Abstract
Background
The EANM Research Ltd. (EARL) guidelines give recommendations for harmonization of [18F]FDG PET-CT image acquisition and reconstruction, aiming to ensure reproducibility of quantitative data between PET scanners. Recent technological advancements in PET-CT imaging resulted in an updated version of the EARL guidelines (EARL2). The aim of this study is to compare quantitative [18F]FDG uptake metrics of the primary tumor and lymph nodes in patients with head and neck squamous cell carcinoma (HNSCC) on EARL2 versus EARL1 reconstructed images and to describe clinical implications for nodal staging and treatment.
Methods
Forty-nine consecutive patients with HNSCC were included. For all, both EARL1 and EARL2 images were reconstructed from a singular [18F]FDG PET-CT scan. Primary tumors and non-necrotic lymph nodes ≥ 5 mm were delineated on CT-scan. In the quantitative analysis, maximum standardized uptake values (SUVmax) and standardized uptake ratios (SURmax, i.e., SUVmax normalized to cervical spinal cord uptake) were calculated for all lesions on EARL1 and EARL2 reconstructions. Metabolic tumor volume (MTV) and total lesion glycolysis were compared between EARL1 and EARL2 using different segmentation methods (adaptive threshold; SUV2.5/3.5/4.5; SUR2.5/3.5/4.5; MAX40%/50%). In the qualitative analysis, each lymph node was scored independently by two nuclear medicine physicians on both EARL1 and EARL2 images on different occasions using a 4-point scale.
Results
There was a significant increase in SUVmax (16.5%) and SURmax (9.6%) of primary tumor and lymph nodes on EARL2 versus EARL1 imaging (p < 0.001). The proportional difference of both SUVmax and SURmax between EARL2 and EARL1 decreased with increasing tumor volume (p < 0.001). Absolute differences in MTVs between both reconstructions were small (< 1.0 cm3), independent of the segmentation method. MTVs decreased on EARL2 using relative threshold methods (adaptive threshold; MAX40%/50%) and increased using static SUV or SUR thresholds. With visual scoring of lymph nodes 38% (11/29) of nodes with score 2 on EARL1 were upstaged to score 3 on EARL2, which resulted in an alteration of nodal stage in 18% (6/33) of the patients.
Conclusions
Using the EARL2 method for PET image reconstruction resulted in higher SUVmax and SURmax compared to EARL1, with nodal upstaging in a significant number of patients.
Similar content being viewed by others
Background
Positron emission tomography (PET) with fluor-18-fluorodeoxyglucose ([18F]FDG) in combination with computed tomography (CT) is increasingly utilized for radiation treatment planning in patients with head and neck squamous cell carcinoma (HNSCC). The use of PET-CT scanners with different hardware specifications or methods of image acquisition and reconstruction can result in undesired variation of quantitative [18F]FDG uptake metrics [1]. To ensure the reproducibility of quantitative data between PET scanners, the European Association of Nuclear Medicine (EANM) has initiated the EANM Research Ltd. (EARL) harmonization program. These give guidelines on how to perform PET imaging, aiming to harmonize patient preparation, scan acquisition, and image reconstruction [2].
The first version of the EANM guidelines (EARL1) was introduced in 2010 [3, 4]. Over the years, multiple technological advances in PET-CT imaging regarding both hard- and software have improved contrast recovery with better spatial resolution and lesion detectability [5, 6]. Among these new developments are the introduction of time-of-flight, point spread function, smaller voxel sizes and digital silicon photomultiplier detectors. An updated version of the EANM guidelines (EARL2) was introduced in 2019 to take these developments into account [6, 7]. Compared to EARL1, application of the EARL2 image reconstruction methods can result in significant changes in quantitative [18F]FDG uptake metrics, such as the maximum standardized uptake value (SUVmax), SUVmean, metabolic target volume (MTV), and total lesion glycolysis (TLG) [8]. Changes in quantitative PET readings can have important clinical implications for tumor staging and treatment. Ly et al. reported that the use of EARL2 versus EARL1 reconstructions for lymphoma lesions led to an upgrade in Deauville score in 33% of the patients, resulting in a treatment intensification in 9% of the patients [9].
Changes of quantitative [18F]FDG uptake metrics as a result from EARL2 image reconstruction methods may also affect treatment of patients with HNSCC. For radiation treatment, [18F]FDG PET-CT imaging can be used for primary tumor segmentation and to guide dose escalation to a metabolic subvolume within the tumor [10,11,12]. In addition, enhanced contrast ratios with EARL2 can also improve the detection of nodal metastases and thus consequentially alter nodal staging and radiation treatment.
Therefore, the aim of this study is to compare quantitative [18F]FDG uptake metrics of the primary tumor and lymph nodes in patients with HNSCC using EARL2 versus EARL1 reconstructed images and to describe clinical implications for nodal staging and treatment.
Methods
Patient selection
This is a single center cohort study. The need for written informed consent was waived by the local ethics committee as the study was conducted retrospectively from data obtained for clinical purposes (reference number 2021-9835). A sequential cohort of 230 patients with squamous cell carcinoma of the oropharynx, hypopharynx or larynx that received definitive (chemo)radiotherapy between November 2020 and October 2021 was screened for eligibility. Acquisition of a [18F]FDG PET-CT scan in radiation treatment position with both EARL1 and EARL2 PET image reconstructions was mandatory. As from November 2020, acquisition of both EARL1 and EARL2 reconstructed images is standard practice at our institution. Patients with previous oncologic treatment (e.g. radiotherapy or tumor reductive surgery) of the head and neck area were excluded.
PET-CT acquisition and reconstruction
A PET scan, a low-dose CT scan for attenuation correction and an iodine contrast enhanced diagnostic CT scan for radiation treatment planning was acquired in one session on a Biograph mCT40 PET-CT scanner (Siemens Medical Solutions, Knoxville TN, USA). Imaging was acquired in radiation treatment position, using a customized neck support (AccuForm Custom Cushions, Accuform, MEDTEC, Orange City, IA) and a five-point fixation mask for immobilization of the head, neck and shoulders (HNS Mask-Nose Hole in Efficast 2.0 mm MAXI, Orfit Masks, Orfit Industries NV, Wijnegem, Belgium). Prior to [18F]FDG administration, patients fasted for at least 4 h and a serum glucose level of < 11 mmol/L was mandatory. [18F]FDG was intravenously administrated approximately 60 min prior to the scanning procedures (dose calculated using Eq. 1) [7].
All patients were scanned from the lower border of the clavicle to the cranium. The acquisition time was 3 min per bed position with an overlap of 43% between bed positions. The slice thickness of the CT-scan was 3 mm. EARL1 images were reconstructed with an ordered-subsets expectation–maximization (OSEM) algorithm including point spread function and time-of-flight, Gaussian Filter 7.5 mm full width at half maximum, image matrix 256*256 and voxel size 4.1*4.1*5.0 mm. EARL2 images were reconstructed with point spread function and time-of-flight OSEM, Gaussian Filter 4.3 mm, image matrix 400*400 and voxel size 2.0*2.0*5.0 mm.
Primary tumor
For all patients, [18F]FDG PET-CT scans were imported into the radiation treatment planning system Pinnacle version 3.2.0.27 (Philips Medical Systems, Fitchburg, MA, USA). Primary tumors were delineated on the CT-scan based on information gathered from physical examination and diagnostic imaging. The volume and the maximum [18F]FDG uptake was determined in terms of SUVmax and maximum standardized uptake ratio (SURmax) on both EARL reconstructions for each delineated tumor. The tumor to cervical spinal cord standardized uptake ratio (SUR) has been shown to improve the reproducibility of quantitative [18F]FDG-PET data in a multicenter setting compared to SUV based approaches [13]. SUVmax and SURmax were calculated using Eqs. 2 and 3.
Three different segmentation methods were used to determine MTVs on both EARL1 and EARL2 reconstructed images. Delineation of MTVs was performed automatically with customized Pinnacle scripting. Thresholds used were (1) an adaptive threshold as a percentage of SURmax (threshold = 116.93 * SURmax−0.75) [13], (2) a percentage of maximum [18F]FDG uptake (MAX40% and MAX50%) and (3) a static threshold of SUV or SUR (2.5, 3.5 and 4.5). For the SUV based segmentation methods, TLGs are calculated using Eq. 4.
The method of classification errors (CE) was used to evaluate spatial overlap of the MTVs based on EARL1 and EARL2 reconstructed images [14]. An important advantage of the CE method is that it does not only take volume into account, but also the spatial position and shape of the contours due to both false-negative and false-positive volumes. The CE can range from 0 to infinite, in which a lower CE implies better spatial overlap, and is calculated using Eq. 5.
The false-negative volume is defined as MTV that is delineated on EARL1 but not on EARL2, and vice versa for the false-positive volume.
Lymph nodes
All lymph nodes having a short-axis diameter of ≥ 5 mm in the axial plane were manually delineated on the CT-scan. This threshold was chosen because histopathological validation studies suggest that nodal metastases of this size can be detected by [18F]FDG PET-CT [15, 16]. Necrotic lymph nodes with irrefutably disturbed [18F]FDG distribution were not considered. Short-axis diameters, nodal volumes and quantitative [18F]FDG uptake parameters (i.e., SUVmax and SURmax) on both EARL1 and EARL2 reconstructed images were determined for each node.
For the qualitative analysis of nodal [18F]FDG uptake, both the EARL1 and EARL2 reconstructed image series were read independently by two experienced nuclear medicine physicians (AA and MvR), specialized in head and neck cancer. Each lymph node was scored separately on EARL1 and EARL2 reconstructed images using a 4-point scale (1—definitely benign, 2—probably benign, 3—probably malignant, 4—definitely malignant). To minimize observer recall bias, the time between scoring EARL1 and EARL2 reconstructed images was at least 4 weeks. Discrepancies between observers involving scores ‘3—probably malignant’ or ‘4—definitely malignant’ were resolved by consensus. Visual scores on EARL1 and EARL2 images were compared to identify consequences for radiation treatment and for N-classification (8th edition of UICC TNM classification) [17]. A change from score 1 or 2 to score 3 or 4 or vice versa was assumed to have consequence for staging and treatment.
Statistics
All statistical analyses were performed using SPSS version 26 (IBM Corporation, New York, NY, USA). Statistical significance level was set to p < 0.05. Normal distribution of data was tested using the Shapiro–Wilk test. Data characterized by normal distribution were presented as mean with 95% confidence interval (95% CI) and parameters not normally distributed as median with the interquartile range (IQR). Scatter plots and intraclass correlation coefficients (with a two-way mixed model testing absolute agreement) were used to describe the relationship of maximum [18F]FDG uptake (i.e., SUVmax and SURmax) on EARL1 and EARL2 reconstructed imaging. To evaluate the magnitude of differences between EARL1 and EARL2, the relative differences in SUVmax or SURmax were plotted against the average SUVmax or SURmax on both EARL reconstructions, according to the Bland–Altman method. Mean/median differences in quantitative metrics between both EARL reconstructions were calculated based on the differences of paired data. Comparison of means between groups was done using the Student T test for paired data in case of a normal distribution and the Wilcoxon signed rank test for data not normally distributed. In the qualitative nodal evaluation, agreement between observers was calculated by the kappa statistic. The kappa score can range between 0 and 1, with a score of 0.00–0.20 indicating none to slight interobserver agreement, 0.21–0.40 fair, 0.41–0.60 moderate, 0.61–0.80 substantial, and 0.81–1.00 almost perfect agreement [18].
Results
A total of 49 patients met all the in- and exclusion criteria. Patient and treatment characteristics are listed in Table 1. The mean administered dose of [18F]FDG was 178 MBq (95% CI 95–261). The mean time between FDG administration and image acquisition was 69 min (95% CI 55–83). The median blood glucose level was 5.7 mmol/L (IQR 5.2–6.2) at the time of [18F]FDG administration.
Primary tumor
For this analysis, four patients were excluded because tumor segmentation was not possible as a result of insufficient [18F]FDG uptake in the tumor (n = 1), or overlapping [18F]FDG uptake of the tumor with adjacent nodal metastases (n = 3). Thus, for the primary tumor analysis, 45 of 49 patients were evaluable. The median primary tumor volume as delineated on CT was 9.4 cm3 (IQR 5.5–17.3). The mean SUVmax of the primary tumor was 11.2 (95% CI 2.6–19.7) and 13.2 (95% CI 3.5–22.9) on EARL1 imaging and EARL2 imaging, respectively. The SURmax was 7.0 (95% CI 1.9–12.1) on EARL1 and 7.8 (95% CI 2.4–13.2) on EARL2. For all lesions combined (primary tumors and lymph nodes), there was a strong linear relationship between maximum [18F]FDG uptake (i.e., SUVmax and SURmax) on EARL1 and EARL2 imaging, with an intraclass correlation coefficient of 0.97 (95% CI 0.83–0.99; p < 0.001) for SUVmax and 0.98 (95% CI 0.93–0.99; p < 0.001) for SURmax (Fig. 1A–B). Bland–Altman plots showed a mean increase in SUVmax of 16.5% (95% CI − 3.4 to 36.8; p < 0.001) and SURmax of 9.6% (95% CI − 9.0–28.1; p < 0.001) on EARL2 reconstructed imaging compared to EARL1 (Fig. 1C, D). The proportional difference of both SUVmax and SURmax between EARL1 and EARL2 decreased with increasing tumor volume (Fig. 2).
Scatter plots and Bland–Altman plots of SUVmax and SURmax. A and B Scatter plots demonstrating the relationship of SUVmax (A) and SURmax (B) between EARL1 and EARL2. Abbreviations: ICC: intraclass correlation coefficient. C and D Bland–Altman plots demonstrating the relative differences of SUVmax (C) and SURmax (D) on EARL2 versus EARL1
MTVs and TLGs of the primary tumors for EARL1 and EARL2 reconstructed images for the various segmentation methods are shown in Tables 2 and 3, respectively. For most segmentation methods (7/9) there was a difference of the MTV on EARL2 compared to EARL1, with MTVs being significantly larger on EARL2 for 6/9 methods. Relative differences in MTVs were small using the adaptive threshold method and larger using static SUV or SUR thresholds. Also, relative differences were more pronounced using higher static thresholds (i.e., SUV4.5/SUR4.5) compared to lower static thresholds (SUV2.5/SUR2.5). For all SUV based segmentation methods, there was a significant difference of TLG between EARL1 and EARL2. The MAX40% segmentation method resulted in the smallest difference of TLG between EARL1 and EARL2.
The CE values for spatial overlap of MTVs based on EARL1 and EARL2 reconstructed images for the various segmentation methods were relatively small, ranging between 0.10 and 0.23 (Table 4). For the majority of segmentation methods, the false-negative volume was < 1 cm3 (MTV that is delineated on EARL1 but not on EARL2) and the false-positive volume < 0.5 cm3 (MTV delineated on EARL2 but not on EARL1).
Lymph nodes
In total, 175 lymph nodes in the first 34 consecutive patients were delineated on the CT scans and analyzed, as this number of lymph nodes was considered to provide sufficient power for both the quantitative and qualitative analysis. One of the 34 patients was excluded because no lymph nodes with a short-axis diameter ≥ 5 mm were present. The median short-axis diameter of lymph nodes on CT was 6 mm (IQR 5–8), with a median nodal volume of 0.6 cm3 (IQR 0.4–1.3). The median SUVmax of lymph nodes was 2.1 (IQR 1.7–3.1) and 2.4 (IQR 1.8–3.7) on EARL1 and EARL2, respectively. The SURmax was 1.3 (IQR 1.1–1.8) on EARL1 and 1.4 (IQR 1.1–2.2) on EARL2.
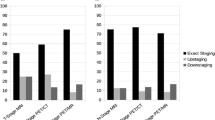
All 175 delineated lymph nodes were scored independently by two nuclear medicine physicians by means of visual interpretation of nodal [18F]FDG uptake. The interobserver agreement was high, with a kappa of 0.84 using dichotomized scores (1–2 vs. 3–4) and kappa 0.73 using scores 1–2 vs. 3 vs. 4. Figure 3 demonstrates the maximum [18F]FDG uptake (i.e., SUVmax and SURmax) stratified by the visual interpretation score of lymph nodes on EARL1 imaging. All nodes that were visually scored "3 – probably malignant" on EARL1 had a SURmax ≥ 1.5 and ≥ 1.6 on EARL1 and EARL2, respectively. All nodes that were scored "4 – definitely malignant" on EARL1 had a SURmax of ≥ 2.2 on EARL1 and ≥ 2.7 on EARL2. For lymph nodes visually scored “2—probably benign” on EARL1, 38% (11/29) was upstaged to score “3—probably malignant” on EARL2 (Table 5). For lymph nodes visually scored “3—probably malignant” on EARL1, 29% (6/21) was upstaged to score “4—definitely malignant” on EARL2. As a result, the N-classification changed in 18% (6/33) of the patients, with consequences for radiotherapy target volume in 24% (8/33) of the patients (i.e., additional lymph nodes irradiated with a high dose). There were no lymph nodes downstaged on EARL2 that were scored 3 or 4 on EARL1.
Boxplots of SUVmax and SURmax on EARL1 and EARL2, stratified by nodal score on EARL1. Box plots showing the distribution of SUVmax (A) and SURmax (B) of lymph nodes on EARL1 (blue) and EARL2 (red), stratified by the visual interpretation score of these nodes on EARL1. The horizontal line in the middle of the box represents the median, the colored box represents the interquartile range, whiskers represent 95% confidence intervals, and dots represent outliers. Statistically significant differences (p < 0.05) between EARL1 and EARL2 per nodal score group are indicated by * on the x-axis
Discussion
This study demonstrates a significant increase in SUVmax (16.5%) and SURmax (9.6%) of primary tumor and lymph nodes on EARL2 reconstructed imaging compared to EARL1 in patients with HNSCC. Absolute differences in volume and spatial overlap of MTVs were small between EARL1 and EARL2 reconstructed images, irrespective of the segmentation method used. Relative differences in MTVs were small using the adaptive threshold method and larger when using static SUV or SUR thresholds. Moreover, as a result of a higher SUVmax on EARL2 reconstructed images, more lymph nodes were likely to be scored as (probably) malignant with visual interpretation. This would have had consequences for the N-classification in 18% (6/33) and affecting radiation treatment in 24% (8/33) of the patients. These observations in a cohort with head and neck cancer patients are in line with the results of several previous phantom and clinical studies in other tumor sites, such as lymphoma and non-small cell lung cancer [6, 8, 9].
The SUVmax was on average 16.5% higher on EARL2 compared to EARL1 reconstructed images, with a strong correlation for both SUVmax and SURmax between EARL1 and EARL2. In patients with lymphoma and non-small cell lung cancer, Kaalep et al. found that SUVmax on EARL2 was on average 34% higher compared to EARL1 [8]. In line with our study, the largest differences in maximum [18F]FDG uptake between EARL1 and EARL2 were observed in smaller lesions. This can be explained by the better resolution of EARL2 reconstructed images and thus reducing the partial volume effect [5, 6]. The current study demonstrates a smaller but still significant increase in the maximum [18F]FDG uptake on EARL2 when using a target to background ratio (SURmax) compared to SUVmax. Few other studies demonstrate that the use of tumor-to-liver ratios also do not completely mitigate the effect of different EARL reconstructions [8, 19].
Absolute differences of primary tumor MTVs between EARL1 and EARL2 were small (< 1.0 cm3), independent of the segmentation method used. This is clinically important for radiation dose escalation to MTVs within the primary tumor volume based on [18F]FDG PET imaging. Although absolute differences in MTVs between both EARL reconstructions were small, the differences were still statistically significant for most segmentation methods (7/9). In contrast to static SUV or SUR thresholds, we observed that MTVs were smaller on EARL2 using relative threshold methods (i.e., MAX40% & MAX50%). This is in line with the results reported by Kaalep et al. [8]. However, they reported a median difference in MTV on EARL2 of -27% compared to EARL1 with the MAX41% segmentation method, compared to only -7.5% in our study [8]. Recently Ferrandez et al. calculated changes in MTV between EARL1 and EARL2 in 56 lymphoma lesions [20]. For the MAX41% and SUV2.5 method MTVs decreased with 27% and 4%, respectively. The smaller differences in MTVs observed between EARL1 and EARL2 in the current study may result from the use of time-of-flight and point spread function in both EARL reconstructions while this was not the case in the other studies. Therefore, differences in MTVs were most likely the result of different pixel and filter sizes only. Finally, patients with lymphoma and non-small cell lung cancer generally have larger tumor volumes than patients with HNSCC. Although absolute tumor volumes were not reported by Kaalep et al., and thus cannot be compared to the current data, this could potentially have contributed to the different findings in our study.
In literature several post-acquisition harmonization methods have been described to minimize variability in MTVs when using EARL2 vs. EARL1 reconstructed images. Kaalep et al. performed post-filtering of EARL2 reconstructed images with a 6–7 mm Gaussian filter, in order to generate EARL1 compliant quantitative data from EARL2 images [8]. This would obviate the need to perform a EARL1 compliant reconstruction, while both EARL2 and EARL1 images are still available to allow comparison of quantitative data with historic cohorts. Recently Ferrandez et al. investigated the ComBat harmonization method, aiming to align MTVs from EARL1 and EARL2 reconstructed images [20]. This ComBat harmonization resulted in an improved agreement of MTVs from different reconstructions for most segmentation methods. The advantage of ComBat is that it directly applies to quantitative metrics already extracted from the images based on assumptions and estimations of batch effects, without the need to actually have access to the images [21]. A limitation is that the transformation is specific for each type of tissue, tumor, scanner and segmentation method. In a prospective setting, such as in our study, we strongly believe in the importance of upfront harmonization strategies (like EARL) and advise that both EARL1 and EARL2 reconstructed images are acquired for each patient. This allows for a direct comparison of quantitative [18F]FDG uptake metrics on both images, next to morphological features of the lesion. However, in a retrospective setting, post-acquisition harmonization methods such as ComBat and post-filtering can be useful when comparing quantitative metrics based on the latest EARL protocol (e.g. EARL2 or in the future EARL3) with historic cohorts.
For the majority of segmentation methods (8/9), CE values ranged between 0.10 and 0.20, indicating a good spatial overlap of MTVs on both EARL images. This is especially important in radiation treatment planning, as false-negative and false-positive volumes may impact tumor control probability or treatment induced toxicity.
For TLG, differences between EARL1 and EARL2 were also dependent on the segmentation method used. Relative differences were smallest using the MAX40% method and larger using static SUV thresholds. Kaalep et al. reported a median relative difference in TLG on EARL2 of 23% compared to EARL1 with a static threshold of SUV4 [8]. For the MAX41% method the TLG on EARL2 decreased with only 2%. These results are comparable to the findings in our study when using SUV3.5/4.5 and MAX40% thresholds. As TLG reflects the total [18F]FDG accumulation in the lesion, which obviously should be equal for both EARL reconstructions, it should be less sensitive to different reconstruction methods and lesion size compared with SUVmax [8, 22, 23]. Based on our results, the MAX40% method may be a good candidate for estimating the TLG because the differences between EARL1 and EARL2 were small. This is relevant because there is an increasing interest in TLG in literature as several studies reported that changes in TLG during treatment are predictive for loco-regional control and overall survival in patients with HNSCC [24, 25].
Our analysis demonstrated that quantitative visual evaluation of cervical lymph nodes on EARL2 compared to EARL1 would have changed the N-classification in 18% and affected radiation treatment in 24% of the patients. Similarly, Ly et al. showed that in 52 lymphoma patients EARL2 versus EARL1 reconstructions led to an upgrade in Deauville score in 18 patients (33%), resulting in a treatment intensification in 5 patients (9%) [9]. As such, caution is warranted when applying quantitative [18F]FDG uptake thresholds, that are based on EARL1 imaging, directly to EARL2 diagnostic imaging as this comes with a risk of upstaging and overtreatment. Therefore, EARL1 based quantitative thresholds should be re-evaluated before being implemented on EARL2 imaging.
Conclusions
Implementation of the EARL2 reconstruction methods for [18F]FDG-PET imaging resulted in a higher SUVmax and SURmax in primary tumors and lymph nodes, compared to the EARL1 image reconstruction. Using EARL2 versus EARL1 images for the visual interpretation of lymph nodes led to nodal upstaging and alteration of radiation treatment volumes in a significant amount of patients with HNSCC. Further research is needed to re-evaluate [18F]FDG uptake thresholds based on EARL1 before they can be applied on EARL2 imaging.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PET:
-
Positron emission tomography
- [18F]FDG:
-
Fluor-18-fluorodeoxyglucose
- CT:
-
Computed tomography
- HNSCC:
-
Head and neck squamous cell carcinoma
- EANM:
-
European Association of Nuclear Medicine
- EARL:
-
EANM Research Ltd.
- SUV:
-
Standardized uptake value
- MTV:
-
Metabolic target volume
- TLG:
-
Total lesion glycolysis
- OSEM:
-
Ordered-subsets expectation–maximization
- SUR:
-
Standardized uptake ratio
- CE:
-
Classification errors
- CI:
-
Confidence interval
- IQR:
-
Interquartile range
References
Aide N, Lasnon C, Veit-Haibach P, Sera T, Sattler B, Boellaard R. EANM/EARL harmonization strategies in PET quantification: from daily practice to multicentre oncological studies. Eur J Nucl Med Mol Imaging. 2017;44(Suppl 1):17–31.
EANM Research Ltd. (EARL). https://earl.eanm.org. Accessed 10 November 2022.
Kaalep A, Sera T, Oyen W, Krause BJ, Chiti A, Liu Y, et al. EANM/EARL FDG-PET/CT accreditation - summary results from the first 200 accredited imaging systems. Eur J Nucl Med Mol Imaging. 2018;45(3):412–22.
Boellaard R, O’Doherty MJ, Weber WA, Mottaghy FM, Lonsdale MN, Stroobants SG, et al. FDG PET and PET/CT: EANM procedure guidelines for tumour PET imaging: version 1.0. Eur J Nucl Med Mol Imaging. 2010;37(1):181–200.
Ferretti A, Chondrogiannis S, Rampin L, Bellan E, Marzola MC, Grassetto G, et al. How to harmonize SUVs obtained by hybrid PET/CT scanners with and without point spread function correction. Phys Med Biol. 2018;63(23):235010.
Kaalep A, Sera T, Rijnsdorp S, Yaqub M, Talsma A, Lodge MA, et al. Feasibility of state of the art PET/CT systems performance harmonisation. Eur J Nucl Med Mol Imaging. 2018;45(8):1344–61.
Boellaard R, Delgado-Bolton R, Oyen WJ, Giammarile F, Tatsch K, Eschner W, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2015;42(2):328–54.
Kaalep A, Burggraaff CN, Pieplenbosch S, Verwer EE, Sera T, Zijlstra J, et al. Quantitative implications of the updated EARL 2019 PET-CT performance standards. EJNMMI Phys. 2019;6(1):28.
Ly J, Minarik D, Edenbrandt L, Wollmer P, Tragardh E. The use of a proposed updated EARL harmonization of (18)F-FDG PET-CT in patients with lymphoma yields significant differences in Deauville score compared with current EARL recommendations. EJNMMI Res. 2019;9(1):65.
van den Bosch S, Dijkema T, Kunze-Busch MC, Terhaard CH, Raaijmakers CP, Doornaert PA, et al. Uniform FDG-PET guided GRAdient Dose prEscription to reduce late Radiation Toxicity (UPGRADE-RT): study protocol for a randomized clinical trial with dose reduction to the elective neck in head and neck squamous cell carcinoma. BMC Cancer. 2017;17(1):208.
Gouw ZAR, La Fontaine MD, Vogel WV, van de Kamer JB, Sonke JJ, Al-Mamgani A. Single-center prospective trial investigating the feasibility of serial FDG-PET guided adaptive radiation therapy for head and neck cancer. Int J Radiat Oncol Biol Phys. 2020;108(4):960–8.
Heukelom J, Hamming O, Bartelink H, Hoebers F, Giralt J, Herlestam T, et al. Adaptive and innovative Radiation Treatment FOR improving Cancer treatment outcomE (ARTFORCE); a randomized controlled phase II trial for individualized treatment of head and neck cancer. BMC Cancer. 2013;13:84.
van den Bosch S, Dijkema T, Philippens MEP, Terhaard CHJ, Hoebers FJP, Kaanders J, et al. Tumor to cervical spinal cord standardized uptake ratio (SUR) improves the reproducibility of (18)F-FDG-PET based tumor segmentation in head and neck squamous cell carcinoma in a multicenter setting. Radiother Oncol. 2019;130:39–45.
Hatt M, Lamare F, Boussion N, Turzo A, Collet C, Salzenstein F, et al. Fuzzy hidden Markov chains segmentation for volume determination and quantitation in PET. Phys Med Biol. 2007;52(12):3467–91.
Kitajima K, Murakami K, Yamasaki E, Kaji Y, Sugimura K. Accuracy of integrated FDG-PET/contrast-enhanced CT in detecting pelvic and paraaortic lymph node metastasis in patients with uterine cancer. Eur Radiol. 2009;19(6):1529–36.
Roh JL, Park JP, Kim JS, Lee JH, Cho KJ, Choi SH, et al. 18F fluorodeoxyglucose PET/CT in head and neck squamous cell carcinoma with negative neck palpation findings: a prospective study. Radiology. 2014;271(1):153–61.
O’Sullivan B, Brierley J, Byrd D, Bosman F, Kehoe S, Kossary C, et al. The TNM classification of malignant tumours-towards common understanding and reasonable expectations. Lancet Oncol. 2017;18(7):849–51.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Kuhnert G, Boellaard R, Sterzer S, Kahraman D, Scheffler M, Wolf J, et al. Impact of PET/CT image reconstruction methods and liver uptake normalization strategies on quantitative image analysis. Eur J Nucl Med Mol Imaging. 2016;43(2):249–58.
Ferrandez MC, Eertink JJ, Golla SSV, Wiegers SE, Zwezerijnen GJC, Pieplenbosch S, et al. Combatting the effect of image reconstruction settings on lymphoma [(18)F]FDG PET metabolic tumor volume assessment using various segmentation methods. EJNMMI Res. 2022;12(1):44.
Orlhac F, Eertink JJ, Cottereau AS, Zijlstra JM, Thieblemont C, Meignan M, et al. A guide to ComBat harmonization of imaging biomarkers in multicenter studies. J Nucl Med. 2022;63:172–9.
Armstrong IS, Kelly MD, Williams HA, Matthews JC. Impact of point spread function modelling and time of flight on FDG uptake measurements in lung lesions using alternative filtering strategies. EJNMMI Phys. 2014;1(1):99.
Huang K, Feng Y, Liang W, Li L. Impact of time of flight and point spread function on quantitative parameters of lung lesions in (18)F-FDG PET/CT. BMC Med Imaging. 2021;21(1):169.
Pak K, Cheon GJ, Nam HY, Kim SJ, Kang KW, Chung JK, et al. Prognostic value of metabolic tumor volume and total lesion glycolysis in head and neck cancer: a systematic review and meta-analysis. J Nucl Med. 2014;55(6):884–90.
Kim S, Oh S, Kim JS, Kim YK, Kim KH, Oh DH, et al. Prognostic value of FDG PET/CT during radiotherapy in head and neck cancer patients. Radiat Oncol J. 2018;36(2):95–102.
Acknowledgments
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SvdB developed the study concept. AA and MvR executed the visual scoring of lymph nodes. MC and TJ performed data acquisition and analysis. MC drafted and revised the manuscript. SvdB and JK supervised the writing process. SvdB and JK critically reviewed and edited the manuscript. All authors approved the final version of the report.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
For this single center sequential retrospective cohort study, ethical approval and consent to participate were waived by the local ethics committee because the study was conducted retrospectively from data obtained for clinical purposes (reference number 2021–9835).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cox, M.C., Jurcka, T., Arens, A.I.J. et al. Quantitative and clinical implications of the EARL2 versus EARL1 [18F]FDG PET-CT performance standards in head and neck squamous cell carcinoma. EJNMMI Res 13, 91 (2023). https://doi.org/10.1186/s13550-023-01042-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13550-023-01042-w