Abstract
Background
Although the present diagnosis of acute kidney injury (AKI) involves measurement of acute increases in serum creatinine (SC) and reduced urine output (UO), measurement of UO is underutilized for diagnosis of AKI in clinical practice. The purpose of this investigation was to conduct a systematic literature review of published studies that evaluate both UO and SC in the detection of AKI to better understand incidence, healthcare resource use, and mortality in relation to these diagnostic measures and how these outcomes may vary by population subtype.
Methods
The systematic literature review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist. Data were extracted from comparative studies focused on the diagnostic accuracy of UO and SC, relevant clinical outcomes, and resource usage. Quality and validity were assessed using the National Institute for Health and Care Excellence (NICE) single technology appraisal quality checklist for randomized controlled trials and the Newcastle–Ottawa Quality Assessment Scale for observational studies.
Results
A total of 1729 publications were screened, with 50 studies eligible for inclusion. A majority of studies (76%) used the Kidney Disease: Improving Global Outcomes (KDIGO) criteria to classify AKI and focused on the comparison of UO alone versus SC alone, while few studies analyzed a diagnosis of AKI based on the presence of both UO and SC, or the presence of at least one of UO or SC indicators. Of the included studies, 33% analyzed patients treated for cardiovascular diseases and 30% analyzed patients treated in a general intensive care unit. The use of UO criteria was more often associated with increased incidence of AKI (36%), than was the application of SC criteria (21%), which was consistent across the subgroup analyses performed. Furthermore, the use of UO criteria was associated with an earlier diagnosis of AKI (2.4–46.0 h). Both diagnostic modalities accurately predicted risk of AKI-related mortality.
Conclusions
Evidence suggests that the inclusion of UO criteria provides substantial diagnostic and prognostic value to the detection of AKI.
Similar content being viewed by others
Background
As a subgroup of kidney disease, acute kidney injury (AKI) is defined by abnormalities in kidney function over six hours to one week and affects around 32% to 75% of intensive care unit (ICU) patients [1,2,3,4,5,6,7,8]. Notably, AKI has been associated with an adjusted incremental cost of over $8417 (2017 US dollars) and 2.9 days incremental length of hospital stay [9]. The pathophysiology of AKI in the ICU is multi-factorial, with the reported incidence varying between patient populations and history of comorbidities (e.g., cardiovascular disease, hemodynamic instability, infection, chronic kidney disease, liver disease, diabetes, surgery, and nephrotoxic drugs) [10].
Early detection of AKI can lead to sooner diagnosis and implementation of management techniques aimed at preventing or delaying the progression to increasingly severe disease [11]. Diagnosis of AKI can be assessed through multiple classification systems including the RIFLE (Risk, Injury, Failure, Loss of kidney function, and End-stage kidney disease), AKIN (Acute Kidney Injury Network), VARC-2 (Valve Academic Research Consortium-2), and KDIGO (Kidney Disease: Improving Global Outcomes) criteria, which all involve measurement of acute increases in serum creatinine (SC) and reduced urine output (UO) [12–14]. Most recently in 2012, the KDIGO organization released a newer classification, offering simplified and integrated diagnostic criteria [15, 16]. While diagnostic criteria have been standardized, variable assessment impedes researchers from comparing results and making conclusions about the precise impact of AKI care guidelines and bundles on patient outcomes [11].
Contributing to this assessment variability, UO is sometimes omitted in clinical practice as there are technical difficulties associated with accurate manual measurement at regular intervals, uploading values into an information system, and complexity in interpretation [17]. However, the value of UO measurement both alone or in combination with SC is reported to have the ability to detect AKI sooner and more accurately [18, 19], with intensive monitoring of UO having been associated with improved outcomes [20]. This suggests that there may be an overreliance on using SC as a trigger for AKI detection, which can result in missed or delayed diagnosis of approximately 20% of cases of AKI, potentially diagnosing the condition later than if UO were the trigger [8]. This is especially important in populations with fluid accumulation or hemodilution, where impaired UO can be detected without measurable increases in SC or adequate UO in patients with elevated SC without other symptoms of developing AKI [21,22,23].
Several studies have assessed the use of one or both of UO and SC to detect AKI across various subpopulations [24, 25]. However, the rates of AKI and associated outcomes substantially vary. As no systematic assessments of these data have been published, the potential explanation for these contradictory results is unclear. The purpose of the present investigation was to summarize all published studies that evaluate both UO and SC in the detection of AKI through a systematic literature review (SLR). This novel SLR will establish a baseline understanding of the incidence, healthcare resource use, morbidity, and mortality in relation to these diagnostic measures, and how these outcomes may vary by subgroups.
Methods
Search strategy
An a priori SLR protocol (unpublished) was developed that outlined the PICOS criteria (i.e., population, intervention, comparator, outcomes, and study design) and methodology (Additional file 1). This systematic literature review followed the Preferred Reporting for Systematic Reviews and Meta-Analyses (PRSIMA) guidelines (Additional file 2) [26]. The search strategy (Additional file 1) was developed by a medical information specialist in consultation with the review team, and peer reviewed prior to execution using the Peer Review of Electronic Search Strategies (PRESS) checklist [27]. Using the OVID platform, a systematic search of MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials (CENTRAL) was conducted on July 6, 2022. Strategies utilized controlled vocabulary and keywords relevant to the research question (e.g., acute kidney injury, serum creatinine terms, urine output terms). Searches were limited by date from 2012 onwards to align with publication of recent KDIGO guidelines, and no language limits were applied. The search strategy aimed to locate appropriate research on UO as a marker of AKI, specifically focusing on comparative studies between UO and SC. Conference abstracts, posters, and narrative reviews were excluded. Reference lists of retrieved articles and relevant SLRs and meta-analyses were manually searched for additional studies.
Study selection
Studies were selected for inclusion in the SLR based on pre-defined PICOS criteria. Studies that have a very small population, typically fewer than 20 patients, or that solely focus on infants or newborns have been excluded. Studies deemed eligible upon title and abstract screening were screened in full text using DistillerSR software (Ottawa, Ontario, Canada) [28]. Publications were reviewed in duplicate (KT and ATZ) at each stage and discrepancies were resolved by consensus, or by adjudication by a third reviewer (NF).
Data extraction and outcomes
Baseline characteristics and outcomes from the included studies were extracted using a standardized extraction form developed in Microsoft Excel (Redmond, Washington, USA). Extracted details included study characteristics, population and baseline characteristics, results (e.g., time to diagnosis of AKI, incidence of AKI, mortality, health care resource use, follow-up period), and variables required for study quality assessments. Additional outcomes considered for extraction included, but were not limited to, the use of renal replacement therapy (RRT), organ failure-free days, vasopressor-free days, and ventilator-free days. In addition to specific diagnostic criteria used, deviations from these criteria were extracted (e.g., intensity and time interval for UO/SC collection, thresholds for AKI staging, etc.). Data were extracted by one reviewer (KT) and then examined for accuracy and completeness by a second reviewer (ATZ).
The outcome of focus was the incidence of AKI given the frequency of reporting and data availability by various subpopulations. Additional outcomes assessed were as follows: (1) timing to diagnosis of AKI, (2) adjusted mortality risk, and (3) hospital and ICU length of stay.
Analysis
Acute kidney injury-related outcomes were evaluated according to the following diagnostic methods used to detect presence of AKI:
-
1.
AKIUO (i.e., positive on UO alone)
-
2.
AKISC (i.e., positive on SC alone)
-
3.
AKIUO or SC (i.e., both criteria applied, patient positive on at least one)
-
4.
AKIUO and SC (i.e., both criteria applied, patient positive on both).
For incidence of AKI, box plots were generated describing the median and inter-quartile range (IQR) across studies. Data were presented according to subgroups to assess how incidence rates varied. Data were stratified according to UO measurement frequency [i.e., intensive measurement (hourly recordings) versus less intensive (recordings occurred more than one hour apart)], age [i.e., > 60 versus ≤ 60 years and adult versus pediatric patients (excluding infants and newborns)], and cardiac versus non-cardiac patients. Given the fluid overload and accumulation implications [29], another subgroup analysis was performed on cardiovascular-focused studies that enrolled cardiopulmonary bypass (CPB) patients versus those that did not [30].
Studies that reported timing of diagnosis of AKI after admission were qualitatively summarized. Hospital and ICU length of stay were reported by study according to diagnostic method; results from studies were typically unadjusted. Lastly, mortality related to AKI was explored by generating forest plots of adjusted odds ratios (ORs) or hazard ratios (HRs) and 95% confidence intervals (CIs) were extracted from studies reporting adjusted mortality risk between those with and without diagnosed AKI; studies were not pooled due to substantial heterogeneity in population characteristics and timepoints for mortality assessments, but rather presented individually.
In addition, meta-analyses were not performed given the substantial heterogeneity across studies in terms of patient population and reporting of outcomes.
Quality assessment
The quality of studies included in the SLR was assessed using the National Institute for Health and Care Excellence (NICE) single technology appraisal quality checklist for randomized controlled trials (RCTs) and the Newcastle–Ottawa Quality Assessment Scale (NOS) for observational studies [31, 32]. Modified versions of the scale were also considered, and total scores were converted to an eight-point scale. The quality of included studies was assessed independently by two reviewers (KT, ATZ) and reconciled by a third reviewer (NF), if required.
Results
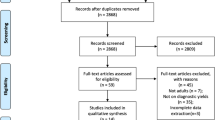
A total of 1771 citations were identified from searches. After removing duplicates, 1729 unique records were screened. Of those, 1326 were excluded for various reasons (e.g., non-human, noncomparative) (Fig. 1). One RCT and 49 observational studies were included in the SLR.
Study characteristics are presented in Table 1. The sample sizes of the 50 included studies ranged from 57 in a single center observational cohort study to 155,624 in a retrospective database analysis. Most studies (76%) used the KDIGO criteria to classify AKI and focused on the comparison of UO alone with SC alone; however, a few studies also included comparisons with UO and SC (AKIUO and SC criteria), and UO or SC (AKIUO or SC criteria). A third of the included studies enrolled patients with cardiovascular-related conditions (33%). Of these, four studies (7%) enrolled patients undergoing cardiac surgery with CPB and one study (2%) enrolled patients undergoing cardiac surgery with or without CPB. Another third enrolled all patients admitted to the general ICU (30%). The remaining third was comprised of studies that enrolled pediatric patients (11%), liver-related conditions (7%), kidney-related conditions (7%), non-cardiac surgery (4%), orthopedic surgery (2%), cancer (2%), parasitic infection (2%), and COVID-19 (2%). The study follow-up durations ranged from 48 h to over 5 years.
Quality assessment
Risk of bias and study quality assessments for the single RCT included are presented in Additional file 3 [33]. The quality of the study by McCullough et al. was acceptable as it had low or unclear risk of bias across all domains.
The NOS assessments for observational studies are presented in Additional file 4, with scores that ranged from six to eight stars. Most studies included patients who were either truly or somewhat representative of the exposed cohort. Two retrospective studies selected patients who were on RRT and were not given a star due to selection bias [34, 35]. All studies drew the cohorts from the same community, used secure surgical records for the ascertainment of exposure, used links to surgical records to assess the outcomes, and had follow-up durations that were long enough for outcomes to occur. All studies had either complete follow-up of all patients or some loss to follow-up unlikely to bias results (i.e., less than 20%). The studies varied most regarding the comparability of the cohorts. One star was given to studies that controlled for select demographic characteristics [8, 20, 24, 36,37,38,39,40,41,42,43,44,45,46,47,48], whereas two stars were given to studies that controlled for several confounders using regression analyses [34, 49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66]. Some studies only reported univariate or unadjusted results and no regression analyses showing lack of effect on outcomes and were not given a star due to potential confounding bias [4, 35, 67,68,69,70,71,72,73,74,75,76,77,78].
Incidence of AKI
The proportion of patients diagnosed with AKI was reported in all the included studies, except one in which the incidence of AKI was displayed as a heatmap (data could not be reliably extracted) [44]. The SLR results demonstrated that the incidence of AKI was highest among studies that used AKIUO or SC criteria (median, IQR: 63%, 40%–70%) followed by those that used AKIUO only (median, IQR: 36%, 21%–60%; Fig. 2). The incidence of AKI by staging is displayed in Fig. 3. It was observed that pooled rates of moderate to severe AKI staging (i.e., stages 2 and 3) were highest with the most sensitive criteria of AKIUO or SC.
Incidence of AKI—All patient populations. *Some studies contributed multiple data points for a given diagnostic method. Boxplots compare AKI incidence based on diagnostic criteria used. The error bars are the range excluding outliers. The bottom and top of the box are the 25th and 75th percentiles, and the line inside the box is the 50th percentile (median). AKI acute kidney injury, AKISC AKI-positive according to SC criteria alone, AKIUO AKI-positive according to UO criteria alone, AKIUO and SC AKI-positive according to both UO and SC criteria—both tests collected, AKIUO or SC AKI-positive according to UO criteria SC criteria, or both—both tests collected, IQR interquartile range
Incidence of AKI by staging – All patient populations. *Some studies contributed multiple data points for a given diagnostic method. Boxplots comparing AKI incidence based on diagnostic criteria used. The error bars are the range excluding outliers, the bottom and top of the box are the 25th and 75th percentiles, the line inside the box is the 50th percentile (median). AKI acute kidney injury, AKISC AKI-positive according to SC criteria alone, AKIUO AKI-positive according to UO criteria alone, AKIUO and SC AKI-positive according to both UO and SC criteria—both tests collected, AKIUO or SC AKI-positive according to UO criteria SC criteria, or both—both tests collected, IQR interquartile range
Subgroup analyses
These findings remain consistent across the various patient subgroups (Table 2). Interestingly, more intensive UO monitoring (defined as repeat UO monitoring at least once every hour) was associated with almost twice (56% versus 31%) the incidence of AKI diagnosis compared with less intensive UO monitoring (defined as delay in between UO measurements spaced at least one hour apart). Irrespective of subgroup, UO alone tended to be associated with a higher incidence of AKI compared to the use of SC alone. The incidence of AKI appeared to be greatest in those patients undergoing CPB and was twice the rate (61% versus 31%) of those without CPB as measured by UO criteria alone. While it was expected that the incidence of AKIUO or SC would be highest compared to the other diagnostic methods, there were some subgroups where AKIUO or AKIUO and SC were greater. For example, the ≤ 60-year-old subgroup incidence by AKIUO was greater than AKIUO or SC (34% vs. 23%), which may be a product of low study and patient numbers for this subgroup.
Time to AKI diagnosis
Specific reporting of timing of AKI diagnosis was identified in six studies (Fig. 4) [4, 24, 48, 59, 62, 75]. Overall, AKI was diagnosed 2.4 to 46.0 h sooner using UO criteria alone compared with SC criteria alone. In one study, AKI was diagnosed 2.5 h sooner using AKIUO and SC criteria compared with SC criteria alone [59]. There was no information on time to AKI diagnosis based on AKIUO or SC criteria. These findings remain consistent across all AKI classification criteria (i.e., KDIGO, RIFLE, AKIN, and VARC-2 criteria). Given the limited data on the timing of AKI diagnosis, subgroup analyses were not performed for this outcome.
Time to AKI diagnosis – All patient populations. * Data presented as mean (± SD) where no median (IQR) was reported. Error bars correspond to the IQR or SD. AKIN Acute Kidney Injury Network, AKISC AKI-positive according to SC criteria alone, AKIUO AKI-positive according to UO criteria alone, AKIUO and SC AKI-positive according to both UO and SC criteria—both tests collected, AKIUO or SC AKI-positive according to UO criteria, SC criteria, or both—both tests collected, IQR interquartile range, KDIGO Kidney Disease: Improving Global Outcomes, RIFLE Risk, Injury, Failure, Loss, and End-stage kidney disease, SD standard deviation, VARC-2 Valve Academic Research Consortium-2
Adjusted mortality risk
Adjusted mortality risk in AKI patients (all stages) versus no AKI patients was reported in nine studies (Fig. 5) [45, 47, 50, 55, 58, 59, 61, 62]. These studies showed that UO is often a significant predictor of short- and long-term mortality in patients with AKI versus those without. Two studies also indicate that testing positive for both UO and SC is associated with the greatest mortality risk. In one study, the adjusted risk of mortality among patients diagnosed with AKI using UO or SC criteria (AKIUO or SC; HR: 3.38 [95% CI 1.63–7.02]) was comparable to those diagnosed with AKI using SC criteria alone (AKISC; HR: 3.10 [95% CI 1.46–6.57]) [58].
Adjusted mortality risk in AKI patients versus no AKI patients. *Data presented as HR (95% CI) where no OR (95% CI) was reported. Error bars correspond to the 95% CI and may extend past visible axis. **UO < 0.3 mL/kg/h for 6 h. The OR/HR of mortality is graphically represented per study and method as a point, with error bars as the 95%CI. The values for the OR/HR with the associated 95%CI are listed to the right of the figure. AKI acute kidney injury, CI confidence interval, HR hazard ratio, OR odds ratio, SC serum creatinine, UO urine output
In a 2021 report, Bianchi et al. found an association of 90-day mortality by UO criteria with stage 2 (OR: 2.43 [95% CI 1.57–3.77], p < 0.001) or stage 3 (OR: 6.24 [95% CI 3.69–10.52], p < 0.001) AKI after adjusting for several variables, including SC criteria and SC level [51]. For another study that focused on comparing more intensive (n = 2529) versus less intensive UO monitoring (n = 7461), for individuals diagnosed with AKI, results indicated that more intensive monitoring was associated with significantly reduced risk of 30-day mortality (HR: 0.90 [95% CI 0.81–0.99], p < 0.04) [20]. This same benefit was not seen for patients that received more intensive (n = 7973) versus less intensive (n = 2017) SC monitoring (HR: 1.10 [95% CI 0.98–1.24], p < 0.11). A detailed breakdown of adjusted mortality risk data (including by AKI stage) is summarized in Additional files 5 and 6.
Length of stay
Intensive care unit and hospital length of stay among patients with AKI were reported in 19 and 13 studies, respectively (Fig. 6). Overall, patients with AKIUO had a median ICU length of stay that ranged from two to eight days and those with AKISC ranged from 0.75 to 10 days. The range was most broad for studies of patients diagnosed with combined criteria (i.e., 1.9 to 15 days with AKIUO or SC, and 2.8 to 15 days with AKIUO and SC; data not shown). These findings remain consistent among the studies that reported hospital length of stay in patients diagnosed with AKI (Additional file 7).
ICU length of stay among patients with AKI. The median ICU length of stay is graphically represented per study and method as a point, with error bars as the IQR. Median values with the associated IQR are listed to the right of the figure. Note that unadjusted results are presented. AKI acute kidney injury, ICU intensive care unit, IQR interquartile range, SC serum creatinine, UO urine output
Discussion
General findings
Although UO is an important component of AKI detection, it is often omitted from clinical practice [17] as the recordings are often missed, late, or a challenge for nursing workflow [79]. Despite the present attempt to systematically review the impact of UO and SC on AKI-related outcomes across 50 clinical studies, clinically relevant characteristics and outcomes have been underreported. Based on available data, the incidence of AKI in hospitalized populations appeared to be highest when UO criteria were used in pooled populations and across each subgroup tested. Furthermore, the use of UO criteria allowed for AKI diagnosis earlier than SC criteria by 2.5 to 46 h. Similar to SC criteria, UO was found to be a strong predictor of AKI-related mortality.
Acute kidney injury incidence
Interesting patterns of AKI detection were observed amongst subgroups. Except for the pediatric cohort, the incidence of AKI was greater with UO compared to SC criteria across several subgroups. This difference was especially pronounced in the cardiac patient subgroup, where the incidence of AKI measured by UO criteria was 2.5 times greater than SC criteria (45% versus 18%) and 3.2 times greater in those that underwent CPB (61% versus 19%). The increased detection of AKI by UO criteria is consistent with the implications of post-surgical fluid accumulation and imbalance, where SC may often be diluted [80, 81]. Fluid accumulation may lead to fluid accumulation syndrome reflecting in tissue edema, necessitating de-resuscitation active fluid removal by either diuretics or ultrafiltration) and close monitoring of UO [82]. A recent study of cardiac surgery patients with urinary catheter dwell times greater than 24 h found that all exhibited some degree of intra-abdominal hypertension, increasing the risk of AKI [83]. Increased AKI detection with UO criteria was also expected in older populations, where SC is reduced due to decreased muscle mass [84]. For patients over 60 years old, the greatest incidence was detected among AKIUO or SC patients, indicating that more cases may be missed when omitting UO criteria from practice (66% compared to 20% by AKISC). While UO measurements are robust in these populations, UO is still susceptible to artificial increases by therapies such as diuretics [85].
Recent studies have examined the detection of AKI within specific populations. In a study conducted by Zarbock et al., KDIGO Stage 1 AKI was detected more frequently by SC alone compared to UO alone (54% vs. 30%), whereas KDIGO stage 2 was detected more often by UO alone (40% vs. 28%) [86]. Zarbock et al. also observed that patients diagnosed by UO alone, regardless of KDIGO stage, had less persistent AKI. In a similar analysis, White et al. found that UO alone detected more sepsis-associated AKI than SC alone (44% vs. 35%); furthermore, patients diagnosed by UO alone had a three times greater chance of complete renal recovery [87]. Our findings and recent research highlight the importance of adhering to guidelines suggesting monitoring both UO and SC to diagnose AKI as early as possible for the greatest likelihood of detection. Additional studies are needed to further explore the prognostic value that may derive from examining one metric in the confirmed absence of the other.
Impact of intensive urine output monitoring
Guidelines recommend that hourly monitoring of UO for a six-hour window and changes in SC within 48 h support timely definition of AKI [14]. In a large, retrospective study conducted by Jin et al. in 2017 of approximately 45,568 patients admitted to the ICU, intensive monitoring of UO (defined as hourly collection), compared with less intensive monitoring, resulted in increased detection of AKI and improved mortality outcomes for people with AKI, after adjustment for age and severity of illness [20]. These findings were supported by the present review, where AKI detection rates were higher in studies that collected UO measurements at an intensive frequency (maximum 1 h between measurements). However, it is unclear if these detection rates were a product of increased monitoring frequency, or if the populations included in the subgroup analyses were at higher risk for AKI. Hospitals that strive for hourly monitoring of UO are also likely attentive to the clinical and economic burden posed by infections associated with indwelling urinary catheters [88]—the very devices which facilitate efficient, accurate measurement of UO. Recently introduced, suction-assisted external wicking catheters can achieve the objective of reducing indwelling urinary catheter utilization while allowing for accurate urine output measurements without the necessity to weigh absorbent products or bed pads [89]. A study of urine capture in healthy volunteers found median urine capture rates for suction-assisted external wicking catheters exceeded 95% [90]. If hospitals verify these results in acute populations, suction-assisted external wicking catheters should prove to be effective alternatives for the early detection of AKI risk.
Across the eight studies that reported time-to-diagnosis outcomes, the use of AKIUO criteria resulted in diagnosis 2.4 to 46.0 h earlier than AKISC criteria, which may support disease management efforts. As an example, hypovolemia is a primary factor in UO reductions, and is treated by initiation of fluid resuscitation [91]. Clinical observation has shown that renal function did not improve after fluid resuscitation in half of critically ill patients with oliguria [92]. As a result, oliguria unresponsive to fluid administration may be a strong predictive marker of AKI in hypovolemic patients. Similarly, UO monitoring may be important even after AKI diagnosis as UO is a therapeutic target representing a predictor of successful cessation during the 24 h prior to stopping continuous RRT [93]. Notably, patients are often kept on dialysis longer than may be appropriate, with a need for clinically- and cost-effective strategies that support successful and timely cessation of RRT [94]. Overall, there is a current lack of standardization in the implementation of AKIUO criteria, and this may challenge clinical utility [38].
Clinical and economic implications
The clinical and economic consequences of AKI can be substantial. For example, a 2017 study reporting on a 2012 National Inpatient Sample analysis of over 29 million patients demonstrated the excess costs associated with AKI in hospitalized patients. In this study, an incremental cost of $7933 and incremental length of stay of 3.2 days was reported in patients with AKI versus patients without AKI across variable diagnoses [95]. Such economic burden in the United States was noted to warrant further attention from hospitals and policymakers to enhance process of care. These data are further substantiated by a Canadian population-based study of 239,906 hospitalized patients which demonstrated that the severity of AKI, need for dialysis, and lack of kidney recovery were associated with significant healthcare costs persisting a year after admission. Furthermore, it was estimated that the incremental cost of AKI in Canada was estimated to be over $200 million dollars per year [96].
Recent developments in UO monitoring may be one step in helping to alleviate this economic burden. Urine output has been more recently established as a continuous, dynamic and low-cost parameter, providing improvements on manual collection methods, and allowing for real-time monitoring [19, 97, 98]. Notably, compared to manual UO monitoring, automated UO monitoring improves timeliness of documentation, and reduces hospital workloads without compromising accuracy [19]. As a result, it can be argued that continuous UO monitoring more closely adheres to AKI guidelines, and provides more data and information compared to a discrete laboratory parameter like SC [79]. One study demonstrated that a computerized decision support system that evaluates the patient for AKI every time a new UO value is charted in the clinical information system was found to reduce the progression of AKI from 42.0% of Stage 1 AKI patients to 33.5% of those Stage 1 patients [99]. Cost-effectiveness data on the impact of AKI detection automation is limited. A model of intensive UO monitoring resulting in early detection of AKI, and early initiation of renal replacement therapy in appropriate patients, estimated that the resultant shorter ICU length of stay would translate to organizational saving of $651 for each ICU patient [100]. Future studies should evaluate whether integration of automated and continuous UO measurements into the electronic health record allows for near-immediate implementation of AKI management strategies further improving upon these clinical results with decreased length of stay, hospital costs and mortality.
Strengths and limitations of the present work
The current review represents a rigorous, objective, and systematic effort to comprehensively summarize the breadth of studies assessing outcomes with use of UO and/or SC criteria; no systematic reviews to date have reported diagnosis and outcomes data to this extent. Furthermore, the search included many newer studies that were published since the most recent guidelines (KDIGO, 2012 [14]). The present review was restricted to a qualitative analysis given the high heterogeneity of the included studies in design and patient characteristics. Key factors which may bias the detection of AKI were found to be heterogeneous (e.g., methods for establishing baseline SC, and use of hourly or average UO measurement) or not uniformly reported (e.g., history of chronic kidney disease, diuretic use, etc.). Variation in AKI incidence by up to 15% can result from the choice of methods used to estimate missing baseline serum creatinine levels [70]. Therefore, it is crucial to consider standardizing these methods. Furthermore, it is recognized that the monitoring of AKI is anticipated to be more frequent in high-risk populations, potentially leading to an inclination towards increased detection. This is evident in two studies that incorporated patients undergoing RRT, who might be at a more advanced stage of AKI disease progression, consequently potentially skewing the detection process [34, 35]. Although a lack of control for these factors is a notable limitation, the present study highlights the gaps in the current evidence base and the subsequent challenges associated with synthesizing the available information and making direct comparisons. Despite these challenges, subgroup analyses were conducted to identify unique trends and allow better interpretability of these data, where possible. Also, the design of the studies limited a true comparison of the longer-term impact of diagnosing with either SC or UO or a combination of criteria. For example, while many studies reported on the length of hospital or ICU stay, they were not designed to assess if earlier or more accurate diagnosis with one measure were significantly associated with a reduction in healthcare resource use, or disease progression. Additional research is needed to elucidate the mechanisms by which AKIUO and AKISC lead to different outcomes, and this will likely vary by subgroup (for example, through influencing clinical decision-making). Ideally, future studies might be designed much like the study by Jin et al. from 2017 which appropriately controls for heterogeneity and potential confounding bias within the AKI-diagnosed cohort of patients. Finally, while the scope of this review focused on SC and UO as validated measures to diagnose AKI, additional work is needed to compare each to the evolving serum and urinary biomarkers as the field evolves [101, 102].
Conclusions
Acute kidney injury is a multifactorial disease that results in significant healthcare resource utilization, contributing to prolonged lengths of ICU and hospital stay, and increased mortality [2,3,4,5,6,7,8, 10, 95, 103]. While diagnostic criteria for AKI have been standardized, variable hospital compliance for UO components of guidelines impedes researchers from assessing the total potential impact of AKI care guidelines on patient outcomes [11]. Despite technical difficulties associated with accurate intermittent manual measurement [17], UO in combination with SC is the most sensitive indicator of AKI with UO alone offering additional prognostic value compared to SC alone. Further, UO monitoring appears to identify AKI earlier than SC monitoring alone offering opportunity for earlier intervention. Future data synthesis that aligns with these findings are contemplated in the Scope of Work for the KDIGO AKI/Acute Kidney Disease Guideline Update, which will examine whether and how UO should be combined with SC criteria for defining and staging AKI [104]. The Scope of Work will also examine whether UO should be weighted differently from SC criteria, and how weighting may vary for each stage of AKI.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its additional information files].
Abbreviations
- AKI:
-
Acute kidney injury
- AKISC :
-
AKI-positive according to SC criteria alone
- AKIUO :
-
AKI-positive according to UO criteria alone
- AKIUO and SC :
-
AKI-positive according to both UO and SC criteria—both tests collected
- AKIUO or SC :
-
AKI-positive according to UO criteria, SC criteria, or both—both tests collected
- AKIN:
-
Acute Kidney Injury Network
- CAN:
-
Canadian dollars
- CPB:
-
Cardiopulmonary bypass
- CENTRAL:
-
Cochrane central register of controlled trials
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- COVID-19:
-
Coronavirus disease 2019
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- KDIGO:
-
Kidney Disease: Improving Global Outcomes
- OR:
-
Odds ratio
- PICOS:
-
Population, intervention, comparator, outcomes, and study design
- PRESS:
-
Peer review of electronic search strategies
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- NICE:
-
National institute for health and care excellence
- NOS:
-
Newcastle–ottawa quality assessment scale
- RIFLE:
-
Risk, injury, failure, loss of kidney function, and End-stage kidney disease
- RCT:
-
Randomized controlled trial
- RRT:
-
Renal replacement therapy
- SAPS:
-
Simplified Acute Physiology Score
- SC:
-
Serum creatinine
- SLR:
-
Systematic literature review
- UO:
-
Urine output
- USD:
-
United States Dollar
- VARC-2:
-
Valve Academic Research Consortium-2
References
Levey AS. Defining AKD: the spectrum of AKI, AKD, and CKD. Nephron. 2022;146(3):302–5.
Luo X, Jiang L, Du B, Wen Y, Wang M, Xi X. Beijing Acute Kidney Injury Trial w: a comparison of different diagnostic criteria of acute kidney injury in critically ill patients. Crit Care. 2014;18(4):R144.
Srisawat N, Sileanu FE, Murugan R, Bellomod R, Calzavacca P, Cartin-Ceba R, Cruz D, Finn J, Hoste EE, Kashani K, et al. Variation in risk and mortality of acute kidney injury in critically ill patients: a multicenter study. Am J Nephrol. 2015;41(1):81–8.
Koeze J, Keus F, Dieperink W, van der Horst IC, Zijlstra JG, van Meurs M. Incidence, timing and outcome of AKI in critically ill patients varies with the definition used and the addition of urine output criteria. BMC Nephrol. 2017;18(1):70.
Shinjo H, Sato W, Imai E, Kosugi T, Hayashi H, Nishimura K, Nishiwaki K, Yuzawa Y, Matsuo S, Maruyama S. Comparison of kidney disease: improving global outcomes and acute kidney injury network criteria for assessing patients in intensive care units. Clin Exp Nephrol. 2014;18(5):737–45.
Fujii T, Uchino S, Doi K, Sato T, Kawamura T, Group JA. Diagnosis, management, and prognosis of patients with acute kidney injury in Japanese intensive care units: the JAKID study. J Crit Care. 2018;47:185–91.
Hoste EA, Bagshaw SM, Bellomo R, Cely CM, Colman R, Cruz DN, Edipidis K, Forni LG, Gomersall CD, Govil D, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41(8):1411–23.
Kellum JA, Sileanu FE, Murugan R, Lucko N, Shaw AD, Clermont G. Classifying AKI by urine output versus serum creatinine level. J Am Soc Nephrol. 2015;26(9):2231–8.
Prasad A, Rosenthal NA, Kartashov A, Knish K, Dreyfus J. Contemporary trend of acute kidney injury incidence and incremental costs among US patients undergoing percutaneous coronary procedures. Catheter Cardiovasc Interv. 2020;96(6):1184–97.
Thongprayoon C, Hansrivijit P, Kovvuru K, Kanduri SR, Torres-Ortiz A, Acharya P, Gonzalez-Suarez ML, Kaewput W, Bathini T, Cheungpasitporn W. Diagnostics, risk factors, treatment and outcomes of acute kidney injury in a new paradigm. J Clin Med. 2020;9(4):1104.
Schaubroeck HAI, Vargas D, Vandenberghe W, Hoste EAJ. Impact of AKI care bundles on kidney and patient outcomes in hospitalized patients: a systematic review and meta-analysis. BMC Nephrol. 2021;22(1):335.
Kellum JA, Sileanu FE, Bihorac A, Hoste EA, Chawla LS. Recovery after acute kidney injury. Am J Respir Crit Care Med. 2017;195(6):784–91.
Lopes JA, Jorge S. The RIFLE and AKIN classifications for acute kidney injury: a critical and comprehensive review. Clin Kidney J. 2013;6(1):8–14.
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179-184.
Gameiro J, Agapito Fonseca J, Jorge S, Lopes JA. Acute kidney injury definition and diagnosis: a narrative review. J Clin Med. 2018;7(10):307.
Lameire NH, Levin A, Kellum JA, Cheung M, Jadoul M, Winkelmayer WC, Stevens PE, Conference P. Harmonizing acute and chronic kidney disease definition and classification: report of a Kidney Disease: Improving Global Outcomes (KDIGO) Consensus Conference. Kidney Int. 2021;100(3):516–26.
Makris K, Spanou L. Acute kidney injury: diagnostic approaches and controversies. Clin Biochem Rev. 2016;37(4):153–75.
Goldstein SL. Urine output assessment in acute kidney injury: the cheapest and most impactful biomarker. Front Pediatr. 2020;7:565.
Kushnir A, Palte E, Morris N, Shahabuddin ZA, Hammond J, Vukelic S, Rabbani LE. Improving fluid output monitoring in the intensive care unit. J Intensive Care Med. 2022;37(1):114–9.
Jin K, Murugan R, Sileanu FE, Foldes E, Priyanka P, Clermont G, Kellum JA. Intensive monitoring of urine output is associated with increased detection of acute kidney injury and improved outcomes. Chest. 2017;152(5):972–9.
Svenmarker S, Haggmark S, Holmgren A, Naslund U. Serum markers are not reliable measures of renal function in conjunction with cardiopulmonary bypass. Interact Cardiovasc Thorac Surg. 2011;12(5):713–7.
Jin J, Xu J, Xu S, Hu J, Jiang W, Shen B, Wang C, Teng J, Ding X. Hemodilution is associated with underestimation of serum creatinine in cardiac surgery patients: a retrospective analysis. BMC Cardiovasc Disord. 2021;21(1):61.
Mazzeffi MA, Stafford P, Wallace K, Bernstein W, Deshpande S, Odonkor P, Grewal A, Strauss E, Stubbs L, Gammie J, et al. Intra-abdominal hypertension and postoperative kidney dysfunction in cardiac surgery patients. J Cardiothorac Vasc Anesth. 2016;30(6):1571–7.
Willner D, Goldman A, Azran H, Stern T, Kirshenbom D, Rosenthal G. Early identification of acute kidney injury in the ICU with real-time urine output monitoring: a clinical investigation. BMC Nephrol. 2021;22(1):293.
Fishman G, Ram E, Gorfil D, Kassif Y, David R, Hershko T, Malbrain M, Singer P, Sessler DI. Early detection of oliguric events in critically ill patients in the ICU with a novel continuous urine flow measurement device: results of an initial validation study. J Clin Monit Comput. 2023;37(5):1341–9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6.
DistillerSR Inc.: DistillerSR. Version2.35. In.; 2021.
Malbrain MLNG, Van Regenmortel N, Saugel B, De Tavernier B, Van Gaal P-J, Joannes-Boyau O, Teboul J-L, Rice TW, Mythen M, Monnet X. Principles of fluid management and stewardship in septic shock: It is time to consider the four D’s and the four phases of fluid therapy. Ann Intensive Care. 2018;8(1):66.
Koskinen A, Aittokallio J, Gunn J, Lehto J, Relander A, Viikinkoski E, Vasankari T, Jalkanen J, Hollmen M, Kiviniemi TO. Risk of fluid accumulation after cardiac surgery. JTCVS Open. 2023;16:602–9.
National Institute for Health and Care Excellence. Single technology appraisal and highly specialized technologies evaluation: user guide for company evidence submission template. National Institute for Health and Care Excellence; 2022.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford; 2000.
McCullough PA, Bennett-Guerrero E, Chawla LS, Beaver T, Mehta RL, Molitoris BA, Eldred A, Ball G, Lee HJ, Houser MT, et al. ABT-719 for the prevention of acute kidney injury in patients undergoing high-risk cardiac surgery: a randomized phase 2b clinical trial. J Am Heart Assoc. 2016;5(8): e003549.
Leite TT, Macedo E, Pereira SM, Bandeira SR, Pontes PH, Garcia AS, Militao FR, Sobrinho IM, Assuncao LM, Liborio AB. Timing of renal replacement therapy initiation by AKIN classification system. Crit Care. 2013;17(2):R62.
Tulgar S, Cakiroglu B, Cevik BE, Karakilic E, Ates NG, Gergerli R, Ozdemir E. Modified KDIGO for predicting mortality in ICU patients receiving continuous renal replacement therapy for acute renal failure: KDIGO-urinary output vs KDIGO-serum creatinine level. Acta Medica Mediterranea. 2016. https://doi.org/10.19193/0393-6384_2016_3_88.
D’Arienzo D, Hessey E, Ali R, Perreault S, Samuel S, Roy L, Lacroix J, Jouvet P, Morissette G, Dorais M, et al. A validation study of administrative health care data to detect acute kidney injury in the pediatric intensive care unit. Can J Kidney Health Dis. 2019;6:2054358119827525.
Vanmassenhove J, Steen J, Vansteelandt S, Morzywolek P, Hoste E, Decruyenaere J, Benoit D, Van Biesen W. The importance of the urinary output criterion for the detection and prognostic meaning of AKI. Sci Rep. 2021;11(1):11089.
Allen JC, Gardner DS, Skinner H, Harvey D, Sharman A, Devonald MAJ. Definition of hourly urine output influences reported incidence and staging of acute kidney injury. BMC Nephrol. 2020;21(1):19.
Bressan AK, James MT, Dixon E, Bathe OF, Sutherland FR, Ball CG. Acute kidney injury following resection of hepatocellular carcinoma: prognostic value of the acute kidney injury network criteria. Can J Surg. 2018;61(5):E11–6.
Amathieu R, Al-Khafaji A, Sileanu FE, Foldes E, DeSensi R, Hilmi I, Kellum JA. Significance of oliguria in critically ill patients with chronic liver disease. Hepatology. 2017;66(5):1592–600.
Engoren M, Maile MD, Heung M, Jewell ES, Vahabzadeh C, Haft JW, Kheterpal S. The association between urine output, creatinine elevation, and death. Ann Thorac Surg. 2017;103(4):1229–37.
Cordova-Sanchez BM, Herrera-Gomez A, Namendys-Silva SA. Acute kidney injury classified by serum creatinine and urine output in critically ill cancer patients. Biomed Res Int. 2016;2016:6805169.
Mizota T, Minamisawa S, Imanaka Y, Fukuda K. Oliguria without serum creatinine increase after living donor liver transplantation is associated with adverse post-operative outcomes. Acta Anaesthesiol Scand. 2016;60(7):874–81.
Harris SK, Lewington AJ, Harrison DA, Rowan KM. Relationship between patients’ outcomes and the changes in serum creatinine and urine output and RIFLE classification in a large critical care cohort database. Kidney Int. 2015;88(2):369–77.
McIlroy DR, Argenziano M, Farkas D, Umann T, Sladen RN. Incorporating oliguria into the diagnostic criteria for acute kidney injury after on-pump cardiac surgery: impact on incidence and outcomes. J Cardiothorac Vasc Anesth. 2013;27(6):1145–52.
Han SS, Kang KJ, Kwon SJ, Wang SJ, Shin SH, Oh SW, Na KY, Chae DW, Kim S, Chin HJ. Additional role of urine output criterion in defining acute kidney injury. Nephrol Dial Transplant. 2012;27(1):161–5.
Tarvasmaki T, Haapio M, Mebazaa A, Sionis A, Silva-Cardoso J, Tolppanen H, Lindholm MG, Pulkki K, Parissis J, Harjola VP, et al. Acute kidney injury in cardiogenic shock: definitions, incidence, haemodynamic alterations, and mortality. Eur J Heart Fail. 2018;20(3):572–81.
Bouchard J, Malhotra R, Shah S, Kao YT, Vaida F, Gupta A, Berg DT, Grinnell BW, Stofan B, Tolwani AJ, et al. Levels of protein C and soluble thrombomodulin in critically ill patients with acute kidney injury: a multicenter prospective observational study. PLoS ONE. 2015;10(3): e0120770.
Koeze J, van der Horst ICC, Keus F, Wiersema R, Dieperink W, Kootstra-Ros JE, Zijlstra JG, van Meurs M. Plasma neutrophil gelatinase-associated lipocalin at intensive care unit admission as a predictor of acute kidney injury progression. Clin Kidney J. 2020;13(6):994–1002.
Jiang J, Zhang J, Liu Y, Xu D, Peng Z. Urine output calculated using actual body weight may result in overestimation of acute kidney injury for obese patients. Shock. 2021;56(5):737–43.
Bianchi NA, Stavart LL, Altarelli M, Kelevina T, Faouzi M, Schneider AG. Association of oliguria with acute kidney injury diagnosis, severity assessment, and mortality among patients with critical illness. JAMA Netw Open. 2021;4(11): e2133094.
Nikkinen O, Jamsa E, Aaltonen T, Alahuhta S, Ohtonen P, Vakkala M. Perioperative acute kidney injury and urine output in lower limb arthroplasties. Acta Anaesthesiol Scand. 2021;65(8):1054–64.
Priyanka P, Zarbock A, Izawa J, Gleason TG, Renfurm RW, Kellum JA. The impact of acute kidney injury by serum creatinine or urine output criteria on major adverse kidney events in cardiac surgery patients. J Thorac Cardiovasc Surg. 2021;162(1):143-151 e147.
Oshomah-Bello EO, Esezobor CI, Solarin AU, Njokanma FO. Acute kidney injury in children with severe malaria is common and associated with adverse hospital outcomes. J Trop Pediatr. 2020;66(2):218–25.
Joliat G-R, Labgaa I, Demartines N, Halkic N. Acute kidney injury after liver surgery: does postoperative urine output correlate with postoperative serum creatinine? HPB. 2020;22(1):144–50.
Howitt SH, Grant SW, Caiado C, Carlson E, Kwon D, Dimarakis I, Malagon I, McCollum C. The KDIGO acute kidney injury guidelines for cardiac surgery patients in critical care: a validation study. BMC Nephrol. 2018;19(1):149.
Hessey E, Morissette G, Lacroix J, Perreault S, Samuel S, Dorais M, Phan V, Jouvet P, Lafrance JP, LeLorier J, et al. Healthcare utilization after acute kidney injury in the pediatric intensive care unit. Clin J Am Soc Nephrol. 2018;13(5):685–92.
Hessey E, Morissette G, Lacroix J, Perreault S, Samuel S, Dorais M, Jouvet P, Lafrance JP, LeLorier J, Phan V, et al. Long-term mortality after acute kidney injury in the pediatric ICU. Hosp Pediatr. 2018;8(5):260–8.
Petaja L, Vaara S, Liuhanen S, Suojaranta-Ylinen R, Mildh L, Nisula S, Korhonen AM, Kaukonen KM, Salmenpera M, Pettila V. Acute kidney injury after cardiac surgery by complete KDIGO criteria predicts increased mortality. J Cardiothorac Vasc Anesth. 2017;31(3):827–36.
Quan S, Pannu N, Wilson T, Ball C, Tan Z, Tonelli M, Hemmelgarn BR, Dixon E, James MT. Prognostic implications of adding urine output to serum creatinine measurements for staging of acute kidney injury after major surgery: a cohort study. Nephrol Dial Transplant. 2016;31(12):2049–56.
Qin JP, Yu XY, Qian CY, Li SS, Qin TH, Chen EZ, Lin JD, Ai YH, Wu DW, Liu DX, et al. Value of kidney disease improving global outcomes urine output criteria in critically ill patients: a secondary analysis of a multicenter prospective cohort study. Chin Med J (Engl). 2016;129(17):2050–7.
Vaara ST, Parviainen I, Pettila V, Nisula S, Inkinen O, Uusaro A, Group FS. Association of oliguria with the development of acute kidney injury in the critically ill. Kidney Int. 2016;89(1):200–8.
Lagny M-G, Jouret F, Koch J-N, Blaffart F, Donneau A-F, Albert A, Roediger L, Krzesinski J-M, Defraigne J-O. Incidence and outcomes of acute kidney injury after cardiac surgery using either criteria of the RIFLE classification. BMC Nephrol. 2015;16(1):1–9.
Tujjar O, Mineo G, Dell’Anna A, Poyatos-Robles B, Donadello K, Scolletta S, Vincent JL, Taccone FS. Acute kidney injury after cardiac arrest. Crit Care. 2015;19(1):169.
Md Ralib A, Pickering JW, Shaw GM, Endre ZH. The urine output definition of acute kidney injury is too liberal. Crit Care. 2013;17(3):1–11.
Chau K, Schisler T, Er L, Jaswal D, Cheung C, Israel A, Bowering J, Levin A. Fluid balance, change in serum creatinine and urine output as markers of acute kidney injury post cardiac surgery: an observational study. Can J Kidney Health Dis. 2014;1:19.
Tornblom S, Wiersema R, Prowle JR, Haapio M, Pettila V, Vaara ST. Fluid balance-adjusted creatinine in diagnosing acute kidney injury in the critically ill. Acta Anaesthesiol Scand. 2021;65(8):1079–86.
Katabi LJ, Pu X, Yilmaz HO, Jia Y, Leung S, Duncan AE. Prognostic utility of KDIGO urine output criteria after cardiac surgery. J Cardiothorac Vasc Anesth. 2021;35(10):2991–3000.
Luther T, Bulow-Anderberg S, Larsson A, Rubertsson S, Lipcsey M, Frithiof R, Hultstrom M. COVID-19 patients in intensive care develop predominantly oliguric acute kidney injury. Acta Anaesthesiol Scand. 2021;65(3):364–72.
Wiersema R, Jukarainen S, Eck RJ, Kaufmann T, Koeze J, Keus F, Pettila V, van der Horst ICC, Vaara ST. Different applications of the KDIGO criteria for AKI lead to different incidences in critically ill patients: a post hoc analysis from the prospective observational SICS-II study. Crit Care. 2020;24(1):164.
Goldani JC, Poloni JA, Klaus F, Kist R, Pacheco LS, Keitel E. Urine microscopy as a biomarker of Acute Kidney Injury following cardiac surgery with cardiopulmonary bypass. Braz J Nephrol. 2019;42:18–23.
Kaddourah A, Basu RK, Goldstein SL, Sutherland SM. Assessment of worldwide acute kidney injury RAaEI: oliguria and acute kidney injury in critically ill children: implications for diagnosis and outcomes. Pediatr Crit Care Med. 2019;20(4):332–9.
Palermo J, Dart AB, DeMello A, Devarajan P, Gottesman R, Guerra GG, Hansen G, Joffe AR, Mammen C, Majesic N. Biomarkers for early acute kidney injury diagnosis and severity prediction: a pilot multi-centre Canadian study of children admitted to the intensive care unit. Pediatr Crit Care Med. 2017;18(6): e235.
Hocine A, Defrance P, Lalmand J, Delcour C, Biston P, Piagnerelli M. Predictive value of the RIFLE urine output criteria on contrast-induced nephropathy in critically ill patients. BMC Nephrol. 2016;17:36.
Shacham Y, Rofe M, Leshem-Rubinow E, Gal-Oz A, Arbel Y, Keren G, Roth A, Ben-Assa E, Halkin A, Finkelstein A, et al. Usefulness of urine output criteria for early detection of acute kidney injury after transcatheter aortic valve implantation. Cardiorenal Med. 2014;4(3–4):155–60.
Wlodzimirow KA, Abu-Hanna A, Slabbekoorn M, Chamuleau RA, Schultz MJ, Bouman CS. A comparison of RIFLE with and without urine output criteria for acute kidney injury in critically ill patients. Crit Care. 2012;16(5):1–9.
Sims AJ, Hussein HK, Prabhu M, Kanagasundaram NS. Are surrogate assumptions and use of diuretics associated with diagnosis and staging of acute kidney injury after cardiac surgery? Clin J Am Soc Nephrol. 2012;7(1):15–23.
Vandenberghe W, Van Laethem L, Herck I, Peperstraete H, Schaubroeck H, Zarbock A, Meersch M, Dhondt A, Delanghe S, Vanmassenhove J, et al. Prediction of cardiac surgery associated - acute kidney injury (CSA-AKI) by healthcare professionals and urine cell cycle arrest AKI biomarkers [TIMP-2]*[IGFBP7]: a single center prospective study (the PREDICTAKI trial). J Crit Care. 2022;67:108–17.
Minor J, Smith A, Deutsch F, Kellum JA. Automated versus manual urine output monitoring in the intensive care unit. Sci Rep. 2021;11(1):17429.
Liu KD, Thompson BT, Ancukiewicz M, Steingrub JS, Douglas IS, Matthay MA, Wright P, Peterson MW, Rock P, Hyzy RC, et al. Acute kidney injury in patients with acute lung injury: impact of fluid accumulation on classification of acute kidney injury and associated outcomes. Crit Care Med. 2011;39(12):2665–71.
Macedo E, Bouchard J, Soroko SH, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL. Program to improve care in acute renal disease s: fluid accumulation, recognition and staging of acute kidney injury in critically-ill patients. Crit Care. 2010;14(3):R82.
Malbrain M, Martin G, Ostermann M. Everything you need to know about deresuscitation. Intensive Care Med. 2022;48(12):1781–6.
Khanna AK, Minear S, Kurz A, Moll V, Stanton K, Essakalli L, Prabhakar A, Predict AKIG. Intra-abdominal hypertension in cardiac surgery patients: a multicenter observational sub-study of the Accuryn registry. J Clin Monit Comput. 2023;37(1):189–99.
Anderson S, Eldadah B, Halter JB, Hazzard WR, Himmelfarb J, Horne FM, Kimmel PL, Molitoris BA, Murthy M, O’Hare AM, et al. Acute kidney injury in older adults. J Am Soc Nephrol. 2011;22(1):28–38.
Reyes AJ. Effects of diuretics on outputs and flows of urine and urinary solutes in healthy subjects. Drugs. 1991;41(Suppl 3):35–59.
Zarbock A, Weiss R, Albert F, Rutledge K, Kellum JA, Bellomo R, Grigoryev E, Candela-Toha AM, Demir ZA, Legros V, et al. Epidemiology of surgery associated acute kidney injury (EPIS-AKI): a prospective international observational multi-center clinical study. Intensive Care Med. 2023;49(12):1441–55.
White KC, Serpa-Neto A, Hurford R, Clement P, Laupland KB, See E, McCullough J, White H, Shekar K, Tabah A, et al. Sepsis-associated acute kidney injury in the intensive care unit: incidence, patient characteristics, timing, trajectory, treatment, and associated outcomes. A multicenter, observational study. Intensive Care Med. 2023;49(9):1079–89.
Kelly T, Ai C, Jung M, Yu K. Catheter-associated urinary tract infections (CAUTIs) and non-CAUTI hospital-onset urinary tract infections: Relative burden, cost, outcomes and related hospital-onset bacteremia and fungemia infections. Infect Control Hosp Epidemiol. 2024. https://doi.org/10.1017/ice.2024.26.
Warren C, Fosnacht JD, Tremblay EE. Implementation of an external female urinary catheter as an alternative to an indwelling urinary catheter. Am J Infect Control. 2021;49(6):764–8.
McRae AD, Kennelly M. Outpatient PureWick™ female external catheter system performance: healthy volunteer study. Continence. 2023;7: 100712.
Klein SJ, Lehner GF, Forni LG, Joannidis M. Oliguria in critically ill patients: a narrative review. J Nephrol. 2018;31(6):855–62.
Legrand M, Le Cam B, Perbet S, Roger C, Darmon M, Guerci P, Ferry A, Maurel V, Soussi S, Constantin JM, et al. Urine sodium concentration to predict fluid responsiveness in oliguric ICU patients: a prospective multicenter observational study. Crit Care. 2016;20(1):165.
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294(7):813–8.
National Institute for Health and Care Excellence. Renal replacement therapy and conservative management. In: Evidence review for indicators for transferring/discontinuing RRT. National Institute for Health and Care Excellence; 2018.
Silver SA, Long J, Zheng Y, Chertow GM. Cost of acute kidney injury in hospitalized patients. J Hosp Med. 2017;12(2):70–6.
Collister D, Pannu N, Ye F, James M, Hemmelgarn B, Chui B, Manns B, Klarenbach S. Alberta kidney disease N: health care costs associated with AKI. Clin J Am Soc Nephrol. 2017;12(11):1733–43.
Panagiotou A, Garzotto F, Gramaticopolo S, Piccinni P, Trentin C, Cruz DN, Ronco C. Continuous real-time urine output monitoring for early detection of acute kidney injury. Contrib Nephrol. 2011;171:194–200.
Chang AJ, Nomura Y, Barodka VM, Hori D, Magruder JT, Katz NM, Berkowitz DE, Hogue CW. Validation of a real-time minute-to-minute urine output monitor and the feasibility of its clinical use for patients undergoing cardiac surgery. Anesth Analg. 2017;125(6):1883–6.
Bourdeaux C, Ghosh E, Atallah L, Palanisamy K, Patel P, Thomas M, Gould T, Warburton J, Rivers J, Hadfield J. Impact of a computerized decision support tool deployed in two intensive care units on acute kidney injury progression and guideline compliance: a prospective observational study. Crit Care. 2020;24(1):656.
Kelly T. PUK7 economic analysis of the impact of intensive urine output monitoring (IUOM) upon early detection of acute kidney injury (AKI) and intensive care unit length of stay (ICU LOS). Value in Health. 2021;24:S235.
Lima C, Macedo E. Urinary biochemistry in the diagnosis of acute kidney injury. Dis Markers. 2018;2018:4907024.
Zou C, Wang C, Lu L. Advances in the study of subclinical AKI biomarkers. Front Physiol. 2022;13: 960059.
Mohsenin V. Practical approach to detection and management of acute kidney injury in critically ill patient. J Intensive Care. 2017;5:57.
Scope of Work KDIGO Clinical Practice Guideline for Acute Kidney Injury (AKI) and Acute Kidney Disease (AKD) Update; 2023. http://kdigo.org/wp-content/uploads/2023/10/KDIGO-AKI-Guideline_Scope-of-Work_25Oct2023_Final.pdf.
Acknowledgements
The authors would like to acknowledge Joanna Bielecki who developed, conducted, and documented the database search. JB is employed by EVERSANA, Canada. The authors would also like to acknowledge Becky Skidmore who was contracted by EVERSANA, Canada to peer review the search strategy prior to execution using the Peer Review of Electronic Search Strategies (PRESS) checklist.
Funding
This work was supported by Becton, Dickinson and Company, who provided funding to conduct the analysis and prepare the manuscript.
Author information
Authors and Affiliations
Contributions
All authors were responsible for study conception, design, and data interpretation. KT and ATZ were additionally responsible for acquisition and analysis, and drafting the manuscript, and all authors were responsible for revising the manuscript critically. All authors agree to be held accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
MLNGM is Professor of Critical Care Research at the First Department of Anesthesiology and Intensive Therapy, Medical University of Lublin, Poland. He is co-founder, past-President, and current Treasurer of WSACS (The Abdominal Compartment Society, http://www.wsacs.org). He is member of the medical advisory Board of Pulsion Medical Systems (part of Getinge group), Serenno Medical, Potrero Medical, Sentinel Medical and Baxter. He consults for B.Braun, Becton, Dickinson and Company, ConvaTec, Spiegelberg, and Holtech Medical, and received speaker's fees from PeerVoice. He holds stock options for Serenno, Sentinel and Potrero. He is co-founder and President of the International Fluid Academy (IFA). The IFA (http://www.fluidacademy.org) is integrated within the not-for-profit charitable organization iMERiT, International Medical Education and Research Initiative, under Belgian law. KT, ATZ, and NCF are employees of EVERSANA™ which was engaged by Becton, Dickinson and Company for the purposes of this research. TK is an employee of Becton, Dickinson and Company. WD is Head of First Department of Anesthesiology and Intensive Therapy, Medical University of Lublin, Poland.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Malbrain, M.L.N.G., Tantakoun, K., Zara, A.T. et al. Urine output is an early and strong predictor of acute kidney injury and associated mortality: a systematic literature review of 50 clinical studies. Ann. Intensive Care 14, 110 (2024). https://doi.org/10.1186/s13613-024-01342-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-024-01342-x