Abstract
Background
Capillary refill time (CRT) may improve more rapidly than lactate in response to increments in systemic flow. Therefore, it can be assessed more frequently during septic shock (SS) resuscitation. Hyperlactatemia, in contrast, exhibits a slower recovery in SS survivors, probably explained by the delayed resolution of non-hypoperfusion-related sources. Thus, targeting lactate normalization may be associated with impaired outcomes. The ANDROMEDA-SHOCK trial compared CRT- versus lactate-targeted resuscitation in early SS. CRT-targeted resuscitation associated with lower mortality and organ dysfunction; mechanisms were not investigated. CRT was assessed every 30 min and lactate every 2 h during the 8-h intervention period, allowing a first comparison between groups at 2 h (T2). Our primary aim was to determine if SS patients evolving with normal CRT at T2 after randomization (T0) exhibited a higher mortality and organ dysfunction when allocated to the LT arm than when randomized to the CRT arm. Our secondary aim was to determine if those patients with normal CRT at T2 had received more therapeutic interventions when randomized to the LT arm. To address these issues, we performed a post hoc analysis of the ANDROMEDA-SHOCK dataset.
Results
Patients randomized to the lactate arm at T0, evolving with normal CRT at T2 exhibited significantly higher mortality than patients with normal CRT at T2 initially allocated to CRT (40 vs 23%, p = 0.009). These results replicated at T8 and T24. LT arm received significantly more resuscitative interventions (fluid boluses: 1000[500–2000] vs. 500[0–1500], p = 0.004; norepinephrine test in previously hypertensive patients: 43 (35) vs. 19 (19), p = 0.001; and inodilators: 16 (13) vs. 3 (3), p = 0.003). A multivariate logistic regression of patients with normal CRT at T2, including APACHE-II, baseline lactate, cumulative fluids administered since emergency admission, source of infection, and randomization group) confirmed that allocation to LT group was a statistically significant determinant of 28-day mortality (OR 3.3; 95%CI[1.5–7.1]); p = 0.003).
Conclusions
Septic shock patients with normal CRT at baseline received more therapeutic interventions and presented more organ dysfunction when allocated to the lactate group. This could associate with worse outcomes.
Similar content being viewed by others
Background
ANDROMEDA-SHOCK was a randomized controlled trial comparing capillary refill time (CRT)- versus lactate-targeted (LT) resuscitation in early septic shock [1], that suggested a lower mortality, and demonstrated significantly less organ dysfunction and treatment intensity in the CRT group. A subsequent Bayesian post hoc analysis supported the survival benefit of a CRT-targeted resuscitation [2].
CRT is a flow-sensitive variable that may improve rapidly after an increase in systemic blood flow [3,4,5,6]. Therefore, it can be assessed more frequently, and resuscitation could be stopped earlier than when a lactate endpoint is pursued; indeed, lactate exhibits a slow kinetics of recovery even in septic shock survivors [7, 8]. CRT was the first perfusion variable to reach a significant improvement 2 h after ICU-based resuscitation [3], and 70% of septic shock survivors exhibited a normal CRT at 2 h[7]. A normal CRT at 2 h after initial or advanced fluid resuscitation was associated with less than 15% mortality risk [3, 4]. Moreover, in a previous pilot study, fluid resuscitation could be safely withheld in septic shock patients with normalized peripheral perfusion, a fact that was associated with less organ dysfunction [9]. In ANDROMEDA-SHOCK, CRT was assessed every 30 min and lactate every 2 h during the intervention period of 8 h [10, 11]. Accordingly, and considering the published evidence, the first time-point where the impact of resuscitation could be compared between study arms was as early as at 2 h (T2). Besides, the status of CRT at 2 h could have prognostic value and aid to take decisions on further resuscitation [3, 4].
The lower mortality and less organ dysfunction observed in septic shock patients randomized to CRT-targeted resuscitation is significant and deserves further exploration. Eventually, a normal CRT in septic shock patients with hyperlactatemia signals a predominant non-hypoperfusion-related source for lactate where no subsequent and potentially deleterious resuscitation is probably required [5]. In fact, there are several non-hypoxia related alternative explanations for persistent hyperlactatemia [12]. Stress-related hyperlactatemia is triggered by the neurohumoral response to sepsis that generates aerobic lactate production in skeletal muscles via beta-2 epinephrine stimulation. This lactate acts as a metabolic shuttle providing energy to other organs, and this process can be blocked by specific interventions [13, 14]. On the other hand, Tapia et al. demonstrated a severe impairment in exogenous lactate clearance very early after experimental endotoxic shock induction, not related to liver hypoperfusion as demonstrated by several techniques [15]. The authors suggested a metabolic blockade as a potential explanation for this finding.
Our hypothesis was that in SEPSIS-3 septic shock patients evolving with normal CRT at 2 h, the T0 randomization to the LT arm was associated with a higher mortality compared to patients randomized to the CRT arm. Our primary aim was to determine if septic shock patients evolving with normal CRT at T2 exhibited a higher mortality and organ dysfunction after being randomized to the LT arm at T0 than when randomized to the CRT arm. Our secondary aim was to determine if those septic shock patients evolving with normal CRT at T2 received more therapeutic interventions when randomized to the LT arm at T0 than when randomized to the CRT arm.
To address this issue, we performed a post hoc analysis of the ANDROMEDA-SHOCK dataset.
Materials and methods
Data collection and processing
The ANDROMEDA-SHOCK trial patients fulfilled the SEPSIS-3 criteria [16] (i.e., presence of suspected infection accompanying life-threatening organ dysfunction, requirement use of vasopressors to maintain mean arterial pressure (MAP) > 65 mmHg, and lactate levels > 2 mmol/L). Conversely, CRT status was not incorporated as inclusion criteria.
The detailed protocol of ANDROMEDA-SHOCK trial including the stepwise interventional procedures can be found elsewhere [10, 11]. Briefly, during the 8-h intervention period, the goal for the CRT arm was to normalize CRT (normal value ≤ 3 s as assessed with a standardized technique), whereas the goal for the LT arm was to normalize (normal values ≤ 2 mmol/L) or to decrease lactate levels by 20% every 2 h. Following initial fluid resuscitation and norepinephrine (NE) to reach and maintain a mean arterial pressure (MAP) ≥ 65 mm Hg, both groups were managed with an identical sequential protocolized approach. In both groups, the first step was assessment of fluid responsiveness, followed by fluid challenges with 500 ml of crystalloids every 30 min in fluid-responders until the goal was achieved or a central venous pressure safety limit was reached, or the patient became fluid unresponsive, whichever came first. As a second step, a vasopressor test was performed in previously chronic hypertensive patients in whom targets were not achieved with fluids. NE was transiently increased until reaching a MAP of 80 to 85 mmHg followed by a reassessment of CRT or lactate after one or two hours, respectively. If the goal was met, this MAP level was maintained throughout the intervention period. The third step consisted of the use of low dose dobutamine or milrinone. Patients were again reassessed after one or two hours in the CRT and LT group, respectively. If the endpoints were still not met, or a safety issue arose, the inodilator was discontinued.
We examined the relationship between CRT status at 2 h after randomization (T2) with clinical characteristics, interventions, and outcomes, including mortality at 28 days for the whole cohort and according to the study group allocation. Then, we analyzed the impact of the randomization arm in both groups in patients with normal CRT at T2. Finally, we performed the same analysis in lactate target achievers (normalization or 20% decrease) at T2.
The main outcome of this study was all-cause mortality at 28 days. Secondary outcomes included severity scores, like the Acute Physiology and Chronic Health Evaluation (APACHE) II score [17], Charlson index [18], and daily Sequential Organ Failure Assessment (SOFA) [19]. Severity of hemodynamic derangements and intensity of therapy was assessed through the evolution of perfusion variables along time, including lactate, CRT, central venous oxygen saturation (ScvO2), central venous-to-arterial pCO2 gradient (P(cv‑a)CO2) or dCO2), dosage of vasopressors, total amount of fluid boluses and fluid balance.
As therapeutic interventions were guided by a predefined protocol that included a stepwise approach to resolve hypoperfusion, we developed a composite outcome that included each protocol-driven resuscitative step taken by attending physicians. Every 500 ml of fluid bolus, vasopressor test, or inodilator test was considered a resuscitative action with a numerical value of 1, and the cumulative number of actions were summed-up for each patient. Finally, other clinically relevant outcomes were registered, like need for mechanical ventilation (MV), renal replacement therapy (RRT), plus ICU and hospital length of stay.
For variables with non-normal distribution, non-parametric tests were used. Accordingly, descriptive statistics are shown as medians [interquartile range 25–75] or percentages (%). Mann–Whitney U, Kruskal–Wallis, Chi-square, and Fisher’s exact, were used when appropriate. Data was analyzed with Minitab v17 (Minitab Inc, State College, PA) and Graphpad Prism (Graphpad Softwares, La Joya, CA) softwares. Two-tailed p value of < 0.05 was considered as statistically significant.
Results
ANDROMEDA-SHOCK study included 424 patients whose main characteristics are presented in Additional File 1. As previously reported [1], 378 patients had available data at 2 h, so this subset was used for T2 data analysis.
Impact of normal CRT at T2
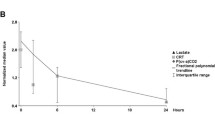
After two hours of protocolized ICU-resuscitation, 49% of patients (184/378) progressed with a normal CRT (Table 1). Regardless of the study group allocation, those patients received less resuscitative interventions, evolved with lower SOFA score at 24 h (7 [4,5,6,7,8,9,10] vs 10 [6,7,8,9,10,11,12,13], p = 0.0001), and exhibited a lower mortality at 28 days (30% vs 46%, p = 0.002) compared to patients with abnormal CRT at T2 (Table 1, Fig. 1, Additional File 2).
Normal CRT and randomization arm at T2
Patients with normal CRT at T2 randomized to the LT arm evolved exhibiting a significantly higher mortality than patients with normal CRT at T2 that were randomized to the CRT group (40 vs 23%, p = 0.009) (Table 2, Figs. 2 and 3). They also received significantly more supportive therapies and resuscitative interventions (fluids, vasopressor and inodilator tests) at the end of the intervention period (Table 2). This difference was mainly driven by patients in the LT group that had not reached their resuscitation endpoint at T2 (44 vs 23%, p = 0.007) (Table 2, Figs. 2 and 3) and was maintained at protocol end at T8 (35 vs 34%, p = 0.055) and at T24 (32 vs 19%, p = 0.02) (Fig. 3). Figure 3 also shows differences between patients who maintained abnormal CRT across timepoints, according to the randomization group.
Patients distribution at 0 and 2 h after ICU admission and associated outcome according to randomization group, under CRT state perspective. Percentages refer to 28-day mortality. All patients started with hyperlactatemia. Lactate arm pursued lactate normalization or significant lowering, irrespective of CRT state. CRT arm pursued CRT normalization
Patients distribution at 0, 2, 8 and 24 h and associated outcome according to randomization group, under CRT perspective. Percentages refer to 28-day mortality. All patients started with hyperlactatemia. Lactate arm pursued lactate normalization or significant lowering, irrespective of CRT state. CRT arm pursued CRT normalization
Moreover, a multivariate logistic regression of patients with normal CRT at T2, including clinically relevant variables at baseline (APACHE-II, baseline lactate, fluids administered since emergency admission until T2, source of infection, and randomization group) confirmed that allocation to the LT study group was a statistically significant determinant of 28 day mortality (OR 3.3; 95%CI[1.5-7.1]); p = 0.003). In the same regression, APACHE II (OR 1.1; 95%CI[1.0-1.2]); p < 0.001) and pulmonary source of infection (OR 4.2; 95%CI[1.7-10.6]; p = 0.002) impacted significantly on mortality at 28 days.
Lactate endpoint achievement and randomization arm at T2
Patients with normal or 20% reduction on lactate at T2, exhibited no statistically significant difference in mortality (25 vs 33%, p = 0.4), APACHE-II score (20 [17,18,19,20,21,22,23,24,25,26,27] vs 19 [16,17,18,19,20,21,22,23,24,25], p = 0.6), and resuscitative interventions (2 [1,2,3,4] vs 2 [1,2,3,4], p = 0.85), when compared by randomization arm.
Discussion
Our results suggest that septic shock patients exhibiting normal peripheral perfusion early after starting protocolized resuscitation could present worse outcomes when treated with a lactate-targeted strategy. In fact, in this post hoc analysis, these patients presented higher mortality, received more interventions such as fluids or vasoactive agents, and evolved with a slower decrease in organ dysfunction scores when compared to those treated with a CRT-targeted resuscitation strategy.
Current Surviving Sepsis Campaign (SSC) guidelines recommend targeting normalization of lactate during septic shock resuscitation [20]. However, this recommendation does not consider that there are multiple pathogenic mechanisms involved in persistent hyperlactatemia, and that a relatively high proportion appears to be non-hypoperfusion-related [12, 21]. A previous retrospective proof-of-concept study showed that septic shock patients with hyperlactatemia but without a hypoperfusion context, as demonstrated by concomitant normal ScvO2, dCO2 or CRT, tended to exhibit lower mortality and to require less therapeutic interventions [5]. In this sense, our results confirm the safety of withholding further resuscitation in septic shock patients with normal CRT. Moreover, and on the contrary, pursuing lactate as a therapeutic target in septic shock patients without a hypoperfusion context appears as deleterious, as this practice was associated with more interventions and higher mortality.
Septic shock patients present with hypotension and hypoperfusion, and are resuscitated in general, with rapid fluid loading and goal-directed endpoints [20, 22]. After the acute period, however, they frequently display net positive fluid balance [22, 23] and although fluid administration practices are highly variable worldwide [24], fluid overload is still a clinical problem [25]. The importance of fluid overload and fluid balance cannot be underestimated since it is a key determinant of higher morbidity and mortality in critically ill patients [22, 25,26,27,28,29,30]. According to our results, it seems that after very early protocolized resuscitation, the selected target determines the intensity of further resuscitation. Indeed, patients with normal CRT at 2 h but randomized to LT resuscitation received more fluid boluses.
In addition, per design, these patients were subjected to more protocol-loop routing and supportive therapies, eventually increasing the burden of over-resuscitation [27, 30,31,32]. It may be highlighted that patients randomized to the LT arm evolving with normal CRT were also exposed to more vasopressor and inodilator tests to achieve the lactate’s goal. Indeed, although previously hypertensive patients may benefit from higher MAP goals, the obligatory increase in NE dose to achieve this level has been associated with increased risk of arrhythmias [33]. The negative impact of excessive catecholamine support in septic shock has been suggested [34] and sparing of these drugs may have also contributed to the improved outcome in the CRT arm. This possible explanation should be clarified by further studies.
A cautionary note must be introduced here since at T0, patients with normal CRT randomized to the LT arm did not demonstrate overall a significantly higher mortality compared to those randomized to CRT. This may argue against the concept of the excess mortality related to an excess of resuscitative interventions, as patients in CRT with normal CRT should have received less interventions than patients with normal CRT in high lactate group. Also, the normal CRT group in the LT arm increased their mortality from 30 to 40% from T0 to T2 probably due to patients with abnormal CRT at baseline who normalized their CRT. Per protocol, these patients should have received some resuscitative interventions, even if they had been randomized to the CRT arm instead of the LT one. This finding may argue against the postulate that some excess in mortality was undoubtedly related to excess on interventions in the LT group, since in both groups they should have been similar. Other factors may have played a role, as randomization was not stratified to CRT values at baseline and subgroups with normal CRT in the LT arm may have been more severe than the subgroup with normal CRT in the CRT group.
The present study presents some insights in trying to understand the outcome differences suggested by the original ANDROMEDA-SHOCK trial report [1] and the Bayesian reanalysis of the same data [2]. Peripheral perfusion normalization may be a better resuscitation endpoint than lactate. Indeed, as patients did not differ on baseline demographics, previous fluids administration, sepsis sources or severity indices, the randomization to the group pursuing a lactate target could have determined a higher risk of death.
The clinical implications of these findings can only be expressed as hypothesis-generating ideas at this point: First, the selected resuscitation target may strongly influence the intensity of treatment with fluids or vasoactive agents since potential targets such as CRT or lactate are not equivalent in this aspect. Second, our results confirm the findings of a previous pilot study concerning the safety of withholding fluid resuscitation in septic shock patients with normal CRT [9], even though they had not cleared hyperlactatemia. Third, our data also validate the concept of non-hypoperfusion-related hyperlactatemia as suggested by previous observational studies [5, 7]. This condition might represent a less severe sepsis-related acute circulatory dysfunction that could be treated more conservatively. Fourth, pursuing lactate as a target without considering the state of peripheral perfusion might be potentially deleterious. In consequence, further resuscitation steps should be cautiously considered and on an individual basis in patients with septic shock that have already normalized CRT. Finally, the design of future randomized controlled studies on the best resuscitation target for septic shock should consider potential clinical phenotypes derived from a multimodal perfusion monitoring, a fact that deserves further research.
Limitations
This study has some limitations. First, it is a post hoc analysis of an original study with a different design. Therefore, the suggestion that septic shock patients with a normal CRT could have a higher mortality when pursuing lactate normalization as a target is only hypothesis-generating. Second, CRT is not a perfect perfusion marker tool since there is inter-rater variability [35] that demands training and standardization. It could be difficult to apply in some clinical scenarios as hypothermia, surgery, vasculitis, etc. Novel techniques to further standardize CRT measurement have been recently proposed [36, 37] and should be tested in proper scenarios.
Conclusions
Septic shock patients with normal CRT at baseline received more therapeutic interventions and presented more organ dysfunction when allocated to the lactate group. This could associate with worse outcomes.
Abbreviations
- CRT:
-
Capillary refill time
- LT:
-
Lactate-targeted
- ICU:
-
Intensive care unit
- MAP:
-
Mean arterial pressure
- T0:
-
0-hours
- T2:
-
2-hours
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- SOFA:
-
Sequential Organ Failure Assessment
- ScvO2:
-
Central venous oxygen saturation
- delta pCO2:
-
Central venous–arterial pCO2 gradients
- MV:
-
Mechanical ventilation
- RRT:
-
Renal replacement therapy
- SSC:
-
Surviving Sepsis Campaign
References
Hernandez G, Ospina-Tascon G, Petri Damiani L, Estenssoro E, Dubin A, Hurtado J, et al. Effect of a resuscitation strategy targeting peripheral perfusion status vs serum lactate levels on 28-day mortality among patients with septic shock The ANDROMEDA-SHOCK Randomized Clinical Trial. JAMA. 2019;321:654–64.
Zampieri FG, Damiani LP, Bakker J, Ospina-Tascón GA, Castro R, Cavalcanti AB, et al. Effect of a resuscitation strategy targeting peripheral perfusion status vs serum lactate levels on 28-day mortality among patients with septic shock: a bayesian reanalysis of the ANDROMEDA-SHOCK Trial. Am J Respir Crit Care Med. 2019. https://doi.org/10.1164/rccm.201905-0968OC.
Hernandez G, Pedreros C, Veas E, Bruhn A, Romero C, Rovegno M, et al. Evolution of peripheral vs metabolic perfusion parameters during septic shock resuscitation a clinical-physiologic study. J Crit Care. 2012;27:283–8.
Lara B, Enberg L, Ortega M, Leon P, Kripper C, Aguilera P, et al. Capillary refill time during fluid resuscitation in patients with sepsis-related hyperlactatemia at the emergency department is related to mortality. PLoS ONE. 2017;12:e0188548.
Alegría L, Vera M, Dreyse J, Castro R, Carpio D, Henriquez C, et al. A hypoperfusion context may aid to interpret hyperlactatemia in sepsis-3 septic shock patients: a proof-of-concept study. Ann Intensive Care. 2017;7:29.
JacquetLagrèze M, Bouhamri N, Portran P, Schweizer R, Baudin F, Lilot M, et al. Capillary refill time variation induced by passive leg raising predicts capillary refill time response to volume expansion. Crit Care. 2019;23:281.
Hernandez G, Luengo C, Bruhn A, Kattan E, Friedman G, OspinaTascon G, et al. When to stop septic shock resuscitation: clues from a dynamic perfusion monitoring. Ann Intensive Care. 2014;4:30.
Bakker J, de Backer D, Hernandez G. Lactate-guided resuscitation saves lives: we are not sure. Intensive Care Med. 2016;42:472–4.
van Genderen ME, Engels N, van der Valk RJP, Lima A, Klijn E, Bakker J, et al. Early peripheral perfusion–guided fluid therapy in patients with septic shock. Am J Respir Crit Care Med. 2015;191:477–80.
Hernández G, Cavalcanti AB, Ospina-Tascón G, Zampieri FG, Dubin A, Hurtado FJ, et al. Early goal-directed therapy using a physiological holistic view: the ANDROMEDA-SHOCK—a randomized controlled trial. Ann Intensive Care. 2018;8:52.
Hernández G, Cavalcanti AB, Ospina-Tascón G, Dubin A, Hurtado FJ, Damiani LP, et al. Statistical analysis plan for early goal-directed therapy using a physiological holistic view–The andromeda-shock: a randomized controlled trial. Rev Bras Ter Intensiva. 2018;30:253–63.
Hernandez G, Bellomo R, Bakker J. The ten pitfalls of lactate clearance in sepsis. Intensive Care Med. 2019;45:82–5.
Levy B, Perez P, Gibot S, Gerard A. Increased muscle-to-serum lactate gradient predicts progression towards septic shock in septic patients. Intensive Care Med. 2010;36:1703–9.
Levy B, Gibot S, Franck P, Cravoisy A, Bollaert PE. Relation between muscle Na + K + ATPase activity and raised lactate concentrations in septic shock: a prospective study. Lancet. 2005;365:871–5.
Tapia P, Soto D, Bruhn A, Alegría L, Jarufe N, Luengo C, et al. Impairment of exogenous lactate clearance in experimental hyperdynamic septic shock is not related to total liver hypoperfusion. Crit Care. 2015;19:188.
Singer M, Deustchman C, Warren Seymour C, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–10.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis England. 1987;40:373–83.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22:707–10.
Rhodes A, Evans L, Alhazzani W, Levy M, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Crit Care Med. 2017;45:486–552.
Hernandez G, Bruhn A, Castro R, Regueira T. The holistic view on perfusion monitoring in septic shock. Curr Opin Crit Care. 2012;18:280–6.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early-goal directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77.
Li D, Wang X, Liu D. Association between elevated central venous pressure and outcomes in critically ill patients. Ann Intensive Care. 2017;7:83.
Cecconi M, Hofer C, Teboul JL, Pettila V, Wilkman E, Molnar Z, et al. Fluid challenges in intensive care: the FENICE study: a global inception cohort study. Intensive Care Med. 2015;41:1529–37.
Malbrain MLNG, Chiumello D, Pelosi P, Bihari D, Innes R, Ranieri VM, et al. Incidence and prognosis of intraabdominal hypertension in a mixed population of critically ill patients: a multiple-center epidemiological study. Crit Care Med. 2005;33:315–22.
Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, DeBoisblanc B, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–75.
Bagshaw SM, Brophy PD, Cruz D, Ronco C. Fluid balance as a biomarker : impact of fluid overload on outcome in critically ill patients with acute kidney injury. Crit Care. 2008;12:1–3.
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, et al. Consensus on circulatory shock and hemodynamic monitoring Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40:1795–815.
Dres M, Teboul JL, Anguel N, Guerin L, Richard C, Monnet X. Passive leg raising performed before a spontaneous breathing trial predicts weaning-induced cardiac dysfunction. Intensive Care Med. 2015;41:487–94.
Payen D, de Pont AC, Sakr Y, Spies C, Reinhart K, Vincent JL. A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit Care. 2008;12:1–7.
Malbrain MLNG, Van Regenmortel N, Saugel B, De Tavernier B, Van Gaal PJ, Joannes-Boyau O, et al. Principles of fluid management and stewardship in septic shock: it is time to consider the four D’s and the four phases of fluid therapy. Ann Intensive Care. 2018;8:66.
Boyd JH, Forbes J, Nakada TA, Walley KR, Russell JA, Frcp C, et al. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med. 2011;39:259–65.
Asfar P, Meziani F, Hamel J-F, Grelon F, Megarbane B, Anguel N, et al. High versus Low blood-pressure target in patients with septic shock. N Engl J Med. 2014;370:1583–93.
Lesur O, Delile E, Asfar P, Radermacher P. Hemodynamic support in the early phase of septic shock: a review of challenges and unanswered questions. Ann Intensive Care. Springer International Publishing; 2018;8.
Valenzuela Espinoza ED, Welsh S, Dubin A. Lack of agreement between different observers and methods in the measurement of capillary refill time in healthy volunteers: an observational study. Rev Bras Ter Intensiva. 2014;26:269–76.
Shinozaki M, Nakada TA, Kawaguchi R, Yoshimura Y, Nakaguchi T, Haneishi H, et al. Feedback function for capillary refilling time measurement device. Crit Care. 2019;23:295.
Kawaguchi R, Nakada TA, Oshima T, Shinozaki M, Nakaguchi T, Haneishi H, et al. Optimal pressing strength and time for capillary refilling time. Crit Care. 2019;23:23–5.
Acknowledgements
The ANDROMEDA-SHOCK and the Latin America Intensive Care Network (LIVEN) Investigators is listed below. Writing and Steering Committee: Glenn Hernandez (co-chair), Gustavo Ospina-Tascón, Lucas Petri Damiani, Elisa Estenssoro, Arnaldo Dubin, Javier Hurtado, Gilberto Friedman, Ricardo Castro, Leyla Alegría, Jean-Louis Teboul, Maurizio Cecconi, Giorgio Ferri, Manuel Jibaja, Ronald Pairumani, Paula Fernández, Diego Barahona, Alexandre Biasi Cavalcanti, Jan Bakker (co-chair).Study Coordinating Center: Glenn Hernandez, Leyla Alegría, Giorgio Ferri, Nicolás Rodriguez, Patricia Holger, Natalia Soto, Mario Pozo, Jan Bakker. Data Safety Monitoring Committee: Deborah Cook, Jean-Louis Vincent, Andrew, Rhodes, Bryan P. Kavanagh, Phil Dellinger, Wim Rietdijk (Statistician). LATINOAMERICAN INTENSIVE CARE NETWORK (LIVEN) Chile: Pontificia Universidad Católica de Chile, Santiago (David Carpio, Nicolás Pavéz, Elizabeth Henriquez, Sebastian Bravo, Emilio Daniel Valenzuela, Magdalena Vera, Jorge Dreyse, Vanessa Oviedo); Hospital Barros-Luco Trudeau, Santiago (Maria Alicia Cid, Macarena Larroulet, Edward Petruska, Claudio Sarabia); Hospital San Juan de Dios, Santiago (David Gallardo, Juan Eduardo Sanchez, Hugo González, José Miguel Arancibia, Alex Muñoz, Germán Ramirez, Florencia Aravena); Hospital Dr. Sótero del Río, Santiago (Andrés Aquevedo, Fabián Zambrano); Hospital Del Salvador, Santiago (Milan Bozinovic, Felipe Valle, Manuel Ramirez, Victor Rossel, Pilar Muñoz, Carolina Ceballos); Hospital Herminda Martinez, Chillán (Christian Esveile, Cristian Carmona, Eva Candia, Daniela Mendoza); Hospital San Juan de Dios, Curicó (Aída Sanchez); Hospital Guillermo Grant Benavente, Concepción (Daniela Ponce, Jaime Lastra, Bárbara Nahuelpán, Fabrizio Fasce); Hospital Clínico Universidad de Chile, Santiago (Cecilia Luengo, Nicolas Medel, Cesar Cortés). Argentina: Clínica La Pequeña Familia, Junín (Luz Campassi); Sanatorio Otamendi y Miroli, Buenos Aires (Paolo Rubatto, Brenda Nahime Horna, Mariano Furche); Hospital Provincial del Centenario, Rosario (Juan Carlos Pendino, Lisandro Bettini); Sanatorio Parque, Rosario (Carlos Lovesio, María Cecilia González, Jésica Rodruguez); Hospital Interzonal San Martín, La Plata (Héctor Canales, Francisco Caminos); Sanatorio Allende Nueva Córdoba (Cayetano Galletti, Estefanía Minoldo, María José Aramburu, Daniela Olmos); Uruguay: Hospital Español Juan J Crottogini, Montevideo (Nicolás Nin, Jordán Tenzi, Carlos Quiroga, Pablo Lacuesta, Agustín Gaudín, Richard Pais, Ana Silvestre, Germán Olivera); Hospital de Clínicas, Montevideo (Gloria Rieppi, Dolores Berrutti). Ecuador: Hospital Universitario del Rio, Cuenca (Marcelo Ochoa, Paul Cobos, Fernando Vintimilla); Hospital Eugenio Espejo, Quito (Vanessa Ramirez, Milton Tobar, Fernanda García, Fabricio Picoita, Nelson Remache); Hospital San Francisco, Quito (Vladimir Granda, Fernando Paredes, Eduardo Barzallo, Paul Garcés); Hospital Carlos Andrade Marín, Quito (Fausto Guerrero, Santiago Salazar, German Torres, Cristian Tana, José Calahorrano, Freddy Solis); Hospital IESS, Ibarra (Pedro Torres, Luís Herrera, Antonio Ornes, Verónica Peréz, Glenda Delgado, Alexei López, Eliana Espinosa, José Moreira); Hospital General Docente Calderón, Quito (Blanca Salcedo, Ivonne Villacres, Jhonny Suing, Marco Lopez, Luis Gomez, Guillermo Toctaquiza, Mario Cadena Zapata, Milton Alonso Orazabal, Ruben Pardo Espejo, Jorge Jimenez, Alexander Calderón); Hospital Enrique Garcés, Quito (Gustavo Paredes, José Luis Barberán, Tatiana Moya). Colombia: Hospital San Vicente de Paul, Medellín (Horacio Atehortua, Rodolfo Sabogal); Hospital de Santa Clara, Bogotá (Guillermo Ortiz, Antonio Lara); Hospital Universitario de Ñarino E.S.E, Pasto (Fabio Sanchez, Alvaro Hernán Portilla, Humberto Dávila, Jorge Antonio Mora); Fundación Valle del Lili, Cali (Luis Eduardo Calderón, Ingrid Alvarez, Elena Escobar, Alejandro Bejarano, Luis Alfonso Bustamante, José Luis Aldana).
Funding
The present post hoc analysis was supported in part by a FONDECYT Chile Grant project number 1170043.
Author information
Authors and Affiliations
Consortia
Contributions
RC and GH are guarantors of the entire manuscript; EK, GOT, GH, JB and RC designed the study. All the authors helped in the data interpretation and the final manuscript draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by institutional review boards at each of the 28 study sites. Informed consent was obtained from patients or legally authorized surrogates. The first and main institutional review board was: Comité Ético-Científico, Facultad de Medicina, Pontificia Universidad Católica de Chile, March 2017, ID 161012007.
Consent for publication
Not applicable.
Competing interests
All authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
ClinicalTrials ClinicalTrials.gov identifier: NCT03078712. Registered retrospectively on March 13th, 2017
Supplementary information
Additional File 1:
Baseline characteristics and clinical outcomes of septic shock patients at ANDROMEDA-SHOCK protocol inclusion. Data at 8-hours are reported for clarification purposes.
Additional File 2:
Demographic, perfusion and hemodynamic characteristics and clinical outcomes of patients according to CRT status at T0 and T2.
Additional File 3:
Clinical and interventions comparison between CRT non-responders at T2, according to study group.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kattan, E., Hernández, G., Ospina-Tascón, G. et al. A lactate-targeted resuscitation strategy may be associated with higher mortality in patients with septic shock and normal capillary refill time: a post hoc analysis of the ANDROMEDA-SHOCK study. Ann. Intensive Care 10, 114 (2020). https://doi.org/10.1186/s13613-020-00732-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-020-00732-1