Abstract
Opioids are effective analgesics but can cause harm. Opioid stewardship is key to ensuring that opioids are used effectively and safely. There is no agreed set of quality indicators relating to the use of opioids perioperatively. This work is part of the Yorkshire Cancer Research Bowel Cancer Quality Improvement programme and aims to develop useful quality indicators for the improvement of care and patient outcomes at all stages of the perioperative journey.
A rapid review was performed to identify original research and reviews in which quality indicators for perioperative opioid use are described. A data tool was developed to enable reliable and reproducible extraction of opioid quality indicators.
A review of 628 abstracts and 118 full-text publications was undertaken. Opioid quality indicators were identified from 47 full-text publications. In total, 128 structure, process and outcome quality indicators were extracted. Duplicates were merged, with the final extraction of 24 discrete indicators. These indicators are based on five topics: patient education, clinician education, pre-operative optimization, procedure, and patient-specific prescribing and de-prescribing and opioid-related adverse drug events.
The quality indicators are presented as a toolkit to contribute to practical opioid stewardship. Process indicators were most commonly identified and contribute most to quality improvement. Fewer quality indicators relating to intraoperative and immediate recovery stages of the patient journey were identified. An expert clinician panel will be convened to agree which of the quality indicators identified will be most valuable in our region for the management of patients undergoing surgery for bowel cancer.
Similar content being viewed by others
Background
Inappropriate opioid prescribing is an internationally recognized threat to population health and a pressing challenge for healthcare services (Kiang et al. 2020; Curtis et al. 2019; Degenhardt et al. 2019). The North American ‘opioid crisis’ continues, with an ongoing rise in opioid-related mortality, initially due to prescription opioids and more recently illicit heroin and fentanyl use (Berterame et al. 2016). Despite increased awareness of risks and opioid abuse, prescription opioid use remains historically high in both North America and Europe (Jani et al. 2020; Schieber et al. 2019; Verhamme and Bohnen 2019; Lancet 2022). Inappropriate prescribing following surgery is increasingly recognized as a contributor to the problem. Opioids are effective analgesics for managing acute pain following surgical trauma (Small and Laycock 2020) and were increasingly used in longer and higher doses following the publication of guidelines on post-operative pain management (Ballantyne et al. 2016). However, opioids also have significant adverse effects, including sedation, constipation, nausea, and confusion. Long-term use can lead to tolerance, dependence, hyperalgesia, addiction and increased mortality (Colvin et al. 2019). There is increasing attention being paid to the role of postoperative opioids in slowing recovery from surgery and contributing to long-term opioid use (Glare et al. 2019; Levy et al. 2021; Daliya et al. 2021). Enhanced recovery after surgery (ERAS) programmes often include the provision of multi-modal analgesia to promote faster recovery with fewer complications. Whilst short-term opioid use provides effective relief from acute pain following surgery, it is increasingly recognized that the perioperative period is a time when longer-term opioid usage may begin. Effective opioid stewardship in the perioperative period is therefore of critical importance.
Improving opioid stewardship in the peri- and post-operative management of patients with bowel cancer has the potential to improve recovery, lead to faster discharge, improve outcomes and most importantly, prevent patient harm. A requirement for an effective opioid stewardship program is the ability to measure the appropriateness of opioid use.
Health care quality indicators are a type of performance measure (Stelfox and Straus 2013) that evaluate aspects of quality of care, without which the monitoring of healthcare quality is impossible (Mainz 2003; Arah et al. 2006). Quality indicators are used to measure the variability in the quality of care, identify potential areas for improvement and can be used to feedback on performance to healthcare teams to change clinical practice. They should be relevant, actionable, reliable, show room for improvement and data collection should be feasible (Ivers et al. 2012; Kelley and Hurst 2006; Fabian and Geppert 2011). Donabedian’s framework (Donabedian 1988) describes quality as a function of three domains: structure, process and outcome. The structure is defined by the attributes of the setting in which care is provided, process by the input of the practitioners working in that system and outcome by the change in health status of the patient.
No quality indicators for perioperative opioid use are currently described in the National Institute for Health and Care Excellence Standards and Indicators library (Standards and Indicators | NICE (accessed 22nd March 2022). A rapid review was performed to identify quality indicators for perioperative opioid stewardship for patients undergoing abdominal surgery for bowel cancer. This is a form of knowledge synthesis that streamlines the process of conducting a traditional systematic review to produce evidence in a rapid resource-efficient manner (Hamel et al. 2021) and has been chosen to allow timely evidence synthesis to inform decision-making (Haby et al. 2016).
The objective of this rapid review was to identify and extract potential quality indicators from the best available evidence on perioperative opioid use in patients undergoing major abdominal surgery for bowel cancer. This approach to the development of actionable quality indicators has been described and applied effectively in other clinical settings (Kallen et al. 2018).
Methods
Cochrane rapid review methods were followed (Garrity et al. 2021). A systematic literature search of Medline was performed and included all articles available to April 2021. Systematic reviews and primary studies were sought. The types of participants were not restricted and could be individuals, organizations or systems. Search terms are shown in Table 1 and include terms and truncations for quality indicators, opioids, surgery (with potential limitation to colorectal cancer surgery) and development. The search was limited to studies of adult subjects and studies published in English. A manual search was conducted of the reference lists of the selected papers. Searches were conducted between the 1st and the 25th August 2021 and supplementary searches of reference lists were conducted in December 2021. The National Quality Measures Clearinghouse project (2022) was also reviewed for relevant content.
The initial search identified 588 abstracts. These results were imported into Rayyan (http://rayyan.qcri.org/) (Ouzzani et al. 2016) a free web tool used to facilitate the screening and selection of studies for systematic and scoping reviews.
Three members of the project team (MA, KP, DY) screened all titles and abstracts for inclusion. Duplicate studies, case reports, editorials, non-English language studies, quality improvement not concerning opioid use, abdominal or colorectal surgery, or performance measures and quality improvement in specific subgroups of patients were excluded. Where a decision on inclusion could not be reached, two further team members (CT, SH) reviewed the titles and abstracts. All studies included at this stage underwent full-text review, undertaken by two members of the project team (CT, SH). MA, KP, and DY accessed the full-text articles of all included papers, which were uploaded and accessed using Rayyan. The extraction of quality indicators from the full texts was undertaken by CT and SH. All those included were papers from which quality indicators could be extracted. A quality indicator extraction tool was developed in advance of data extraction, with potential indicators categorized to the stage of perioperative care they relate to (Supplementary materials 1) to enable reproducible results. Finally, a full list of potential indicators was composed, in which indicators were rephrased where needed and duplicate indicators removed. Reporting has been guided by the PRISMA extension for scoping reviews (PRISMA-ScR) (Extension and for Scoping Reviews (PRISMA-ScR): Checklist and Explanation | The EQUATOR Network (equator-network.org) (accessed 22nd March 2022).
Results
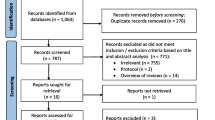
Five hundred eighty-eight publications were identified by the literature search. Three duplicates and a further 425 abstracts were removed as they did not meet inclusion criteria. Eighty-three of these papers were included for full-text review, of which 53 were excluded because they reported on another outcome or population, or because the paper did not include quality indicators. Thirty papers were included, the references of which were reviewed. A further 35 full-text papers were reviewed, of which 17 were included. The study selection flowchart (Fig. 1) details this process. In total, 47 papers were identified from which quality indicators were extracted. Review of the quality indicators clearinghouse did not yield results.
The characteristics (study design and numbers of participants) of the included papers are shown in Supplementary Materials 2.
One hundred twenty-eight quality indicators from 47 papers were extracted, with some papers describing several indicators. See Supplementary materials 1 for full details of all raw extracted quality indicators. Duplicates were removed, leading to the identification of 24 discrete indicators. Table 2 shows the numbers of discrete quality indicators identified at each stage of the patient journey.
Instruments for collecting data on quality indicators, and structural, process, and outcome indicators were collated. These are grouped according to stage in the perioperative journey and are shown in Table 3.
The quality indicators identified which could be grouped into five topics: patient education, staff education, preoperative patient optimization, patient and procedure-specific prescribing and deprescribing and opioid-related adverse drug events (ORADEs) and are shown in Table 4. Full details of the quality indicator topics are shown in Supplementary materials 3.
Discussion
Opioids are highly effective analgesics but can cause harm and there is now increasing concern about their perioperative use. A number of contributing problems have been identified. Opioid tolerance preoperatively is a risk factor for poorer outcome (Cron et al. 2017; Gan et al. 2020; Gan et al. 2015; Kessler et al. 2013). When opioids are used by either opioid-naïve or opioid tolerant patients, they are put at risk of opioid-related adverse drug events (ORADEs) (Macintyre et al. 2014; Minkowitz et al. 2014; Keller et al. 2019; Kessler et al. 2013; Oderda et al. 2013), and opioid use is associated with postoperative complications and increased length of stay (Cron et al. 2017; Gan et al. 2020; Gan et al. 2015). Additionally, the perioperative period has been identified as a period of risk for the development of chronic opioid use (Lee et al. 2017; Brummett et al. 2017; Clarke et al. 2014; Macintyre et al. 2014; Roughead et al. 2019; Srivastava et al. 2021). At discharge, opioid prescriptions in excess of requirements are widely reported (Neuman et al. 2019; Bromberg et al. 2021; Hill et al. 2017; Hill et al. 2018; Pruitt et al. 2020; Bartels et al. 2016; Agarwal et al. 2021; Howard et al. 2019; Meyer et al. 2021) and opioids initially used for short-term pain relief can become part of repeat prescriptions following hospital discharge. Poor practice around safe storage and disposal of opioids following discharge contributes to increased opioid in the community with the potential for opioid diversion (Fujii et al. 2018; Hill et al. 2017; Bartels et al. 2016). These factors contribute to the development of persistent postoperative opioid use (PPOU) with the increased potential for ORADEs in the community following discharge.
Effective opioid stewardship is therefore an important part of the provision of opioids in the perioperative period, and a need to improve has been identified (Srivastava et al. 2021). Quality indicators are used to monitor and improve quality in healthcare (Stelfox and Straus 2013; Mainz 2003; Fabian and Geppert 2011; Donabedian 1988; Rademakers et al. 2011). Good quality indicators are based on the best available evidence, should be highly specific and sensitive, with the integration of best clinical evidence, clinical expertise, and patient values. No quality indicators for perioperative opioid stewardship currently exist. The review of the supporting evidence base is required to enable the development of a practical set of reliable quality indicators (Stelfox and Straus 2013).
Extracted quality indicators
Our review identified indicators relating to five key topics during the perioperative patient journey. These five topics are patient education, staff education, preoperative patient optimization, patient and procedure-specific prescribing and deprescribing and opioid-related adverse drug events. All five topics include structure, process, and outcome quality indicators (Table 4).
Definitions and comparisons
Varying definitions used in the literature have emerged from this review and consideration of these when discussing quality indicators is useful. Persistent perioperative opioid use is frequently described as the ongoing use of opioids at 90–180 days postoperatively (Fields et al. 2019; Lee et al. 2017; Clarke et al. 2014; Roughead et al. 2019; Pullman et al. 2021). Opioid tolerance is variably described as being present if a patient has used opioids for more than 7 days in the 60 days prior to surgery, any opioid use in 12 months prior to surgery or any opioid on the admission medication list (Fields et al. 2019; Brat et al. 2018; Cron et al. 2017; Gan et al. 2020; Hilliard et al. 2018; Truong et al. 2019). Milligrams of morphine equivalents (MME) or oral morphine equivalents (OME) are the most widely used methods to describe and compare opioid use. When reviewing postoperative patients in the community, the postoperative prescription can be considered to have been used if the prescribed opioids are dispensed between 2 and 7 days following discharge (Roughead et al. 2019). The detection of opioid misuse or PPOU after discharge is defined as at least one of the ICD-9 diagnosis code of opioid dependence, abuse or overdose (Brat et al. 2018). When reviewing the time to opioid cessation, a suggested definition is a period without an opioid prescription equivalent to three times the estimated supply duration in preoperatively opioid naïve patients (Roughead et al. 2019).
Data collection tools
Instruments to collect data for quality indicators are also reported although none have been specifically developed for postoperative opioid use. The Opioid Risk Tool (ORT), Screener for Opioid Assessment and Patients with Pain (SOAPP), and Brief Risk Interview (BRI) have been proposed for use in perioperative practice when screening patients preoperatively for risk of PPOU (Macintyre et al. 2014). The frequency, severity, and distress caused by opioid-related side effects can be scored as 0 to 60 on the Perioperative Opioid-related Symptom Distress scale and has been reported as a tool to assess ORADEs (Lee et al. 2010).
Addressing the gaps
More process quality indicators than structure or outcome quality indicators are described in the literature. However, the factors which are reported to make the greatest difference to a patient’s assessment of healthcare quality are process-related and process quality indicators are especially useful to consider when quality improvement is desired (Rademakers et al. 2011). Fewer quality indicators concern the intraoperative and immediate recovery period. The impact of specific changes in practice on long-term outcomes remains unclear, and our rapid review of quality indicators will enable rigorous studies of the implementation and impact of interventions to improve opiate stewardship in the perioperative period.
Algorithms and electronic systems
The screening of patients for potential opioid tolerance, future likelihood of PPOU, and patient-group-specific prescribing with limits on the type, dose, and duration of opioid prescription may be best undertaken with the use of algorithms and the development in machine learning (Ellis et al. 2019). Electronic records and prescribing (which are already well-embedded in primary care) are now used increasingly in hospital clinical practice and this may present a good opportunity to develop patient-or patient-group-specific guidelines for opioid prescribing with limits and alerts if there is deviation from agreed protocols.
Limitations
Limitations of this work include those relating to rapid review methodology. This is a relatively recently developed form of knowledge synthesis, and while valid (Garrity et al. 2021), is less comprehensive than a systematic review. Most of the studies included are retrospective cohort studies, and most originate using data from patients in a different healthcare systems (often from the USA). The characteristics of papers are reported (Supplementary Materials 2) but an assessment of risk of bias was not undertaken. This work has been done to drive improvement in outcomes for patients undergoing bowel cancer and this may limit its applicability to a wider perioperative population.
Conclusion and future work
The concept of ‘universal precautions’ have been suggested as being applicable to the prescribing and administration of opioids in the perioperative period (Lee et al. 2017; Macintyre et al. 2014) and encompass strategies at each stage of a patient’s perioperative journey to ensure that the lowest dosage, shortest acting opioids are used for the shortest possible time, while ensuring good analgesia and patient satisfaction. This will be used as an underpinning principle for our ongoing work.
This project forms part of the wider YCRBCIP program for use in the improvement of outcomes for patients with bowel cancer undergoing surgery. We have identified a set of quality indicators which may help to improve quality of care for patients undergoing major abdominal surgery for bowel cancer who receive perioperative opioids. We will now integrate the extracted quality indicators with clinician expertise and patient values to develop a more concise toolkit which providers in our region can use to benchmark and improve quality in the use of perioperative opioids for patients with bowel cancer.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
Agarwal A, Lee D, Ali Z, et al. Patient-reported opioid consumption and pain intensity after common orthopedic and urologic surgical procedures with use of an automated text messaging system. JAMA. 2021;4:e213243.
Arah OA, Westert GP, Hurst J, Klazinga NS. A conceptual framework for the OECD Health Care Quality Indicators Project. Int J Qual Health Care. 2006;18:5–13.
Ballantyne JC, Kalso E, Stannard C. WHO analgesic ladder: a good concept gone astray. Br Med J. 2016;352:i20.
Bardiau F, Braeckman M, Seidel L, Albert A, Boogaerts J. Effectiveness of an acute pain service inception in a general hospital. J Clin Anesth. 1999;11:583–9.
Bartels K, Mayes L, Dingmann C, Bullard K, Hopfer C, Binswanger I. Opioid use and storage patterns by patients after hospital discharge following surgery. PLOS ONE. 2016;11: e0147972.
Berterame S, Erthal J, Thomas J, Fellner S, Vosse B, Clare P, et al. Use of and barriers to access to opioid analgesics: a worldwide, regional, and national study. The Lancet. 2016;387:1644–56.
Bongiovanni T, Hansen K, Lancaster E, O’Sullivan P, Hirose K, Wick E. Adopting best practices in post-operative analgesia prescribing in a safety-net hospital: Residents as a conduit to change. Am J Surg. 2020;219:299–303.
Brandal D, Keller MS, Lee C, et al. Impact of enhanced recovery after surgery and opioid-free anesthesia on opioid prescriptions at discharge from the hospital: a historical-prospective study. Anesth Analg. 2017;125:1784–92.
Brat G, Agniel D, Beam A, et al. Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: a retrospective cohort study. Br Med J. 2018;360:j5790.
Bromberg W, Emanuel T, Zeller V, et al. Assessment of post-operative opioid prescribing practices in a community hospital ambulatory surgical center. J Opioid Manag. 2021;17:241–9.
Brummett C, Waljee J, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. J Am Med Assoc Surg. 2017;152:e170504.
Chen E, Marcantonio A, Tornetta P. Correlation between 24-hour predischarge opioid use and amount of opioids prescribed at hospital discharge. J Am Med Assoc Surg. 2018;153:e174859.
Cheung C, Ying C, Lee L, Tsang S, Tsui S, Irwin M. An audit of postoperative intravenous patient-controlled analgesia with morphine: evolution over the last decade. Eur J Pain. 2009;13:464–71.
Clarke H, Soneji N, Ko D, Yun L, Wijeysundera D. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. Br Med J. 2014;348:g1251.
Colvin LA, Bull F, Hales TG. Perioperative opioid analgesia—when is enough too much? A review of opioid-induced tolerance and hyperalgesia. The Lancet. 2019;393:1558–68.
Cron D, Engelsbe M, Bolton C, et al. Preoperative opioid use is independently associated with increased costs and worse outcomes after major abdominal surgery. Ann Surg. 2017;265:695–701.
Curtis HJ, Croker R, Walker AJ, Richards GC, Quinlan J, Goldacre B. Opioid prescribing trends and geographical variation in England, 1998–2018: a retrospective database study. The Lancet Psychiatry. 2019;6:140–50.
Daliya P, Adiamah A, Roslan F, et al. Opioid prescription at postoperative discharge: a retrospective observational cohort study. Anaesthesia. 2021;76:1367–76.
Degenhardt L, Grebely J, Stone J, Hickman M, Vickerman P, Marshall BDL, et al. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. The Lancet. 2019;394:1560–79.
Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260:1743–8.
Ellis R, Wang Z, Genes N, Ma’ Ayan A. Predicting opioid dependence from electronic health records with machine learning. BioData Mining. 2019;12:3.
Fabian L, Geppert J. Quality indicator measure development, implementation, maintenance, and retirement summary. Rockville, MD. Agency for Healthcare Research and Quality, 2011.
Felling D, Jackson M, Ferraro J, et al. Liposomal bupivacaine transversus abdominis plane block versus epidural analgesia in a colon and rectal surgery enhanced recovery pathway: a randomized clinical trial. Dis Colon Rectum. 2018;61:1196–204.
Fields A, Cavallaro P, Correll D, et al. Predictors of prolonged opioid use following colectomy. Dis Colon Rectum. 2019;62:1117–23.
Fujii M, Hodges A, Russell R, et al. Post-discharge opioid prescribing and use after common surgical procedures. J Am Coll Surg. 2018;226:1004–12.
Gan T, Robinson S, Oderda G, Scranton R, Pepin J, Ramamoorthy S. Impact of postsurgical opioid use and ileus on economic outcomes in gastrointestinal surgeries. Curr Med Res Opin. 2015;31:677–86.
Gan T, Jackson N, Castle J. A retrospective review: patient-reported preoperative prescription opioid, sedative, or antidepressant use is associated with worse outcomes in colorectal surgery. Dis Colon Rectum. 2020;63:965–73.
Garrity C, Gartlehner G, Nussbaumer-Streit B, et al. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol. 2021;130:13–22.
Glare P, Aubrey KR, Myles PS. Transition from acute to chronic pain after surgery. The Lancet. 2019;393:1537–46.
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg. 2014;38:1531–41.
Haby M, Chapman E, Clark R, Barreto J, Reveiz L, Lavis J. What are the best methodologies for rapid reviews of the research evidence for evidence-informed decision making in health policy and practice: a rapid review. Health Res Policy Syst. 2016;14:83.
Hamel C, Michaud A, Thuku M, et al. Defining rapid reviews: a systematic scoping review and thematic analysis of definitions and defining characteristics of rapid reviews. J Clin Epidemiol. 2021;129:74–85.
Hill MV, McMahon ML, Stucke RS, Barth RJ Jr. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017;265:709–14.
Hill MV, Stucke RS, McMahon ML, Beeman JL, Barth RJ Jr. An educational intervention decreases opioid prescribing after general surgical operations. Ann Surg. 2018;267:468–72.
Hilliard P, Waljee J, Moser S, et al. Prevalence of preoperative opioid use and characteristics associated with opioid use among patients presenting for surgery. J Am Med Assoc Surg. 2018;153:929–37.
Hoang S, Vemuru S, Hassinger T, Friel C, Hedrick T. An unintended consequence of a new opioid legislation. Dis Colon Rectum. 2020;63:389–96.
Hopkins R, Bui T, Konstantatos A, et al. Educating junior doctors and pharmacists to reduce discharge prescribing of opioids for surgical patients: a cluster randomised controlled trial. Med J Aust. 2020;213:417–23.
Howard R, Fry B, Gunaseelan V, et al. Association of opioid prescribing with opioid consumption after surgery in Michigan. J Am Med Assoc Surg. 2019;154:e184234.
Ivers N, Jamtvedt G, Flottorp S et al. Audit and feedback: effects on professional practice and healthcare outcomes. The Cochrane Library 2012; 6: CD000259–CD000259
Jani M, Birlie Yimer B, Sheppard T, Lunt M, Dixon WG. Time trends and prescribing patterns of opioid drugs in UK primary care patients with non-cancer pain: a retrospective cohort study. PLOS Med. 2020;17:e1003270.
Jiang X, Orton M, Feng R. Chronic opioid usage in surgical patients in a large academic center. Ann Surg. 2017;265:722–7.
Kallen M, Roos-Blom M, Dongelmans D, et al. Development of actionable quality indicators and an action implementation toolbox for appropriate antibiotic use at intensive care units: a modified-RAND Delphi study PLOS ONE. 2018;13: e0207991.
Keller D, Zhang J, Chand M. Opioid-free colorectal surgery: a method to improve patient & financial outcomes in surgery. Surg Endosc. 2019;33:1959–66.
Kessler ER, Shah M, Gruschkus SK, Raju A. Cost and quality implications of opioid-based postsurgical pain control using administrative claims data from a large health system: opioid-related adverse events and their impact on clinical and economic outcomes. Pharmacotherapy. 2013;33:383–91.
Kelley, E, Hurst J. Health care quality indicators project: Conceptual Framework Paper. OECD Health Working Papers 2006; 23.
Kiang MV, Humphreys K, Cullen MR, Basu S. Opioid prescribing patterns among medical providers in the United States, 2003–17: a retrospective, observational study. Br Med J. 2020;368:l6968.
Lancet The. Managing the opioid crisis in North America and beyond. The Lancet. 2022;399:495.
Lee A, Chan SK, Chen PP, Gin T, Lau AS, Chiu CH. The costs and benefits of extending the role of the acute pain service on clinical outcomes after major elective surgery. Anesth Analg. 2010;111:1042–50.
Lee JS, Hu HM, Edelman AL, et al. New persistent opioid use among patients with cancer after curative-intent surgery. J Clin Oncol. 2017;35:4042–9.
Levy N, Quinlan J, El-Boghdadly K, Fawcett WJ, Agarwal V, Bastable RB, et al. An international multidisciplinary consensus statement on the prevention of opioid-related harm in adult surgical patients. Anaesthesia. 2021;76:520–36.
Macintyre PE, Huxtable CA, Flint SL, Dobbin MD. Costs and consequences: a review of discharge opioid prescribing for ongoing management of acute pain. Anaesth Intensive Care. 2014;42:558–74.
Mainz J. Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care. 2003;15:523–30.
Meyer DC, Hill SS, McDade JA, et al. Dis Colon Rectum. 2021;64:103–11.
Minkowitz HS, Gruschkus SK, Shah M, Raju A. Adverse drug events among patients receiving postsurgical opioids in a large health system: risk factors and outcomes. Am J Health Syst Pharm. 2014;71:1556–65.
Mujukian A, Truong A, Tran H, Shane R, Fleshner P, Zaghiyan K. A standardized multimodal analgesia protocol reduces perioperative opioid use in minimally invasive colorectal surgery. J Gastrointest Surg. 2020;24:2286–94.
National Quality Measures Clearinghouse. Agency for Healthcare Research and Quality; Patient Safety Network Home | PSNet (ahrq.gov) (accessed 2nd January 2022).
Neuman MD, Bateman BT, Wunsch H. Inappropriate opioid prescription after surgery. Lancet. 2019;393:1547–57.
Oderda GM, Gan TJ, Johnson BH, Robinson SB. Effect of opioid-related adverse events on outcomes in selected surgical patients. J Pain Palliat Care Pharmacother. 2013;27:62–70.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan; a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation | The EQUATOR Network (equator-network.org) (accessed 22nd March 2022).
Pruitt LCC, Swords DS, Vijayakumar S, et al. Implementation of a quality improvement initiative to decrease opioid prescribing in general surgery. J Surg Res. 2020;247:514–23.
Pullman A, Syrowatka A, Businger A, et al. Development and alpha testing of specifications for a prolonged opioid prescribing electronic clinical quality measure (eCQM). AMIA Annu Symp Proc. 2021;2020:1022–30.
Rademakers J, Delnoij D, de Boer D. Structure, process of outcome: which contributes most to patients’ overall assessment of healthcare quality? BMJ Qual Saf. 2011;20:326–31.
Roughead EE, Lim R, Ramsay E, Moffat AK, Pratt NL. Persistence with opioids post discharge from hospitalisation for surgery in Australian adults: a retrospective cohort study. BMJ Open. 2019;4:e023990.
Schieber LZ, Guy GP Jr, Seth P, Young R, Mattson CL, Mikosz CA, et al. Trends and patterns of geographic variation in opioid prescribing practices by State, United States, 2006–2017. JAMA Network Open. 2019;2: e190665.
Small C, Laycock H. Acute postoperative pain management. British Journal of Surgery. 2020;107:e70–80.
Standards and Indicators | NICE (accessed 22nd March 2022)
Stafford C, Francone T, Roberts PL, Ricciardi R. What factors are associated with increased risk for prolonged postoperative opioid usage after colorectal surgery? Surg Endosc. 2018;32:3557–61.
Stelfox H, Straus S. Measuring quality of care: considering measurement frameworks and needs assessment to guide quality indicator development. J Clin Epidemiol. 2013;66:1320–7.
Srivastava D, Hill S, Carty S et al. BJA 2021 126, 1208-16. Surgery and opioids: evidence based consensus guidelines on the perioperative use of opioids in the UK. British J Anesth. 2021;126:1208-16.
Syrowatka A, Pullman A, Kim W, et al. Re-tooling an Existing Clinical Quality Measure for Chronic Opioid Use to an Electronic Clinical Quality Measure (eCQM) for Post-operative opioid prescribing: development and testing of draft specifications. AMIA Annu Symp Proc. 2021;2020:1200–9.
Thiele R, Rea K, Turrentine F. Standardization of care: impact of an enhanced recovery protocol on length of stay, complications, and direct costs after colorectal surgery. J Am Coll Surg. 2015;220:430–43.
Thiels CA, Anderson SS, Ubl DS, et al. Wide variation and overprescription of opioids after elective surgery. Ann Surg. 2017;266:564–73.
Truong A, Mujukian A, Fleshner P, Zaghiyan K. No pain, more gain: reduced postoperative opioid consumption with a standardized opioid-sparing multimodal analgesia protocol in opioid-tolerant patients undergoing colorectal surgery. Am Surg. 2019;85:1155–8.
Tsui SL, Tong WN, Irwin M, et al. The efficacy, applicability and side-effects of postoperative intravenous patient-controlled morphine analgesia: an audit of 1233 Chinese patients. Anaesth Intensive Care. 1996;24:658–64.
Verhamme KMC, Bohnen AM. Are we facing an opioid crisis in Europe? The Lancet Public Health. 2019;4:e483–4.
Wang TV, Okose O, Abt NB, Kamani D, Emerick KS, Randolph GW. One institution’s experience with self-audit of opioid prescribing practices for common cervical procedures. Head Neck. 2021;43:2385–94.
Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. J Am Med Assoc Surg. 2017;152:691–7.
Yap R, Nassif G, Hwang G, et al. Achieving opioid-free major colorectal surgery: is it possible? Dig Surg. 2020;37:376–82.
Acknowledgements
Not applicable
Funding
The Yorkshire Cancer Research Bowel Cancer Improvement Programme is funded by Yorkshire Cancer Research (YCR) Grant L394. YCR had no direct involvement in the design of the study, collection, analysis, interpretation of data or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
SA performed the literature search. MA, KP, and DY reviewed all abstracts. CT and SJH read all full texts. CT and SJH extracted all indicators. CT wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary materials 1.
Extracted quality indicators
Additional file 2: Supplementary materials 2.
Characteristics of papers
Additional file 3: Supplementary materials 3.
Quality indicators and themes
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Thomas, C., Ayres, M., Pye, K. et al. Process, structural, and outcome quality indicators to support perioperative opioid stewardship: a rapid review. Perioper Med 12, 34 (2023). https://doi.org/10.1186/s13741-023-00312-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13741-023-00312-4