Abstract
Background
One of the most common types of congenital adrenal hyperplasia is an autosomal recessive disorder with 21-hydroxylase deficiency. The classical form, defined by cortisol insufficiency, is accompanied by prenatal androgen excess causing variable masculinization degrees of external genitalia in babies with a 46, XX karyotype.
Cases presentation
These five case reports highlight the management of Syrian females aged between 0 and 32 years with congenital adrenal hyperplasia. Two of the patients have been raised as males, while two had reconstructive surgery and one had hormonal therapy. Becoming mother was achieved by two patients
Conclusion
The integrated treatment of females with classical congenital adrenal hyperplasia CAH, which includes appropriate surgical procedures and controlled hormonal therapy, gives these females the opportunity to live as they are, and perhaps as mothers in the future.
Similar content being viewed by others
Introduction
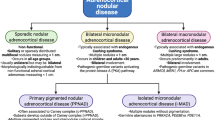
Congenital adrenal hyperplasia (CAH) with 21-hydroxylase deficiency (21-OHD) deficiency is an autosomal recessive disorder [18] caused by mutations in the CYP21A2 gene [19], and is considered one of the most common causes of genital ambiguity [28]. CAH clinical manifestations have been classified into two forms: classical CAH, which includes two types, severe salt wasting (SW) and non-SW or simple virilizing (SV), and a nonclassical (NC) form, in which postnatal androgen excess occurs during late puberty or early adulthood [12].
Female patients having a 46, XX karyotype with classical CAH are born with variable degrees of external genital ambiguity due to excess androgen during in utero development [3]. In addition to ambiguous female genitalia, affected patients with SW may exhibit life-threatening salt-losing crises during the neonatal period. Accelerated growth and skeletal maturation, hirsutism, oligomenorrhea, and infertility are faced later in life if patients were not treated or are affected by NC [25]. Appropriate treatment, regular follow-ups, and patient compliance are crucial factors for successful pregnancies. However, psychosocial factors or sexual orientation and the will to bear children influence the fertility rate [17].
In Syria, in cases of virilized external genitalia, parents used to consider these females newborns as males, especially in cases of severe virilization, until proven otherwise.
Almost all females with SW-CAH and more than 50% of those with SV-CAH had undergone at least one genital surgery on the clitoris and/or the vagina early in their childhood [23]. Early surgical treatment, rather than delayed or staged approaches for 46, XX CAH patients with specific degrees of genital virilization, has been included in guidelines for the Development of Comprehensive Care Centers for Congenital Adrenal Hyperplasia [4].
The role of the parents in sex assignment becomes crucial in all aspects of the decision-making process and all possible therapeutic options for the intersex child, particularly early versus delayed surgery [8].
Here we report the cases of five CAH females, two of them have been raised as males, two had reconstructive surgery, and one had hormonal therapy.
Materials and methods
Patients
The patients were being treated in the Children University Hospital, Al-Assad University Hospital, or in private endocrinology clinics between 2017 and 2020 in Damascus. Informed consent forms were signed by the patient or her guardian. This study was approved by the Damascus University research ethics committee (HRECPHARMDU Resolution No. 2). To establish the clinical diagnosis of 21-OHD, we collected the data from the medical records of each patient, including measurements of serum electrolytes, 17-hydroxy progesterone (17-OHP), glucose, bone age determination, and abdominal and pelvic ultrasonography. Cytogenetic evaluation was performed for sex determination.
Sample preparation
Peripheral blood samples were drawn from patients on ethylenediaminetetraacetic acid (EDTA) and frozen at −20 °C. We preformed DNA extraction using the QIAamp DNA Mini Kit (Qiagen, Germany) and measured DNA concentration using NanoVue (Biochom, UK). The extracted DNA sample was kept at 4 °C and thereafter used for mutation analysis as reported by [26]. Samples used for karyotype testes were heparinized peripheral blood and the Giemsa staining protocol was applied [15].
Case 1
In 2011, a first baby (46, XX) (Fig. 1) was born from a marriage between cousins. The baby had male-appearing external genitalia and untraceable testes. The abdominal ultrasound revealed the presence of a uterus and ovaries. Blood analysis shown high level of 17-OHP and normal levels of Na and K (Table 1). This baby girl had SV-CAH, due to the hetero compound mutations V281L and Q318X [11]. She was treated with hydrocortisone (20 mg/day).
Because the baby’s aunts had been previously diagnosed with classical CAH with ambiguous genitalia, her parents made the decision of eradicating the uterus and ovaries, and preserving the masculine appearance in the absence of gonads, regardless of the endocrinologists’ advice. This female was raised as a male but he is infertile, and the outcome of genital surgery was negative due to gender reassignment as a boy. She had not got menarche.
However, this infant has a sister who was born with SV-CAH and ambiguous genitalia, but who underwent reconstructive surgeries and was treated as a girl.
Case 2
The first child of 5 years old was born to an unrelated couple in 1998. Despite the presence of ambiguous genitalia (Tunner V), the abdominal echography revealed adrenal hypertrophy and a vagina. High levels of 17-OH and potassium were detected, in addition to low levels of sodium (Table 1). This baby girl (46, XX) (Fig. 2), had SW-CAH due to the inheritance of the homozygote mutation Q318X [11]. She was treated by hydrocortisone (30 mg/day) and fludrocortisone (0.1 mg/day). Only one reconstructive surgery was performed on her at the age of two, but the parents chose to treat her as a boy. Puberty had begun at age of 9 years, but it was disabled to increase the stature using hormonal therapy. Facial and pubic hirsutism appeared: she had a male look with beard and mustache, and she went to serve in the military. This case treatment had a negative outcome, and she had not got menarche due to hormonal therapy.
She had a sister with SW-CAH, who underwent reconstructive surgeries and was treated as a girl.
Case 3
A baby was born in 2017 to a couple of cousins, she was their third child. At birth, ambiguous genitalia were present (Fig. 3), karyotyping revealed 46, XX (Fig. 4), and echography detected a uterus and ovaries. She had SW-CAH due to the inheritance of two heterozygote mutations I2G and V281L, in addition to the homozygote mutation I172N [11]. Hyponatremia and hyperkalemia were detected (Table 1). Hydrocortisone (20 mg/day) and fludrocortisone (0.1 mg/day) were used as treatment, and the baby girl underwent several reconstructive surgeries to correct her external genitalia. This is a positive outcome as natal gender was preserved.
Case 4
A female was born in 2002 to a couple of cousins. Ambiguous genitalia were present at birth. Karyotyping revealed 46, XX (Fig. 5), echography detected a uterus and ovaries, and 17-OHP was elevated (Table 1). She had SW-CAH, but mutations were not explored. She was treated with hydrocortisone (10 mg/day) and fludrocortisone (0.1 mg/day), and underwent reconstructive surgery at the age of 18 months. At the age of 15 years, she reached puberty, and she was followed-up well by the endocrinologist. She got married in 2020 and had a baby. A positive outcome.
Case 5
A female was born in 1990 to a couple of cousins. She was their first child out of four children (three females and one male).
At the age of 4 years, she was diagnosed with SV-CAH owing to the appearance of hirsutism in the genital areas, slight enlargement in the clitoris, and the detection of high levels of 17-OHP (Table 1). She got menarche at 14 years old, but a menstrual disorder appeared later. She had compound heterozygous of I2G and R356W mutations [10]. She underwent treatment with hydrocortisone (20 mg/day) and was followed-up by an endocrinologist for the treatment of her menstrual disorder. She got married in 2014 and had twin daughters.
Discussion
One of the genetic diseases prevalent in Syria is CAH caused by a deficiency of the enzyme 21-OH. The most important factor affecting its heredity is consanguineous marriage [11]. A relatively high consanguinity rate of 30–39% is reported among the Syrian population [24].
The percentage of consanguineous marriage in CAH studies conducted in Iraq was 82% [2], 63% in Jordan [7], 40% in Lebanon [9], 65.5% in Egypt [13], 28.8% in Turkey [5], and 57.1% in Iran [14]. It is important to avoid this regional social habit that helps spread the disease.
The differences in health care provision and treatment regimens affect the quality of life for patients with CAH. Challenges allegedly vary according to sex, but all patients are subject to the emotional stress of living with a chronic disease, and many have weight and height disturbances and are at risk of infertility [22].
CAH Patients should be followed-up by a multidisciplinary team including a gynecologist, endocrinologist, pediatrician, and a psychologist [6].
Female patients (46, XX) with CAH are born with variable degrees of external genital ambiguity due to excess androgen during in utero development. Their internal reproductive anatomy includes a normal uterus, fallopian tubes, and ovaries with a potential for fertility. The ambiguous genitalia, and the often-related uncertainty regarding the gender assignment, can represent psychosocial trauma for the family, and carries a risk of social stigma for the patient [3].
The study we conducted to identify the eight most common mutations in patients with classical CAH showed that the rate of female genital ambiguity is high in classical CAH (27/38 CAH female) [11]. Upon reviewing the medical archives of a group of affected females with CAH, we noticed the role of the parents in making the decision to determine the gender of the newborn, and therefore the type of surgical procedure that is appropriate for the chosen gender. In the majority of cases, the chosen gender is compatible with the 46, XX karyotype.
In cases 1 and 2 in the present study, the masculine gender was selected by parents according to regional and cultural traditions of having a male that can be relied upon, despite the genetic and endocrinologist counseling. A similar unethical practice was also found in India [21], Pakistan [16], Algeria [20], and the Kingdom of Saudi Arabia [1]. The child has the right to develop according to their natal sex.
Reconstructive surgery, as in cases 3 and 4, could offer psychological relief, by resolving the sexual ambiguity of the genitalia, and may facilitate sexual intercourse, although it may enhance the feeling of being different [23]. Psychological support provides the CAH female patient and those around her with the best solution to adapt to this health condition, which she inherited from her parents. Having the female reproductive system that is proportional to the genetic pattern favors the idea of dealing with the newborn as a girl, and removes the first and main problem in the parents’ behavior, and encourages them to support her morally.
When the endocrine aspects of fertility are normalized, a normal pregnancy rate could result, as in cases 4 and 5. Suppression of testosterone hyper secretion, which induces anovulation, is relatively simple to achieve. The consequence of genital surgery is a key factor for the fertility outcome as vaginal function and sexual activity are closely related [27]. Recently, it was found that the fertility rate increases by 90% in women with classical CAH when they follow the stages of integrated treatment for CAH [17].
Conclusion
The integrated treatment of females with classical CAH, which includes psychological support in addition to the use of appropriate hormones, appropriate surgical procedures to correct the external genitalia of an ambiguous appearance into a female appearance in the presence of a female karyotype, and the corresponding reproductive system, gives these females the opportunity to live as they are and perhaps as mothers in the future. Patients with CAH should be followed by a team including a gynecologist, endocrinologist, pediatrician, and a psychologist.
Availability of data and materials
All the information about patients is in their medical records with the clinicians participating in this article.
Abbreviations
- CAH:
-
Congenital adrenal hyperplasia
- C:
-
Classical
- NC:
-
Non-classical
- SW:
-
Salt wasting
- SV:
-
Simple virilizing
- 17-OHP:
-
17-hydroxy progesterone
References
Al-Jurayyan NA. Ambiguous genitalia: two decades of experience. Ann Saudi Med. 2011;31(3):284–8. https://doi.org/10.4103/0256-4947.81544.
Al-Obaidi RG, Al-Musawi BM, Al-Zubaidi MA, Oberkanins C, Németh S, Al-Obaidi YG. Molecular analysis of CYP21A2 gene mutations among Iraqi patients with congenital adrenal hyperplasia. Enzyme Res. 2016;2016:9040616. https://doi.org/10.1155/2016/9040616.
Almasri J, Zaiem F, Rodriguez-Gutierrez R, Tamhane SU, Iqbal AM, Prokop LJ, Speiser PW, Baskin LS, Bancos I, Murad MH. Genital reconstructive surgery in females with congenital adrenal hyperplasia: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2018;103(11):4089–96. https://doi.org/10.1210/jc.2018-01863.
Auchus RJ, Witchel SF, Leight KR, Aisenberg J, Azziz R, Bachega TA, Baker LA, Baratz AB, Baskin LS, Berenbaum SA, Breault DT, Cerame BI, Conway GS, Eugster EA, Fracassa S, Gearhart JP, Geffner ME, Harris KB, Hurwitz RS, Katz AL, et al. Guidelines for the development of comprehensive care centers for congenital adrenal hyperplasia: guidance from the CARES foundation initiative. Int J Pediatr Endocrinol. 2010;2010: 275213. https://doi.org/10.1155/2010/275213.
Baş F, Kayserili H, Darendeliler F, Uyguner O, Günöz H, YükselApak M, Atalar F, Bundak R, Wilson RC, New MI, Wollnik B, Saka N. CYP21A2 gene mutations in congenital adrenal hyperplasia: genotype-phenotype correlation in Turkish children. J Clin Res Pediatr Endocrinol. 2009;1(3):116–28. https://doi.org/10.4008/jcrpe.v1i3.49.
Chatziaggelou A, Sakkas EG, Votino R, Papagianni M, Mastorakos G. Assisted reproduction in congenital adrenal hyperplasia. Front Endocrinol. 2019;10:723. https://doi.org/10.3389/fendo.2019.00723.
Daggag H, Batayneh A, Al-Khawaja N, Fathallah R, Al-Masri M, Abu-Khashabeh R, El-Khateeb M, Ajlouni K. Prevalence of congenital adrenal hyperplasia (CAH) due to 21-hydroxylase deficiency, in a Jordanian sample pool. Amman: National Center for Diabetes, Endocrinology and Genetics; 2011. p. 2–739. https://doi.org/10.1210/endo-meetings.2011.PART3.P14.
de Jesus LE, Costa EC, Dekermacher S. Gender dysphoria and XX congenital adrenal hyperplasia: how frequent is it? Is male-sex rearing a good idea? J Pediatr Surg. 2019;54(11):2421–7. https://doi.org/10.1016/j.jpedsurg.2019.01.062.
Delague V, Souraty N, Khallouf E, Tardy V, Chouery E, Halaby G, Loiselet J, Morel Y, Mégarbané A. Mutational analysis in Lebanese patients with congenital adrenal hyperplasia due to a deficit in 21-hydroxylase. Horm Res. 2000;53(2):77–82. https://doi.org/10.1159/000023518.
Dehneh N, Jarjour R, Al Fahoum S. Frequency of the point mutation R356W in a group of Syrian patients with congenital adrenocortical hyperplasia due to 21-hydroxylase deficiency. J Med Sci Damascus Univ. 2021. http://journal.damascusuniversity.edu.sy/index.php/heaj/article/view/1392.
Dehneh N. Phenotype and genotype of 21-hydroxylase deficiency in patients with congenital adrenal hyperplasia in Syria. Doctorate thesis. Department of Biochemistry and Microbiology, Faculty of pharmacy, Damascus University, Damascus; 2022. p. 150.
Dumic KK, Grubic Z, Yuen T, Wilson RC, Kusec V, Barisic I, Stingl K, Sansovic I, Skrabic V, Dumic M, New MI. Molecular genetic analysis in 93 patients and 193 family members with classical congenital adrenal hyperplasia due to 21-hydroxylase deficiency in Croatia. J Steroid Biochem Mol Biol. 2017;165(Pt A):51–6. https://doi.org/10.1016/j.jsbmb.2016.03.035.
Elmougy F, Elsharkawy M, Hafez M, Atty SA, Baz H, Ibrahim A, Soliman H, Ekladious S, Abdullatif M, Thabet G, Rady N, Afif A, Tolba A, Zaki Z, Musa N. Genetic profiling of CAH Egyptian children: rapid guide to clinical interpretation of common mutations. J Endocrinol Invest. 2021;44(1):83–93. https://doi.org/10.1007/s40618-020-01271-z.
Forouzanfar K, Seifi M, Hashemi-Gorji F, Karimi N, Estiar MA, Karimoei M, Sakhinia E, Karimipour M, Ghergherehchi R. Mutation analysis of the CYP21A2 gene in congenital adrenal hyperplasia. Cell Mol Biol. 2015;61(4):51–5.
Gustashaw KM. Chromosome stains. In: Barch MJ, editor. The ACT cytogenetics laboratory manual. 2nd ed. New York: The Association of Cytogenetic Technologists, Raven Press; 1991.
Khan AH, Nasir MI, Moatter T. Characterization of pathogenic mutations in 21-hydroxylase gene of Pakistani patients with congenital adrenal hyperplasia and their family members—a preliminary report. J Pak Med Assoc. 2002;52(7):287–91.
Kocova M, Anastasovska V, Bitovska I. The impact of CYP21A2 (P30L/I172N) genotype on female fertility in one family. Eur J Med Res. 2019;24(1):21. https://doi.org/10.1186/s40001-019-0379-4.
Krishnan GD, Yahaya N. Case report of an adult female with neglected congenital adrenal hyperplasia (CAH). J ASEAN Fed Endocr Soc. 2018;33(2):199–201. https://doi.org/10.15605/jafes.033.02.14.
Krone N, Dhir V, Ivison HE, Arlt W. Congenital adrenal hyperplasia and P450 oxidoreductase deficiency. Clin Endocrinol. 2007;66(2):162–72. https://doi.org/10.1111/j.1365-2265.2006.02740.x.
Ladjouze A, Yala I, Yahiaoui M, Zerguini D, Tardy V, Mohammedi K, et al. Age at diagnosis and outcome in Maghreb patients with 21-hydroxylase deficient congenital adrenal hyperplasia. ESPE Abstracts. 89:P-P3-005. Horm Res Paediatr. 2018;82(Suppl 1).
Marumudi E, Sharma A, Kulshreshtha B, Khadgawat R, Khurana ML, Ammini AC. Molecular genetic analysis of CYP21A2 gene in patients with congenital adrenal hyperplasia. Indian J Endocrinol Metab. 2012;16(3):384–8. https://doi.org/10.4103/2230-8210.95679.
Merke DP, Auchus RJ. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. N Engl J Med. 2020;383(13):1248–61. https://doi.org/10.1056/NEJMra1909786.
Meyer-Bahlburg H, Khuri J, Reyes-Portillo J, Ehrhardt AA, New MI. Stigma associated with classical congenital adrenal hyperplasia in women’s sexual lives. Arch Sex Behav. 2018;47(4):943–51. https://doi.org/10.1007/s10508-017-1003-8.
Othman H, Saadat M. Prevalence of consanguineous marriages in Syria. J Biosoc Sci. 2009;41(5):685–92. https://doi.org/10.1017/S0021932009003411.
Prasad R, Khajuria R, Bhansali A. Biochemistry, molecular biology and molecular genetics of congenital adrenal hyperplasia. In: Prasad R, editor. Biochemistry, molecular biology and molecular genetics of genetic disorders. Trivandrum: Transworld Research Network; 2013. p. 83–105. ISBN: 978-81-7895-609-1.
Ramazani A, Kahrizi K, Razaghiazar M, Mahdieh N, Koppens P. The frequency of eight common point mutations in CYP21 gene in Iranian patients with congenital adrenal hyperplasia. Iran Biomed J. 2008;12(1):49–53.
Reisch N. Review of health problems in adult patients with classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Exp Clin Endocrinol Diabetes. 2019;127(2–03):171–7. https://doi.org/10.1055/a-0820-2085.
Sheikh Alshabab LI, AlebrahIm A, Kaddoura A, Al-Fahoum S. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency: a five-year retrospective study in the children’s hospital of Damascus, Syria. Qatar Med J. 2015;2015(1):11. https://doi.org/10.5339/qmj.2015.11.
Acknowledgements
The authors would like to thank the Atomic Energy Commission of Syria (AECS) for their Genetics laboratory with modern equipment and their cooperation throughout the period of study. Great thanks to Miss Laïla Haddad for participation in manuscript rectification.
Funding
This study was not supported by any institute and all of the authors declare no conflict of interest and financial involvement.
Author information
Authors and Affiliations
Contributions
ND conducted all molecular experiments, clinical data acquisition, and clinical data interpretation. RJ and SA were responsible for overall practical and theoretical aspects of the study. Clinicians SI and AA followed the patients mentioned in this article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent form was signed by the patient or their guardian. This study was approved by Damascus University research ethics committee (HRECPHARMDU Resolution No. 2).
Consent for publication
Written informed consent was obtained from the patients or their guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
There is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dehneh, N., Jarjour, R., Idelbi, S. et al. Syrian females with congenital adrenal hyperplasia: a case series. J Med Case Reports 16, 371 (2022). https://doi.org/10.1186/s13256-022-03609-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-022-03609-y