 countries. The study was approved by SCCM Scientific Review Committee, SCCM Discovery Steering Committee, and King Faisal Specialist Hospital and Research Center (KFSH&RC) Institutional Review Board (IRB) (IRB# 2201053, registered at ClinicalTrials.gov NCT04486521). In some participating hospitals, verbal consent was obtained from patients or surrogate decision-makers and documented in electronic medical records (EMRs); in other countries, consent was waived by local research ethics committees. Local investigators were responsible for obtaining local approval in line with applicable regulations. VIRUS is one of the largest registries that consecutively collects data on COVID-19 patients. Details of this database are described elsewhere [16, 17] (Additional file 1: Table S1). This study is reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) and the Risk Of Bias In Nonrandomized Studies of Interventions (ROBINS-I) guidelines [18, 19].
Study population
Adult patients (18–85 years old) were eligible if admitted to ICU from March 01, 2020 to January 10, 2021, required iMV, had positive polymerase chain reaction (PCR) SARS-CoV-2, and received IL-6RAs (tocilizumab or sarilumab), corticosteroids (dexamethasone, hydrocortisone, methylprednisolone, or prednisone), or combination. We excluded patients who were < 17 years, repeatedly admitted to ICU during the same hospital visit, on chronic systemic steroids at home or taking steroids for indications other than COVID-19, or died before receiving IL-6RAs or steroids. We stratified the population into three groups: IL-6RA, corticosteroid, and combination. Corticosteroid group was stratified further based on dexamethasone equivalent dose (mg) into high and low-dose. High-dose was defined as > 15 mg/day of dexamethasone or equivalent. This cut-off was chosen based on the data from prior literature [20, 21]. The patients were followed for clinical outcomes and adverse events (AEs) up to day 28.
Data collection
The following variables were collected on days 0 (ICU admission), 1–3, 7, 14, 21, and 28 from EMRs according to standard operating procedure: demographics and comorbidities (including immunocompromised patients such as patients with solid tumors, hematological malignancy, metastatic cancer, history of solid organ or bone marrow transplant, and HIV), biomarkers and labs [ferritin, interleukin-6 (IL-6), d-dimer, fibrinogen, C-reactive protein (CRP), lactate dehydrogenase (LDH), and lymphocyte count], microbiology, concomitant medications, MV duration, discharge status, PaO2(mmHg)/FiO2 (arterial partial pressure of oxygen over fractional inspired oxygen concentration; PF ratio), and timing of drug initiation and dose. Data were collected online and stored on a secure data server using Mayo Clinic’s Research Electronic Data Capture application (REDCap). Data quality was assessed routinely to ensure completeness and accuracy. We reported the clinical outcomes for ventilator-free days (VFDs) from iMV at day 28, which was chosen as a patient-centered outcome and highly influenced by mortality [22]. VFDs were defined as the number of days between successful weaning of MV and day 28 after study enrollment. Patients who were on MV and died before day 28 were determined to have 0 VFDs. We also reported ICU and hospital mortality, 28-day mortality, hospital and ICU length of stay (LOS), median change in PF ratio, and AEs. Details on outcome definitions and variables collected are provided in Additional file 1: Table S2.
Statistical analyses
Sample size was determined pragmatically, based on all available ICU patients in VIRUS database who met eligibility criteria. Statistical analyses were performed using R software, V3.6.3 (Vienna, Austria). Counts and percentages were used to represent categorical variables. Continuous data were summarized using means ± standard deviations (SDs) or medians [interquartile ranges (IQR)]. Chi-square test was used to compare distribution of categorical variables, and Kruskal–Wallis test and ANOVA were used to compare distributions of continuous non-normal and normal variables, respectively. For outcome analysis, we used three statistical models. In model 1, marginal structural model (MSM) was used to compare three regimens after adjusting for non-time and time-varying covariates and included the overall treatment strategy not solely restricted to the first 48 h [23]. Observations were weighted by inverse probability of treatment weight (IPTW). Nonparametric modeling using generalized boosted model (GBM) estimate IPTWs with automatic handling of missing data [24]. TWANG package in R was used for analysis. Covariate distributions were compared before and after applying propensity weights. Standardized mean difference (SMD) was used to assess the balance of pseudo-population using Kolmogorov–Smirnov stop rule. Average treatment effect (ATE) estimation method was used throughout analysis of entire sample. Covariates included in model were judged as likely to influence outcomes and have been identified in several studies: age; sex; ethnicity; asthma/chronic obstructive pulmonary disease (COPD); acute respiratory distress syndrome (ARDS) grade; history of diabetes, hypertension, coronary heart disease, or congestive heart failure; the lowest FiO2; therapeutic anticoagulation; hydroxychloroquine; azithromycin; and antivirals (including remdesivir); vasopressors; and paralytics (details available at Additional file 2). Analyses were performed using robust variance estimators, taking into account clustering within hospitals and patients. Quasi-Poisson generalized linear modeling was used to compare VFDs after weighting. Quasi-Poisson regression coefficients were exponentiated to obtain incidence rate ratio (IRR), which is the expected change in VF-days (ratio), compared to reference category. Quasibinomial generalized linear modeling was used to compare mortality between three groups. Weighted Kaplan–Maier estimator was used to compare hospital and ICU LOS. Patients who were still in ICU after a 28-day study period were censored at 28 days. Log-rank test was used to compare survival before and after weighting. Cause-specific Cox regression analysis was used to assess factors associated with mortality at 28 days. Discharge and mortality were included as competing risks. Linear mixed modeling was used to compare changes in PF ratio. Hypothesis testing was performed at 5% level of significance.
Model 2 included exploratory analyses of potential factors associated with variation in VFDs and mortality by adding Sequential Organ Failure Assessment (SOFA) score and highest FiO2 to the base model 1.
In model 3, we performed a sensitivity analysis to emulate target trial to reduce immortal time bias, which is restricted to the treatment received in the first 48 h. Patients eligible for target trial approach were those on iMV, received IL-6RAs or steroids within ICU days 0 or 1. Patients who died within first 48 h were excluded. Those who get treatment of interest after day 1 were classified by treatment exposure in first 48 h [similar to intention-to-treat analysis in randomized controlled trial (RCT)] [25]. The outcomes of interest in target trial approach were VFDs and 28-day mortality. Post hoc analyses were conducted for clinical outcomes stratified by age (> 60 vs. ≤ 60) and to examine changes in biomarkers over time using linear mixed models.
Results
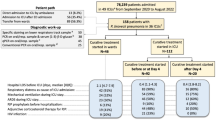
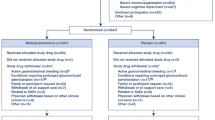
A total of 23,783 patients were screened; 860 met eligibility criteria and were classified as follows: 170 received IL-6RA, 589 received steroids, and 101 received both therapies. In sensitivity analysis to emulate target trial, 562 patients fulfilled inclusion criteria: 406 received steroids (72.2%), 121 received IL6-RAs (21.5%), and 35 received both (6.23%) (Fig. 1).
Patient characteristics
In the unadjusted analysis presented in Additional file 1: Table S3, baseline characteristics were not balanced. Patients who received IL-6RAs were younger (median age 57.5 years vs. 61.1 and 61.8 years in the steroid and combination groups, respectively; p = 0.009), and chronic pulmonary diseases, excluding asthma (COPD, bronchiectasis, and interstitial lung disease) were more prevalent in combination group (16 [15.8%] vs. 7 [4.12%] and 59 [10%] in IL-6RA and steroid groups, respectively; p = 0.005). The ARDS was prevalent in 35.5% of steroid-treated patients, 14.7% in IL-6RAs, and 36.6% in combination therapy; most of these patients had severe ARDS grades (PF ratio < 100). Patients in IL-6RAs and combination groups presented more frequently with fever, nasal congestion, and rhinorrhea than those in steroid group, while myalgia or fatigue was most frequently reported in steroid group. The incidence of dyspnea and shortness of breath was similar among the three groups. After adjusting for baseline covariates, SMD was ~ 0.1 for the majority of the covariates, indicating that the three groups were well-balanced (Table 1).
Table 2 illustrates the biomarker and laboratory levels at ICU day 0 after adjusting for covariates. The CRP level (assessed in 413) was > 75 mg/L across all groups, while IL-6 concentrations (assessed in 24) were highest in the combination group. The FiO2 was the highest in the combination group during the first 24 h. The mean LDH concentration (µkat/L) was 12.66 [SD 8.84] in steroid, 9.65 [SD 5.03] in IL-6RAs, and 9.46 [SD 5.32] in combination groups (p = 0.001).
Table 3 summarizes the utilization pattern of steroids and IL6-RAs in relation to ICU admission. The median daily steroid dose was 7.5 mg dexamethasone equivalent (IQR 6–14 mg). Of these, 80.8% received low-dose steroids, and 19.2% received high-dose steroids. Of the patients who received IL-6RAs, the majority (84.5%) received one dose of tocilizumab, while second and third doses were administered to 13.1% and 2.3% of patients, respectively. Similarly, most patients (84.7%) in sarilumab group received a single dose. The dosage range of tocilizumab was 600–800 mg, and sarilumab was 200–400 mg. Regarding the timing of the IL-6RA administration, 39.5% were received on day 0 of ICU admission, and ~ 30% started on days 1 and 2 (20.3% and 11.1%, respectively).
Additional comorbidities, ventilator and radiological characteristics, and ICU supports are included in Additional file 1: Tables S4–S9. IL-6RAs and the combination arm had more multifocal and bilateral interstitial patterns on chest radiography on day 1 of the ICU stay. Matched patients received comparable amounts of sedatives, paralytics, and anticoagulation.
Outcome data
The results for outcomes before adjusting for covariates are displayed in Additional file 1: Table S10. Table 4 summarizes the main clinical outcomes data. When compared to steroid alone by day 28, the use of IL-6RAs was associated with adjusted aIRR of 1.12 (95% CI 0.88, 1.4) for VFDs, while combination therapy was associated with aIRR of 0.83 (95% CI 0.6, 1.14) (model 1). Exploratory analysis findings (model 2) were comparable to primary analysis. Sensitivity analysis of target trial design (model 3) showed consistent results when compared to steroids alone (aIRR [95% CI]): IL-6RAs (1.13 [0.87, 1.45]), combination (0.64 [0.34, 1.23]). Linear regression analysis was performed stratified by steroid dose (Additional file 1: Table S11). Compared to IL-6RAs, low-dose steroid was associated with VFDs β value of 0.62 (95% CI − 1.54, 2.78) and high-dose steroid was associated with VFD β value of − 1.19 (95% CI − 3.85, 1.47). Factors associated with a higher likelihood of VFDs were non-use of paralytics, therapeutic anticoagulation use, and low FiO2.
When compared to steroid alone by day 28, IL-6RAs was associated with adjusted odds ratio (aOR) of 0.68 (95% CI 0.44, 1.07) for the mortality rate, while combination was associated with aOR of 1.07 (95% CI 0.67, 1.70) (model 1). Similarly, exploratory analyses (model 2), sensitivity analysis findings of target trial approach (model 3), and hospital mortality were consistent with primary analysis when compared to steroids (hospital mortality aOR [95% CI]: IL6-RA (0.68, [0.43, 1.09]), combination (1.23, [0.72, 2.11]). Regarding the AEs, liver dysfunction was higher in IL-6RAs (p = 0.04), while bacteremia rate did not differ among groups (Table 5). Detailed data of other outcomes are available in Additional file 1: Tables S12–S16, Figures S1–S5, and Additional file 3. Binary logistic regression was used to assess 28-day mortality stratified by steroid dose and showed no significant association between the use of steroids (low- or high-dose) and mortality. Post hoc analysis for the outcomes (VFDs and mortality) stratified by age (> 60 vs. ≤ 60) showed that younger patients perhaps had more favorable outcomes with IL-6RA compared with the older population. We examined the changes in biomarkers (LDH, CRP, and ferritin) over time using linear mixed models for repeated measurements. On day 28, both IL-6RAs [coefficients β = − 0.98] and combination groups [coefficients β = − 3.39] had a clinically meaningful reduction in CRP than the steroids-only group (reference group). Similarly, IL-6RAs [coefficients β = − 51.65] and combination groups [coefficients β = − 32.19] had a clinically meaningful reduction in ferritin than the steroid. No reduction was observed in LDH levels in IL-6RAs or combination groups.
Discussion
The IL-6RAs were investigated in multiple RCTs, and some found lower duration of ICU and hospital stay, lower MV and death composite rates, and an increased number of organ support-free days in COVID-19 patients requiring respiratory support [26]. Herein, we reported characteristics and outcomes of adult ICU COVID-19 patients, who required iMV, and received IL-6RAs or steroids within a large, multinational registry over the past 11 months. We observed that the majority of our study cohort had a baseline CRP level of > 75 mg/L, indicating that our study population was skewed toward a hyperinflammatory phenotype and had higher baseline levels of critical illness, thereby supporting the mechanism of action of immunomodulators. Moreover, the number of tocilizumab and sarilumab doses that were administered in our study were comparable to those reported in prior RCTs, where the majority of the population received one dose of either drug.
Notably, our study included only patients on iMV (i.e., more severe end of the critical care trajectory), while recent RCTs included patients with varying degrees of respiratory support (iMV at baseline constitute 29% in REMAP-CAP, 14% in RECOVERY, 16% in TOCIBRAS, and 37% in COVACTA) [26]. We observed that IL-6RAs were associated with improvement in VFDs and 28-day mortality. We hypothesized possible reasons to explain these findings. First, monoclonal antibodies reside almost exclusively in the blood plasma and extracellular fluid due to their large size and hydrophilicity. Moreover, IL-6RAs have a long half-life (e.g., half-life of tocilizumab is roughly 13 days), resulting in a longer and persistent effect [5, 27]. Importantly, the incidence of secondary bacterial pneumonia was numerically higher in combination than IL-6RAs monotherapy group, possibly due to the additive immunosuppressant effect with combination therapy. These findings may indirectly relate to worse ICU mortality and prolonged ventilation days in combination group compared with IL-6RAs monotherapy. Likewise, recent studies have demonstrated the benefit of IL-6RAs in terms of the reduction in biomarkers, specifically CRP and ferritin levels [27]. Our study showed a clinically meaningful reduction in CRP and ferritin levels with IL-6RA use, perhaps another explanation for the observed favorable outcomes with this group. Lastly, there are potential other factors that could influence the observed outcomes over time. Changes in the severity of critical care patients, health system operational strain, the emergence of new COVID-19 variants, racial and ethnic differences in populations studied, and differences in the study conduction time, among others.
It is worth mentioning that the prescribing pattern and timing of administration observed in data registry for steroids and IL-6RA utilization were inconsistent with the best practice recommendation to optimize the effectiveness of immunomodulators. For example, we observed that only 55.6% of steroid administration occurred on day 0 of ICU admission. Ideally, this percentage should be closer to 100% in patients with iMV who are admitted to ICU, particularly since the announcement of RECOVERY steroids domain, indicating that the equipoise for withholding corticosteroids is no longer justifiable given the convincing evidence in favor of steroid use which now become standard care for ICU COVID-19 patients requiring MV [7]. One can argue that a portion of our data were collected before June 2020, when steroids use was limited due to the concerns of delayed viral clearance as shown in Middle East respiratory syndrome coronavirus [28]. Moreover, we also observed that IL-6RA administration was 39.48% on day 0 of ICU admission, 20.3% on day 1, and 11% on day 2, respectively. Ideally, this percentage in ICU patients with iMV should also be higher at baseline given the benefit of early administration of IL-6RAs, as observed in previous RCTs. In the REMAP-CAP, more than 75% of the participants received IL-6RAs within 3 days of hospital admission (i.e., early in their critical care trajectory) [8]. In WHO meta-analysis, a lower 28-day mortality rate was more marked among patients who received supplemental oxygen, NIV, and HFNC at randomization [12]. Similarly, the Bayesian reanalysis of RECOVERY trial showed that probabilities for a clinically significant mortality reduction (absolute risk difference > 3%) were 77%, 96%, and 56% in patients on simple oxygen, NIV, and iMV, respectively [14]. Taken together, the immunomodulatory effect of IL6-RAs and steroid appears to be most beneficial shortly following clinical deterioration at systemic hyper-inflammation onset and ideally before intubation, as their effect appears to be less pronounced if administered late for subsets of patients with iMV [29].
Additionally, we observed different types and doses of steroids, including high-dose steroids (19.2% of our study cohort). The REMAP-CAP included fixed duration steroids and shock-dependent hydrocortisone while RECOVERY used low-dose dexamethasone 6 mg IV daily. The Italian National Institute for Infectious Diseases recommends 5 days of methylprednisolone 1 mg/kg or dexamethasone 20 mg daily (defined as high-dose steroids in our study) [30]. This regimen is higher than the fixed dexamethasone dose used in RECOVERY and described in non-COVID ARDS literature [20, 21]. Prior studies suggested that moderate- to high-dose steroid regimens resulted in a greater reduction in mortality, organ dysfunction, MV requirement, and no increase in medical or infectious complications compared to low-dose regimens in ICU COVID-19 patients [31, 32]. In COVID STEROID 2 RCT (preprint), the use of 12 mg dexamethasone was compared to 6 mg dexamethasone in severe COVID-19 and there was no significant difference observed in the number of days alive without life support at day 28, or 28-day mortality. However, the 95% CI suggests that the results are most compatible with a benefit from higher dexamethasone dose (adjusted mean difference 1.3 days alive without life support [95% CI 0, 2.6], and 14% reduction in mortality [95% CI 0.68, 1.08]). An upcoming Bayesian analysis of COVID STEROID 2 RCT data will provide a more clinically meaningful interpretation to aid in the decision-making process [33]. Whether the beneficial immunomodulatory effects of IL-6R blockade could be achieved more easily and with less cost by using a different steroid regimen (higher dose) and its safety is unclear and need to be investigated in an adequately powered RCT [26].
Strengths of this study lie in its multinational nature. We used data from the largest COVID-19 registry and represented a spectrum of intensive care with racially and ethnically diverse cohorts. To our knowledge, we included relatively large numbers of patients on iMV at baseline, which was a limited subset of the population included in the previous trials. Additionally, we included laboratory-confirmed COVID-19 PCR tests, thereby minimizing selection or surveillance bias at each center. Lastly, prior observational studies could be biased by immortal time and indication bias [25, 34]. We used a novel statistical analysis to overcome these limitations and application of target trial design, which is likely a better approach to reduce immortal time bias and best resembling clinical practice. Although COVID-19 treatments were not used uniformly before matching and patients did not receive up-to-date standards of care, especially in early pandemic phases, we utilized rigorous methods to match the three groups concerning anticoagulation use, hydroxychloroquine, antivirals, and azithromycin. Importantly, this study highlights the risk of liver injury with IL-6 inhibition. Clinicians should be aware of these effects and weigh treatment risks and benefits accordingly. Whether this risk is intensified with repeated IL-6RA administration or related to patients’ critical presentation warrants investigation in future research.
We acknowledge some limitations. First, due to the observational nature of this study, the results for clinical outcome data are exploratory and possibly inconclusive due to insufficient power and frequentist statistical framework. Second, a fair number of patients were excluded due to missing outcomes and incomplete data for time-dependent confounders to be used in MSM. We may have missed patients who would have met the eligibility criteria, but were not included because of those reasons (possible elimination for non-random missingness). Although we used the best available methods to compare well-balanced groups, controlling for confounders in observational study may remain incomplete despite all efforts. Notably, some imbalances in potential confounders (e.g., sex, cardiovascular disease, respiratory diseases, and treatments offered) were observed after weighting (SMD > 0.1). Such potential residual confounding may have a role in the observed outcome findings. Moreover, there was a large proportion of incomplete data for SOFA and APACHE II scores due to the heavy burden of workload experienced by participating clinicians during the pandemic. Furthermore, our study included a relatively small sample size to examine changes in biomarkers (LDH, CRP, and ferritin) with immunomodulators and a lack of serial data to evaluate the association between the trajectory of other biomarkers and outcome (e.g., the potential role of IL-6 level in predicting IL-6RA responses). Steroid duration was also highly variable with inconsistent data entry, making it impossible to minimize its effect fully. Furthermore, this preliminary report is mainly focused on the first COVID-19 wave (March 01, 2020, to January 10, 2021) and before COVID-19 vaccines became widely available. We plan to include the COVID-19 vaccination status in subsequent reports of the data registry. Finally, our follow-up was limited to 28 days. Considering the risk of secondary infections and the apparent long half-life of IL-6RAs, it is logical to consider the need for long-term infection risk follow-up. Therefore, our data likely did not capture the true incidence of secondary infections attributed to IL-6RA or steroids, and a longer follow-up is needed to help characterize long-term sequelae, especially mucormycosis, aspergillosis, pneumocystis pneumonia, and multi-drug resistant organisms. Therefore, results should be interpreted within the limitations of the retrospective registry studies.
Through this preliminary report, we identified areas of improvement in prescribing patterns for steroids and IL-6RA utilization over the past 11 months, particularly in the timing of administration in patients requiring iMV. As the evidence has now become clearer, we expect that subsequent iterations of the registry data for steroid and IL-6RA utilization will be more consistent with the recent data coinciding with the accrual of scientific evidence.
Conclusions
This study reports the features of critically ill mechanically ventilated COVID-19 patients receiving IL-6RA and steroid therapy. We observed that the prescribing pattern in the data registry over the past 11 months for these agents, particularly in the timing of administration, was inconsistent with the best practice recommendation set forth to optimize the effectiveness of immunomodulators, which may have resulted in the outcome findings observed here. The lessons learned from this study may help to identify areas of improvement in prescribing patterns, improve the decision-making process, and enhance our understanding of IL-6RA safety with different steroid regimens. Further studies are needed to evaluate the drivers of hospital variation and their impact on clinical outcomes.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- APACHE II:
-
Acute Physiology and Chronic Health Evaluation II
- ICU:
-
Intensive care unit
- IRB:
-
Institutional Review Board
- LOS:
-
Length of stay
- iMV:
-
Invasive mechanical ventilation
- SOFA:
-
Sequential Organ Failure Assessment
- COVID-19:
-
Coronavirus disease 2019
- IL-6RA:
-
Interleukin-6 receptor antagonists
- REMAP-CAP:
-
Randomized, Embedded, Multi-factorial, Adaptive Platform Trial for Community-Acquired Pneumonia
- RECOVERY:
-
Randomized Evaluation of COVID-19 Therapy
- NIV:
-
Non-invasive ventilation
- HFNC:
-
High-flow nasal cannula
- WHO:
-
World Health Organization
- MSM:
-
Marginal structural model
- SMD:
-
Standardized mean difference
References
Rizvi MS, Gallo De Moraes A. New decade, old debate: blocking the cytokine pathways in infection-induced cytokine cascade. Crit Care Explor. 2021;3(3):e0364. https://doi.org/10.1097/CCE.0000000000000364.
Zhang C, Wu Z, Li JW, Zhao H, Wang GQ. Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality. Int J Antimicrob Agents. 2020;55(5): 105954. https://doi.org/10.1016/j.ijantimicag.2020.105954.
Moore J, June CH. Cytokine release syndrome in severe COVID-19. Science. 2020;368(6490):473–4. https://doi.org/10.1126/science.abb8925.
Amer M, Bawazeer M, Dahhan T, Kseibi E, Butt A, Abujazar M, et al. The current use of anti-IL6 and corticosteroids in COVID-19 patients with cytokine-release syndrome. Saudi Crit Care J. 2020;4(5):21–4. https://doi.org/10.4103/sccj.sccj_38_20.
Parr JB. Time to reassess tocilizuma’s role in COVID-19 pneumonia. JAMA Intern Med. 2021;181(1):12–5. https://doi.org/10.1001/jamainternmed.2020.6557.
Rubin EJ, Longo DL, Baden LR. Interleukin-6 receptor inhibition in COVID-19—cooling the inflammatory soup. N Engl J Med. 2021;384(16):1564–5. https://doi.org/10.1056/NEJMe2103108.
RECOVERY Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021;384(8):693–704. https://doi.org/10.1056/NEJMoa2021436.
REMAP-CAP Investigators, Gordon AC, Mouncey PR, Al-Beidh F, Rowan KM, et al. Interleukin-6 receptor antagonists in critically ill patients with Covid-19. N Engl J Med. 2021;384(16):1491–502. https://doi.org/10.1056/NEJMoa2100433.
RECOVERY Collaborative Group, Horby PW, Pessoa-Amorim G, et al. Tocilizumab’ in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021;397(10285):1637–45. https://doi.org/10.1016/S0140-6736(21)00676-0.
COVID-19 real-time learning network. IDSA treatment guideline for COVID-19. 2021. https://www.idsociety.org/covid-19-real-time-learning-network/therapeutics-and-interventions/Tocilizumab-IL-6-Inhibitors/. Accessed 17 Mar 2021.
NIH guideline for COVID-19. 2021. https://www.covid19treatmentguidelines.nih.gov/whats-new/. Accessed 17 Mar 2021.
The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Domingo P, Mur I, Mateo GM, del Mar Gutierrez M, Pomar V, et al. Association between administration of IL-6 antagonists and mortality among patients hospitalized for COVID-19: a meta-analysis. JAMA. 2021;326(6):499. https://doi.org/10.1001/jama.2021.11330.
Rochwerg B, Agarwal A, Siemieniuk RA, Agoritsas T, Lamontagne F, Askie L, et al. A living WHO guideline on drugs for covid-19. BMJ. 2020;370: m3379. https://doi.org/10.1136/bmj.m3379.
Albuquerque AM, Tramujas L, Sewanan LR, Brophy JM. Tocilizumab in COVID-19—a Bayesian reanalysis of RECOVERY. medRxiv. 2021. https://doi.org/10.1101/2021.06.15.21258966.
Garcia MA, Johnson SW, Sisson EK, Sheldrick CR, Kumar VK, Boman K, et al. Variation in use of anti-viral and anti-inflammatory medications in patients hospitalized with COVID-19: results from the International Viral Infection and Respiratory Illness Universal Study (VIRUS). Am J Respir Crit Care Med. 2021;203(9):A3839.
Walkey AJ, Kumar VK, Harhay MO, Bolesta S, Gajic O, et al. The viral infection and respiratory illness universal study (VIRUS): an international registry of coronavirus 2019-related critical illness. Crit Care Explor. 2020;2(4): e0113. https://doi.org/10.1097/CCE.0000000000000113.
Walkey AJ, Sheldrick RC, Kashyap R, Kumar VK, Boman K, Bolesta S, et al. Guiding principles for the conduct of observational critical care research for coronavirus disease 2019 pandemics and beyond: the society of critical care medicine discovery viral infection and respiratory illness universal study registry. Crit Care Med. 2020;48(11):e1038–44. https://doi.org/10.1097/CCM.0000000000004572.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. https://doi.org/10.1016/j.ijsu.2014.07.013.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355: i4919. https://doi.org/10.1136/bmj.i4919.
Villar J, Ferrando C, Martínez D, Ambrós A, Muñoz T, Soler JA, et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med. 2020;8(3):267–76. https://doi.org/10.1016/S2213-2600(19)30417-5.
Chaudhuri D, Sasaki K, Karkar A, Sharif S, Lewis K, Mammen MJ, et al. Corticosteroids in COVID-19 and non-COVID-19 ARDS: a systematic review and meta-analysis. Intensive Care Med. 2021;47(5):521–37. https://doi.org/10.1007/s00134-021-06394-2.
Yehya N, Harhay MO, Curley MAQ, Schoenfeld DA, Reeder RW. Reappraisal of ventilator-free days in critical care research. Am J Respir Crit Care Med. 2019;200(7):828–36. https://doi.org/10.1164/rccm.201810-2050CP.
Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–60. https://doi.org/10.1097/00001648-200009000-00011.
Almirall D, Griffin BA, McCaffrey DF, Ramchand R, Yuen RA, Murphy SA. Time-varying effect moderation using the structural nested mean model: estimation using inverse-weighted regression with residuals. Stat Med. 2014;33(20):3466–87. https://doi.org/10.1002/sim.5892.
Vail EA, Gershengorn HB, Wunsch H, Walkey AJ. Attention to immortal time bias in critical care research. Am J Respir Crit Care Med. 2021;203(10):1222–9. https://doi.org/10.1164/rccm.202008-3238CP.
Angriman F, Ferreyro BL, Burry L, Fan E, Ferguson ND, Husain S, et al. Interleukin-6 receptor blockade in patients with COVID-19: placing clinical trials into context. Lancet Respir Med. 2021;9(6):655–64. https://doi.org/10.1016/S2213-2600(21)00139-9.
Brosnahan SB, Chen XJC, Chung J, Altshuler D, Islam S, Thomas SV, et al. Low-dose tocilizumab with high-dose corticosteroids in patients hospitalized for COVID-19 hypoxic respiratory failure improves mortality without increased infection risk. Ann Pharmacother. 2021. https://doi.org/10.1177/10600280211028882.
Arabi YM, Mandourah Y, Al-Hameed F, Sindi AA, Almekhlafi GA, Hussein MA, et al. Corticosteroid therapy for critically ill patients with Middle East respiratory syndrome. Am J Respir Crit Care Med. 2018;197(6):757–67. https://doi.org/10.1164/rccm.201706-1172OC.
Butler E, Munch MW, Venkatesh B. Time for tocilizumab in COVID-19? Intensive Care Med. 2021;47(6):692–4. https://doi.org/10.1007/s00134-021-06441-y.
Nicastri E, Petrosillo N, Ascoli Bartoli T, Lepore L, Mondi A, Palmieri F, et al. National institute for the infectious diseases “L. Spallanzani”, IRCCS recommendations for COVID-19 clinical management. Infect Dis Rep. 2020;12(1):8543. https://doi.org/10.4081/idr.2020.8543.
Monedero P, Gea A, Castro P, Candela-Toha AM, Hernández-Sanz ML, Arruti E, et al. Early corticosteroids are associated with lower mortality in critically ill patients with COVID-19: a cohort study. Crit Care. 2021;25(1):2. https://doi.org/10.1186/s13054-020-03422-3.
Tomazini BM, Maia IS, Cavalcanti AB, Berwanger O, Rosa RG, Veiga VC, et al. Effect of dexamethasone on days alive and ventilator-free in patients with moderate or severe acute respiratory distress syndrome and COVID-19: the CoDEX randomized clinical trial. JAMA. 2020;324(13):1307–16. https://doi.org/10.1001/jama.2020.17021.
Munch MW, Myatra SN, et al. Dexamethasone 12 mg versus 6 mg for patients with COVID-19 and severe hypoxia: an international, randomized, blinded trial. medRxiv. 2021. https://doi.org/10.1101/2021.07.22.21260755.
Tleyjeh IM, Kashour Z, Damlaj M, Riaz M, Tlayjeh H, Altannir M, et al. Efficacy and safety of tocilizumab in COVID-19 patients: a living systematic review and meta-analysis. Clin Microbiol Infect. 2021;27(2):215–27. https://doi.org/10.1016/j.cmi.2020.10.036.
Acknowledgements
We thank the SCCM Discovery VIRUS data registry and the Collaborative Co-authors listed in Additional file 4 for providing and maintaining the database of hospitalized COVID-19 patients. We are grateful to Professor Yaseen M. Arabi at King Saud bin Abdulaziz University for his inputs of this manuscript.
Funding
The VIRUS Registry is supported, in part, by the Gordon and Betty Moore Foundation, and Janssen Research & Development, LLC.
Author information
Authors and Affiliations
Consortia
Contributions
MA: proposed the study, led the manuscript writing, revisions, and did the data collection. AK: conducted the statistical analysis of this study, and post hoc analysis as requested in the peer-review process. All authors made substantial contributions to the concept, design, data collection, and have further participated in the analysis and interpretation of the data. All authors participated in revising the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
All authors agreed to this publication.
Competing interests
Drs. Kumar’s, Walkey’s, and Kashyap’s institutions received funding from the Gordon and Betty Moore Foundation. Drs. Kumar’s and Kashyap’s institutions received funding from Janssen Research & Development, LLC.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Additional data and statistical analyses.
Additional file 2.
Details for marginal structural model (MSM).
Additional file 3.
Labs and biomarkers data on day 7, 14, 21.
Additional file 4.
Collaborative authorship list.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Amer, M., Kamel, A.M., Bawazeer, M. et al. Clinical characteristics and outcomes of critically ill mechanically ventilated COVID-19 patients receiving interleukin-6 receptor antagonists and corticosteroid therapy: a preliminary report from a multinational registry. Eur J Med Res 26, 117 (2021). https://doi.org/10.1186/s40001-021-00591-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-021-00591-x