Abstract
Background
The rapid development of coronavirus disease 2019 vaccines during the pandemic has left their long-term effects largely unknown. Instances of autoimmune and subacute thyroiditis showing features of autoimmune/inflammatory syndrome induced by adjuvants have been reported post-vaccination. This case report aims to highlight the autoimmune/inflammatory syndrome induced by adjuvants syndrome after coronavirus disease 2019 vaccination, drawing attention to a possible connection with thyroid dysfunction and urging for further thorough research.
Case presentation
We present a case of thyroiditis induced by the COVISHIELD vaccine in a 37-year-old Indian woman. An apparently normal and healthy adult woman developed neck pain and easy fatigability 2 weeks after the second dose of COVISHIELD, which gradually increased and was associated with irritability, decreased sleep, excessive sweating, tremor, palpitation, and weight loss. She presented to the outpatient department after 1 week of symptoms and was evaluated with laboratory tests and imaging. She was diagnosed with thyroiditis due to the coronavirus disease 2019 vaccine and was treated with propranolol.
Conclusion
This case report adds to the growing evidence of coronavirus disease 2019 vaccine-related thyroid issues. The development of thyroiditis is rare and underreported post-coronavirus disease 2019 vaccination; hence, research to evaluate the association of coronavirus disease 2019 vaccines with thyroid dysfunction needs to be done in the future.
Similar content being viewed by others
Background
The novel coronavirus disease 2019 (COVID-19), which is caused by the virus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has resulted in pandemic worldwide. It created a devastating effect on the demographics of the world, causing 3.8 million deaths worldwide [1]. Multiple vaccines, each producing effects through different mechanisms, were developed rapidly, and at present, more than 1 billion people have been vaccinated. COVISHIELD is a monovalent vaccine developed by the Serum Institute of India. It consists of a single recombinant, replication-deficient chimpanzee adenovirus Oxford 1 (ChAdOx1) vector, which carries the genetic code for the S-glycoprotein of the coronavirus. Following its administration, the S-glycoprotein triggers localized activity, provoking the production of neutralizing antibodies and initiating a cellular immune response [2].
Several adjuvants are employed to enhance the vaccine responsiveness, and they can induce autoimmune and inflammatory responses by promoting immunogenic cross-reactivity in genetically predisposed individuals [3, 4]. Several autoimmune and subacute cases of thyroiditis have been documented after vaccine exposure, displaying characteristics akin to the autoimmune/inflammatory syndrome induced by adjuvants (ASIA) [3]. Very few cases of ASIA following COVID-19 vaccine have been reported [5, 6]. The endocrine system is primarily affected by COVID-19, with thyroid dysfunction being the most common endocrine condition following vaccination [7]. The aim of this case report is to bring attention to the potential connection between the COVID-19 vaccine and the emergence of thyroid dysfunction, thereby supplementing the existing occurrences and strengthening the evidential basis and consequently promoting more in-depth research into this subject.
Case presentation
A 37-year-old Indian woman who was apparently normal before the COVID-19 vaccination presented to the outpatient department (OPD) with complaints of pain in the neck for 2 weeks, which were present throughout the day. This was accompanied by easy fatigability, irritability, decreased sleep, increased sweating, tremor, palpitation, and weight loss of approximately 3 kg in the previous 3 weeks. One week before the onset of these symptoms, she had been administered the second dose of the COVISHIELD vaccine. There were no records of any viral or respiratory sickness prior to the emergence of the symptoms. The patient received the first dose of COVISHIELD 3 months before the second dose. The patient had no history of adverse events to the first dose of COVISHIELD, except for 2 days of mild fever that resolved spontaneously. The patient had no history of any comorbidities such as diabetes mellitus, hypertension, or cardiac conditions. There was no personal or family history of autoimmune disorders. She was a non-smoker, non-alcoholic, and a teacher by profession. On thyroid examination, there was no visible swelling; however, upon palpation, tenderness was present. Primary hyperthyroidism was found in the thyroid function test. On ultrasound of the neck, multiple colloid cysts on the right lobe of the thyroid along with ill-defined hypoechoic areas in both the lobes were identified. Thyroid scan report was suggestive of thyroiditis with decreased uptake of technetium (Fig. 1). The results of the complete laboratory investigations performed for this patient during the first OPD visit have been provided in Table 1. The patient was diagnosed with thyroiditis induced by COVISHIELD and was treated with a beta blocker (propranolol) for 3 weeks to control palpitation and tremors. This incident was reported to the Indian Pharmacopoeia Commission (IPC) with a worldwide unique identification, IN-IPC-300617048. The patient adhered to the treatment and tolerated the drug well. She developed no side effects during the treatment period. All the presented symptoms resolved within a month, and her thyroid function test became normal. The patient developed no symptoms during the next 2 months of follow-up.
Discussion
The presented case underscores a notable clinical association between COVID-19 vaccination and the subsequent development of thyroiditis. This 37-year-old woman exhibited a constellation of symptoms within weeks of receiving the second dose of the COVISHIELD vaccine. The temporal proximity of symptom onset to vaccination, coupled with the absence of any preexisting comorbidities, suggests a plausible link between the vaccine and the thyroid dysfunction. Thyroid function tests indicated primary hyperthyroidism, further supporting the diagnosis of vaccine-induced thyroiditis. The ultrasound findings, along with thyroid scan, added weight to the diagnosis. Notably, the patient’s symptoms ameliorated within a month, indicating the self-limiting nature of the condition. This case contributes to the growing evidence regarding potential autoimmune responses triggered by COVID-19 vaccines, particularly involving thyroid-related sequelae.
While COVID-19 infection is known to be associated with thyroiditis [8, 9], COVID-19 vaccines were also found to cause subacute thyroiditis. Few subacute thyroiditis cases have been documented following the Pfizer-BioNTech messenger RNA (mRNA) vaccine administration [10], as well as with CoronaVac, which is composed of inactivated SARS-CoV-2 virus [5]. There were a few new cases of Graves’ disease after the administration of the Pfizer vaccine. These cases were thought to potentially result from an autoimmune inflammatory syndrome triggered by adjuvants [11]. Adjuvants play a crucial role within the vaccine composition that basically improves the response of the vaccine [12]. Nonetheless, a portion of individuals with a genetic predisposition may experience significant adverse reactions when adjuvants are introduced. This is attributed to the initiation of autoimmune responses and pathways, which disrupt the delicate immunological equilibrium within the host. Such disruption promotes the widespread activation of B lymphocytes through mechanisms such as molecular mimicry or other analogous etiopathogenic pathways [3].
While ASIA elucidates the underlying mechanism of thyroiditis due to adjuvants, AstraZeneca’s COVISHIELD, which is manufactured using genetically modified human embryonic kidney 293 cells [13], encompasses additional pathways contributing to vaccine-triggered thyroid inflammation. Notably, the angiotensin-converting enzyme 2 (ACE2) receptor has been identified as the point of entry for the SARS-CoV-2 spike protein into thyroid cells [14]. This might be the cause of immunization-mediated damage to the thyroid gland. Spike proteins of COVID-19 attach to ACE2 receptors present on the endothelium, resulting in inflammation of endothelial cells. This will cause downregulation of ACE2 receptors leading to decreased production of nitric oxide and secondary mitochondrial damage [15]. It is also known that the antibodies developed against the coronavirus have the potential to interact with antigens present in cells, including those in the thyroid [16]. Furthermore, spike proteins demonstrate molecular mimicry with thyroid peroxidase. Consequently, the antibodies prompted by COVID-19 vaccination engage with the surface receptors of the thyroid gland, leading to a transient thyroiditis that gradually resolves.
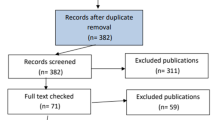
The strength of this case report lies in its documentation of the patient’s clinical presentation, laboratory findings, and response to treatment. The detailed thyroid function tests, ultrasound, and thyroid scan results provide comprehensive evidence to support the diagnosis. The reporting of this case to IPC adds value to the report, facilitating traceability and further investigation if necessary. Our case report was compiled in accordance with the Consensus-based Clinical Case Reporting (CARE) guidelines (Additional file 1). However, there are limitations to consider. This is a single case report, and thus causality cannot be definitively established. Individual variations in immune responses and underlying susceptibilities could contribute to the development of thyroiditis. Additionally, the long-term consequences or potential recurrence of thyroid dysfunction following subsequent vaccinations are yet to be determined. Despite these limitations, this case report raises an important flag for clinicians and researchers to monitor and investigate potential thyroid-related adverse events following COVID-19 vaccination.
Conclusion
This case adds to the growing evidence of COVID-19-vaccine-related thyroid issues. While this report highlights the need for further investigation, it also serves as a reminder of the importance of continuous monitoring and prompt reporting of potential vaccine-related adverse effects.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study. All necessary information related to the case report have been provided in the article. Waiver from the ethics committee and the patient’s consent form will be provided on reasonable request of the corresponding author.
Abbreviations
- COVID-19:
-
Novel coronavirus disease 2019
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- ChAdOx1:
-
Chimpanzee adenovirus Oxford 1
- ASIA:
-
Autoimmune/inflammatory syndrome induced by adjuvants
- OPD:
-
Outpatient department
- IPC:
-
Indian Pharmacopoeia Commission
- T3:
-
Triiodothyronine
- T4:
-
Thyroxine
- TSH:
-
Thyroid stimulating hormone
- ACE2:
-
Angiotensin converting enzyme 2
References
Cascella M, Rajnik M, Aleem A, Dulebohn SC, Di Napoli R. Features, evaluation, and treatment of coronavirus (COVID-19). StatPearls Treasure Island (FL): StatPearls Publishing; 2021.
Marathe S. Covishield-ChAdOx1 nCoV-19 Corona Virus Vaccine Insert, Domestic - New 02012021.cdr. :2.
Bragazzi NL, Hejly A, Watad A, Adawi M, Amital H, Shoenfeld Y. ASIA syndrome and endocrine autoimmune disorders. Best Pract Res Clin Endocrinol Metab. 2020;34(1): 101412.
Oyibo SO. Subacute thyroiditis after receiving the adenovirus-vectored vaccine for coronavirus disease (COVID-19). Cureus. 2021;13(6): e16045.
İremli BG, Şendur SN, Ünlütürk U. Three cases of subacute thyroiditis following SARS-CoV-2 vaccine: postvaccination ASIA syndrome. J Clin Endocrinol Metab. 2021;106(9):2600–5.
Das L, Bhadada SK, Sood A. Post-COVID-vaccine autoimmune/inflammatory syndrome in response to adjuvants (ASIA syndrome) manifesting as subacute thyroiditis. J Endocrinol Invest. 2022;45(2):465–7.
Wu Z, Hu Y, Xu M, Chen Z, Yang W, Jiang Z, et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy adults aged 60 years and older: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect Dis. 2021;21(6):803–12.
Dworakowska D, Morley S, Mulholland N, Grossman AB. COVID-19-related thyroiditis: a novel disease entity? Clin Endocrinol (Oxf). 2021;95(3):369–77.
Brancatella A, Ricci D, Cappellani D, Viola N, Sgrò D, Santini F, et al. Is subacute thyroiditis an underestimated manifestation of SARS-CoV-2 infection? Insights from a case series. J Clin Endocrinol Metab. 2020;105(10): dgaa537.
Subacute Thyroiditis After mRNA Vaccine for Covid-19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8089609/. Accessed 27 Oct 2021.
Vera-Lastra O, Ordinola Navarro A, Cruz Domiguez MP, Medina G, Sánchez Valadez TI, Jara LJ. Two cases of Graves’ Disease following SARS-CoV-2 vaccination: an autoimmune/inflammatory syndrome induced by adjuvants. Thyroid Off J Am Thyroid Assoc. 2021;31(9):1436–9.
Shoenfeld Y, Agmon-Levin N. “ASIA” - autoimmune/inflammatory syndrome induced by adjuvants. J Autoimmun. 2011;36(1):4–8.
Hernández AF, Calina D, Poulas K, Docea AO, Tsatsakis AM. Safety of COVID-19 vaccines administered in the EU: Should we be concerned? Toxicol Rep. 2021;8:871–9.
Li M-Y, Li L, Zhang Y, Wang X-S. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020;9(1):45.
Lei Y, Zhang J, Schiavon CR, He M, Chen L, Shen H, et al. SARS-CoV-2 spike protein impairs endothelial function via downregulation of ACE 2. Circ Res. 2021;128(9):1323–6.
Vojdani A, Vojdani E, Kharrazian D. Reaction of human monoclonal antibodies to SARS-CoV-2 proteins with tissue antigens: implications for autoimmune diseases. Front Immunol. 2020;11: 617089.
Acknowledgements
We acknowledge Indian Pharmacopoeia Commission (IPC) for their committed work in upholding the standards, safety, and effectiveness of medicines and vaccines, along with their contributions to the field of pharmacovigilance and for allowing us to publish this case report (worldwide unique ID: IN-IPC-300617048).
Funding
The authors declare that there was no funding source for this work.
Author information
Authors and Affiliations
Contributions
SJ and SSi initiated the conception of the case report for this patient. SJ, AA, AS, and SSa drafted the manuscript, table and figure. RSG, SBV, SSi, and SA contributed to the organization of the contents and provided expert guidance in writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Waiver for ethics committee approval has been obtained from the institute due to the nature of the article being a case report. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
CARE Checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sachin, J., Shukla, R., Anil, A. et al. COVISHIELD vaccine-induced thyroiditis: a case report. J Med Case Reports 17, 542 (2023). https://doi.org/10.1186/s13256-023-04279-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-023-04279-0