Abstract
Background
Premorbid conditions influence the outcome of acutely ill adult patients aged 80 years and over who are admitted to the ICU. The aim of this study was to determine the influence of such premorbid conditions on 6 month survival.
Methods
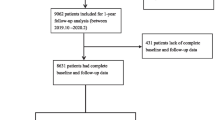
Prospective cohort study in 242 ICUs from 22 countries including patients 80 years or above, admitted over a 6 months period to an ICU between May 2018 and May 2019. Only emergency (acute) ICU admissions in adult patients ≥ 80 years of age were eligible. Patients who were admitted after planned/elective surgery were excluded. We measured the Clinical Frailty Scale (CFS), the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE), disability with the Katz activities of daily living (ADL) score, comorbidities and a Polypharmacy Score (CPS).
Results
Overall, the VIP2 study included 3920 patients. During ICU stay 1191 patients died (30.9%), and another 436 patients (11.1%) died after ICU discharge but within the first 30 days of admission, and an additional 895 patients died hereafter but within the first 6 months after admission (22.8%). The 6 months mortality was 64%. The median CFS was 4 (IQR 3–6). Frailty (CFS ≥ 5) was present in 26.6%. Cognitive decline (IQCODE above 3.5) was found in 30.2%. The median IQCODE was 3.19. A Katz ADL of 4 or less was present in 27.7%. Patients who surviving > 6 months were slightly younger (median age survivors 84 with IQR 81–86) than patients dying within the first 6 months (median age 84, IQR 82–87, p = 0.013), were less frequently frail (CFS > 5 in 19% versus 34%, p < 0.01) and were less dependent based on their Katz activities of daily living measurement (median Katz score 6, IQR 5–6 versus 6 points, IQR 3–6, p < 0.01).
Conclusions
We found that Clinical Frailty Scale, age, and SOFA at admission were independent prognostic factors for 6 month mortality after ICU admission in patients age 80 and above. Adding other geriatric syndromes and scores did not improve the model. This information can be used in shared-decision making.
ClinicalTrials.gov: NCT03370692.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Currently, more than 15% of patients admitted to intensive care units (ICUs) are 80 years of age or older. This proportion of “very old intensive care patients” (VIPs) is estimated to increase to 36% by 2025 [1,2,3]. This has been identified as a public health challenge, because patients aged 80 years and older consume a large proportion of healthcare resources and budgets, while mortality rates are consistently reported to be higher than in younger patients. This is particularly true for older adult patients aged 80 years and over who are admitted acutely [4]. For unplanned admissions, the overall 30-day survival rate for ICU patients is approximately 60% [5, 6].
However, looking at short-term prognosis may be of limited value, as patients usually aim for long-term survival with a good quality of life (QoL) [7]. Intensive care may even be perceived as disproportionate if it only causes suffering and anxiety without achieving the goal of long-term survival. It is, therefore, of paramount importance to better identify elderly patients who are likely to have a good long-term outcome. Previous reports have found an association between pre-morbid conditions and 30 day survival [6]. In very old adult patients, the ability to cope with severe stressors such as critical illness appears to be related to geriatric syndromes such as frailty [5, 6], cognitive decline [8, 9] and reduced performance on the Activities of Daily Living (ADL) scale, in addition to comorbidity. However, the impact of these premorbid conditions on the long-term outcome of acutely admitted elderly ICU patients has not been established. Does the severity of illness on admission to the ICU or premorbid conditions predict a patient's chance of long-term survival?
In this European-based study, we aimed to examine the influence of three common geriatric syndromes: frailty, cognitive impairment and disability, and the presence of comorbidity and polypharmacy, and to assess their influence on 6 month survival.
Methods
Design and setting
This was a prospective observational study in 242 ICUs from 22 European countries, including Turkey. The inclusion period was from May 2018 to May 2019. Most patients were included in the winter of 2018–2019. The 6 month follow-up period ended on 1 December 2019.
The study was coordinated by the Health Services Resource and Outcome (HSRO) and Nurses and Allied Health care Professionals (NAHP) sections of the European Society of Intensive Care Medicine (ESICM). Each country had a national coordinator responsible for ICU recruitment and application for national or regional ethical and regulatory approval of the study. Institutional research ethics committee approval was obtained at each study site. Individual ICUs were asked to enrol consecutive patients for 6 months during the 1 year study period and were allowed to stop when ≥ 20 patients had been enrolled. Participation in the 6 month follow-up was optional for the ICUs. A dedicated website was set up to facilitate information about the study and its progress, and to allow data entry using an electronic case record form (eCRF). The trial is registered at www.ClinicalTrials.gov (ID: NCT03370692). There was no specific funding for this study or for the participating ICUs (Additional file 1).
Participants
Only emergency (acute) ICU admissions of adult patients aged ≥ 80 years were eligible. Patients admitted after planned/elective surgery were excluded, because their mortality rates are completely different (lower) than those of acutely admitted very old critically ill patients [4].
Data collection
Data collection at admission
For each eligible patient, demographic data were collected: age, sex, place of residence prior to hospital admission, and reason for admission according to a predefined list (see Additional file 3). Second, the study collected mandatory data on the patient’s geriatric conditions prior to this hospital admission, including the Clinical Frailty Scale (CFS) [10]. For the assessment of frailty, we defined the level of frailty present prior to hospital admission and unaffected by the current acute illness. The information needed to make this assessment was provided by the patient or proxy, or obtained from the patient’s medical record. The profession of the assessor was documented. The simple description of CFS was used with permission [10]. Frail patients were defined as having a CFS of ≥ 5. We also recorded Katz activities of daily living (Katz ADL) [11], with an ADL score ≤ 4 defining disability. Pre-admission cognitive function was assessed using the Short form of Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) [12]. The information used to calculate the IQCODE was provided by caregivers who had known the patient well for the previous 10 years. We defined cognitive decline as an IQCODE > 3.5 [12]. A comorbidity and polypharmacy score (CPS) was calculated [13]. The CPS was defined as the simple sum of the number of known comorbidities and the number of different medications taken daily before admission (1 point for each chronic comorbidity and 1 point for each medication). Cardiovascular dysfunction was counted per morbidity (e.g., a patient with hypertension, atrial fibrillation and congestive heart failure would receive 3 points, even if they were all cardiovascular comorbidities). The number can vary from 0 (no comorbidity, no medication) to infinity, although in most patients the number was < 20. The severity of CPS has traditionally been stratified as minor/mild (CPS 0–7), moderate (8–14) and severe (≥ 15). In the analyses, the total CPS score was used for analyses (Additional files 4, 5, 6).
Data collection of variables during ICU admission
The Sequential Organ Failure Assessment (SOFA) score was calculated within the first 24 h of ICU admission.14 The total SOFA score on admission was calculated using an online calculator in the eCRF. Length of stay (LOS) in the ICU was recorded as the number of hours between admission and discharge and later converted to days (consecutive 24 h periods rather than calendar days) for analysis. Any period of non-invasive or invasive (with endotracheal intubation or tracheostomy) mechanical ventilation, use of vasoactive drugs and renal replacement therapy (RRT) was recorded with the start (which ICU treatment day) and duration of the procedure (in hours).
Limitation of life-sustaining therapies (LST), such as withholding or withdrawing life-sustaining treatments, was documented when applied and the timing of LST limitation was recorded (in days since ICU admission) [15].
Outcome was assessed as survival at ICU discharge, 30 days and 6 months (180 days) after ICU admission. The source of information for vital status at 6 months was documented.
The CRF and database were hosted on a secure server on the campus of Aarhus University, Denmark.
Bias
The ICUs were asked to include all consecutive patients ≥ 80 years that were acutely admitted to the ICU, irrespective of the anticipated duration of ICU stay.
Study size
We had no formal calculation in this purely observational study. We estimated the 6 month mortality to be approximately 50%, as seen in similar study populations [5, 6].
Data imputation
We used multiple imputation of data to compensate for missing values in both predictors and outcomes. In short, missing data were imputed to create 100 different data sets, in which we used 50 iterations to achieve value stability. Non-linear models were used and variable order and predictors were set to avoid feedback loops. Post-processing was set to limit extreme values in continuous variables. Rubin’s rules were used to pool the results of the final analysis. Further details of the methods have been described in previously published papers [5, 16].
Statistical analysis
Baseline characteristics of patients were analyzed as frequencies and percentages for categorical variables and as medians and interquartile ranges (IQRs) for continuous variables.
After multiple imputations we used these datasets to calculate the area-under-the-curve (AUC) for various geriatric variables that were available premorbid to predict 6 month outcome:
-
a)
age of the patient at admission to the ICU
-
b)
the CFS as determined prior to this disease episode.
-
c)
the cumulative CPS score as determined at admission to the ICU
-
d)
the Katz ADL
-
e)
the SOFA-score at admission to the ICU
All analyses were performed with R software, version 3.2.2 (R Foundation for Statistical Computing).
Results
Participants
There were 242 participating ICUs in the 22 European countries including Turkey. The characteristics of these ICUs are listed in the electronic Additional file and recruitment per country is presented in Additional file 1.
A total of 3920 patients were enrolled in the VIP2 study. The demographics of these patients are shown in Tables 1 and 2. The median age of participants was 84 years (IQR 81–86), 53% were male, the median number of chronic comorbidities was 4 (IQR 3–4) and the median number of different medications taken daily was 6 (IQR 4–9). This resulted in a median CPS of 10 (IQR 7–14). 61% of patients had a CFS > 3, meaning that they were either pre-frail or frail at the time of ICU admission. The median SOFA score was 6 (IQR 6–9).
During their stay in the ICU, 1191 patients (30.9%) died, a further 436 patients (11.1%) died after discharge from the ICU but within the first 30 days of admission, and a further 895 patients died afterwards but within the first 6 months of admission (22.8%). After 6 months, 64% of patients had died. The characteristics of the surviving patients are shown in Table 2. These figures are derived from the complete data set.
Patients who survived up to 6 months were slightly younger (median age of survivors 84, IQR 81–86) than those who died within the first 6 months (median age 84, IQR 82–87, p = 0.013), less likely to be frail (CFS > 5 in 19% versus 34%, p < 0.01) and less dependent on their Katz ADL (median Katz score 6, IQR 5–6 versus 6 points, IQR 3–6, p < 0.01).
Outcome data
The relationship between the geriatric variables available before the current period of illness (premorbid) and the scores for the predictability of death in the first 6 months after ICU admission is shown in Fig. 1. The C-statistic (area under the curve of the sensitivity and specificity calculations) varies over time. The full model consisting of all variables (age, SOFA score, frailty, CPS and Katz) had the highest AUC for the outcome of death at 6 months. Note that the AUC for frailty associated with death at 6 months had an upward slope. After 12 days in the ICU, CFS on admission has a higher C-statistic for 6 month mortality than SOFA score on admission.
Predictive value of various patients characteristics on 6 month mortality expressed by the area-under-the-curve over time. The SOFA score has the highest association with mortality in the first 6 days after admission to the ICU for an acute reason (pink line and confidence interval). However, after approximately 12 days the AUC of the CFS (brown line) was higher than the AUC of the SOFA-score, which means that CFS, from that point onwards, is more associated with 6 month outcome. The blue line with the highest AUC is all variables combined (age, CFS, CPS, Katz and SOFA)
Discussion
We have shown that the 6 month survival rate for patients aged 80 years and older after acute admission to the ICU is 36%. Survival up to 6 months depends on several factors, which can be divided into factors associated with severity of illness (SOFA score) or factors that are patient-dependent (such as age, frailty, cognitive function and independence in activities of daily living). Severity can be modified by treatments administered in the ICU, but premorbid patient characteristics are fixed and cannot be modified by interventions in such acute settings.
In this study, we showed that when patients aged ≥ 80 years who were acutely admitted to the ICU were alive for more than 12 days, the Clinical Frailty Scale (CFS) model outperformed the SOFA score model and the age-based model in predicting 6 month mortality. Therefore, for patients who have survived their acute critical illness (the severity of illness associated with the reason for admission, e.g. trauma or infection), long-term survival is now more dependent on their ability to fully recover. Obviously, this is inversely related to the level of comorbidity and frailty of the patient.
The impact of frailty on 6 month mortality increases over time (represented by the increasing C-statistic during the 30 days in the ICU). Frailty, defined as CFS 6–9, was associated with 6 month survival of 31.9%, compared with 53.9% for fit patients (CFS 1–3) and 47.4% for frail patients (CFS 4–5) (p < 0.01). Frailty is associated with an inability to cope with the physical stress associated with acute critical illness. Once the acute effects of the illness have subsided, the patient is left with further organ damage that they are unable to cope with. This results in very high mortality rates during and after ICU treatment.
In shared decision making with patients or their families, one of the key questions is: "What are the long-term chances of being alive? This question is particularly important for adult patients aged 80 and over. Their chances of long-term survival are already limited because of their advanced age. In addition, their chances of survival decrease significantly if they require acute hospitalisation for a serious illness [4]. Here we have shown an overall survival of 36% after 6 months. This low survival in the first 6 months after ICU admission is in line with previous publications [17,18,19,20,21] and remains higher than in an age- and sex-matched population in the first year after ICU discharge [22].
We have also shown that long-term survival is inversely associated with pre-morbid conditions (age and frailty) and the severity of illness at admission. Unfortunately, many of these variables are not amenable to intervention. As frustrating as this may be, it also shows that we can inform our patients (or, more likely, surrogate decision makers) about possible outcomes early in the course of the disease. While it is impossible to predict complete futility of treatment, we can explain to surrogate decision makers what a patient's chances are based on their premorbid conditions [23]. Such information is of paramount importance in shared decision making. Interestingly, cognitive impairment and age alone were only weakly associated with 6 month survival.
Limitation of this study
Older patients discharged from the ICU often have lower functional capacity and independence than before admission to the ICU. In a cohort of 610 Canadian patients aged ≥ 80 years admitted to an ICU, only 26% were alive at 12 months and had recovered their baseline physical function [24]. This is particularly important as many older patients prioritise quality of life over longevity [7]. Indeed, the majority of patients (74%) reported that they would not choose treatment if the burden of that treatment was high and the expected outcome was survival with severe functional impairment [25, 26]. When community-dwelling older people (average age 85 years) were well informed about potential ICU treatments by watching videos of what this treatment would actually look like, many chose not to undergo such treatments [26]. This clearly shows that survival alone is not enough to fully inform patients or surrogate decision makers. Estimated quality of life, functional independence and autonomy may be more important in this age group. These outcomes are missing from our study and are a major limitation.
Another limitation could be ‘admission bias’; we did not record the reasons or outcomes of patients who were refused ICU admission. Therefore, we may be looking at a selected population that may have a better outcome than all patients aged 80 and over.
Another limitation of our study is that “advanced directives” and/or “restrictions on life-sustaining treatment” can have a huge impact on outcome. Here we see a self-fulfilling prophecy. We see reduced survival in patients for whom physicians expect limited survival and have discussed limitations on life-sustaining treatments. We have previously reported that frail patients have more restrictions on life-sustaining treatments [15].
Another limitation is that 6 month survival data were not available for all patients. We cannot exclude that patients with missing 6 month survival data were different from those included in the study.
Finally, we did not collect information on other explanatory variables, such as individual socio-economic status, education, nutritional status, lack of delirium assessment on admission and severity of illness later during the ICU stay. These variables are important for future research.
Strong feature of this study
A strong feature of this study is that we prospectively examined outcomes in a well-defined group of consecutive, acutely admitted, elderly patients over 80 years of age in 20 European countries. The results are, therefore, valid for a large proportion of these older patients (external validity).
Conclusions
We found that geriatric conditions that were present before a patient's acute illness (so-called premorbid conditions) were associated with the likelihood of survival. Apart from the SOFA score, which reflects acute illness, the Clinical Frailty Scale and age were independent prognostic factors for 6 month mortality after ICU admission in patients aged 80 years and older. The addition of other geriatric syndromes and scores did not improve this association with mortality. Knowledge of these premorbid conditions is important information that can be used to guide decisions about both the benefits of ICU admission and the benefits of continued ICU treatment as part of the shared decision-making process with the patient, family, or surrogate decision-makers.
Availability of the data and materials
The data sets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CFS:
-
Clinical frailty scale
- CPS:
-
Comorbidity and polypharmacy score
- ICU:
-
Intensive care unit
- IQCODE:
-
Informant questionnaire on cognitive decline in the elderly
- SOFA:
-
Sequential organ failure assessment
References
Laake JH, Dybwik K, Flaatten HK, Fonneland IL, Kvåle R, Strand K. Impact of the post-World War II generation on intensive care needs in Norway. Acta Anaesthesiol Scand. 2010;54(4):479–84.
Haas LE, Karakus A, Holman R, Cihangir S, Reidinga AC, de Keizer NF. Trends in hospital and intensive care admissions in the Netherlands attributable to the very ƒ in an ageing population. Crit Care. 2015;19:353. https://doi.org/10.1186/s13054-015-1061-z.
Bagshaw SM, Webb SA, Delaney A, et al. Very old patients admitted to intensive care in Australia and New Zealand: a multi-centre cohort analysis. Crit Care. 2009;13:R45.
Jung C, Wernly B, Muessig JM, Kelm M, Boumendil A, Morandi A, et al. A comparison of very old patients admitted to intensive care unit after acute versus elective surgery or intervention. J Crit Care. 2019;52:141–8.
Flaatten H, de Lange DW, Morandi A, Andersen F, Artigas A, Bertolini G, et al. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years). Intensive Care Med. 2017;43:1820–8. https://doi.org/10.1007/s00134-017-4940-8.
Guidet B, de Lange DW, Boumendil A, Leaver S, Watson X, Boulanger C, et al. The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med. 2019;43(1):217.
Heyland DK, Dodek P, Mehta S, Cook D, Garland A, Stelfox HT, Day AG. Admission of the very elderly to the intensive care unit: family members’ perspectives on clinical decision-making from a multicenter cohort study. Palliat Med. 2015;29(4):324–35. https://doi.org/10.1177/0269216314566060.
Yu WC, Chou MY, Pen LN, Lin YT, Liang CK, Chen LK. Synergistic effects of cognitive impairment on physical disability in all-cause mortality among men aged 80 years and over: results from longitudinal older veterans study. PLoS ONE. 2017;12:e0181741. https://doi.org/10.1371/journal.pone.0181741.
Level C, Tellier E, Dezou P, Chaoui K, Kherchache A, Sejourné P, Rullion-Pac Soo AM. Outcome of older persons admitted to intensive care unit, mortality, prognosis factors, dependency scores and ability trajectory within 1 year: a prospective cohort study. Aging Clin Exp Res. 2018;30:1041–51. https://doi.org/10.1007/s40520-017-0871-z.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–95. https://doi.org/10.1503/cmaj.050051.
Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983;31:721–7. https://doi.org/10.1111/j.1532-5415.1983.tb03391.x.
Quinn TJ, Fearon P, Noel-Storr AH, Young C, McShane R, Stott DJ. Informant questionnaire on cognitive decline in the elderly (IQCODE) for the diagnosis of dementia within community dwelling populations. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.CD010079.pub2.
Evans DC, Cook CH, Christy JM, Murphy CV, Gerlach AT, Eiferman D, et al. Comorbidity-polypharmacy scoring facilitates outcome prediction in older trauma patients. J Am Geriatr Soc. 2012;60:1465–70. https://doi.org/10.1111/j.1532-5415.2012.04075.x.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG. The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the ESICM. Intensive Care Med. 1996;22:707–10.
Guidet B, Flaatten H, Boumendil A, et al. Withholding or withdrawing of life-sustaining therapy in older adults (≥ 80 years) admitted to the intensive care unit. Intensive Care Med. 2018;44:1027–38. https://doi.org/10.1007/s00134-018-5196-7.
Soliman IW, Frencken JF, Peelen LM, Slooter AJ, Cremer OL, van Delden JJ, van Dijk D, de Lange DW. The predictive value of early acute kidney injury for long-term survival and quality of life of critically ill patients. Crit Care. 2016;20(1):242. https://doi.org/10.1186/s13054-016-1416-0.PMID:27488839;PMCID:PMC4973091.
Andersen FH, Flaatten H, Klepstad P, Follestad T, Strand K, Krüger AJ, Hahn M, Buskop C, Rime AK, Kvåle R. Long-term outcomes after ICU admission triage in octogenarians. Crit Care Med. 2017;45(4):e363–71. https://doi.org/10.1097/CCM.0000000000002098.
Guidet B, Leblanc G, Simon T, Woimant M, Quenot JP, Ganansia O, Maignan M, Yordanov Y, Delerme S, Doumenc B, Fartoukh M, Charestan P, Trognon P, Galichon B, Javaud N, Patzak A, Garrouste-Orgeas M, Thomas C, Azerad S, Pateron D, Boumendil A, Network I-CS. Effect of systematic intensive care unit triage on long-term mortality among critically ill elderly patients in France: a randomized clinical trial. JAMA. 2017;318:1450–9.
Kim DY, Lee MH, Lee SY, Yang BR, Kim HA. Survival rates following medical intensive care unit admission from 2003 to 2013. Medicine. 2019;98(37):e17090.
Boumendil A, Latouche A, Guidet B. On the benefit of intensive care for very old patients. Arch Intern Med. 2011;171(12):1116–7. https://doi.org/10.1001/archinternmed.2011.102.
Schrøder MA, Poulsen JB, Perner A. Acceptable long-term outcome in elderly intensive care unit patients. Dan Med Bull. 2011;58(7):A4297.
Andersen FH, Flaatten H, Klepstad P, et al. Long-term survival and quality of life after intensive care for patients 80 years of age or older. Ann Inten Care. 2015;5:13. https://doi.org/10.1186/s13613-015-0053-0.
de Lange DW, Brinkman S, Flaatten H, Boumendil A, Morandi A, Andersen FH, et al. Cumulative prognostic score predicting mortality in patients older than 80 years admitted to the ICU. J Am Geriatr Soc. 2019;67(6):1263–7.
Heyland DK, Garland A, Bagshaw SM, et al. Recovery after critical illness in patients aged 80 years or older: a multi-center prospective observational cohort study. Inten Care Med. 2015;41:1911–20.
Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. New Engl J Med. 2002;346:1061–6.
de Rooij SE, Abu-Hanna A, Levi M, de Jonge E. Factors that predict outcome of intensive care treatment in very elderly patients: a review. Crit Care. 2005;9:R307–14.
Acknowledgements
The researchers that have participated in the study and should be acknowledged are named in the Acknowledgments. DRC Ile de France and URC Est helped conducting VIP2 in France. The VIP2-study collaborators are listed in the Acknowledgments.
other contributors to the VIP-2 study are named in the list contributors—Michael Joannidis, Philipp Eller, Raimund Helbok, René Schmutz, Joke Nollet, Nikolaas de Neve, Pieter De Buysscher, Sandra Oeyen, Walter Swinnen, Marijana Mikačić, Anders Bastiansen, Andreas Husted, Bård E. S. Dahle, Christine Cramer, Christoffer Sølling, Dorthe Ørsnes Christensen, Jakob Edelberg Thomsen, Jonas Juul Pedersen, Mathilde Hummelmose Enevoldsen, Thomas Elkmann, Agnieszka Kubisz-Pudelko, Alan Pope, Amy Collins, Ashok S. Raj, Carole Boulanger, Christian Frey, Ciaran Hart, Clare Bolger, Dominic Spray, Georgina Randell, Helder Filipe, Ingeborg D. Welters, Irina Grecu, Jane Evans, Jason Cupitt, Jenny Lord, Jeremy Henning, Joanne Jones, Jonathan Ball, Julie North, Kiran Salaunkey, Laura Ortiz-Ruiz De Gordoa, Louise Bell, Madhu Balasubramaniam, Marcela Vizcaychipi, Maria Faulkner, McDonald Mupudzi, Megan Lea-Hagerty, Michael Reay, Michael Spivey, Nicholas Love, Nick Spittle Nick Spittle, Nigel White, Patricia Williams, Patrick Morgan, Phillipa Wakefield, Rachel Savine, Reni Jacob, Richard Innes, Ritoo Kapoor, Sally Humphreys, Steve Rose, Susan Dowling, Susannah Leaver, Tarkeshwari Mane, Tom Lawton, Vongayi Ogbeide, Waqas Khaliq, Yolanda Baird, Antoine Romen, Arnaud Galbois, Bertrand Guidet, Christophe Vinsonneau, Cyril Charron, Didier Thevenin, Emmanuel Guerot, Guillaume Besch, Guillaume Savary, Hervé Mentec, Jean-Luc Chagnon, Jean-Philippe Rigaud, Jean-Pierre Quenot, Jeremy Castaneray, Jérémy Rosman, Julien Maizel, Kelly Tiercelet, Lucie Vettoretti, Maud Mousset Hovaere, Messika Messika, Michel Djibré, Nathalie Rolin, Philippe Burtin, Pierre Garcon, Saad Nseir, Xavier Valette, Christian Rabe, Eberhard Barth, Henning Ebelt, Kristina Fuest, Marcus Franz, Michael Horacek, Michael Schuster, Patrick Meybohm, Raphael Romano Bruno, Sebastian Allgäuer, Simon Dubler, Stefan J Schaller, Stefan Schering, Stephan Steiner, Thorben Dieck, Tim Rahmel, Tobias Graf, Anastasia Koutsikou, Aristeidis Vakalos, Bogdan Raitsiou, Elli Niki Flioni, Evangelia Neou, Fotios Tsimpoukas, Georgios Papathanakos, Giorgos Marinakis, Ioannis Koutsodimitropoulos, Kounougeri Aikaterini, Nikoletta Rovina, Stylliani Kourelea, Tasioudis Polychronis, Vasiiios Zidianakis, Vryza Konstantinia, Zoi Aidoni, Brian Marsh, Catherine Motherway, Chris Read, Ignacio Martin-Loeches, Andrea Neville Cracchiolo, Aristide Morigi, Italo Calamai, Stefania Brusa, Ahmed Elhadi, Ahmed Tarek, Ala Khaled, Hazem Ahmed, Wesal Ali Belkhair, Alexander D. Cornet, Diederik Gommers, Dylan de Lange, Eva van Boven, Jasper Haringman, Lenneke Haas, Lettie van den Berg, Oscar Hoiting, Peter de Jager, Rik T. Gerritsen, Tom Dormans, Willem Dieperink, Alena Breidablik Alena Breidablik, Anita Slapgard, Anne-Karin Rime, Bente Jannestad, Britt Sjøbøe, Eva Rice, Finn H. Andersen, Hans Frank Strietzel, Jan Peter Jensen, Jørund Langørgen, Kirsti Tøien, Kristian Strand, Michael Hahn, Pål Klepstad, Aleksandra Biernacka, Anna Kluzik, Bartosz Kudlinski, Dariusz Maciejewski, Dorota Studzińska, Hubert Hymczak, Jan Stefaniak, Joanna Solek-Pastuszka, Joanna Zorska, Katarzyna Cwyl, Lukasz J. Krzych, Maciej Zukowski, Małgorzata Lipińska-Gediga, Marek Pietruszko, Mariusz Piechota, Marta Serwa, Miroslaw Czuczwar, Mirosław Ziętkiewicz, Natalia Kozera, Paweł Nasiłowski, Paweł Sendur, Paweł Zatorski, Piotr Galkin, Ryszard Gawda, Urszula Kościuczuk, Waldemar Cyrankiewicz, Wojciech Gola, Alexandre Fernandes Pinto, Ana Margarida Fernandes, Ana Rita Santos, Cristina Sousa, Inês Barros, Isabel Amorim Ferreira, Jacobo Bacariza Blanco, João Teles Carvalho, Jose Maia, Nuno Candeias, Nuno Catorze, Vladislav Belskiy, Africa Lores, Angela Prado Mira, Catia Cilloniz, David Perez-Torres, Emilio Maseda, Enver Rodriguez, Estefania Prol-Silva, Gaspar Eixarch, Gemma Gomà, Gerardo Aguilar, Gonzalo Navarro Velasco, Marián Irazábal Jaimes, Mercedes Ibarz Villamayor, Noemí Llamas Fernández, Patricia Jimeno Cubero, Sonia López-Cuenca, Teresa Tomasa, Anders Sjöqvist, Camilla Brorsson, Fredrik Schiöler, Henrik Westberg, Jessica Nauska, Joakim Sivik, Johan Berkius, Karin Kleiven Thiringer, Lina De Geer, Sten Walther, Filippo Boroli, Joerg C. Schefold, Leila Hergafi, Philippe Eckert, Ismail Yıldız, Ihor Yovenko, Yuriy Nalapko, Yuriy Nalapko, Richard Pugh
Funding
None.
Author information
Authors and Affiliations
Consortia
Contributions
BG, DDL, HF designed the study; IWS and AB performed the statistical analysis; JF run the database and the eCRF; BG, DDL, HF, IWS and AB drafted the manuscript; AM provided geriatric expertise in designing the protocol. All other authors were country coordinators and validated the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Each country had a national coordinator responsible for securing the required ethical and regulatory approvals. A waiver of informed consent for participation in the study was granted in some countries.
Consent fort publication
Not applicable.
Competing interests
Joerg C. Schefold declares that the Dept. of Intensive Care Medicine Bern has/had research and/or development/consulting contracts with (full disclosure): Orion Corporation, Abbott Nutrition International, B. Braun Medical AG, CSEM SA, Edwards Lifesciences Services GmbH/SA, Kenta Biotech Ltd, Maquet Critical Care AB, Omnicare Clinical Research AG, and Nestlé. Educational grants were received from Fresenius Kabi; GSK; MSD; Lilly; Baxter; Astellas; AstraZeneca; B. Braun Medical AG, CSL Behring, Maquet, Novartis, Covidien, Nycomed, Pierre Fabre Pharma (Roba Pharma); Pfizer, Orion Pharma. The money went into departmental funds. No personal financial gain applies. All other authors do not have any conflict of interest to declare related to this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Participating ICUs and countries.
Additional file 2.
Inclusion period: number of patients included per week.
Additional file 3.
Recorded study variables.
Additional file 4.
Clinical frailty scale (CFS).
Additional file 5.
Katz activity of daily living (ADL).
Additional file 6.
Cognitive decline questionnaire (IQCODE).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Lange, D.W., Soliman, I.W., Leaver, S. et al. The association of premorbid conditions with 6-month mortality in acutely admitted ICU patients over 80 years. Ann. Intensive Care 14, 46 (2024). https://doi.org/10.1186/s13613-024-01246-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-024-01246-w