Abstract
Background
Breast cancer incidence has been on the rise significantly in the Asian population, occurring at an earlier age and a later stage. The potential predictive value of molecular subtypes, biomarkers, and genetic variations has not been deeply explored in the Asian population. This study evaluated the effect of molecular subtype classification and the presence or absence of biomarkers and genetic variations on pathological complete response (pCR) after neoadjuvant treatment in Asian breast cancer patients.
Methods
A systematic search was conducted in MEDLINE (PubMed), Science Direct, Scopus, and Cochrane Library databases. Studies were selected if they included Asian breast cancer patients treated with neoadjuvant chemotherapy and contained data for qualitative or quantitative analyses. The quality of the included studies was assessed using the Newcastle Ottawa Scale. Following the random effects model, pooled odds ratios or hazard ratios with 95% confidence intervals for pCR were analysed using Review Manager Software. Heterogeneity between studies was assessed using Cochran’s Q-test and I2 test statistics.
Results
In total, 19,708 Asian breast cancer patients were pooled from 101 studies. In the neoadjuvant setting, taxane-anthracycline (TA) chemotherapy showed better pCR outcomes in triple-negative breast cancer (TNBC) (p<0.0001) and human epidermal growth factor receptor 2 enriched (HER2E) (p<0.0001) than luminal breast cancer patients. Similarly, taxane-platinum (TP) chemotherapy also showed better pCR outcomes in TNBC (p<0.0001) and HER2E (p<0.0001). Oestrogen receptor (ER)-negative, progesterone receptor (PR)-negative, HER2-positive and high Ki-67 were significantly associated with better pCR outcomes when treated with either TA or TP. Asian breast cancer patients harbouring wildtype PIK3CA were significantly associated with better pCR outcomes when treated with TA in the neoadjuvant setting (p=0.001).
Conclusions
In the neoadjuvant setting, molecular subtypes (HER2E and TNBC), biomarkers (ER, PR, HER2, HR, Ki-67, nm23-H1, CK5/6, and Tau), and gene (PIK3CA) are associated with increased pCR rates in Asian breast cancer patients. Hence, they could be further explored for their possible role in first-line treatment response, which can be utilised to treat breast cancer more efficiently in the Asian population. However, it needs to be further validated with additional powered studies.
Systematic review registration
PROSPERO CRD42021246295.
Similar content being viewed by others
Background
Breast cancer is one of the most prevalent and heterogeneous cancers that predominantly affect women. According to GLOBOCAN 2020 [1], 2.3 million women were diagnosed with breast cancer, and 685,000 had died from the disease. This is a trend expected to rise due to early screening and detection [1]. Early diagnosis of the disease and effective treatment are paramount to improve patients’ condition, mortality, survival outcome, and prognosis [2].
Biomarkers are utilised to determine the type of systemic treatment to be administered to cancer patients [3]. Biomarkers can be genetic and non-genetic; they can be detected through gene sequencing and conventional immunohistochemistry (IHC). Clinically, gene sequencing is not always readily available compared to the assessment of IHC for the biomarkers. The most defined therapeutic molecular classification of breast cancer is based on the status of oestrogen receptors (ER), progesterone receptors (PR), human epidermal growth factor receptor 2 (HER2), and Ki-67 [4,5,6]. An extensive molecular classification of breast cancer characterising each subtype was first proposed by Perou et al. [6]. Through the expression of 496 intrinsic genes, breast cancer classification was subgrouped as luminal, HER2+, normal-like, and basal-like [6]. Subsequently, the luminal subtype was further subgrouped into luminal A, luminal B, and luminal C [7]. After re-evaluation, the luminal subtype was reduced to luminal A and luminal B [8]. Despite the advances in molecular subtyping, the St. Gallen Consensus allows IHC assessment of ER, PR, HER2, and several biomarkers as a surrogate classification for the molecular subtype of breast cancer. The panel agreed to molecularly characterise the subtypes as luminal A, luminal B, HER2-enriched (HER2E), and triple-negative breast cancer (TNBC) [5].
Biomarkers offer a wide range of potential uses in cancer, including risk assessment, screening, differential diagnosis, prognosis, treatment outcome prediction, and monitoring disease progression [9]. Biomarkers can be prognostic or predictive; the former allows insight into the overall cancer outcome of the patient regardless of the therapy given, while the latter provides information on whether a patient will benefit from a particular treatment [10]. Consequently, this allows the discernment of aggressive and non-aggressive breast cancer, especially in later stages. Due to this, biomarkers remain an area that is actively under investigation and validation [11]. The role of ER, PR, HER2, and Ki-67 in breast cancer remains important as biomarkers, nevertheless there are other expressions worth investigating. Amongst the investigated biomarkers include Tau, nm-23-H1, CK5/6, and epidermal growth factor receptor (EGFR) [12]. In this study, we defined these IHC-expressed markers as biomarkers.
Despite not being clinically available in most countries, nowadays, genetic biomarkers (henceforth referred to as genetic variations in this study) have gained significant interest in oncology practice, as they can be used for targeted treatment selections [13]. The variation in the genetic component is understood as the changes in the DNA sequence in an individual’s genome, which occurs at different frequencies within an individual across the population [13]. Genetic variations can exist in various forms, such as single-nucleotide polymorphism (SNP), short insertions or deletions, large mutations, null alleles, and transposable elements [13]. Some of the commonly mutated genes associated with breast cancer include TP53, PIK3CA, BRCA1, and BRCA2 [14]. Consequently, these genetic variations have been reported to affect drug metabolism and disease susceptibility [15].
The emergence of personalised and precision medicine (PPM) is thought to be a better-fit therapeutic approach for oncology. Separately, precision medicine is defined as a therapeutic approach based on selecting definite biomarkers that predict a targeted therapy’s efficacy in a specific group of patients. Although the term personalised medicine is often interchangeably used as its synonym, it refers to the justification of the therapeutical choices for each patient [16]. Hence, it provides an opportunity to offer a better-fit treatment tailored to each patient, fitting the discovery that not all cancer is the same and varies heavily in each individual depending on their genetic changes [17, 18]. In this study, we used both precision and personalised terms and defined PPM as an emerging practice of medicine that uses an individual’s genetic profile, derived from their disease diagnosis, which includes molecular subtypes, biomarkers, and genetic variations, to guide decisions made concerning their therapeutic approach or choice.
The efficacy of cancer treatment can be evaluated through pathological complete response (pCR), disease-free survival (DFS), and overall survival (OS) [19]. pCR, defined as the absence of any residual disease in the breast and lymph nodes, can be used to predict DFS and OS since it is typically used as an endpoint for novel neoadjuvant chemotherapy (NAC) to predict the therapeutic outcome in the long run [19]. In this study, we emphasised the attainment of pCR following NAC as the focused efficacy outcome.
Classifying breast cancer based on molecular subtypes is a growing clinical practice that warrants benefits [2, 20, 21] and it is primarily conducted in the West [22, 23]. There is limited information on this practice in the Asian population [24]. Breast cancer incidence in the Asian population occurs at an earlier age with later stages compared to the Western population [25]. Furthermore, there are differences in the genetic polymorphism, epigenetics, and environmental interplay, which may cause treatment outcomes to differ [25, 26]. Therefore, it is imperative to evaluate the association between breast cancer diagnoses and their response to treatment. This systematic review and meta-analysis aimed to assess the involvement of PPM in breast cancer treatment in the Asian population by evaluating the association between breast cancer treatment response, specifically pCR and NAC treatment provided to breast cancer patients based on their breast cancer molecular subtypes, biomarkers, and genetic variation characterisation.
Methods
Study design
This study protocol was registered at PROSPERO (CRD42021246295). The systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-2020 checklist guideline (Additional file 1) [27].
Inclusion and exclusion criteria
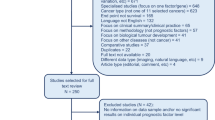
The type of studies included in this review consists of randomised trials, observational studies, case-control studies, and cohort studies written in the English language. All Asian breast cancer aged ≥ 18 years, who underwent systemic neoadjuvant chemotherapy treatment reporting the involvement of somatic genetic polymorphisms or biomarkers or molecular subtype classification on breast cancer treatment response were included. Studies were excluded if one or more of the following reasons were met: (1) non-Asian breast cancer cohort studies or non-breast cancer patients; (2) breast cancer patients undergoing other treatment that is not related to drug, i.e., radiotherapy, herbal medicine, and surgery; (3) studies with incomplete data for qualitative and/or quantitative synthesis. Fig. 1 shows how the studies were searched and identified in the various databases and registers.
Literature searches
The search was electronically performed in the MEDLINE (PubMed), Science Direct, Scopus, and Cochrane Library databases to retrieve articles that studied the role of molecular subtypes, biomarkers, and genetic variations in the outcome of breast cancer patients undergoing chemotherapy. Search terms were constructed based on patients, interventions and comparison, and outcomes (Additional file 2). The search term strategies were adapted for different databases utilising a combination of Medical Subject Heading (MeSH) and keywords that are relevant which can be found in the titles and abstract. Articles available from 1st January 2000 to 31st March 2021 were searched on MEDLINE, Science Direct, Scopus and the Cochrane Library. The search strategy was conducted from 24th March 2021 to 31st March 2021, with the finalised MeSH terms and search strategies were run again and harvested on the 31st of March 2021 to ensure the same results were generated. The search strategy can be found in detail for MEDLINE (Supplementary Table 2.2 in Additional file 2), Science Direct (Supplementary Table 2.3 in Additional file 2), Scopus (Supplementary Table 2.4 in Additional file 2), and the Cochrane Library (Supplementary Table 2.5 in Additional file 2).
Data extraction
The retrieved search results were uploaded to Rayyan [28] for automated detection of duplicate records after manual removal with Mendeley, followed by initial eligibility screening of the abstracts and titles, applying the inclusion and exclusion criteria. The full-text articles for the remaining abstracts were retrieved and read for eligibility screening, applying the same inclusion and exclusion criteria. Two independent reviewers (NWSB and SNIM) conducted the eligibility screening. Any conflict was resolved by a third independent reviewer (AM). The included studies were randomly distributed amongst three independent reviewers (NWSB, SNIM, and AM) to extract relevant data using a standardised data extraction format using Microsoft Excel (Additional file 3).
For each study, the extracted parameters include the article information (article title, first author, year published, journal published, country, and year of recruitment), study design, study population and sample size, characteristics of patients in three variables (molecular subtypes, biomarkers, and genetic variations), and the pCR data in selected variables. Notably, in the absence of molecular subtype classification in the included studies, whenever possible, they were approximated through the available biomarkers detected through IHC data [5]. In this study, the molecular subtype classification is defined as luminal A (ER+, PR+, HER2−, and low Ki-67), luminal B (ER+, PR+, HER2+/HER2−, and high Ki-67), HER2E (ER−, PR−, and HER2+), and TNBC (ER−, PR−, and HER2−). Due to limited resources, the same reviewers (NWSB, SNIM, and AM) checked the data extraction process. Each reviewer is assigned a different article from the one they extracted in the previous stage. Notably, the reference lists of all selected publications and review articles were checked to identify further eligible studies missed in the MEDLINE (PubMed), Science Direct, Scopus, and Cochrane Library search.
All extracted data from selected parameters which include the study ID, country, quality assessment score, molecular subtypes, number of patients, number of pCR events in breast cancer patients treated with each NAC treatment, and crude and adjusted reported pCR association were combined and evaluated by the reviewer (NWSB) using standardised data synthesis excel sheets (Additional file 4). Two independent reviewers (SNIM and AM) cross-checked the synthesised data.
Risk of bias in individual studies
The quality of all included studies was appraised independently by two reviewers (NWSB and SNIM) using a quality score system based on the Newcastle-Ottawa Scale (NOS) adapted for case-control studies or cohort studies (Additional file 5), with scores ranging from 0 (lowest) to 9 (highest). NOS utilised three domains: (1) selection, (2) comparability, and (3) exposure for case-control studies or outcomes for cohort studies [29]. The selection domain of case-control studies was appraised based on the description of study subjects and setting, while the exposure domain was appraised based on exposure measurement. Comparatively, the selection domain of cohort studies was appraised based on the description of study subjects and settings as well as the exposure measurement. The outcome domain was appraised by the outcome and follow-up assessment. The comparability domain of both case-control and cohort studies was appraised based on study design, analysis, and characterisation. Studies with an overall score of 0–3 were considered low quality, 4–5 were deemed medium quality, and 6 or above were regarded as high quality. Any discrepancies were resolved by consensus.
Data analysis and synthesis
Data analysis was done using Review Manager Software (RevMan version 5.4.1) [30]. The odds ratio (OR), hazards ratio (HR), and their corresponding 95% confidence interval (95% CI) were assessed to evaluate the association between treatment response (pCR) and NAC treatment provided to breast cancer patients based on their molecular subtypes, biomarkers, and genetic variations. The strength of associations was estimated by calculating pooled ORs/HRs and 95% CIs, by which significance was stated using the p-value. A p-value <0.05 was considered statistically significant.
Two methods provided in RevMan were used. The first method utilises dichotomous outcomes parameters to measure the OR depicting the association between pCR and selected variables using the Mantel-Haenszel method [31] under the random effect model. The second method utilises the inverse-variance approach to evaluate the studies’ pooled association data, included under the random effects model using the DerSimonian and Laird method [32]. The preference for the favoured variable significantly associated with treatment response was based on the most frequent report in the pooled included studies (Supplementary Table 4.6 in Additional file 4). In any case of discordance of the 95% CI value entered intoRevMan obtained from the study, the software-generated value was used. Both crude and adjusted results were included in the analysis when available. For both methods, whenever possible or required, subgroup analysis was conducted. By convention, a pooled OR/HR <1 represents a worse treatment response, while a pooled OR/HR >1 represents a better treatment response for breast cancer patients.
Meta-bias assessment
The between-study heterogeneity was assessed by Cochran’s chi-square-based Q-test and I2 index. It is considered statistically significant when p-value <0.05 and/or I2 index >50% [33]. The publication bias assessment was done when at least six studies were pooled for meta-analysis. The evaluation was made through visual inspection of funnel plot asymmetry and fail-Safe N test using the Rosenthal approach. Rank correlation and regression tests, using the standard error of the observed outcomes as predictors, are also used to check for funnel plot asymmetry.
Results
Article selection
A total of 8963 records were identified using different databases including MEDLINE, PubMed, ScienceDirect, Scopus and Cochrane Library. In total, 2284 records were excluded because of duplication, the removal was conducted through both manual removal and using an automation tool known as Rayyan. Then 6564 records were excluded after the initial title and abstract screening due to unmet inclusion criteria. Of the remaining 115 records, the full-text articles were carefully read, and 14 records were excluded due to insufficient pCR data and inaccessibility. Finally, 101 studies fulfilled the eligibility criteria and were included in the systematic review and meta-analysis (Fig. 1).
Overview of included studies
Altogether, 19,708 Asian breast cancer patients were gathered from the 101 studies, with an average of 195 patients per study (Supplementary Table 4.1 in Additional file 4). The study population comprised 91 studies from Eastern Asia (China [8, 12, 34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115], Hong Kong [116, 117], Korea [118], and Japan [119,120,121,122]), 7 studies from Western Asia (Egypt [123], Iran [124], Turkey [125, 126], and Saudi Arabia [127,128,129]), 2 studies from Southeast Asia (Indonesia [130], Singapore and Malaysia [131]), and 1 study from South Asia (India [132]). The recruitment period for the patients enrolled in the studies ranged from 1991 to 2020. Most of the study cohorts followed hospital-based study design (76.2%) and clinical trials (14.9%), while 8.9% were not reported. 61.3% of the hospital-based study designs were conducted in unicenter, while 14.9% were in multicenter. Of the 101 studies, only 65 studies provided molecular subtype data (n=11361) - TNBC (29.2%), HER2E (20.7%), luminal B (13.2%), and luminal A (7.2%), while 1.6% were missing. Several studies did not categorise their luminal subtype into luminal A or B. Hence, they were reported as luminal-like (24.9%) in this study. Only 69 studies provided data on biomarkers, comprising the routinely analysed biomarkers—ER (25.1%), PR (25.1%), HR (5.7%), HER2 (27.4%), and Ki-67 (15.5%)—and several non-conventional biomarkers investigated specifically for the study including EGFR (11.0%), CK5/6 (8.0%), Tau (11.7%), Androgen Receptor (AR) (8.6%), PDL1 (3.6%), P-glycoprotein (P-gp) (3.3%), DNA topoisomerase II-alpha (TopoIIa) (3.2%), p53 (9.8%), and others (0.8–4.0%) (Supplementary Table 3.1 in Additional file 3). Meanwhile, 7 studies provided information on genetic variations and differential expression, where the common genetic variations reported were from TP53 (15.7%), PIK3CA (24.6%), MYC (5.8%), ERRB2 (5.8%), CCDN1 (5.8%), BRCA1 (15.7%), BRCA2 (15.7%), and others (10.9%).
All the patients in the studies received NAC, and 25.0% of patients received follow-up adjuvant therapy. Collectively, NAC taxane-anthracycline (TA), taxane-platinum (TP), and taxane-anthracycline-platinum (TAP) combination were mentioned in 41.5%, 18.6%, and 1.5% of the studies, respectively. Meanwhile, 18.3% were treated with NAC anthracycline-based chemotherapy, 14.0% were treated with NAC taxane-based chemotherapy, and 8 studies did not provide specific treatment information. Some patients were treated concomitantly with targeted therapy and endotherapy (23.0%). The definition of pCR used in the included studies was mostly not reported according to any guideline (71.3%), with only 28.7% reported pCR following the Miller-Payne grading (17.8%), Kuerer et al. (1.9%), RECIST (2.9%), and other grading systems (6.1%) including the Ribero classification, Japanese Breast Cancer Society v2007, USFDA guideline, WHO criteria, and pathological TNM system.
Furthermore, 33 of the included studies conducted the multivariate analysis. Most of the included variables used to adjust the multivariate analysis were the commonly reported biomarkers (ER, PR, HER2, and Ki-67), age, tumour size and grade, age at diagnosis, lymph node stage, histological grade, body mass index (BMI), chemotherapy regimens, chemotherapy cycles, and other biomarkers and genetic variations unique to the study.
Quality of the included studies
The quality assessment of the studies was presented in Supplementary Tables 6.1 and 6.2 (Additional file 6). Fourteen (14) case-control studies and 87 cohort studies were included in our systematic review. NOS scores for the 87 cohort studies ranged from 5 to 9 stars, and NOS scores for the 14 case-control studies ranged from 4 to 9 stars. No study was excluded since all studies scored ≥4 stars.
A summary of the risk of bias assessed on each question using the NOS for cohort and case-control studies is shown in Supplementary Figures 6.1 and 6.2 (Additional file 6). We considered both breast cancer treatment and characterisation as the most important factors for adjustment in the comparability domain because our study eligibility criteria required adjustment for the involvement of somatic genetic polymorphisms or biomarkers or molecular subtypes in breast cancer treatment response. Following this consideration, only 33% (n=29/87) cohort studies earned a star for comparability regarding pCR and breast cancer treatment, while 94% (n=82/87) cohort studies earned a star regarding pCR and breast cancer characterisation. As for case-control studies, 79% (n=11/14) studies earned a star for comparability regarding pCR and breast cancer treatment, while 93% (n=13/14) studies earned a star regarding pCR and breast cancer characterisation. Notably, when both adjustment factors were combined, only 31% (n=27/87) cohort studies and 71% (n=10/14) case-control studies earned both stars in the comparability domain. Amongst the cohort studies, evaluation of the selection of the non-exposed cohort was the question with the lowest count of stars, with only 32% (n=28/87) of the studies having a low risk of bias. Meanwhile, amongst the case-control studies, apart from the first adjustment in the comparability domain, the lowest count of stars was for the question evaluating the selection of controls, with 79% (n=11/14) of studies showing a low risk of bias.
Association of breast cancer characterisation and treatment response
The molecular subtypes classification of breast cancer, presence or absence of specific biomarkers, and genetic variations in the breast cancer diagnosis can be utilised to predict the pCR outcome in patients treated with specific chemotherapeutic agents. Five molecular subtypes, fourteen biomarkers, and eleven genetic variations were qualitatively evaluated for their predictive value in Asian breast cancer patients (Supplementary Table 4.2.2 in Additional file 4). Meanwhile, of the 101 studies, 60 studies provided data that could be used for meta-analysis (Figs. 2, 3, 4, 5, 6 and 7 in the manuscript and Supplementary Figures 7.1– 7.8 in Additional file 7). All the qualitative and meta-analyses results are presented by the molecular classification, biomarkers, and genetic characterisation of Asian breast cancer patients. Additionally, meta-analysis results using the Mantel-Haenszel method listed under each breast cancer characteristic are grouped according to the chemotherapeutic agents. Meta-analysis results using the inverse-variance method are presented separately since it is pooling the reported association data, for which they are presented by the breast cancer characteristics as well.
Pooled pCR outcome of TA-treated Asian breast cancer patients according to molecular subtypes. Forest plots describing the random effect ORs and 95% CIs from studies assessing the association of pCR outcome in NAC TA-treated breast cancer patients between (A) HER2E and luminal-like; (B) HER2E and luminal A; (C) HER2E and luminal B; (D) HER2E and luminal, combined; and (E) TNBC and luminal-like; (F) TNBC and luminal A; (G) TNBC and luminal B; and (H) TNBC and luminal, combined. I2 and p-value for X2 of heterogeneity are reported for each group analysis
Pooled pCR outcome of TP-treated Asian breast cancer patients according to molecular subtypes. Forest plots describing the random effect ORs and 95% CIs from studies assessing the association of pCR outcome in NAC TP-treated Asian breast cancer patients between (A) HER2E and luminal-like; (B) HER2E and luminal A; (C) HER2E and luminal B; (D) HER2E and luminal, combined; (E) Luminal B and luminal A; (F) TNBC and luminal A; (G) TNBC and luminal B. I2 and p-value for X2 of heterogeneity are reported for each group analysis
Pooled pCR outcome of NAC-treated Asian breast cancer patients according to molecular subtypes and biomarkers. Forest plots describing the random effect ORs and 95% CIs from studies assessing the association of pCR outcome in (A) NAC TP-treated Asian breast cancer patients between TNBC and luminal, combined; (B) between Asian TNBC patients treated with NAC TP and TA; Asian breast cancer patients treated with anthracycline-based chemotherapy with (C) ER; (D) PR; and (E) HER2 biomarkers; (F) Asian breast cancer patients treated with taxane-based chemotherapy and HR biomarker; (G) Asian breast cancer patients treated with TA and ER biomarker. I2 and p-value for X2 of heterogeneity are reported for each group analysis
Pooled pCR outcome of TA-treated Asian breast cancer patients according to biomarkers. Forest plots describing the random effect ORs and 95% CIs from studies assessing the association of pCR outcome in NAC TA-treated breast cancer patients in biomarkers (A) PR; (B) HR; (C) HER2; (D) nm23-H1; and (E) CK5/6. I2 and p-value for X2 of heterogeneity are reported for each group analysis
Pooled pCR outcome of NAC-treated Asian breast cancer patients according to biomarkers. Forest plots describing the random effect ORs and 95% CIs from studies assessing the association of pCR outcome in (A) NAC TA-treated breast cancer patients in biomarkers Ki-67; NAC TP-treated breast cancer patients in biomarkers (B) ER; (C) PR; (D) HR; and (E) Ki-67. I2 and p-value for X2 of heterogeneity are reported for each group analysis
Pooled pCR outcome of NAC-treated Asian patients according to biomarkers and genetic variation. Forest plots describing the random effect ORs and 95% CIs from studies assessing the (A) Association of pCR outcome in NAC TP-treated Asian breast cancer patients in HER2; (B) Association between pCR in Asian patients with HER2+ biomarker treated with NAC TP and TA; and (C) Association of pCR outcome in NAC TA-treated Asian breast cancer patients in PIK3CA gene. I2 and p-value for X2 of heterogeneity are reported for each group analysis
Molecular subtype classification
Qualitatively, most studies with molecular subtype classification provide data on the pCR rates of patients treated with TA and TP regimens. When treated with TP, luminal A had the lowest pCR rate of 7.7% (n=4), while the highest pCR rate was observed in HER2E at 52.4% (n=7). In comparison, the pCR rates in the other subtypes were 32.5% (n=3), 28.1% (n=4), and 41.7% (n=7) for luminal-like, luminal B, and TNBC, respectively. However, when treated with NAC TA, the highest pCR rate was observed in TNBC at 30.4% (n=20), and similarly, the lowest pCR rate was observed in luminal A at 4.3% (n=5). Comparatively, the pCR rates in luminal-like, luminal B, and HER2E were 9% (n=6), 12% (n=5), and 27.8% (n=9), respectively. Our findings suggest that patients with TNBC and HER2E subtypes treated with NAC TP and TA were more likely to obtain pCR, while luminal A was less likely to obtain pCR with both regimens.
Under meta-analysis, the role of molecular subtypes was examined in NAC TA-treated (Figure 2 and Supplementary Figure 7.1 in Additional file 7) and TP-treated (Figures 3 and 4 and Supplementary Figure 7.1 in Additional file 7) breast cancer patients.
Taxane-anthracycline (TA) chemotherapy
Our study first compares the effect of HER2E and luminal subtypes on pCR outcomes in TA-treated patients (Fig. 2A–D). In the analysis of four pooled studies [34, 35, 98, 100] comparing HER2E and luminal-like subtypes, 494 were identified with HER2E subtype and 764 patients with luminal-like subtype. Despite the large number of patients with luminal-like subtypes, our findings significantly associate patients with HER2E subtypes with better pCR outcomes (OR: 4.08; 95% CI; 2.78–6.00; p<0.0001; Fig. 2A). When HER2E patients were compared with patients with luminal A subtype, patients with HER2E subtypes were also found to be significantly more likely to achieve pCR (OR 5.27; 95% CI 1.16–23.86; p=0.03; Fig. 2B). Similarly, when HER2E was analysed against luminal B, HER2E was significantly associated with pCR (OR 2.78; 95% CI 1.42–5.44; p=0.003; Fig. 2C). To confirm and elucidate the effect of luminal subtypes on pCR outcome in NAC TA-treated breast cancer patients, we combined all luminal data (luminal-like, luminal A, and luminal B) as luminal, combined and compared it against HER2E patients. Nine studies [34, 35, 71, 80, 84, 95, 98, 100, 113] were pooled, yet our findings still showed that HER2E subtype was significantly associated with pCR outcome in NAC TA-treated patients (OR 3.89; 95% CI 2.69-5.64; p<0.0001; Fig. 2D).
Similarly, analyses conducted comparing the effect of TNBC and luminal subtypes on pCR outcome in TA-treated patients (Fig. 2E–H) significantly associate TNBC with better pCR outcome compared to luminal-like (OR 4.45; 95% CI 2.79–7.11; p<0.0001; Fig. 2E), luminal A (OR 11.66; 95% CI 3.64-37.38; p<0.0001; Fig. 2F), luminal B (OR 3.89; 95% CI 2.20–6.87; p<0.0001; Fig. 2G), and luminal, combined (OR 4.59; 95% CI 3.35–6.29; p<0.0001; Fig. 2H).
To further explore the effect of molecular subtypes on the pCR outcome of NAC TA-treated breast cancer patients, the TNBC subtype was compared to the HER2E subtype revealing that neither was associated with pCR (OR 1.17; 95% CI 0.80-1.70; p=0.43; Supplementary Figure 7.1A in Additional file 7). Similarly, an analysis between luminal A and luminal B showed that neither was associated with better pCR outcome when treated with NAC TA (OR 2.47; 95% CI 0.79–7.73; p=0.12; Supplementary Figure 7.1B in Additional file 7).
Taxane-platinum (TP) chemotherapy
In the analysis pooling three studies [45,64,102] comparing HER2E and luminal-like subtypes, 321 patients were identified with HER2E subtype, and 382 patients were luminal-like. When treated with NAC TP, neither HER2E nor luminal-like patients were associated with pCR (OR 1.69; 95% CI 0.70–4.11; p=0.25; Fig. 3A). However, in the analysis pooling four studies [41, 69, 97, 115] comparing HER2E and luminal A subtypes, HER2E was significantly associated with pCR outcome (OR 12.11; 95% CI 4.41–33.26; p<0.0001; Fig. 3B). Similarly, when comparing against luminal B and luminal, combined, HER2E was significantly associated with pCR outcome (OR 5.92; 95% CI 2.59–13.54; p<0.0001; Fig. 3C and OR 3.37; 95% CI 1.66–6.84; p=0.0008; Fig. 3D, respectively). Substantial heterogeneity was reported for two of the pooled analyses: (1) in studies comparing HER2E and luminal-like (Fig. 3A); and (2) in studies comparing HER2E and luminal, combined (Fig. 3D). Although all three and seven studies pooled in the two analyses were performed in the Chinese population, the primary outcome assessed in Li et al. [57] and Xu et al. [97] focused on the contribution of genetic mutations or long non-coding RNAs (lncRNAs) as a predictor of pCR status in the recruited population. Consequently, pooled analysis excluding Li et al. eliminates the heterogeneity in the first analysis revealing significant association (OR 2.30; 95% CI 1.66–3.19; p<0.00001), while pooled analysis excluding Li et al. and Xu et al. in the second analysis decreased the heterogeneity, and maintaining the significant association (OR 3.80; 95% CI 2.02–7.13; p<0.0001).
Notably, when HER2E and TNBC patients were compared, neither was associated with pCR (OR 1.46; 95% CI 0.63–3.37; p=0.38; Supplementary Figure 7.1C in Additional file 7). We then compared luminal B and luminal A patients and found that luminal B patients were significantly associated with better pCR outcomes (OR 3.26; 95% CI 1.14–9.26; p=0.03; Fig. 3E). Similar to NAC TA-treated patients, analyses conducted comparing the effect of TNBC and luminal subtypes on pCR outcome in TP-treated patients also significantly associate TNBC with better pCR outcome compared to luminal A (OR 7.14; 95% CI 2.82–18.04; p<0.0001; Fig. 3F), luminal B (OR 2.19; 95% CI 1.09–4.41; p=0.03; Fig. 3G), and luminal, combined (OR 3.79; 95% CI 1.94–7.40; p<0.0001; Fig. 4A).
Our study compared the effect of chemotherapeutic agents on the pCR outcome in TNBC patients (Fig. 4B). Pooled analysis involving two studies [69, 108] showed that TNBC patients were significantly more likely to achieve pCR when treated with NAC TP (n=25/62) compared to NAC TA (n=7/48) (OR 3.76; 95% CI 1.43-9.87; p=0.007).
Biomarkers
Qualitatively, most studies with biomarkers data comprise of routinely analysed biomarkers—ER, PR, HER2, and Ki-67. In ER− and ER+ patients, anthracycline-based chemotherapy showed pCRrate of 27.2% (n=4) vs 15.3% (n=4). Meanwhile, TP, TA, and TAP chemotherapy showed pCR rate of 48.1% (n=6) vs 19.4% (n=5), 25.0% (n=6) vs 9.0% (n=7), and 29.7% (n=1) vs 12.9% (n=1), respectively. As for PR− and PR+ patients, anthracycline-based, TP, TA, and TAP chemotherapy showed pCR rate of 28.3% (n=2) vs 13.9% (n=2), 46.6% (n=5) vs 21.8% (n=5), 20.6% (n=4) vs 8.2% (n=4), and 25% (n=1) vs 13.3% (n=1), respectively. Collectively, ER− and PR− breast cancer patients were likely to benefit more from TP regimen than TA, TAP, and anthracycline-based chemotherapy. Notably, some studies combined their report of ER and PR as hormone receptors (HR). Analysis of HR+ and HR− patients showed pCR rate of 11.9% (n=1) vs 10% (n=1), 33.1% (n=2) vs 49.3% (n=2), 31.3% (n=2) vs 50.7% (n=3), and 12.4% (n=5) vs 23.2% (n=5) when treated with anthracycline-based, taxane-based, TP, and TA chemotherapy, respectively. Our findings suggested that HR+ breast cancer patients achieved a better pCR rate when treated with a single-based chemotherapeutic agent, while HR− patients benefit more combination chemotherapy regimens.
In HER2+ and HER2− patients, anthracycline-based chemotherapy showed pCR rate of 10.5% (n=3) vs 19.3% (n=4). Meanwhile, TP, TA, and TAP chemotherapy showed pCR rate of 44.6% (n=15) vs 24.3% (n=6), 20.1% (n=14) vs 11.3% (n=12) and 33% (n=1) vs 13.5% (n=1), respectively. One study [44] utilising CDK4/6 inhibitor on ER+/HER2− breast cancer patients and another study [118] utilising kinase inhibitor on ER+/HER2+ patients showed pCR rate of 5% (n=1) and 0% (n=1), respectively. Collectively, with the exception of anthracycline-based and targeted therapy, HER2+ breast cancer patients were likely to benefit more from TP, TA, and TAP regimens. Meanwhile, in patients with high and low Ki-67, anthracycline-based and taxane-based chemotherapy showed pCR rate of 12.2% (n=1) vs 11.4% (n=1) and 57.1% (n=1) vs 32.1% (n=1). When treated with TP and TA chemotherapy, the patients showed pCR rate of 39.9% (n=5) vs 24% (n=5) and 19.9% (n=12) vs 7.7% (n=12), respectively. Overall, breast cancer patients with high Ki-67 were likely to benefit more from taxane-based chemotherapy than TP, TA, and anthracycline-based regimen.
On the other hand, fourteen non-conventional biomarkers investigated in a few of the included studies were evaluated qualitatively. Three biomarkers—Bcl-2, Smac, and Survivin—were included for the evaluation of anthracycline-based chemotherapy. Anthracycline-based chemotherapy showed pCR benefit of 26.1% (n=1) vs 4.3% (n=1) in Bcl-2- and Bcl2+ breast cancer patients, 35.0% (n=1) vs 8.6% (n=1) in high and low Smac, and 28.3% (n=1) vs 11.5% (n=1) in low and high Survivin. Only one biomarker—ZEB1—was evaluated for TP chemotherapy which revealed pCR rates of 36.1% (n=1) in patients with low ZEB1 and 12.8% (n=1) in patients with high ZEB1.
Ten biomarkers—Tau, P-gp, Topo-II, T-cadherin, CK5/6, EGFR, p53, LAG-3, cyclin D1, and nm23-H1—were included for the evaluation of TA chemotherapy. Our findings showed pCR benefit of 31.3% (n=1) vs 4.5% (n=1) in Tau− and Tau+, 43.2% (n=1) vs 7.7% (n=1) in P-gp− and P-gp+, and 17% (n=1) vs 3.4% (n=1) in Topo-II- and Topo-II+ breast cancer patients. The pCR rates observed in T-cadherin- and T-cadherin+, CK5/6− and CK5/6+, EGFR− and EGFR+, and p53− and p53+ breast cancer patients were 45.2% (n=1) vs 7.4% (n=1), 40% (n=2) vs 25.6% (n=2), 45.5% (n=1) vs 28.1% (n=1), and 33.3% (n=1) vs 27.3% (n=1), respectively. As for breast cancer patients with low and high expression of LAG-3, the pCR rates was observed at 64.7% (n=2) vs 35.3% (n=2). Lastly, breast cancer patients with cyclin D1+ and nm23-H1+ reported pCR benefits of 45.8% (n=1) and 29.5% (n=2) than 29.4% (n=1) in cyclin D1− and 5.3% (n=2) in nm23-H1− breast cancer patients.
Under meta-analysis, the role of biomarkers was investigated in NAC anthracycline-based and taxane-based treated (Fig. 4), TA-treated (Figs. 4, 5 and 6 and Supplementary Figure 7.1 in Additional file 7), and TP-treated (Figs. 6 and 7) breast cancer patients.
Anthracycline-based and taxane-based chemotherapy
Four studies [53, 88, 102, 124] were pooled for the effect of ER on pCR outcome in anthracycline-treated patients, where ER was not associated with pCR (OR 1.95; 95% CI 0.98–3.89; p=0.06; Fig. 4C). Substantial heterogeneity was reported for the pooled analysis of ER− vs ER+, which could be explained by the study by Mohammadianpanah et al. [124] which was conducted in the Iranian population. In contrast, the other studies [53, 88, 102] were performed in the Chinese population. Subgroup analysis of ER− vs ER+ pooling studies in the Chinese population only showed that ER− patients were significantly associated with pCR (OR 2.52; 95% CI 1.43–4.44; p=0.001; Fig. 4C), supporting our hypothesis that the observed heterogeneity could be due to the difference in the Asian population. Notably, the observed moderate heterogeneity in the subgroup analysis can allude to by the differences in the population sizes of the three studies. Only two studies [88, 102] were pooled to analyse PR effect on pCR outcome in anthracycline-treated patients. Our findings showed that PR− patients were significantly associated with pCR (OR 2.40; 95% CI 1.52–3.80; p=0.0002; Fig. 4D). Meanwhile, an analysis of three pooled studies [88, 102, 109] on the effect of HER2 on pCR outcome in anthracycline-treated breast cancer patients revealed that patients with HER2− biomarker were significantly more likely to achieve pCR (OR 2.31; 95% CI 1.42–3.75; p=0.0008; Fig. 4E). Only one biomarker, HR, was evaluated for its effect on pCR outcome in Asian breast cancer patients treated with taxane-based chemotherapy (Fig. 4F). Two studies [74, 107] were pooled where patients with HR− biomarkers were significantly more likely to achieve pCR than HR− patients (OR 1.96; 95% CI 1.24–3.08; p=0.004).
Taxane-anthracycline (TA) chemotherapy
Eight biomarkers comprising ER, PR, HR, HER2, nm23-H1, CK5/6, EGFR, and Ki-67 were investigated for their effect on pCR outcome in Asian breast cancer patients treated with NAC TA. Six studies [45, 49, 52, 77, 81, 112] and four studies [36, 54, 80, 113] were pooled to evaluate the association of ER and PR, respectively. Both ER− (OR 3.19; 95% CI 2.15–4.75; p<0.0001; Fig. 4G) and PR− (OR 3.11; 95% CI 2.12-4.56; p<0.0001; Fig. 5A) were significantly associated with pCR outcome in TA-treated patients. Moderate heterogeneity was reported for the pooled analysis of ER− vs ER+. However, considering all the studies pooled for the analysis were performed in the Chinese population, the heterogeneity result was rejected.
In an analysis pooling five studies [60, 81, 98, 100, 127], HR was not associated with pCR outcome (OR 2.38; 95% CI 0.87–6.53; p=0.09; Fig. 5B). The observed substantial heterogeneity could be due to the study by Elnemr et al. [127] conducted in Saudi Arabia, while the other four studies were performed in China. Consequently, subgroup analysis of HR− vs HR+ removing the study by Elnemr et al. showed a decrease in the heterogeneity and significantly associated HR− with better pCR outcome when treated with TA (OR 3.58; 95% CI 1.62–7.90; p=0.002). An analysis of nine pooled studies [36, 54, 60, 80,81,82, 100, 113, 127] showed that HER2+ is significantly associated with pCR (OR 1.78; 95% CI 1.05–3.02; p=0.03; Fig. 5C) with substantial heterogeneity observed between the studies. Although the analysis also includes the study by Elnemr et al., which was conducted in Saudi Arabia, the heterogeneity could be influenced by the results pooled from seven studies that heavily pushed the effect of our analysis in one direction.
Our study synthesised meta-analysis data for other biomarkers apart from the commonly reported ones—ER, PR, HR, and HER2. In particular, two studies were evaluated for pCR outcome for nm23-H1 [12, 60] and CK5/6 [12, 90]. It was observed that nm23-H1− (OR 6.74; 95% CI 2.13–21.30; p=0.001; Fig. 5D) and CK5/6– (OR 1.87; 95% CI 1.03–3.39; p=0.04; Fig. 5E) are significantly associated with pCR. Two studies [12, 90] were pooled for analysis in the evaluation of pCR outcome with EGFR. Considerable heterogeneity was observed between the studies, perhaps alluded to the clinical differences between the studies of Li et al. [12] (n=22/41) and Wang et al. [90] (n=170/195) according to the distribution of patients with EGFR+. Despite that, EGFR is not associated with pCR outcome in TA-treated patients (OR 2.02; 95% CI 0.28–28.00; p=0.38; Supplementary Figure 7.1D in Additional file 7).
The proliferation index biomarker, Ki-67, was evaluated through an analysis of 12 pooled studies [12, 36, 54, 60, 80, 84, 90, 95, 98, 100, 111, 127], revealing significant association between pCR outcome and high Ki-67 (OR 2.98; 95% CI 1.79–4.97; p<0.0001; Fig. 6A). The observed moderate heterogeneity between the studies could be due to differences in the Ki-67 cut-off value. Subgroup analysis pooling four studies [36, 84, 111, 127] with 14% Ki-67 cut-off did not significantly associate Ki-67 with pCR outcome (OR 1.82; 95% CI 0.65–5.10; p=0.26). Significant heterogeneity was observed which could be explained by the primary research question addressed in the studies where Zhang et al. [111] focused on the prognostic value of magnetic resonance imaging (MRI), P-gp, and Ki-67, while the other three studies focused on the correlation of Ki-67 expression and pCR. Furthermore, the results pooled from the three studies heavily pushed the effect of our analysis in one direction. Thus, a pooled analysis excluding the study by Zhang et al. reveals null heterogeneity between the studies and a significant association between pCR and high Ki-67 with 14% cut-off value (OR 3.12; 95% CI 1.93–5.04; p<0.00001). Meanwhile, subgroup analysis pooling five studies [60, 90, 95, 98, 100] with 20% Ki-67 cut-off significantly associate pCR outcome with high Ki-67 (OR 2.88; 95% CI 1.36–6.10; p=0.006).
Taxane-platinum (TP) chemotherapy
Our study investigated five biomarkers comprising ER, PR, HR, HER2, and Ki-67 on their effect on pCR outcome in Asian breast cancer patients treated with NAC TP. Five studies [41, 43, 97, 114, 115] and two studies [100,102] were pooled to evaluate the association of ER and PR, and HR, respectively. pCR outcome was significantly associated with ER− (OR 4.91; 95% CI 3.20–7.53; p<0.00001; Fig. 6B), PR− (OR 3.82; 95% CI 2.48–5.90; p<0.00001; Fig. 6C), and HR− (OR 2.71; 95% CI 1.43–5.15; p=0.002; Fig. 6D).
Ki-67 was evaluated by analysing five pooled studies [47, 57, 97, 114, 115], showing that pCR outcome was not significantly associated with either high Ki-67 or low Ki-67 (OR 2.20; 95% CI 0.74–6.59; p=0.16; Fig. 6E). The observed considerable heterogeneity was perhaps due to differences in the Ki-67 cut-off value, and four of the five studies heavily pushed the effect of our analysis to one direction. Subgroup analysis pooling two studies [97, 114] with 20% Ki-67 cut-off indicates that pCR outcome is significantly associated with high Ki-67 (OR 4.37; 95% CI 1.62–11.75; p=0.003). This implicates the importance of having a standardised cut-off value for Ki-67, as at different cut-offs of 15 and 30%, neither Ki-67 biomarker was favoured as opposed to the 20% cut-off favours High Ki-67 to achieve pCR.
In the analysis of the effect of HER2 in breast cancer patients pooling five studies [41, 43, 97, 114, 115], pCR outcome was not significantly associated with neither HER2+ nor HER2− (OR 2.44; 95% CI 0.84–7.06; p=0.10; Fig. 7A). The observed substantial heterogeneity could be influenced by the results pooled from four of the five studies that heavily pushed the effect of our analysis in one direction. Consequently, a pooled analysis excluding the study by Zhou et al. [114] reveals null heterogeneity between the studies and a significant association between pCR and HER2+ (OR 4.14; 95% CI 2.51–6.85; p<0.00001).
Our study also evaluated the effect of chemotherapeutic agents on the pCR outcome in Asian breast cancer patients with HER2+ biomarker (Fig. 7B). Four studies [39, 51, 59, 110] were pooled and estimated. Our findings revealed neither NAC TP nor NAC TA was associated with pCR outcome in patients with HER2+ biomarker (OR 1.60; 95% CI 0.66–7.06; p=0.30). Substantial heterogeneity was reported which could be explained by the difference in the study design of the pooled studies. Of the four studies, Huang et al. [51] was the only study that conducted a randomised controlled trial (RCT) where the recruited HER2+ breast cancer patients were assigned to either TA or TP chemotherapy by the investigator. In contrast, HER2+ breast cancer patients recruited in the other three studies [39, 59, 110] were given either TA or TP regimen based on their preferences. Notably, subgroup analysis excluding Huang et al. decreased the heterogeneity I2 and significantly associated HER2+ breast cancer patients with better pCR outcome when treated with TP (OR 2.36; 95% CI 1.07–5.20; p=0.03).
Genetic variations and differential expression
Eleven genes—PIK3CA, TP53, EPIC1, TOP2A, ERBB2, MYC, CCND1, PCDH17, EPIC1, BRCA1, and BRCA2—were included for the qualitative evaluation of NAC regimens. No specific single variant vs wildtype was compared for most of the genes since most of the evaluated studies did not report them. Therefore, our analysis only compared wildtype (wt) and mutated (mt), where the mutated gene might contain single or multiple variants.
Breast cancer patient harbouring wt and mutated mtPIK3CA showed pCR rate of 19.4% (n=1) vs 14.1% (n=1) and 18.8% (n=1) vs 16.1% (n=1) when treated with anthracycline-based and taxane-based chemotherapy, respectively. Meanwhile, patients treated with TA chemotherapy showed a pCR rate of 21.3% (n=2) vs 9.4% (n=2). Thus, breast cancer patients with wtPIK3CA were likely to benefit more from TA regimen than anthracycline-based and taxane-based chemotherapy. Interestingly, breast cancer patient harbouring wt and mtTP53 showed pCR rate of 7.1% (n=1) vs 28.6% (n=1), 11.3% (n=1) vs 15.2% (n=1), and 6.1% (n=1) vs 16.1% (n=1) when treated with anthracycline-based, taxane-based, and TA chemotherapy, respectively. Our findings suggested that breast cancer patients with mtTP53 were likely to benefit more from anthracycline-based chemotherapy than taxane-based and TA regimen.
Our findings also showed that breast cancer patients with TOP2A, ERBB2, and MYC amplification (amp) achieved higher pCR rates than wtTOP2A, ERBB2, and MYC (56.3% (n=1) vs 13.8% (n=1), 28.4% (n=1) vs 6.1% (n=1), and 13.7% (n=1) vs 11.2% (n=1), respectively) when treated with TA regimens. On another note, breast cancer patients with wtCCND1 and unmethylated (unm) PCDH17 achieved higher pCR rate than those with CCND1 amp andmethylated (m) PCDH17 (13.8% (n=1) vs 2.7% (n=1) and 67.3% (n=1) vs 31.6% (n=1), respectively).
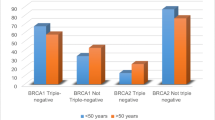
One included study by Mou et al. [71] focused on the effect of UGT2B7 rs7435335 on NAC TA efficacy. It was observed that patients with the genotype GA achieved higher pCR rate (42.3% (n=1)) than patients with the genotype GG (18.9% (n=1)). Another study by Xu et al. [96] analysed the effect of BRCA1 and BRCA2 mRNA expression in breast cancer patients treated with anthracycline-based and taxane-based chemotherapy. Our findings showed pCR benefit of 24.6% (n=1) vs 16.9% (n=1), 16.9% (n=1) vs 17.5% (n=1), and 14% (n=1) vs 20.8% (n=1) in anthracycline-based treated patients with low, intermediate, and high BRCA1 vs BRCA2 mRNA expression, respectively. Meanwhile, in taxane-based treated patients, our findings showed pCR benefit of 19.6% (n=1) vs 24.4% (n=1), 26.8% (n=1) vs 23.4% (n=1), and 21.4% (n=1) vs 18.9% (n=1) with low, intermediate, and high BRCA1 vs BRCA2 mRNA expression, respectively. Notably, breast cancer patients with low EPIC1 showed higher pCR rate (40.7% (n=1)) when treated with TP regimen than patients with high EPIC1 (33.3% (n=1)).
Under meta-analysis, only one gene was analysed for its effect on pCR outcome in Asian breast cancer patients treated with NAC TA (Fig. 7).
Taxane-anthracycline (TA) chemotherapy
From the analysis of two studies [100, 106], 564 patients were pooled for PIK3CA analysis. It was observed that patients harbouring wtPIK3CA were significantly associated with better pCRoutcomes compared to patients with mtPIK3CA gene (OR: 2.44; 95% CI 1.42–4.19; p=0.001; Fig. 7).
The overall summary results of pooled pCR outcome of NAC-treated Asian breast cancer patients of this study can be found in Table 1 whereby the favoured outcome for molecular subtypes with various NAC treatments were HER2E, TNBC, and Luminal B. The favoured outcome for biomarkers across different NAC treatments was ER−, PR−, HR− and high ki67. Lastly, the favoured outcome for genetic variation was the PIK3CA wildtype. The overall summary of the steps conducted in completing this systematic review is presented in Table 2.
Pooled reported association
Meta-analyses of pooled reported association of pCR were evaluated according to molecular classification, genetic variations, and biomarkers characterisation of the Asian breast cancer patients.
Molecular classification
An adjusted pooled analysis of TNBC against non-TNBC patients showed that TNBC patients were significantly associated with better response when treated with neoadjuvant chemotherapy (OR 3.02; 95% CI 1.54–5.95; p=0.001; Supplementary Figure 7.2A in Additional file 7). The observed moderate heterogeneity could be due to the study by Lv et al. [69] that did not specifically study TNBC vs non-TNBC patients. Moreover, the recruited patients were either treated with anthracycline-based or TP or TA regimens. Meanwhile, Wu et al. [91] specifically recruited TNBC and non-TNBC patients, and all were treated with TA. Hence, Wu et al.’s result carried more weight than that of Lv et al. in this analysis. However, Lv et al. compensated for these differences by adjusting their multivariate analysis with molecular subtypes. Overall, this result should be taken with caution.
Genetic variations
Amongst pooled reported associations of pCR for genetic variations, our study evaluated the effect of PIK3CA and TP53 genes in NAC-treated Asian BC patients. Notably, no specific or single variant vs wildtype was addressed for both genes as well. In the adjusted analysis of three [51, 100, 106] and two studies [51, 100] for PIK3CA and TP53 genes, respectively, breast cancer patients harbouring mutation in the PIK3CA gene was associated with worse response (OR 0.64; 95% CI 0.42-0.98; p=0.04; Supplementary Figure 7.2B in Additional file 7) while TP53 gene was not associated with pCR outcome (OR 1.34; 95% CI 0.59–3.05; p=0.49; Supplementary Figure 7.2B in Additional file 7).
Biomarkers
Amongst pooled reported associations of pCR for biomarkers, our study evaluated the effect of Tau, nm23-H1, ER, PR, HR, HER2, and Ki-67 biomarkers in NAC-treated Asian BC patients (Supplementary Figures 7.2–7.8 in Additional file 7). In an adjusted analysis of Tau pooling two studies [61, 83], the result suggests that Tau+ was associated with worse response in the neoadjuvant setting (OR 0.22, 95% CI 0.09–0.54, p=0.0008; Supplementary Figure 7.2C in Additional file 7). Meanwhile in adjusted analysis of nm23-H1 pooling two studies [12, 60], nm23-H1 was not associated with pCR outcome in TA-treated patients (OR 1.56, 95% CI 0.55–4.45, p=0.41; Supplementary Figure 7.2C in Additional file 7).
The association between pCR in NAC-treated breast cancer patients and ER was evaluated in Supplementary Figure 7.3 (Additional file 7). In the crude analysis of ER+ vs ER− pooling five studies [61, 94, 97, 112, 115], ER was not associated with pCR outcome (OR 0.39; 95% CI 0.13–1.15; p=0.09). The reported moderate heterogeneity between the studies was perhaps due to the difference in favoured outcomes in one study [112] compared to the rest. Moreover, the heterogeneity is attributable to the different NAC treatments received in each study, whereby the patients were either treated with TP or anthracycline-containing regimens. Therefore, subgroup analyses of ER− vs ER+ pooling studies with patients treated with anthracycline-containing chemotherapy [61, 112] and taxane-platinum chemotherapy [94, 97, 115] were conducted. Our analysis revealed that ER was not associated with pCR outcome when patients were treated with an anthracycline-containing agent (OR 1.19; 95% CI 0.07–19.28; p=0.90) with considerable heterogeneity observed between the studies. The heterogeneity is perhaps due to differences in the favoured outcome in each study caused by the addition of the taxane regimen with the anthracycline in Li et al. [61]. Contrarily, ER+ patients were significantly associated with worse response when treated with TP (OR 0.19; 95% CI 0.11–0.32; p<0.00001).
Meanwhile, adjusted analysis of ER+ vs ER− pooling fourteen studies [54, 56, 61, 68, 71, 72, 83, 94, 97, 102, 103, 106, 112, 131] also showed that ER was not associated with pCR outcome (OR 0.59; 95% CI 0.32–1.08; p=0.09; Supplementary Figure 7.3 in Additional file 7). The observed substantial heterogeneity between the studies was perhaps due to differences in the chemotherapeutic agents received in each study. Subgroup analysis pooling five studies [56, 72, 83, 106, 131] with patients treated in the neoadjuvant setting revealed that ER was not associated with pCR outcome (OR 0.47; 95% CI 0.19–1.14; p=0.09) with considerable heterogeneity reported between the studies probably due to clinical variances between the studies. Another two subgroup analyses pooling studies with patients treated with TP [94, 97] and TA [54, 61, 71] regimens indicate that ER+ was significantly associated with worse response (OR 0.21; 95% CI 0.06–0.70; p=0.01 and OR 0.34; 95% CI 0.19–0.61; p=0.0003, respectively). While subgroup analysis pooling studies with patients treated with anthracycline-based chemotherapy [102, 112] showed that ER was not associated with pCR response (OR 4.29; 95% CI 0.67–27.39; p=0.12). Substantial heterogeneity was reported probably due to the difference in effect size between the studies attributed to the study sample size, whereby Zhao et al. [112] recruited 98 locally advanced breast cancer patients while Yao et al. [102] recruited 538 breast cancer patients.
Meanwhile, analyses pooling studies based on the characteristics of the patients showed that ER was not associated with pCR in patients achieving a complete pathological response in the breast only (OR 0.93; 95% CI 0.18–4.85; p=0.94; Supplementary Figure 7.3 in Additional file 7). The observed heterogeneity between the studies is probably due to the smaller number of studies pooled (n=2) and each study favoured a different outcome. Notably, ER− patients were significantly associated with pCR in studies pooling anthracycline-treated patients (OR 2.78; 95% CI 1.61–4.78; p=0.0002; Supplementary Figure 7.3 in Additional file 7).
The role of the biomarker PR was assessed in Asian breast cancer patients subjected to neoadjuvant chemotherapy (Supplementary Figure 7.4 in Additional file 7). In an analysis with crude OR results pooling five studies [61, 94, 97, 112, 115], it was observed that patients with PR+ were significantly associated with worse response (OR 0.40; 95% CI 0.20–0.79; p=0.009). The observed substantial heterogeneity between the studies was perhaps due to the difference in the favoured outcome in one study [112] and differences in weightage and population size. Subgroup analysis pooling studies with TP-treated patients [94, 97, 115] revealed PR+ patients were significantly associated with worse response (OR 0.29; 95% CI 0.13–0.62; p=0.001). Although moderate heterogeneity was reported, all the three studies pooled for the subgroup analysis were conducted in the Chinese population with no clinical variances. Thus, the heterogeneity result was rejected. Meanwhile, in subgroup analysis pooling patients treated with anthracycline-containing NAC [61, 112], the biomarker PR was not associated with treatment response (OR 0.66; 95% CI 0.17–2.62; p=0.55).
PR was also not associated with treatment response in the adjusted analysis pooling eight studies [54, 56, 61, 94, 97, 102, 103, 106] (OR 1.01; 95% CI 0.64–1.60; p=0.97; Supplementary Figure 7.4 in Additional file 7). The observed moderate heterogeneity was probably due to differences in population size and differences in treatment given in each study. We then conducted four subgroup analyses focusing on the treatment regimen and found that PR was not associated with treatment response in breast cancer patients treated: (1) in the neoadjuvant setting (OR 1.01; 95% CI 0.47–2.18; p=0.99); (2) with TP (OR 0.94; 95% CI 0.34–2.58; p=0.91); and (3) TA regimens (OR 0.37; 95% CI 0.05–2.94; p=0.35), but PR− was significantly associated with better response in anthracycline-containing treated patients (OR 1.63; 95% CI 1.03–2.57; p=0.04). Meanwhile, in adjusted analysis pooling studies with anthracycline-treated patients [88, 96] revealed that PR was not significantly associated with treatment response (OR 1.43; 95% CI 0.74–2.77; p=0.29).
The association between treatment response and hormone receptors (HR) comprising ER and PR was assessed in Asian breast cancer patients (Supplementary Figure 7.5 in Additional file 7). In an analysis with crude OR pooling four studies [51, 62, 64, 116], it was observed that patients with HR+ were significantly associated with worse treatment response in the neoadjuvant setting (OR 0.47; 95% CI 0.24–0.92; p=0.03). In a subgroup analysis whereby all the recruited patients in the pooled studies [51, 64] were of HER2+, it was observed that HR+ were significantly associated with a worse response (OR 0.40; 95% CI 0.18–0.89; p=0.02). Excluding the aforementioned studies, subgroup analysis pooling two studies [62, 116] revealed that HR was not significantly associated with treatment response in the neoadjuvant setting (OR 1.16; 95% CI 0.22–6.22; p=0.87).
Similarly, analysis with adjusted OR pooling five studies [51, 60, 62, 64, 70] indicated that HR was not significantly associated with treatment response (OR 1.27; 95% CI 0.47–3.45; p=0.64; Supplementary Figure 7.5 in Additional file 7). The observed substantial heterogeneity was perhaps due to the clinical variance in the characteristics of the recruited breast cancer population in each study. Subgroup analysis pooling studies analysing HR+ vs HR− in the neoadjuvant setting [62, 70] showed that HR− were significantly associated with better treatment responses (OR 2.39; 95% CI 1.17–04.87; p=0.02). Meanwhile, subgroup analysis pooling studies with HER2+ patients [51, 64] revealed that HR+/HER2+ breast cancer were significantly associated with worse treatment responses in the neoadjuvant setting (OR 0.43; 95% CI 0.21–0.88; p=0.02).
The association between pCR outcome and HER2 was estimated in Supplementary Figure 7.6 (Additional file 7). In an analysis pooling crude OR of seven studies [61, 62, 77, 94, 97, 112, 115], it was observed that HER2+ breast cancer patients were significantly associated with better treatment response (OR 2.50; 95% CI 1.44–4.35; p=0.001). The moderate heterogeneity reported between the studies was perhaps due to the differences in treatment regimens given to the recruited breast cancer population in each study. Subsequently, two subgroup analyses pooling studies according to the chemotherapy regimens administered to the breast cancer patients revealed that HER2+ patients treated with TP regimen [94, 97, 115] were significantly associated with better response (OR 4.64; 95% CI 2.74–7.86; p<0.00001), while HER2 was not associated with treatment response in patients treated with anthracycline-containing regimen (84,141) (OR 2.08; 95% CI 0.90–4.78; p=0.09).
Similarly, in an analysis pooling adjusted OR of 12 studies [56, 60, 61, 70, 77, 83, 94, 97, 102, 103, 106, 131], it was observed that HER2+ breast cancer patients were significantly associated with better treatment response (OR 2.29; 95% CI 1.56–3.35; p<0.0001; Supplementary Figure 7.6 in Additional file 7). Substantial heterogeneity was reported, perhaps due to the clinical variances in each study, based on the treatment received by the patients and the characteristics of the recruited breast cancer population. Subgroup analysis pooling five studies in the neoadjuvant setting [56, 70, 83, 106, 131] showed patients with HER2+ were significantly associated with better response (OR 2.33; 95% CI 1.31–4.15; p=0.004). Some differences between the studies might explain the observed substantial heterogeneity: (1) two of the studies [56, 83] main objective was to investigate the association of Tau with response to neoadjuvant chemotherapy, while Yuan et al. [106] focused on the association of PIK3CA mutation status with response to neoadjuvant chemotherapy, and Lim et al. [131] and Lv et al. [70] assessed factors affecting neoadjuvant treatment response; (2) Lim et al. [131] was the only study including multi-ethnic cohort of breast cancer patients since it was conducted in Singapore and Malaysia, although one of the ethnicity included in Lim et al. was Chinese. Meanwhile, subgroup analyses pooling two studies of patients treated with TP [94, 97] and two studies of patients treated with anthracycline-containing chemotherapy [102, 103] indicate HER2+ patients were significantly associated with better treatment response (OR 7.07; 95% CI 2.88–17.40; p<0.0001 and OR 2.65; 95% CI 1.66–4.23; p<0.0001, respectively). However, subgroup analysis pooling two studies of patients treated with TA [60, 61] revealed that HER2 was not associated with treatment response (OR 1.08; 95% CI 0.47–2.51; p=0.85).
Notably, HER2 was also not associated with pCR in patients achieving a complete pathological response in the breast only (OR 1.96; 95% CI 0.78–4.89; p=0.15; Supplementary Figure 7.6 in Additional file 7) and in anthracycline-treated patients (OR 1.52; 95% CI 0.97–2.40; p=0.07; Supplementary Figure 7.6 in Additional file 7).
As for Ki-67, an analysis pooling crude OR of eight studies [46, 51, 61, 64, 94, 97, 115, 123] observed that patients with high Ki-67 were significantly associated with better treatment responses (OR 2.63; 95% CI 1.69–4.07; p<0.0001; Supplementary Figure 7.7 in Additional file 7). Subgroup crude analyses pooling studies with TNBC patients [46, 123] and patients treated with TP [94, 97, 115] and TA [46, 61] revealed that patients with high Ki-67 were significantly favoured to achieve better treatment responses (OR 4.42; 95% CI 1.41–13.85; p=0.01, OR 2.13; 95% CI 1.21–3.75; p=0.009, and OR 4.26; 95% CI 1.90–9.54; p=0.0004, respectively). Meanwhile, subgroup crude analysis pooling studies with HER2+ patients [51, 64] showed that Ki-67 was not associated with treatment response (OR 1.55; 95% CI 0.79–3.07; p=0.20).
Similarly, an analysis of adjusted OR pooling seven studies [12, 46, 51, 54, 94, 97, 110] showed that patients with high Ki-67 were significantly associated with better treatment response (OR 2.63; 95% CI 1.56–4.41; p=0.0003; Supplementary Figure 7.7 in Additional file 7). In subgroup adjusted analysis pooling studies with HER2+ patients [51, 110], breast cancer patients with high Ki-67 were significantly associated with better response in the neoadjuvant setting (OR 3.67; 95% CI 1.11–12.12; p=0.03). Congruent with the subgroup crude analysis, a subgroup adjusted analysis of pooled studies with TNBC patients [12, 46] also revealed patients with high Ki-67 were significantly associated with better treatment response (OR 2.16; 95% CI 1.00–4.64; p=0.05). Notably, the analysis was also influenced by the fact that the TNBC patients were treated with the TA regimen. Breast cancer patients with high Ki-67 were also significantly associated with better treatment response when treated with TA regimen (OR 2.24; 95% CI 1.34–3.74; p=0.002). However, in patients treated with NAC TP, Ki-67 was not associated with treatment response (OR 4.63; 95% CI 0.35–61.14; p=0.24).
Three biomarkers—ER, HR, and Ki-67—were evaluated by pooling studies reporting their association using hazards ratio (Supplementary Figure 7.8 in Additional file 7). Our pooled adjusted analysis of two studies [73, 80] showed that ER− patients were significantly associated with better treatment response (HR 2.75; 95% CI 1.25–6.05; p=0.01). Both crude and adjusted analysis of HR− vs HR+ and high vs low Ki-67 in HER2+ patients treated with taxane-containing chemotherapy showed that HR− patients and patients with high Ki-67 were significantly associated with a better response. However, in an adjusted result analysis of high vs low Ki-67 in patients treated with taxane-containing chemotherapy, Ki-67 was not significantly associated with treatment response (HR 1.26; 95% CI 1.26–8.25; p=0.81) with substantial heterogeneity. The significant heterogeneity might be explained by the variation in the taxane-based treatment regimen where Zhang et al. [107] included patients submitted to either single taxane-based regime or taxane-platinum combination, while all patients recruited in Wang et al. [80] and Ding et al. [47] were submitted to taxane-anthracycline and taxane-platinum combination regimens, respectively. Moreover, Zhang et al. and Ding et al. incorporated trastuzumab as part of their neoadjuvant regimen while Wang et al. subjected their patients to trastuzumab in the adjuvant setting.
Publication bias
Publication bias assessment was done using the Jamovi Software (version 2.3) [133] (Supplementary Figures 8.1- 8.13 in Additional file 8). The occurrence of publication bias was observed in two analyses.
First, in the overall analysis evaluating the association of pCR outcome with HER2+ and HER2− breast cancer patients submitted to TA chemotherapy, the regression test indicated funnel plot asymmetry (p=0.03) but not the rank correlation test (p=0.34). File drawer analysis indicated that at least 51 studies would be required to nullify the effect (p<0.001). Hence, there is less chance of publication bias in the analysis. As indicated in Fig. 5, subgroup analysis was not conducted for the overall analysis because although the effect is estimated to favour HER2+ significantly, in some studies the true effect may in fact favour HER2−.
Second, in the overall analysis evaluating the association of treatment response with PR− and PR+ breast cancer patients in the neoadjuvant setting, the rank correlation test indicated funnel plot asymmetry (p=0.03) but not the regression test (p=0.08). File drawer analysis suggested the presence of publication bias in the analysis, which could be explained by the heterogeneity observed between the pooled studies, specifically in the treatment regimens assessed in each study. Thus, four subsequent subgroup analyses—pooling two studies at each treatment regimen the patients were subjected to—were conducted for the overall PR− vs PR+ (adjusted results) analysis (Supplementary Figure 7.4 in Additional file 7).
Discussion
There are many options for breast cancer treatment. Often, this includes surgery, radiotherapy, and systemic therapy comprising chemotherapy with or without targeted therapy. Systemic treatment is commonly decided based on the target biomarkers, ensuring the treatment would be effective. Improvements in systemic therapy and targeted therapies utilising an individual’s diagnosis have improved overall pCR rates in breast cancer patients. Studies reported pCR benefits of 44.4% (n=8/18) in TNBC patients treated with NAC TP than 0% (n=0/9) in Luminal A [69], 8.9% (n=56/632) in ER+ breast cancer patients treated with NAC TA than 19.8% (n=75/378) in ER− patients [36], and 24.7% (n=55/223) in breast cancer patients with wildtype PIK3CA gene treated with NAC TA than 11.7% (n=11/94) in mutated PIK3CA [106]. Preoperative chemotherapy or neoadjuvant chemotherapy is typically the standard of care in treating both operable and inoperable locally advanced breast cancer owing to its advantage for breast conservation surgery and aids in shrinking an inoperable tumour to improve resectability [134]. The success of neoadjuvant chemotherapy associated with treatment response (pCR) could be used as a prognostic value in managing breast cancer since the efficacy of a treatment often translates into a highly favourable overall survival and disease-free progression. Often, the best pCR outcomes were observed with TNBC, moderate for HER2E, and the worst for Luminal [134]. Notably, different breast cancer subtypes have different sensitivities to NAC and frequently, a combination of them is given to be effective.
We systematically evaluated the effect of breast cancer molecular subtypes, biomarkers, and genetic variations on breast cancer treatment in Asian breast cancer patients, focusing on treatment response (pCR) in the neoadjuvant setting. In our study, the common NAC treatments used in the pooled analyses were TA, TP, anthracycline-based, and taxane-based chemotherapies with reported pCR rates of 2.7–64.7%, 7.7–60%, 4.3–35%, and 11.3–57.1%, respectively owing to the molecular subtypes, biomarkers, and genetic variations present in the breast cancer patients. There were limited studies focused on breast cancer treatment in Asian breast cancer patients utilising the molecular subtypes classification of breast cancer clinically. In particular, most studies reported the association between breast cancer treatment response with biomarkers and/or genetic variations. From our study, the most frequent subtypes in the Asian population are TNBC and HER2E, followed by luminal B and luminal A. This trend was not consistent with previous studies on the Asian population conducted on 560 Malaysian breast cancer tumours [24] and 2791 Chinese women with breast cancer [76]. Notably, the subtype frequencies in our study might not reflect the entirety of the Asian population. Most of the studies included in this paper were mainly from the Chinese population and fewer of the others (Korean, Japanese, Malaysian, and Indian). Moreover, not all the studies included focused on all four subtypes. Some studies have a different definition of a luminal A, luminal B, and luminal-like subtype when using IHC as a surrogate to classify breast cancer since it is readily available and cost-effective than gene panels.
Our findings suggest Asian TNBC patients subjected to TA and TP in the neoadjuvant setting were observed to favour better response. In particular, although TNBC subtypes were reported to be more likely to benefit from NAC treatment compared to non-TNBC, it is significantly associated through statistical analysis with better response when treated with NAC TP than TA in our study. These findings are consistent with meta-analysis conducted in the general population by Pandy et al. [135] pooling 2415 breast cancer patients treated with NAC TA and TP, which revealed that there was an improvement in the pCR rates in TP-treated patients (44.6%) compared to TA-treated patients (27.8%). TNBC has a poor prognosis and is a more aggressive subtype, with a higher recurrence rate and metastasis (138). Due to the lack of receptor expression, it is not responsive to hormonal therapy [136]. While pCR was observed to be higher in TNBC, which often translates to a desirable long-term outcome [75], some studies have observed the opposite effect whereby there was no difference in survival in patients that have achieved pCR [137, 138]. Similarly, our study showed that HER2E patients were more likely to achieve pCR benefit from NAC TP (52.4%) than TA treatment (27.8%). HER2E is an aggressive subtype with a poor prognosis [139]. However, it can be sensitive to cytotoxic chemotherapy and slightly resistant to hormonal therapy and has shown some positive outcomes with targeted therapy [139,140,141].
Our study revealed that patients with luminal A subtype were less likely to benefit from TA (7.7%) and TP (4.3%) regimens in the neoadjuvant setting. Meanwhile, luminal B has a slightly better pCR rate when treated with TP (28.1%) and TA (12%) and similarly, luminal-like treated with TP (32.5%) and TA (9%). Despite poor responses to NAC, luminal A has a good prognosis [142] with a significantly lower relapse rate than other subtypes, and usually responds well to hormonal therapy [141, 142]. Luminal B has a slightly worse prognosis than luminal A, with an increased chance of recurrence rate, decreased survival rate after relapse, and less sensitivity to hormonal therapy [141, 143]. Notably, the distinct characteristics of each subtype make it challenging to find a treatment that would be effective for all of them. Thus, a combination of chemotherapy, targeted therapy, and endocrine therapy is frequently utilised. Taken together, our study showed that each subtype responds differently to different single or combination of chemotherapeutic agents in the neoadjuvant setting.
Our study’s evaluation of the effect of biomarkers on the pCR outcome suggested the commonly reported biomarkers ER, PR, HER2, and Ki-67 as predictors of the likelihood of better pCR outcomes in breast cancer patients. In particular, patients with negative expression of ER and PR, positive expression of HER2, and higher expression of Ki-67 are significantly associated with better pCR outcomes when treated with either TA or TP chemotherapeutic regimens in the neoadjuvant setting. Patients with negative expression of PR and HER2 are also significantly associated with better pCR outcomes when treated with an anthracycline agent, while patients with HR-negative (ER− and PR−) are significantly associated with better pCR outcomes when treated with taxane. In contrast, although Łukasiewicz et al. supported the expression of ER, PR, HER2, and Ki-67 as predictive and potential prognostic factors, the updated review on breast cancer specified that patients with higher expression of these biomarkers are those who are usually present significantly better clinical outcomes [144]. Unfortunately, Łukasiewicz et al. did not review the predictive or prognostic value of the biomarkers concerning specific chemotherapeutic regimens.
The proper Ki-67 cut-off value in positive hormone receptors (HR+) breast cancer was often discussed due to its importance in evaluating the aggressiveness of the cancer and to distinguish between luminal A and luminal B (HER2−) subtypes when IHC is used as a surrogate classification since both subtypes are of ER+ and HER2− [5, 144]. Furthermore, experts at the St Gallen Consensus Meeting have changed the threshold for Ki-67 over time, from 14% in 2011 to 20% in 2013 [5]. Without the establishment of an optimal Ki-67 cut-off value, it has become challenging to discern what constitutes truly a high or low proliferation of Ki-67 in some studies which led to low reproducibility for the Ki-67 marker. In resolving this issue, the International Ki67 in Breast Cancer Working Group (IKWG) agrees that without improvements in the standardisation of the Ki-67 cut-off value, routine, non-trial settings can reliably categorise very low Ki-67 as ≤5% and very high as ≥30% [145]. Notably, our study congruently suggested that high Ki-67 is significantly associated with better treatment response only at 14 and 20% cut-off values.
Our meta-analysis findings also suggested other biomarkers such as nm23-H1 and CK5/6 as predictors in TA-treated Asian breast cancer patients and Tau in NAC-treated patients. These other biomarkers can be further evaluated and utilised as potential targets in treating breast cancer due to their involvement in the cell signalling pathway and cell division [12, 60]. Tau protein behaves as a microtubule-association protein, which can be found in normal breast epithelial and cancer cells [61]. The expression of Tau protein was found higher in metastatic breast cancer and is often associated with better prognosis and better response to taxanes [61, 146]. Interestingly, our findings suggest the opposite effect where Tau- breast cancer was favoured to have a better response when treated with taxane-containing chemotherapy. However, this could be due to the clinical variance in the study pooled in our analysis. In particular, breast cancer patients in Li et al. [61] were treated with combination TA regimens, while patients in Wang et al. [83] were treated with TP regimens. Furthermore, both studies excluded metastatic breast cancer patients from their study. Meanwhile, CK5/6—often used to define basal-like TNBC—is an intermediate filament protein that provides structure to the cell and is also associated with poor prognosis [90]. CK5/6 and EGFR expression were accepted as biomarkers for classification of Basal-like breast cancer within the TNBC subtype [90].
There were several genes included for analysis in this study. Our meta-analysis results suggested the PIK3CA gene as a predictor for pCR in TA-treated breast cancer patients with PIK3CA mt (17.1%) and PIK3CAwt (24.7%) [106]. Similarly, patients harbouring mutated PIK3CA gene in the Caucasian population who received either trastuzumab, lapatinib, or the combination in addition to a taxane-based chemotherapy are associated with a lower pCR rate [147]. PIK3CA mutations are commonly found in the luminal subtypes, involving signalling pathways to attain a multi-lineage potential, leading to resistance to endocrine therapy [148]. The current treatment recently approved by the US FDA for breast cancer with PIK3CA mutation includes an oral medication Alpelisib acting as PI3K Alpha-Selective Inhibitor. This works as an inhibitor on the common mutation site and induces p110α degradation. This type of PIK3 inhibitor showed more tolerable effects in patients. However, substantial toxicities are still present [149, 150].
Although our study did not reveal a significant association between pCR and the TP53 gene, TP53 is one of the frequently mutated genes in breast cancer and has an involvement in gene transcription that curates cell cycle processes, apoptosis, and DNA repair [151]. TP53 mutations are correlated with HER2+, HR−, and high Ki-67 and contribute to the aggressive characteristics of cancer, leading to treatment resistance [152]. Therefore, it is often associated with a poor prognosis. The molecular profile involving gene expression has been associated with breast cancer recurrence. While the molecular profiling of advanced breast cancer is crucial, it can also be very costly. There is a complex interplay between the genes and the signal pathways which subsequently affect the pCR outcome that needs to be further understood.
In this study, we have explored the role of molecular subtypes, biomarkers, and genetic variations on treatment outcome. It was evident that the treatment given to patients based on their breast cancer characterisation in the neoadjuvant settings has yielded variable pCR outcome. The combination of classifying the patient’s molecular subtypes and identifying the status of their biomarkers can effectively predict the treatment outcome. Apart from use of the routine biomarkers (ER, PR, and HER2), further classification and diagnosis can be done utilising several of the non-conventional biomarkers (Tau, CK5/6, EGFR, Topo-II) and genes (TP53 and PIK3CA) especially in the Asian population in hopes to achieve better individualised treatment through PPM. Thus, there is a need for high-quality validated biomarkers that can predict treatment responses.
Limitations
Despite the efforts during the development and completion of this study, some limitations need to be addressed. First, our study is inclusive of different analytical study designs such as observational (case-control and cohort study) and experimental (randomised controlled trials and non-randomised controlled trials) which might be prone to bias and heterogeneity when they are pooled for analysis. Second, the number of individual studies pooled for each of the analyses was mostly small, both in the overall and subgroup analyses. Third, for a considerable number of studies, there was a need to (1) indirectly categorised their molecular subtypes based on IHC which may not be entirely correct since we are only utilising the data available in the article, and (2) indirectly calculate the 95% CI value in RevMan which may deviate from the original value. Lastly, our tests for publication bias should be considered carefully as the number and size of studies included were limited. Notwithstanding the first limitation of this study, the inclusion of several different analytical study designs allowed us to increase the number of individual studies gathered for the identification of genetic determinants of treatment outcome in breast cancer patients submitted to neoadjuvant chemotherapy. Moreover, we have accounted for heterogeneity using best practices that are consistent with those employed by The Cochrane Collaboration [153]. Nonetheless, future studies should be focused on each of the breast cancer characterisations to validate our findings. In particular, future studies focusing on investigating the effect of specific variant of a gene—utilising the homozygous and heterozygous nature of the variant—against their wildtype on treatment outcome in Asian breast cancer patients will justify the importance and benefits of PPM.
Conclusions
To the best of our knowledge, this SLR is the only comprehensive review currently available that analyses the effect of molecular subtype classification, biomarkers, and genetic variations on the pCR outcome of breast cancer patients in the neoadjuvant setting focusing on the Asian population. The SLR search spanned 20 years and identified over 6000 records which was further reduced to 3725 records after the exclusion of non-Asian breast cancer patients, suggesting that although this area is still understudied, there is a growing interest to pursue the research area. Notably, this SLR adhered to best practices and followed PRISMA reporting guidelines. Our findings justified that molecular subtype (HER2E and TNBC), biomarkers (ER, PR, HER2, HR, Ki-67, nm23-H1, CK5/6, and Tau), and gene (PIK3CA) could be further explored for their possible role in first-line treatment response in Asian breast cancer clinical studies. Understanding the effect of these determinants might be a crucial step to tailor treatment to each patient, which can avoid overtreatment of the tumour with non-aggressive nature and undertreatment of the tumour with aggressive nature. Thus, with further validation, this information can be utilised to treat breast cancer more efficiently in the Asian population.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- CI:
-
Confidence interval
- EGFR:
-
Epidermal growth factor receptor
- ER:
-
Oestrogen receptor
- HER2:
-
Human epidermal growth factor receptor-2
- HER2E:
-
Human epidermal growth factor receptor-2 enriched
- HR:
-
Hazards ratio
- IHC:
-
Immunohistochemistry
- NAC:
-
Neoadjuvant chemotherapy
- OR:
-
Odds ratio
- pCR:
-
Pathological complete response
- PR:
-
Progesterone receptor
- TA:
-
Taxane-anthracycline
- TNBC:
-
Triple-negative breast cancer
- TP:
-
Taxane-platinum
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. Am Cancer Soc Journals. 2021;71(3):209–49.
Harris EER. Precision Medicine for Breast Cancer: The Paths to Truly Individualized Diagnosis and Treatment. Toillon R-A, editor. Int J Breast Cancer. 2018;2018(Special Issue):1–8. https://doi.org/10.1155/2018/4809183.
Duffy MJ, Harbeck N, Nap M, Molina R, Nicolini A, Senkus E, et al. Clinical use of biomarkers in breast cancer: Updated guidelines from the European Group on Tumor Markers (EGTM). Eur J Cancer. 2017;75:284–98.
Eliyatkın N, Yalçın E, Zengel B, Aktaş S, Vardar E. Molecular Classification of Breast Carcinoma: From Traditional, Old-Fashioned Way to A New Age, and A New Way. J Breast Heal. 2015;11(2):59–66.
Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thürlimann B, et al. Personalizing the treatment of women with early breast cancer: Highlights of the stgallen international expert consensus on the primary therapy of early breast Cancer 2013. Ann Oncol. 2013;24(9).
Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000;406(6797):747–52.
Sørlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98(19):10869–74. Available from: https://pubmed.ncbi.nlm.nih.gov/11553815.
Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA. 2003;100(14):8418–23. Available from: https://pubmed.ncbi.nlm.nih.gov/12829800.
Henry NL, Hayes DF. Cancer biomarkers. Mol Oncol. 2012;6(2):140–6. Available from: https://pubmed.ncbi.nlm.nih.gov/22356776.
Meehan J, Gray M, Martínez-Pérez C, Kay C, Pang LY, Fraser JA, et al. Precision Medicine and the Role of Biomarkers of Radiotherapy Response in Breast Cancer. Front Oncol. 2020;10:628. Available from: https://pubmed.ncbi.nlm.nih.gov/32391281.
Mueller C, Haymond A, Davis JB, Williams A, Espina V. Protein biomarkers for subtyping breast cancer and implications for future research. Expert Rev Proteomics. 2018;15(2):131–52. Available from: https://pubmed.ncbi.nlm.nih.gov/29271260.
Li XR, Liu M, Zhang YJ, Wang JD, Zheng YQ, Li J, et al. CK5/6, EGFR, Ki-67, cyclin D1, and nm23-H1 protein expressions as predictors of pathological complete response to neoadjuvant chemotherapy in triple-negative breast cancer patients. Med Oncol. 2011;28(SUPPL. 1).
Talseth-Palmer BA, Scott RJ. Genetic variation and its role in malignancy. Int J Biomed Sci. 2011;7(3):158–71. Available from: https://pubmed.ncbi.nlm.nih.gov/23675233.
Liefaard MC, Lips EH, Wesseling J, Hylton NM, Lou B, Mansi T, et al. The Way of the Future: Personalizing Treatment Plans Through Technology. Am Soc Clin Oncol Educ B. 2021;41:12–23. https://doi.org/10.1200/EDBK_320593.
Pinto N, Dolan ME. Clinically relevant genetic variations in drug metabolizing enzymes. Curr Drug Metab. 2011;12(5):487–97. Available from: https://pubmed.ncbi.nlm.nih.gov/21453273.
Garraway LA, Verweij J, Ballman KV. Precision Oncology: An Overview. J Clin Oncol. 2013;31(15):1803–5. https://doi.org/10.1200/JCO.2013.49.4799.
Abrahams E, Ginsburg GS, Silver M. The personalized medicine coalition: Goals and strategies. Am J Pharmacogenomics. 2005;5
Goetz LH, Schork NJ. Personalized medicine: motivation, challenges, and progress. Fertil Steril. 2018;109(6):952–63. Available from: https://pubmed.ncbi.nlm.nih.gov/29935653.
Liu H, Lv L, Gao H, Cheng M. Pathologic Complete Response and Its Impact on Breast Cancer Recurrence and Patient’s Survival after Neoadjuvant Therapy: A Comprehensive Meta-Analysis. Huang T, editor. Comput Math Methods Med. 2021;2021:7545091. https://doi.org/10.1155/2021/7545091.
André F, Bachelot T, Commo F, Campone M, Arnedos M, Dieras V, et al. Comparative genomic hybridisation array and DNA sequencing to direct treatment of metastatic breast cancer: A multicentre, prospective trial (SAFIR01/UNICANCER). Lancet Oncol. 2014;15(3):267–74.
Howlader N, Cronin KA, Kurian AW, Andridge R. Differences in breast cancer survival by molecular subtypes in the United States. Cancer Epidemiol Biomarkers Prev. 2018;27(6).
Gianni L, Eiermann W, Semiglazov V, Lluch A, Tjulandin S, Zambetti M, et al. Neoadjuvant and adjuvant trastuzumab in patients with HER2-positive locally advanced breast cancer (NOAH): follow-up of a randomised controlled superiority trial with a parallel HER2-negative cohort. Lancet Oncol. 2014;15(6):640–7. https://doi.org/10.1016/S1470-2045(14)70080-4.
McCarthy N, Boyle F, Zdenkowski N, Bull J, Leong E, Simpson A, et al. Neoadjuvant chemotherapy with sequential anthracycline–docetaxel with gemcitabine for large operable or locally advanced breast cancer: ANZ 0502 (NeoGem). Breast. 2014;23(2):142–51. https://doi.org/10.1016/j.breast.2013.12.001.
Pan J-W, Zabidi MMA, Ng P-S, Meng M-Y, Hasan SN, Sandey B, et al. The molecular landscape of Asian breast cancers reveals clinically relevant population-specific differences. Nat Commun. 2020;11(1):6433. https://doi.org/10.1038/s41467-020-20173-5.
Leong SPL, Shen Z-Z, Liu T-J, Agarwal G, Tajima T, Paik N-S, et al. Is Breast Cancer the Same Disease in Asian and Western Countries? World J Surg. 2010;34(10):2308–24. https://doi.org/10.1007/s00268-010-0683-1.
Yap Y-S, Lu Y-S, Tamura K, Lee JE, Ko EY, Park YH, et al. Insights Into Breast Cancer in the East vs the West: A Review. JAMA Oncol. 2019;5(10):1489–96. https://doi.org/10.1001/jamaoncol.2019.0620.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. Available from: http://www.bmj.com/content/372/bmj.n71.abstract.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan — a web and mobile app for systematic reviews. Systematic Reviews. 2006;
Wells GA, Wells G, Shea B, Shea B, O’Connell D, Peterson J, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. In 2014.
Review Manager (RevMan). The Cochrane Collaboration; 2020.
Greenland S. Generalized Mantel-Haenszel Estimators for K 2 x J Tables. Biometrics. 1989;45(1):183–91. Available from: http://www.jstor.org/stable/2532044.
DerSimonian R, Laird N. Meta-Analysis in Clinical Trials. Control Clin Trials. 1986;7:177–88.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses Testing for heterogeneity; 2003.
Bi Z, Chen P, Liu YB, Zhao T, Sun X, Song XR, et al. Efficacy and safety analysis of paclitaxel, docetaxel and liposomal paclitaxel after neoadjuvant therapy in breast cancer. Breast Cancer Res Treat. 2020;184(2):397–405.
Bi Z, Liu J, Chen P, Liu Y, Zhao T, Wang C, et al. Neoadjuvant chemotherapy and timing of sentinel lymph node biopsy in different molecular subtypes of breast cancer with clinically negative axilla. Breast Cancer. 2019;26(3):373–7.
Chen R, Ye Y, Yang C, Peng Y, Zong B, Qu F, et al. Assessment of the predictive role of pretreatment Ki-67 and Ki-67 changes in breast cancer patients receiving neoadjuvant chemotherapy according to the molecular classification: a retrospective study of 1010 patients. Breast Cancer Res Treat. 2018;170(1):35–43.
Chen S, Huang L, Chen C-M, Shao Z-M. Progesterone receptor loss identifies luminal-type local advanced breast cancer with poor survival in patients who fail to achieve a pathological complete response to neoadjuvant chemotherapy. Oncotarget. 2015;6(20):18174–82.
Chen S, Huang L, Liu Y, Chen CM, Wu J, Shao ZM. The predictive and prognostic significance of pre- and post-treatment topoisomerase IIα in anthracycline-based neoadjuvant chemotherapy for local advanced breast cancer. Eur J Surg Oncol. 2013;39(6):619–26.
Chen W, He J, Song S, Wang M, Wu H, Wang X. Efficacy of TCH/TEC neoadjuvant chemotherapy for the treatment of HER-2-Overexpressing breast cancer. Oncol Lett. 2015;9(4):1922–6.
Chen X, Ye G, Zhang C, Li X, Shen K. Non-anthracycline-containing docetaxel and cyclophosphamide regimen is associated with sustained worse outcome compared with docetaxel, anthracycline and cyclophosphamide in neoadjuvant treatment of triple negative and HER2-positive breast cancer patients. Chin J Cancer Res. 2016;28(6):561–9.
Chen XS, Nie XQ, Chen CM, Wu JY, Wu J, Lu JS, et al. Weekly paclitaxel plus carboplatin is an effective nonanthracycline-containing regimen as neoadjuvant chemotherapy for breast cancer. Ann Oncol. 2010;21(5):961–7.
Chen XS, Wu JY, Huang O, Chen CM, Wu J, Lu JS, et al. Molecular subtype can predict the response and outcome of Chinese locally advanced breast cancer patients treated with preoperative therapy. Oncol Rep. 2010;23(5).
Chen YZ, Xue JY, Chen CM, Yang BL, Xu QH, Wu F, et al. PPAR signaling pathway may be an important predictor of breast cancer response to neoadjuvant chemotherapy. Cancer ChemotherPharmacol. 2012;70(5):637–44.
Chow LWC, Morita S, Chow CYC, Ng WK, Toi M. Neoadjuvant palbociclib on ER+ breast cancer (N007): Clinical response and EndoPredict’s value. EndocrRelat Cancer. 2018;25(2):123–30.
Da YK, Wu SY, Liu GY, Wu J, Di GH, Hu Z, et al. Concurrent neoadjuvant chemotherapy and estrogen deprivation in patients with estrogen receptor–positive, human epidermal growth factor receptor 2–negative breast cancer (CBCSG-036): A randomized, controlled, multicenter trial. Cancer. 2019;125(13):2185–93.
Di KD, Fu RZ, Li L, Wang W, Wang SB. Association between the methylation status of PCDH17 and the efficacy of neoadjuvant chemotherapy in triple-negative breast cancer. Oncol Lett. 2020;20(2):1649–56.
Ding J, Yang Y, Jiang L, Wu W, Shao Z. Predictive factors of pathologic complete response in HER2-positive and axillary lymph node positive breast cancer after neoadjuvant paclitaxel, carboplatin plus with trastuzumab Gao Y, Hu YJ, Yang HJ, et al. Low expression of stathmin in tumor predicts high response to neoadjuvant chemotherapy with docetaxel-containing regimens in locally advanced breast cancer. Genet Test Mol Biomarkers. 2012;16(7):689–94.
Fei F, Chen C, Xue J, Di GH, Lu JS, Liu GY, et al. Efficacy and safety of docetaxel combined with oxaliplatin as a neoadjuvant chemotherapy regimen for Chinese triple-negative local advanced breast cancer patients : A prospective, open, and unicentric phase II clinical trial. Am J Clin Oncol Cancer Clin Trials. 2013;36(6):545–51.
Gu X, Zhang Y, Chen L, Guo J, Zhang WH. Efficacy of neo-adjuvant chemotherapy with TEC regimen on breast cancer. Cancer ChemotherPharmacol. 2015;75(2):301–8.
Hong J, Wu J, Huang O, He J, Zhu L, Chen W, et al. Early response and pathological complete remission in Breast Cancer with different molecular subtypes: A retrospective single center analysis. J Cancer. 2020;11(23):6916–24.
Huang L, Chen S, Yang W, Xu B, Huang T, Yang H, et al. Efficacy and safety analysis of trastuzumab and paclitaxel based regimen plus carboplatin or epirubicin as neoadjuvant therapy for clinical stage II-III, HER2-positive breast cancer patients: a phase 2, open-label, multicenter, randomized trial. Oncotarget. 2015;6 Available from: www.impactjournals.com/oncotarget/.
Huang L, Chen S, Yao L, Liu G, Wu J, Shao Z. Phase II trial of weekly nab-paclitaxel and carboplatin treatment with or without trastuzumab as nonanthracycline neoadjuvant chemotherapy for locally advanced breast cancer. Int J Nanomedicine. 2015;10:1969–75.
Huang O, Chen CM, Wu JY, Chen SJ, Chen XS, Liu GY, et al. Retrospective analysis of 119 Chinese noninflammatory locally advanced breast cancer cases treated with intravenous combination of vinorelbine and epirubicin as a neoadjuvant chemotherapy: A median follow-up of 63.4 months. BMC Cancer. 2009;9:375.
Kong D, Wang M-H, Yang J, Li L. Association of T-cadherin levels with the response to neoadjuvant chemotherapy in locally advanced breast cancer. Oncotarget. 2017;8:13747–53. Available from: www.impactjournals.com/oncotarget/.
Kong Y, Dong Q, Ji H, Sang M, Ding Y, Zhao M, et al. The effect of the Leptin and leptin receptor expression on the efficacy of neoadjuvant chemotherapy in breast cancer. Med Sci Monit. 2019;25:3005–13.
Lei C, Yang C, Xia B, Ji F, Zhang Y, Gao H, et al. Analysis of Tau protein expression in predicting pathological complete response to neoadjuvant chemotherapy in different molecular subtypes of breast cancer. J Breast Cancer. 2020;23(1):47–58.
Li K, Liao N, Chen B, Zhang G, Wang Y, Guo L, et al. Genetic mutation profile of Chinese HER2-positive breast cancers and genetic predictors of responses to Neoadjuvant anti-HER2 therapy. Breast Cancer Res Treat. 2020;183(2):321–32.
Li M, Zhang J, Ouyang T, Li J, Wang T, Fan Z, et al. Incidence of BRCA1 somatic mutations and response to neoadjuvant chemotherapy in Chinese women with triple-negative breast cancer. Gene. 2016;584(1):26–30.
Li S, Wei W, Jiang Y, Li Q, Huang Q, Yang H, et al. Comparison of the efficacy and survival analysis of neoadjuvant chemotherapy for Her-2-positive breast cancer. Drug Des Devel Ther. 2018;12:3085–93.
Li XR, Liu M, Zhang YJ, Wang JD, Zheng YQ, Li J, et al. ER, PgR, HER-2, Ki-67, topoisomerase IIα, and nm23-H1 proteins expression as predictors of pathological complete response to neoadjuvant chemotherapy for locally advanced breast cancer. Med Oncol. 2011;28(SUPPL. 1).
Li Z, Xiong Q, Tu J, Gong Y, Qiu W, Zhang H, et al. Tau proteins expressions in advanced breast cancer and its significance in taxane-containing neoadjuvant chemotherapy. Med Oncol. 2013;30(3):591. https://doi.org/10.1007/s12032-013-0591-y.
Liu F, Li Y, Ren M, Zhang X, Guo X, Lang R, et al. Peritumoral FOXP3+ regulatory T cell is sensitive to chemotherapy while intratumoral FOXP3+ regulatory T cell is prognostic predictor of breast cancer patients. Breast Cancer Res Treat. 2012;135(2):459–67.
Liu J, Wang S, Wang C, Kong X, Sun P. Prognostic value of using glucosylceramide synthase and cytochrome P450 family 1 subfamily A1 expression levels for patients with triple-negative breast cancer following neoadjuvant chemotherapy. Exp Ther Med. 2021;21(3).
Liu S, Duan X, Xu L, Ye J, Cheng Y, Liu Q, et al. Nuclear Gli1 expression is associated with pathological complete response and event-free survival in HER2-positive breast cancer treated with trastuzumab-based neoadjuvant therapy. Tumour Biol. 2016;37(4):4873–81.
Liu Y, Xu Z, Zhang Z, Wen G, Sun J, Han F. Efficacy and safety of TE/TEC/intensive paclitaxel neoadjuvant chemotherapy for the treatment of breast cancer. Oncol Lett. 2019;17(1):907–12.
Liu YX, Zhang KJ, Tang LL. Clinical significance of androgen receptor expression in triple negative breast cancer-an immunohistochemistry study. Oncol Lett. 2018;15(6):10008–16.
Luo J, Zhou Z, Yang Z, Chen X, Cheng J, Shao Z, et al. The Value of 18F-FDG PET/CT imaging combined with pretherapeutic ki67 for early prediction of pathologic response after neoadjuvant chemotherapy in locally advanced breast cancer. Med (United States). 2016;95(8).
Lv M, Guo H, Wang C, Tian P, Ma Y, Chen X, et al. Neoadjuvant docetaxel with or without carboplatin plus dual HER2 blockade for HER2-positive breast cancer: a retrospective multicenter Chinese study. Gland Surg. 2020;9(6):2079–90.
Lv M, Li B, Li Y, Mao X, Yao F, Jin F. Predictive Role of Molecular Subtypes in Response to Neoadjuvant Chemotherapy in Breast Cancer Patients in Northeast China. Asian Pac J Cancer Prev. 2011;12:2411–7.
Lv Y, Li Y, Mu W, Fu H. Factors Affecting Pathological Complete Response After Neoadjuvant Chemotherapy in Operable Primary Breast Cancer. J Coll Physicians Surg Pak. 2020;30(4):389–93.
Mou P, Wang HJ, An L, Yin Q, Chang J. RS7435335 located in the UGT2B7 gene may be a possible genetic marker for the clinical response and prognosis of breast cancer patients receiving neoadjuvant chemotherapy. J Cell Biochem. 2019;120(5):7167–73.
Nie C, Lv H, Bie L, Hou H, Chen X. Hypoxia-inducible factor 1-alpha expression correlates with response to neoadjuvant chemotherapy in women with breast cancer. Med (United States). 2018;97(51).
Shan BJ, Shen XB, Jin W, Dong MH, Han XH, Lin L, et al. Standard-doseepirubicin increases the pathological complete response rate in neoadjuvant chemotherapy for breast cancer: A multicenter retrospective study. Gland Surg. 2020;9(4):1026–35.
Shao Z, Pang D, Yang H, Li W, Wang S, Cui S, et al. Efficacy, Safety, and Tolerability of Pertuzumab, Trastuzumab, and Docetaxel for Patients with Early or Locally Advanced ERBB2-Positive Breast Cancer in Asia: The PEONY Phase 3 Randomized Clinical Trial. JAMA Oncol. 2020;6(3).
Spring LM, Fell G, Arfe A, Sharma C, Greenup R, Reynolds KL, et al. Pathologic Complete Response after Neoadjuvant Chemotherapy and Impact on Breast Cancer Recurrence and Survival: A Comprehensive Meta-analysis. Clin Cancer Res. 2020;26(12):2838–48. Available from: https://pubmed.ncbi.nlm.nih.gov/32046998.
Su Y, Zheng Y, Zheng W, Gu K, Chen Z, Li G, et al. Distinct distribution and prognostic significance of molecular subtypes of breast cancer in Chinese women: a population-based cohort study. BMC Cancer. 2011;11(1):292. https://doi.org/10.1186/1471-2407-11-292.
Tan Q-X, Qin Q-H, Yang W-P, Mo Q-G, Wei C-Y. Prognostic value of Ki67 expression in HR-negative breast cancer before and after neoadjuvant chemotherapy. Int J Clin Exp Pathol. 2014;7:6862–70. Available from: www.ijcep.com/.
Tang Y, Zhu L, Li Y, Ji J, Li J, Yuan F, et al. Overexpression of epithelial growth factor receptor (EGFR) predicts better response to neo-adjuvant chemotherapy in patients with triple-negative breast cancer. J Transl Med. 2012;10(Suppl):1.
Wan F, Dong L, Zhang F, Wang Y, Chen F, Ni S, et al. Clinical study of the relationship between γ-synuclein and the response of neoadjuvant chemotherapy in breast cancer. J Int Med Res. 2013;41(3):743–53.
Wang J, Di S, Xu B, Yuan P, Ma F, Luo Y, et al. Value of breast cancer molecular subtypes and ki67 expression for the prediction of efficacy and prognosis of neoadjuvant chemotherapy in a Chinese population. Med (United States). 2016;95(18):e3518.
Wang J, Xu B, Yuan P, Li Q, Zhang P, Cai R, et al. HER2 as a predictive factor for successful neoadjuvant anthracycline chemotherapy of locally advanced and early breast cancer. Int J Biol Markers. 2014;29(3):e187–92.
Wang J, Xu B, Yuan P, Zhang P, Li Q, Ma F, et al. TOP2A amplification in breast cancer is a predictive marker of anthracycline-based neoadjuvant chemotherapy efficacy. Breast Cancer Res Treat. 2012;135(2):531–7.
Wang K, Deng QT, Liao N, Zhang GC, Liu YH, Xu FP, et al. Tau expression correlated with breast cancer sensitivity to taxanes-based neoadjuvant chemotherapy. Tumour Biol. 2013;34(1):33–8.
Wang LC, Wang LS, Li AX, Shi ZZ, Li YQ, Huang W, et al. Combinational Treatment of Doxorubicin With Neoadjuvant Docetaxel for Different Subtypes of Patients With Breast Cancer. Technol Cancer Res Treat. 2020;19
Wang X, Cai L, Ye F, Li M, Ma L, Geng C, et al. Elevated expression of MTDH predicts better prognosis of locally advanced HER-2 positive breast cancer patients receiving neoadjuvant chemotherapy plus trastuzumab. Med (United States). 2019;98(36).
Wang Y, Dong T, Xuan Q, Zhao H, Qin L, Zhang Q. Lymphocyte-activation gene-3 expression and prognostic value in neoadjuvant-treated triple-negative breast cancer. J Breast Cancer. 2018;21(2):124–33.
Wang Y, Liu H, Mao F, Jin F, Ma B, Jiang J, et al. Identifying the role of PTPN12 expression in predicting the efficacy of capecitabine to neoadjuvant chemotherapy in breast cancer treatment; 2016. p. 3400–9.
Wang Y, Xu Y, Chen J, Ouyang T, Li J, Wang T, et al. TP53 mutations are associated with higher rates of pathologic complete response to anthracycline/cyclophosphamide-based neoadjuvant chemotherapy in operable primary breast cancer. Int J Cancer. 2016;138(2):489–96.
Wang YJ, Huang XY, Mo M, Li JW, Jia XQ, Shao ZM, et al. Serum tumor marker levels might have little significance in evaluating neoadjuvant treatment response in locally advanced breast cancer. Asian Pac J Cancer Prev. 2015;16(11):4603–8.
Wang Z, Liu L, Li Y, Song Z, Jing Y, Fan Z, et al. Analysis of CK5/6 and EGFR and Its Effect on Prognosis of Triple Negative Breast Cancer. Front. Oncol. 2021:10.
Wu J, Li S, Jia W, Su F. Response and prognosis of taxanes and anthracyclines neoadjuvant chemotherapy in patients with triple-negative breast cancer. J Cancer Res Clin Oncol. 2011;137(10):1505–10.
Wu X, Tang P, Li S, Wang S, Liang Y, Zhong L, et al. A randomized and open-label phase II trial reports the efficacy of neoadjuvant lobaplatin in breast cancer. Nat Commun. 2018;9(1).
Wu Z, Zhang L, Peng J, Xu S, Zhou L, Lin Y, et al. Predictive and prognostic value of PDL1 protein expression in breast cancer patients in neoadjuvant setting. Cancer Biol Ther. 2019;20(6):941–7.
Wu Z, Zhang L, Xu S, Lin Y, Yin W, Lu J, et al. Predictive and prognostic value of ZEB1 protein expression in breast cancer patients with neoadjuvant chemotherapy. Cancer Cell Int. 2019;19(1).
Xie F, Chen R, Zhang L, Yin Z, Zhu Q, You S, et al. Efficacy of two-weekly nanoparticle albumin-bound paclitaxel as neoadjuvant chemotherapy for breast cancer. Nanomedicine. 2019;14(12):1595–603.
Xu Y, Ouyang T, Li J, Wang T, Fan Z, Fan T, et al. Predictive value of BRCA1/2 mRNA expression for response to neoadjuvant chemotherapy in BRCA-negative breast cancers. Cancer Sci. 2018;109(1):166–73.
Xu Y, Wang Y, Yuan C, Sheng X, Sha R, Dai H, et al. Predictive and prognostic value of EPIC1 in patients with breast cancer receiving neoadjuvant chemotherapy. Ther Adv Med Oncol. 2020;12
Xuhong J, Qi X, Tang P, Fan L, Chen L, Zhang F, et al. Neoadjuvant Pyrotinib plus Trastuzumab and Chemotherapy for Stage I–III HER2-Positive Breast Cancer: A Phase II Clinical Trial. Oncologist. 2020;25(12):e1909–20.
Yan H, Xiao H, Zhu J, Zhang J, Liu Z. Association between the HER2 protein expression level and the efficacy of neoadjuvant chemotherapy in HER2-positive breast cancer. Cancer Manag Res. 2020;12:12715–22.
Yang L, Ye F, Bao L, Zhou X, Wang Z, Hu P, et al. Somatic alterations of TP53, ERBB2, PIK3CA and CCND1 are associated with chemosensitivity for breast cancers. Cancer Sci. 2019;110(4):1389–400.
Yang M, Qu H, Liu A, Liu J, Sun P, Li H. Efficacy and safety of nanoparticle albumin-bound paclitaxel as neoadjuvant chemotherapy in HER2-negative breast cancer. J Cancer Res Ther. 2019;15(7):1561–6.
Yao L, Liu Y, Li Z, Ouyang T, Li J, Wang T, et al. HER2 and response to anthracycline-based neoadjuvant chemotherapy in breast cancer. Ann Oncol. 2011;22(6):1326–31.
Yao L, Zhang J, Liu Y, Ouyang T, Li J, Wang T, et al. Association between HER2 status and response to neoadjuvant anthracycline followed by paclitaxel plus carboplatin chemotherapy without trastuzumab in breast cancer. Chin J Cancer Res. 2015;27(6):553–61.
Yin Y, Zhang P, Xu BH, Zhang BL, Li Q, Yuan P, et al. Unfavorable pathological complete response rate of neoadjuvant chemotherapy epirubicin plus taxanes for locally advanced triple-negative breast cancer. J Huazhong Univ Sci Technol - Med Sci. 2013;33(2):262–5.
Yu K, Liu G, Zhou X, Zhou Y, Wu J, Chen C, et al. Association of HER-2 Copy Number and HER-2/CEP-17 Ratio with Neoadjuvant Taxane-Containing Chemotherapy Sensitivity in Locally Advanced Breast Cancer. Oncologist. 2012;17(6):792–800.
Yuan H, Chen J, Liu Y, Ouyang T, Li J, Wang T, et al. Association of PIK3CA Mutation Status before and after Neoadjuvant Chemotherapy with Response to Chemotherapy in Women with Breast Cancer. Clin Cancer Res. 2015;21(19):4365–72.
Zhang GC, Qian XK, Guo ZB, Ren CY, Yao M, Li XR, et al. Pre-treatment hormonal receptor status and Ki67 index predict pathologic complete response to neoadjuvant trastuzumab/taxanes but not disease-free survival in HER2-positive breast cancer patients. Med Oncol. 2012;29(5):3222–31.
Zhang P, Yin Y, Mo H, Zhang B, Wang X, Li Q, et al. Better pathologic complete response and relapse-free survival after carboplatin plus paclitaxel compared with epirubicin plus paclitaxel as neoadjuvant chemotherapy for locally advanced triple-negative breast cancer: a randomized phase 2 trial . Vol. 7. 2016. Available from: www.impactjournals.com/oncotarget.
Zhang S, Zhang C, Liu J, Qin L, Cui S, Zhang J. A Phase II trial of Zoladex combined with CEF chemotherapy as neoadjuvant therapy in premenopausal women with hormone-responsive, operable breast cancer. Med Oncol. 2012;29(2):479–85.
Zhang W, Tian H, Yang SH. The Efficacy of Neoadjuvant Chemotherapy for HER-2-Positive Locally Advanced Breast Cancer and Survival Analysis. Anal Cell Pathol. 2017;2017
Zhang Z, Zhang W, Jin Y, Wang H, Gu F, Zhou J, et al. Evaluating the response of neoadjuvant chemotherapy for treatment of breast cancer: Are tumor biomarkers and dynamic contrast enhanced MR images useful predictive tools? J Thorac Dis. 2014;6(6):785–94.
Zhao YC, Wang Y, Ni XJ, Li Y, Wang XM, Zhu YY, et al. Clinical significance of Smac and survivin expression in breast cancer patients treated with anthracycline-based neoadjuvant chemotherapy. Mol Med Rep. 2014;9(2):614–20.
Zheng Y, Li S, Boohaker RJ, Liu X, Zhu Y, Zhai L, et al. A microRNA expression signature in taxane-anthracycline-based neoadjuvant chemotherapy response. J Cancer. 2015;6(7):671–7.
Zhou L, Xu S, Yin W, Lin Y, Du Y, Jiang Y, et al. Weekly paclitaxel and cisplatin as neoadjuvant chemotherapy with locally advanced breast cancer: a prospective, single arm, phase II study. Oncotarget. 2017;8:79305–14. Available from: www.impactjournals.com/oncotarget/.
Zhu T, Liu CL, Zhang YF, Liu YH, Xu FP, Zu J, et al. A phase II trial of dose-dense (biweekly) paclitaxel plus carboplatin as neoadjuvant chemotherapy for operable breast cancer. Breast Cancer Res Treat. 2016;156(1):117–24.
Chiu JW, Leung R, Tang V, Cheuk WY, Lo J, Kwok GW, et al. Changing pattern of recurrences in patients with early HER2-positive breast cancer receiving neoadjuvant chemotherapy in the era of dual anti-HER2 therapy. Postgrad Med J. 2019;
Man VCM, Cheung PSY. Neoadjuvant chemotherapy increases rates of breast-conserving surgery in early operable breast cancer. Hong Kong Med J. 2017;23(3):251–7.
Park JH, Kang MJ, Ahn JH, Kim JE, Jung KH, Gong G, et al. Phase II trial of neoadjuvant letrozole and lapatinib in Asian postmenopausal women with estrogen receptor (ER) and human epidermal growth factor receptor 2 (HER2)-positive breast cancer [Neo-ALL-IN]: Highlighting the TILs, ER expressional change after ne. Cancer ChemotherPharmacol. 2016;78(4):685–95.
Hasegawa Y, Tanino H, Horiguchi J, Miura D, Ishikawa T, Hayashi M, et al. Randomized controlled trial of zoledronic acid plus chemotherapy versus chemotherapy alone as neoadjuvant treatment of HER2-negative primary breast cancer (JONIE Study). PLoS One. 2015;10(12).
Ishikawa T, Narui K, Tanabe M, Kida K, Oba MS, Yamada A, et al. BRCAness is beneficial for indicating triple negative breast cancer patients resistant to taxane. Eur J Surg Oncol. 2016;42(7):999–1001.
Sugitani I, Ueda S, Sakurai T, Shigekawa T, Hirokawa E, Shimada H, et al. Neoadjuvant chemotherapy with trastuzumab, docetaxel, and carboplatin administered every 3 weeks for Japanese women with HER2-positive primary breast cancer: efficacy and safety. Int J Clin Oncol. 2017;22(5):880–6.
Teraoka S, Sato E, Narui K, Yamada A, Fujita T, Yamada K, et al. Neoadjuvant Chemotherapy With Anthracycline-Based Regimen for BRCAnessTumors in Triple-Negative Breast Cancer. J Surg Res. 2020;250:143–7.
Mohammed AA, Elsayed FM, Algazar M, Rashed HE, Anter AH. Neoadjuvant Chemotherapy In Triple Negative Breast Cancer: Correlation Between Androgen Receptor Expression And Pathological Response. Asian Pac J Cancer Prev. 2020;21(2):563–8.
Mohammadianpanah M, Ashouri Y, Hoseini S, Amadloo N, Talei A, Tahmasebi S, et al. The efficacy and safety of neoadjuvant chemotherapy +/2 letrozole in postmenopausal women with locally advanced breast cancer: A randomized phase III clinical trial. Breast Cancer Res Treat. 2012;132(3):853–61.
Duman BB, Afşar CU, Günaldi M, Sahin B, Kara IO, Erkisi M, et al. Retrospective analysis of neoadjuvant chemotherapy for breast cancer in Turkish patients. Asian Pac J Cancer Prev. 2012;13(8):4119–23.
Salim DK, Mutlu H, Eryilmaz MK, Musri FY, Tural D, Gunduz S, et al. Molecular types and neoadjuvant chemotherapy in patients with breast cancer - while molecular shifting is more common in luminal a tumors, the pathologic complete response is most frequently observed in Her-2 like tumors. Asian Pac J Cancer Prev. 2014;15(21):9379–83.
Elnemr GM, El-Rashidy AH, Osman AH, Issa LF, Abbas OA, Al-Zahrani AS, et al. Response of triple negative breast cancer to neoadjuvant chemotherapy: Correlation between Ki-67 expression and pathological response. Asian Pac J Cancer Prev. 2016;17(2):807–13.
Elsamany S, Elemam O, Elmorsy S, Alzahrani A, Abbas MM. Predictive value of the pattern of β-catenin expression for pathological response to neoadjuvant chemotherapy in breast cancer patients. Asian Pac J Cancer Prev. 2016;17(8):4091–5.
Elsamany S, Elmorsy S, Alzahrani A, Rasmy A, Abozeed WN, Mohammed AA, et al. Predictive value of IHC4 score for pathological response to neoadjuvant chemotherapy in hormone receptor-positive breast cancer. Asian Pac J Cancer Prev. 2015;16(17):7975–9.
Prajoko YW, Aryandono T. Expression of nuclear factor kappa B (NF-κB) as a predictor of poor pathologic response to chemotherapy in patients with locally advanced breast cancer. Asian Pac J Cancer Prev. 2014;15(2):595–8.
Lim LY, Miao H, Lim JSJ, Lee SC, Bhoo-Pathy N, Yip CH, et al. Outcome after neoadjuvant chemotherapy in Asian breast cancer patients. Cancer Med. 2017;6(1):173–85.
Tewari M, Pradhan S, Singh U, Singh TB, Shukla HS. Assessment of Predictive Markers of Response to Neoadjuvant Chemotherapy in Breast Cancer. Asian Journal of Surgery. 2010;33
The jamovi project. jamovi. 2022. Available from: https://www.jamovi.org.
NCCN Clinical Practice Guidelines in Oncology-Breast Cancer. Available from: https://www.nccn.org/guidelines/recently-published-guidelines.
Pandy JGP, Balolong-Garcia JC, Cruz-Ordinario MVB, Que FVF. Triple negative breast cancer and platinum-based systemic treatment: a meta-analysis and systematic review. BMC Cancer. 2019;19(1):1065. Available from: https://pubmed.ncbi.nlm.nih.gov/31703646.
Yin L, Duan JJ, Bian XW, Yu SC. Triple-negative breast cancer molecular subtyping and treatment progress. Breast Cancer Res. 2020;22
Bianchini G, Balko JM, Mayer IA, Sanders ME, Gianni L. Triple-negative breast cancer: challenges and opportunities of a heterogeneous disease. Nat Rev Clin Oncol. 2016;13(11):674–90. Available from: https://pubmed.ncbi.nlm.nih.gov/27184417.
Fornier M, Fumoleau P. The Paradox of Triple Negative Breast Cancer: Novel Approaches to Treatment. Breast J. 2012;18(1):41–51. https://doi.org/10.1111/j.1524-4741.2011.01175.x.
Godoy-Ortiz A, Sanchez-Muñoz A, Parrado MRC, Álvarez M, Ribelles N, Dominguez AR, et al. Deciphering her2 breast cancer disease: Biological and clinical implications. Front. Oncol. 2019:9(OCT).
Wang J, Xu B. Targeted therapeutic options and future perspectives for her2-positive breast cancer. Signal Transduction and Targeted Therapy. 2019;4
Yersal O, Barutca S. Biological subtypes of breast cancer: Prognostic and therapeutic implications. World Journal of Clinical Oncology. 2014;5
Gao JJ, Swain SM. Luminal A Breast Cancer and Molecular Assays: A Review. Oncologist. 2018;23(5):556–65. Available from: https://pubmed.ncbi.nlm.nih.gov/29472313.
Li ZH, Hu PH, Tu JH, Yu NS. Luminal B breast cancer: Patterns of recurrence and clinical outcome. Oncotarget. 2016;7(40).
Łukasiewicz S, Czeczelewski M, Forma A, Baj J, Sitarz R, Stanisławek A. Breast Cancer-Epidemiology, Risk Factors, Classification, Prognostic Markers, and Current Treatment Strategies-An Updated Review. Cancers (Basel). 2021;13(17):4287. Available from: https://pubmed.ncbi.nlm.nih.gov/34503097.
Nielsen TO, Leung SCY, Rimm DL, Dodson A, Acs B, Badve S, et al. Assessment of Ki67 in Breast Cancer: Updated Recommendations From the International Ki67 in Breast Cancer Working Group. J Natl Cancer Inst. 2021;113(7):808–19. Available from: https://pubmed.ncbi.nlm.nih.gov/33369635.
Darlix A, Hirtz C, Thezenas S, Maceski A, Gabelle A, Lopez-Crapez E, et al. The prognostic value of the Tau protein serum level in metastatic breast cancer patients and its correlation with brain metastases. BMC Cancer. 2019;19(1):110. https://doi.org/10.1186/s12885-019-5287-z.
Loibl S, Majewski I, Guarneri V, Nekljudova V, Holmes E, Bria E, et al. PIK3CA mutations are associated with reduced pathological complete response rates in primary HER2-positive breast cancer: pooled analysis of 967 patients from five prospective trials investigating lapatinib and trastuzumab. Ann Oncol Off J Eur Soc Med Oncol. 2016;27(8):1519–25. Available from: https://pubmed.ncbi.nlm.nih.gov/27177864.
Feng Y, Spezia M, Huang S, Yuan C, Zeng Z, Zhang L, et al. Breast cancer development and progression: Risk factors, cancer stem cells, signaling pathways, genomics, and molecular pathogenesis. Genes Dis. 2018;5(2):77–106. Available from: https://pubmed.ncbi.nlm.nih.gov/30258937.
Chang D-Y, Ma W-L, Lu Y-S. Role of Alpelisib in the Treatment of PIK3CA-Mutated Breast Cancer: Patient Selection and Clinical Perspectives. Ther Clin Risk Manag. 2021;17:193–207. Available from: https://pubmed.ncbi.nlm.nih.gov/33707948.
Cho YA, Ko SY, Suh YJ, Kim S, Park JH, Park H-R, et al. PIK3CA Mutation as Potential Poor Prognostic Marker in Asian Female Breast Cancer Patients Who Received Adjuvant Chemotherapy. Curr Oncol. 2022;29(5):2895–908. Available from: https://www.mdpi.com/1718-7729/29/5/236.
Shahbandi A, Nguyen HD, Jackson JG. TP53 Mutations and Outcomes in Breast Cancer: Reading beyond the Headlines. Trends in cancer. 2020;6(2):98–110. Available from: https://pubmed.ncbi.nlm.nih.gov/32061310.
Andrikopoulou A, Terpos E, Chatzinikolaou S, Apostolidou K, Ntanasis-Stathopoulos I, Gavriatopoulou M, et al. TP53 mutations determined by targeted NGS in breast cancer: a case-control study. Oncotarget. 2021;12(21):2206–14. Available from: https://pubmed.ncbi.nlm.nih.gov/34676052.
The Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions. Version 5. Higgins J, Green S, editors. 2011. Available from: www.handbook.cochrane.org.
Acknowledgements
We would like to extend our deep gratitude to Dr. Nik Ani Afiqah Haji Mohammad Tuah and Dr. Ravi Sekhar Patnaik for the helpful discussion, and Madam Sriyani Perera for proofreading our manuscript and the valuable insight.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MA conceptualised the original topic content. SM conceptualised and designed the research protocol. NS and SM searched the studies. NS, SM, and AM extracted all necessary data and checked the data extraction process. NS and SM led the meta-analysis. NS prepared the original draft manuscript. SM and AM led the revision and edited the manuscript. SP proofread the original manuscript. LH, SP, and MA revised and edited the final version of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable; the analysis is based on published aggregate data and does not require ethical approval or informed consent. Thus, the ethics approval was waived by the University Research Ethics Committee (UREC).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA 2020 Checklist.
Additional file 2.
Search term strategy. Supplementary Table 2.1. The keywords and search terms formulated from the SLR PICO question. Supplementary Table 2.2. Search strategy and results from MEDLINE (PubMed) database. Supplementary Table 2.3. Search strategy and results from Science Direct database. Supplementary Table 2.4. Search strategy and results from Scopus database. Supplementary Table 2.5. Search strategy and results from Cochrane Library database.
Additional file 3.
Data Extraction. Supplementary Table 3.1. Extraction of data from the included studies in the systematic literature review and meta-analysis. Supplementary Table 3.2. Extraction of pCR data from the included studies in the systematic literature review and meta-analysis.
Additional file 4.
Data Synthesis. Supplementary Table 4.1. Data synthesised for overview of all included studies. Supplementary Table 4.2.1. Data synthesised for the association of breast cancer treatment response according to breast cancer characterisation. Supplementary Table 4.2.2. Analysis of breast cancer treatment response according to chemotherapeutic agents in different breast cancer characteristics. Supplementary Table 4.3. Pooled reported association of pCR in included studies. Supplementary Table 4.4. Evaluation of synthesised tpCR data. Supplementary Table 4.5. Evaluation of synthesised tpCR data. Supplementary Table 4.6. Evaluation of synthesised pooled reported association of pCR data.
Additional file 5.
Modified Newcastle-Ottawa Quality Assessment Scale.
Additional file 6.
Quality of the included studies. Supplementary Table 6.1. Newcastle-Ottawa Scale of each included cohort study. Supplementary Figure 6.1. Risk of bias by domain and question in 87 cohort studies using Newcastle-Ottawa Scale. Numbers on the green bar represent the number of studies with low risk of bias over the number of studies assessed. Supplementary Table 6.2. Newcastle-Ottawa Scale of each included case-control study. Supplementary Figure 6.2. Risk of bias by domain and question in 14 case-cohort studies using Newcastle-Ottawa Scale. Numbers on the green bar represent the number of studies with low risk of bias over the number of studies assessed.
Additional file 7.
Meta-analysis results. Supplementary Figure 7.1. Pooled pCR outcome of NAC-treated Asian breast cancer patients. Forest plots describing the random effect ORs and 95% CIs from studies assessing the association of pCR outcome in: NAC TA-treated breast cancer patients between (A) TNBC and HER2E; (B) Luminal B and Luminal A; NAC TP-treated breast cancer patients between (C) HER2E and TNBC; NAC TA-treated breast cancer patients with (D) EGFR. I2 and p-value for X2 of heterogeneity are reported for each group analysis. Supplementary Figure 7.2. Pooled reported association of pCR in NAC-treated Asian breast cancer patients presented in different variables. Forest plots describing the random effect ORs and 95% CIs from studies assessing the pooled reported association of pCR in NAC-treated breast cancer patients presented according to (A) Molecular classification; (B) Genetic variations; and (C) Biomarkers. I2 and p-value for X2 of heterogeneity are reported for each group analysis. Supplementary Figure 7.3. Pooled reported association of pCR in NAC-treated Asian breast cancer patients with ER. Forest plot describing the random effect ORs and 95% CIs from studies assessing the association between the biomarker ER and pCR in NAC-treated breast cancer patients. I2 and p-value for X2 of heterogeneity are reported for each group analysis. Supplementary Figure 7.4. Pooled reported association of pCR in NAC-treated Asian breast cancer patients with PR. Forest plot describing the random effect ORs and 95% CIs from studies assessing the association between the biomarker PR and pCR in NAC-treated breast cancer patients. I2 and p-value for X2 of heterogeneity are reported for each group analysis. Supplementary Figure 7.5. Pooled reported association of pCR in NAC-treated Asian breast cancer patients with HR. Forest plot describing the random effect ORs and 95% CIs from studies assessing the association between the hormone receptors (HR) – comprising ER and PR – and pCR in NAC-treated breast cancer patients. I2 and p-value for X2 of heterogeneity are reported for each group analysis. Supplementary Figure 7.6. Pooled reported association of pCR in NAC-treated Asian breast cancer patients with HER2. Forest plot describing the random effect ORs and 95% CIs from studies assessing the association between the biomarker HER2 and pCR in NAC-treated breast cancer patients. I2 and p-value for X2 of heterogeneity are reported for each group analysis. Supplementary Figure 7.7. Pooled reported association of pCR in NAC-treated Asian breast cancer patients with Ki-67. Forest plot describing the random effect ORs and 95% CIs from studies assessing the association between Ki-67 and pCR in NAC-treated breast cancer patients. I2 and p-value for X2 of heterogeneity are reported for each group analysis. Supplementary Figure 7.8. Pooled reported association of pCR in NAC-treated Asian breast cancer patients presented in different biomarkers. Forest plot describing the random effect HRs and 95% CIs from studies assessing the association between pCR in NAC-treated breast cancer patients and the biomarkers ER, HR, and Ki-67. I2 and p-value for X2 of heterogeneity are reported for each group analysis.
Additional file 8.
Publication Bias. Supplementary Figure 8.1. Funnel plot of pooled pCR outcome of Asian breast cancer patients treated with TA chemotherapy. Funnel plot assessing the publication bias in evaluating the effect of HER2E and Luminal, combined in breast cancer pCR outcome of patients treated with TA regimen in the neoadjuvant setting. Supplementary Figure 8.2. Funnel plot of pooled pCR outcome of Asian breast cancer patients treated with TA chemotherapy. Funnel plot assessing the publication bias in evaluating the effect of TNBC and Luminal, combined in breast cancer pCR outcome of patients treated with TA regimen in the neoadjuvant setting. Supplementary Figure 8.3. Funnel plot of pooled pCR outcome of Asian breast cancer patients treated with TA chemotherapy. Funnel plot assessing the publication bias in evaluating the effect of TNBC and HER2E in breast cancer pCR outcome of patients treated with TA regimen in the neoadjuvant setting. Supplementary Figure 8.4. Funnel plot of pooled pCR outcome of Asian breast cancer patients treated with TP chemotherapy. Funnel plot assessing the publication bias in evaluating the effect of HER2E and Luminal, combined in breast cancer pCR outcome of patients treated with TP regimen in the neoadjuvant setting. Supplementary Figure 8.5. Funnel plot of pooled pCR outcome of Asian breast cancer patients treated with TA chemotherapy. Funnel plot assessing the publication bias in evaluating the effect of ER in breast cancer pCR outcome of patients treated with TA regimen in the neoadjuvant setting. Supplementary Figure 8.6. Funnel plot of pooled pCR outcome of Asian breast cancer patients treated with TA chemotherapy. Funnel plot assessing the publication bias in evaluating the effect of HER2 in breast cancer pCR outcome of patients treated with TA regimen in the neoadjuvant setting. Supplementary Figure 8.7. Funnel plot of pooled pCR outcome of Asian breast cancer patients treated with TA chemotherapy. Funnel plot assessing the publication bias in evaluating the effect of Ki-67 in breast cancer pCR outcome of patients treated with TA regimen in the neoadjuvant setting. Supplementary Figure 8.8. Funnel plot of pooled pCR association of Asian breast cancer patients in the neoadjuvant setting. Funnel plot assessing the publication bias in evaluating the effect of ER+ and ER- (adjusted OR association) in breast cancer pCR outcome of patients treated in the neoadjuvant setting. Supplementary Figure 8.9. Funnel plot of pooled pCR association of Asian breast cancer patients in the neoadjuvant setting. Funnel plot assessing the publication bias in evaluating the effect of PR- and PR+ (adjusted OR association) in breast cancer pCR outcome of patients treated in the neoadjuvant setting. Supplementary Figure 8.10. Funnel plot of pooled pCR association of Asian breast cancer patients in the neoadjuvant setting. Funnel plot assessing the publication bias in evaluating the effect of HER2- and HER2+ (crude OR association) in breast cancer pCR outcome of patients treated in the neoadjuvant setting. Supplementary Figure 8.11. Funnel plot of pooled pCR association of Asian breast cancer patients in the neoadjuvant setting. Funnel plot assessing the publication bias in evaluating the effect of HER2+ and HER2- (adjusted OR association) in breast cancer pCR outcome of patients treated in the neoadjuvant setting. Supplementary Figure 8.12. Funnel plot of pooled pCR association of Asian breast cancer patients in the neoadjuvant setting. Funnel plot assessing the publication bias in evaluating the effect of high and low Ki-67 (crude OR association) in breast cancer pCR outcome of patients treated in the neoadjuvant setting. Supplementary Figure 8.13. Funnel plot of pooled pCR association of Asian breast cancer patients in the neoadjuvant setting. Funnel plot assessing the publication bias in evaluating the effect of high and low Ki-67 (adjusted OR association) in breast cancer pCR outcome of patients treated in the neoadjuvant setting.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bahrin, N.W.S., Matusin, S.N.I., Mustapa, A. et al. Exploring the effectiveness of molecular subtypes, biomarkers, and genetic variations as first-line treatment predictors in Asian breast cancer patients: a systematic review and meta-analysis. Syst Rev 13, 100 (2024). https://doi.org/10.1186/s13643-024-02520-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-024-02520-5