Abstract
Background
In patients treated for head and neck cancer, imaging studies are usually obtained within 3–6 months after treatment for assessment of treatment response. After 6 months, most guidelines advocate clinical follow-up, with imaging reserved for patients with clinically suspect or equivocal findings. However, some guidelines do recommend systematic imaging surveillance, and many clinicians tend to include some type of imaging in their follow-up schemes.
Objectives
This systematic review focuses on the usefulness of routine (systematic) post-treatment imaging surveillance of head and neck cancer beyond the first 3–6-month baseline imaging study.
Methods
A systematic literature search was conducted using PubMed and Google Scholar. Additional studies were identified by reviewing reference lists. Only original studies and review papers were considered. Results obtained with systematic post-treatment surveillance imaging were compared to symptom-directed imaging and/or clinical finding-directed imaging.
Results
Five hundred twenty-one records were identified through the database search, and 44 additional records were identified through other sources. Forty-eight articles were selected for the final review.
Analysis of these records showed that almost half of cases of locoregional recurrences and/or metastases were only detected by imaging (40.9%), and the mean time of detection of recurrent or metastatic disease (11.5 months) was well beyond the period of the first post-treatment scan. Most authors reported superior results with PET-CT when compared to other imaging techniques.
Conclusion
Strong arguments were found in favor of systematic imaging surveillance in locoregional advanced head and neck cancer during at least one and preferably 2 years after treatment.
Critical relevance statement
Analysis of the selected records showed that almost half of cases of locoregional recurrences and/or metastases were only detected by imaging. This systematic review suggests that imaging may currently be underused in the post-treatment surveillance of patients with head and neck cancer.
Key points
• This systematic review focuses on the usefulness of long-term systematic imaging surveillance in patients treated for head and neck cancer.
• Analysis of 521 articles revealed that systematic imaging allowed the initial detection of locoregional recurrences and/or metastases in more than 40% of patients.
• Imaging may currently be underused in the post-treatment surveillance of patients with advanced head and neck cancer.
Graphical Abstract

Similar content being viewed by others
Introduction
Worldwide head and neck cancer accounts for approximately 900,000 cases and over 400,000 deaths annually [1]. Most malignant tumors are head and neck squamous cell carcinomas (HNSCC). Treatment options include surgery, radiation therapy, and chemotherapy, or a combination of these modalities.
Approximately 50% of patients with locally advanced head and neck cancer will develop a recurrence [2, 3]. Distant metastases are present in about 10% of cases at the time of diagnosis, with an additional 20–30% developing during the course of the disease [4]. Up to 80–85% of metastases from HNSCC are observed in the lungs. Bone metastases account for 15–39%, while the liver is a affected in 10–30% of cases.
Patients treated for primary HNSCC also have a high rate (3 to 5% per year) of developing second primary tumors [5, 6].
After treatment, there are two principal periods of surveillance: immediate posttreatment (within 6 months) and long-term (6 months onward).
There is now a consensus that, for patients with locoregionally advanced disease (e.g., T3-T4 primary or N1 + nodal staging), imaging should be performed within 3 months to 6 months after completion of definitive treatment in order to assess treatment response [7,8,9].
On the other hand, the utility of long-term imaging surveillance is subject of debate. Currently, controlled prospective data demonstrating a survival benefit for any follow-up strategy in this specific context do not exist. While some guidelines recommend systematic imaging, others state that additional post-treatment imaging should be reserved for patients with worrisome or equivocal signs and/or symptoms [8,9,10,11,12,13,14,15,16,17]. The National Comprehensive Cancer Network (NCCN), for instance, does not recommend routine imaging for surveillance in asymptomatic patients, except for specific patient populations. These include patients with primary nasopharyngeal carcinoma, a history of smoking, or a primary tumor in areas inaccessible by clinical examination [8].
Surveys of practicing physicians have shown that many clinicians do not follow the NCCN guidelines and believe systematic imaging may be appropriate in at least some of their patients, despite lack of symptoms [18,19,20]. In other words, current guidelines are inconsistent and contradictory, and clinicians tend to develop their own strategy, based on personal and institutional preference.
This systematic review exclusively focuses on the usefulness of routine post-treatment imaging of head and neck cancer beyond the first 3–6-month baseline imaging study. Hereby, the strategy of systematic follow-up imaging is compared to symptom-directed imaging and/or clinical finding-directed imaging. This is an important issue because both overuse and underuse of imaging bears significant risk and disadvantages. Overuse of imaging may cause patient stress, unnecessary expenses [21] and iatrogenic side effects (e.g., related to radiation in CT or PET/CT). Underuse of imaging, on the other hand, may lead to missed opportunities for early detection of recurrences and salvage treatment.
In this study, we review the retrospective data and observational studies that are available. Possible outcomes studied are the detection of locoregional recurrence or metastases, change of therapeutic regimen, and survival. The focus is on squamous cell carcinoma of the pharynx, oral cavity, and larynx. Both qualitative and quantitative results are obtained, and the collected data are used to provide practical recommendations.
Methods
Study protocol and registration
Methods of the analysis and inclusion criteria were specified in advance and documented in a protocol accordingly to the PRISMA guidelines [22, 23].
Eligibility criteria
Study eligibility criteria are given below according to the PICOS framework (populations, interventions, comparators, outcomes, and study designs of interest) as well as other study-specific elements.
-
(1)
Types of participants/populations (P): patients who underwent treatment for head and neck cancer, with curative intent. Further inclusion criteria:
-
Squamous cell carcinoma
-
Primary tumor in nasopharynx, oropharynx, hypopharynx, larynx, or oral cavity
-
Patients treated with surgery, radiotherapy, and/or systemic therapy
-
Patients with or without risk factors (smoking etc.)
-
-
(2)
Types of intervention (I): systematic (planned) post-treatment surveillance imaging studies.
-
This review does not cover the first post-treatment scan, typically performed after 3–6 months
-
Included are studies on post-treatment imaging surveillance after the first post-treatment scan
-
Techniques: computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET), PET-CT, ultrasonography (US)
-
Body locations studied: neck, chest, and/or full body
-
Search for local recurrence, regional recurrence (e.g., lymph nodes in the neck), distant metastases
-
-
(3)
Types of comparators (C): other methods used for detection of locoregional recurrence or metastases.
-
Clinical exam
-
Patient anamnesis (symptoms)
-
Imaging studies requested based on suspect clinical exam of patient symptoms (in contrast to systematic—planned—imaging surveillance)
-
Endoscopic studies
-
Other types of imaging studies (e.g., PET-CT versus CT)
-
Any other test
-
-
(4)
Types of outcome measures (O):
-
Detection of local recurrence, regional recurrence (e.g., metastatic lymph nodes), distant metastases
-
Change in therapeutic regimen
-
Impact on survival
-
-
(5)
Types of studies (S):
-
Included: original studies, abstracts of conference papers (if containing sufficiently detailed information), doctoral dissertations
-
Excluded: letters, editorials, reviews, and case reports
-
Studies can be prospective or retrospective. Studies using mathematical models (e.g., Markov models) were also included
-
-
(6)
Other study-specific elements:
-
Reports published before 2000 were not considered during the initial search
-
Report language was restricted to English, French, and Dutch
-
Only published reports were considered
-
No restriction was put on the length of follow-up
-
Information sources
PubMed and Google Scholar were used for database search. The PubMed and Google Scholar search was done between August 1 and September 27, 2022. The search was developed and conducted by SVH.
Supplementary approaches to identify studies are as follows: first, the reference lists of all review articles obtained via the database search described above were checked, and additional records fulfilling the eligibility criteria were identified. Next, all articles citing the records found via the database search described above were identified via Google Scholar. Next, the reference list of the article “Posttreatment surveillance of squamous cell carcinoma of the head and neck” in the electronic database “UpToDate” was checked. Finally, the reference lists of the articles obtained via the last two steps were scrutinized.
Electronic database search strategy
The following searches were done:
-
PUBMED SEARCH: ((head and neck cancer[Title/Abstract]) AND (surveillance[Title/Abstract])) AND (imaging[Title/Abstract])
-
PUBMED SEARCH: ((head and neck cancer[Title/Abstract]) AND (surveillance[Title/Abstract])) AND (posttreatment[Title/Abstract])
-
References in NCCN guidelines
-
PUBMED SEARCH: ((head and neck cancer[Title/Abstract]) AND (follow-up[Title/Abstract])) AND (posttreatment[Title/Abstract])
-
PUBMED SEARCH: ((head and neck cancer[Title/Abstract]) AND (surveillance[Title/Abstract])) AND (tomography[Title/Abstract])
-
PUBMED SEARCH: (((cancer[Title/Abstract]) AND (surveillance[Title/Abstract])) AND (imaging[Title/Abstract])) AND (pharynx)
-
PUBMED SEARCH: (((cancer[Title/Abstract]) AND (surveillance[Title/Abstract])) AND (imaging[Title/Abstract])) AND (oral cavity[Title/Abstract])
-
PUBMED SEARCH: (((cancer[Title/Abstract]) AND (surveillance[Title/Abstract])) AND (imaging[Title/Abstract])) AND (larynx[Title/Abstract])
-
GOOGLE SCHOLAR SEARCH: “head and neck cancer posttreatment imaging surveillance”
-
GOOGLE SCHOLAR SEARCH: “head and neck cancer posttreatment imaging follow-up”
-
GOOGLE SCHOLAR SEARCH: “pharynx cancer imaging surveillance”
-
GOOGLE SCHOLAR SEARCH: “oral cavity cancer imaging surveillance”:
-
GOOGLE SCHOLAR SEARCH: “larynx cancer imaging follow-up surveillance”:
-
GOOGLE SCHOLAR SEARCH: “head and neck cancer tomography surveillance”:
-
GOOGLE SCHOLAR SEARCH: all articles citing the records found via the database search described above were identified via Google Scholar (“cited by”).
-
UPTODATE: the reference list of the article “Posttreatment surveillance of squamous cell carcinoma of the head and neck” [24] in the electronic database “UpToDate” was checked.
Study selection
Eligibility assessment was performed by one author (S.V.H.) and reviewed by a second author (R.H.). Records obviously not covering the topic of the review were excluded from further consideration. Disagreements between reviewers were resolved by consensus.
Records obtained from the PubMed and Google Scholar searches were compared, and duplicates were removed. Records obtained via the supplementary approaches to identify studies (see above) were only retained if the record was not yet available in the list of records obtained via database search (i.e., duplicates were removed on a record-by-record basis).
All records obtained via the database search and via the supplementary approaches were screened based on evaluation of title and abstract. Inclusion and exclusion criteria are described above in accordance with the PICOS framework.
The potentially eligible records not excluded during this step were promoted to the next stage of the review: full text screening (see Fig. 1). All articles selected for full text review were read by one author (S.V.H.). This work was reviewed by RH and discrepancies were resolved in consensus.
During all steps in the process, special attention was given to the removal of duplicate studies.
The details of each article (author, title, publication year) were recorded in an excel file. In the file, each article was assigned to one of the following categories, in accordance with the methodology described above:
-
Category 1: Record obtained via database search or via the supplementary approaches but excluded based on evaluation of title and abstract
-
Category 2: Records considered eligible based on review of title and abstract but excluded after full text review
-
Category 3: Records included after full text review
An overview of all articles, together with their category, is given in the electronic supplementary material (Manuscript selection sheet).
In addition to the reasons given above, reasons to exclude articles were as follows:
-
Missing details in the materials and methods or results section, making interpretation or data extraction difficult or impossible
-
Full text article not accessible
-
Different research topic than anticipated based on reading the title and abstract
-
No comparison between systematic (routine) surveillance imaging and another type of surveillance (presentation of results obtained with one method, without any comparison)
The records that were selected for qualitative review were divided in one or more of the following categories:
-
Results obtained in a group of patients with different types of head and neck cancer (different in terms of primary location)
-
Results obtained in a subgroup of patients with oropharyngeal cancer
-
Results obtained in a subgroup of patients with cancer of the oral cavity
-
Results obtained in a subgroup of patients with cancer of the hypopharynx/larynx
-
Results for comparison of imaging techniques
In addition, records referring to guidelines pertinent to post-treatment surveillance of head and neck tumors were identified.
Data collection process
We developed a data extraction sheet, pilot-tested it on ten randomly selected included studies, and used it accordingly (see Manuscript selection sheet). Data extraction was done by one author (S.V.H.) and reviewed by RH. Discrepancies were resolved in consensus.
Extracted data items
The following quantitative data were extracted if available:
-
Percentage of locoregional recurrences/metastases observed more than 6 months after treatment
-
Average time of detection of locoregional recurrences/metastases (months after the end of treatment)
-
Percentage of locoregional recurrences/metastases detected by surveillance imaging versus other methods
Presentation of results
For clarity, results are divided in 4 categories:
-
1.
Study selection (including PRISMA flowchart)
-
2.
Overview of existing guidelines
-
3.
Overview of included studies and qualitative results per category
-
4.
Quantitative results
Results
Study selection
The following results were obtained:
-
The PUBMED SEARCH: ((head and neck cancer[Title/Abstract]) AND (surveillance[Title/Abstract])) AND (imaging[Title/Abstract]) resulted in 133 hits. After exclusion of records obviously not covering the topic of the review, 91 records remained (Manuscript selection sheet, column B).
-
The PUBMED SEARCH: ((head and neck cancer[Title/Abstract]) AND (surveillance[Title/Abstract])) AND (posttreatment[Title/Abstract]) resulted in 101 hits. After exclusion of records obviously not covering the topic of the review and duplicates, 69 records remained (Manuscript selection sheet, column C).
-
References in NCCN guidelines: 6 records selected (Manuscript selection sheet, column D).
-
The PUBMED SEARCH: ((head and neck cancer[Title/Abstract]) AND (follow-up[Title/Abstract])) AND (posttreatment[Title/Abstract]) resulted in 244 hits. After exclusion of records obviously not covering the topic of the review and duplicates, 74 records remained (Manuscript selection sheet, column E).
-
The PUBMED SEARCH: ((head and neck cancer[Title/Abstract]) AND (surveillance[Title/Abstract])) AND (tomography[Title/Abstract]) resulted in 70 hits. After exclusion of records obviously not covering the topic of the review and duplicates, 50 records remained (Manuscript selection sheet, column F).
-
The PUBMED SEARCH: (((cancer[Title/Abstract]) AND (surveillance[Title/Abstract])) AND (imaging[Title/Abstract])) AND (pharynx) resulted in 10 hits. After exclusion of records obviously not covering the topic of the review and duplicates, 3 records remained (Manuscript selection sheet, column G).
-
The PUBMED SEARCH: (((cancer[Title/Abstract]) AND (surveillance[Title/Abstract])) AND (imaging[Title/Abstract])) AND (oral cavity[Title/Abstract]) resulted in 20 hits. After exclusion of records obviously not covering the topic of the review and duplicates, 8 records remained (Manuscript selection sheet, column H).
-
The PUBMED SEARCH: (((cancer[Title/Abstract]) AND (surveillance[Title/Abstract])) AND (imaging[Title/Abstract])) AND (larynx[Title/Abstract]) resulted in 8 hits. After exclusion of records obviously not covering the topic of the review and duplicates, 2 records remained (Manuscript selection sheet, column I).
-
The GOOGLE SCHOLAR SEARCH: “head and neck cancer posttreatment imaging surveillance”: resulted in 20,400 hits. The first 350 hits were checked. After exclusion of records obviously not covering the topic of the review and duplicates, 105 records remained (Manuscript selection sheet, column J, marked with “1”).
-
The GOOGLE SCHOLAR SEARCH: “head and neck cancer posttreatment imaging follow-up”: resulted in 23,800 hits. The first 100 hits were checked. After exclusion of records obviously not covering the topic of the review and duplicates, 4 records remained (Manuscript selection sheet, column J, marked with “2”).
-
The GOOGLE SCHOLAR SEARCH: “pharynx cancer imaging surveillance”: resulted in 15,000 hits. The first 100 hits were checked. After exclusion of records obviously not covering the topic of the review and duplicates, 8 records remained (Manuscript selection sheet, column J, marked with “3”).
-
The GOOGLE SCHOLAR SEARCH: “oral cavity cancer imaging surveillance”: resulted in 46,700 hits. The first 100 hits were checked. After exclusion of records obviously not covering the topic of the review and duplicates, 12 records remained (Manuscript selection sheet, column J, marked with “4”).
-
The GOOGLE SCHOLAR SEARCH: “larynx cancer imaging follow-up surveillance”: resulted in 25,300 hits. The first 100 hits were checked. After exclusion of records obviously not covering the topic of the review and duplicates, 16 records remained (Manuscript selection sheet, column J, marked with “5”).
-
The GOOGLE SCHOLAR SEARCH: “head and neck cancer tomography surveillance”: resulted in 66,900 hits. The first 100 hits were checked. After exclusion of records obviously not covering the topic of the review and duplicates, 7 records remained (Manuscript selection sheet, column J, marked with “6”).
-
The GOOGLE SCHOLAR SEARCH: “cited by”: for every article, a search through Google Scholar was conducted looking for (newer) articles that cite the initially found articles in their reference list (“cited by”). After exclusion of records obviously not covering the topic of the review and duplicates, 182 records remained (Manuscript selection sheet, column K).
-
UPTODATE: Also was checked if the database "UpToDate" contained additional information or references. Eight new records were found (Manuscript selection sheet, column L).
In total, 521 records were identified through database search. In addition, 44 additional records were identified through other sources.
In total, 565 records were screened on basis of title and abstract. From these, 432 records were excluded. Reasons for exclusion were as follows: letters, review papers, editorials, case reports, studies on tumor types other than squamous cell carcinoma, tumors in locations other than nasopharynx, oropharynx, hypopharynx, larynx, or oral cavity, articles focusing on the first post-treatment scan (typically performed after 3–6 months), articles focusing on diagnosis, staging or treatment, articles failing to provide a comparison between systematic imaging-based surveillance and surveillance directed by symptoms and/or clinical/endoscopic exam, articles with methodological errors or missing information, articles in languages other than English, French, or Dutch, and articles published before 2000.
Thus, 133 (565 minus 432) records were promoted to the next step in the review process: assessment of full-text articles (Manuscript selection sheet, column M, marked with “x”). From these 133 articles, 85 were excluded for one or more of the above given reasons. So, 48 articles were selected for the final review (Manuscript selection sheet, column N, marked with “x”).
The process is summarized in Fig. 1.
Overview of existing guidelines
An overview of existing international guidelines regarding surveillance imaging after the initial (3–6 months) post-treatment baseline imaging study are given in Table 1.
-
As shown in Table 1, nine different guidelines were found during full text search of the selected articles. All guidelines support the use of initial (3–6 months) post-treatment imaging. However, subsequent imaging recommendations for asymptomatic patients span the spectrum from no routine imaging to regular periodic imaging.
-
During our search, we found that many papers refer to the NCCN guidelines. In these guidelines, imaging after the first post-treatment scan is recommended only in locoregionally advanced disease and only if clinically indicated (symptomatic patient or suspect clinical finding). A possible exception to this general rule may be the post-treatment assessment of areas inaccessible to routine clinical examination (deep-seated anatomic locations or areas obscured by extensive treatment change). The NCCN guidelines also suggest that PET-CT may be the most sensitive imaging modality [8].
-
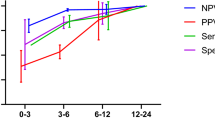
While several guidelines [10, 12, 15, 16] follow the general NCCN preference for non-systematic symptom-directed imaging and/or clinical finding-directed imaging, some propose a clearly different approach. AWMF, for instance, recommends CT scan of the head and neck region every 6 months in the first 2 years after treatment and every 12 months for the third to fifth years [11]. The most intensive recommendations come from NI-RADS, which advocates (at minimum) annual surveillance imaging with more frequent studies for concerning or equivocal findings [17]. The NI-RADS approach makes follow-up strategies dependent on initial imaging findings. NI-RADS provides a structured reporting template and suggests classifying imaging findings in one of four categories: NI-RADS 1 (no evidence of recurrence), NI-RADS 2 (low suspicion, defined as ill-defined non-mass-like areas(s) of soft tissue with only mild differential enhancement or mild fluorine-18–2-fluoro-2-deoxy-D-glucose (FDG) uptake), NI-RADS 3 (high suspicion), and NI-RADS 4 (definite recurrence).
Overview of included studies and summarized qualitative results per category
Tables 2, 3, 4, and Supplementary Tables 1 and 2 provide an overview of the studies that were selected for qualitative review in one of the following categories:
-
Head and neck cancer in general (Table 2)
-
Oropharyngeal cancer (Table 3)
-
Cancer of the oral cavity (Table 4)
-
Cancer of the hypopharynx/larynx (Supplementary Table 1)
-
Results for comparison of imaging techniques (Supplementary Table 2)
Summary of results for head and neck cancer in general (Table 2)
-
A large majority (18/25) of reports analyzed in this study suggest that systematic post-treatment surveillance imaging may be useful in terms of additional lesion detection when compared to a strategy where imaging is reserved for cases with suspect symptoms or clinical findings.
-
In 11/17 studies with positive results, PET-CT was (predominantly or exclusively) used as imaging modality (65%). The average publication year of the studies with positive results was 2015. In 1/4 studies with negative results, PET-CT was (predominantly or exclusively) used as imaging modality (25%). The average publication year of the studies with positive results was 2013. In other words, there is a tendency toward better results in recently published studies using PET-CT as imaging modality.
-
Most authors agree that imaging screening after 2 years is probably not effective. Several authors suggest performing surveillance imaging (mainly PET-CT) at 1 or 2 time points after the initial post-treatment scan. Suggested regimens are PET-CT exams at 12 months [41], 12 and 24 months [40], 9 months [33], 12 months [36], 12 months and 18–24 months [32], 18 months [42], 8 and 14 months [38], and 24 months [39].
-
Of particular interest is the report of McDermott et al. [38]. These authors showed that a single PET-CT with negative findings carries a NPV of 91%, which the authors consider insufficient to defer further radiologic surveillance. On the other hand, two consecutive PET-CT examinations with negative findings within a 6-month period, resulted in an NPV of 98%, which could obviate further radiologic imaging in the absence of clinical signs of recurrence.
Summary of results for oropharyngeal cancer (Table 3)
Only five reports focused exclusively on oropharyngeal cancer (OPC). The results for oropharyngeal cancer are more mixed than those for the larger group of head and neck cancers. Among other factors, this may be related to the fact that this group contains both HPV-positive (HPV +) and HPV-negative (HPV −) OPCs, which have a quite distinct clinical behavior and prognosis.
Summary of results for cancer of the oral cavity (Table 4)
-
As in the studies summarized in Table 2 (general group), most reports on oral cavity cancer Imaging surveillance (at least once) after 3–6 months appears to be beneficial in terms of lesion detection. Also, imaging surveillance after 2 years post-treatment appears to be less effective.
-
When a free or pedicled flap reconstruction is required, a certain degree of distortion of the anatomical configuration of the residual hemitongue and floor of mouth is often produced, and clinical detection of recurrence may be difficult. It is not surprising that, in such cases, data show superior results with systematic imaging surveillance.
Summary of results for cancer of the hypopharynx/larynx (Supplementary Table 1)
-
Only a limited number of studies is available for this body part. Submucosal recurrence appears to be an important issue, making imaging surveillance mandatory [61, 62].
Summary of results for comparison of imaging techniques (Supplementary Table 2)
-
In this category, PET-CT appears to be the preferred modality for imaging surveillance [63,64,65,66,67,68,69,70]. Depending on the specific case (e.g., location of recurrence), MRI may be useful for confirmation and additional staging.
Quantitative results
The quantitative results of the different studies are summarized in Table 5.
Summary of the quantitative results on recurrences (Table 5)
-
For all records together, in summary, 40.9% locoregional recurrences and/or metastases were detected by routing post-treatment surveillance imaging and not by symptoms or clinical/endoscopic exam. Moreover, 52% of locoregional recurrences and/or metastases are detected after 6 months post-treatment, and the average time of detection of recurrent or metastatic disease is 11.5 months.
-
Comparable results are obtained in the subcategories, except for oropharynx. For oropharynx, locoregional recurrences and/or metastases were detected by routine post-treatment surveillance imaging (and not by symptoms or clinical/endoscopic exam) in 60.7% versus 40.9% for the entire group. Moreover, the average time of detection of recurrent or metastatic disease was 15 months versus 11.5 months. In other words, imaging appears to be even more important in patients with treated oropharyngeal cancer (which may be related to the detection of asymptomatic distant metastases), and recurrences/metastases disease tend to occur later in time.
Discussion
Need for systematic imaging surveillance
Currently, there are no prospective randomized studies showing that systematic post-treatment surveillance imaging of patients with treated head and neck cancer is beneficial in terms of survival (with the exception of the first post-treatment study, see the “Introduction” section).
However, a large majority (18/25) of reports analyzed in this study suggest that systematic post-treatment surveillance imaging is useful in terms of additional lesion detection when compared to a strategy where imaging is reserved for cases with suspect symptoms or clinical findings. In 40.9% of cases, locoregional recurrences and/or metastases were detected by routine post-treatment surveillance imaging and not by symptoms or clinical/endoscopic exam. Thus, this systematic review provides strong arguments in favor of systematic post-treatment imaging surveillance beyond the first post-treatment scan.
This is not surprising for several reasons. First, in some anatomical locations (nasopharynx, subglottis, etc.), tumor detection and/or evaluation of submucosal spread may be difficult by clinical exam/direct inspection only. Second, tissue fibrosis, oedema, necrosis, and anatomic changes after radiotherapy and/or surgery can interfere with early detection of residual viable tumor or recurrence by the usual sequential physical and endoscopic examinations [71]. Third, a free or pedicled flap reconstruction may be required in patients with oral cavity cancer, often precluding the detection of submucosal relapse [54].
Duration of systematic imaging surveillance
Another debated topic is the optimal length of post-treatment surveillance. Our results show that, on average, 52% of locoregional recurrences and/or metastases were detected after 6 months post-treatment, and the mean time of detection of recurrent or metastatic disease was 11.5 months. These numbers give strong arguments in favor of routine imaging surveillance during at least 1 (and preferably 2) year post-treatment. As suggested by others, routine surveillance imaging beyond the first 24 months may be of limited value and may not be cost effective [8, 40].
The case of oropharyngeal cancer
The discussion about the usefulness of post-treatment surveillance in oropharyngeal cancer is complicated by the fact that HPV+ and HPV- OPCs can be considered as two different disease entities. The behavior of HPV+ poses an extra challenge for surveillance: on the one hand, HPV+ patients with OPC have better outcomes, a lower risk of recurrence and metastatic disease [72], and a longer overall survival, thus apparently making post-treatment surveillance less useful. On the other hand, recurrences in HPV+ OPC tend to occur later in time, and often correspond to distant metastases detected with whole body imaging only [48], thus providing theoretical arguments for prolonged screening with imaging. The peculiar behavior of oropharyngeal cancer was also observed in our study: in comparison with other head and neck cancers, oropharyngeal recurrences and/or metastases were detected later in time (15 months versus 11.5 months) and more exclusively by imaging (60.7%, versus 40.9% for the entire group).
Recently, promising results have been obtained with plasma circulating tumor HPV DNA for the surveillance of cancer recurrence in HPV+ oropharyngeal cancer [73, 74]. This type of tests could possibly be used for posttreatment surveillance in HPV+ patients, whereby the role of imaging could potentially be limited to confirmation of suspect cases.
Imaging techniques for surveillance
Concerning the choice of imaging technique for post-treatment surveillance, we found better results with PET-CT when compared to CT or MRI. Treatment with radiotherapy and surgery causes inflammation, scarring, and tissue distortion, which can hinder the interpretation of anatomic imaging techniques such as CT and MRI. The metabolic information provided by 18F-FDG PET-CT allows it to serve as an effective tool for detecting recurrence, regional lymphatic spread, and distant metastases [39]. However, PET scanning is quite costly and may lead to additional diagnostic evaluation to rule out false positive results. As an alternative to PET-CT and depending on institutional preference, contrast-enhanced CT or MRI can be used for locoregional surveillance and low-dose CT for detection of metastatic lung disease [8]. MRI may also be useful for confirmation in case equivocal findings are found with PET-CT or for optimal assessment of specific anatomical areas (e.g., nasopharynx) [75].
Overall conclusion
This systematic review focuses on the importance of systematic post-treatment imaging surveillance beyond the initial post-treatment scan in patients with head and neck cancer. While most current guidelines do not recommend post-treatment surveillance beyond the first post-treatment scan, we found strong arguments in favor of this approach.
Our data show that almost half of cases of locoregional recurrences and/or metastases were only detected by imaging (40.9%), and the mean time of detection of recurrent or metastatic disease (11.5 months) was well beyond the first post-treatment scan (3–6 months). As a result, we conclude that systematic imaging surveillance during at least 1 and possibly 2 years in the post-treatment period, with PET-CT being the preferred imaging modality, appears to be justified in cases of advanced head and neck cancer.
The further development of consensus guidelines regarding the surveillance of head and neck cancer by imaging methods would help to standardize the follow-up of these patients in the most effective way possible, with the goal of improving the eventual treatment outcome. This should ideally be done under the guidance of recognized organizations in the field.
Availability of data and materials
See Supplementary Table 3.
Abbreviations
- ACS:
-
American Cancer Society
- ASCO:
-
American Society of Clinical Oncology
- AWMF:
-
Association of Scientific Medical Societies in Germany
- HNSCC:
-
Head and neck squamous cell carcinomas
- HPV:
-
Human papilloma virus
- NCCN:
-
National Comprehensive Cancer Network
- NI-RADS:
-
Neck imaging reporting and data system
- NPV:
-
Negative predictive value
- OC:
-
Oral cavity
- OP:
-
Oropharynx
- OPC:
-
Oropharyngeal cancer
- RX:
-
Radiography
References
Stenson K, Brockstein B, Ross M (2023) Epidemiology and risk factors for head and neck cancer. In: UpToDate, Post TW (Ed), Wolters Kluwer (accessed on January 15, 2023)
Nissi L, Suilamo S, Kyto E, Vaittinen S, Irjala H, Minn H (2021) Recurrence of head and neck squamous cell carcinoma in relation to high-risk treatment volume. Clin Transl Radiat Oncol 27:139–146
Agarwal V, Branstetter B, Johnson J (2008) Indications for PET/CT in the head and neck. Otolaryngol Clin North Am 41:23–49
Pisani P, Airoldi M, Allais A et al (2020) Metastatic disease in head & neck oncology. Acta Otorhinolaryngol Ital 40:S1–S86
Leon X, Quer M, Diez S et al (1999) Second neoplasm in patients with head and neck cancer. Head Neck 21:204–210
Atienza JA, Dasanu CA (2012) Incidence of second primary malignancies in patients with treated head and neck cancer: a comprehensive review of literature. Curr Med Res Opin 28:1899–1909
Isles MG, McConkey C, Mehanna HM (2008) A systematic review and meta-analysis of the role of positron emission tomography in the follow up of head and neck squamous cell carcinoma following radiotherapy or chemoradiotherapy. Clin Otolaryngol 33:210–222
Pfister DG, Spencer S, Adelstein D et al (2022) Head and neck cancers, version 2.2022, NCCN clinical practice guidelines in oncology
You H, Subramaniam RM (2022) PET/computed tomography: post-therapy follow-up in head and neck cancer. PET Clin 17:319–326
EviCore 2.1 Clinical Guidelines. Oncology Imaging Policy 2020. https://www.evicore.com/-/media/files/evicore/clinical-guidelines/solution/cardiology-and-radiology/2020/evicore_oncology_final_v21_eff100120_pub100120.pdf
Wolff KD, Follmann M, Nast A (2012) The diagnosis and treatment of oral cavity cancer. Dtsch Arztebl Int 109:829–835
British Association of Head and Neck Oncologists (2001) Practice care guidance for clinicians participating in the management of head and neck cancer patients in the UK. Drawn up by a Consensus Group of Practising Clinicians. Eur J Surg Oncol 27:1–17
Koyfman S, Ismaila N, Crook D et al (2019) Management of the neck in squamous cell carcinoma of the oral cavity and oropharynx: ASCO clinical practice guideline. J Clin Oncol 37:1753–1774
Cohen E, LaMonte S, Erb N et al (2016) American Cancer Society Head and Neck Cancer Survivorship Care Guideline. CA Cancer J Clin 66:203–239
https://www.esmo.org/guidelines/guidelines-by-topic/head-and-neck-cancers
Roman BR, Goldenberg D, Givi B (2016) AHNS series: do you know your guidelines? Guideline recommended follow-up and surveillance of head and neck cancer survivors. Head Neck 38:168–174
Aiken A, Rath T, Anzai Y et al (2018) ACR Neck Imaging Reporting and Data Systems (NI-RADS): a white paper of the ACR NI-RADS committee. J Am Coll Radiol 15:1097–1108
Gill A, Vasan N, Givi B, Joshi A (2018) AHNS Series: Do you know your guidelines? Evidence-based management of oral cavity cancers. Head Neck 40:406–416
Ng SP, Ajayi T, Schaefer AJ et al (2020) Surveillance imaging for patients with head and neck cancer treated with definitive radiotherapy: a partially observed Markov decision process model. Cancer 126:749–756
Roman B, Patel S, Wang M et al (2015) Guideline familiarity predicts variation in self-reported use of routine surveillance PET/CT by physicians who treat head and neck cancer. J Natl Compr Canc Netw 13:69–77
Nocon CC, Kennedy A, Jaffe J, Pruitt J, Kuchta K, Bhayani MK (2021) Costs associated with imaging surveillance after treatment for head and neck cancer. JAMA Otolaryngol Head Neck Surg 147:632–637
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 21:6
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100
Saba NF (2023) Posttreatment surveillance of squamous cell carcinoma of the head and neck. In: UpToDate, Post TW (Ed), Wolters Kluwer (accessed on January 15, 2023)
Alnefaie M, Alamri A, Saeedi A et al (2022) Pulmonary screening practices of otolaryngology-head and neck surgeons across Saudi arabia in the posttreatment surveillance of squamous cell carcinoma: cross-sectional survey study. Interact J Med Res 18:e24592
Ng SP, Ajayi T, Schaefer AJ et al (2020) Surveillance imaging for patients with head and neck cancer treated with definitive radiotherapy: a partially observed Markov decision process model. Cancer 126:749–756
Gore A, Baugnon K, Beitler J et al (2020) Posttreatment imaging in patients with head and neck cancer without clinical evidence of recurrence: should surveillance imaging extend beyond 6 months? AJNR Am J Neuroradiol 41:1238–1244
Ng SP, Pollard C, Berends J et al (2019) Usefulness of surveillance imaging in patients with head and neck cancer who are treated with definitive radiotherapy. Cancer 125:1823–1829
Iovoli AJ, Platek AJ, Degraaff L et al (2018) Routine surveillance scanning in HNSCC: Lung screening CT scans have value but head and neck scans do not. Oral Oncol 86:273–277
Jackowska J, Abelak Y, Piersiala K, Wierzbicka M (2018) The effectiveness of the follow-up of patients after surgery due to cancer of the head and neck. J Comp Eff Res 7:765–773
Meregaglia M, Cairns J, Licitra L, Bossi P (2018) The use of intensive radiological assessments in routine surveillance after treatment for head and neck cancer: an economic evaluation. Eur J Cancer 93:89–98
Kim SA, Roh JL, Kim JS et al (2017) 18F-FDG PET/CT surveillance for the detection of recurrence in patients with head and neck cancer. Eur J Cancer 72:62–70
Kikuchi M, Shinohara S, Hino M et al (2016) Detection of subclinical recurrence or second primary cancer using (18) F-FDG PET/CT in patients treated curatively for head and neck squamous cell carcinoma. Head Neck 38(Suppl 1):E511–E518
Jung YH, Song CM, Park JH et al (2014) Efficacy of current regular follow-up policy after treatment for head and neck cancer: need for individualized and obligatory follow-up strategy. Head Neck 36:715–721
Dunsky KA, Wehrmann DJ, Osman MM, Thornberry BM, Varvares MA (2013) PET-CT and the detection of the asymptomatic recurrence or second primary lesions in the treated head and neck cancer patient. Laryngoscope 123:2161–2164
Kim JW, Roh JL, Kim JS et al (2013) (18)F-FDG PET/CT surveillance at 3–6 and 12 months for detection of recurrence and second primary cancer in patients with head and neck squamous cell carcinoma. Br J Cancer 109:2973–2979
Kostakoglu L, Fardanesh R, Posner M et al (2013) Early detection of recurrent disease by FDG-PET/CT leads to management changes in patients with squamous cell cancer of the head and neck. Oncologist 18:1108–1117
McDermott M, Hughes M, Rath T et al (2013) Negative predictive value of surveillance PET/CT in head and neck squamous cell cancer. AJNR Am J Neuroradiol 34:1632–1636
Paidpally V, Tahari AK, Lam S et al (2013) Addition of 18F-FDG PET/CT to clinical assessment predicts overall survival in HNSCC: a retrospective analysis with follow-up for 12 years. J Nucl Med 54:2039–2045
Beswick DM, Gooding WE, Johnson JT, Branstetter BF (2012) Temporal patterns of head and neck squamous cell carcinoma recurrence with positron-emission tomography/computed tomography monitoring. Laryngoscope 122:1512–1517
Abgral R, Querellou S, Potard G et al (2009) Does 18F-FDG PET/CT improve the detection of posttreatment recurrence of head and neck squamous cell carcinoma in patients negative for disease on clinical follow-up? J Nucl Med 50:24–29
Lee JC, Kim JS, Lee JH et al (2007) F-18 FDG-PET as a routine surveillance tool for the detection of recurrent head and neck squamous cell carcinoma. Oral Oncol 43:686–692
Ho AS, Tsao GJ, Chen FW et al (2013) Impact of positron emission tomography/computed tomography surveillance at 12 and 24 months for detecting head and neck cancer recurrence. Cancer 119:1349–1356
Sullivan BP, Parks KA, Dean NR, Rosenthal EL, Carroll WR, Magnuson JS (2011) Utility of CT surveillance for primary site recurrence of squamous cell carcinoma of the head and neck. Head Neck 33:1547–1550
Saussez S, Dekeyser C, Thill MP, Chantrain G (2007) Importance of clinical and radiological follow-up in head and neck cancers. B-ENT 3:179–184
Zhang I, Branstetter BF, Beswick DM, Maxwell JH, Gooding WE, Ferris RL (2011) The benefit of early PET/CT surveillance in HPV-associated head and neck squamous cell carcinoma. Arch Otolaryngol Head Neck Surg 137:1106–1111
Nair V, Auger S, Kochanny S et al (2022) Development and validation of a decision analytical model for posttreatment surveillance for patients with oropharyngeal carcinoma. JAMA Netw Open 5:e227240
Su W, Miles BA, Posner M, et al. (2018) Surveillance imaging in HPV-related oropharyngeal cancer. Anticancer Res 38:1525–1529
You H, Xi Y, Moore W, Sher D, Sanli Y, Subramaniam RM (2019) Timing and impact of posttreatment PET/CT after first 6 months on patient management and outcomes in oropharyngeal squamous cell carcinoma. AJR Am J Roentgenol 5:1–6
Corpman DW, Masroor F, Carpenter DM, Nayak S, Gurushanthaiah D, Wang KH (2019) Posttreatment surveillance PET/CT for HPV-associated oropharyngeal cancer. Head Neck 41:456–462
Kangelaris GT, Yom SS, Huang K, Wang SJ (2010) Limited utility of routine surveillance MRI following chemoradiation for advanced-stage oropharynx carcinoma. Int J Otolaryngol 2010:904297
Fukumoto C, Oshima R, Sawatani Y et al (2021) Surveillance for patients with oral squamous cell carcinoma after complete surgical resection as primary treatment: a single-center retrospective cohort study. Cancers (Basel) 13:5843
Liu SA, Wang CC, Jiang RS, Tung YC (2021) Less is more? The association between survival and follow-up protocol after treatment in oral cavity cancer patients from a betel quid-prevalent region. Int J Environ Res Public Health 18:12596
Ravanelli M et al (2021) Value of [18F] FDG PET-CT in the follow-up of surgically treated oral tongue squamous cell carcinoma: single centre cohort analysis on 87 patients. Nucl Med Rev 24:58–62
Chi J, Chung S, Lopez C et al (2020) The role of routine surveillance imaging in detecting oral cavity cancer recurrence in asymptomatic patients. J Clin Oncol 38(15_suppl):e18561–e18561
Lin HC, Kang CJ, Huang SF et al (2017) Clinical impact of PET/CT imaging after adjuvant therapy in patients with oral cavity squamous cell carcinoma. Eur J Nucl Med Mol Imaging 44:1702–1711
Peisker A, Raschke GF, Guentsch A, Luepke P, Roshanghias K, Schultze-Mosgau S (2017) Evaluation of a post-treatment follow-up program in patients with oral squamous cell carcinoma. Clin Oral Investig 21:135–141
Rivelli V, Luebbers HT, Weber FE, Cordella C, Grätz KW, Kruse AL (2011) Screening recurrence and lymph node metastases in head and neck cancer: the role of computer tomography in follow-up. Head Neck Oncol 3:18
Al-Shwaiheen FA, Wang SJ, Uzelac A, Yom SS, Ryan WR (2015) The advantages and drawbacks of routine magnetic resonance imaging for long-term post-treatment locoregional surveillance of oral cavity squamous cell carcinoma. Am J Otolaryngol 36:415–423
Krabbe CA, Pruim J, Dijkstra PU et al (2009) 18F-FDG PET as a routine posttreatment surveillance tool in oral and oropharyngeal squamous cell carcinoma: a prospective study. J Nucl Med 50:1940–1947
Hermans R, Pameijer FA, Mancuso AA, Parsons JT, Mendenhall WM (2000) Laryngeal or hypopharyngeal squamous cell carcinoma: can follow-up CT after definitive radiation therapy be used to detect local failure earlier than clinical examination alone? Radiology 214:683–687
Marchi F, Piazza C, Ravanelli M et al (2017) Role of imaging in the follow-up of T2–T3 glottic cancer treated by transoral laser microsurgery. Eur Arch Otorhinolaryngol 274:3679–3686
Morgan R, Karam S (2020) Surveillance imaging of laryngeal cancer-does FDG PET/CT impact survival? J Nucl Med 61(supplement 1):1291–1291
House AE, Zebolsky AL, Jacobs J et al (2021) Surveillance imaging following head and neck cancer treatment and microvascular reconstruction. Laryngoscope 131:2713–2718
Breik O, Kumar A, Birchall J, Mortimore S, Laugharne D, Jones K (2020) Follow up imaging of oral, oropharyngeal and hypopharyngeal cancer patients: comparison of PET-CT and MRI post treatment. J Craniomaxillofac Surg 48:672–679
Suenaga Y, Kitajima K, Ishihara T et al (2016) FDG-PET/contrast-enhanced CT as a post-treatment tool in head and neck squamous cell carcinoma: comparison with FDG-PET/non-contrast-enhanced CT and contrast-enhanced CT. Eur Radiol 26:1018–1030
Ichpujani VK, Rao SA, Chaturvedi AK, Dewan AK, Choudhary PS (2014) Positron emission tomography-computed tomography: a superior and one-stop shop modality for treated head and neck carcinoma compared with conventional tomography. J Oral Maxillofac Surg 72:2319–2332
Ghanooni R, Delpierre I, Magremanne M et al (2011) 18F-FDG PET/CT and MRI in the follow-up of head and neck squamous cell carcinoma. Contrast Media Mol Imaging 6:260–266
Wang YF, Liu RS, Chu PY, et al. (2009) Positron emission tomography in surveillance of head and neck squamous cell carcinoma after definitive chemoradiotherapy. Head Neck 31:442–451
Fakhry N, Lussato D, Jacob T, Giorgi R, Giovanni A, Zanaret M (2007) Comparison between PET and PET/CT in recurrent head and neck cancer and clinical implications. Eur Arch Otorhinolaryngol 264:531–538
Salaun PY, Abgral R, Querellou S et al (2007) Does 18fluoro-fluorodeoxyglucose positron emission tomography improve recurrence detection in patients treated for head and neck squamous cell carcinoma with negative clinical follow-up? Head Neck 29:1115–1120
Bird T, Barrington S, Thavaraj S et al (2016) (18)F-FDG PET/CT to assess response and guide risk-stratified follow-up after chemoradiotherapy for oropharyngeal squamous cell carcinoma. Eur J Nucl Med Mol Imaging 43:1239–1247
Berger BM, Hanna GJ, Posner MR et al (2022) Detection of occult recurrence using circulating tumor tissue modified viral HPV DNA among patients treated for HPV-driven oropharyngeal carcinoma. Clin Cancer Res 28:4292–4301
Chera BS, Kumar S, Shen C et al (2020) Plasma circulating tumor HPV DNA for the surveillance of cancer recurrence in HPV-associated oropharyngeal cancer. J Clin Oncol 38:1050–1058
Hermans R (2008) Posttreatment imaging in head and neck cancer. Eur J Radiol 66:501–511
Funding
No funding was received for this paper.
Author information
Authors and Affiliations
Contributions
SVH did the database search with help from RH. SVH analyzed the manuscripts and summarized the results; RH supervised the entire process. The manuscript was written by SVH with contributions from RH. Both authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was waived by the University Hospitals Leuven and KU Leuven’s Research Ethics Committee and The Educational Supervisory Committee on Medical Ethics.
Consent for publication
Not applicable.
Competing interests
RH is Emeritus Editor of Insights into Imaging. He has not taken part in the review or selection process of this article.
The authors declare that they have no financial or non-financial competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Post-treatment imaging of cancer of the hypopharynx/larynx beyond the first 3–6-month baseline imaging study. Overview of included studies evaluating the results obtained with routine imaging surveillance compared to symptom- and/or clinical finding- directed imaging. Supplementary Table 2. Post-treatment imaging of head and neck cancer beyond the first 3–6-month baseline imaging study. Comparison of imaging techniques.
Additional file 2:
Manuscript selection sheet.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Van Hoe, S., Hermans, R. Post-treatment surveillance imaging in head and neck cancer: a systematic review. Insights Imaging 15, 32 (2024). https://doi.org/10.1186/s13244-023-01578-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-023-01578-4