Abstract
Background
Polyarteritis nodosa is a small vessel to medium vessel vasculitis that frequently presents with multi-organ involvement, but can sometimes be limited to single organs such as the testes. Patients often require treatment with glucocorticoids, plus or minus additional immunosuppressive therapy depending on the severity of the disease. We describe a rare case of polyarteritis nodosa involving the right testis and urinary bladder without other systemic features of vasculitis.
Case presentation
A previously healthy 54-year-old First Nations Canadian man presented with intermittent gross hematuria. He underwent surgical excision of his right testis for cryptorchidism and a transurethral resection of a bladder mass. Histology showed an active medium vessel vasculitis in both organs. On extensive clinical, laboratory, and radiographic review, he had no systemic features of vasculitis. On 2-year follow-up, he has not required any systemic therapy and has not developed further symptoms.
Conclusion
Single organ polyarteritis nodosa can sometimes be managed with surgical excision of the involved organ alone. Although our patient had two organs involved, we extrapolated the results of our literature search to guide his care. This case highlights the potential for surgical excision to cure polyarteritis nodosa despite the involvement of two organs in the absence of symptoms and signs of systemic vasculitis.
Similar content being viewed by others
Introduction
Polyarteritis nodosa (PAN) is a vasculitis characterized by necrotizing inflammation of medium and small arteries. It can affect many organ systems; most often, it affects the peripheral nerves, skin, gastrointestinal system, muscles, and kidneys. The disease often presents with multi-organ involvement, but cases of isolated organ involvement have been described [1, 2]. A detailed history and physical examination are required to identify features consistent with PAN, such as constitutional symptoms, skin lesions, abdominal pain, and peripheral neuropathy. Once PAN is suspected, a biopsy is usually required to confirm the diagnosis. If a biopsy is not possible, angiography is a reasonable alternative [1]. Treatment is based on the severity of illness and involved organs.
In general, cases of mild PAN can be treated with glucocorticoids alone. More severe cases necessitate the addition of immunosuppressive agents, such as cyclophosphamide. Isolated or single organ PAN can be managed by excision of the organ involved (for example, testis) and serial follow-up to ensure that systemic features do not develop [1, 2].
Our case report explores a rare case of PAN affecting both the testis and urinary bladder.
Case presentation
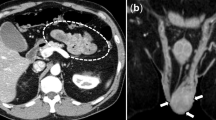
A previously healthy 54-year-old First Nations Canadian man presented with a several-month history of urinary retention and intermittent gross hematuria. In the course of his initial evaluation, he was found to have an enlarged prostate and was started on tamsulosin with improvement in his urinary symptoms. He noted the absence of his testicle on the right side for at least 30 years, consistent with cryptorchidism. He subsequently underwent cystoscopy, which demonstrated a superficial-appearing mass at the dome of his bladder. A radical right orchiectomy and transurethral resection of the bladder tumor (TURBT) were performed. Surprisingly, a pathologic examination revealed the presence of small and medium vessel vasculitis in both the urinary bladder and undescended testis (Fig. 1). There was no evidence of malignancy. He was referred to rheumatology for further evaluation.
An extensive review revealed no evidence of systemic vasculitis. He had no features of another underlying rheumatologic disorder. His investigations including basic blood work, C-reactive protein (CRP)/erythrocyte sedimentation rate (ESR), and antineutrophil cytoplasmic antibody (ANCA) were normal. Although antinuclear antibody (ANA) was positive (1:320), double-stranded deoxyribonucleic acid (DNA) (dsDNA) and extractable nuclear antigen (ENA) were negative and complements were normal. Rheumatoid factor (RF) was positive at 43 kU/L (reference range < 12 kU/L), but anti-cyclic citrullinated peptides (CCP) antibody was negative and our patient had no features of an inflammatory arthritis. Hepatitis B and C serologies were negative. A diagnosis of PAN was made. His testicular involvement and findings of active small and medium vessel vasculitis on urinary bladder and testis pathology were most consistent with this diagnosis. Given the lack of clinically apparent systemic vasculitis, no immunosuppressive therapy was initiated. Following his radical orchiectomy and TURBT, he had ongoing intermittent hematuria that was investigated with several repeat cystoscopies. An area of erythema was identified on one occasion. A repeat biopsy of the site demonstrated reactive changes and no evidence of vasculitis. A computed tomography (CT) angiogram was done of his abdomen and pelvis to evaluate the possibility of occult vessel involvement elsewhere, and was negative other than wall thickening and fat stranding noted at the anterior bladder. His symptoms have completely resolved following surgery and he has remained asymptomatic over the last 2 years.
Discussion
To the best of our knowledge, this is the first case reported in the literature of PAN affecting both the bladder and testis in the absence of systemic involvement. Moreover, this is also the first case of PAN reported in the setting of cryptorchidism. We performed a literature search to find reports of patients with isolated testicular or bladder vasculitis and found 45 such cases (Table 1). The average age of presentation was 39 years (median, 36 years). Of the 45 cases, 39 had isolated testicular vasculitis and 6 had isolated bladder vasculitis. Most cases (34/45) had biopsies that were pathologically consistent with PAN.
For the patients with isolated testicular vasculitis in whom treatment information was available, most (21/32) were treated with surgical excision alone with no reported cases of emergent systemic disease over a mean follow-up of 29 months (median, 24 months). Of the 11 patients who were treated with surgical excision as well as glucocorticoids +/− additional immunosuppressive therapy, 8/11 had evidence of more systemic illness at disease onset (for example, elevated CRP/ESR or constitutional symptoms) (Fig. 2). It is unclear what prompted treatment in the other three cases. Three patients were treated with glucocorticoids alone. Eight patients were treated with glucocorticoids in conjunction with at least one other immunosuppressive therapy [19,20,21,22,23]. Of those eight, four were treated with steroids and cyclophosphamide and the other four were treated with steroids in conjunction with cyclophosphamide and methotrexate, mycophenolate mofetil, methotrexate alone, or azathioprine and rituximab.
Of the 11 patients with isolated testicular vasculitis who received systemic therapy, three went on to develop systemic vasculitis [19] and one patient had persistent episodes of mild cutaneous vasculitis [21]. All four patients had evidence of more systemic disease on initial presentation.
Six patients who had isolated bladder vasculitis were included in our literature review. Four of the patients had evidence of more systemic illness at disease onset. The patients who did not have any systemic features underwent either a TURBT as well as therapy with prednisone and azathioprine, or treatment with steroids and cyclophosphamide without surgical excision [24, 28]. Of the other four patients, one underwent TURBT alone [27], two underwent TURBT as well as systemic therapy [24, 26], and one received prednisolone alone [25]. All six patients had no evidence of emergent systemic vasculitis over a mean follow-up of 17.2 months (median, 10.5 months).
It appears from the result of our literature review that patients who present with isolated testicular vasculitis and no evidence to suggest more systemic disease do not go on to develop systemic vasculitis after orchiectomy, regardless of whether or not they receive concomitant immunosuppressive therapy. Therefore, orchiectomy alone in isolated testicular vasculitis seems to be a reasonable therapeutic approach. There were only six patients with isolated bladder vasculitis, and one of them underwent TURBT alone with no emergent systemic illness. We used these findings to guide our management of a patient with PAN affecting both the right testis and urinary bladder.
Conclusion
This case summarizes the current literature regarding the treatment of isolated testicular or bladder vasculitis. Our findings support withholding immunosuppressive therapy after surgical excision in these patients if there is no evidence of more systemic disease at onset. While single organ PAN has been treated in the past with surgical excision, there is a lack of data regarding treatment of PAN involving two organs, with no other systemic features. We extrapolated the results of our literature review to guide the management of a patient who presented with PAN affecting both the urinary bladder and right testis. He underwent radical right orchiectomy and TURBT, with no systemic therapy. On 2-year follow-up, he has not developed any systemic PAN symptoms. The risk of developing future extratesticular and extravesicular involvement appears to be low.
Availability of data and materials
Not applicable.
References
Pipitone N, Salvarani C. Polyarteritis Nodosa. In: Dammacco F, Ribatti D, Vacca A, editors. Systemic Vasculitides: Current Status and Perspectives. Cham: Springer International Publishing; 2016. p. 189–96.
Hernández-Rodríguez J, Hoffman GS. Updating single-organ vasculitis. Curr Opin Rheumatol. 2012;24(1):38–45.
Persellin ST, Menke DM. Isolated polyarteritis nodosa of the male reproductive system. J Rheumatol. 1992;19(6):985–8.
Halim A, Neild GH, Levine T, Shaw PJ. Isolated necrotizing granulomatous vasculitis of the epididymis and spermatic cords. World J Urol. 1994;12(6):357–8.
Mukamel E, Abarbanel J, Savion M, Konichezky M, Yachia D, Auslaender L. Testicular mass as a presenting symptom of isolated polyarteritis nodosa. Am J Clin Pathol. 1995;103(2):215–7.
Kessel A, Toubi E, Golan TD, Toubi A, Mogilner JG, Jaffe M. Isolated epididymal vasculitis. Isr Med Assoc J. 2001;3(1):65–6.
Hashiguchi Y, Matsuo Y, Torii Y, Kajiwara T, Kayajima T, Irie K, et al. Polyarteritis nodosa of the epididymis. Abdom Imaging. 2001;26(1):102–4.
Eilber KS, Freedland SJ, Rajfer J. Polyarteritis nodosa presenting as hematuria and a testicular mass. J Urol. 2001;166(2):624.
Fraenkel-Rubin M, Ergas D, Sthoeger ZM. Limited polyarteritis nodosa of the male and female reproductive systems: diagnostic and therapeutic approach. Ann Rheum Dis. 2002;61(4):362–4.
Dotan ZA, Laufer M, Heldenberg E, Langevitz P, Fridman E, Duvdevani M, et al. Isolated testicular polyarteritis nodosa mimicking testicular neoplasm-long-term follow-up. Urology. 2003;62(2):352.
Tanuma Y, Oda T, Yokoo A, Ito S, Takeuchi K. Recurrent polyarteritis nodosa limited to the testis. J Urol. 2003;170(5):1953.
Fleischmann A, Studer UE. Isolated polyarteritis nodosa of the male reproductive system associated with a germ cell tumor of the testis: a case report. Cardiovasc Pathol. 2007;16(6):354–6.
Giannarini G, Pomara G, Moro U, Mogorovich A, Fabris FM, Morelli G, et al. Isolated polyarteritis nodosa of the genitourinary tract presenting with severe erectile dysfunction: a case report with long-term follow-up. J Sex Med. 2009;6(4):1189–93.
Atis G, Memis OF, Güngör HS, Arikan O, Saglican Y, Caskurlu T. Testicular polyarteritis nodosa mimicking testicular neoplasm. ScientificWorldJournal. 2010;10:1915–8.
Saito K, Washino S, Hirai M, Matuzaki A, Nokubi M, Terai C, et al. A case of isolated polyarteritis nodosa appeared in bilateral epididymides with asynchronous onset. Nihon Hinyokika Gakkai Zasshi Jpn J Urol. 2013;104(1):22–5.
Lintern N, Johnson NR, Mckenzie I, Martin B. Testicular Vasculitis - Literature Review and Case Report in Queensland. Curr Urol. 2013;7(2):107–9.
Garg K, Dawson L. Single organ variant of polyarteritis nodosa in epididymis. J Cancer Res Ther. 2015;11(3):662.
Dixit A, Hague C, Bicknell S. Testicular Vasculitis: A Sonographic and Pathologic Diagnosis. Case Rep Radiol. 2017;2017:1–4.
Brimo F, Lachapelle J, Epstein JI. Testicular vasculitis: a series of 19 cases. Urology. 2011;77(5):1043–8.
Pastor-Navarro H, Broseta-Viana L, Donate-Moreno MJ, Pastor-Guzmán JM, Lorenzo-Romero JG, Segura-Martín M, et al. Isolated testicular polyarteritis nodosa. Urology. 2007;70(1):178.e7–8.
Breuer GS, Reinus K, Nesher G, Munter G. Recurrent Unilateral Orchitis as a Presenting Symptom of Polyarteritis Nodosa. Isr Med Assoc J. 2015;17(9):585–6.
Bhatia S, Herrera Hernandez LP, Kamboj AK, Rieck KM. Isolated Polyarteritis Nodosa Presenting as Bilateral Testicular Swelling. Am J Med. 2018;131(2):e55–6.
Islam N, Sinha D, Ghosh P, Datta C, Chatterjee U. Orchitis: An unusual presentation of polyarteritis nodosa. Indian J Pathol Microbiol. 2018;61(4):600.
Fischer AH, Wallace VL, Keane TE, Clarke HS. Two cases of vasculitis of the urinary bladder: diagnostic and pathogenetic considerations. Arch Pathol Lab Med. 1998;122(10):903–6.
Katz DJ, Sengupta S, Snow RM. Isolated vasculitis of the bladder. Urology. 2005;65(4):797.
Becker A, Astroza G, Quezada N, Riaño C, Urrutia J, Guzman S. Isolated manifestation of necrotizing vasculitis of the bladder: a case report. Urol. 2008;47(10):1347–9.
Kassir R, Mouracade P, Barabino G, Peoc’h M, Cuilleron M, Gigante M. Vasculitis of the bladder: An extremely rare case report. Int J Surg Case Rep. 2013;4(9):782–4.
Fall M, Höper L, Kåbjörn-Gustafsson C, Trysberg E. Isolated vasculitis of the urinary bladder: a note on diagnosis and prognosis. Scand J Urol. 2018;8:1–2.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MS and GM made substantial contributions to the literature review and compilation of data from previously published case reports, as well as writing the manuscript. MAS provided the histologic analysis and interpretation, the histology figures, and revised the manuscript. ND performed the initial assessment and ongoing management of the patient, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The patient involved in the case report gave consent to participate prior to inclusion in the manuscript. As per the University of British Columbia Clinical Research Ethics Board guidelines, individual case reports do not require ethics review. More information is available at https://ethics.research.ubc.ca/ore/ubc-clinical-research-ethics-general-guidance-notes section 4.4.2.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Stewart, M., Marcotte, G., Seidman, M.A. et al. Polyarteritis nodosa isolated to the testis and urinary bladder in the setting of cryptorchidism: a case report and literature review. J Med Case Reports 13, 236 (2019). https://doi.org/10.1186/s13256-019-2172-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-019-2172-y