Abstract
Background
Burn trauma is one of the major causes of morbidity and mortality worldwide. The standard management of burn wounds consists of early debridement, dressing changes, surgical management, and split-thickness skin autografts (STSGs). However, there are limitations for the standard management that inclines us to find alternative treatment approaches, such as innovative cell-based therapies. We aimed to systematically review the different aspects of cell-based treatment approaches for burn wounds in clinical trials.
Methods
A systematic search through PubMed, Medline, Embase, and Cochrane Library databases was carried out using a combination of keywords, including “Cell transplantation”, “Fibroblast”, “Keratinocyte”, “Melanocyte”, or “Stem Cell” with “Burn”, “Burn wound”, or “Burn injury”. Firstly, titles and abstracts of the studies existing in these databases until “February 2024” were screened. Then, the selected studies were read thoroughly, and considering the inclusion and exclusion criteria, final articles were included in this systematic review. Moreover, a manual search was performed through the reference lists of the included studies to minimize the risk of missing reports.
Results
Overall, 30 clinical trials with 970 patients were included in our study. Considering the type of cells, six studies used keratinocytes, nine used fibroblasts, eight used combined keratinocytes and fibroblasts, one study used combined keratinocytes and melanocytes, five used combined keratinocytes and fibroblasts and melanocytes, and one study used mesenchymal stem cells (MSCs). Evaluation of the preparation type in these studies showed that cultured method was used in 25 trials, and non-cultured method in 5 trials. Also, the graft type of 17 trials was allogeneic, and of 13 other trials was autologous.
Conclusions
Our study showed that employing cell-based therapies for the treatment of burn wounds have significant results in clinical studies and are promising approaches that can be considered as alternative treatments in many cases. However, choosing appropriate cell-based treatment for each burn wound is essential and depends on the situation of each patient.
Similar content being viewed by others
Introduction
Burn trauma is one of the major causes of morbidity and mortality worldwide. According to the World Health Organization (WHO), an estimated 180,000 deaths every year are caused by burn injuries. The study of the global burden of disease showed that approximately nine million new cases of burn injury sought medical care in 2019 [1]. Currently, burn wounds’ standard of care consists of infection prevention, early debridement, dressing changes, and surgical management (excising the necrotic tissue followed by skin grafting) [2]. Standard treatment for larger burn injuries is meshed split-thickness skin graft (STSG). Prolonged preparation process, less functionality, and donor site-associated morbidities are limitations in severely burned patients [3,4,5]. Therefore, healing time and prevention of scar formation in patients with severe burn injuries are still major concerns [6], which may not be satisfactory in all patients treated with standard of care. In addition, major burn injuries with ≥ 15% of the total body surface area (TBSA) [7] are at high risk of infection and consequent co-morbidities, which may also lead to septic shock and death [8]. For this reason, other treatment approaches should also be considered for managing burn wounds.
Innovative cell therapies are rapidly advancing as a regenerative strategy for burn wounds management and may offer great hope in the future [4, 9]. Different types of cells, such as keratinocytes, fibroblasts, mesenchymal stem cells (MSCs), embryonic stem cells (ESCs), umbilical cord stem cells (USCs), and induced pluripotent stem cells (iPSCs), have been assessed for the treatment of burn wounds in preclinical and clinical studies [10, 11]. These cells can be delivered by different routes, including local application (e.g. matrices/scaffold-assisted delivery and spraying methods) [12, 13], local injection (subcutaneously or intradermal) [14], and systemic delivery by intravenous injection [15, 16]. However, an ideal cell type and delivery method for the effective administration of cells for burn wounds has not yet been elucidated. Cell transplantation can be used in autologous, allogeneic, or xenogeneic settings and by cultured or non-cultured methods [17]. Studies have shown that transplantation of autologous [18] and allogeneic [19] keratinocytes and fibroblasts can improve burn wound healing in patients. Nevertheless, the superiority of stem cells over other cell types for the healing of burn wounds has been shown by preclinical and clinical studies [14]. Transplantation of stem cells promotes faster wound healing and effective tissue regeneration through multiple mechanisms: reducing the formation of granulation tissue, enhancing neoangiogenesis, reducing immune cell infiltration, accelerating extracellular matrix (ECM) synthesis, inhibiting inflammatory responses, and reducing infection and fibrosis. In addition, stem cells have the capability to differentiate and proliferate in the transplanted area [20,21,22]. These cells can also create a favorable niche for wound healing through the secretion of cytokines, chemokines, and growth factors in response to environmental stimuli. Chemokines, cytokines, and growth factors secreted from stem cells cause the migration and proliferation of fibroblasts, endothelial cells and keratinocytes, leading to the acceleration of wound healing [21, 23].
To the best of our knowledge, there is still a lack of a comparative study to outline the advantages and disadvantages of different cell-based treatment approaches. In this systematic review, we outlined the feasibility and effectiveness of cell-based therapy in clinical trials. Some of these clinical trials have used cells alone, while others used a combination of cells with adjuvants, including biomaterials and scaffolds. However, the adjuvants served to optimize the delivery of the cells, while the cells themselves were responsible for the main therapeutic effects. This highlights the importance of the cells in the therapeutic process, with the adjuvants playing a supportive role in enhancing their efficacy. We aimed to review the variations in the used cell types (keratinocytes, melanocytes, fibroblasts, or stem cells), preparation type (cultured or non-cultured), graft type (autologous or allogeneic), and the delivery rout (local application or graft) (Fig. 1), and their influence on the outcomes of the treatment approaches such as wound healing, scar quality, graft take, and complications.
Methods
Literature search strategy
The selection of studies in this review was performed using the PRISMA-2020 scoping review protocol and checklist. A comprehensive search of the electronic databases PubMed, Medline, Embase, and Cochrane Library was conducted for studies published until February 2024 on the clinical use of cell-based therapies for the treatment of burn wounds. Specific search strategies used for each database are presented in the Supplementary file (Table S1); briefly, a combination of the search terms including “Cell transplantation”, “Fibroblast”, “Keratinocyte”, “Melanocyte”, or “Stem Cell” with “Burn”, “Burn wound”, or “Burn injury” was used to search through he databases. Also, a search through google scholar was performed and reference lists of the included studies were screened to minimize the risk of missing relevant studies.
Inclusion and exclusion criteria
The inclusion criteria for this systematic review were all published randomized or non-randomized clinical trials, published until February 2024, and in the English language. The studies must have assessed a cell-based treatment approach for burn wounds in patients of any age.
The exclusion criteria were case-controls, case reports, case-series, observational studies, commentaries, editorials, non-English language studies, and studies not available in full-text, including conference abstracts.
Study screening and reporting
Two authors (YN, YY) independently screened titles and abstracts followed by full-texts using the inclusion criteria and selected studies to be included in the review. The data extracted from these studies include number of participants, mean age, burn degree (superficial-, superficial/deep partial-, or full-thickness), mean TBSA, trial design, cell type (keratinocyte, melanocyte, fibroblast, or stem cell), preparation type (cultured or non-cultured), graft type (autologous or allogeneic), dose (number of cells), biomaterial composition, delivery route (spraying, local application or graft), control type, and combination with other treatments.
Results
Study selection
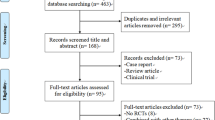
Overall, 5923 reports were found from databases by the search strategy after removing duplicate reports of these databases (1118 reports), and were screened for titles and abstracts. As a result, 5723 reports were excluded, and 200 reports were searched for the availability of full-texts. A number of 200 full-texts were read thoroughly and carefully for the assessment of their eligibility. Eventually, 22 clinical trials were included from the databases. Also, a search through google scholar was performed, and the reference lists of the included studies from databases were checked for possible remaining studies. Fifteen studies were found from this search, of which, eight studies were included. Overall, a total number of 30 clinical trials were included in this systematic review (Fig. 2).
Main findings
A total of 970 patients were enrolled in all 30 included trials. The minimum mean TBSA was 5%, and the maximum was 76.9% among trials. The degree of burns was partial-thickness in 14 trials [19, 24,25,26,27,28,29,30,31,32,33,34,35,36], full-thickness in 11 trials [3, 37,38,39,40,41,42,43,44,45,46], and mixed in five trials [18, 47,48,49,50]. Six studies used keratinocytes [24, 29, 31, 35, 37, 42], nine used fibroblasts [25,26,27, 38, 41, 44, 46, 48, 49], eight used combined keratinocytes and fibroblasts [19, 33, 39, 40, 43, 45, 47, 50], one study used combined keratinocytes and melanocytes [3], five used combined keratinocytes and fibroblasts and melanocytes [18, 28, 30, 32, 36], and one study used MSCs [34]. The cultured method was used in 25 trials [3, 19, 24,25,26,27, 29, 31, 33,34,35, 37,38,39,40,41,42,43,44,45,46,47,48,49,50] and the non-cultured method was used in five trials [18, 28, 30, 32, 36]. The graft type of 17 trials was allogeneic [19, 24,25,26,27, 29, 31, 33,34,35, 38, 41, 43, 44, 48,49,50], and 13 trials were autologous [3, 18, 28, 30, 32, 36, 37, 39, 40, 42, 45,46,47]. All five non-cultured trials used the autologous method [18, 28, 30, 32, 36], while cultured trials used both allogeneic and autologous [3, 19, 24,25,26,27, 29, 31, 33,34,35, 37,38,39,40,41,42,43,44,45,46,47,48,49,50]. STSG was the most common type of control and combination therapy across all studies. Eighteen studies have also used biomaterials and scaffolds as adjuvants in their cell-based treatment approaches [3, 19, 25,26,27, 29, 31, 33, 38,39,40, 43,44,45, 47,48,49,50]. A wide variety of scaffolds and dermal or skin substitutes were used, including Biobrane® synthetic wound dressing, TransCyte®, StrataGraft®, Apligraf®, MatriDerm®, and Alloskin. The most common biomaterial used in these scaffolds and products was collagen type I derived from animal sources.
A summary of the included studies is presented in Table 1, depicting study characteristics, including number of participants, mean age, burn degree (superficial-, superficial/deep partial-, or full-thickness), mean TBSA percentage, trial design, cell type (keratinocyte, melanocyte, fibroblast, or stem cell), preparation type (cultured or non-cultured), graft type (autologous/allogeneic), dose (number of cells), biomaterial composition, delivery route (spraying, local application or graft), control type, and combination with other treatments. There is also a summary of results of the studies, including re-epithelialization, scar quality (the Patient and Observer Scar Assessment Scale; POSAS, and Vancouver Scar Scale; VSS), graft take or loss, and complications which are presented in Table 2.
Discussion
In this section, we offer critical insights into different aspects of cell-based therapies from the included studies, providing the latest updates with more detail in this exciting field of research.
Cell types
Different types of cells have been used in clinical trials to promote healing and tissue regeneration in burn wounds. These trials have mainly compared cell-based therapies with skin grafts and conventional dressings. Cell-based therapy promotes the wound healing process mainly by enhancing re-epithelialization and angiogenesis. Keratinocytes and fibroblasts are the principal cells that are involved in the regeneration of the burnt tissue. Therefore, keratinocytes and fibroblasts are potential therapeutic targets as they are necessary in all three phases of burn wound healing (inflammatory, proliferative, and remodeling phases) [51, 52]. These cells are used in clinical trials in different forms, such as autologous or allogeneic, cultured or non-cultured, and with adjuvant or scaffold-loaded. Here we describe the application of different types of cells and their possible underlying mechanisms of action in skin regeneration.
Keratinocytes are the main cells that participate in epidermal remodeling in the proliferative phase of burn wound healing. Migrating keratinocytes can form a new epidermal layer, regenerate hair follicles and sweat glands, restore barrier functions, promote angiogenesis, and regulation of immune responses via secretion of various proteins, growth factors, and cytokines such as collagen IV, collagen VII, laminin V, migration stimulating factor (MSF), nerve growth factor (NGF), vascular endothelial growth factor (VEGF), tumor necrosis factor (TNF)-α, interleukin (IL)-1 [11, 53]. Epidermal cell transplantation or epidermal substitutes are currently used as biological burn wound dressing in clinical trials. Application of keratinocytes in different forms, such as cultured epithelial autografts (CEA) [29, 35, 37], cultured epidermal allograft (CEAllo) [24, 31], and other bioengineered skin substitute (BSS) [3, 43] in deep partial- and full-thickness burn wounds had promising results. In trials using CEA and CEAllo for deep partial-thickness burns, the wound healing and re-epithelialization time were significantly faster than in the control site [24, 29, 31, 35, 37]. The dried form of CEAllo was recently used in a phase I/II clinical trial. It is more beneficial since it can be stored at room temperature and used as an off-the-shelf product. Dried CEAllo contains bioactive substances involved in the construction of physiological-like niches to promote recipient cell proliferation and migration in the wound bed [35]. Cultured proliferating epidermal cells consisting of allogeneic keratinocytes and melanocytes have been reported to have significantly better epithelialization compared to the standard treatment. Significantly better POSAS score of the observer and of the patient, better melanin and erythema index, improved skin colorimeters, and higher elasticity for the experimental area were also reported in this trial [3].
As the second type of cells, fibroblasts are the main cells responsible for dermal remodeling and connective tissue formation in the proliferative and remodeling phase of burn wound healing. They promote reconstruction of ECM by the deposition of collagen, fibrillin, elastin, and secretion of matrix metalloproteinases (MMPs), the tissue inhibitors of metalloproteinases (TIMPs), fibroblast growth factor (FGF), transforming growth factor (TGF)-β, keratinocyte growth factor (KGF), and granulocyte-macrophage colony-stimulating factor (GM-CSF) within the wound site. They can also promote angiogenesis and granulation tissue formation, and they can support the epithelial layer via promoting epidermal cell replication, differentiation, migration, and spreading 56. Autologous and allogeneic fibroblast transplantation trials were designed to accelerate wound healing in the treatment of full-thickness burn wounds. Different sources of fibroblasts were used, including healthy donor skin for allograft [41, 44] and patients’ own skin for autograft [46]. Accelerated wound epithelialization and significantly lower average healing time with reduced formation of a hypertrophic cicatrix, mean scar formation and pigmentation score were reported in these studies [41, 44, 46]. FDA-approved allogeneic fibroblast-derived temporary dermal substitute (TransCyte®) (formerly marketed as Dermagraft-TC) is a product that were used in clinical trials for partial-thickness burns. Re-epithelialization time was faster with less hypertrophic scarring and better VSS and pain scale in wounds treated with TransCyte®. The wound care time, and the number of wounds requiring autografting were also less in this approach [25,26,27, 38, 48, 49].
The combination of keratinocytes and fibroblasts for the management of burn wounds seems to be more efficient than single cell therapy as full-thickness burns do not typically heal completely by themselves and result in scar formation, contracture, changes in skin texture, and loss of sensation. Complete epidermal-dermal replacements are required to minimize these complications and improve quality of life [11, 54]. Complete skin substitutes containing both epidermal and dermal cells have been investigated recently to treat full-thickness burns as a temporary or permanent replacement of both layers. [39, 40, 43, 45, 50]. Complete skin substitutes improve the wound healing process more efficiently than epidermal or dermal substitutes alone. ReCell® spraying device, an FDA-approved cell harvesting device that uses non-cultured autologous skin cell suspension (ASCS) containing viable keratinocytes (about 64%), fibroblasts (about 30%), and melanocytes (about 3.5%) [55], is used in randomized control trials (RCTs) to promote thermal burn wound healing. Using ReCell® in deep partial-thickness burns resulted in complete wound healing and reduction in VSS and maximum pain scores. In addition, less donor site and long-term satisfaction with donor site morbidity compared with the controls was reported in trials using ReCell® [18, 32, 36]. Superiority of ASCS combined with STSG for reduction in donor site area has also been reported in other full-thickness skin defects in a recent RCT [56].
Cultured keratinocytes or fibroblasts alone or in combination with each other were also used in the studies. RCTs using cultured skin substitutes (CSS) containing autologous fibroblasts and keratinocytes, also known as autologous engineered skin substitutes (ESS), reported reduced mortality and requirements for donor skin harvesting for grafting [39, 40, 45, 47]. Apligraf® is an FDA-approved cellular full-thickness skin substitute consisting of living allogeneic neonatal fibroblasts and keratinocytes cultured with bovine type I collagen matrix. Using Apligraf® in an RCT resulted in faster healing time and other clinical improvements, including significant better VSS score, pigmentation, vascularity, pliability, and overall cosmetic appearance in Apligraf® sites compared to control sites [50]. Near-diploid neonatal human keratinocyte cell line (NIKS)-based BSS, which is another full-thickness skin substitute consisting of keratinocytes combined with fibroblasts, was also used in full-thickness burns, resulted in 100% closure of burn wounds and improvement in the POSAS scores with minimal clinical evidence of fibrosis compared with cadaver allograft [43]. Using StrataGraft®, human skin substitute containing NIKS and human dermal fibroblasts cultured with type I collagen, in deep partial-thickness burns resulted in durable wound closure, significant reduction in required autografting, significant lower mean pain scores [19, 33].
In addition, bone marrow-derived MSCs (BM-MSCs) was the only stem cell used in published clinical trials for burn wounds. The safety and efficacy of local application of BM-MSC were reported in deep partial-thickness burn wounds. BM-MSC therapy for deep partial-thickness burn wounds resulted in 100% wound closure, improvement in the POSAS scores, re-pigmentation, and regenerative changes [34]. Overall, although the use of aforementioned cells has been shown to be promising, the combination of these cells seems to be more beneficial; however, more studies are necessary for choosing the best approach depending on the clinical situation.
Cell preparation methods (cultured/non-cultured)
Both cultured and non-cultured cell-based strategies were used in clinical trials with promising outcomes. However, the advantages and limitations of each strategy should be considered. The cultured-based strategy was the most frequent method that has been used in these clinical trials [3, 19, 24,25,26,27, 29, 31, 33, 35, 37,38,39,40,41,42,43,44,45,46,47,48,49,50]. This strategy offers several advantages and also has some disadvantages over non-cultured strategies for burn wound healing. In the cultured-based strategy, the expanded population of cells provides an adequate supply for effective grafting, especially in extensive burns, which have limited donor sites and need more cells for transplantation [57,58,59]. However, the procedure of culturing is more expensive, complex, and time-consuming and it cannot be used immediately for urgent patients [60]. Improved deposition and remodeling of collagen, formation of the dermo-epidermal junction, keratinocytes survival, decreased myofibroblast formation and decreased wound contraction can be achieved by culturing methods [44]. On the other hand, non-cultured strategies are more simple, cost-effective, and immediately available, but the number of available cells may be limited in some cases. Although the non-cultured strategy was less used in clinical trials [18, 28, 30, 32, 36], it has been shown promising results in improving burn wound repair. Further research is needed to optimize its use and determine long-term safety and efficacy. Herein, we describe the cell preparation approaches which were used in clinical trials [58, 59].
CEA, CEAllo, cultured fibroblasts, and CSS are cultured-based strategies that were used in clinical trials [3, 19, 24,25,26, 29, 31, 33, 35, 37,38,39,40,41,42,43,44,45,46,47,48,49,50]. Culturing epidermal keratinocytes were one of the most used cultured-based cell approaches in clinical trials [3, 24, 29, 31, 35, 37]. The epidermal keratinocyte culturing method was first introduced by Rheinwald and Green in 1975 [61] and has developed for a long time in order to accelerate wound healing. CEA and CEAllo are considered alternative care for the homeostatic stage of wound healing. They have been used in sheet or suspension form to accelerate re-epithelialization in burn wounds [29, 42]. There were some culturing-related limitations in clinical trials using CEA and CEAllo. The culture period of CEA and CEAllo is long (approximately 2–4 weeks from biopsy to transplantation) mainly due to the slow proliferation rate of keratinocytes [3, 29, 37]. This long culture time with delayed healing results in an excessive accumulation of ECM and more hypertrophic scarring. Failure to improve scar formation and quality in trials using CEA and CEAllo was associated with this long culture time [24, 29, 31, 35, 37]. Using human undifferentiated keratinocytes (HUKs) instead of using fully differentiated keratinocytes or using biological membranes to promote epidermal cell proliferation was useful to overcome the long culture time in some studies. Significant improvements in skin colorimeters, POSAS, melanin index, and erythema index were reported in a trial using proliferating keratinocytes [3].
In addition to the beneficial role of CSS for full-thickness burns replacement, co-culturing of keratinocytes and fibroblasts in CSS preparation can provide better skin structure. There is a crosstalk between keratinocytes and dermal fibroblasts, which improve the burn wound healing process. Disruption of this crosstalk, as seen in delayed epithelialization, increases the risk of hypertrophic scar formation [62]. Co-cultured keratinocytes and fibroblasts promote proliferation and migration by creating cytokine loops between the two cell types, similar to native skin [63, 64]. Despite these advantages, long culture time of autologous CSS (about four weeks from biopsy to preparation) limits its availability for severe burn patients [39].
The only non-cultured product that was used in clinical trials was ReCell® [18, 28, 32, 36]. This spraying device can be used alone to directly spray epithelial cells isolated from the patients’ skin biopsy [28], applied along with STSG [18, 32], or combined with biosynthetic skin dressings [36]. In the comparison of the ReCell® with conventional grafting, biopsy areas, and postoperative pain were significantly smaller [28]. Using ReCell® combined with STSG reduced the donor site area and increased satisfaction with donor site outcomes [18, 32]. In addition, using ReCell® combined with Biobrane® synthetic wound dressing decreased healing time with fewer dressing changes, less pain, and better scar outcomes [36]. However, the non-inferiority properties of ReCell® have been mainly reported in non-cultured based clinical trials while better re-epithelialization was more significant in the cultured-based trials. This may be due to the less number of keratinocytes in the non-cultured method, which was reported in a preclinical study [65]. ReCell® system needs a smaller harvested area due to its ability to spread cells with a high ratio (1:80) to cover a large area [28]. The main advantages of this non-cultured method are faster procedure time and minimal tissue manipulation, which results in better management in urgent patients and fewer donor site-related complications.
Using non-cultured skin cell suspension or cultured skin cells can be beneficial for re-pigmentation to some degree. But it should be considered that culturing melanocytes alongside with keratinocytes (in CEA) or with fibroblasts and keratinocytes (in CSS) may result in non-uniform pigmentation, as mentioned in some studies. This may be due to a more rapid growth rate of keratinocytes than melanocytes which leads to melanocyte dilution to small proportions known as “passenger melanocytes” [40]. Therefore, using non-cultured skin cell suspension (melanocytes existed in epidermal harvests [55]) or adding selective cultured melanocytes into CEA or CSS may be more appropriate to achieve uniform pigmentation [39, 66].
In conclusion, the choice between cultured and not-cultured methods for burn wound repair depends on several factors, including the severity of the burn wound, the patient’s condition and urgency, and available resources.
Type of graft (autologous/allogeneic)
Both autografts and allografts were used in clinical trials, and the most suitable approach differs in every patient. The advantages and limitations of each strategy are mentioned as follows. Autografts are immunologically compatible and do not require immunosuppressive drugs leading to no rejection risk and lower risk of infection, respectively. However, there are some limitations which may interrupt wound healing in some patients. The available donor skin is limited, which may be an obstacle in patients with extensive burns. Surgical procedure is required in autografts leading to increased pain, scarring, infection, and longer recovery time in donor sites. Autografts may not be the first choice in critical patients with extensive burns as the procedure of harvesting is time-consuming, and this may result in complications in patients. On the other hand, allografts are immediately available as “off-the-shelf” products, which are beneficial, especially for critical patients. These grafts are not limited by the availability of the patient’s donor site, so they can cover larger areas with no donor site-associated morbidities. However, there might be an increased risk of rejection as they are immunologically incompatible, and immunosuppressive drugs may be needed to address this risk leading to a higher risk of infection. Some clinical studies have reported better healing outcomes with autografts as they can effectively integrate with the wound bed [67,68,69].
CEA, autologous fibroblasts, ASCS (ReCell®), and CSS are autografts, and CEAllo, allogeneic fibroblasts, NIKS-based-substitute, TransCyte®, and Apligraf® are allografts which were used in the included clinical trials. Among autografts, ReCell® is the only non-cultured method which doesn’t have culture time, but the procedure time is reported to be longer than skin grafts, mainly due to the trypsin digestion time (20 min). This leads to patients’ surgical stress and increased economic aspects [28]. Therefore, allografts should be considered in some cases depending on the patient’s condition.
It has been noted that using CEA for deep partial-thickness burns may result in contracture of anatomic parts due to delayed re-epithelialization. So, it may not be an optimal option in urgent situations. Using allogeneic keratinocytes as CEAllo for easy and immediate use in burn wounds reduces the procedure time and associated complications. Cultured epidermal allograft releases various growth factors which stimulate the migration and proliferation of autologous keratinocytes and suppress the contraction of fibroblasts leading to accelerated re-epithelialization and wound closure. Therefore, early coverage with CEAllo can reduce the healing time of wounds and prevent the formation of hypertrophic burn scars in deep partial-thickness burns [24].
Despite concerns about immune rejection in allografts, no significant adverse effects, including immunologic reactions were reported in clinical trials. Allogeneic fibroblast is an example that seems to be tolerated by immunologically unmatched donors [41, 44]. Using CEAllo may carry a risk of rejection, but it has been demonstrated that CEAllo accelerates the wound healing process without immune rejection and can be replaced with autologous cells after a needed period [29]. NIKS-based BSS was also acutely non-antigenic and strong immune responses were not present after transplantation [43]. Although some adverse events reported after using StrataGraft®, no patients showed signs of a clinically detrimental immune response to StrataGraft®, such as tissue rejection. No adverse effects or immune rejection were also observed with BM-MSC transplantation [34].
Allograft is used as a temporary cover in some trials to protect the dermis, promote wound healing, and prepare an uncolonized and well-vascularized wound environment to promote the proliferation and migration of cells. Allograft doesn’t seem to remain permanently in the wound bed and may gradually be replaced by the patient’s epidermal cells [35]. This may lead to the need for the application of autografts following allografts to complete healing in some cases. Therefore, requiring autografting can be measured in clinical studies using allograft to determine the adequacy of allogeneic transplantation. In some clinical trials that used allograft, faster wound healing resulted in less need for autografting [27].
Combination therapies and biomaterial adjuvants
Among the included studies, 10 studies have used cell-based therapies combined with other treatments [3, 18, 30, 31, 36, 42, 44, 46, 48, 50]. Six of them have used autologous meshed STSG [3, 18, 30, 44, 48, 50], and the others have used Biobrane® synthetic wound dressing [36], silicone net dressing [31], low-level laser irradiation [46], and fibrin sealant [42]. However, the combination effect of these treatments was not assessed for the following reasons: (1) studies did not have a control group [42, 46], (2) studies used the same treatments in the control groups [3, 18, 30, 31, 36, 44, 48, 50], or (3) studies compared the combination of these treatments with a different treatment group [36]. In the latter study [36], the effect of Biobrane® was assessed alone or in combination with ASCS (ReCell®) in comparison to standard care. Both treatment groups healed approximately 50% faster than the control group, and adding ASCS to Biobrane® decreased the healing time by about 15% (statistical analysis was not performed). In one study, ASCS combined with meshed STSG was compared with meshed STSG alone in mixed-depth burn wounds [18]. In order to use ASCS for the treatment of burn wounds, a dermis-containing wound bed is necessary [30]. Similarly, combination of ASCS + STSG was used in a recent RCT for the treatment of other full-thickness skin defects [56]. Consistently, in four other included studies that used ASCS without skin graft, the treatment was used in partial-thickness burn wounds that contained dermis [28, 32, 36]. Therefore, the combination effect of ASCS and STSG was not assessed since ASCS could not be used alone in full-thickness burn wounds.
An important challenge in the process of cell-based therapy approaches is to maintain the viability and functionality of the cells in order to result in favorable outcomes. Major hindering factors include mechanical stress during cell delivery, lack of cell adhesion to wound bed resulting in anoikis (cell death due to ECM detachment), and deficiency of growth factors in wound environment [70].
Formerly, epidermal substitutes were used without a supporting scaffold [71], which had several disadvantages: (1) these substitutes were weak and easily torn, (2) they had insufficient vascular support, (3) they had lower graft takes leading to post-grafting infections, and (4) their production took a considerable amount of time [60]. Consistently, studies have shown that CEAs were not stable during long-term recovery [66]. Moreover, the lack of dermal support would cause significant scar formation. Afterward, studies used biomaterials as support matrices for grafting, which proposed better outcomes and minimized complications [72]. However, if there is sufficient dermal support in partial-thickness burn wounds, CEAs can be used without a dermal scaffold with acceptable outcomes. Twenty-two of the included studies have used cultured dermal or skin substitutes [3, 19, 24,25,26,27, 29, 31, 33, 35, 37,38,39,40,41, 43,44,45, 47,48,49,50]. Except three of these studies [24, 37, 41], all other 19 studies have used biomaterials in the process of dermal or skin substitute production. Moreover, seven studies used topical application of cell suspensions [18, 28, 30, 32, 36, 42, 46] of which two had used biomaterials in the preparation process [36, 42]. Collagen was the mostly used biomaterial in these studies that was used in grafting, local application, and spraying methods.
In skin substitute grafts, collagen plays role as a matrix for the containment of fibroblasts to be grafted alone or with overlaying cultured keratinocytes. Collagen was the only biomaterial in some of the matrices including Apligraf® [50] (bovine type I collagen [73]), Biobrane® [25,26,27, 38, 49] (a silicon nylon membrane bonded with porcine type I collagen [74]), StrataGraft® (murine type I collagen) [19, 33], and a dermal analog [43] (non-bovine type I collagen [75]). In the other matrices collagen was used in combination with other biomaterials including elastin [3] (MatriDerm®; bovine collagen type I, III, and V coated with bovine elastin [76]) and glycosaminoglycan (GAG) [39, 40, 45, 47] (bovine collagen and chondroitin-6-sulfate [77]). Other used biomaterials in the included studies were thermosensitive hydrogel [29, 31], silicon sheet with GAG (Alloskin) [44], and polyglactin acid vicryl mesh in Dermagraft [48]. Biomaterials were also used in spraying cell suspension studies. Biobrane® [36] and fibrin sealant [42] (containing fibrinogen and thrombin [78]) were biomaterials used in these studies.
GAGs are a group of polysaccharides that are present in the cell membrane and ECM of all tissues in the body [79] and play role in several signaling pathways, including cell migration and proliferation [80]. Despite this role, GAGs alone have been shown to decrease the migration rate of keratinocytes in vitro [81]. Therefore, the majority of products that contain GAGs, especially in skin substitutes, are a combination of GAGs and other materials, including type I collagen [82,83,84]. Producing scaffolds similar to the skin’s structure for wound healing is an important goal. Therefore, the majority of skin substitutes that consist of a dermal analog, contain type I collagen. Collagen matrix has been used as a model to simulate wound healing process in in vitro studies [85]. Although collagen alone has been used in skin substitutes [43, 50], studies have shown that this method results in a less stable barrier function and delayed keratinization compared to cadaveric skin graft in mice [86]. To overcome this disadvantage, a combination of collagen with other biomaterials can be used [87], including chitosan [88], GAGs [89], and elastin [90].
Using biomaterials as adjuvants of cell therapy for burn wounds seem to be beneficial. However, most of these biomaterials, especially collagens, are xenogeneic materials. Examples for xenogeneic collagens as biomaterials in the included studies are Apligraf® [73], MatriDerm® [76], and Biobrane® [74]. Although animal-derived collagens have been used widely, it has been reported that they are immunogenic [91]. Therefore their clinical use should always be with caution in those who are not previously sensitized to xenogeneic proteins [92].
Degree and extent of burn injury
Another aspect of the included studies that can be discussed is the degree and extent of burn injury. The degree of burn wounds in the included studies were full-thickness/third-degree [3, 18, 37,38,39,40,41,42,43,44,45,46,47,48,49,50] and partial thickness/second-degree [19, 24,25,26,27,28,29,30,31,32,33,34,35,36, 47,48,49,50]. First-degree burn wounds mainly require conservative treatment [93], and therefore, no study with first-degree burn wounds that had used cell-based therapies was found. From the studies that included full-thickness burn wounds, seven studies have used allogeneic [38, 41, 43, 44, 48,49,50], and nine studies have applied autologous cells [3, 18, 37, 39, 40, 42, 45,46,47]. All of the allogeneic cell approaches have used dermal or skin substitutes, while three of the autologous cell studies have used non-cultured approaches (two cell sprays [18, 42] and one local application with sampler [46]). Of the remaining six autologous cell studies with cultured methods, five used dermal or skin substitutes, and one used CEA without a dermal scaffold. From the studies that included partial-thickness burn wounds, 15 used allogeneic cells (12 dermal or skin substitutes [19, 24,25,26,27, 29, 31, 33, 35, 48,49,50], two local applications of hydrogel-cultured cells [29, 31], and one BM-MSC [34]), and five used autologous cells (four ReCell® spraying method [28, 30, 32, 36] and one CSS [47]). It can be understood that most full-thickness burn wounds were treated with cultured grafting methods, especially with the use of dermal or skin substitutes. This can be due to the necessity of wound closure as soon as possible to prevent subsequent complications [94] and also the essential role of ECM in wound healing [95, 96] and in supporting the transplanted cells [70, 97]. This notion is further supported by the two studies that used spraying methods for CEA and ASCS delivery, which were sprayed in combination with fibrin sealant [42] or over a prior autologous meshed STSG [18]. Although Nilforoushzadeh et al. [46] have not used any scaffolds in combination with the local application of cells for full-thickness burn wounds, they have used autologous fibroblasts which can produce growth factors and ECM components necessary for wound healing [98]. Only one study by Munster et al. [37] used CEA for full-thickness burn wounds, which did not contain any components of dermal ECM. It should be considered that untreated deep partial-thickness burn wounds have compromised healing process and produce high rates of scar tissue. Therefore, early treatment of these wounds are necessary [99]. Moreover, although superficial partial-thickness burn wounds only require standard care or specific wound dressings [100], major superficial partial-thickness burns (TBSA > 15% [7]) need proper cell-based treatment approaches [101].
Depending on the situation, it should be decided which approach is most appropriate. For instance, in full-thickness burn wounds using autologous culturing methods may be more beneficial than other methods. However, these methods require a considerable amount of time to be prepared for grafting [67]. Also, there should be enough healthy donor sites, which is further challenging in extensive burn wounds [68]. Allogeneic dermal or skin substitutes can be used to address this matter since they are ready to use at any time needed, and their production does not require a donor site [69]. However, using allogeneic products have a risk of inducing an immune response [69]. Lack of available donor site is also challenging for extensive partial-thickness burn wounds. Nevertheless, ReCell® autologous cell harvesting device is especially beneficial for these burn wounds if enough donor site is available. It has been shown that using ReCell® reduced the required donor site area by 40 folds compared to STSG for the same wound size [32]. Although, if the extent of the burn wound is so high that enough healthy donor sites cannot not be provided, other cell-based methods should be considered, such as allogeneic dermal or skin substitutes.
Stem cells
Only one study among the included studies used stem cells (local application of allogeneic BM-MSCs) for the treatment of deep partial-thickness burn wounds [34]. The results of this study indicate that BM-MSCs transplantation caused wound healing in all patients with no rejections and improved re-pigmentation. Nevertheless, in the screening process of our study, several studies had used stem cells for the treatment of burn wounds. Although these studies were not included since they were case reports, non-trial clinical studies, or clinical trials with no published results, their assessment may be helpful for future studies (Table 3). Of these studies, eight were clinical trials of which MSCs were used in six of them (ChiCTR2000040932, EUCTR2018-002870-27-DK, NCT02619851, IRCT201209178177N5, IRCT201202169044N1, EUCTR2012-001596-36-ES) and one study used human amniotic epithelial cells (hAECs, NCT05652816). The source of the MSCs in all but one trial (allogeneic umbilical cord-derived MSCs, ChiCTR2000040932) was adipose tissue. In one trial, stem cells were derived from burn wounds, but the type of stem cells was not specified (NCT05344521). Allogeneic stem cells were mostly derived from adipose tissue and were used alone (EUCTR2018-002870-27-DK) or loaded on a hydrogel sheet (NCT02619851) or acellular amniotic membrane (IRCT201209178177N5). Autologous stem cells (MSCs) were also derived from adipose tissue and were used on a silicon sheet scaffold in one study (IRCT201202169044N1), and in another study, stem cells were derived from patients’ own burn wound tissues (no specified type of stem cells) and were loaded on Integra® (NCT05344521). One study did not state whether the MSCs were autologous or allogeneic (EUCTR2012-001596-36-ES). Both deep partial-thickness and full-thickness burn wounds were treated with stem cells in these clinical trials.
A total of 16 non-trial clinical studies and case reports were also found which had used stem cells. The types of these stem cells were mostly MSCs of different sources, including: (1) allogeneic bone marrow (applied alone [102], on pre-clotted platelet-rich plasma [103], and sprayed with fibrin sealant [104]), (2) autologous BM (applied alone [105] and combined with autologous skin graft [106, 107] or surgical treatment [108]), (3) allogeneic umbilical cord blood used alone [105], (4) chorionic tissue alone [109], (5) a combination of allogeneic umbilical cord-lining stem cells used with fibrin sealant [109], (6) allogeneic amniotic membrane with the support of an acellular dermal matrix [110], (7) autologous adipose tissue (in the form of stromal vascular fraction (SVF) used alone [111] or with Integra® [112]), and (8) cadaveric with no specified source tissue [113]. Aside from the mentioned stem cells, amniotic membrane has also been transplanted combined with amniotic fluid stem cells [114] or applied alone [115] for the treatment of burn wounds. Although the treatment effects of amniotic membrane transplantation and amniotic fluid application cannot solely be related to their stem cells content, they should be considered as a way of delivering stem cells to burn wounds. Amniotic membrane contains MSCs alongside with hAECs [116] and amniotic fluid contains a heterogeneous population of cells [117], including MSCs [118].
It can be indicated that MSCs are the most frequently used type of stem cells for the treatment of burn wounds. The studies with available full-text reported that MSCs transplantation improves wound healing [102, 105, 106, 109, 110], re-epithelialization and re-pigmentation [103], decreases pain [110], causes limited hypertrophic scar formation [103, 109], results in good cosmetic and functional outcomes [111, 112], and reduces the time of hospitalization [105, 110].
There are three main sources of stem cells including embryonic stem cells, adult stem cells, and extra-embryonic stem cells. Embryonic stem cell transplantation, in their undifferentiated form, leads to teratoma formation [119, 120], and transplantation of their differentiated form also leads to the induction of immune response [121]. Moreover, providing embryonic stem cells requires the destruction of embryonic structures, and the ethical justification of their use is under debate [122]. Adult stem cells, however, have been widely used since they are found in most body organs (multipotent, oligopotent, and unipotent stem cells) and can be used for autologous purposes [123], but as they are more differentiated, they express more major histocompatibility complex (MHC) molecules and have more immunogenicity; therefore, their allogeneic use is limited. The exceptions are MSCs that despite the low levels of MHC-I and MHC-II antigen expression and being potentially immunogenic [124], induce low levels of immune response due to their immunosuppressive [124] and immunomodulatory effects [125] majorly mediated by MSC-secretome. MSC-secretome mostly contain DNAs, RNAs, micro-RNAs, long non-coding RNAs, surface markers, growth factors, cytokines, and chemokines [126]. This immunomodulatory effect, alongside their migration to the damaged site, induction of skin cell proliferation, and angiogenesis have made them a favorable choice for the treatment of wounds [10]. MSCs can be extracted from various tissues including BM (0.01 − 0.001% of the BM sample content), adipose tissue (5000 cells per 1 gr of the tissue, being 500 times more cells than the same amount of BM), and peripheral blood (1.2–13 cells per one million mononuclear cells) [127]. Overall, the trend toward using BM- and adipose tissue-derived MSCs can be explained by the available number of MSCs in these tissues. Although BM-MSCs were mostly used for burn wounds, it has been shown that adipose-derived MSCs have more proliferative capability, immunomodulatory effects, and growth factor secretion than BM-MSCs [128] and are potentially more beneficial for wound treatments.
Although adult MSCs have shown superiority over other stem cells, extra-embryonic tissues (amnion, chorion, and umbilical cord) also contain MSCs and epithelial stem cells. MSCs of these sources have shown significantly lower immunogenicity [129], higher immunosuppressive, proliferative [130], and differentiation capability [131] compared to adult-MSCs. Moreover, they are isolated at 10–30 × 106 cells per amniotic membrane [132], their extraction is non-invasive, and there is less argument about the ethical justification of their use. Similar to extra-embryonic MSCs, another population of stem cells are present in amniotic membranes called hAECs. They also have immunomodulatory and immunosuppressive capacities, have low immunogenicity and tumorigenicity potential [133], and are isolated at a considerable amount (about 80–300 × 106 cells per placenta) [134]. Although there are approximately ten times more available hAECs than MSCs in an amniotic membrane of a placenta, there are various other parts of a placenta that MSCs can be isolated from [135]. In addition to stem cells isolated from extra-embryonic tissues, the transplantation of whole amniotic membrane has been shown to improve the wound healing process [136]. Amniotic membrane contains the aforementioned stem cells, and therefore, it has anti-inflammatory, pain relieving, anti-scarring, and re-epithelialization properties with low immunogenicity and rejection, which has been used in both cellularized and decellularized (as a scaffold) forms for the treatment of different conditions [137].
Future aspects
Several aspects can be suggested to direct future studies. The results of the studies that used stem cells for the treatment of burn wounds are promising [102, 103, 105, 106, 109,110,111,112]. However, there are still no FDA-approved stem cell-based products for the treatment of these wounds. The interesting characteristics and capabilities of stem cells to evade immune response and induce the wound healing process [124, 125] make them a special target for future studies. Although most of the studies have focused on BM-MSCs and adipose tissue-derived MSCs, other sources of stem cells, especially extra-embryonic sources, can be of interest. Extra-embryonic stem cells can be obtained easily and abundantly while BM and adipose tissue give limited number of stem cells and their extraction is invasive [127]. Of these extra-embryonic sources, hAECs have the potential to differentiate to several types of skin cells, including keratinocytes [138]. Therefore, these cells can be used to improve the outcomes of existing cell-based therapy approaches for burn wound treatment or producing cultured skin substitutes as a replacement for allogeneic skin graft.
Aside from the sources of cells, the methods of delivering cells to the burn wound should also be considered for future studies. The majority of studies have used culturing methods to expand cells on scaffolds or matrices. A limited number of studies have used spraying methods for delivering autologous cells. The spraying delivery method can also be modified for delivering stem cells or a combination of autologous skin cells and stem cells for better wound healing outcomes. Enhanced spraying methods may also be useful such as electro-spray; we previously reviewed different aspects of cell spraying methods, which produce a mist of cells with a more uniform expansion over the wound area [139]. Additionally, cells can also be embedded into dressings for local application. Moreover, 3D bioprinted skin may be inspiring for the treatment of burn wounds. This method can be used to create customized skin grafts with improved functionality and compatibility.
Another aspect for future studies is the combination of cells with other biomaterials. Keratin and chitosan as biomaterials other than collagen can be used as scaffolds for cell delivery [140]. Also, a combined delivery of cells with cell supporting materials for local application of cells can be considered. Furthermore, studies have used amniotic membrane in different ways for burn wounds; although, using a powder form of this membrane may also be of interest. This amniotic ECM powder can be used in combination with different cells as a supporting component. This combination has been used in our recent pilot study for the treatment of burn wounds (unpublished data). In addition, using nanomaterial in cell therapy for burn wounds may be considered in the future. Nanocarriers can be used to contain cells and protect them from the injured and inflamed environment of the burn wound so that these cells can function better and stay viable. Furthermore, nanofibers and nanotubes can be used for the regeneration of burn wounds by improving the produced ECM, which enhances cell adhesion and growth. Although systemic delivery of stem cells for local injuries like burn wounds seems to be impractical, but nanoparticles or nanocarriers may be useful. Magnetic nanoparticles or nanocarriers may be helpful as they can be used to guide the delivered cells to the injured location. Moreover, nanobiomaterials and nano-enriched bioinks can be employed to help produce a 3D bioprinted skin for the treatment of burn wounds [141]. Considering ecological safety, green biomaterials, which have potential clinical implications [142], can also be used as alternatives to conventionally produced nanomaterials combined with cell-based therapies for burn wounds. As for other adjuvants, plants- and seeds-derived products, such as oil and pulp can be used in combination with cell-based therapies to maintain moisture of the wound area and reduce the harshness of the environment for the delivered cells [143,144,145]. Another adjuvant that can be combined with cell-based therapy are exosomes. Stem cell-derived exsosomes have shown various capabilities in regenerative medicine [146]. Co-delivery of these exosomes with cells may have promising results for the treatment of burn wounds. Also, cells can be delivered with certain growth factors like epidermal growth factor (EGF) or FGFs for further support.
Conclusion
Our study showed that using cell-based therapies for the treatment of burn wounds have promising results in clinical studies. Cell-based therapies are emerging as novel approaches for the treatment of several skin disorders, such as melanoma [147], vitiligo [148], and other skin disorders [149]. Therefore, considering the promising results of our study and the employment of cell-based therapies for various skin disorders, we can suggest these approaches as alternatives to the existing treatments for burn wounds.
However, suggesting an absolute and certain alternative cell-based treatment approach for burn wounds seems to be challenging since different types of burn wounds require different approaches. Nevertheless, the advantages and limitations of these approaches in different aspects for different types of burn wounds were discussed in this systematic review.
Data availability
Not applicable.
Abbreviations
- STSG:
-
Split-thickness Skin Autograft
- MSC:
-
Mesenchymal Stem Cell
- WHO:
-
World Health Organization
- TBSA:
-
Total Body Surface Area
- ESC:
-
Embryonic Stem Cell
- USC:
-
Umbilical Cord Stem Cell
- iPSC:
-
Induced Pluripotent Stem Cell
- ECM:
-
Extracellular Matrix
- POSAS:
-
Patient and Observer Scar Assessment Scale
- VSS:
-
Vancouver Scar Scale
- MSF:
-
Migration Stimulating Factor
- NGF:
-
Nerve Growth Factor
- VEGF:
-
Vascular Endothelial Growth Factor
- TNF:
-
Tumor Necrosis Factor
- IL:
-
Interleukin
- CEA:
-
Cultured Epithelial Autografts
- CEAllo:
-
Cultured Epidermal Allograft
- BSS:
-
Bioengineered Skin Substitute
- MMP:
-
Matrix Metalloproteinase
- TIMP:
-
Tissue Inhibitors of Metalloproteinase
- FGF:
-
Fibroblast Growth Factor
- TGF:
-
Transforming Growth Factor
- KGF:
-
Keratinocyte Growth Factor
- GM-CSF:
-
Granulocyte-Macrophage Colony-Stimulating Factor
- ASCS:
-
Autologous Skin Cell Suspension
- RCT:
-
Randomized Control Trial
- CSS:
-
Cultured Skin Substitute
- ESS:
-
Engineered Skin Substitutes
- NIKS:
-
Near-Diploid Neonatal Human Keratinocyte Cell Line
- BM:
-
Bone Marrow
- HUK:
-
Human Undifferentiated Keratinocyte
- GAG:
-
Glycosaminoglycan
- hAEC:
-
Human Amniotic Epithelial Cell
- SVF:
-
Stromal Vascular Fraction
- MHC:
-
Major Histocompatibility Complex
References
Yakupu A, Zhang J, Dong W, Song F, Dong J, Lu S. The epidemiological characteristic and trends of burns globally. BMC Public Health. 2022;22(1):1596.
Browning JA, Cindass R. Burn Debridement, Grafting, and Reconstruction. In: StatPearls. edn. Treasure Island (FL): StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.; 2022.
Gardien KL, Marck RE, Bloemen MC, Waaijman T, Gibbs S, Ulrich MM, Middelkoop E. Outcome of Burns treated with autologous cultured proliferating epidermal cells: a prospective Randomized Multicenter Intrapatient comparative trial. Cell Transplant. 2016;25(3):437–48.
Stone Ii R, Natesan S, Kowalczewski CJ, Mangum LH, Clay NE, Clohessy RM, Carlsson AH, Tassin DH, Chan RK, Rizzo JA, et al. Advancements in regenerative strategies through the continuum of burn Care. Front Pharmacol. 2018;9:672.
Asuku M, Yu TC, Yan Q, Böing E, Hahn H, Hovland S, Donelan MB. Split-thickness skin graft donor-site morbidity: a systematic literature review. Burns: J Int Soc Burn Injuries. 2021;47(7):1525–46.
Abdul Kareem N, Aijaz A, Jeschke MG. Stem cell therapy for Burns: Story so far. Biologics: Targets Therapy. 2021;15:379–97.
McCann C, Watson A, Barnes D. Major burns: part 1. Epidemiology, pathophysiology and initial management. BJA Educ. 2022;22(3):94–103.
Markiewicz-Gospodarek A, Kozioł M, Tobiasz M, Baj J, Radzikowska-Büchner E, Przekora A. Burn Wound Healing: clinical complications, Medical Care, Treatment, and dressing types: the current state of knowledge for clinical practice. Int J Environ Res Public Health 2022, 19(3).
Mirhaj M, Labbaf S, Tavakoli M, Seifalian AM. Emerging treatment strategies in wound care. Int Wound J. 2022;19(7):1934–54.
Jo H, Brito S, Kwak BM, Park S, Lee MG, Bin BH. Applications of mesenchymal stem cells in skin regeneration and rejuvenation. Int J Mol Sci 2021, 22(5).
Shpichka A, Butnaru D, Bezrukov EA, Sukhanov RB, Atala A, Burdukovskii V, Zhang Y, Timashev P. Skin tissue regeneration for burn injury. Stem Cell Res Ther. 2019;10(1):94.
Hamrahi VF, Goverman J, Jung W, Wu JC, Fischman AJ, Tompkins RG, Yu YY, Fagan SP, Carter EA. In vivo molecular imaging of murine embryonic stem cells delivered to a burn wound surface via Integra® scaffolding. J burn care Research: Official Publication Am Burn Association. 2012;33(2):e49–54.
Liu P, Deng Z, Han S, Liu T, Wen N, Lu W, Geng X, Huang S, Jin Y. Tissue-engineered skin containing mesenchymal stem cells improves burn wounds. Artif Organs. 2008;32(12):925–31.
Francis E, Kearney L, Clover J. The effects of stem cells on burn wounds: a review. Int J Burns Trauma. 2019;9(1):1–12.
Sordi V, Malosio ML, Marchesi F, Mercalli A, Melzi R, Giordano T, Belmonte N, Ferrari G, Leone BE, Bertuzzi F, et al. Bone marrow mesenchymal stem cells express a restricted set of functionally active chemokine receptors capable of promoting migration to pancreatic islets. Blood. 2005;106(2):419–27.
Liu L, Yu Y, Hou Y, Chai J, Duan H, Chu W, Zhang H, Hu Q, Du J. Human umbilical cord mesenchymal stem cells transplantation promotes cutaneous Wound Healing of severe burned rats. PLoS ONE. 2014;9(2):e88348.
Liu S, Zhou J, Zhang X, Liu Y, Chen J, Hu B, Song J, Zhang Y. Strategies to optimize adult stem cell therapy for tissue regeneration. Int J Mol Sci 2016, 17(6).
Holmes JHt, Molnar JA, Shupp JW, Hickerson WL, King BT, Foster KN, Cairns BA, Carter JE. Demonstration of the safety and effectiveness of the RECELL(®) System combined with split-thickness meshed autografts for the reduction of donor skin to treat mixed-depth burn injuries. Burns: J Int Soc Burn Injuries. 2019;45(4):772–82.
Gibson ALF, Holmes JHt, Shupp JW, Smith D, Joe V, Carson J, Litt J, Kahn S, Short T, Cancio L, et al. A phase 3, open-label, controlled, randomized, multicenter trial evaluating the efficacy and safety of StrataGraft® construct in patients with deep partial-thickness thermal burns. Burns: J Int Soc Burn Injuries. 2021;47(5):1024–37.
Lee DE, Ayoub N, Agrawal DK. Mesenchymal stem cells and cutaneous wound healing: novel methods to increase cell delivery and therapeutic efficacy. Stem Cell Res Ther. 2016;7(1):37.
Nourian Dehkordi A, Mirahmadi Babaheydari F, Chehelgerdi M, Raeisi Dehkordi S. Skin tissue engineering: wound healing based on stem-cell-based therapeutic strategies. Stem Cell Res Ther. 2019;10(1):111.
Ayavoo T, Murugesan K, Gnanasekaran A. Roles and mechanisms of stem cell in wound healing. Stem cell Invest. 2021;8:4.
Tamama K, Kerpedjieva SS. Acceleration of Wound Healing by multiple growth factors and cytokines secreted from multipotential stromal Cells/Mesenchymal stem cells. Adv Wound care. 2012;1(4):177–82.
Rivas-Torres MT, Amato D, Arámbula-Alvarez H, Kuri-Harcuch W. Controlled clinical study of skin donor sites and deep partial-thickness burns treated with cultured epidermal allografts. Plast Reconstr Surg. 1996;98(2):279–87.
Noordenbos J, Doré C, Hansbrough JF. Safety and efficacy of TransCyte for the treatment of partial-thickness burns. J Burn Care Rehabil. 1999;20(4):275–81.
Demling RH, DeSanti L. Management of partial thickness facial burns (comparison of topical antibiotics and bio-engineered skin substitutes). Burns: J Int Soc Burn Injuries. 1999;25(3):256–61.
Kumar RJ, Kimble RM, Boots R, Pegg SP. Treatment of partial-thickness burns: a prospective, randomized trial using Transcyte. ANZ J Surg. 2004;74(8):622–6.
Gravante G, Di Fede MC, Araco A, Grimaldi M, De Angelis B, Arpino A, Cervelli V, Montone A. A randomized trial comparing ReCell system of epidermal cells delivery versus classic skin grafts for the treatment of deep partial thickness burns. Burns: J Int Soc Burn Injuries. 2007;33(8):966–72.
Yim H, Yang HT, Cho YS, Kim D, Kim JH, Chun W, Hur J. A clinical trial designed to evaluate the safety and effectiveness of a thermosensitive hydrogel-type cultured epidermal allograft for deep second-degree burns. Burns: J Int Soc Burn Injuries. 2014;40(8):1642–9.
Sood R, Roggy DE, Zieger MJ, Nazim M, Hartman BC, Gibbs JT. A comparative study of spray keratinocytes and autologous meshed split-thickness skin graft in the treatment of acute burn injuries. Wounds: Compendium Clin Res Pract. 2015;27(2):31–40.
Yoon J, Yang HT, Yim H, Cho YS, Kym D, Hur J, Chun W, Lee JW, Yoon C. Effectiveness and safety of a thermosensitive hydrogel cultured epidermal allograft for Burns. Adv Skin Wound Care. 2017;30(12):559–64.
Holmes Iv JH, Molnar JA, Carter JE, Hwang J, Cairns BA, King BT, Smith DJ, Cruse CW, Foster KN, Peck MD, et al. A comparative study of the ReCell® device and autologous spit-thickness meshed skin graft in the treatment of Acute burn injuries. J burn care Res. 2018;39(5):694–702.
Holmes JHt, Schurr MJ, King BT, Foster K, Faucher LD, Lokuta MA, Comer AR, Rooney PJ, Barbeau KF, Mohoney ST, et al. An open-label, prospective, randomized, controlled, multicenter, phase 1b study of StrataGraft skin tissue versus autografting in patients with deep partial-thickness thermal burns. Burns: J Int Soc Burn Injuries. 2019;45(8):1749–58.
Schulman CI, Namias N, Pizano L, Rodriguez-Menocal L, Aickara D, Guzman W, Candanedo A, Maranda E, Beirn A, McBride JD, et al. The effect of mesenchymal stem cells improves the healing of burn wounds: a phase 1 dose-escalation clinical trial. Scars Burns Healing. 2022;8:20595131211070783.
Sakamoto M, Minaki Y, Nakano T, Tsuge I, Yamanaka H, Sowa Y, Shimizu Y, Inoie M, Saito S, Morimoto N. A novel approach for wound treatment using dried cultured epidermal allograft: a phase I/II, single-center, open-label clinical trial. Burns: J Int Soc Burn Injuries 2022.
Wood F, Martin L, Lewis D, Rawlins J, McWilliams T, Burrows S, Rea S. A prospective randomised clinical pilot study to compare the effectiveness of Biobrane® synthetic wound dressing, with or without autologous cell suspension, to the local standard treatment regimen in paediatric scald injuries. Burns: J Int Soc Burn Injuries. 2012;38(6):830–9.
Munster AM. Cultured skin for massive burns. A prospective, controlled trial. Ann Surg. 1996;224(3):372–5. discussion 375–377.
Purdue GF, Hunt JL, Still JM Jr., Law EJ, Herndon DN, Goldfarb IW, Schiller WR, Hansbrough JF, Hickerson WL, Himel HN, et al. A multicenter clinical trial of a biosynthetic skin replacement, Dermagraft-TC, compared with cryopreserved human cadaver skin for temporary coverage of excised burn wounds. J Burn Care Rehabil. 1997;18(1 Pt 1):52–7.
Boyce ST, Kagan RJ, Yakuboff KP, Meyer NA, Rieman MT, Greenhalgh DG, Warden GD. Cultured skin substitutes reduce donor skin harvesting for closure of excised, full-thickness burns. Ann Surg. 2002;235(2):269–79.
Boyce ST, Kagan RJ, Greenhalgh DG, Warner P, Yakuboff KP, Palmieri T, Warden GD. Cultured skin substitutes reduce requirements for harvesting of skin autograft for closure of excised, full-thickness burns. J Trauma. 2006;60(4):821–9.
Ermolov AS, Smirnov SV, Khvatov VB, Istranov LP, Koniushko OI, Kolokolchikova EG, Sychevsky MV, Bocharova VS. The use of bioactive wound dressing, stimulating epithelial regeneration of IIIa-degree burn wounds. Bull Exp Biol Med. 2008;146(1):153–7.
Yim H, Yang HT, Cho YS, Seo CH, Lee BC, Ko JH, Kwak IS, Kim D, Hur J, Kim JH, et al. Clinical study of cultured epithelial autografts in liquid suspension in severe burn patients. Burns: J Int Soc Burn Injuries. 2011;37(6):1067–71.
Schurr MJ, Foster KN, Lokuta MA, Rasmussen CA, Thomas-Virnig CL, Faucher LD, Caruso DM, Allen-Hoffmann BL. Clinical evaluation of NIKS-Based bioengineered skin substitute tissue in Complex skin defects: phase I/IIa clinical trial results. Adv Wound care. 2012;1(2):95–103.
Moravvej H, Hormozi AK, Hosseini SN, Sorouri R, Mozafari N, Ghazisaidi MR, Rad MM, Moghimi MH, Sadeghi SM, Mirzadeh H. Comparison of the application of allogeneic fibroblast and autologous mesh grafting with the Conventional Method in the treatment of third-degree Burns. J burn care Research: Official Publication Am Burn Association. 2016;37(1):e90–95.
Boyce ST, Simpson PS, Rieman MT, Warner PM, Yakuboff KP, Bailey JK, Nelson JK, Fowler LA, Kagan RJ. Randomized, paired-site comparison of Autologous Engineered skin substitutes and Split-Thickness skin graft for Closure of extensive, Full-Thickness Burns. J burn care Research: Official Publication Am Burn Association. 2017;38(2):61–70.
Nilforoushzadeh MA, Kazemikhoo N, Mokmeli S, Zare S, Dahmardehei M, Vaghar Doost R, Momeni M, Ansari F. An open-label study of low-level laser therapy followed by autologous fibroblast transplantation for Healing Grade 3 burn wounds in Diabetic patients. J Lasers Med Sci. 2019;10(Suppl 1):S7–12.
Hansbrough JF, Boyce ST, Cooper ML, Foreman TJ. Burn wound closure with cultured autologous keratinocytes and fibroblasts attached to a collagen-glycosaminoglycan substrate. JAMA. 1989;262(15):2125–30.
Hansbrough JF, Doré C, Hansbrough WB. Clinical trials of a living dermal tissue replacement placed beneath meshed, split-thickness skin grafts on excised burn wounds. J Burn Care Rehabil. 1992;13(5):519–29.
Hansbrough JF, Mozingo DW, Kealey GP, Davis M, Gidner A, Gentzkow GD. Clinical trials of a biosynthetic temporary skin replacement, Dermagraft-Transitional Covering, compared with cryopreserved human cadaver skin for temporary coverage of excised burn wounds. J Burn Care Rehabil. 1997;18(1 Pt 1):43–51.
Waymack P, Duff RG, Sabolinski M. The effect of a tissue engineered bilayered living skin analog, over meshed split-thickness autografts on the healing of excised burn wounds. The apligraf burn Study Group. Burns: J Int Soc Burn Injuries. 2000;26(7):609–19.
Rodrigues M, Kosaric N, Bonham CA, Gurtner GC. Wound Healing: a Cellular Perspective. Physiol Rev. 2019;99(1):665–706.
Rousselle P, Braye F, Dayan G. Re-epithelialization of adult skin wounds: Cellular mechanisms and therapeutic strategies. Adv Drug Deliv Rev. 2019;146:344–65.
Lootens L, Brusselaers N, Beele H, Monstrey S. Keratinocytes in the treatment of severe burn injury: an update. Int Wound J. 2013;10(1):6–12.
Singer AJ, Boyce ST. Burn Wound Healing and tissue Engineering. J burn care Research: Official Publication Am Burn Association. 2017;38(3):e605–13.
Wood FM, Giles N, Stevenson A, Rea S, Fear M. Characterisation of the cell suspension harvested from the dermal epidermal junction using a ReCell® kit. Burns: J Int Soc Burn Injuries. 2012;38(1):44–51.
Henry S, Mapula S, Grevious M, Foster KN, Phelan H, Shupp J, Chan R, Harrington D, Mashruwala N, Brown DA, et al. Maximizing wound coverage in full-thickness skin defects: a randomized-controlled trial of autologous skin cell suspension and widely meshed autograft versus standard autografting. J Trauma Acute care Surg. 2024;96(1):85–93.
Jackson CJ, Tønseth KA, Utheim TP. Cultured epidermal stem cells in regenerative medicine. Stem Cell Res Ther. 2017;8(1):155.
Li Z, Maitz P. Cell therapy for severe burn wound healing. Burns Trauma. 2018;6:13.
Hosseini M, Dalley AJ, Shafiee A. Convergence of Biofabrication Technologies and Cell therapies for Wound Healing. Pharmaceutics 2022, 14(12).
Tottoli EM, Dorati R, Genta I, Chiesa E, Pisani S, Conti B. Skin wound healing process and New Emerging technologies for skin Wound Care and Regeneration. Pharmaceutics 2020, 12(8).
Rheinwald JG, Green H. Serial cultivation of strains of human epidermal keratinocytes: the formation of keratinizing colonies from single cells. Cell. 1975;6(3):331–43.
Amiri N, Golin AP, Jalili RB, Ghahary A. Roles of cutaneous cell-cell communication in wound healing outcome: an emphasis on keratinocyte-fibroblast crosstalk. Exp Dermatol. 2022;31(4):475–84.
Wang Z, Liu X, Zhang D, Wang X, Zhao F, Shi P, Pang X. Co–culture with human fetal epidermal keratinocytes promotes proliferation and migration of human fetal and adult dermal fibroblasts. Mol Med Rep. 2015;11(2):1105–10.
Spiekstra SW, Breetveld M, Rustemeyer T, Scheper RJ, Gibbs S. Wound-healing factors secreted by epidermal keratinocytes and dermal fibroblasts in skin substitutes. Wound Repair Regeneration: Official Publication Wound Healing Soc [and] Eur Tissue Repair Soc. 2007;15(5):708–17.
Svensjö T, Yao F, Pomahac B, Eriksson E. Autologous keratinocyte suspensions accelerate epidermal wound healing in pigs. J Surg Res. 2001;99(2):211–21.
Boyce ST, Kagan RJ. Composition and performance of Autologous Engineered skin substitutes for repair or regeneration of excised, Full-Thickness Burns. J burn care Research: Official Publication Am Burn Association. 2023;44(Suppl1):S50–6.
Halim AS, Khoo TL, Mohd Yussof SJ. Biologic and synthetic skin substitutes: an overview. Indian J Plast Surgery: Official Publication Association Plast Surg India. 2010;43(Suppl):S23–28.
Domaszewska-Szostek AP, Krzyżanowska MO, Czarnecka AM, Siemionow M. Local Treatment of Burns with cell-based therapies tested in Clinical studies. J Clin Med 2021, 10(3).
Goyer B, Larouche D, Kim DH, Veillette N, Pruneau V, Bernier V, Auger FA, Germain L. Immune tolerance of tissue-engineered skin produced with allogeneic or xenogeneic fibroblasts and syngeneic keratinocytes grafted on mice. Acta Biomater. 2019;90:192–204.
Mitrousis N, Fokina A, Shoichet MS. Biomaterials for cell transplantation. Nat Reviews Mater. 2018;3(11):441–56.
O’Connor NEMJ, Banks-Schlegel S, Kehinde O, Green H. Grafting of burns with cultured epithelium prepared from autologous epidermal cells. Lancet (London England). 1981;1(8211):75–8.
Ronfard V, Rives JM, Neveux Y, Carsin H, Barrandon Y. Long-term regeneration of human epidermis on third degree burns transplanted with autologous cultured epithelium grown on a fibrin matrix. Transplantation. 2000;70(11):1588–98.
Zaulyanov L, Kirsner RS. A review of a bi-layered living cell treatment (apligraf) in the treatment of venous leg ulcers and diabetic foot ulcers. Clin Interv Aging. 2007;2(1):93–8.
Smith DJ Jr. Use of Biobrane in wound management. J Burn Care Rehabil. 1995;16(3 Pt 1):317–20.
Schurr MJ, Foster KN, Centanni JM, Comer AR, Wicks A, Gibson AL, Thomas-Virnig CL, Schlosser SJ, Faucher LD, Lokuta MA, et al. Phase I/II clinical evaluation of StrataGraft: a consistent, pathogen-free human skin substitute. J Trauma. 2009;66(3):866–73. discussion 873 – 864.
Haslik W, Kamolz LP, Nathschläger G, Andel H, Meissl G, Frey M. First experiences with the collagen-elastin matrix Matriderm as a dermal substitute in severe burn injuries of the hand. Burns: J Int Soc Burn Injuries. 2007;33(3):364–8.
Boyce ST, Christianson DJ, Hansbrough JF. Structure of a collagen-GAG dermal skin substitute optimized for cultured human epidermal keratinocytes. J Biomed Mater Res. 1988;22(10):939–57.
Spotnitz WD. Fibrin sealant: the only approved Hemostat, Sealant, and Adhesive-a laboratory and clinical perspective. ISRN Surg. 2014;2014:203943.
Raman R, Sasisekharan V, Sasisekharan R. Structural insights into biological roles of protein-glycosaminoglycan interactions. Chem Biol. 2005;12(3):267–77.
Lin X. Functions of heparan sulfate proteoglycans in cell signaling during development. Development. 2004;131(24):6009–21.
Corsuto L, Rother S, Koehler L, Bedini E, Moeller S, Schnabelrauch M, Hintze V, Schiraldi C, Scharnweber D. Sulfation degree not origin of chondroitin sulfate derivatives modulates keratinocyte response. Carbohydr Polym. 2018;191:53–64.
Orgill DP, Butler C, Regan JF, Barlow MS, Yannas IV, Compton CC. Vascularized collagen-glycosaminoglycan matrix provides a dermal substrate and improves take of cultured epithelial autografts. Plast Reconstr Surg. 1998;102(2):423–9.
Wessels Q, Pretorius E. Development and ultra-structure of an ultra-thin silicone epidermis of bioengineered alternative tissue. Int Wound J. 2015;12(4):428–31.
Panayi AC, Haug V, Liu Q, Wu M, Karvar M, Aoki S, Ma C, Hamaguchi R, Endo Y, Orgill DP. Novel application of autologous micrografts in a collagen-glycosaminoglycan scaffold for diabetic wound healing. Biomedical Mater (Bristol England) 2021, 16(3).
Carlson MA, Longaker MT. The fibroblast-populated collagen matrix as a model of wound healing: a review of the evidence. Wound Repair Regeneration: Official Publication Wound Healing Soc [and] Eur Tissue Repair Soc. 2004;12(2):134–47.
Supp AP, Wickett RR, Swope VB, Harriger MD, Hoath SB, Boyce ST. Incubation of cultured skin substitutes in reduced humidity promotes cornification in vitro and stable engraftment in athymic mice. Wound Repair Regeneration: Official Publication Wound Healing Soc [and] Eur Tissue Repair Soc. 1999;7(4):226–37.
Nicholas MN, Jeschke MG, Amini-Nik S. Methodologies in creating skin substitutes. Cell Mol Life Sci. 2016;73(18):3453–72.
Han CM, Zhang LP, Sun JZ, Shi HF, Zhou J, Gao CY. Application of collagen-chitosan/fibrin glue asymmetric scaffolds in skin tissue engineering. J Zhejiang Univ Sci B. 2010;11(7):524–30.
Haugh MG, Jaasma MJ, O’Brien FJ. The effect of dehydrothermal treatment on the mechanical and structural properties of collagen-GAG scaffolds. J Biomedical Mater Res Part A. 2009;89(2):363–9.
Rnjak-Kovacina J, Wise SG, Li Z, Maitz PK, Young CJ, Wang Y, Weiss AS. Electrospun synthetic human elastin:collagen composite scaffolds for dermal tissue engineering. Acta Biomater. 2012;8(10):3714–22.
Chevallay B, Herbage D. Collagen-based biomaterials as 3D scaffold for cell cultures: applications for tissue engineering and gene therapy. Med Biol Eng Comput. 2000;38(2):211–8.
Lynn AK, Yannas IV, Bonfield W. Antigenicity and immunogenicity of collagen. J Biomedical Mater Res Part B Appl Biomaterials. 2004;71(2):343–54.
Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. Burn injury. Nat Reviews Disease Primers. 2020;6(1):11.
Kagan RJ, Matsuda T, Hanumadass M, Jonasson O. Serious wound infections in burned patients. Surgery. 1985;98(4):640–7.
Clause KC, Barker TH. Extracellular matrix signaling in morphogenesis and repair. Curr Opin Biotechnol. 2013;24(5):830–3.
Potekaev NN, Borzykh OB, Medvedev GV, Pushkin DV, Petrova MM, Petrov AV, Dmitrenko DV, Karpova EI, Demina OM, Shnayder NA. The role of Extracellular Matrix in skin Wound Healing. J Clin Med 2021, 10(24).
Smink AM, de Vos P. Therapeutic strategies for modulating the Extracellular Matrix to improve pancreatic islet function and survival after transplantation. Curr Diab Rep. 2018;18(7):39.
Wong T, McGrath JA, Navsaria H. The role of fibroblasts in tissue engineering and regeneration. Br J Dermatol. 2007;156(6):1149–55.
Papini R. Management of burn injuries of various depths. BMJ (Clinical Res ed). 2004;329(7458):158–60.
Csenkey A, Hargitai E, Pakai E, Kajtar B, Vida L, Lorincz A, Gergics M, Vajda P, Jozsa G, Garami A. Effectiveness of four topical treatment methods in a rat model of superficial partial-thickness burn injury: the advantages of combining zinc-hyaluronan gel with silver foam dressing. Injury. 2022;53(12):3912–9.
Wood FM, Kolybaba ML, Allen P. The use of cultured epithelial autograft in the treatment of major burn injuries: a critical review of the literature. Burns: J Int Soc Burn Injuries. 2006;32(4):395–401.
Rasulov MF, Vasilchenkov AV, Onishchenko NA, Krasheninnikov ME, Kravchenko VI, Gorshenin TL, Pidtsan RE, Potapov IV. First experience of the use bone marrow mesenchymal stem cells for the treatment of a patient with deep skin burns. Bull Exp Biol Med. 2005;139(1):141–4.
Wittig O, Diaz-Solano D, Chacín T, Rodriguez Y, Ramos G, Acurero G, Leal F, Cardier JE. Healing of deep dermal burns by allogeneic mesenchymal stromal cell transplantation. Int J Dermatol. 2020;59(8):941–50.
Mansilla E, Marín GH, Berges M, Scafatti S, Rivas J, Núñez A, Menvielle M, Lamonega R, Gardiner C, Drago H, et al. Cadaveric bone marrow mesenchymal stem cells: first experience treating a patient with large severe burns. Burns Trauma. 2015;3:17.
Abo-Elkheir W, Hamza F, Elmofty AM, Emam A, Abdl-Moktader M, Elsherefy S, Gabr H. Role of cord blood and bone marrow mesenchymal stem cells in recent deep burn: a case-control prospective study. Am J stem Cells. 2017;6(3):23–35.
Bey E, Prat M, Duhamel P, Benderitter M, Brachet M, Trompier F, Battaglini P, Ernou I, Boutin L, Gourven M, et al. Emerging therapy for improving wound repair of severe radiation burns using local bone marrow-derived stem cell administrations. Wound Repair Regeneration: Official Publication Wound Healing Soc [and] Eur Tissue Repair Soc. 2010;18(1):50–8.
Xu Y, Huang S, Fu X. Autologous transplantation of bone marrow-derived mesenchymal stem cells: a promising therapeutic strategy for prevention of skin-graft contraction. Clin Exp Dermatol. 2012;37(5):497–500.
Lataillade JJ, Doucet C, Bey E, Carsin H, Huet C, Clairand I, Bottollier-Depois JF, Chapel A, Ernou I, Gourven M, et al. New approach to radiation burn treatment by dosimetry-guided surgery combined with autologous mesenchymal stem cell therapy. Regen Med. 2007;2(5):785–94.
Jeschke MG, Rehou S, McCann MR, Shahrokhi S. Allogeneic mesenchymal stem cells for treatment of severe burn injury. Stem Cell Res Ther. 2019;10(1):337.
Kitala D, Łabuś W, Klama-Baryła A, Kraut M, Maj M, Szapski M. Application of amniotic stem cells on an acellular dermal Matrix Scaffold in a burned patient: a Case Report. Transpl Proc. 2020;52(8):2563–9.
Yastı AÇ, Akgün AE, Akın M. Use of stromal vascular fraction stem cell therapy for functional and cosmetic outcomes in a young female patient with deep dermal flame burns on the face. Burns Open. 2022;6(3):116–9.
Arkoulis N, Watson S, Weiler-Mithoff E. Stem cell enriched dermal substitutes for the treatment of late burn contractures in patients with major burns. Burns: J Int Soc Burn Injuries. 2018;44(3):724–6.
Portas M, Mansilla E, Drago H, Dubner D, Radl A, Coppola A, Di Giorgio M. Use of human cadaveric mesenchymal stem cells for cell therapy of a Chronic Radiation-Induced skin lesion: a Case Report. Radiat Prot Dosimetry. 2016;171(1):99–106.
Bhattacharya N. Use of amniotic membrane, amniotic fluid, and placental dressing in advanced burn patients. Transplantation. 2010;90:182.
Hatzfeld AS, Pasquesoone L, Germain N, Danzé PM, Drucbert AS, Tardivel M, Bongiovanni A, Duquennoy-Martinot V, Guerreschi P, Marchetti P. Benefits of cryopreserved human amniotic membranes in association with conventional treatments in the management of full-thickness burns. Int Wound J. 2019;16(6):1354–64.
Pappa KI, Anagnou NP. Novel sources of fetal stem cells: where do they fit on the developmental continuum? Regen Med. 2009;4(3):423–33.
Simoni G, Colognato R. The amniotic fluid-derived cells: the biomedical challenge for the third millennium. J Prenatal Med. 2009;3(3):34–6.
Roubelakis MG, Pappa KI, Bitsika V, Zagoura D, Vlahou A, Papadaki HA, Antsaklis A, Anagnou NP. Molecular and proteomic characterization of human mesenchymal stem cells derived from amniotic fluid: comparison to bone marrow mesenchymal stem cells. Stem Cells Dev. 2007;16(6):931–52.
Stachelscheid H, Wulf-Goldenberg A, Eckert K, Jensen J, Edsbagge J, Björquist P, Rivero M, Strehl R, Jozefczuk J, Prigione A, et al. Teratoma formation of human embryonic stem cells in three-dimensional perfusion culture bioreactors. J Tissue Eng Regen Med. 2013;7(9):729–41.
Prokhorova TA, Harkness LM, Frandsen U, Ditzel N, Schrøder HD, Burns JS, Kassem M. Teratoma formation by human embryonic stem cells is site dependent and enhanced by the presence of Matrigel. Stem Cells Dev. 2009;18(1):47–54.
Swijnenburg RJ, Tanaka M, Vogel H, Baker J, Kofidis T, Gunawan F, Lebl DR, Caffarelli AD, de Bruin JL, Fedoseyeva EV, et al. Embryonic stem cell immunogenicity increases upon differentiation after transplantation into ischemic myocardium. Circulation. 2005;112(9 Suppl):I166–172.
Grompe M. Adult versus embryonic stem cells: it’s still a tie. Mol Therapy: J Am Soc Gene Therapy. 2002;6(3):303–5.
Bacakova L, Zarubova J, Travnickova M, Musilkova J, Pajorova J, Slepicka P, Kasalkova NS, Svorcik V, Kolska Z, Motarjemi H, et al. Stem cells: their source, potency and use in regenerative therapies with focus on adipose-derived stem cells - a review. Biotechnol Adv. 2018;36(4):1111–26.
Klyushnenkova E, Mosca JD, Zernetkina V, Majumdar MK, Beggs KJ, Simonetti DW, Deans RJ, McIntosh KR. T cell responses to allogeneic human mesenchymal stem cells: immunogenicity, tolerance, and suppression. J Biomed Sci. 2005;12(1):47–57.
Aggarwal S, Pittenger MF. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood. 2005;105(4):1815–22.
Műzes G, Sipos F. Mesenchymal stem cell-derived secretome: a potential therapeutic option for Autoimmune and Immune-mediated inflammatory diseases. Cells 2022, 11(15).
Hass R, Kasper C, Böhm S, Jacobs R. Different populations and sources of human mesenchymal stem cells (MSC): a comparison of adult and neonatal tissue-derived MSC. Cell Communication Signaling: CCS. 2011;9:12.
Li CY, Wu XY, Tong JB, Yang XX, Zhao JL, Zheng QF, Zhao GB, Ma ZJ. Comparative analysis of human mesenchymal stem cells from bone marrow and adipose tissue under xeno-free conditions for cell therapy. Stem Cell Res Ther. 2015;6(1):55.
Lee M, Jeong SY, Ha J, Kim M, Jin HJ, Kwon SJ, Chang JW, Choi SJ, Oh W, Yang YS, et al. Low immunogenicity of allogeneic human umbilical cord blood-derived mesenchymal stem cells in vitro and in vivo. Biochem Biophys Res Commun. 2014;446(4):983–9.
Deuse T, Stubbendorff M, Tang-Quan K, Phillips N, Kay MA, Eiermann T, Phan TT, Volk HD, Reichenspurner H, Robbins RC, et al. Immunogenicity and immunomodulatory properties of umbilical cord lining mesenchymal stem cells. Cell Transplant. 2011;20(5):655–67.
Barlow S, Brooke G, Chatterjee K, Price G, Pelekanos R, Rossetti T, Doody M, Venter D, Pain S, Gilshenan K, et al. Comparison of human placenta- and bone marrow-derived multipotent mesenchymal stem cells. Stem Cells Dev. 2008;17(6):1095–107.
Magatti M, Pianta S, Silini A, Parolini O. Isolation, culture, and phenotypic characterization of mesenchymal stromal cells from the amniotic membrane of the Human Term Placenta. Methods Mol Biology (Clifton NJ). 2016;1416:233–44.
Abbasi-Kangevari M, Ghamari SH, Safaeinejad F, Bahrami S, Niknejad H. Potential therapeutic features of human amniotic mesenchymal stem cells in multiple sclerosis: Immunomodulation, inflammation suppression, Angiogenesis Promotion, oxidative stress inhibition, neurogenesis induction, MMPs regulation, and Remyelination Stimulation. Front Immunol. 2019;10:238.
Gramignoli R, Srinivasan RC, Kannisto K, Strom SC. Isolation of Human Amnion Epithelial Cells According to Current Good Manufacturing Procedures. Curr Protoc Stem Cell Biol. 2016;37:1e10.11-1e10.13.
Zhang Y, Zhong Y, Zou L, Liu X. Significance of placental mesenchymal stem cell in Placenta Development and implications for Preeclampsia. Front Pharmacol. 2022;13:896531.
ElHeneidy H, Omran E, Halwagy A, Al-Inany H, Al-Ansary M, Gad A. Amniotic membrane can be a valid source for wound healing. Int J Women’s Health. 2016;8:225–31.
Fénelon M, Catros S, Meyer C, Fricain JC, Obert L, Auber F, Louvrier A, Gindraux F. Applications of human amniotic membrane for tissue Engineering. Membranes 2021, 11(6).
Biniazan F, Manzari-Tavakoli A, Safaeinejad F, Moghimi A, Rajaei F, Niknejad H. The differentiation effect of bone morphogenetic protein (BMP) on human amniotic epithelial stem cells to express ectodermal lineage markers. Cell Tissue Res. 2021;383(2):751–63.
Motamedi S, Esfandpour A, Babajani A, Jamshidi E, Bahrami S, Niknejad H. The current challenges on Spray-based cell delivery to the skin wounds. Tissue Eng Part C Methods. 2021;27(10):543–58.
Deng X, Gould M, Ali MA. A review of current advancements for wound healing: Biomaterial applications and medical devices. J Biomedical Mater Res Part B Appl Biomaterials. 2022;110(11):2542–73.
Salahshour P, Abdolmaleki S, Monemizadeh S, Gholizadeh S, Khaksar S. Nanobiomaterials/Bioinks Based Scaffolds in 3D Bioprinting for Tissue Engineering and Artificial Human Organs. Adv Biology Earth Sci 2024, 9.
kazemi S, Hosseingholian A, Gohari SD, Feirahi F, Moammeri F, Mesbahian G, Moghaddam ZS, Ren Q. Recent advances in green synthesized nanoparticles: from production to application. Mater Today Sustain. 2023;24:100500.
Karadağ M, Omarova S. USE OF Prunus armeniaca L. Seed Oil and Pulp in Health and Cosmetic Products. Adv Biology Earth Sci 2024, 9.
Karadag M, Baran A, Güneş Z. Production of Value-Added Cosmetic Products from Cold-Pressed Helianthus annuus L. OIL AND PULP. Adv Biology Earth Sci 2024, 9.
Karadag M, Doğan S, Mask for Moisturizing Skin and Body Made from Cold-Pressed. Paste of Peanuts (Arachis hypogaea L). Adv Biology Earth Sci 2024, 9(1).
Hade MD, Suire CN, Suo Z. Mesenchymal stem cell-derived exosomes: applications in Regenerative Medicine. Cells 2021, 10(8).
Chesney J, Lewis KD, Kluger H, Hamid O, Whitman E, Thomas S, Wermke M, Cusnir M, Domingo-Musibay E, Phan GQ et al. Efficacy and safety of lifileucel, a one-time autologous tumor-infiltrating lymphocyte (TIL) cell therapy, in patients with advanced melanoma after progression on immune checkpoint inhibitors and targeted therapies: pooled analysis of consecutive cohorts of the C-144-01 study. J Immunother Cancer 2022, 10(12).
Orouji Z, Bajouri A, Ghasemi M, Mohammadi P, Fallah N, Shahbazi A, Rezvani M, Vaezirad F, Khalajasadi Z, Alizadeh A, et al. A single-arm open-label clinical trial of autologous epidermal cell transplantation for stable vitiligo: a 30-month follow-up. J Dermatol Sci. 2018;89(1):52–9.
Khandpur S, Gupta S, Gunaabalaji DR. Stem cell therapy in dermatology. Indian J Dermatol Venereol Leprol. 2021;87(6):753–67.
Wardhana A. Biological Skin Graft With Keratinocyte-stem Cell Co-cultre for Burn Patients. ClinicalTrialsgov identifier:NCT05652816, 2022(https://clinicaltrials.gov/study/NCT05652816 (accessed 2022-12-15)).
Fernández-Alvés MC. Application of Mesenchymal Stem Cells and full of plasma in the management of the burn wound in patients with large burn injury. Clinical trials for eudract_number:2012-001596-36 (EUCTR2012-001596-36-ES) 2012 (https://www.clinicaltrialsregister.eu/ctr-search/search?query=eudract_number:2012-001596-36 (accessed 2012-11-20)).
Asadi K. Adipose Cell Derived Stem Cell application in deep burn healing. IRCT identifier: IRCT201202169044N1 2012 (https://trialsearch.who.int/Trial2.aspx?TrialID=IRCT201202169044N1).
Fatemi MJ. Effect of amniotic membrane loaded with adipose-derived stem cells on skin graft. IRCT identifier: IRCT201209178177N5 2013 (https://trialsearch.who.int/Trial2.aspx?TrialID=IRCT201209178177N5).
Anterogen Co. LRP: a clinical trial to evaluate the Safety and Efficacy of ALLO-ASC-DFU for Second Deep Degree burn Injury subjects. ClinicalTrialsgov Identifier NCT02619851 2015 (https://clinicaltrials.gov/show/NCT02619851).
2102 R. Fat-derived stem cells in the treatment of acute burns. Clinical trials for eudract_number:2018-002870-27 (EUCTR 2018-002870-27-DK) 2018 (https://www.clinicaltrialsregister.eu/ctr-search/search?query=eudract_number:2018-002870-27).
Rong X. Combined Treatment of Umbilical Cord Mesenchymal Stem Cells and MEEK Micrografting on Severe Burn Patients. Trial identifier: ChiCTR2000040932 2020 (https://trialsearch.who.int/Trial2.aspx?TrialID=ChiCTR2000040932).
Jeschke MA, Phase I, Single-blind. Randomized Study of the Safety and Efficacy of Cellularized Integra® Using Autologous Burn-derived Stem Cells (Integra®-SC). ClinicalTrialsgov Identifier NCT05344521 2022 (https://clinicaltrials.gov/show/NCT05344521).
Acknowledgements
This work was supported by Vice-Chancellor’s in Research Affairs, Shahid Beheshti University of Medical Sciences, Tehran, Iran (research No: 43009424). The authors would like to thank Amirhossein Nazerian for his assistance with creating figures for the manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YY, YN, FN, and HN contributed to the design and conception of the review. YY and YN screened the databases and extracted the clinical trials for the systematic review. YY and YN contributed to the writing of the manuscript. HN and FN supervised and contributed to the revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yassaghi, Y., Nazerian, Y., Niazi, F. et al. Advancements in cell-based therapies for thermal burn wounds: a comprehensive systematic review of clinical trials outcomes. Stem Cell Res Ther 15, 277 (2024). https://doi.org/10.1186/s13287-024-03901-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-024-03901-2