Abstract
Background/aims
Although volumetric imaging by computed tomography (CT) is the gold standard for preoperative assessment of the future liver remnant, nuclear imaging studies have shown promising data. This systematic review summarized the results from trials investigating volumetric and nuclear medicine imaging for the prediction of postoperative mortality and liver failure (LF).
Methods
MEDLINE and Web of Science were searched for papers investigating nuclear imaging methods for the prediction of postoperative clinical outcomes in patients undergoing local, liver-directed treatments. Only papers investigating both preoperative nuclear imaging and CT or magnetic resonance imaging (MR) for the prediction of postoperative mortality and/or LF were included.
Results
Twenty-five trials were qualified for this review. All trials but two used technetium-based tracers for the nuclear imaging examination. Four papers used MR imaging and the remaining used CT for the volumetric evaluation. Overall, the studies were heterogeneous both in terms of methodology and imaging technique. Of the thirteen studies reporting on postoperative mortality, most were descriptive without detailed diagnostic data. A few with detailed data found that nuclear imaging had better predictive value than volumetric imaging. Nineteen studies investigated the prediction of postoperative LF of which seven papers investigated the predictive value of both modalities in multivariable regression analysis. Two papers found that only nuclear imaging parameters were predictive of LF, one paper found that the CT parameter was predictive, and four papers found that combined nuclear and CT/MR imaging parameters were predictive of LF.
Conclusion
Both methodologies were useful in the preoperative assessment of patients scheduled for liver interventions, especially in combination, but nuclear imaging demonstrated better predictive value for postoperative mortality and LF in a few trials. The overall technical and methodological heterogeneity of the included studies complicates the ability to directly compare the clinical utility of the two imaging techniques.
Similar content being viewed by others
Introduction
The volume of the future liver remnant (FLR) assessed by computed tomography (CT) is broadly considered the gold standard for preoperative liver assessment both in terms of determining eligibility for surgery and the extent of surgery [1]. By assuming a uniformly distributed liver function, CT-volumetry serves as an indirect assessment of the functional capacity of the FLR along with global liver function tests, biochemical markers, and clinical scores. However, in patients with underlying parenchymal liver disease, the functional capacity of the liver is not necessarily homogenously distributed. If the liver morphology and function are considered normal, 75–80% of the total liver volume can be safely resected [2,3,4,5,6,7,8]. However, if the liver function is suspected to be impaired, for example, due to chemotherapy or liver cirrhosis, the liver volume to be resected is greatly reduced [5, 7, 8].
With nuclear medicine imaging, it is possible to evaluate the function of the FLR directly. Therefore, one cutoff level for a safe liver resection might suffice irrespective of the underlying liver condition [9, 10]. Nuclear imaging may therefore offer a better risk estimation prior to liver surgery than volumetric assessments. Moreover, based on a previously published systematic review from the same literature search, preoperative nuclear imaging has been shown to predict postoperative liver failure (LF) in several studies [11]. Nonetheless, the incremental value of nuclear imaging techniques over volumetric imaging for preoperative assessment of the FLR has not yet been thoroughly clarified. The purpose of this systematic review was to summarize the studies investigating both preoperative functional imaging with nuclear medicine and volumetric imaging with CT or magnetic resonance (MR) imaging for the prediction of postoperative mortality and/or liver failure (LF) in patients undergoing local liver-directed treatments.
Methods
Literature search strategy
This review included papers from a previously published systematic review investigating preprocedural nuclear imaging methods for the prediction of postprocedural clinical outcomes after local intervention in the liver [11]. In brief, the literature search was performed in two bibliographic databases with a deadline of search of May 27, 2020. The criteria for patients, interventions, comparators, outcomes, and study design were customized for each bibliographic database [11]. The systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [12].
Eligibility criteria and study selection
The eligibility criteria have been described in detail previously [11]. For this sub-study of the original systematic review, we identified original studies where patients underwent a functional nuclear imaging-based examination as well as an anatomical examination by CT or MR imaging prior to localized, liver-directed treatments with the purpose of removing impaired liver tissue (e.g., liver resection, cryotherapy, radiotherapy, etc.). The included papers had to report the results of the preprocedural imaging examination with regard to postprocedural clinical outcomes, including mortality and/or LF. For this analysis, we sought to investigate whether preprocedural nuclear imaging was significantly better than CT/MR imaging for the prediction of postprocedural mortality and LF.
Data extraction
Two investigators reviewed relevant papers, and three investigators extracted data. We extracted details regarding study demographics, imaging technique and therapeutic interventions, and study methodology, such as patient enrollment (prospective/retrospective), selection (consecutive/non-consecutive), and outcome measures. Classification of major versus minor surgery was based on Couinaud’s criteria [13]. Extent of surgery (major vs. minor) was not included as a volumetric parameter for our data extraction, and only preoperative or combined pre-/perioperative volumetric measurements were included. Some studies analyzed mortality and LF as part of a composite outcome; such papers were included, denoted in the tables as ≠. Postoperative LF encompasses both terms described as posthepatectomy liver failure, hepatic insufficiency, liver dysfunction, and the like—in our paper, it is referred to as postoperative LF under one heading. Details on mortality and LF distinctions and data extraction have been described in further detail previously [11].
Results
Study demographics of the included papers
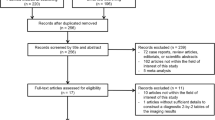
From a total of 82 eligible studies included in the original systematic review, 25 papers investigated both preoperative nuclear medicine and volumetric imaging for the prediction of postoperative mortality and/or LF (Fig. 1). These 25 papers constituted the systematic review of functional versus anatomical preoperative imaging. Most trials were from Japan (n = 13), the Netherlands (n = 5), and Belgium (n = 3) (Table 1). The median publication year was 2013. Six studies enrolled patients prospectively. Consecutive recruitment was ensured in 20 trials. The median number of patients was 100 (range 11–625 patients). The surgical procedures involved both major and minor surgery. The nuclear imaging assessments commonly involved technetium-based tracers: [99mTc]Tc-galactosyl human serum albumin (GSA) (n = 12) and [99mTc]Tc-mebrofenin (n = 11). Two studies employed positron emission-based tracers [14, 15]. Most studies used CT for volumetric imaging; only four studies applied MR imaging. All studies used preoperative volumetric assessments; two papers investigated a combined pre-/peroperative volumetric parameter (resected parenchymal fraction) [16, 17]. Seven papers investigated a combined functional and volumetric preoperative parameter incorporating both volumetric and functional assessments. Overall, there were notable variations in the technical methodology, both in terms of the nuclear imaging parameters and calculations (also within the same tracer type) and the CT/MR imaging parameters (data not shown).
Prediction of postoperative mortality
Thirteen papers reported on preoperative imaging for the prediction of postoperative mortality of which five were comparative studies with prespecified aims to compare functional, nuclear imaging with volumetric imaging for the prediction of postoperative mortality and/or LF [18,19,20,21,22] (Table 2). Most studies investigated 90-day mortality; mortality rates varied from 0 to 27%. Eight papers reported outcomes in a descriptive fashion and/or reported imaging parameters in patients with and without a fatal outcome without any statistical analyses. Four studies reported clinically relevant prognostic information for both imaging modalities. Two studies compared preoperative nuclear uptake values and CT volume measurements in patients with and without postoperative mortality [19, 23]. Dinant et al. found that uptake in the FLR determined by nuclear imaging was significantly lower in patients with LF-related mortality (mean 2.3 vs. 4.2%/min/BSA, p = 0.02), whereas volume of the FLR determined by CT was not significantly different in patients with and without LF-related mortality (mean 45 vs. 52%, p = 0.51) [19]. However, neither FLR uptake nor volume was significantly different in patients with and without overall mortality. Likewise, neither functional nor volumetric assessment of the FLR was significantly associated with 90-day mortality in patients with hepatocellular carcinoma undergoing liver resection [23].
In terms of the key diagnostic characteristics of the cutoff levels, Dinant et al. found that FLR function and volume had an area under the curve (AUC) of 88% (95%CI 75–100%) and 61% (95%CI 21–100%), respectively, for predicting LF-related mortality [19]. Olthof et al. found that FLR function and volume had an AUC of 70% (95%CI 57–82%) and 60% (95%CI 42–79%) for predicting posthepatectomy LF-related (PHLF) mortality [22]. None of the papers directly compared the predictive value of nuclear versus CT/MR imaging parameters for the prediction of postoperative mortality. In univariable logistic regression analysis, only marginal FLR function (OR 8.78, p = 0.008), and not FLR volume (OR 1.99, p = 0.367), was associated with an increased risk of postoperative mortality [20].
Prediction of postoperative liver failure
Nineteen studies reported data for the prediction of postoperative LF of which seven were comparative studies with prespecified aims to compare functional, nuclear imaging with volumetric imaging for the prediction of postoperative LF [10, 18,19,20,21,22, 24] (Table 3). Most studies defined LF though the definitions varied across the studies (data not shown). The International Study Group of Liver Surgery’s criteria [25] for the definition of postoperative LF were used in several studies [18, 22, 23, 26,27,28,29]. The LF rate ranged from 1 to 33%. Seven papers investigated the predictive value of a predetermined cutoff value, eight papers established a post hoc cutoff value, and three studies investigated both [10, 22, 30]. Several studies (n = 15) reported detailed diagnostic data on the preoperative imaging tests for the prediction of postoperative LF (Table 4).
Fourteen studies compared the results of both preoperative nuclear and CT/MR imaging in patients with and without postoperative LF. Eleven of these papers demonstrated a significantly lower functional liver capacity based on preoperative nuclear imaging in patients with postoperative LF compared to those without. In contrast, eight of these papers reported a significantly lower volumetric liver capacity or higher resected liver volume based on preoperative CT/MR imaging in patients with postoperative LF compared to those without. Four studies investigated the results of a combined nuclear and CT/MR imaging parameter in patients with and without LF [14, 17, 18, 26], of which three found a statistically significant difference.
Overall, the sensitivity and specificity of the nuclear imaging cutoffs for the prediction of postoperative LF varied across the studies from 50 to 100% and 32 to 96%, respectively. In comparison, the specificity and sensitivity of the CT/MR imaging cutoff varied from 57 to 78% and 80 to 91%, respectively. Lastly, the combined nuclear and CT/MR imaging parameters resulted in sensitivities and specificities ranging from 57 to 92% and 46 to 98%, respectively. The volumetric parameter (FLRV%) and the combined nuclear and MR imaging parameter (eFLRF) had a higher AUC than the nuclear imaging parameter alone (HBSBSA) for the prediction of postoperative LF [26]. Moreover, nuclear imaging with [99mTc]Tc-GSA was not significantly better in predicting LF than CT-volumetry when comparing the AUC for the prediction of LF for the nuclear (AUC: 0.97) and CT (AUC: 0.93) imaging parameter [24]. Cho et al. found that the volumetric parameter had a higher AUC for the prediction of postoperative LF, although not significantly better than that of the other evaluated parameters including nuclear functional imaging [14].
Five papers analyzed the predictive value of both a nuclear and CT/MR imaging parameter for the prediction of postoperative LF in univariable regression analyses [14, 18, 20, 22, 26]. Two of these found that both the nuclear and CT/MR imaging parameters were predictive of LF [18, 22]. However, whereas Hayashi et al. only demonstrated a significant predictive value of marginal future remnant function but not volume [20], two papers demonstrated a significant predictive value of the CT/MR imaging parameter alone and not the nuclear imaging parameter in univariable regression analyses [14, 26]. Moreover, three papers found that a combined nuclear and volumetric imaging parameter was predictive of LF in univariable regression analyses [14, 18, 26]. Seven papers investigated the predictive value of both nuclear and CT/MR imaging parameters or a combination of both in multivariable regression analysis. Two papers demonstrated a significant predictive value of the nuclear and not CT imaging parameter for the prediction of postoperative LF [22, 31], whereas Nanashima et al. only demonstrated a significant predictive value of the estimated resected volume (%) from the CT examination for overall postoperative complications including LF in multivariable analysis [32]. Four papers analyzed the predictive value of a combined functional and morphological parameter (combined nuclear and CT/MR imaging) [14, 17, 18, 26]. These papers found that the combined parameters were predictive of LF in both univariable and/or multivariable analysis. Three of these papers also investigated strictly nuclear and/or the CT/MR imaging parameters and found that they were not predictive of postoperative LF in multivariable analysis [14, 17, 26].
In terms of historical comparisons, mortality and LF rates were significantly higher in an observational study using only FLR volume ratio for determining eligibility for hepatectomy compared to a prospective interventional study employing the FLR function cutoff for determining eligibility (6 vs. 0%, p = 0.016 and 15 vs. 14%, p = 0.001, respectively) [27].
Discussion
Several studies have investigated both preoperative nuclear and CT/MR imaging for predicting postoperative clinical outcomes in the same study setup. Both functional nuclear imaging and volumetric imaging with CT/MR were useful in the preoperative assessment of patients undergoing liver surgery, especially in combination. However, nuclear imaging demonstrated a better predictive value for postoperative mortality and LF than CT/MR imaging alone in a few studies. Yet, the methodology, imaging techniques, and parameters across the studies were heterogeneous and detailed diagnostic data were limited, especially in terms of postoperative mortality. Only a few of the trials included prespecified aims to compare preoperative nuclear imaging with volumetric imaging for the prediction of postoperative mortality and/or LF. As a result, despite theoretical advantages of nuclear imaging, it is difficult to directly compare the clinical utility of the two imaging techniques across the included studies and determine whether nuclear functional imaging offers incremental value as opposed to CT/MR volumetric imaging for the prediction of both postoperative mortality and LF.
Our review of the published reports revealed very limited detailed diagnostic data on the association between preoperative nuclear and CT/MR imaging and postoperative mortality. Among the few studies with detailed diagnostic data, the AUC for predicting LF-related mortality was higher for the nuclear imaging techniques compared to CT, although no statistical comparison of difference in the AUC was conducted. Moreover, one study found that the preoperative FLR functional uptake and not FLR volume was significantly lower in patients with postoperative LF-related mortality compared to those without [19], whereas neither function nor volume of the FLR was associated with overall mortality. Only one paper [20] investigated the predictive value of both CT and nuclear imaging in univariable analysis and found that only marginal FRL function and not marginal FRL volume was predictive of postoperative mortality.
There were several studies with detailed diagnostic data on the predictive value of preoperative nuclear and CT/MR imaging parameters with regard to postoperative LF. Overall, more papers demonstrated significant differences in preoperative nuclear imaging uptake values in patients with and without postoperative LF as opposed to differences in the preoperative CT imaging parameters (11 vs. 8 papers). Moreover, nuclear imaging more often proved to be an independent significant predictor of postoperative LF in multivariable analyses compared to CT/MR imaging (in 2 vs. 1 paper). However, the differences were too small for firm conclusions about the predictive value of nuclear vs. CT/MR imaging. Moreover, two studies compared the predictive value of the nuclear versus CT imaging parameters directly and found no significant differences in the AUC of the nuclear and CT imaging technique for predicting postoperative LF [14, 24]. However, in all but one of the comparative studies with prespecified aims to compare nuclear imaging with volumetric imaging for the prediction of postoperative LF, nuclear imaging, or combined nuclear/volumetric imaging proved to be better than volumetric imaging alone for predicting postoperative LF [10, 18,19,20,21,22]. These studies highlight the theoretical and clinical importance of functional nuclear imaging in the preoperative assessment.
Interestingly, when combining the preoperative functional and volumetric imaging results in a single parameter, the combined parameter demonstrated optimized predictive value for estimating the risk of postoperative LF [14, 17, 18, 26]; the combined parameter showed better predictive potential for postoperative LF than did nuclear or CT/MR imaging alone. These findings underscore the importance of both volumetric and functional assessments of the FLR and the added potential of incorporating both in the preoperative assessment.
Overall, there was a great heterogeneity in the included studies both in terms of methodology, aims, study populations as well as the nuclear imaging acquisition techniques and calculation of the nuclear and CT/MR imaging parameters. In a minority of studies, the prespecified primary or secondary aims involved comparing functional nuclear imaging with volumetric imaging for predicting postoperative mortality and/or LF [10, 18,19,20,21,22, 24]. Other studies evaluated several pre- or perioperative factors associated with postoperative outcomes including nuclear and volumetric imaging [30, 32]. In most studies, however, the volumetric evaluation with regard to postoperative mortality and/or LF was part of additional results not necessarily pertaining to the main objectives of the study. Moreover, the study populations varied both in terms of the number of patients included, the underlying indication for liver surgery, and the involved surgical technique (major vs. minor surgery, and staged hepatectomy). Moreover, the small samples sizes of some of the original studies may cause selection bias due to the effective use of functional imaging in these patient groups. The methodological and technical differences in the studies complicate the comparison of functional versus volumetric imaging across the studies and warrant a standardization of methodology and imaging techniques. This would offer a better comparison of nuclear imaging versus CT/MR imaging in the preoperative assessment of postoperative risk in patients undergoing liver surgery.
Whereas volumetric imaging with CT is a well-established routine examination prior to liver surgery for evaluating resectability and eligibility for surgery, there are still no widely accepted international guidelines or consensus statements on the use of nuclear imaging in the preoperative assessment. Nonetheless, nuclear imaging has gained increasing use in the preoperative assessment over the last decade. The limitations of volumetric imaging as an indirect estimate of the functional capacity of the FLR seem to be overcome by the potential of nuclear imaging to directly estimate the regional function of FLR and thus the actual postoperative functional capacity. Indeed, our previously published systematic review focusing solely on the predictive value of nuclear imaging techniques for the prediction of postoperative mortality and LF revealed that despite technical and methodological heterogeneity across the studies, a notable number of trials found a significant predictive value of nuclear imaging for the prediction of postoperative LF.
As this review is based on studies included in a previously published systematic review of nuclear medicine imaging methods [11], the literature search was set up to find original research papers investigating preoperative nuclear imaging for the prediction of postoperative clinical outcomes and not necessarily papers comparing nuclear to CT/MR imaging for the prediction of postoperative clinical outcomes which was the focus of this review. Therefore, this analysis should not be regarded as a systematic review of anatomical imaging methods: There are likely many trials examining anatomical methods without comparison to nuclear medicine methods. The literature search for original papers covered papers published up until May 27, 2020, so we may have missed very recent reports. Moreover, some groups published several similarly appearing papers with increasing number of included patients and we did not contact individual authors to enquire about overlapping data. This may, therefore, cause a potential bias due to overlapping data.
Conclusion
In conclusion, 25 papers investigated both preoperative nuclear imaging and CT/MR imaging for predicting postoperative clinical outcomes in patients undergoing local, liver-directed treatments. Both volumetric imaging and nuclear imaging were useful in the preoperative assessment of postoperative risk, especially in combination, but nuclear imaging demonstrated a better predictive value for postoperative mortality and LF than volumetric imaging alone in a few trials. However, the abundant technical and methodological heterogeneity across the included studies complicates the ability to directly compare the results of functional nuclear imaging with that of volumetric imaging with CT/MR for the prediction of postoperative mortality and LF. Larger, prospective studies would be beneficial in order to establish the added benefit of nuclear imaging to the standard of care, CT/MR imaging, in the preoperative assessment.
Availability of data and materials
All data generated or analyzed in this study are included in this published article.
Abbreviations
- FLR:
-
Future liver remnant
- CT:
-
Computed tomography
- MR:
-
Magnetic resonance
- LF:
-
Liver failure
- GSA:
-
(Human) galactosyl serum albumin
- AUC:
-
Area under the curve
References
Cieslak KP, Runge JH, Heger M, Stoker J, Bennink RJ, van Gulik TM. New perspectives in the assessment of future remnant liver. Dig Surg. 2014;31:255–68. https://doi.org/10.1159/000364836.
Shoup M, Gonen M, D’Angelica M, Jarnagin WR, DeMatteo RP, Schwartz LH, Tuorto S, Blumgart LH, Fong Y. Volumetric analysis predicts hepatic dysfunction in patients undergoing major liver resection. J Gastrointest Surg. 2003;7:325–30. https://doi.org/10.1016/s1091-255x(02)00370-0.
Ferrero A, Viganò L, Polastri R, Muratore A, Eminefendic H, Regge D, Capussotti L. Postoperative liver dysfunction and future remnant liver: where is the limit? World J Surg. 2007;31:1643–51. https://doi.org/10.1007/s00268-007-9123-2.
Breitenstein S, Apestegui C, Petrowsky H, Clavien PA. “State of the art” in liver resection and living donor liver transplantation: a worldwide survey of 100 liver centers. World J Surg. 2009;33:797. https://doi.org/10.1007/s00268-008-9878-0.
Abdalla EK, Adam R, Bilchik AJ, Jaeck D, Vauthey J-N, Mahvi D. Improving resectability of hepatic colorectal metastases: expert consensus statement. Ann Surg Oncol. 2006;13:1271–80. https://doi.org/10.1245/s10434-006-9045-5.
Abdalla EK, Barnett CC, Doherty D, Curley SA, Vauthey J-N. Extended hepatectomy in patients with hepatobiliary malignancies with and without preoperative portal vein embolization. Arch Surg. 2002;137:675–81. https://doi.org/10.1001/archsurg.137.6.675.
Vauthey J-N, Dixon E, Abdalla EK, Helton WS, Pawlik TM, Taouli B, Brouquet A, Adams RB, American Hepato-Pancreato-Biliary A, Society of Surgical O, Society for Surgery of the Alimentary T. Pretreatment assessment of hepatocellular carcinoma: expert consensus statement. HPB (Oxford). 2010;12:289–99. https://doi.org/10.1111/j.1477-2574.2010.00181.x.
Ribero D, Chun YS, Vauthey J-N. Standardized liver volumetry for portal vein embolization. Semin Intervent Radiol. 2008;25:104–9. https://doi.org/10.1055/s-2008-1076681.
de Graaf W, Bennink RJ, Vetelainen R, van Gulik TM. Nuclear imaging techniques for the assessment of hepatic function in liver surgery and transplantation. J Nucl Med. 2010;51:742–52. https://doi.org/10.2967/jnumed.109.069435.
de Graaf W, van Lienden KP, Dinant S, Roelofs JJTH, Busch ORC, Gouma DJ, Bennink RJ, van Gulik TM. Assessment of future remnant liver function using hepatobiliary scintigraphy in patients undergoing major liver resection. J Gastrointest Surg. 2010;14:369–78. https://doi.org/10.1007/s11605-009-1085-2.
Espersen C, Borgwardt L, Larsen PN, Andersen TB, Stenholt L, Petersen LJ. Nuclear imaging methods for the prediction of postoperative morbidity and mortality in patients undergoing localized, liver-directed treatments: a systematic review. EJNMMI Res. 2020;10:101. https://doi.org/10.1186/s13550-020-00687-1.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clin Res ed). 2009;339:b2535–b2535. https://doi.org/10.1136/bmj.b2535.
Brown KM, Geller DA. What is the learning curve for laparoscopic major hepatectomy? J Gastrointest Surg. 2016;20:1065–71. https://doi.org/10.1007/s11605-016-3100-8.
Cho A, Chung YE, Choi JS, Kim KS, Choi GH, Park YN, Kim M-J. Feasibility of preoperative FDG PET/CT total hepatic glycolysis in the remnant liver for the prediction of postoperative liver function. Am J Roentgenol. 2017;208:624–31. https://doi.org/10.2214/ajr.16.16450.
Otsuki K, Asano T, Okazumi S, Enomoto K, Takayama W, Shinohara Y, Miura F, Isono K. Preoperative evaluation of residual liver function for extended hepatic resection with positron emission tomography and l-[methyl-11C] methionine. Hepatol Res. 1997;7:43–7. https://doi.org/10.1016/S0928-4346(97)00371-X.
Yumoto Y, Yagi T, Sato S, Nouso K, Kobayashi Y, Ohmoto M, Yumoto E, Nagaya I, Nakatsukasa H. Preoperative estimation of remnant hepatic function using fusion images obtained by 99mTc-labelled galactosyl-human serum albumin liver scintigraphy and computed tomography. Br J Surg. 2010;97:934–44. https://doi.org/10.1002/bjs.7025.
Kokudo N, Vera DR, Tada K, Koizumi M, Seki M, Matsubara T, Ohta H, Yamaguchi T, Takahashi T, Nakajima T, Muto T. Predictors of successful hepatic resection: prognostic usefulness of hepatic asialoglycoprotein receptor analysis. World J Surg. 2002;26:1342–7. https://doi.org/10.1007/s00268-002-6262-3.
Chapelle T, Op De Beeck B, Huyghe I, Francque S, Driessen A, Roeyen G, Ysebaert D, De Greef K. Future remnant liver function estimated by combining liver volumetry on magnetic resonance imaging with total liver function on 99m Tc-mebrofenin hepatobiliary scintigraphy: can this tool predict post-hepatectomy liver failure? HPB. 2016;18:494–503. https://doi.org/10.1016/j.hpb.2015.08.002.
Dinant S, de Graaf W, Verwer BJ, Bennink RJ, van Lienden KP, Gouma DJ, van Vliet AK, van Gulik TM. Risk assessment of posthepatectomy liver failure using hepatobiliary scintigraphy and CT volumetry. J Nucl Med. 2007;48:685–92. https://doi.org/10.2967/jnumed.106.038430.
Hayashi H, Beppu T, Okabe H, Kuroki H, Nakagawa S, Imai K, Nitta H, Chikamoto A, Ishiko T, Baba H. Functional assessment versus conventional volumetric assessment in the prediction of operative outcomes after major hepatectomy. Surgery. 2015;157:20–6. https://doi.org/10.1016/j.surg.2014.06.013.
Cieslak KP, Bennink RJ, de Graaf W, van Lienden KP, Besselink MG, Busch ORC, Gouma DJ, van Gulik TM. Measurement of liver function using hepatobiliary scintigraphy improves risk assessment in patients undergoing major liver resection. HPB. 2016;18:773–80. https://doi.org/10.1016/j.hpb.2016.06.006.
Olthof PB, Coelen RJS, Bennink RJ, Heger M, Lam MF, Besselink MG, Busch OR, van Lienden KP, van Gulik TM. (99m)Tc-mebrofenin hepatobiliary scintigraphy predicts liver failure following major liver resection for perihilar cholangiocarcinoma. HPB (Oxford). 2017;19:850–8. https://doi.org/10.1016/j.hpb.2017.05.007.
Rassam F, Olthof PB, Takkenberg BR, Beuers U, Klümpen HJ, Bennink RJ, van Lienden KP, Besselink MG, Busch OR, Verheij J, van Gulik TM. Scintigraphic liver function and transient elastography in the assessment of patients with resectable hepatocellular carcinoma. HPB (Oxford). 2019;21:626–35. https://doi.org/10.1016/j.hpb.2018.09.021.
Hirai I, Kimura W, Fuse A, Suto K, Urayama M. Evaluation of preoperative portal embolization for safe hepatectomy, with special reference to assessment of nonembolized lobe function with 99mTc-GSA SPECT scintigraphy. Surgery. 2003;133:495–506. https://doi.org/10.1067/msy.2003.138.
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, Koch M, Makuuchi M, Dematteo RP, Christophi C, Banting S, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Yokoyama Y, Fan ST, Nimura Y, Figueras J, Capussotti L, Büchler MW, Weitz J. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149:713–24. https://doi.org/10.1016/j.surg.2010.10.001.
Chapelle T, Op de Beeck B, Driessen A, Roeyen G, Bracke B, Hartman V, Huyghe I, Morrison S, Ysebaert D, Francque S. Estimation of the future remnant liver function is a better tool to predict post-hepatectomy liver failure than platelet-based liver scores. Eur J Surg Oncol. 2017;43:2277–84. https://doi.org/10.1016/j.ejso.2017.08.009.
Chapelle T, Op de Beeck B, Roeyen G, Bracke B, Hartman V, De Greef K, Huyghe I, Van der Zijden T, Morrison S, Francque S, Ysebaert D. Measuring future liver remnant function prior to hepatectomy may guide the indication for portal vein occlusion and avoid posthepatectomy liver failure: a prospective interventional study. HPB (Oxford). 2017;19:108–17. https://doi.org/10.1016/j.hpb.2016.11.005.
Serenari M, Collaud C, Alvarez FA, de Santibañes M, Giunta D, Pekolj J, Ardiles V, de Santibañes E. Interstage assessment of remnant liver function in ALPPS using hepatobiliary scintigraphy: prediction of posthepatectomy liver failure and introduction of the HIBA index. Ann Surg. 2018;267:1141–7. https://doi.org/10.1097/sla.0000000000002150.
Serenari M, Pettinato C, Bonatti C, Zanoni L, Odaldi F, Cucchetti A, Ravaioli M, Fanti S, Pinna AD, Cescon M. Hepatobiliary scintigraphy in the preoperative evaluation of potential living liver donors. Transpl Proc. 2019;51:167–70. https://doi.org/10.1016/j.transproceed.2018.04.087.
Okabe H, Beppu T, Chikamoto A, Hayashi H, Yoshida M, Masuda T, Imai K, Mima K, Nakagawa S, Kuroki H, Nitta H, Ishiko T, Hashimoto D, Yamashita Y, Baba H. Remnant liver volume-based predictors of postoperative liver dysfunction after hepatectomy: analysis of 625 consecutive patients from a single institution. Int J Clin Oncol. 2014;19:614–21. https://doi.org/10.1007/s10147-013-0591-0.
Yoshida M, Shiraishi S, Sakaguchi F, Utsunomiya D, Tashiro K, Tomiguchi S, Okabe H, Beppu T, Baba H, Yamashita Y. Fused 99m-Tc-GSA SPECT/CT imaging for the preoperative evaluation of postoperative liver function: can the liver uptake index predict postoperative hepatic functional reserve? Jpn J Radiol. 2012;30:255–62. https://doi.org/10.1007/s11604-011-0041-8.
Nanashima A, Sumida Y, Abo T, Tanaka K, Takeshita H, Hidaka S, Yano H, Sawai T, Obatake M, Yasutake T, Nagayasu T. Clinicopathological and intraoperative parameters associated with postoperative hepatic complications. Hepatogastroenterology. 2007;54:839–43.
Fujioka H, Kawashita Y, Kamohara Y, Yamashita A, Mizoe A, Yamaguchi J, Azuma T, Furui J, Kanematsu T. Utility of technetium-99m-labeled-galactosyl human serum albumin scintigraphy for estimating the hepatic functional reserve. J Clin Gastroenterol. 1999;28:329–33. https://doi.org/10.1097/00004836-199906000-00009.
Kwon AH, Matsui Y, Ha-Kawa SK, Kamiyama Y. Functional hepatic volume measured by technetium-99m-galactosyl-human serum albumin liver scintigraphy: comparison between hepatocyte volume and liver volume by computed tomography. Am J Gastroenterol. 2001;96:541–6. https://doi.org/10.1111/j.1572-0241.2001.03556.x.
Kwon AH, Matsui Y, Kaibori M, Kamiyama Y. Functional hepatic regeneration following hepatectomy using galactosyl-human serum albumin liver scintigraphy. Transpl Proc. 2004;36:2257–60. https://doi.org/10.1016/j.transproceed.2004.08.075.
Kwon AH, Matsui Y, Kaibori M, Ha-Kawa SK. Preoperative regional maximal removal rate of technetium-99m-galactosyl human serum albumin (GSA-Rmax) is useful for judging the safety of hepatic resection. Surgery. 2006;140:379–86. https://doi.org/10.1016/j.surg.2006.02.011.
Nanashima A, Abo T, Kudo T, Sakamoto I, Hayashi H, Murakami G, Takeshita H, Hidaka S, Kido Y, Nagayasu T. Usefulness of examining hepatic functional volume using technetium-99m galactosyl serum albumin scintigraphy in hepatocellular carcinoma. Nucl Med Commun. 2013;34:478–88. https://doi.org/10.1097/MNM.0b013e32835f945f.
Truant S, Baillet C, Deshorgue AC, El Amrani M, Huglo D, Pruvot FR. Contribution of hepatobiliary scintigraphy in assessing ALPPS most suited timing. Updates Surg. 2017;69:411–9. https://doi.org/10.1007/s13304-017-0481-5.
Acknowledgements
None.
Funding
CE received a research scholarship from Aalborg University Hospital for the completion of the study.
Author information
Authors and Affiliations
Contributions
LJP, LB, PNL, and CE contributed to conception and design. LS was involved in the literature search. TBA, LJP, and CE contributed to title and abstract screening. TBA and LJP were involved in full text screening. CE, LB, PNL, and LJP contributed to data extraction. CE, LB, PNL, and LJP were involved in analysis/interpretation of data. CE contributed to drafting the manuscript. All authors discussed the results and implications, commented on the manuscript at all stages, and critically revised the manuscript. All authors contributed to final approval of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. No ethical approval or informed consent was obtained for this systematic review, as it only contains data from previously published articles and no individual data.
Consent for publication
Not applicable.
Competing interests
Lars J. Petersen has received speaker fees from Astellas Pharma and Bayer, but has no competing interests related to this manuscript. The remaining authors have no conflicts of interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Espersen, C., Borgwardt, L., Larsen, P.N. et al. Comparison of nuclear imaging techniques and volumetric imaging for the prediction of postoperative mortality and liver failure in patients undergoing localized liver-directed treatments: a systematic review. EJNMMI Res 11, 80 (2021). https://doi.org/10.1186/s13550-021-00816-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13550-021-00816-4