Abstract
Background
Healthcare-associated infection is a serious global problem, particularly in developing countries. In North African countries, comprehensive research on the incidence and effects of such infections is rare. This study evaluated the epidemiology and determined the impact of healthcare-associated infections in Libyan national teaching hospitals.
Methods
A prospective longitudinal study was carried out in Libya’s four largest teaching and referral hospitals (Tripoli Medical Center, Tripoli-Central Hospital, Benghazi Medical Center, and Sabha Medical Center) from November 1, 2021, to October 31, 2022. The epidemiological events and the parameters incorporated in this study were based on the data published by the Libyan Centers for Disease Control. The surveillance was carried out on all patients admitted to the wards of medicine, surgery, intensive care, gynecology & obstetrics, and pediatrics in all four hospitals. Trained staff reviewed the medical records and compared the percentages of patients with healthcare-associated infections. Bio-statistical and multivariable logistic regression analyses were carried out to test the variables associated with healthcare-associated infections and the resulting deaths.
Results
A total of 22,170 hospitalized patients in four hospitals were included in the study. Hospital-acquired infection was reported in 3037 patients (13.7%; 95% CI: 12.9–14.4%). The highest incidence was in Benghazi Medical Center (17.9%; 95% CI: 16.9–18.7%), followed by Sabha Medical Center (14.8%; 95% CI:14.9-16.51%). Surgical site infection was the most prevalent (31.3%), followed by ventilator-associated pneumonia (29.3%), urinary tract infection (26.8%), and bloodstream infection (12.6%). Patients with healthcare-associated infections experienced severe morbidity requiring intervention. New antimicrobial regimens were needed for 1836 patients (93%), and 752 patients (34%) required admission to intensive care. Surgical intervention, respiratory support, and inotropes were also needed as a consequence of HAI events.
Conclusions
The high incidence of healthcare-associated infections in Libyan hospitals should be considered a major problem and a serious burden. This should alert healthcare authorities at the national and hospital levels to the urgent need for preventive and control strategies to combat hospital-acquired infections.
Similar content being viewed by others
Background
Hospital-acquired or healthcare-associated infection (HAI), formerly called nosocomial infection) has been defined as “an infection occurring in a patient in a hospital or other healthcare facility in whom the infection was not present or incubating on admission to that hospital/facility” [1]. However, depending on the incubation period and the length of stay, some of these infections may be manifested only after patient discharge. The commonly reported HAIs are surgical site infections (SSIs), urinary tract infections (UTIs), pneumonia, and bloodstream infections [2]. A recent European study revealed that of every 20 patients hospitalized, at least one acquired a preventable HAI [3]. Most HAIs involve Staphylococcus aureus, P. aeruginosa, Klebsiella pneumonia, or the Acinetobacter species highly resistant to multiple antimicrobials, and the lack of new antimicrobials increases the huge burden in Europe [3, 4]. Similar findings have been reported in Southeast Asian countries, where the overall incidence ratio of HAI was 9.1% and the most common microorganisms were P. aeruginosa, Klebsiella species, and Acinetobacter baumannii [4].
Hospital-associated Infections have a large impact on morbidity and mortality worldwide. They prolong hospital stays, substantially increase healthcare costs, and pose a threat to the safety of patients and healthcare workers [5]. Given the wide range of microorganisms and hospitals involved, reliable data on HAI at national and international levels are difficult to get [5, 6]. Different studies have revealed a fragmented picture of the endemic burden of HAI in the world. Assessment of the global burden of HAI has been hampered by the lack of accurate data describing endemic infections at national and regional levels, particularly in resource-limited countries [6]. An epidemiological study carried out by the World Health Organization (WHO) in 14 countries reported that the overall incidence of HAIs was 7.6% in North America and Europe and 10.1% in Asia, Latin America, and Sub-Saharan Africa [7].
Europe’s overall HAI incidence ratio ranged from 3·5% to 14·8%. About 2–3 million people are affected annually, with an economic burden of €800 million [8]. The Centers for Disease Control and Prevention (CDC) estimated that HAIs in American hospitals account for approximately 1.7 million infections and 99,000 associated deaths each year, with an estimated excess healthcare cost of $28–33 billion each year [9].
In African countries, the magnitude of HAI is not clear and it is complicated by economic constraints and internal conflicts that make it difficult to control [10, 11]. The limited number of healthcare professionals and overcrowding in hospitals result in inadequate infection control practices. On top of these, the lack of infection control policies, guidelines, and trained personnel makes the problem even worse. However, the magnitude of the problem remains largely unknown, and in most cases, it is underestimated due to the complex nature of its diagnosis and the lack of proper surveillance [12].
Only a few African countries have established national surveillance systems for HAI, as emphasized by the WHO patient safety module [13]. In Ethiopia, HAI incidence reached up to 40%. The surgical site, urinary tract, and bloodstream infections were the commonest. The type of surgery, patients’ underlying medical conditions, and the type of ward were important factors associated with increased risk of HAI in Ethiopia [13, 14]. Similar results were reported in West Africa and Tanzania, where the infection incidence reached over 15%, including highly resistant Gram-positive and Gram-negative bacteria [15, 16]. In Uganda, the incidence of HAIs was reported to be over 14%, with UTI and SSI ratios reaching 38% and 21.9%, respectively [17]. However, encouraging results were reported in South Africa, where the overall HAI incidence was only 7.7% [18].
Literature on HAIs in North African countries is scarce. Libya is the second largest country in North Africa and has the longest coast in the Mediterranean basin facing Europe. Studies on HAIs have rarely been reported, and the country has no system for estimating the burden of such infections. The extreme scarcity of data on hospitalized patients in Libya limits the estimation of the impact of HAIs on mortality and healthcare costs. Therefore, this prospective active surveillance study aimed to evaluate the epidemiology and investigate the spectrum, risk factors, and impact of HAI in Libyan referral hospitals. The findings provide baseline information for healthcare providers to implement proper prevention strategies to control the incidence and complications of HAIs.
Methods
Healthcare settings
This study was conducted at four teaching and referral hospitals in Libya: Tripoli Medical Center (TMC), Tripoli Central Hospital (TCH), Benghazi Medical Center (BMC), and Sabha Medical Center (SMC). TMC is the largest hospital in the country, with over 1450 beds, and THC has about 1000 beds. Together, these two hospitals serve a population of over four million people. BMC is the largest hospital in the eastern region, with 1200 beds serving over two million people. SMC, located in the southern region, has 1000 beds and serves over one million people.
Study design and data collection
This is a prospective surveillance study conducted from November 1, 2021, to October 31, 2022. The surveillance of HAI events and data collection followed the surveillance definition of HAI published by the Centers for Disease Control/National Healthcare Safety Network (CDC/NHSN) [19].
The study included all patients admitted to the medicine, surgery, intensive care, gynecology & obstetrics, and pediatrics wards during the study period. Epidemiological information, including demographics (age, sex, hospitalization period), treatment received, and clinical, diagnostic, and HAI event data, were collected from each patient. Data were collected weekly for all patients admitted for 48 h or longer without evidence of bacterial infection at admission. HAI definitions were based on the CDC/NHSN criteria as in our previous studies and only the first infection per patient was counted [10, 20]. They included surgical site infection (SSI), bloodstream infection (BSI), urinary tract infection (UTI), and ventilator-associated pneumonia (VAP) [20]. Trained physicians and senior nurses collected the data under the supervision of a senior clinical epidemiologist from the Department of Medical Microbiology, Faculty of Medicine, Tripoli (M.A. Daw).
Statistical analysis
Statistical analysis and data management were carried out using Statistical Software version 13.0 IC (Stata Corp LP; College Station, USA). HAI incidence was calculated for a 95% confidence interval (95% CI). Chi-square test and logistic regression analysis were used to test variables for association with HAI events and death from HAI. The statistical level was considered to be significant at a p-value of < 0.01.
Results
A total of 22,170 patients were enrolled from four teaching hospitals in Libya. The distribution of the patients across the hospitals was as follows: 7650 (34.5%) were from TMC, 3921 (17.7%) were from TCH, 6259 (28.2%) were from BMC, and 4340 (19.6%) were from SMC. The clinical and demographic characteristics of the patients are summarized in Table 1. The median age of the patients was 39.6 years, with 11,959 (53.9%) females and 10,211 (46.1%) males. More than 60% of the patients were over 40 years of age, while only 18% were below 30 years. The distribution of the patients across the different wards was as follows: 33.2% in medical wards, 30.3% in surgical wards, 17.3% in gynecology & obstetrics, 12.9% in pediatrics, and 5.7% in intensive care units (ICU). Underlying non-communicable diseases among the patients with HAI were reported in 4368 patients (19.7%), with the following distribution: hypertension (27.3%), cardiovascular diseases (23.9%), diabetes mellitus (22.3%), renal failure (19.7%), and cancer (6.8%).
Hospital-acquired infections within Libyan national hospitals (Table 2) were observed in 3037 patients, giving an overall incidence of 13.7% (95% CI: 12.9-14.4%) (Table 2). The highest HAI incidence was observed in BMC (17.9%; 95% CI: 16.9-18.7%), followed by SMC (14.8%; 95% CI: 14.5.9-16.5%) and TCH (14.2%; 95% CI: 13.7-15.8%). The lowest incidence was in TMC (9.4%; 95% CI: 8.7-10.7%). Overall, the intensive care units had the highest HAI incidence (29.8%), followed by the pediatrics and surgery wards (14.7% and 13.7%, respectively). The lowest incidence was found in the medical wards (11.8%) and obstetrics & gynecology wards (11.3%). Table 3 shows the logistic regression analysis to obtain the odds ratio in the presence of more than one explanatory variable. Patients with HIS were more likely to be females, particularly from SMC and BMC, and aged over sixty (OR 0.7201; 95% CI, 0.6350–0.8166).
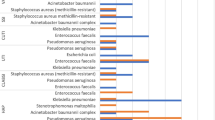
The incidence of the different types of infections in each hospital is shown in Fig. 1. Ventilator-associated pneumonia (41.3%), and urinary tract infection (37.2%), were the most frequent, followed by surgical site infection (34,7%) and bloodstream infection (22.1%). Benghazi Medical Center reported the highest incidence of all HAI, particularly ventilator-associated pneumonia, followed by Tripoli Central Hospital and then Sabha Medical Center (Fig. 1-Source file 1).
The duration of hospitalization ranged from 3 to 37 days. The mean duration of hospital stay for patients with HAI (14.8 days; SD ± 9.7) was longer than for those without HAI (8.3 days; ± 6.98). There was a significant mean difference in hospital stay of 6.34 days (95% C.I: 5.86–17.41) between these two patient groups.
Different microorganisms were isolated and identified from the HAI patients (Table 4). E. coli (24.2%) was the most frequent one, followed by S. aureus (20.4%), Pseudomonas aeruginosa (11.9%), Klebsiella spp. (10.9%), Enterobacter spp. (16.4%) and Acinetobacter spp. (16.2%).
Some patients with HAI experienced severe morbidity that required intervention (Table 5). New antimicrobial regimens were needed for 1836 patients (93%) and 752 (34%) required ICU admission. In addition to surgical intervention, respiratory support, and inotropes were used when needed.
Table 6 shows the mortality associated with healthcare-associated infections in Libyan national hospitals. Overall, there were 386 deaths (12.8%) in patients with HAI, and the highest fatality ratio was reported among patients with ventilator-associated pneumonia (14.8%) followed by patients with bloodstream infection (10.3%), surgical site infection (3.7%) and urinary tract infection (3.1%).
Discussion
Herein, we present the first comprehensive study on the incidence and impact of HAI in the four largest referral hospitals in Libya. The overall HAI incidence in the four hospitals was 13.7%. BMC had the highest ratio (17.9%), followed by SMC (14.8%) and TCH (14.2%). The lowest was observed in TMC (9.4%).
HAI incidence varies greatly among countries, in developed countries such as Ireland and Germany reporting a ratio of about 3.5% according to a Euro-surveillance report, while developing countries and Sub-Saharan countries had ratios as high as 21.7% [21,22,23]. Our data are in concordance with other data reported in North African countries, such as Tunisia, Morocco, and Algeria, as they have an HAI ratio as high as 18%. Therefore, efforts at national and regional levels should be combined to reduce the impact of HAI in these countries [24, 25].
The HAI in Libyan hospitals was found to be 3.1%. It was influenced by sex, age, and ward of admission. Female patients had a higher incidence of HAI, with a 1.25:1 female-to-male ratio, which is supported by other studies conducted in other African countries. Older hospitalized patients (51 years and above) experienced a higher impact of HAI than younger patients, which agrees with studies reported from Russia and Ethiopia [26, 27]. Gram-negative bacilli, particularly E. coli, P. aeruginosa, and Klebsiella spp., and Gram-positive cocci, mainly S. aureus, were the most commonly isolated HAI-causing pathogens, which is consistent with studies from other African countries [22, 23].
Among the different hospital wards, the highest incidence of HAI was observed in the ICU (29.8%) followed by the pediatrics (14.7%), surgery (13.7%), medical (11.8%), and obstetrics & gynecology wards (11.3%). These ratios are similar to those reported from Tunisia and Ethiopia but lower than those in Morocco [28, 29].
The most common type of HAI in our study was ventilator-associated pneumonia (41.3%), followed by urinary tract infection (37.2%) and surgical site infection (34,7%). Those ratios are higher than those reported in the USA and France, but lower than in Nigerian studies [30,31,32,33,34]. The high SSI ratio in our study could be due to various factors, such as ineffective sterilization, inadequate wound dressing, and inadequate procedures during surgery. The admission ratio of patients whose surgery was classified as contaminated was high, particularly at BMC and SMC. The lack or insufficient implementation of guidelines and antimicrobial stewardship in Libya may also contribute to the higher incidence of SSI. Further research is needed to investigate the association between HAI and specific surgical procedures, as well as the implementation of guidelines for antimicrobial use [35].
The pneumonia infection ratio was similar to or lower than in studies carried out in other countries in the MENA region, such as Iran and Saudi Arabia, where pneumonia accounted for 28.9% and 70% of HAI, respectively. It is worth noting that studies in these countries mainly focused on ICU patients, which could contribute to the discrepancy [36, 37]. In our study, the ratio of admission to the intensive care unit varied among the four hospitals. BMC reported the highest ratio (27%), followed by TMC (19%) and SMC (15%).
Urinary tract infection was observed in 37.2%, of the patients. This is a higher percentage than reported in studies conducted in Lithuania (28.5%), Tanzania (31.1%), and Ethiopia (19.8%). Improper catheterization practices may contribute to a high UTI ratio. Several studies have indicated that 79.3% of UTIs can be prevented by avoiding catheterization in hospitals [38,39,40]. Bloodstream infection was the least frequently reported HAI (22.1.6%), which is in agreement with other studies carried out in North and Sub-Saharan African countries. Inadequate aseptic techniques during the collection of blood specimens or administration of intravenous drugs may contribute to bloodstream HAI. Therefore, proper attention to aseptic techniques is important [5, 41, 42].
Our study revealed that most of the reported HAIs were systemic infections rather than localized wound or soft tissue infection. The overlapping of multiple HAI in patients was also noticeable and thus it deserves specific attention due to the magnitude of the problem and the threat to the patient population getting service at the hospital. In line with this, the most frequently isolated bacteria were E coli, S. aureus, and Klebsiella species. These bacteria are also known to cause community-acquired infection in Libya [20]. This may suggest that such bacteria might have colonized the hospital environment and devices. Therefore, further studies are needed to evaluate the interaction between hospital and community-acquired infections.
HAI has a significant impact on morbidity and mortality. They prolong hospitalization, increase the requirement for ICU admission, and necessitate additional diagnostic and therapeutic interventions. In our study, 34% of the patients were admitted to the ICU, and over 90% needed antimicrobials. These factors led to extended hospital stays, resulting in overcrowding (particularly in the ICU) and difficulties in admitting new patients. Furthermore, patients with bloodstream infections can serve as reservoirs for the transmission of drug-resistant pathogens. Our findings are in concordance with other studies carried out in South African hospitals. These factors reflect the consequences of HAI and may act as predictors of hospital mortality. However, such associations need further study [43,44,45]. Surgical intervention, respiratory support, and device removal were needed for HAI events. Interestingly, they varied among the hospitals. The highest frequency of inappropriate management of HAI was seen in BMC, followed by SMC and then TMC. This is contrary to studies carried out in developed countries. This could be attributed to a lack of proper management, monitoring, and efficient safety procedures in our study settings [1, 46]. The crude mortality associated with HAI events in our study was high as it reached up to 12.8% compared with other studies published from other developing countries such as South Africa (5,3%) and Indonesia (8%). This may be attributed to a lack of ICU access, laboratory investigations, and antimicrobials for multi-drug resistant pathogens. This finding is important and deserves further explanation.
Strengths and limitations
A major strength of this study is its comprehensive perspective of HAI in Libya. To our knowledge, this is the largest study characterizing the epidemiological manifestations of HAI in the MENA region. Our findings should alert the decision-makers to the fact that HAI is endemic and represents a hidden and serious burden for the Libyan healthcare system. Hence, health authorities and decision-makers should take the actions needed to fulfill the requirements of the pledge of WHO’s First Global Patient Safety Challenge [47,48,49]. On the other hand, several limitations need to be considered when interpreting the results of this study. There could be misreporting of some surveillance data that may not reflect the real situation in the participating hospitals. Another limitation was the inability to follow up with every patient, particularly for surgical site infections, which were highly prevalent. We were unable to investigate the treatment and the clinical outcomes of HAIs due to differences in the hospitals studied [10, 11].
The scope of this study was principally limited by data availability. The incidence of antimicrobial resistance, particularly MRSA-causing HAI is alarmingly high, and resistant infections may be more expensive to treat. However, data limitations prevented us from determining the burden of antimicrobial resistance in the studied hospitals.
Despite these limitations, our study gives good insights into HAI in Libyan hospitals, particularly as the country has been involved in a major internal conflict since 2011. Our findings could be used as a reference for future studies and to plan HAI prevention strategies and research [50, 51]. The problem of HAI in Libya is particularly serious because there are no national programs for HAI prevention or mandatory reporting of data in healthcare settings [11, 20]. Unfortunately, lack of awareness and low levels of staff preparedness and knowledge are the main factors leading to poor infection control in Libya. Furthermore, there is no active surveillance of HAI, which is not seen as a priority in Libyan hospitals, and even in ICU settings. Therefore, education and comprehensive training programs for hospital staff should be provided. National guidelines have to be implemented. Doctors and nurses should be obliged to follow and fulfill the requirements for HAI prevention and control.
Conclusion and recommendations
The incidence of HAI is high in Libyan hospitals, where pneumonia and surgical site infection were the most common infections, followed by urinary tract infection and bloodstream infection. This is combined with a lack of proper clinical management, resulting in a heavy burden on the Libyan healthcare system. National guidelines for HAI and improvements in microbiological diagnosis and antibiotic susceptibility testing are crucial. The Libyan national health authority should implement appropriate management of HAI. Development of national guidelines for HAI and improvement of microbiological diagnosis and antibiotic susceptibility testing are needed.
Data Availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- TMC:
-
Tripoli Medical Center
- TCH:
-
Tripoli-Central Hospital
- BMC:
-
Benghazi Medical Center
- SMC:
-
Sabha Medical Center
- HAI:
-
Hospital-acquired infection
- BSI:
-
bloodstream infection
- ICU:
-
intensive care unit
- SSI:
-
surgical site infection
- UTI:
-
urinary tract infection
- CDC:
-
Center for Disease Control
References
Haque M, McKimm J, Sartelli M, Dhingra S, Labricciosa FM, Islam S, Jahan D, Nusrat T, Chowdhury TS, Coccolini F, Iskandar K, Catena F, Charan J. Strategies to Prevent Healthcare-Associated Infections: a narrative overview. Risk Manag Healthc Policy. 2020;13:1765–80. https://doi.org/10.2147/RMHP.S269315. PMID: 33061710; PMCID: PMC7532064.
Magill SS, Edwards JR, Bamberg W, et al. Emerging Infections Program Healthcare-Associated Infections and Antimicrobial Use Prevalence Survey Team. Multistate point-prevalence survey of health care-associated Infections. N Engl J Med. 2014;370(13):1198–208.
Cassini A, Plachouras D, Eckmanns T, et al. Burden of Six Healthcare Associated Infections on European Population Health: estimating incidence-based disability-adjusted life years through a Population prevalence-based Modelling Study. PLoS Med. 2016;13(10):e1002150.
-Ling ML, Apisarnthanarak A, Madriaga G. The Burden of Healthcare Associated Infections in Southeast Asia: a systematic literature review and Meta-analysis. Clin Infect Dis. 2015;60(11):1690–9.
-Haque M, Sartelli M, McKimm J, Abu Bakar M. Health care-associated Infections - an overview. Infect Drug Resist. 2018;11:2321–33. https://doi.org/10.2147/IDR.S177247. PMID: 30532565; PMCID: PMC6245375.
Ganter B. Regional strategy on healthcare associated Infections. The International Consultation on Prevention and Control of HealthcareAssociated Infections; Venice, Italy; April 26–28, 2004.
World Health Organization. Report on the burden of endemic health care-associated infection worldwide.
Fabry J. Surveillance of hospital-acquired Infections. Comparison of methods. The methodology. The International Consultation on Prevention and Control of Healthcare-Associated Infections; Venice, Italy; April 26–28, 2004.
Department of Health. Healthcare-Associated Infections. Department of Health, District of Columbia; Available from: http://doh.dc.gov/page/healthcare-associated-infections.
Daw MA, El-Bouzedi A, Dau AA. The assessment of efficiency and coordination within the Libyan health care system during the armed conflict-2011. Clin Epidemiol Global Health. 2016;4(3):120–7.
Daw MA. Libyan healthcare system during the armed conflict: challenges and restoration. Afr J Emerg Med. 2017;7(2):47–50. https://doi.org/10.1016/j.afjem.2017.04.010. Epub 2017 May 9. PMID: 30456107; PMCID: PMC6234156.
Houghton C, Meskell P, Delaney H, Smalle M, Glenton C, Booth A, Chan XHS, Devane D, Biesty LM. Barriers and facilitators to healthcare workers’ adherence with Infection prevention and control (IPC) guidelines for respiratory infectious Diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;4(4):CD013582. https://doi.org/10.1002/14651858.CD013582. PMID: 32315451; PMCID: PMC7173761.
Alemu AY, Endalamaw A, Bayih WA. The burden of healthcare-associated Infection in Ethiopia: a systematic review and meta-analysis. Trop Med Health. 2020;48:77. https://doi.org/10.1186/s41182-020-00263-2. PMID: 32939151; PMCID: PMC7487565.
Sahiledengle B, Tekalegn Y, Woldeyohannes D. The critical role of Infection prevention overlooked in Ethiopia, only one-half of health-care workers had safe practice: a systematic review and meta-analysis. PLoS ONE. 2021;16(1):e0245469. https://doi.org/10.1371/journal.pone.0245469. PMID: 33444417; PMCID: PMC7808611.
Afle FCD, Agbankpe AJ, Johnson RC, Houngbégnon O, Houssou SC, Bankole HS. Healthcare-associated Infections: bacteriological characterization of the hospital surfaces in the University Hospital of Abomey-Calavi/so-ava in South Benin (West Africa). BMC Infect Dis. 2019;19(1):28. https://doi.org/10.1186/s12879-018-3648-x. PMID: 30616550; PMCID: PMC6323744.
Allegranzi -SepidehBNB, Shamsuzzoha B, Syed BE, Didier Pittet. & (2011) Health-care-associated infection in Africa: a systematic review, Bulletin of the World Health Organization 2011;89:757–765. https://doi.org/10.2471/BLT.11.088179.
Okello TR, Kansiime J, Odora J. Invasive procedures and hospital acquired Infection (HAI) in a large hospital in northern Uganda. East Cent Afr J Surg. 2014;19(3):77–84.
Nair A, Steinberg WJ, Habib T, Saeed H, Raubenheimer JE. Prevalence of healthcare-associated Infection at a tertiary hospital in the Northern Cape Province, South Africa. South Afr Family Pract. 2018;60(5):162–7.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated Infection and criteria for specific types of Infections in the acute care setting. Am J Infect Control. 2008;36(5):309–32.
Wareg SE, Foster HA, Daw MA. Antimicrobial susceptibility patterns of Methicillin-resistant Staphylococcus aureus isolates collected from healthcare and community facilities in Libya show a high level of resistance to fusidic acid. J Infect Dis Therapy. 2014 Dec 8.
Suetens C, Latour K, Kärki T, Ricchizzi E, Kinross P, Moro ML, Jans B, Hopkins S, Hansen S, Lyytikäinen O, Reilly J. Prevalence of healthcare-associated Infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Eurosurveillance. 2018;23(46):1800516.
Gastmeier P, Kampf G, Wischnewski N, et al. Prevalence of nosocomial Infections in representative German hospitals. J Hosp Infect. 1998;38(1):37–49. https://doi.org/10.1016/S0195-6701(98)90173-6.
Allegranzi B, Nejad SB, Combescure C, Graafmans W, Attar H, Donaldson L, Pittet D. Burden of endemic health-care-associated Infection in developing countries: systematic review and meta-analysis. The Lancet. 2011;377(9761):228–41.
Kallel H, Bahoul M, Ksibi H, et al. Prevalence of hospital-acquired Infection in a Tunisian hospital. J Hosp Infect. 2005;59(4):343–7. https://doi.org/10.1016/j.jhin.2004.09.015.
Jroundi I, Khoudri I, Azzouzi A, Zeggwagh AA, Benbrahim NF, Hassouni F, Oualine M, Abouqal R. Prevalence of hospital-acquired Infection in a Moroccan university hospital. Am J Infect Control. 2007;35(6):412–6.
Hajdu A, Samodova O, Carlsson T, Voinova L, Nazarenko S, et al. A point prevalence survey of hospital-acquired Infections and antimicrobial use in a paediatric hospital in north-western Russia. J Hosp Infect. 2007;66:378–84. https://doi.org/10.1016/j.jhin.2007.04.018. PMID: 17573155.
Kumie A, Yehuala FM. Point prevalence of hospital-acquired Infections in two teaching hospitals of Amhara region in Ethiopia. Drug Healthc Patient Saf. 2016;8:71. https://doi.org/10.2147/DHPS.S107344. PMID: 27601932.
Yallew WW, Kumie A, Yehuala FM. Point prevalence of hospital-acquired Infections in two teaching hospitals of Amhara region in Ethiopia. Drug Healthc Patient Saf. 2016;8:71.
Razine R, Azzouzi A, Barkat A, et al. Prevalence of hospital-acquired Infections in the university medical center of Rabat, Morocco. Int Arch Med. 2012;5:26.
Miliani K, L’he´riteau F, Astagneau P. Non-compliance with recommendations for the practice of antibiotic prophylaxis and risk of surgical site Infection: results of a multilevel analysis from the INCISO Surveillance Network. J Antimicrob Chemother. 2009;64:1307–15. https://doi.org/10.1093/jac/dkp367. PMID: 19837713.
Garey KW, Dao T, Chen H, Amrutkar P, Kumar N et al. (2006) Timing of vancomycin prophylaxis for cardiac surgery patients and the risk of surgical site infections. Journal of Antimicrobial Chemotherapy 58: 645–650. https://doi.org/10.1093/jac/dkl279 PMID: 16807254.
Amoran O, Sogebi A, Fatugase O. Rates and risk factors Associated with Surgical Site Infections in a. Tertiary Care Center in South-Western Nigeria; 2013.
Kwong JC, Ratnasingham S, Campitelli MA, Daneman N, Deeks SL, Manuel DG, Allen VG, Bayoumi AM, Fazil A, Fisman DN, Gershon AS, Gournis E, Heathcote EJ, Jamieson FB, Jha P, Khan KM, Majowicz SE, Mazzulli T, McGeer AJ, Muller MP, Raut A, Rea E, Remis RS, Shahin R, Wright AJ, Zagorski B, Crowcroft NS. The impact of Infection on population health: results of the Ontario burden of infectious Diseases study. PLoS ONE. 2012;7(9):e44103. https://doi.org/10.1371/journal.pone.0044103. Epub 2012 Sep 4. PMID: 22962601; PMCID: PMC3433488.
Cassini A, Plachouras D, Eckmanns T, Abu Sin M, Blank HP, Ducomble T, Haller S, Harder T, Klingeberg A, Sixtensson M, Velasco E, Weiß B, Kramarz P, Monnet DL, Kretzschmar ME, Suetens C. Burden of six Healthcare-Associated Infections on European Population Health: estimating incidence-based disability-adjusted life years through a Population prevalence-based Modelling Study. PLoS Med. 2016;13(10):e1002150. https://doi.org/10.1371/journal.pmed.1002150. PMID: 27755545; PMCID: PMC5068791.
Smaoui H, Tali-Maamar H, Zouhair S, Bouheraoua S, Mefteh K, Bouskraoui M, Amiche A, Khris M, Deghmane AE, Taha MK, Study group. Implementation of a prospective study for enhancing surveillance of invasive bacterial Infections in North Africa. Int J Infect Dis. 2022;115:101–5. Epub 2021 Nov 27. PMID: 34843957.
Tabatabaei SM, Pour FB, Osmani S. (2015) Epidemiology of hospital-acquired Infections and related anti-microbial resistance patterns in a tertiary-care Teaching Hospital in Zahedan, Southeast Iran. Int J Infect 2.
Balkhy HH, Cunningham G, Chew FK, Francis C, Al Nakhli DJ et al. (2006) Hospital-and communityacquired infections: a point prevalence and risk factors survey in a tertiary care center in Saudi Arabia. International journal of infectious diseases 10: 326–333. https://doi.org/10.1016/j.ijid.2005.06.013 PMID: 16678467.
Vizujė G, Gierasimovič Z, Petrusˇevičienė D, Macijauskiene A. The prevalence of health care associated Infections and risk factors in a University Hospital. Medicina. 2012;48:399–403. PMID: 23128459.
Moyo S, Aboud S, Kasubi M, Maselle S. (2010) Bacteria isolated from bloodstream infections at a tertiary hospital in Dar es Salaam, Tanzania: antimicrobial resistance of isolates. SAMJ: South African Medical Journal 100: 835–838. https://doi.org/10.7196/samj.4186 PMID: 21414278.
Laloto TL, Gemeda DH, Abdella SH. Incidence and predictors of surgical site Infection in Ethiopia: prospective cohort. BMC Infect Dis. 2017;17:119. https://doi.org/10.1186/s12879-016-2167-x. PMID: 28158998.
Ataiyero Y, Dyson J, Graham M. Barriers to hand hygiene practices among health care workers in sub-saharan African countries: a narrative review. Am J Infect Control. 2019;47(5):565–73. Epub 2018 Nov 20. PMID: 30470526.
Fraser JL, Mwatondo A, Alimi YH, Varma JK, Vilas VJDR. Healthcare-associated outbreaks of bacterial Infections in Africa, 2009–2018: a review. Int J Infect Dis. 2021;103:469–77. https://doi.org/10.1016/j.ijid.2020.12.030. Epub 2020 Dec 17. PMID: 33333248.
Dramowski A, Whitelaw A, Cotton MF. Burden, spectrum, and impact of healthcare-associated Infection at a South African children’s hospital. J Hosp Infect. 2016;94(4):364–72. https://doi.org/10.1016/j.jhin.2016.08.022. Epub 2016 Sep 1. PMID: 27717603; PMCID: PMC7132424.
Barrasa-Villar JI, Aibar-Remón C, Prieto-Andrés P, Mareca-Doñate R, Moliner-Lahoz J. Impact on Morbidity, Mortality, and Length of Stay of Hospital-Acquired Infections by Resistant Microorganisms. Clin Infect Dis. 2017;65(4):644–652. https://doi.org/10.1093/cid/cix411. PMID: 28472416.
Schreiber PW, Sax H, Wolfensberger A, Clack L, Kuster SP, Swissnoso. The preventable proportion of healthcare-associated Infections 2005–2016: systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2018;39(11):1277–95. Epub 2018 Sep 20. PMID: 30234463.
Khan HA, Baig FK, Mehboob R. Nosocomial Infections: Epidemiology, prevention, control and surveillance. Asian Pac J Trop Biomed. 2017;7(5):478–82.
WHO. Clean Care is Safer Care. http://www.who.int/gpsc/en/ (accessed July 23, 2010).
Panesar SS, deSilva D, Carson-Stevens A, Cresswell KM, Salvilla SA, Slight SP, Javad S, Netuveli G, Larizgoitia I, Donaldson LJ, Bates DW, Sheikh A. How safe is primary care? A systematic review. BMJ Qual Saf. 2016;25(7):544–53. https://doi.org/10.1136/bmjqs-2015-004178. Epub 2015 Dec 29. PMID: 26715764.
Pittet D, Donaldson L. Clean Care is Safer Care: a worldwide priority. Lancet. 2005;366(9493):1246–7. https://doi.org/10.1016/S0140-6736(05)67506-X. PMID: 16214584; PMCID: PMC7134620.
Daw MA, El-Bouzedi A, Dau AA. Libyan armed conflict 2011: mortality, injury and population displacement. Afr J Emerg Med. 2015;5(3):101–7.
Daw MA, El-Bouzedi AH, Dau AA. Trends and patterns of deaths, injuries and intentional disabilities within the Libyan armed conflict: 2012–2017. PLoS ONE. 2019;14(5):e0216061. https://doi.org/10.1371/journal.pone.0216061. PMID: 31075119; PMCID: PMC6510427.
Acknowledgements
The thank the Department of Medical Microbiology, Faculty of Medicine, University of Tripoli, and the Libyan Society of Hospital Infection for their continuous support.
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
Authors’ contributionsMD, MHM, designed study, supervised of data collection, analysis, and manuscript writing. SW, AHB MOA acted equally on the supervision of data collection and writing of the manuscript. All the authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics declarations
The Medical Ethics Committee at the Faculty of Medicine, University of Tripoli approved the study and the waiver of individual informed consent by the Libyan National Ethics Committee under reference no. LNC/079/257/21.
Consent for publication
Not applicable – This manuscript does not contain any individual personal data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Daw, M.A., Mahamat, M.H., Wareg, S.E. et al. Epidemiological manifestations and impact of healthcare-associated infections in Libyan national hospitals. Antimicrob Resist Infect Control 12, 122 (2023). https://doi.org/10.1186/s13756-023-01328-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-023-01328-7