Abstract
Vascular tissue engineering is a promising approach for regenerating damaged blood vessels and developing new therapeutic approaches for heart disease treatment. To date, different sources of cells have been recognized that offer assistance within the recovery of heart supply routes and veins with distinctive capacities and are compelling for heart regeneration. However, some challenges still remain that need to be overcome to establish the full potential application of these cells. In this paper, we review the different cell sources used for vascular tissue engineering, focusing on extraembryonic tissue-derived cells (ESCs), and elucidate their roles in cardiovascular disease. In addition, we highlight the intricate interplay between mechanical and biochemical factors in regulating mesenchymal stem cell (MSC) differentiation, offering insights into optimizing their application in vascular tissues.
Similar content being viewed by others
Introduction
Despite progressive advances in pharmacological and surgical therapy, cardiovascular diseases remain the leading cause of mortality worldwide [1]. These diseases typically involve the buildup of fatty deposits within arteries and an increased risk of blood clot formation. The increasing demand for organ transplants and the limited supply of donor organs have resulted in organ shortage crises. Conventional synthetic vascular grafts are incompetent at remodeling and have limited patency, particularly at smaller diameters. This is where tissue engineering has emerged as a promising solution. By combining bioactive cells with biodegradable scaffolds, tissue-engineered vascular grafts can be developed, offering the advantages of growth and self-healing capacity. These features have the potential to overcome the limitations of conventional treatment approaches [2].
Presently, the treatment of cardiovascular diseases primarily involves a combination of dietary and lifestyle modifications, medical intervention, and surgical procedures, with surgery typically reserved for advanced cases. Surgical interventions include endovascular techniques such as angioplasty and stent placement to widen or clear narrowed blood vessels. Vascular bypass grafting is another surgical method that is employed to circumvent damaged or blocked vessels. This procedure commonly utilizes autologous arteries or veins. However, due to the limited availability of arteries and severe complications associated with their removal, the saphenous vein is more frequently used as an autograft vessel than the arteries [3]. Nevertheless, the use of autologous vessels also presents certain drawbacks, such as low quality and site morbidity stemming from the extraction process [4].
Tissue engineering represents a rapidly evolving field with the ambitious goal of creating functional tissues and organs through the integration of cells, biomaterials, and biochemical factors. One of the most promising avenues in tissue engineering is stem cell-based therapy. Stem cells possess the remarkable capacity to differentiate into diverse cell types, making them ideal candidates for regenerating damaged or diseased tissues. The use of stem cells in tissue engineering offers several advantages over traditional therapies. First, stem cells can be obtained from various sources, including bone marrow, adipose tissue, or embryonic tissue. This versatility allows for personalized treatment strategies and reduces the risk of immune rejection. Second, stem cells can be cultivated in vitro, enabling the generation of substantial quantities of cells needed for transplantation. This scalability makes it possible to treat a wide range of patients with different tissue defects [5].
Stem cell-based therapy has shown promising results in the treatment of a diverse range of conditions, including heart disease, spinal cord injury, and liver failure. For example, in the realm of cardiac tissue engineering, stem cells can differentiate into cardiomyocytes, specialized heart muscle cells, and subsequently be seeded onto a scaffold to create functional heart muscle patches. These engineered patches have the potential to be transplanted into patients with damaged cardiac tissues, offering a promising avenue for enhancing overall cardiac function and potentially restoring heart health [6].
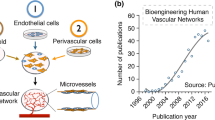
Among the different sources of stem cells, perinatal stem cells have emerged as a promising source for vascular regeneration due to their unique characteristics and potential applications, including lack of need for invasive procedures to obtain them, high degree of plasticity, immunomodulatory properties, low risk of tumorigenesis, younger and healthier cells compared to other adult stem cells, and angiogenic potential [7]. These valuable features make perinatal stem cells ideal candidates for regenerating damaged blood vessels and developing new therapeutic approaches for cardiovascular diseases. One of the key advantages of perinatal stem cells is their easy accessibility. Unlike other sources, such as bone marrow or adipose tissue, perinatal stem cells can be obtained noninvasively and do not pose any risk to the mother or baby during childbirth. Such readiness for availability and ethical advantages have contributed to their increasing popularity in research and clinical settings. Furthermore, perinatal stem cells exhibit high proliferative capacity and immunomodulatory properties [8]. They can be expanded in culture while maintaining their differentiation potential, making them an abundant source for large-scale production of vascular tissues [9]. Perinatal stem cells exhibit a high degree of plasticity, meaning that they can differentiate into various cardiovascular cell types, including endothelial cells, smooth muscle cells, and fibroblasts, which are crucial for vascular tissue engineering. This versatility allows them to contribute to the formation of functional blood vessels and vascular networks. Additionally, these cells possess immunosuppressive capabilities that allow them to evade immune rejection when transplanted into a recipient [7]. However, further research is needed to understand their long-term effects, optimize their differentiation protocols, and enhance their therapeutic efficacy. This paper reviews the different cell sources for vascular tissue engineering, focusing on extraembryonic tissue-derived cells.
Functional requirements for vascular grafts
Blood vessel walls typically consist of three main layers. The innermost layer adjacent to the lumen, known as the “tunica intima”, is composed of endothelial cells (ECs) and intimal smooth muscle cells (SMCs). The middle layer, called the “tunica media”, is composed of medial smooth muscle cells. Eventually, the outermost layer, called the “tunica adventitia”, comprises fibroblasts and extracellular matrix (ECM) components as well as microvessels (vasa vasorum), particularly in large blood vessels [10, 11] (Fig. 1). Although autologous vascular transplantation minimizes immune responses, the high occurrence of occlusion and the need for multiple surgical procedures have restricted the effectiveness of autologous replacement approaches [12].
Vascular graft tissue engineering constitutes a crucial aspect of tissue engineering with the objective of regenerating or generating new blood vessels with the help of bioactive and biocompatible materials [13].
Synthetic vascular grafts serve as substitutes for autologous vessels under certain conditions. In the long term, these grafts have shown satisfactory outcomes when used in large-diameter arteries (> 8 mm); however, their applicability in small-diameter vessels (< 6 mm) is limited due to unfavorable patency rates [14]. To address this limitation, attempts have been made to enhance the performance of synthetic grafts. One such approach involves the seeding of autologous endothelial cells onto the luminal surface of synthetic graft vessels, which has been shown to improve patency rates. Nevertheless, even with these improvements, the performance of synthetic grafts has not surpassed that of autologous vessels [15].
The first engineered blood vessel structures were produced in the mid-1980s by Weinberg and Bell [16]. Since then, various methods have been adopted to produce similar structures. In general, scaffold-based production methods can be classified into three categories: synthetic polymers, biopolymers, and biodegradable polymers [17].
Vascular tissue engineering typically entails meeting four fundamental requirements: suitable mechanical properties, blood compatibility, endothelial support, and biodegradability.
Mechanical properties
Tissue-engineered vascular grafts must have specific mechanical characteristics. These include compliance, which allows seamless integration with adjacent vessels, and the appropriate mechanical strength and elasticity to withstand blood pressure without deformation [18].
Blood compatibility
Blood compatibility refers to the ability of a material or device to interact with blood without causing adverse reactions [19]. Like other blood-related devices, tissue engineering vascular grafts (TEVGs) share similar mechanisms related to thrombosis; however, there are various antithrombotic strategies for the modification of TEVGs, including the use of antithrombotic agents, platelet inhibitors, or fibrinolysis agents. One effective approach involves surface endothelialization because the vascular endothelium on the inner surface of blood vessels is inherently compatible with blood. Another method is surface passivation, which prevents external surfaces from coming into contact with blood and can be achieved through the use of zwitterionic or hydrophilic polymers [18].
Endothelial friendliness
The primary goal of vascular graft tissue engineering is to promote neovascularization and the formation of new blood vessels, which mainly depend on the secretion of ECM by adherent endothelial cells. Therefore, an ideally compatible TEVG should guarantee the adhesion of endothelial cells and provide a conducive microenvironment for cell proliferation supported by the presence of growth factors and bioactive molecules [18].
Several strategies can enhance endothelium friendliness in TEVGs. Some growth factors can be directly incorporated into the polymer solution before electrospinning [20] or attached to heparin through covalent bonding [21]. Polydopamine, known for its anchoring properties, can also be utilized to coat the graft surface with growth factors [22].
However, it is essential to consider the relatively short half-life of growth factors, which can lead to their inactivity. To address this limitation, sustainable release methods have been developed to ensure prolonged release. Another alternative method involves modifying endothelial cells to secrete growth factors. By introducing pDNA to produce growth factors in transfected endothelial cells, both cell viability and ECM production can be significantly increased [23].
Biodegradability
In vascular graft tissue engineering, the choice of polymer is crucial, and it should ideally be biodegradable to reduce concerns related to immunogenicity and thrombus formation. The biodegradation of the polymer should align with the pace of new blood vessel formation. Premature or delayed degradation may hinder blood vessel formation and exacerbate immunogenicity concerns, respectively. Polycaprolactone (PCL), poly glycolic acid (PGA), and Polylactic acid (PLA) are among the common biodegradable polyesters used in this context. These polymers offer controlled degradation properties, allowing for synchronized tissue regeneration and polymer breakdown [24].
Since any deficiency in these aspects causes a disturbance in the neovascularization process, all four requirements must be coordinated and work in harmony [18].
Cell sourcing in vascular tissue engineering
Selecting the right cell source is a crucial step in achieving success in tissue engineering. Considerations should encompass vital characteristics such as the rate of cell survival, proliferation potential, differentiation capabilities, ability to integrate into the host tissue, and ease of accessing these cells (Table 1).
Autologous vascular cells
The term “autologous vascular cells” typically refers to endothelial cells and vascular smooth muscle cells sourced directly from the patient’s own body, making them very compatible in terms of immunity. However, the practical application of primary autologous cells presents certain challenges, prompting researchers to explore alternative approaches, such as deriving ECs and vascular smooth muscle cells (VSMCs) from stem cells. These challenges include limitations in cell quantity due to donor age, as well as issues related to poor proliferation and regeneration capacity [25].
Mesenchymal stem cells (MSCs)
MSCs, also referred to as mesenchymal stromal cells, are the most promising candidates for vascular tissue engineering. These cells are particularly appealing because of their ease of isolation, rapid expansion rate, immune evasion [26] and potential for differentiation into mesodermal lineages, including osteocytes, chondrocytes, adipocytes, and even nonmesodermal lineages, such as neural cells [27], hepatocytes [28] and pneumocytes [29]. The ability of MSCs to differentiate toward vascular lineages, including ECs and SMCs, coupled with their secretion of paracrine factors, position them as valuable contributors to vascular regeneration [30]. This versatility and regenerative potential make MSCs a promising avenue for advancing vascular tissue engineering efforts. In the following section, we will highlight three key attributes of MSCs that make them an appealing cell source for VTE treatment.
Progenitor cells
Progenitor cells are descendants of stem cells and require further differentiation to achieve specialization in specific cell types. These cells exhibit a distinct propensity to mature into their intended cell lineage. Progenitor cells are found throughout the body, obviating the necessity of isolating them from vessels. According to previous studies, progenitor cells such as endothelial progenitor cells (EPCs), smooth muscle progenitor cells (SMPCs), and pericytes are effective in vascular repair. During inflammation and shear stress, these cells are activated and begin to differentiate into different types of vascular cells. They also improve vascularization and angiogenesis [31,32,33]. However, an inherent challenge arises in their application, particularly in the elderly population, as the quantity of these cells and their differentiation potential diminish with age [33].
Emergence of Induced Pluripotent Stem cells (iPSCs)
iPSCs, a breakthrough in stem cell biology pioneered by Yamanaka et al., who earned a Nobel Prize in 2012, can differentiate into any cell type, offering vast potential for personalized medicine. Derived from accessible tissues such as skin or blood, iPSCs circumvent ethical issues and reduce immunogenic risks, representing promising advancements in tissue engineering, such as the production of vascular grafts. However, their use is limited by their potential for tumorigenicity, the presence of mitochondrial DNA mutations, and the complex, costly process of cell reprogramming and standardization [25, 34].
Extraembryonic perinatal tissues: new putative sources of stem cells
Perinatal stem cells (PSCs) are a remarkable category of stem cells derived from tissues that develop from the 20th week of pregnancy through the 4th week after birth [35]. While adult stem cells from various tissues hold promise as potential sources for cell therapy applications, certain challenges, including ease of isolation, pluripotency, self-renewal, and ethical considerations, narrow the range of viable tissue sources for cell isolation. Among the commonly sought-after tissues for stem cell extraction, such as adipose tissue and bone marrow, perinatal tissues such as the placenta, amnion, and chorion have proven to be rich sources of stem cells. The stem cells obtained from these perinatal tissues possess highly desirable characteristics, such as ease of access, abundance, noninvasive extraction methods, minimal ethical problems, and reduced immunologic compatibility problems [36]. Stem cells isolated from perinatal tissue can be broadly categorized into two main groups: hematopoietic stem cells (HSCs) and fetal MSCs. These cells are placed between embryonic and adult cells in terms of their stemness abilities [37].
Hematopoietic stem cells (HSCs)
HSCs, characterized by their multipotent nature, serve as precursors for various types of blood cells. HSCs isolated from bone marrow have a long history of use in the treatment of hematologic malignancies. However, a significant milestone in the field of stem cell therapy occurred in 1988 when umbilical cord blood cells were first successfully transplanted to treat genetic blood disorders. The patient was a young boy with Fanconi anemia who received cord blood cells, marking a pivotal moment in the therapeutic potential of cord blood stem cells. After this success, subsequent research revealed that cord blood cells exhibit remarkable differentiation capabilities, giving rise to erythroid, myeloid, and lymphoid cell lineages [37].
Fetal mesenchymal stem cells
In the past, the prevailing belief was that the main source of MSCs was the bone marrow. However, it has become evident that the number of MSCs in the bone marrow is relatively low, and their regenerative capacity diminishes after passage 10–12 [38]. Therefore, bone marrow-derived MSCs present limitations that restrict their suitability for cell therapy purposes. In contrast, fetal MSCs isolated from perinatal tissue, including the umbilical cord, umbilical cord blood, placental blood, and placenta, do not have these limitations and can be regarded as a valuable alternative for cell therapy purposes [39]. Fetal MSCs can differentiate into three cardiac lineages: cardiomyocytes, endothelial cells, and smooth muscle cells. Additionally, these cells are able to form capillary structures on Matrigel, while mesenchymal cells isolated from adult sources (bone marrow and adipose tissue) cannot. Therefore, the selection of MSCs from fetal sources, such as the umbilical cord or amniotic membrane/fluid, can be an attractive source of young cells for autologous cell transplantation [40]. In the following sections, the use of MSCs from perinatal tissues is discussed in more detail.
Stem cells in perinatal tissues
The use of umbilical cord blood in transplantation has a history spanning over 30 years. In addition to cord blood, the placenta and fetal annexes, including the amniotic membrane, chorionic villi, chorionic plate, Wharton jelly of the umbilical cord, decidua, and amniotic fluid, are rich repositories of diverse stem cell types. Among these, one can find trophoblast epithelial stem cells and mesenchymal stromal cells, further underscoring the abundant and varied stem cell resources within perinatal tissues [7]. The exploration of perinatal stem cell sources offers substantial promise for a broad spectrum of therapeutic applications, notably in the field of cardiovascular diseases. In the subsequent sections, we will delve into the specific applications of these cell sources and elucidate their roles in vascular tissue engineering. (Fig. 2).
Amniotic membrane
The amniotic membrane (AM) is the innermost membrane lining the fetal placenta and consists of five distinct layers, including the epithelial layer, which directly interfaces with amniotic fluid and is composed of amniotic epithelium cells (AECs). Beneath the epithelial layer lies the basement membrane, followed by the compact layer. The fibroblast layer is situated beneath the compact layer, and the spongy layer completes the structure. The basic function of the amniotic membrane is to provide a protective and supportive environment, shielding the developing embryo from external threats, potential infections, and harmful toxins [41]. The membrane has emerged as a suitable candidate for clinical applications, serving as a scaffold for tissue engineering or a carrier for the delivery of various cell types. AM possesses unique biological features, including low immunogenicity, antibacterial capacity, immunomodulation, antiscaring, anti-inflammatory properties, and hemocompatibility, as well as antiangiogenic and proapoptotic qualities, all without presenting ethical challenges [42,43,44]. Amniotic epithelial and mesenchymal cells isolated from AMs exhibit stem cell properties and express stemness markers such as Oct3/4, Sox2, Klf4, Nanog, TRA1-60, TA1-81, and SSEA4. Notably, these cells do not display tumorigenic characteristics after transplantation, largely due to the loss of their telomerase activity. Both AECs and amniotic mesenchymal stem cells (AMSCs) possess unique properties, including low immunogenicity, anti-proliferative effects on immune cells, anti-inflammatory properties, proliferation capability, and multipotent differentiation potential into cells with mesodermal, ectodermal, and endodermal lineages, and there is no need for invasive techniques to harvest them because they are discarded after birth [42, 43].
Amnion-derived epithelial and mesenchymal cells inhibit tumor growth and invasion through three pathways: the induction of B and T lymphocyte apoptosis through the secretion of soluble factors, including TNF-α, FasL, TRAIL, TGF-β, and macrophage migration-inhibitory factors; the stimulation of cell cycle arrest; and the inhibition of angiogenesis. Therefore, a new line of research has been initiated with a focus on the antiproliferative effects of amniotic epithelial and mesenchymal cells on tumor growth in the last decade [42].
AECs can integrate into the tumor vascular lumen, differentiate into ECs or smooth muscle cells, reduce dysregulated tumor angiogenesis, enhance vascular perfusion, and subsequently, induce the cytotoxic effects of cisplatin. Since the vascular structure is not repaired because of the interconnected and unstable molecular pathways of the tumor, the vasculature can only be rebuilt within a limited time. Evaluation of the multipotential stem cell features of AECs to monitor the vascular formation abilities of AECs in vitro and in vivo under different conditions confirmed that AECs differentiated into tumor vascular endotheliocytes or pericytes and enhanced tumor vascular integrity to more efficiently kill the tumor during treatment, providing a new approach for rebuilding tumor vascularity [45].
Amniotic fluid
Amniotic fluid (AF), found within the amnion cavity surrounding the developing fetus, plays a vital role in fetal protection and nourishment during embryogenesis. This fluid consists of water, various chemical substances, and an abundant supply of stem cells (especially amniotic fluid stem cells (AFSCs) and amniotic fluid mesenchymal stem cells (AF-MSCs)). These stem cells exhibit essential stem cell markers, including Oct-4, c-Myc, Sox2, Nanog, and SSEA3, as well as high levels of several MSC markers, including CD29, CD44, CD73, CD90, CD105, CXCR4, stromal cell-derived factor 1 receptor (SDF-1), CD146, CD166, and CD184. Importantly, AFSCs can be safely collected without ethical concerns, either during the second or third trimester of pregnancy or even at later stages. Their unique characteristics combined with their stem cell properties and low immunogenicity make AFSCs highly suitable for various applications in the field of tissue engineering [46].
The pluripotency of AFSCs falls between that of ASCs and ESCs. Amniotic fluid stem cells exhibit remarkable proliferation capacity, with significant growth observed within just 36 h. Importantly, AFSCs maintain stable telomerase activity and a normal karyotype even after undergoing 250 in vitro amplification cycles [47].
Human AFSCs can promote vascular development and increase vessel length, area, and thickness in cocultures. These cells can differentiate into ECs, known as AFSC-derived ECs (AFSC-ECs), which have endothelial-like cell functions and can form cohesive vascular networks. A study conducted in 2015 showed that coculturing AFSCs with AFSCs and ECs within a fibrin/PEG matrix had a synergistic effect on various network parameters. The results revealed that the development of robust vessels relied on the presence of both AFSCs-ECs and AFSCs, each contributing to their vasculogenic and perivascular potential, respectively. In addition, fibrin/PEG hydrogels not only promoted capillary-like network formation but also offered advantages in terms of biocompatibility, mechanical stability, and vasculogenesis [48].
In 2016, Zhang et al. investigated the impact of glial cell line-derived neurotrophic factor (GDNF) on the differentiation of AFSCs into vascular endothelial-like cells. GDNF, known for its role as a neurotrophic factor of dopaminergic neurons, also acts as a tissue morphogen that enhances the differentiation of stem cells. The results indicated that AFSCs express EC markers such as vWF and CD31 after one week of differentiation and can be applied at vascular injury sites to promote angiogenesis. While GDNF improved the capacity of AFSCs to differentiate, these cells did not display the complete vascular morphology of mature ECs [47].
Human AFSCs can be induced to differentiate into vascular ECs by overexpressing the Ets transcription factors (TFs) Etv2, Fli1, and Erg. These converted amniotic cells successfully acquired an EC-like immunophenotype; however, their functional performance in EC assays was inferior to that of fully mature ECs. Sox17 expression is crucial for the proper functioning of ECs in vascular engraftment. Whereas Ets transcription factors help distinguish EC-like cells from nonvascular amniotic cells, Sox17 increases morphogenesis gene expression and facilitates the integration of transplanted converted cells into injured blood vessels. Therefore, the regulation of the Sox17 gene is essential for the generation of long-lasting, engraftable, and stable ECs following initial EC gene induction by Ets [49].
In addition, AF-MSCs have shown superior potential compared to BM-MSCs because they can differentiate into multiple cell lineages representing all three embryonic germ layers, such as chondrocytes, ECs, hepatocytes, and neurons, highlighting their remarkable versatility [50]. The characteristics of amniotic fluid stem cells (AFSCs), amniotic ECs (AECs), and AMSCs are compared in Table 2, and an overview of research in the field of vascular tissue engineering involving these cells is shown in Table 3.
Chorion
The chorion, which lines the inner surface of the trophoblast, is formed from the embryonic mesoderm on the 14th day of human pregnancy, and at this stage, the extracellular space separates it from the amniotic membrane [53].
Chorionic membrane
The chorionic membrane serves as the connection between the fetus and maternal tissue and is separated from the amniotic membrane by a layer of collagen fibers. Comprising two layers, the mesenchymal layer and the trophoblastic layer, the chorionic membrane contains MSCs. These cells can differentiate into all three germ layers: mesodermal, endodermal, and ectodermal [54]. Due to its exceptional biomechanical properties and low immunogenicity, the chorionic membrane can be used as a scaffold either independently or in conjunction with an AM for vascular tissue engineering. In the amniochorionic membrane, the epithelial cells of the amniotic membrane and the trophoblast layer of the chorion can be separated and removed through enzymatic solutions and mechanical scraping, resulting in a membrane that supports the growth of ECs and promotes angiogenesis. This unique structure holds significant promise for applications in vascular tissue engineering [55].
Chorionic villi
Chorionic villi are finger-like projections on the chorion that harbor cells with a multipotent mesenchymal stromal phenotype. Under suitable induction conditions, these cells can differentiate into various cell types, including neurons, cartilage, osteocytes, and adipocytes [56, 57]. Elevated levels of hydrogen peroxide in cardiovascular diseases and diabetes can lead to endothelial dysfunction, resulting in increased side effects and immune responses and ultimately the onset of thrombosis and atherosclerosis. Mesenchymal stem/stromal cells derived from the chorionic villi of human term placentae (v-MSCs) are able to protect human ECs against hydrogen peroxide-induced damage. v-MSCs reduce the detrimental effects of hydrogen peroxide on the proliferation, migration, angiogenesis, and permeability of ECs. Additionally, they modulate the expression of genes associated with EC cell function, including those related to survival and apoptosis. These cells hold promise for cell therapy aimed at repairing vascular damage caused by glucose and hydroxide peroxide, thereby reducing the adverse effects of cardiovascular diseases and diabetes [58].
Using the principle of tissue engineering techniques in conjunction with autologous cells and biodegradable scaffolds opens up possibilities for the fabrication of heart valves, blood vessels, and myocardial structures. Currently, cardiovascular tissue engineering can be a breakthrough for revolutionizing the treatment of congenital heart diseases, particularly among young patients. A significant challenge in treating these individuals is the absence of a suitable replacement structure similar to a cardiovascular valve. The development of a living and growing autologous structure could eliminate a major obstacle in their treatment journey. Advances in high-resolution imaging technologies now enable the early detection of most defects before birth, typically around the 20th week of gestation. To facilitate treatment, it becomes crucial to isolate cells during pregnancy for the subsequent production of tissue engineering implants either at birth or prenatally.
vMSCs hold promise as a suitable cell source for pediatric tissue engineering applications. Schmidt et al. were the first to suggest the possibility of using these cells for in vitro production of living heart valves [59]. In line with this, a study conducted by Weber et al. involved the extraction of MSCs from chorionic villi that are normally sampled from the applicant and cultivated in vitro. The cells were seeded onto a synthetic biodegradable scaffold to produce heart valve leaflets. The surface of this engineered structure was endothelialized with autologous endothelial progenitor cells derived from amniotic fluid or umbilical cord blood during pregnancy. The resulting tissue exhibited cellular phenotypes, an extracellular matrix composition, and a DNA content comparable to that of its native counterpart. vMSCs are significant for advancing congenital tissue engineering approaches [60].
vMSCs have also shown promise in the treatment of acute myocardial infarction, one of the most critical heart diseases. It has been proven that first-trimester placental chorion mesenchymal stem cells (fCMSCs) are better at reducing the symptoms of this disease in vivo than third-trimester placental chorion mesenchymal stem cells (tCMSCs) and BM-MSCs. Compared with tCMSCs, fCMSCs express higher levels of proangiogenic genes (PDGFD, VEGFA, and TNC), leading to significantly enhanced tube formation. Moreover, fCMSCs exhibit significantly lower expression of antiangiogenic genes (SPRY1 and ANGPTL1) than tCMSCs. Additionally, the improvement in cardiac function achieved by fCMSCs is significantly greater than that achieved by treatment with both tCMSCs and BM-MSCs [61].
Chorionic plate
The chorionic plate is composed of the amniochorionic membrane and fetal vessels. As the amniotic membrane is removed, the stem cells of the chorionic plate can be isolated from the area nearest to the umbilical cord. These cells have a mesenchymal phenotype and are able to differentiate into various lineages, including liver, cartilage, adipose, and bone lineages [62]. The decellularized human chorionic plate holds promise for use as a grafting material and in experimental vascularization studies. Cryopreserved human chorionic plate tissue can be decellularized using a perfusion method involving freeze‒thaw steps and chemical treatments. This approach minimizes the use of chemicals and exposure time. In terms of biocompatibility, when primary human umbilical vein endothelial cells (HUVECs) are cultured on this graft, they demonstrate endothelialization. Furthermore, the structure maintains cell-specific phenotypic and expression patterns [63].
The route of cell transplantation to damaged tissue is another critical factor in stem cell therapy. Various methods are available for delivering cells to the heart, including intravenous, intracoronary, coronary sinus, and direct epicardial injection. Among these methods, the direct intramuscular injection method is the most effective in terms of the quantity of delivered cells, with approximately 11% of the transferred cells engrafting into the desired area [64]. Inflammatory cytokines also play a role in the homing and engraftment of stem cells to damaged tissues and organs [65]. Once they reach the target area and are successfully transplanted, these cells can carry out their biological activities, such as proliferation, differentiation, and apoptosis, to facilitate the regeneration of damaged tissue [66].
Jung et al. conducted an in vivo study in rats using labeled chorionic plate-derived MSCs (CP-MSCs) to investigate the optimal transplantation route for treating injured livers. They compared direct transplantation, intrasplenic transplantation, and intravenous transplantation via the tail vein (TTP) with a nontransplanted treatment group and concluded that the therapeutic efficacy of the first two methods was superior to that of the TTP group. This outcome underscores the therapeutic ability of CP-MSCs to promote functional recovery of injured tissues and highlights the importance of selecting the appropriate transplantation routes for achieving the best outcome [67].
Identifying the optimal transplantation route for effective homing of CP-MSCs in cardiovascular diseases remains a significant challenge. Additionally, there is a need to optimize the delivery method to enhance cell engraftment and the survival rate.
Recent studies have shown the advantages of cells derived from the chorionic plate over those derived from the chorionic villi, including greater clonogenic potential and greater expression of cell cycle-related genes, ultimately leading to improved heart function in MI mouse models. Additionally, the exosomes obtained from the culture of these cells show potent angiogenic properties, suggesting that they have valuable potential in vascular tissue engineering [68, 69].
In another study, a comparative analysis involving CP-MSCs, ChorionicVilli-MSCs, decidua-derived MSCs, and umbilical cord blood (UCB) MSCs was conducted, focusing on cell proliferation and migration abilities. The findings showed that CP-MSCs had superior performance in these criteria compared to the other cell types. Additionally, CP-MSCs outperformed other groups in regulating macrophage polarization, specifically shifting macrophages from the M1 phenotype to the M2 phenotype [62]. Notably, compared with CD106-MSCs, CP-MSCs express CD106 markers, which are associated with heightened proliferative capacity and immune regulation potential [70].
Umbilical cord
The umbilical cord (UC), once considered a biological waste at the time of birth, is now recognized as a perinatal organ that plays a crucial role in facilitating the exchange of nutrients and gases (oxygen and carbon dioxide) between the placenta and the fetus. This remarkable organ, with an average length of 50–60 cm and more than 40 L of blood flow, has emerged as a valuable source of HSCs and MSCs. Importantly, it offers the advantage of being noninvasive and without any ethical concerns. An anatomical cross-section of the umbilical cord revealed that the UC is composed of two arteries and a vein without any branches [71], which are surrounded by Wharton’s jelly, a gelatinous substance rich in ECM proteins, including collagens, glycosaminoglycans such as hyaluronic acid and chondroitin sulfate, as well as growth factors such as IGF-1 and PDGF [72]. Wharton’s jelly serves the vital function of preventing blood vessels from clumping and provides flexibility to the cord. The umbilical cord is further enveloped by a membrane consisting of two layers: mesenchymal and epithelial layers.
Umbilical cord stem cells are a rich source of various stem cell types, including endothelial progenitors, epithelial stem cells, MSCs, and HSCs. These stem cells can be isolated from both cord blood and cord tissue and have shown promise in tissue repair through two primary mechanisms: the release of related cytokines and differentiation into specific cell types needed for tissue regeneration [71].
MSCs derived from Wharton’s jelly (WJ-MSCs) offer several advantages over other sources of MSCs, such as those from the BM. These advantages include a high proliferation rate, a significant capacity for differentiation into various cell types, low immunogenicity, ease of harvesting, and the potential to obtain large quantities of cells during the harvest process [71].
WJ-MSCs secrete various growth factors and cytokines, including G-CSF, HGF, PDGFAA, TGF-β, IL-6, and IL-8. These secreted factors play crucial roles in immunomodulation, cell proliferation, differentiation, growth, and tissue repair, making WJ-MSCs valuable for clinical applications [71, 73].
One notable characteristic of WJ-MSCs is their expression of self-renewal and pluripotency markers, including Oct-4, Sox-2, Nanog, SSEA-4, Tra-1-60, and Tra-1-81. These markers indicate the ability of these cells to maintain their undifferentiated state and their potential to differentiate into various cell lineages [74]. Although MSCs can be successfully isolated from Wharton’s jelly (WJ), the perivascular space (PRV) and the umbilical membrane (UCM) in UC differ, and they may exhibit variations depending on the specific region of isolation [73].
The feasibility of using WJ-MSCs as a suitable cell source for cardiovascular tissue engineering was first demonstrated in 2002. Hoerstrup et al. seeded WJ-MSCs onto a bioabsorbable scaffold in a biomimetic flow culture system and demonstrated the feasibility of generating pulmonary artery conduits using WJ-MSCs. Morphological and mechanical analysis revealed that tissue-engineered pulmonary conduits closely resembled native human pulmonary arteries. This research highlighted the potential of human WJ-MSCs as a readily available cell source for tissue engineering applications, eliminating the need to sacrifice intact vascular donor structures [75].
A more recent study conducted in 2020 investigated the ability of WJ-MSCs seeded on chitosan/hyaluronic acid multilayered films to differentiate into endothelial-like cells. The results were promising, indicating that WJ-MSCs could yield endothelial-like cells in a relatively short time (15 days) in a nontraumatic manner. Such polyelectrolyte films containing an endothelium resulting from the differentiation of MSCs can be used to reduce the risk of graft rejection [76].
Investigating the synergistic effects of gene and stem cell-based therapy on preventing neointimal formation, a common issue associated with vein graft failure, was first performed by Qingxi Qu et al. In this study, the miRNA-126-3p gene, an EC-specific angiogenic miRNA, was transfected into human UC-MSCs using a lentiviral vector. Therapeutic upregulation of miRNA-126-3p had several positive effects, including preventing restenosis in vein grafts, improving EC function through paracrine mechanisms, repairing dysfunctional endothelium, and reducing neointimal hyperplasia in vein grafts in rats. This improvement was attributed to the synthesis and secretion of various bioactive molecules, such as angiogenic factors, growth factors, and cytokines, by MSCs [77].
Severe human disorders, such as cardiovascular and peripheral vascular disease, often require the use of vascular grafts. However, the use of autologous vessels such as the saphenous vein of glutaraldehyde-fixed bovine and porcine xenografts is associated with issues such as a limited number of suitable patient vessels and susceptibility to calcification and chronic immune rejection. One suggested approach is the decellularization of human umbilical arteries with inner diameters ranging from 1 to 4 mm. While decellularization removes cellular components and donor antigens, potentially reducing the risk of immune responses, it leaves behind acellular vascular grafts that need to be repopulated with vascular cell populations to become fully functional. In 2018, an efficient method was developed to repopulate decellularized human umbilical arteries (hUAs) with WJ-MSCs. This approach aimed to produce HLA-matched vascular grafts, addressing some of the limitations associated with conventional graft sources [78]. Vessel bioreactors are commonly used for repopulating vascular grafts under specific conditions, but they often face challenges related to low repopulation efficacy. In an investigation, researchers sought to enhance the repopulation process by culturing human umbilical cord mesenchymal stem cells (hUCMSCs) on decellularized human umbilical arteries in media supplemented with cord blood platelet lysate (CBPL). Mallis et al. reported that CBPL significantly improved cell adhesion, proliferation, and differentiation through the presence of various growth factors, including TGF-β1, FGF, TNF-α, IL-1, IL-3, IL-6, PDGF, and matrix metalloproteases. Moreover, the use of CBPL enabled the differentiation of VSMCs from WJ-MSCs [79]. In another study by Mallis and colleagues, this approach successfully repopulated decellularized hUAs, leading to an increase in total hydroxyproline and sGAG contents. These results suggest that in vitro production of VSMCs, which involves collagen and sGAG synthesis, may be facilitated by factors such as SOX9, RUNX2, and MSX2 [80].
The angiogenic effect of MSCs such as WJ-MSCs on HUVECs has been demonstrated in numerous studies. These effects involve stabilizing the EC network and secreting vasculogenic growth factors, including hepatocyte growth factor. In both autogenic and allogenic cell sources, WJ-MSCs have been shown to promote angiogenesis and enhance vascular tube formation when cocultured with ECs for three days [81].
To ensure the success of endothelialization, it is essential to address challenges such as cell coverage loss due to exposure to physiological levels of shear stress in an active environment. Research has shown that shear stress preconditioning can improve cell retention and enhance the performance of ECs. In one study, HUVECs were preconditioned with shear stress on silk fibroin nanofibrous scaffolds at various time intervals and amplitudes. The results of this research suggest that ECs require sufficient time to acclimate to changing shear stress levels to withstand physiological levels. A gradual increase in shear stress over time can improve EC tolerance to shear stress and enhance the antithrombogenic function of engineered vascular grafts. This process involves an extracellular matrix (ECM)-specific mechanosensitive signaling pathway in which integrin β1, focal adhesion kinase (FAK), and fibronectin (FN) play significant roles [82].
ECs were used to form a monolayer of cells in the lumen of a vascular graft made of polycaprolactone/gelatin/fibrinogen, which was modified by a thermoforming process and coated with fibronectin and collagen IV. The results of this study showed that human cord blood-derived endothelial cells (hCB-ECs) can proliferate, produce endothelial nitric oxide synthase (eNOS), respond to interleukin 1β through the upregulation of VCAM-1 and ICAM-1, and reduce platelet deposition [83].
Expanding available resources for autologous to allogeneic (analog) applications in vascular tissue engineering faces a significant challenge due to the expression of human leukocyte antigen class I (HLA I) on the cell surface of ECs, which can lead to antibody-mediated immune responses and graft rejection. Recent advances in the field have used RNA interference (RNAi) to stably silence the expression of HLA I proteins in ECs via lentiviral vectors without affecting the morphological and functional properties of ECs. The silenced ECs were able to maintain the expression of key endothelial markers, including endothelial nitric oxide synthase, von Willebrand factor, CD31, and vascular endothelial cadherin. These markers are essential for maintaining a functional endothelial barrier, regulating blood coagulation, and controlling vessel tone.
Furthermore, HLA I-silenced ECs retained their ability to perform crucial endothelial functions. They are capable of absorbing acetylated low-density lipoprotein (acLDL) and forming capillary-like tube structures when embedded in 3D fibrin gels and exposed to unidirectional flow, similar to nontransduced cells [84]. The proliferation of ECs is aided by sphingosine-1-phosphate (S1P), an effective additive that also protects Syndecan-1 (SDC1) from shedding, which is important for preventing platelet adhesion. Compared to the controls, their results demonstrated that S1P reduced thrombus formation and enhanced HUVEC proliferation [85].
From another point of view, the physiological characteristics of conduit endothelialization strategies are inferior to those of native vessels due to the absence of VSMCs, which play a crucial role in vessel structure and function [86]. As an example of the utilization of smooth muscle cells in vessel engineering, human umbilical artery-derived smooth muscle cells (hUASMCs) were cultured on an electrospun scaffold containing fibrinogen extracted from human umbilical cord blood samples. To enhance the poor elastogenesis property of the scaffold, PCL was incorporated as a reinforcing material [87].
In 2018, Gökçinar-Yagci and her colleagues attempted to create a fully natural triple-layered vascular construct that mimics all the layers of a blood vessel using natural scaffolds and differentiated vascular cells. In this study, a triple-layered vascular construct was created by combining SMCs and fibroblasts, which were differentiated from perivascular cells (PCs) extracted from the human umbilical cord vein. Collagen type I/elastin/dermatan sulfate was used to form the tunica media, and collagen type I/fibrin was used for the tunica adventitia. Subsequently, HUVECs were seeded onto the construct using the cell sheet engineering method [88].
While this vascular graft closely resembled native blood vessels with a diameter of less than 5 millimeters, its weak mechanical properties made it unable to withstand the pressure within a blood vessel. To address this limitation, another study introduced a biocompatible electrospun polyurethane (PU) scaffold between the tunica intima and media layers of the construct to provide mechanical reinforcement. Polyurethane nanofibers create a suitable environment for HUVECs, enhancing their tensile strength and elastic modulus. As a result, layers of HUVECs, SMCs, and fibroblasts align with each other, strengthening the graft [89]. An overview of research in the field of vascular tissue engineering involving cells isolated from the umbilical cord is shown in Table 4.
Decidua
The decidua, a tissue in the uterus, is divided into three regions: the basalis, capsularis, and parietalis. The decidua basalis and parietalis are abundant sources of mesenchymal stem cells. These versatile cells can differentiate into various cell types from different germ layers, including lung cells, liver cells, cartilage, adipocytes, neurons, osteoblasts, and skeletal and cardiac myocytes, under laboratory conditions. They have demonstrated effectiveness in the treatment of several diseases, such as breast cancer, multiple sclerosis, and diabetes, and in reducing inflammation in the central nervous system [96,97,98,99]. Research has indicated that decidual mesenchymal stem cells (DMSCs) are more readily isolated from tissue and more accessible than bone marrow mesenchymal stem cells (BMSCs). Additionally, metabolomics analysis revealed a significant increase in ornithine metabolism, which is related to angiogenesis, in DMSCs.
In vivo studies have shown that the transplantation of DMSCs into murine models of acute myocardial infarction (MI) leads to a significant increase in neovascularization and cardiac remodeling compared to the transplantation of BMSCs. Consequently, compared with BMSCs, DMSCs exhibit superior efficacy in terms of revascularization and cardiac regeneration following MI [100].
Furthermore, the ability of human decidua basalis mesenchymal stem cells (DBMSCs) to survive and function in an inflammatory environment characterized by a high concentration of lipopolysaccharide has been explored. Inflammatory conditions are known triggers for certain diseases, such as arteriosclerosis. The results of this study indicated that there were no significant differences between the DBMSC-treated group and the control group. This finding suggested that DBMSCs can maintain their activities, including adhesion, proliferation, and migration, even under inflammatory conditions. Therefore, DBMSCs have the potential to be promising candidates for the treatment of inflammatory diseases, including arteriosclerosis [101].
In a comparative study, the biological characteristics of UCMSCs and MSCs derived from decidua parietalis (DP-MSCs) were investigated. Various features, including cell doubling times, colony formation rates, immune phenotypes, differentiation capacity, and the levels of secreted factors, were assessed for both cell types. Despite DP-MSCs exhibiting increased levels of keratinocyte growth factor, vascular endothelial growth factor, and stem cell factor, UCMSCs exhibited increased proliferation and colony formation rates. Moreover, UC-MSCs exhibited a shorter doubling time than DP-MSCs. Additionally, the concentration of basic fibroblast growth factor in the supernatant of UC-MSCs was notably greater than that in the supernatant of DP-MSCs. Based on these findings, researchers have concluded that UC-MSCs have great potential for effective applications in vascular tissue engineering and regenerative medicine [102].
Potential clinical application
When exploring cell therapy in clinical trials, it’s crucial to choose diseases for treatment that not only match the cell product’s action mechanism and show promise in preclinical studies but also address severe illnesses lacking effective treatments. This approach is primarily aimed at conditions that are both severely debilitating and critically lacking in medical solutions, underlining the importance of targeting diseases with no current therapy standards [103].
In cardiovascular treatments, for instance, non-autologous valve or conduit implants often face issues like obstructive tissue growth and calcification. This has led to a shift towards developing autologous, living tissues engineered in vitro, which can regenerate damaged cardiovascular tissue. Among the promising candidates for vascular diseases, placenta-derived cell therapies such as placenta derived adherent stromal cells (PLX-PAD) and Human Placenta-derived Cells (PDA-002) have shown potential, particularly for treating peripheral arterial disease (PAD). Within this area, patient groups are identified based on several factors, including those impacting enrolment and regulatory considerations. PLX-PAD, for example, is seen as particularly suited for critical limb ischemia patients, who face a dire prognosis including high rates of amputation and mortality, and significantly reduced quality of life. These patients, especially that ineligible for revascularization, have no existing treatment options, marking a significant unmet medical need that PLX-PAD aims to address. Early-phase trials in this patient group have shown promising signs of safety and effectiveness, including pain reduction and improved tissue perfusion, providing insights into potentially effective dosages [103, 104].
Furthermore, WJ-MSCs have been recognized for their clinical potential in vascular tissue engineering, with successful applications in animal models and human trials. For instance, autologous heart valves derived from human WJ-MSCs have been effectively used in sheep, demonstrating comparable functional and structural qualities to native valves. In a study involving patients with acute myocardial infarction, WJ-MSCs were safely administered and showed significant improvements in heart tissue viability and perfusion, positioning them as a viable alternative to traditional stem cell therapies for heart repair [105, 106].
The first human trial to assess the safety of administering UCMSCs through both intra-arterial and intravenous routes in patients with acute ischemic stroke is recruiting. This Phase 1 study has enrolled 14 participants to test the innovative UCMSCs treatment. The trial includes a follow-up period of 12 months and explores a method of administration never before attempted in humans, presenting potential new risks and benefits [107]. In another study, researchers are investigating the effectiveness of a novel combination therapy using intranasal conditioned medium and intraparenchymal transplantation of UCMSCs to stimulate neurogenesis in patients with acute strokes. This trial features three groups: one receiving the combination therapy, a second receiving only UCMSCs, and a third serving as a control group with standard neurological and neurotrophic drugs. The hypothesis is that the combination therapy will most effectively promote neurogenesis in these patients [108]. Additionally, a study is set to explore the safety and feasibility of UCMSC catheter transplantation for treating left ventricular dysfunction post-acute myocardial infarction. Slated to start in December 2023 and projected to end in December 2025, this Phase 1 trial will involve 40 patients split into two groups: one receiving the UC-MSC transplantation and the other receiving standard care. The primary focus will be monitoring Major Adverse Cardiac Events (MACE) to evaluate safety during the 12 months following treatment [109].The advancements in using extra-embryonic Stem Cells in regenerative medicine highlight the diverse therapeutic possibilities these cells might offer. Despite the promise, the outcomes from both pre-clinical and clinical studies are still in early stages and require further clarification. The characteristics and therapeutic potential of extra-embryonic MSCs are not fully understood, necessitating additional research into their role in cell therapy and tissue engineering. Additionally, developing biomaterials compatible with these stem cells, without compromising their regenerative and immune-modulating capabilities, remains a critical area for future research [110]. Table 5 shows the clinical approaches using extra-embryonic stem cells.
Conclusion
Vascular tissue engineering is a promising approach for regenerating damaged blood vessels and developing new therapeutic strategies for heart diseases. Perinatal stem cells, derived from extraembryonic tissues, have immense potential in addressing the symptoms of cardiovascular diseases due to their angiogenic, immunomodulatory, and endothelialization-promoting properties. Recent studies suggest that not only the perinatal stem cells themselves but also the soluble and insoluble factors they release could play a pivotal role in tissue regeneration. Soluble factors like growth factors (e.g., VEGF, FGF), cytokines (e.g., IL-6, TNF-alpha), and hormones (human Chorionic Gonadotropin, human Placental Lactogen) alongside insoluble factors such as, collagen and fibronectin, may offer a cell-free therapeutic approach. This innovative strategy provides a novel direction for future research that could potentially simplify therapeutic strategies, reduce risks associated with cell-based therapies, and enhance the scalability of treatments. However, more research is required to overcome the existing challenges and to translate these promising findings into effective clinical therapies, which can offer new hope for patients with cardiovascular diseases. In conclusion, the field of vascular tissue engineering, particularly through the innovative use of extraembryonic tissue-derived bioactive factors, is rapidly evolving and holds great promise for the future of cardiovascular disease treatment.
Data availability
Not applicable.
Abbreviations
- acLDL:
-
Acetylated low-density lipoprotein
- AECs:
-
Amniotic epithelium cells
- AF:
-
Amniotic fluid
- AFMSCs:
-
Amniotic fluid mesenchymal stem cells
- AFSCs:
-
Amniotic fluid stem cells
- AFSC-ECs:
-
Amniotic fluid stem cell-derived endothelial cells
- AM:
-
Amniotic membrane
- AMSCs:
-
Amniotic mesenchymal stem cells
- ASCs:
-
Adipose-derived stem cells
- BMSCs:
-
Bone marrow mesenchymal stem cells
- CaMKIIγ:
-
Ca2+/calmodulin-dependent protein kinase II
- CBPL:
-
Cord blood platelet lysate
- CT:
-
Clotting time
- DMSCs:
-
Decidual mesenchymal stem/stromal cells
- DBMSCs:
-
Human Decidual Basalis Mesenchymal Stem Cells
- ECs:
-
Endothelial cells
- ECM:
-
Extracellular matrix
- EPCs:
-
Endothelial progenitor cells
- ESCs:
-
Extraembryonic tissue-derived cells
- ePTFE:
-
Expanded polytetrafluoroethylene
- eNOS:
-
Endothelial nitric oxide synthase
- FAK:
-
Focal adhesion kinase
- fCMSCs:
-
First-trimester placental chorion mesenchymal stem cells
- GDNF:
-
Glial cell line-derived neurotrophic factor
- MSC:
-
Mesenchymal stem cell
- MI:
-
Myocardial infarction
- iPSCs:
-
Induced pluripotent stem cells
- HSCs:
-
Hematopoietic stem cells
- HUVECs:
-
Human umbilical vein endothelial cells
- HLA I:
-
Human leukocyte antigen class I
- hUAs:
-
Human umbilical arteries
- hCB-ECs:
-
Human cord blood-derived endothelial cells
- SMCs:
-
Smooth muscle cells
- SMPCs:
-
Smooth muscle progenitor cells
- SDF-1:
-
Stromal cell-derived factor 1 receptor
- S1P:
-
Sphingosine-1-phosphate
- VEGF:
-
Vascular Endothelial Growth Factor
- VEGFR1:
-
Vascular Endothelial Growth Factor receptor-1
- v-MSCs:
-
Mesenchymal stem/stromal cells derived from chorionic villi
- vWb:
-
von Willebrand factor
- PCL:
-
Polycaprolactone
- PCs:
-
Perivascular cells
- PSCs:
-
Perinatal stem cells
- PDGF:
-
Platelet-Derived Growth Factor
- PDGFR:
-
Platelet-derived growth factor receptor
- PGA:
-
Poly glycolic acid
- PLA:
-
Polylactic acid
- PLX-PAD:
-
Placenta derived adherent stromal cells
- PDA-002:
-
Human Placenta-derived Cells
- PT:
-
Prothrombin time
- PU:
-
Polyurethane
- aPTT:
-
Activated partial thromboplastin time
- RNAi:
-
RNA interference
- TEVGs:
-
Tissue engineering vascular grafts
- TGF-β:
-
Transforming growth factorβ
- TFs:
-
Transcription factors
- tCMSCs:
-
Third-trimester placental chorion mesenchymal stem cells
- SPC:
-
Sphingosylphosphorylcholine
- SMA:
-
Smooth muscle actin
- UC:
-
Umbilical cord
- hUC:
-
Human umbilical cord
- UCB:
-
Umbilical cord blood
- UCPs:
-
Umbilical cord pericytes
- UCMSCs:
-
Umbilical cord mesenchymal stem cells
- VSMCs:
-
Vascular smooth muscle cells
- WJ-MSCs:
-
Wharton’s jelly mesenchymal stem cells
References
Zoghbi WA, Duncan T, Antman E, Barbosa M, Champagne B, Chen D et al. Sustainable development goals and the future of Cardiovascular Health: a Statement from the Global Cardiovascular Disease Taskforce. J Am Heart Assoc. 2014;3(5).
Ong CS, Zhou X, Huang CY, Fukunishi T, Zhang H, Hibino N. Tissue engineered vascular grafts: current state of the field. Expert Rev Med Devices. 2017;14(5):383–92.
Antoniou GA, Chalmers N, Georgiadis GS, Lazarides MK, Antoniou SA, Serracino-Inglott F, et al. A meta-analysis of endovascular versus surgical reconstruction of femoropopliteal arterial disease. J Vasc Surg. 2013;57(1):242–53.
Weintraub WS, Grau-Sepulveda MV, Weiss JM, O’Brien SM, Peterson ED, Kolm P, et al. Comparative effectiveness of revascularization strategies. N Engl J Med. 2012;366(16):1467–76.
Kwon SG, Kwon YW, Lee TW, Park GT, Kim JH. Recent advances in stem cell therapeutics and tissue engineering strategies. Biomater Res. 2018;22(1).
Su T, Huang K, Daniele MA, Hensley MT, Young AT, Tang J, et al. Cardiac stem cell Patch Integrated with Microengineered Blood vessels promotes Cardiomyocyte Proliferation and Neovascularization after Acute myocardial infarction. ACS Appl Mater Interfaces. 2018;10(39):33088–96.
de la Torre P, Flores AI. Current status and future prospects of perinatal stem cells. Genes (Basel). 2020;12(1):6.
Silini AR, Masserdotti A, Papait A, Parolini O. Shaping the future of Perinatal cells: lessons from the past and interpretations of the Present. Front Bioeng Biotechnol. 2019;7.
Balbi C, Bollini S. Fetal and perinatal stem cells in cardiac regeneration: moving forward to the paracrine era. Placenta. 2017;59:96–106.
Dan P, Velot É, Decot V, Menu P. The role of mechanical stimuli in the vascular differentiation of mesenchymal stem cells. J Cell Sci. 2015.
Junqueira LCCJ. Basic histology: text & atlas. New York: McGraw-Hill; 2005.
Schmidt CE, Baier JM. Acellular vascular tissues: natural biomaterials for tissue repair and tissue engineering. Biomaterials. 2000;21(22):2215–31.
Benrashid E, McCoy CC, Youngwirth LM, Kim J, Manson RJ, Otto JC, et al. Tissue engineered vascular grafts: origins, development, and current strategies for clinical application. Methods. 2016;99:13–9.
Chlupáč J, Filová E, Bačáková L. Blood vessel replacement: 50 years of development and tissue engineering paradigms in vascular surgery. Physiol Res. 2009;S119–40.
Deutsch M, Meinhart J, Zilla P, Howanietz N, Gorlitzer M, Froeschl A, et al. Long-term experience in autologous in vitro endothelialization of infrainguinal ePTFE grafts. J Vasc Surg. 2009;49(2):352–62.
Weinberg CB, Bell E. A Blood Vessel Model Constructed from Collagen and Cultured Vascular Cells. Science (1979). 1986;231(4736):397–400.
Devillard CD, Marquette CA. Vascular tissue Engineering: challenges and requirements for an Ideal large scale blood vessel. Front Bioeng Biotechnol. 2021;9.
Wu J, Hu C, Tang Z, Yu Q, Liu X, Chen H. Tissue-engineered vascular grafts: balance of the Four Major requirements. Colloid Interface Sci Commun. 2018;23:34–44.
Ratner BD, Horbett TA, Wagner WR. Evaluation of Blood–Materials Interactions. In: Biomaterials Science. Elsevier; 2020. pp. 879–98.
Asiri A, Saidin S, Sani MH, Al-Ashwal RH. Epidermal and fibroblast growth factors incorporated polyvinyl alcohol electrospun nanofibers as biological dressing scaffold. Sci Rep. 2021;11(1):5634.
Henry JJD, Yu J, Wang A, Lee R, Fang J, Li S. Engineering the mechanical and biological properties of nanofibrous vascular grafts for in situ vascular tissue engineering. Biofabrication. 2017;9(3):035007.
Lee Y, Bin, Shin YM, Lee Jhye, Jun I, Kang JK, Park JC, et al. Polydopamine-mediated immobilization of multiple bioactive molecules for the development of functional vascular graft materials. Biomaterials. 2012;33(33):8343–52.
Liu Y, Lu J, Li H, Wei J, Li X. Engineering blood vessels through micropatterned co-culture of vascular endothelial and smooth muscle cells on bilayered electrospun fibrous mats with pDNA inoculation. Acta Biomater. 2015;11:114–25.
Patel HN, Thai KN, Chowdhury S, Singh R, Vohra YK, Thomas V. In vitro degradation and cell attachment studies of a new electrospun polymeric tubular graft. Prog Biomater. 2015;4(2–4):67–76.
Jouda H, Larrea Murillo L, Wang T. Current progress in Vascular Engineering and its clinical applications. Cells. 2022;11(3):493.
Ankrum JA, Ong JF, Karp JM. Mesenchymal stem cells: immune evasive, not immune privileged. Nat Biotechnol. 2014;32(3):252–60.
Scuteri A, Miloso M, Foudah D, Orciani M, Cavaletti G, Tredici G. Mesenchymal stem cells neuronal differentiation ability: a real perspective for nervous system repair? Curr Stem Cell Res Ther. 2011;6(2):82–92.
Wu XB, Tao R. Hepatocyte differentiation of mesenchymal stem cells. Hepatobiliary Pancreat Dis Int. 2012;11(4):360–71.
HUANG K, KANG X, WANG X, WU S, XIAO J, LI Z, et al. Conversion of bone marrow mesenchymal stem cells into type II alveolar epithelial cells reduces pulmonary fibrosis by decreasing oxidative stress in rats. Mol Med Rep. 2015;11(3):1685–92.
Gu W, Hong X, Potter C, Qu A, Xu Q. Mesenchymal stem cells and vascular regeneration. Microcirculation. 2017;24(1).
Tao J, Cao X, Yu B, Qu A. Vascular Stem/Progenitor cells in Vessel Injury and Repair. Front Cardiovasc Med. 2022;9.
Deng J, Ni Z, Gu W, Chen Q, Nowak WN, Chen T, et al. Single-cell gene profiling and lineage tracing analyses revealed novel mechanisms of endothelial repair by progenitors. Cell Mol Life Sci. 2020;77(24):5299–320.
Gago N, Pérez-López V, Sanz-Jaka JP, Cormenzana P, Eizaguirre I, Bernad A, et al. Age-dependent depletion of human skin-derived progenitor cells. Stem Cells. 2009;27(5):1164–72.
Generali M, Casanova EA, Kehl D, Wanner D, Hoerstrup SP, Cinelli P, et al. Autologous endothelialized small-caliber vascular grafts engineered from blood-derived induced pluripotent stem cells. Acta Biomater. 2019;97:333–43.
Jia H, Caputo M, Ghorbel MT. Stem cells in vascular graft tissue engineering for congenital heart surgery. Interv Cardiol (Lond). 2013;5(6):647–62.
Nur Fariha MMCKTGTAHA. Human chorion-derived stem cells: changes in stem cell properties during serial passage. Cytotherapy. 2011;13(5):582–93.
Zhang Y, Li Z, Liu N. The Stemness of Perinatal stem cells. Perinatal stem cells. Singapore: Springer Singapore; 2019. pp. 27–37.
Karahuseyinoglu S, Cinar O, Kilic E, Kara F, Akay GG, Demiralp DÖ, et al. Biology of Stem cells in human umbilical cord stroma: in situ and in Vitro surveys. Stem Cells. 2007;25(2):319–31.
Parolini O, Alviano F, Bagnara GP, Bilic G, Bühring HJ, Evangelista M et al. Concise Review: Isolation and Characterization of Cells from Human Term Placenta: Outcome of the First International Workshop on Placenta Derived Stem Cells. Stem Cells. 2008;26(2):300–11.
Ramkisoensing AA, Pijnappels DA, Askar SFA, Passier R, Swildens J, Goumans MJ, et al. Human embryonic and fetal mesenchymal stem cells differentiate toward three different cardiac lineages in contrast to their adult counterparts. PLoS ONE. 2011;6(9):e24164.
Dadkhah Tehrani F, Firouzeh A, Shabani I, Shabani A. A review on modifications of amniotic membrane for Biomedical Applications. Front Bioeng Biotechnol. 2021;8.
Niknejad H, Yazdanpanah G, Ahmadiani A. Induction of apoptosis, stimulation of cell-cycle arrest and inhibition of angiogenesis make human amnion-derived cells promising sources for cell therapy of cancer. Cell Tissue Res. 2016;363(3):599–608.
Schwab RHM, Goonetilleke M, Zhu D, Kusuma GD, Wallace EM, Sievert W, et al. Amnion epithelial cells — a therapeutic source. Curr Stem Cell Rep. 2021;7(1):13–29.
McDonald C, Siatskas C, Bernard CA. The emergence of amnion epithelial stem cells for the treatment of multiple sclerosis. Inflamm Regen. 2011;31(3):256–71.
Guan L, Zhang A. Amniotic epithelial cells reverse abnormal vascular structure and function in endometrial carcinoma. Int J Clin Exp Pathol. 2019;12(7):2405–24.
Jafari A, Rezaei-Tavirani M, Farhadihosseinabadi B, Zali H, Niknejad H. Human amniotic mesenchymal stem cells to promote/suppress cancer: two sides of the same coin. Stem Cell Res Ther. 2021;12(1):126.
Zhang R, Lu Y, Li J, Wang J, Liu C, Gao F, et al. Glial cell line-derived neurotrophic factor induced the differentiation of amniotic fluid-derived stem cells into vascular endothelial-like cells in vitro. J Mol Histol. 2016;47(1):9–19.
Benavides OM, Quinn JP, Pok S, Petsche Connell J, Ruano R, Jacot JG. Capillary-Like Network formation by human amniotic fluid-derived stem cells within Fibrin/Poly(Ethylene Glycol) Hydrogels. Tissue Eng Part A. 2015;21(7–8):1185–94.
Schachterle W, Badwe CR, Palikuqi B, Kunar B, Ginsberg M, Lis R, et al. Sox17 drives functional engraftment of endothelium converted from non-vascular cells. Nat Commun. 2017;8(1):13963.
Tancharoen W, Aungsuchawan S, Pothacharoen P, Markmee R, Narakornsak S, Kieodee J, et al. Differentiation of mesenchymal stem cells from human amniotic fluid to vascular endothelial cells. Acta Histochem. 2017;119(2):113–21.
Kakavand M, Yazdanpanah G, Ahmadiani A, Niknejad H. Blood compatibility of human amniotic membrane compared with heparin-coated ePTFE for vascular tissue engineering. J Tissue Eng Regen Med. 2017;11(6):1701–9.
Weber B, Kehl D, Bleul U, Behr L, Sammut S, Frese L, et al. In vitro fabrication of autologous living tissue-engineered vascular grafts based on prenatally harvested ovine amniotic fluid-derived stem cells. J Tissue Eng Regen Med. 2016;10(1):52–70.
Muench MO, Kapidzic M, Gormley M, Gutierrez AG, Ponder KL, Fomin ME et al. The human chorion contains definitive hematopoietic stem cells from the 15th week of gestation. Development. 2017.
Battula VL, Bareiss PM, Treml S, Conrad S, Albert I, Hojak S, et al. Human placenta and bone marrow derived MSC cultured in serum-free, b-FGF-containing medium express cell surface frizzled-9 and SSEA-4 and give rise to multilineage differentiation. Differentiation. 2007;75(4):279–91.
Shariatzadeh S, Shafiee S, Zafari A, Tayebi T, Yazdanpanah G, Majd A, et al. Developing a pro-angiogenic placenta derived amniochorionic scaffold with two exposed basement membranes as substrates for cultivating endothelial cells. Sci Rep. 2021;11(1):22508.
Ventura Ferreira MS, Bienert M, Müller K, Rath B, Goecke T, Opländer C, et al. Comprehensive characterization of chorionic villi-derived mesenchymal stromal cells from human placenta. Stem Cell Res Ther. 2018;9(1):28.
Chien C, Yen BL, Lee F, Lai T, Chen Y, Chan S, et al. In Vitro differentiation of human placenta-derived multipotent cells into hepatocyte‐like cells. Stem Cells. 2006;24(7):1759–68.
Basmaeil YS, Al Subayyil AM, Khatlani T, Bahattab E, Al-Alwan M, Abomaray FM, et al. Human chorionic villous mesenchymal stem/stromal cells protect endothelial cells from injury induced by high level of glucose. Stem Cell Res Ther. 2018;9(1):238.
Schmidt D, Mol A, Breymann C, Achermann J, Odermatt B, Gössi M et al. Living Autologous Heart valves Engineered from Human prenatally harvested progenitors. Circulation. 2006;114(1_supplement).
Weber B, Zeisberger SM, Hoerstrup SP. Prenatally harvested cells for cardiovascular tissue engineering: fabrication of autologous implants prior to birth. Placenta. 2011;32:S316–9.
Yu S, You X, Liang H, Li Y, Fu Y, Zhang X, et al. First trimester placental mesenchymal stem cells improve cardiac function of rat after myocardial infarction via enhanced neovascularization. Heliyon. 2021;7(1):e06120.
Huang Q, Yang Y, Luo C, Wen Y, Liu R, Li S, et al. An efficient protocol to generate placental chorionic plate-derived mesenchymal stem cells with superior proliferative and immunomodulatory properties. Stem Cell Res Ther. 2019;10(1):301.
Schneider KH, Aigner P, Holnthoner W, Monforte X, Nürnberger S, Rünzler D, et al. Decellularized human placenta chorion matrix as a favorable source of small-diameter vascular grafts. Acta Biomater. 2016;29:125–34.
Hashemzadeh MR, Taghavizadeh Yazdi ME, Amiri MS, Mousavi SH. Stem cell therapy in the heart: Biomaterials as a key route. Tissue Cell. 2021;71:101504.
Penn MS, Mangi AA. Genetic enhancement of Stem Cell Engraftment, Survival, and Efficacy. Circ Res. 2008;102(12):1471–82.
Bai X, Yan Y, Coleman M, Wu G, Rabinovich B, Seidensticker M, et al. Tracking long-term survival of Intramyocardially Delivered Human adipose tissue-derived stem cells using Bioluminescence Imaging. Mol Imaging Biol. 2011;13(4):633–45.
Jung J, Na KH, Lee MJ, Moon J, Kim G, Il, Jang JJ, et al. Efficacy of chorionic plate-derived mesenchymal stem cells isolated from placenta in CCl4-injured rat liver depends on transplantation routes. Tissue Eng Regen Med. 2013;10(1):10–7.
Brown C, McKee C, Bakshi S, Walker K, Hakman E, Halassy S, et al. Mesenchymal stem cells: cell therapy and regeneration potential. J Tissue Eng Regen Med. 2019;13(9):1738–55.
Komaki M, Numata Y, Morioka C, Honda I, Tooi M, Yokoyama N, et al. Exosomes of human placenta-derived mesenchymal stem cells stimulate angiogenesis. Stem Cell Res Ther. 2017;8(1):219.
Yang ZX, Han ZB, Ji YR, Wang YW, Liang L, Chi Y, et al. CD106 identifies a subpopulation of mesenchymal stem cells with Unique Immunomodulatory Properties. PLoS ONE. 2013;8(3):e59354.
Alatyyat SM, Alasmari HM, Aleid OA, Abdel-maksoud MS, Elsherbiny N. Umbilical cord stem cells: background, processing and applications. Tissue Cell. 2020;65:101351.
Beiki B, Zeynali B, Seyedjafari E. Fabrication of a three dimensional spongy scaffold using human Wharton’s jelly derived extra cellular matrix for wound healing. Mater Sci Engineering: C. 2017;78:627–38.
Semenova E, Grudniak MP, Machaj EK, Bocian K, Chroscinska-Krawczyk M, Trochonowicz M, et al. Mesenchymal stromal cells from different parts of umbilical cord: Approach to Comparison & characteristics. Stem Cell Rev Rep. 2021;17(5):1780–95.
Semenov V. Mesenchymal stem cells derived from Wharton’s Jelly and their potential for Cardio-Vascular tissue Engineering. Open Tissue Eng Regen Med J. 2011;4(1):64–71.
Hoerstrup SP, Kadner A, Breymann C, Maurus CF, Guenter CI, Sodian R, et al. Living, autologous pulmonary artery conduits tissue engineered from human umbilical cord cells. Ann Thorac Surg. 2002;74(1):46–52.
Dennaoui H, Chouery E, Harmoush C. Endothelial differentiation of Wharton’s Jelly-derived mesenchymal stem cells seeded on chitosan/hyaluronan multilayer films. Cell Ther Transpl. 2020;9(4):59–67.
Qu Q, Wang L, Bing W, Bi Y, Zhang C, Jing X, et al. miRNA-126-3p carried by human umbilical cord mesenchymal stem cell enhances endothelial function through exosome-mediated mechanisms in vitro and attenuates vein graft neointimal formation in vivo. Stem Cell Res Ther. 2020;11(1):464.
Mallis P, Michalopoulos E, Dinou A, Vlachou MS, Panagouli E, Papapanagiotou A, et al. Development of HLA-matched vascular grafts utilizing decellularized human umbilical artery. Hum Immunol. 2018;79(12):855–60.
Mallis P, Sokolis DP, Katsimpoulas M, Kostakis A, Stavropoulos-Giokas C, Michalopoulos E. Improved Repopulation Efficacy of Decellularized Small Diameter Vascular grafts utilizing the cord blood platelet lysate. Bioengineering. 2021;8(9):118.
Mallis P, Papapanagiotou A, Katsimpoulas M, Kostakis A, Siasos G, Kassi E, et al. Efficient differentiation of vascular smooth muscle cells from Wharton’s jelly mesenchymal stromal cells using human platelet lysate: a potential cell source for small blood vessel engineering. World J Stem Cells. 2020;12(3):203–21.
Kunkanjanawan H, Kunkanjanawan T, Khemarangsan V, Yodsheewan R, Theerakittayakorn K, Parnpai R. A Xeno-Free Strategy for Derivation of Human umbilical vein endothelial cells and Wharton’s Jelly Derived Mesenchymal stromal cells: a feasibility study toward personal cell and vascular based therapy. Stem Cells Int. 2020;2020:1–8.
Liu H, Gong X, Jing X, Ding X, Yao Y, Huang Y, et al. Shear stress with appropriate time-step and amplification enhances endothelial cell retention on vascular grafts. J Tissue Eng Regen Med. 2017;11(11):2965–78.
Ardila D, Liou JJ, Maestas D, Slepian M, Badowski M, Wagner W, et al. Surface Modification of Electrospun Scaffolds for endothelialization of tissue-Engineered vascular grafts using human cord blood-derived endothelial cells. J Clin Med. 2019;8(2):185.
Lau SEDCOMWBSCHABRWMFCBU. Low immunogenic endothelial cells maintain morphological and functional properties required for vascular tissue Engineering. Tissue Eng Part A. 2018;24(5–6):432–47.
Hsia K, Yang MJ, Chen WM, Yao CL, Lin CH, Loong CC, et al. Sphingosine-1-phosphate improves endothelialization with reduction of thrombosis in recellularized human umbilical vein graft by inhibiting syndecan-1 shedding in vitro. Acta Biomater. 2017;51:341–50.
Ghorbel MT, Jia H, Swim MM, Iacobazzi D, Albertario A, Zebele C, et al. Reconstruction of the pulmonary artery by a novel biodegradable conduit engineered with perinatal stem cell-derived vascular smooth muscle cells enables physiological vascular growth in a large animal model of congenital heart disease. Biomaterials. 2019;217:119284.
Woods I, Black A, Molloy EJ, Jockenhoevel S, Flanagan TC. Fabrication of blood-derived elastogenic vascular grafts using electrospun fibrinogen and polycaprolactone composite scaffolds for paediatric applications. J Tissue Eng Regen Med. 2020;term.3100.
Gökçinar-Yagci B, Yersal N, Korkusuz P, Çelebi-Saltik B. Generation of human umbilical cord vein CD146 + perivascular cell origined three-dimensional vascular construct. Microvasc Res. 2018;118:101–12.
Çelebi-Saltik B, Öteyaka MÖ, Gökçinar-Yagci B. Stem cell-based small-diameter vascular grafts in dynamic culture. Connect Tissue Res. 2021;62(2):151–63.
Gu WHXLBANWBSDJXYHYRXXQ. Smooth muscle cells differentiated from human mesenchymal stem cells regulated by microRNA (miR)-503 and mir-222-5p are suitable for vascular tissue engineering. J Biol Chem. 2018;293(21):8089–102.
Sasagawa T, Shimizu T, Yamato M, Okano T. Endothelial colony-forming cells for preparing prevascular three-dimensional cell-dense tissues using cell-sheet engineering. J Tissue Eng Regen Med. 2016;10(9):739–47.
Cathery W, Faulkner A, Jover E, Rodriguez-Arabaolaza I, Thomas AC, Avolio E et al. Umbilical cord pericytes provide a viable alternative to mesenchymal stem cells for neonatal Vascular Engineering. Front Cardiovasc Med. 2021;7.
Muniswami DM, Reddy LVK, Amirtham SM, Babu S, Raj AN, Sen D, et al. Endothelial progenitor/stem cells in engineered vessels for vascular transplantation. J Mater Sci Mater Med. 2020;31(12):119.
Chlupac J, Matejka R, Konarik M, Novotny R, Simunkova Z, Mrazova I, et al. Vascular remodeling of clinically used patches and decellularized pericardial matrices recellularized with autologous or allogeneic cells in a porcine carotid artery model. Int J Mol Sci. 2022;23(6):3310.
Keshi E, Tang P, Weinhart M, Everwien H, Moosburner S, Seiffert N, et al. Surface modification of decellularized bovine carotid arteries with human vascular cells significantly reduces their thrombogenicity. J Biol Eng. 2021;15(1):26.
Macias MI, Grande J, Moreno A, Domínguez I, Bornstein R, Flores AI. Isolation and characterization of true mesenchymal stem cells derived from human term decidua capable of multilineage differentiation into all 3 embryonic layers. Am J Obstet Gynecol. 2010;203(5):495.e9-495.e23.
Abomaray FM, Al Jumah MA, Alsaad KO, Jawdat D, Al Khaldi A, AlAskar AS, et al. Phenotypic and functional characterization of mesenchymal Stem/Multipotent stromal cells from Decidua Basalis of Human Term Placenta. Stem Cells Int. 2016;2016:1–18.
Cerrada A, de la Torre P, Grande J, Haller T, Flores AI, Pérez-Gil J. Human decidua-derived mesenchymal stem cells differentiate into functional alveolar type II-Like cells that synthesize and secrete pulmonary surfactant complexes. PLoS ONE. 2014;9(10):e110195.
Bravo B, Gallego MI, Flores AI, Bornstein R, Puente-Bedia A, Hernández J, et al. Restrained Th17 response and myeloid cell infiltration into the central nervous system by human decidua-derived mesenchymal stem cells during experimental autoimmune encephalomyelitis. Stem Cell Res Ther. 2016;7(1):43.
Chen K, Bai L, Lu J, Chen W, Liu C, Guo E et al. Human decidual mesenchymal stem cells obtained from early pregnancy improve Cardiac Revascularization Postinfarction by activating Ornithine Metabolism. Front Cardiovasc Med. 2022;9.
Alshareef GHMAAMBY. Phenotypic and functional responses of human decidua basalis mesenchymal stem/stromal cells to lipopolysaccharide of gram-negative bacteria. Stem Cells Cloning. 2021;51–69.
Guan Y, Xie Y, Li D, Zhu Y, Zhang X, Feng Y et al. Comparison of biological characteristics of mesenchymal stem cells derived from the human umbilical cord and decidua parietalis. Mol Med Rep. 2019.
Sher N, Ofir R. Clinical Development and commercialization of placenta-derived cell therapy. Perinatal stem cells. Elsevier; 2018. pp. 357–75.
Norgren L, Weiss N, Nikol S, Hinchliffe RJ, Lantis JC, Patel MR, et al. PLX-PAD cell treatment of critical limb ischaemia: rationale and design of the PACE trial. Eur J Vasc Endovasc Surg. 2019;57(4):538–45.
Gao LR, Chen Y, Zhang NK, Yang XL, Liu HL, Wang ZG, et al. Intracoronary infusion of Wharton’s jelly-derived mesenchymal stem cells in acute myocardial infarction: double-blind, randomized controlled trial. BMC Med. 2015;13:1–15.
Kim DW, Staples M, Shinozuka K, Pantcheva P, Kang SD, Borlongan CV. Wharton’s jelly-derived mesenchymal stem cells: phenotypic characterization and optimizing their therapeutic potential for clinical applications. Int J Mol Sci. 2013;14(6):11692–712.
’Hsu S, Shyu WC. Clinical trial.gov NCT04434768. 2020 [cited 2024 Apr 22]. Evaluate the Safety and Explore Efficacy of Umbilical Cord Mesenchymal Stem Cells in Acute Ischemic Stroke. https://clinicaltrials.gov/study/NCT04434768.
’Agus Aulia M. Clinical trial.gov. 2022 [cited 2024 Apr 22]. Combination of Conditioned Medium and Umbilical Cord-Mesenchymal Stem Cells Therapy for Acute Stroke Infarct. https://clinicaltrials.gov/study/NCT05008588.
’Shen C. ’LU G. Clinical trials.gov. 2023 [cited 2024 Apr 22]. UC-MSC Transplantation for Left Ventricular Dysfunction After AMI. https://clinicaltrials.gov/study/NCT03902067.
Malek A, Bersinger NA. Human placental stem cells: biomedical potential and clinical relevance. J Stem Cells. 2011;6(2):75.
Acknowledgements
Not applicable.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
MK designed the study, supervised the work, and provided comments. MAG and ZK were responsible for creating the tables and figures. ANS, HHA, MKe, IR, SH, MAG, ZK, and FK contributed to drafting the initial manuscript sections and subsequently revised them. MAG and ZK also participated in modifying and proofreading the initial draft. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
AI disclosure
The authors declare that artificial intelligence is not used in this study.
Competing interests
There are no known competing financial interests or personal relationships that influence this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Goushki, M.A., Kharat, Z., Kehtari, M. et al. Applications of extraembryonic tissue-derived cells in vascular tissue regeneration. Stem Cell Res Ther 15, 205 (2024). https://doi.org/10.1186/s13287-024-03784-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-024-03784-3