Abstract
Background
Infection prevention measures are the gold standard for preventing the spread of hospital-acquired infections (HAIs). COVID-19 pandemic caused major disruptions in infection prevention measures, and this has implications on the rate of HAIs. This study assessed the impact of COVID-19 pandemic on the rate and the types of HAIs at Sultan Ahmed Shah Hospital.
Method
This is a retrospective cohort study that compared the rate of HAIs from April to October 2019 (pre COVID period) and April to October 2020 (during COVID period). Data was collected through the review of patients’ electronic medical records.
Results
There were a total of 578 patients included in the selected wards during the pre- and during the pandemic. Thirty-nine episodes (12.1%) of HAIs were report in the pre COVID period and 29 (11.3%) during COVID-19. In both periods, hospital-acquired pneumonia (HAP) was the most frequent HAI among the patients. There was a rise in catheter-associated bloodstream infections (CLABSI) (0.8%) and ventilator associated pneumonia (VAP) (1.1%) during the COVID-19 period. The most common bacteria were methicillin-resistant Staphylococcus aureus (MRSA) (28.2%) and Enterococcus faecalis (17.9%) in the Pre COVID-19 period, and Pseudomonas aeruginosa (27.6%) and Stenotrophomonas maltophilia (6.9%) during COVID-19.
Conclusion
Our research concluded that the rates of HAIs during the COVID-19 pandemic were not significantly impacted by the improved in-hospital infection prevention efforts to control the pandemic. There is need for further efforts to promote adherence to preventive practices.
Similar content being viewed by others
Introduction
Hospital acquired infections (HAIs) are one of the most prevalent issues affecting hospitalized patients and dramatically increase mortality and morbidity [1]. HAIs impose a substantial financial burden due to the fact that they prolong patient hospitalizations and increase drug consumption [2]. According to the World Health Organisation (WHO), a huge number of people globally are affected by HAIs. Patients with at least one type of HAI account for 7% of patients in high-income countries and 10% of patients in developing countries [3]. Implementing effective HAI surveillance programmes and appropriate infection prevention procedures can reduce infection rates [4, 5]. However, pandemics bring new responsibilities that demand planning and regular interactions [6]. The significance of infection prevention and control (IPC) in preventing the spread of disease has been underscored by COVID-19 pandemics.
The global healthcare system has faced significant challenges as a result of COVID-19 pandemic [7]. Healthcare facilities were struggling to manage COVID-19 outbreak while also providing existing healthcare services [7,8,9]. Hospitals have implemented extensive IPC strategies in response to rising caseloads [8, 9]. However, the impact of COVID-19 preventive measures on HAIs is still inadequate [10]. Multiple studies claim that the COVID-19 pandemic influenced the emergence of HAI throughout time [4, 11]. Nevertheless, others indicate that the wide spread of COVID-19 led to a shift in public behavior and a greater understanding of the need for IPC [12, 13]. The use of contact precautions and implementing preventive measures based on the COVID-19 pandemic had a beneficial indirect impact on preventing HAIs [12,13,14].
In Malaysia, HAIs are a major problem in the healthcare system. Pneumonia, urinary tract infections (UTIs), and surgical site infections (SSIs) accounted for the majority of HAIs, with a prevalence rate of 13% [15, 16]. The strain on the healthcare system during COVID may have indirectly contributed to disruption of conventional healthcare services and compromising patient care [17, 18]. Intensive IPC measures have been implemented as a result of COVID-19 pandemic to stop the spread of infections [17,18,19]. However, the impact of COVID preventive measures on the rate of HAIs in Malaysia is still unknown. We hypothesized that the deployment of extensive protective preventing measures during the COVID-19 pandemic affected the prevalence of HAIs. So, the aim of this study is to evaluate the impact of COVID-19 pandemic on the rate and the type of HAIs and investigate patterns of microorganisms involved in HAI pre- and during the pandemic at the Sultan Ahmed Shah Medical Centre (SASMEC) Hospital in Malaysia.
Methodology
Study design
This was a retrospective cohort study conducted in a tertiary care hospital located on the eastern coast of Malaysia. The study involved two periods, including the period pre-COVID-19 (April to October 2019) and the period during COVID-19 (April to October 2020).
Study setting and population
The study was conducted in the medical, surgical, and critical/intensive care unit (CICU) wards in SASMEC. SASMEC is a tertiary hospital located on the Eastern Coast of Malaysian Peninsular. It provides a range of services including medical, surgery, pediatrics, orthopedic, neuralgy, cardiology and urology. Adult Patients hospitalised in the selected wards during both periods were included. Those hospitalized for at least 48 h were included in the study. Patients with incomplete medical records, those who were transferred to another hospital or dead, and COVID-19 patients were excluded.
Data collection
Data was collected through the review of patients’ electronic medical records. The following information was gathered and extracted from patient medical records including: patient demographics (age, gender), clinical data features (gender, age, diagnosis, and comorbidities), information on hospitalization (date of admission, date of discharge), presence of HAI during hospital admission and type of HAI, and microorganisms isolated. In order to ascertain the HAIs, all hospitalised patients were assessed. Data on HAIs was gathered by a specialised infection control team that included a certified nurse and an expert infection control physician. They were responsible for gathering data on HAIs. After a patient was admitted to the hospital, paraclinical testing was performed. The team maintained updated on any changes in the patient's clinical condition continuously. The head nurses provided daily reports, these reports indicate observations of significant signs like fever, changes at the surgical site that signal infection, and adjustments to antibiotic regimens, as well as feedback from the ward physicians regarding their assessment of potential HAIs. Furthermore, the daily culture results from the lab were received to identify any possible infection. Then the standardized data collection form was filled out for each infected patient [20]. This form was approved and submitted to the infection control unit in the hospital. The diagnostic criteria for diagnosing HAIs were developed in accordance with Malaysia's Ministry of Health (MOH) guidelines. These criteria were based on the CDC definition of Nosocomial Infections [21, 22]. All HAI types that occurred throughout the study period were recorded and categorised, including device-associated HAIs, SSIs, UTIs, and hospital- acquired pneumonia (HAP). HAIs are infections that first manifest 48 h or more after being hospitalised or within 30 days of having surgery [1, 20]. The study protocol was approved by the IIUM Research Ethics Committee with a reference number of IREC 2022–078, and the hospital SASMEC approved the study (IIUM/413/013/14/11/1/IISR 22–11-01).
Statistical analysis
The data was analyzed using the IBM Statistical Package for the Social Sciences (SPSS) version 26 0.0. Descriptive statistics were performed and reported using mean and standard deviation for continuous variables and frequency and percentage for categorical variables. Pearson Chi square test was used to determine the difference in the rate and types of HAIs between the two periods. The overall prevalence of HAI was calculated as the percentage of infected patients out of the total number of hospitalised patients in each period. Percentage change (((new value − old value)/old value) ∗ 100) was used to describe changes in the HAI rates during and pre-COVID-19 [23]. Statistical significance was defined as a p value ≤ 0.05. Multivariable logistic regression was performed to evaluate the potential association between the possible risk factor and HAI acquisition. confidence interval (CI) of 95% and significance of P < 0.05 were used.
Results
A total of 578 patients fulfilled the inclusion criteria, including 321 patients in pre-COVID-19 and 257 during COVID-19. The majority of patients were males (59.5%) in the pre COVID-19 and (55.1%) during COVID-19. The mean age of the patients was 59.5 years and 62.0 years pre and during COVID-19 respectively. Hypertension was the most frequent underlying disease in both periods it was (59.5%) in the pre COVID-19 and (62.8%) in the during COVID-19, followed by diabetes, cancer, and coronary heart disease. The proportion of patients having a medical device decreased during the pandemic period, particularly with the use of urinary catheters (4.3%) and mechanical ventilation (3.1%). As well as there was a decline in the number of surgeries during COVID-19 (2.2%) compared to pre-COVID-19 (8.4%) (Table 1).
Overall, 46 HAI episodes were identified in 39 patients in the pre-COVID-19 period, corresponding to a prevalence of 12.1%. The rate of HAIs during the COVID-19 period was 11.3%, with 32 HAIs episodes reported in 29 patients. HAP was the most common infection in the period pre-COVID-19 (8.1%) and during COVID-19 period (7.4%). There was no statistically significant difference (p = 0.75) in the rate of HAP between the two periods. Similarly, there was no significant difference in the rate of UTIs (1.6% versus 1.1%, p = 0.69) or SSIs (1.2% versus 0.8%, p = 0.57) between the two periods. The rate of ventilator associated pneumonia (VAP) was 0.9% in the pre COVID-19 and 1.2% during COVID-19 (p = 0.78). The rate of catheter-associated blood stream infection (CLABSI) was (0.62% versus 0.81%, p = 0.82) in the pre and during COVID 19 respectively (Table 2).
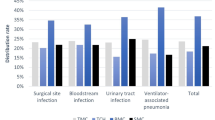
The HAI-related microorganisms did not significantly vary between the two times. A total of 35 microorganisms were isolated from HAIs in the period pre-pandemic and 26 microorganisms were isolated during the pandemic. HAIs were mostly caused by methicillin-resistant Staphylococcus aureus (MRSA) (28.2%) pre COVID-19 and 20.6% during COVID-19 with (p = 0.47). Pseudomonas aeruginosa (27.6%) was the most frequent organism in the during covid while, Enterococcus faecalis (17.9%) and Klebsiella pneumonia (15.3%) in pre COVID-19 (Table 3). By contrast, Stenotrophomonas maltophilia and Enterobacter cloacae complex were identified for HAIs during COVID-19 only with prevalence rate (6.9%). Another organism that detected in both periods was Acinetobacter baumannii complex. MRSA, K. pneumonia and P. aeruginosa were identified among patients with HAP. Whereas, MRSA was around 23.1% pre-COVID and 15.8% during COVID-19. While K. pneumonia was more detected in HAP patients in pre covid with parentage (19.3%). In contrast, P. aeruginosa was the most frequent pathogen causing pneumonia during COVID (26.3%). MRSA was remaining the main pathogen associated with other types of infections including VAP, CLABSI, and SSIs, during and pre COVID-19 (Fig. 1).
In the multivariate logistic regression analysis, both age and gender were found to be non-significant factors associated with HAI acquisition during both the pre-COVID-19 and COVID-19 periods (Table 4). As well as the comorbidities, including hypertension and diabetes mellitus, Conversely, the length of hospital stay emerged as a consistent and statistically significant risk factor associated with HAI acquisition in both timeframes, pre-COVID (OR = 1.27, CI 95%: 1.18–1.37, P < 0.001) and during COVID-19 (OR = 1.57, CI 95%: 1.27–1.94, p < 0.001). Regarding invasive procedures, urinary catheterization demonstrated a significant association with HAI acquisition before the pandemic (OR = 5.024, CI 95%: 1.52–18.01, p < 0.001*). In contrast, during the COVID-19 period, intubation and mechanical ventilation procedures were found to be significantly associated with an increased risk of HAI (OR = 11.10, CI 95%: 1.04–11.69, p < 0.001*) and (OR = 62.66, CI 95%: 2.45–16.00, p = 0.01*), respectively.
Discussion
HAIs have been identified as a leading cause of mortality and impose an enormous financial strain on the healthcare system [2, 24]. Adherence to infection control policies is an essential element in the management of HAIs [5]. Despite the extensive adoption of protocols aimed at mitigating the transmission of COVID-19 during the ongoing global pandemic [8, 17, 25]. This study found no statistically significant difference in the occurrence of HAIs between patients admitted to hospitals pre and during the onset of COVID-19 pandemic. A small reduction was observed in the rates of UTIs, SSIs, and HAP. The rate of UTIs demonstrated a decrease of 31.25%, whereas SSIs exhibited a decline of 33.33%. Furthermore, there was an observed decrease of 8.64% in HAP. These findings align with prior research that suggested that enhanced infection control strategies may not significantly impact HAI rates [26,27,28]. Unfortunately, the challenge of reducing HAIs has not received sufficient attention [24]. The heightened focus on managing COVID-19 pandemic has diverted resources away from traditional IPC measures in hospitals, which may have negatively affected HAI prevention [29, 30]. Additionally, variations in individual compliance with hand hygiene and personal protective equipment (PPE) use, as well as inadequate education, may have played a role [19, 25,26,28, 31]. In contrast, some studies have demonstrated the positive effects of improved IPC methods and strict adherence to established procedures in reducing HAIs during the COVID-19 pandemic [12, 14, 23, 32].
Regarding catheter-associated infections, the current research reveals a 42.10% reduction in the prevalence of CAUTIs, while rates of CLABSIs and VAP increased by 33.0% during the COVID-19 pandemic. These findings are consistent with previous studies that reported higher incidence rates of CLABSIs and VAP, possibly due to systemic stress, resource shortages, and a surge in critically ill patients [6, 33,34,35]. Improper PPE usage and reduced adherence to hand hygiene protocols among healthcare professionals may have contributed to the rise in CLABSIs and VAP [19, 31, 36]. Consequently, it is essential to implement targeted strategies aimed at reducing catheter-associated infections [37]. There is a pressing need to enhance evidence-based intervention approaches while strictly following standard transmission precautions [37, 38].
According to the study results, HAP was mostly caused by Acinetobacter baumannii complex and P. aeruginosa during the COVID-19 period [32, 39]. Notably, infection rates with P. aeruginosa were significantly higher (26.3%) than those caused by other bacteria. These organisms often exhibit antibiotic resistance and are associated with prolonged hospitalizations [4, 40]. In the pre-COVID-19, Enterococcus faecalis was frequently identified in UTIs, CLABSIs, and CAUTIs. However, the implementation of preventive measures during the COVID-19 pandemic may have led to a change in this pattern. E. faecalis was not detected in patients with catheter-related infections, including CAUTIs, CLABSIs, and VAP. The increased emphasis on hand hygiene during the COVID-19 pandemic is the most effective way to prevent the spread of E. faecalis [32, 41]. Therefore, alongside the initiatives implemented during the COVID-19 pandemic, continuous monitoring and prevention efforts are imperative [12, 23, 26].
The study revealed that the length of a patient's hospital stay has consistently been identified as a factor influencing the occurrence of HAIs [26, 42, 43]. Additionally, the use of invasive medical devices is another primary variable significantly contributing to the acquisition of HAIs in the two periods. In the pre-COVID period, urinary catheters were found to be highly relevant. However, during the COVID-19 pandemic, the utilisation of mechanical ventilation and intubation emerged as substantial risk factors for the development of HAIs [4, 30]. These findings underscore previous research findings that emphasise the impact of invasive medical procedures on the prevalence of HAIs [4, 38, 44]. Therefore, it is imperative to conduct a thorough assessment of clinical indications needing for the utilisation of these invasive medical devices [45]. This necessitates a heightened focus on both the initial insertion and ongoing maintenance of these invasive devices [37, 38]. This directive underscores the need for the implementation of a comprehensive and adaptable strategy aimed at effectively mitigating the risk of HAIs associated with invasive medical devices in healthcare settings [4, 32, 37].
The findings provide an overview and baseline awareness of HAIs rate in the hospital, which is essential for tracking future changes and assessing the effectiveness of infection control activities. However, there were no major differences between the two periods. These results may help to increase the effectiveness of the current infection control methods. Assist the hospital in improving its preparedness for any upcoming pandemic incidents.
As far as we are aware, this is the first study that discusses COVID's effect on the HAI rate in Malaysia. However, this study has several limitations. The major limitation of the study is the small sample size and the use of retrospective data analysis, which may limit the deep analysis to the risk factors and predictors of acquisition. Additionally, the generalizability of the study's findings to other healthcare facilities is limited as it was only carried out at one facility. Moreover, we didn’t evaluate compliance with infection control measures such as hand hygiene, using PPE. Further studies are needed to better understand the mechanisms underlying the insignificant decrease in incidence rates.
Conclusion
While the COVID-19 pandemic did not yield a significant impact on decreasing the rate and types of HAIs between the two time periods studied, It is crucial to identify additional beneficial strategies in conjunction with highlighting the continuous necessity of maintaining strict compliance with IPC protocols.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request due to privacy reasons.
Abbreviations
- HAI:
-
Hospital acquired infection
- IPC:
-
Infection prevention and control
- VAP:
-
Ventilator-associated pneumonia
- CLABSIs:
-
Central line-associated blood stream infections
- CAUTIs:
-
Catheter associated urinary tract infections
- UTI:
-
Urinary tract Infection
- COVID-19:
-
Coronavirus disease 2019
- CVC:
-
Central venous catheter
- ICU:
-
Intensive care unit
- SSI:
-
Surgical site infection
References
Haque M, Sartelli M, McKimm J, Abu BM. Health-care associated infections—An overview. Infect Drug Resist. 2018;15:2321–33. https://doi.org/10.2147/IDR.S177247.
Liu X, Cui D, Li H, Wang Q, Mao Z, Fang L, et al. Direct medical burden of antimicrobial-resistant healthcare-associated infections: empirical evidence from China. J Hosp Infect. 2020;105(2):295–305. https://doi.org/10.1016/j.jhin.2020.01.003. PMID31931043.
Guidelines on core components of infection prevention and control programs at the national and acute health care facility level. Geneva: World Health Organization; 2016. 6. The burden of healthcare-associated infection Available from: https://www.ncbi.nlm.nih.gov/books/NBK401766/. Accessed 10 Feb 2019.
Despotovic A, Milosevic B, Cirkovic A, Vujovic A, Cucanic K, et al. The impact of covid-19 on the profile of hospital-acquired infections in adult intensive care units. Antibiotics. 2021;10:1146. https://doi.org/10.3390/antibiotics10101146.
Ershova K, Savin I, Kurdyumova N, Wong D, Danilov G, Shifrin M, et al. Implementing an infection control and prevention program decreases the incidence of healthcare-associated infections and antibiotic resistance in a Russian neuro-ICU. Antimicrob Resist Infect Control. 2018;7:94. https://doi.org/10.1186/s13756-018-0383-4. PMID30083313.
Alsuhaibani M, Kobayashi T, McPherson C, Holley S, Marra AR, et al. Impact of COVID-19 on an infection prevention and control program, Iowa 2020–2021. Am J Infect Control. 2022;50(3):277–82. https://doi.org/10.1016/j.ajic.2021.11.015.
McCabe R, Schmit N, Christen P, D’Aeth JC, Løchen A, et al. Adapting hospital capacity to meet changing demands during the COVID-19 pandemic. BMC Med. 2020;18:329. https://doi.org/10.1186/s12916-020-01781-w.
World Health Organization (WHO). Strenghtening the Health System Response to COVID-19. Maintaining the Delivery of Essential Health Care Services While Mobilizing the Health Workforce for the COVID-19 Response. Copenhagen, Denmark: World Health Organization, Regional Office for Europe; 2020.
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62. https://doi.org/10.1016/S0140-6736(20)30566-3.
Stevens MP, Doll M, Pryor R, Godbout E, Cooper K, Bearman G. Impact of COVID-19 on Traditional Healthcare Associated Infection Prevention Efforts. Infect Control Hosp Epidemiol. 2020;41:946–7. https://doi.org/10.1017/ice.2020.141.
Bardi T, Pintado V, Gomez-rojo M, Escudero-sanchez R, Lopez AA. Nosocomial infections associated to COVID-19 in the intensive care unit: Clinical characteristics and outcome. Eur J Clin Microbiol Infect Dis. 2021;40:495–502. https://doi.org/10.1007/s10096-020-04142-w.
CerulliIrelli E, Orlando B, Cocchi E, Morano A, Fattapposta F, et al. The potential impact of enhanced hygienic measures during the COVID-19 outbreak on hospital-acquired infections: a pragmatic study in neurological units. J Neurol Sci. 2020;418: 117111. https://doi.org/10.1016/j.jns.2020.117111.
Lo SH, Lin CY, Hung CT, He JJ, Lu PL. The impact of universal face masking and enhanced hand hygiene for COVID-19 disease prevention on the incidence of hospital acquired infections in a Taiwanese hospital. Int J Infect Dis. 2021;104:15–8.
Chacón-Quesada T, Rohde V, von der Brelie C. Less surgical site infections in neurosurgery during COVID-19 times-one potential benefit of the pandemic? Neurosurg Rev. 2021;44(6):3421–5. https://doi.org/10.1007/s10143-021-01513-5.
Hughes AJ, Ariffin N, Huat TL, Abdul Molok H, Hashim S, et al. Prevalence of nosocomial infection and antibiotic use at a university medical center in Malaysia. Infect Control Hosp Epidemiol. 2005;26(1):100–4. https://doi.org/10.1086/502494.
Khan OH, Zakaria AD, Hashim MN, Khan AH, AlQarni A, et al. The burden of surgical site infection at Hospital Universiti Sains Malaysia and related postoperative outcomes: a prospective surveillance study. Antibiotics (Basel, Switzerland). 2023;12(2):208. https://doi.org/10.3390/antibiotics12020208.
Ministry of Health Malaysia. COVID-19 Malaysia Updates; Lebih 4,000 Petugasbarisanhadapan KKM Dijangkiti COVID-19 - KP Kesihatan. COVID-19 Malaysia. (2021). Available online at http://covid-19.moh.gov.my. Accessed 9 July 2021.
Tan CS, Lokman S, Rao Y, Kok SH, Ming LC. Public and private sectors collective response to combat COVID-19 in Malaysia. J Pharm Policy Prac. 2021;14:40. https://doi.org/10.1186/s40545-021-00322-x.
Mohamad N, Pahrol MA, Shaharudin R, MdYazin NKR, Osman Y, et al. Compliance to infection prevention and control practices among healthcare workers during COVID-19 pandemic in Malaysia. Front Public Health. 2022;10:878396. https://doi.org/10.3389/fpubh.2022.878396.
Office of the Malaysia One Health Antimicrobial Resistance Portal (MyOHAR). Point Prevalence Survey (PPS) on Healthcare Associated Infections & Antibiotics. Ministry of Health Malaysia. https://myohar.moh.gov.my/point-prevalence-survey-pps-on-healthcare-associated-infection-antibiotics/. Accessed 11 Aug 2023.
Ministry of Health Malaysia. Policies and Procedures on Infection Control. 2nd Ed. https://www.moh.gov.my/moh/images/gallery/Polisi/infection_control.pdf. Accessed 11 Aug 2023.
CDC. National Healthcare Safety Network (NHSN) Patient Safety Component Manual. Available at: https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf. Published January 2017. Accessed 1 Jan 2017.
Jabarpour M, Dehghan M, Afsharipour G, Hajipour Abaee E, Mangolian, et al. The impact of COVID-19 outbreak on nosocomial infection rate: a case of Iran. Can J Infect Dis Med Microbiol. 2021;6650920. https://doi.org/10.1155/2021/6650920.
Suetens C, Latour K, Kärki T, Ricchizzi E, Kinross P, et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Eurosurveillance. 2018;23:1–17. https://doi.org/10.2807/1560-7917.ES.2018.23.46.1800516.
Ministry of Health Malaysia. Annex 21: Management of Healthcare Workers (HCW) During the COVID-19 Pandemic. 2022. Available online at https://covid-19.moh.gov.my/garis-panduan/garis-panduan-kkm/ANNEX-21-MANAGEMENT-OF-HEALTHCARE-WORKERS-HCW-DURING-THE-COVID-19-PANDEMIC-20022022.pdf. Accessed 6 June 2022.
Tham N, Fazio T, Johnson D, Skandarajah A, Hayes IP. Hospital Acquired infections in surgical patients: impact of COVID-19-related infection prevention measures. World J Surg. 2022;46(6):1249–58. https://doi.org/10.1007/s00268-022-06539-4.
Mohammadi A, Khatami F, Azimbeik Z, Khajavi A, Aloosh M, Aghamir SMK. Hospital-acquired infections in a tertiary hospital in Iran before and during the COVID-19 pandemic. Wien Med Wochenschr (1946). 2022;172(9–10):220–6. https://doi.org/10.1007/s10354-022-00918-1.
Losurdo P, Paiano L, Samardzic N, Germani P, Bernardi L, Borelli M, et al. Impact of lockdown for SARS-CoV-2 (COVID-19) on surgical site infection rates: a monocentric observational cohort study. Updates Surg. 2020;72(4):1263–71.
Abbas M, RobaloNunes T, Martischang R, Zingg W, Iten A, Pittet D, et al. Nosocomial transmission and outbreaks of coronavirus disease 2019: the need to protect both patients and healthcare workers. Antimicrob Resist Infect Control. 2021;10(1):7. https://doi.org/10.1186/s13756-020-00875-7. PMID33407833.
Baccolini V, Migliara G, Isonne C, Dorelli B, Barone LC, et al. The impact of the COVID-19 pandemic on healthcare-associated infections in intensive care unit patients: a retrospective cohort study. Antimicrob Resist Infect Control. 2021;10:87. https://doi.org/10.1186/s13756-021-00959-y.
Stangerup M, Hansen MB, Hansen R, et al. Hand hygiene compliance of healthcare workers before and during the COVID-19 pandemic: a long-term follow-up study. Am J Infect Control. 2021;49:1118–22.
Su C, Zhang Z, Zhao X, Peng H, Hong Y, Huang L, et al. Changes in prevalence of nosocomial infection pre-and post- Covid-19 pandemic from a Tertiary Hospital in China. BMC Infect Dis. 2021. https://doi.org/10.1186/s12879-021-06396-x.
Fakih MG, Bufalino A, Sturm L, et al. Coronavirus disease 2019 (COVID-19) pandemic, central-line−associated bloodstream infection (CLABSI), and catheter-associated urinary tract infection (CAUTI): the urgent need to refocus on hardwiring prevention efforts. Infect Control Hosp Epidemiol. 2021;2021:1–6.
LeRose J, Sandhu A, Polistico J, Ellsworth J, Cranis M, Jabbo L, et al. The impact of coronavirus disease 2019, (Covid-19) response on central-line– associated bloodstream infections and blood culture contamination rates at a tertiary-care center in the Greater Detroit area. Infect Control Hosp Epidemiol. 2020. https://doi.org/10.1017/ice.2020.1335.
Verberk JDM, van der Kooi TII, Kampstra NA, Reimes N, van Rooden SM, et al. Healthcare-associated infections in Dutch hospitals during the COVID-19 pandemic. Antimicrob Resist Infect Control. 2023;12(1):2. https://doi.org/10.1186/s13756-022-01201-z.
Kampf G, Bruggemann Y, Kaba HEJ, et al. Potential sources, modes of transmission and effectiveness of prevention measures against SARS-CoV-2. J Hosp Infect. 2020;106:678–97.
Kuy S, Gupta R, Roy C, Awad S. Incidence of catheter-associated urinary tract infections with compliance with preventive guidelines. JAMA Surg. 2020;155(7):661–2. https://doi.org/10.1001/jamasurg.2020.0428. PMID:32320018;PMCID:PMC7177634.
Fortaleza CMCB, Filho SPF, Silva MO, Queiroz SM, Cavalcante RS. Sustained reduction of healthcare-associated infections after the introduction of a bundle for prevention of ventilator-associated pneumonia in medical-surgical intensive care units. Braz J Infect Dis. 2020;24:373–9. https://doi.org/10.1016/j.bjid.2020.08.004.
Isonne C, Baccolini V, Migliara G, Ceparano M, Alessandri F, et al. Comparing the occurrence of healthcare-associated infections in patients with and without COVID-19 hospitalized during the pandemic: a 16-month retrospective cohort study in a hospital intensive care unit. J Clin Med. 2022;11(5):1446. https://doi.org/10.3390/jcm11051446.
Saini V, Jain C, Singh NP, Alsulimani A, Gupta C, et al. Paradigm shift in antimicrobial resistance pattern of bacterial isolates during the covid-19 pandemic. Antibiotics. 2021;10:954. https://doi.org/10.3390/antibiotics10080954.
Zhang Y, Du M, Chang Y, Chen LA, Zhang Q. Incidence, clinical characteristics, and outcomes of nosocomial Enterococcus spp. bloodstream infections in a tertiary-care hospital in Beijing, China: a four-year retrospective study. Antimicrob Resist Infect Control. 2017;6:73. https://doi.org/10.1186/s13756-017-0231-y.
Zhou Q, Fan L, Lai X, et al. Estimating extra length of stay and risk factors of mortality attributable to healthcare-associated infection at a Chinese university hospital: a multi-state model. BMC Infect Dis. 2019;19:975. https://doi.org/10.1186/s12879-019-4474-5.
Jia H, Li L, Li W, Hou T, Ma H, Yang Y, Wu A, Liu Y, Wen J, Yang H, Luo X, Xing Y, Zhang W, Wu Y, Ding L, Liu W, Lin L, Li Y, Chen M. Impact of healthcare-associated infections on length of stay: a study in 68 hospitals in China. Biomed Res Int. 2019;18(2019):2590563. https://doi.org/10.1155/2019/2590563. PMID:31119159;PMCID:PMC6500696.
Pezhman B, Fatemeh R, Amir R, Mahboobeh R, Mohammad F. Nosocomial infections in an Iranian educational hospital: an evaluation study of the Iranian nosocomial infection surveillance system. BMC Infect Dis. 2021;21(1):1256. https://doi.org/10.1186/s12879-021-06948-1. PMID:34911472;PMCID:PMC8672650.
Parker V, Giles M, Graham L, Suthers B, Watts W, O’Brien T, Searles A. Avoiding inappropriate urinary catheter use and catheter-associated urinary tract infection (CAUTI): a pre-post control intervention study. BMC Health Serv Res. 2017;17:314. https://doi.org/10.1186/s12913-017-2268-2.
Acknowledgements
The authors wish to thank all staff of the infection control unit, intensive care unit, surgical unit and medical unit of the Sultan Ahmed Shah medical Centre (SASMEC).
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee of the Sultan Ahmed Shah medical Centre (SASMEC) reference number (IIUM/413/013/14/11/1/IISR 22–11-01) and IIUM Research Ethics Committee (IREC) reference number (IREC 2022–078). All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ismaeil, R., Nahas, A.R.F., Kamarudin, N.B. et al. Evaluation of the impact of COVID-19 pandemic on hospital-acquired infections in a tertiary hospital in Malaysia. BMC Infect Dis 23, 779 (2023). https://doi.org/10.1186/s12879-023-08770-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08770-3