Abstract
Background
Intestinal duplication cyst is an infrequent congenital malformation that can involve all the segments of the gastrointestinal tract. The cases of intestinal duplication cyst involving the colon, appendix, and ileum in children are particularly uncommon. The symptoms of abdominal pain are similar to other acute abdominal diseases in children, such as appendicitis, intussusception, and intestinal obstruction, so sometimes its diagnosis is challenging and leads to misdiagnosis.
Case presentation
We report a 4-year-old Asian boy who presented to the pediatric emergency department with abdominal pain and vomiting but no fever, peritonitis, or mass. No abdominal abnormality was found via radiology and ultrasonography. After 2 days’ anti-inflammatory therapy, the patient was discharged with pain relief. A total of 9 months later, he was readmitted to the pediatric emergency department for the same complaint as the first admission. Abdominal physical examination and ultrasound examination were still negative. Barium examination found a large mass in the colon. Colonoscopy was performed before operation to confirm the rare co-cavity intestinal duplication cyst involving the colon, appendix, and ileum. After resection of intestinal duplication and ileocolonic anastomosis, the patient’s abdominal pain and vomiting has not recurred for 5 years postoperatively.
Conclusions
The diagnosis of intestinal duplication cyst in children is difficult, especially the rare co-cavity and long segmental intestinal duplication, which is easily misdiagnosed. Colonoscopy may be an effective auxiliary diagnostic method, especially for diseases that are difficult to diagnosed clinically, such as recurrent abdominal pain.
Similar content being viewed by others
Introduction
Intestinal duplication cyst is a rare congenital malformation with an estimated incidence of approximately 1:4500 autopsies [1], and it can involve all the segments of the gastrointestinal tract [2]. Most of these duplication cysts develop during the fetal, neonatal, and pediatric periods and have three common features: they are hollow structures lined with secretory gastrointestinal mucosa, and the smooth muscle in their walls is often shared with the contiguous intestine [3]. However, such duplication cysts are often misdiagnosed because of nonspecific clinical symptoms that vary from minor digestive problems to intestinal obstruction, gastrointestinal bleeding, or perforation [4]. Some procedures, such as contrast upper gastrointestinal series and computed tomography (CT) have diagnostic importance. Once diagnosed, surgical resection remains the main method of treatment with a good prognosis. In this report, we present an infrequent case of an intestinal duplication cyst involving the ileum, appendix, and colon in a pediatric patient and discuss the process of diagnosis by colonoscopy.
Case presentation
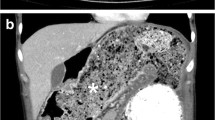
In May 2016, a 4-year-old male Asian patient was admitted to our hospital presenting with complaints of intermittent abdominal pain for 5 hours and vomiting for 1 hour. His parents reported that he was otherwise healthy and denied any family history of intestinal diseases except for what was believed to be an intussusception when he was 1 year old. Because of his previous history of intussusception, he had air enema examination first in the emergency department, but no abnormality was found. Then the patient underwent CT examination, which showed a huge cystic structure involving in the transverse colon of the upper abdomen (Fig. 1A, B). The air enema showed what appeared to be a large cystic mass in or immediately outside the lumen. Even after the air in the small intestine had cleared, the cystic structure persisted (Fig. 1C, D). The patient was finally diagnosed with ileocolonic intussusception and admitted to the surgery department. At admission, his vital signs were good, and his pulse, blood pressure, and temperature were normal. Combined with his medical history, abdominal examination, and imaging findings, the final clinical case discussion results were not consistent with an intussusception. After 2 days of anti-inflammatory treatment and infusion management, the patient’s symptoms improved, and he was discharged from the hospital after the abdominal ultrasound was negative.
CT scan showed a large cystic structure closely related to the intestine in the left abdominal cavity (arrows). A Recumbent position, B Coronal position. C The air enema showed what appeared to be a large cystic mass or immediately outside the lumen. D After the air in the small intestine has been cleared, the cystic structure persists (arrow). E barium enema (BE) showed cystic structure in the transverse colon. F 24 hours later, the ileocecum to the ascending colon showed two cavities, the main intestinal had been emptied of barium (long arrow), and the cystic lumen barium remained (short arrow)
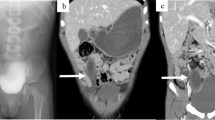
However, in February 2017, 9 months later, the boy went to our emergency department again with symptoms of intermittent abdominal pain for 4 days and vomiting for 3 days. Prior to this, he had received anti-inflammatory treatment in a local hospital, but it had no effect. Clinically, the patient’s vital signs were normal, and he had no bowel movements and did not have any substantial abdominal tenderness. On palpation, an ill-defined mass with minimal mobility was felt. Abdominal x-rays showed cystic structure in the upper abdomen, and the cyst contained a lot of gas and liquid. The patient underwent a barium enema (BE), which showed that the cystic structure communicated with the transverse colon, and barium could enter the cystic structure (Fig. 1E). Re-examination of x-ray after 24 hours showed that there were two intestinal cavities in the region of what would appear to be the ascending colon, the barium in the main intestine had been emptied, and the barium remained in the cystic structure coming off the lumen of the transverse colon (Fig. 1F). Because of the recurrent abdominal pain, we decided to perform a colonoscopy after communicating with the boy’s parents. During colonoscopy, we were surprised to find that the colon cavity was divided into an upper cavity and a lower cavity, with a septum in the middle (Fig. 2A, B). Although the terminal ileum was seen 10 cm after entering the main intestine, there was no appendiceal orifice (Fig. 2C). The appendiceal orifice was seen 15 cm after entering the cystic lumen (Fig. 2D). Therefore, the intraoperative diagnosis was intestinal duplication cyst arising from and communicating with the transverse colon.
Subsequently, an exploratory laparotomy was performed. During the surgical exploration, we found that it was originally a duplication cyst containing appendix (Fig. 3A, B). We decided to remove the ascending colon starting at the ileocolonic junction and transverse colon to include the duplication cyst and then performed an ileocolonic anastomosis. The length of colon removed was 16 cm, which included the duplication cyst. Anatomically, it was found that the entrance of the main intestine and the cystic lumen was located in the middle of the transverse colon, with a diameter of about 1.2 cm (Fig. 3C).
The patient received parenteral nutrition for 4 days after surgery, and resumed oral enteral nutrition on the fifth day. The hospital stay was 1 week. At 1 and 6 months postoperatively, the abdominal x-ray examination showed that the intestinal duplication cyst had completely disappeared. We followed up with the patient by telephone in February 2022, the fifth year after operation. He developed normally and had no complications. His parents were satisfied with our treatment.
Discussion
Intestinal duplication cyst is an uncommon congenital anomaly and usually but not always communicates with the regular bowel from which it arises [5]. The widely accepted classification of intestinal duplication includes five types: intestinal membrane type, intestinal wall cyst type, extra-intestinal cyst type, extra-intestinal tubular type, and solitary type (Fig. 4) [6]. Approximately 75% of duplication cysts are located within the abdominal cavity, of which only 13% are colonic [7]. Duplication of the cecum is very rare. Oudshoorn and Heij have reviewed 362 cases of duplication cysts reported in the literature and found only 16 cases of cecum duplications [8]. The present case was unique, as it was an extra-intestinal cyst that had a common wall with the colon and communicated with the colon lumen. It was a type III intestinal duplication cyst, involving duplication of the colon, cecum, appendix, and ileum. (Fig. 3A).
The clinical symptoms of intestinal duplication cyst depend on the type and structure, size, the presence of complications, and the location of the cyst connected to the surrounding structure [9]. In the absence of specific symptoms and signs, it is often misdiagnosed as other acute abdominal diseases, including acute gastroenteritis or intussusception, or labeled as Meckel’s diverticulum [10]. For this case, a retrospective analysis of the patient’s past medical history showed that he was diagnosed with intussusception due to abdominal pain and vomiting at the ages of 1 and 4 years, respectively. Through later air–barium enema imaging, we postulated intestinal duplication under barium imaging although there was no definitive radiographic confirmation of the diagnosis. Therefore, we believe that he was misdiagnosed in the past because he had similar manifestations with intussusception, including age, abdominal pain, abdominal mass, and air enema examination showing “cystic structure” of the intestinal cavity.
Ultrasonography, gastrointestinal contrast-enhanced abdominal computed tomography, and magnetic resonance imaging are commonly used to diagnose intestinal duplication cysts [10, 11]. In this case, the appearance of the structure in CT was that of a duplication cyst. The special feature of this case was the wide range of symptoms and the unusual radiographic findings of the duplication cyst on CT, which was rare and misdiagnosed. Secondly, we used colonoscopy to confirm the diagnosis, which was rarely reported in the literature.
Conclusions
In summary, the diagnosis of intestinal duplication cysts in children is difficult, especially rare co-cavity and the unusual radiographic findings, which can easily be misdiagnosed. Colonoscopy may be an effective auxiliary diagnostic method, especially for patients with recurrent abdominal pain who have cystic structures closely related to the colon in other examinations. For patients undergoing surgery, the treatment was effective, and the prognosis was good.
Availability of data and materials
Not applicable.
References
Herranz Barbero A, Prat Ortells J, Muñoz Fernández ME, Castañón García-Alix M, Figueras Aloy J. Duplicación quística intestinal. Caso clínico [Intestinal cystic duplication. Case report]. Arch Argent Pediatr. 2017;115(4):e233–6. https://doi.org/10.5546/aap.2017.e233.
Hamza AR, Bicaj BX, Kurshumliu FI, Zejnullahu VA, Sada FE, Krasniqi AS. Mesenteric Meckel’s diverticulum or intestinal duplication cyst: a case report with review of literature. Int J Surg Case Rep. 2016;26:50–2. https://doi.org/10.1016/j.ijscr.2016.06.043.
Cavar S, Bogovic M, Luetic T, Antabak A, Batinica S. Intestinal duplications–experience in 6 cases. Eur Surg Res. 2006;38(3):329–32. https://doi.org/10.1159/000094021.
Ildstad ST, Tollerud DJ, Weiss RG, Ryan DP, McGowan MA, Martin LW. Duplications of the alimentary tract. Clinical characteristics, preferred treatment, and associated malformations. Ann Surg. 1988;208(2):184–9.
Sinha A, Ojha S, Sarin YK. Completely isolated, noncontiguous duplication cyst. Eur J Pediatr Surg. 2006;16(2):127–9. https://doi.org/10.1055/s-2006-924004.
Okuda K. Obstructive disease of the inferior vena cava–an idiopathic type of Budd-Chiari syndrome. Trop Gastroenterol. 1997;18(3):91–2.
La Quaglia MP, Feins N, Eraklis A, Hendren WH. Rectal duplications. J Pediatr Surg. 1990;25(9):980–4. https://doi.org/10.1016/0022-3468(90)90242-2.
Oudshoorn JH, Heij HA. Intestinal obstruction caused by duplication of the caecum. Eur J Pediatr. 1996;155(4):338–40. https://doi.org/10.1007/BF02002724.
Khan RA, Wahab S, Ghani I. Neonatal intestinal obstruction: when to suspect duplication cyst of bowel as the cause. J Neonatal Surg. 2016;5(4):52. https://doi.org/10.21699/jns.v5i4.467.
Huang ZH, Wan ZH, Vikash V, Vikash S, Jiang CQ. Report of a rare case and review of adult intestinal duplication at the opposite side of mesenteric margin. Sao Paulo Med J. 2018;136(1):89–93. https://doi.org/10.1590/1516-3180.2017.0184030817.
Ogino H, Ochiai T, Nakamura N, Yoshimura D, Kabemura T, Kusumoto T, et al. Duplication cyst of the small intestine found by double-balloon endoscopy: a case report. World J Gastroenterol. 2008;14(24):3924–6. https://doi.org/10.3748/wjg.14.3924.
Acknowledgements
Not applicable.
Funding
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Contributions
FC and JL conceived, designed, and coordinated the project. FC collected and assembled data and drafted the manuscript. FC and JL edited the manuscript. JL critically revised the manuscript. FC and JL gave final approval of the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient’s legal guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, F., Liu, J. Colonoscopy diagnosis of recurrent abdominal pain in a 4-year-old boy with intestinal duplication cyst involving colon, appendix, and ileum: a case report. J Med Case Reports 18, 444 (2024). https://doi.org/10.1186/s13256-024-04780-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-024-04780-0