Abstract
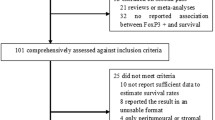
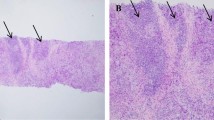
It has been reported that the prognostic significances of tumor-infiltrating FOXP3+ regulatory T cells (Tregs) in breast carcinoma depend on their relative density and tissue locations. We here assessed the changes of Tregs before and after neoadjuvant chemotherapy (NC) and their relationships with tumor response and patient survival. Intratumoral and peritumoral infiltration of FOXP3+ Tregs were evaluated by immunohistochemistry in 132 cases of invasive breast carcinomas before and after NC. After NC, the density of infiltrated Tregs within tumor bed remained stable, whereas it decreased significantly (P = 0.015) in the tissue surrounding tumor. The changes were significant in those tumors that usually response to NC, including the HER2-enriched and basal-like subtypes (P = 0.035; P = 0.004). Univariate and multivariate analyses identified the decreased peritumoral Tregs were an independent predictor for pathologic complete response (pCR), while the intratumoral Tregs after chemotherapy was proved to be associated with overall survival and progression-free survival of the patients. The findings of the study indicated that peritumoral Treg was sensitive to chemotherapy and associated with pCR, while intratumoral Treg was an independent prognostic predictor of breast cancer patients.


Similar content being viewed by others
References
Smith IC, Heys SD, Hutcheon AW et al (2002) Neoadjuvant chemotherapy in breast cancer: significantly enhanced response with docetaxel. J Clin Oncol 20:1456–1466
Fisher B, Bryant J, Wolmark N et al (1998) Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol 16:2672–2685
Rastogi P, Anderson SJ, Bear HD et al (2008) Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol 26:778–785
Lake RA, Robinson BW (2005) Immunotherapy and chemotherapy—a practical partnership. Nat Rev Cancer 5:397–405
Lake RA, van der Most RG (2006) A better way for a cancer cell to die. N Engl J Med 354:2503–2504
Casares N, Pequignot MO, Tesniere A et al (2005) Caspase-dependent immunogenicity of doxorubicin-induced tumor cell death. J Exp Med 202:1691–1701
Obeid M, Tesniere A, Ghiringhelli F et al (2007) Calreticulin exposure dictates the immunogenicity of cancer cell death. Nat Med 13:54–61
Gianni L, Zambetti M, Clark K et al (2005) Gene expression profiles in paraffin-embedded core biopsy tissue predict response to chemotherapy in women with locally advanced breast cancer. J Clin Oncol 23:7265–7277
Apetoh L, Ghiringhelli F, Tesniere A et al (2007) Toll-like receptor 4-dependent contribution of the immune system to anticancer chemotherapy and radiotherapy. Nat Med 13:1050–1059
Bates GJ, Fox SB, Han C et al (2006) Quantification of regulatory T cells enables the identification of high-risk breast cancer patients and those at risk of late relapse. J Clin Oncol 24:5373–5380
Bohling SD, Allison KH (2008) Immunosuppressive regulatory T cells are associated with aggressive breast cancer phenotypes: a potential therapeutic target. Mod Pathol 21:1527–1532
Gobert M, Treilleux I, Bendriss-Vermare N et al (2009) Regulatory T cells recruited through CCL22/CCR4 are selectively activated in lymphoid infiltrates surrounding primary breast tumors and lead to an adverse clinical outcome. Cancer Res 69:2000–2009
Liu F, Lang R, Zhao J et al (2011) CD8(+) cytotoxic T cell and FOXP3(+) regulatory T cell infiltration in relation to breast cancer survival and molecular subtypes. Breast Cancer Res Treat 130:645–655
Perez SA, Karamouzis MV, Skarlos DV et al (2007) CD4+ CD25+ regulatory T-cell frequency in HER-2/neu (HER)-positive and HER-negative advanced-stage breast cancer patients. Clin Cancer Res 13:2714–2721
Ladoire S, Arnould L, Apetoh L et al (2008) Pathologic complete response to neoadjuvant chemotherapy of breast carcinoma is associated with the disappearance of tumor-infiltrating FOXP3+ regulatory T cells. Clin Cancer Res 14:2413–2420
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19:403–410
Ogston KN, Miller ID, Payne S et al (2003) A new histological grading system to assess response of breast cancers to primary chemotherapy: prognostic significance and survival. Breast 12:320–327
Cheang MC, Chia SK, Voduc D et al (2009) Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst 101:736–750
Voduc KD, Cheang MC, Tyldesley S, Gelmon K, Nielsen TO, Kennecke H (2010) Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol 28(10):1684–1691
Curiel TJ, Coukos G, Zou LH et al (2004) Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med 10:942–949
Sato E, Olson SH, Ahn J et al (2005) Intraepithelial CD8(+) tumor-infiltrating lymphocytes and a high CD8(+)/regulatory T cell ratio are associated with favorable prognosis in ovarian cancer. Proc Natl Acad Sci USA 102:18538–18543
Kobayashi N, Hiraoka N, Yamagami W et al (2007) FOXP3(+) regulatory T cells affect the development and progression of hepatocarcinogenesis. Clin Cancer Res 13:902–911
Gao Q, Qiu SJ, Fan J et al (2007) Intratumoral balance of regulatory and cytotoxic T cells is associated with prognosis of hepatocellular carcinoma after resection. J Clin Oncol 25:2586–2593
Hiraoka N, Onozato K, Kosuge T, Hirohashi S (2006) Prevalence of FOXP3(+) regulatory T cells increases during the progression of pancreatic ductal adenocarcinoma and its premalignant lesions. Clin Cancer Res 12:5423–5434
Galon J, Costes A, Sanchez-Cabo F et al (2006) Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 313:1960–1964
Dieu-Nosjean MC, Antoine M, Danel C et al (2008) Long-term survival for patients with non-small-cell lung cancer with intratumoral lymphoid structures. J Clin Oncol 26:4410–4417
Salama P, Phillips M, Grieu F et al (2009) Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. J Clin Oncol 27:186–192
Ghiringhelli F, Menard C, Puig PE et al (2007) Metronomic cyclophosphamide regimen selectively depletes CD4+ CD25+ regulatory T cells and restores T and NK effector functions in end stage cancer patients. Cancer Immunol Immunother 56:641–648
Machiels JP, Reilly RT, Emens LA et al (2001) Cyclophosphamide, doxorubicin, and paclitaxel enhance the antitumor immune response of granulocyte/macrophage-colony stimulating factor-secreting whole-cell vaccines in HER-2/neu tolerized mice. Cancer Res 61:3689–3697
Menard C, Martin F, Apetoh L, Bouyer F, Ghiringhelli F (2008) Cancer chemotherapy: not only a direct cytotoxic effect, but also an adjuvant for antitumor immunity. Cancer Immunol Immunother 57:1579–1587
Gonzalez-Angulo AM, McGuire SE, Buchholz TA et al (2005) Factors predictive of distant metastases in patients with breast cancer who have a pathologic complete response after neoadjuvant chemotherapy. J Clin Oncol 23:7098–7104
Acknowledgments
Research was supported by grants from the National Natural Science Foundation of China (30930038, 81172531), National “973” Program of China (2009CB521700), the Program for Changjiang Scholars and Innovative Research Team in University (IRT0743), and Innovation Funding for graduate of Tianjin Medical University (2010GSI07).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Fangfang Liu, Yaqing Li, Meijing Ren contributed equally to this study.
Rights and permissions
About this article
Cite this article
Liu, F., Li, Y., Ren, M. et al. Peritumoral FOXP3+ regulatory T cell is sensitive to chemotherapy while intratumoral FOXP3+ regulatory T cell is prognostic predictor of breast cancer patients. Breast Cancer Res Treat 135, 459–467 (2012). https://doi.org/10.1007/s10549-012-2132-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2132-3