Abstract
Objectives
This study aimed to investigate the influence of microvascular impairment on myocardial characteristic alterations in remote myocardium at multiple time points, and its prognostic significance after acute ST-segment elevation myocardial infarction (STEMI).
Methods
Patients were enrolled prospectively and performed CMR at baseline, 30 days, and 6 months. The primary endpoint was major adverse cardiac events (MACE): death, myocardial reinfarction, malignant arrhythmia, and hospitalization for heart failure. Cox proportional hazards regression modeling was analyzed to estimate the correlation between T1 mapping of remote myocardium and MACE in patients with and without microvascular obstruction (MVO).
Results
A total of 135 patients (mean age 60.72 years; 12.70% female, median follow-up 510 days) were included, of whom 86 (63.70%) had MVO and 26 (19.26%) with MACE occurred in patients. Native T1 values of remote myocardium changed dynamically. At 1 week and 30 days, T1 values of remote myocardium in the group with MVO were higher than those without MVO (p = 0.030 and p = 0.001, respectively). In multivariable cox regression analysis of 135 patients, native1w T1 (HR 1.03, 95%CI 1.01–1.04, p = 0.002), native30D T1 (HR 1.05, 95%CI 1.03–1.07, p < 0.001) and LGE (HR 1.10, 95%CI 1.05–1.15, p < 0.001) were joint independent predictors of MACE. In multivariable cox regression analysis of 86 patients with MVO, native30D T1 (HR 1.05, 95%CI 1.04–1.07, p < 0.001) and LGE (HR 1.10, 95%CI 1.05–1.15, p < 0.001) were joint independent predictors of MACE.
Conclusions
The evolution of native T1 in remote myocardium was associated with the extent of microvascular impairment after reperfusion injury. In patients with MVO, native30D T1 and LGE were joint independent predictors of MACE.
Key points
-
Microvascular impairment correlated with native T1 of remote myocardium.
-
Native T1 values of remote myocardium changed dynamically.
-
Native30D T1 and LGE were joint independent predictors of MACE.
Similar content being viewed by others
Introduction
In the course of the past 30 years, the mortality rate during the acute phase of ST-elevation myocardial infarction (STEMI) has declined steadily and appeared now to have reached a plateau at lower values when compared with those in the pre-reperfusion era [1]. However, the success of emergency coronary reperfusion therapy in STEMI is usually limited by tissue perfusion failure [2], which has been shown to increase the risk of future cardiovascular events [3]. Several published trials have provided evidence that MVO is the best predictor for prognostic value among all CMR parameters, including clinical scores, left ventricular ejection fraction, and infarct size [4,5,6]. Microvascular injury after acute myocardial infarction affects local T1 value [7]. However, in patients with acute myocardial infarction (AMI), myocardial tissue injury and cardiac remodeling extend beyond the region supplied by the culprit artery; they also affect the remote, non-infarcted myocardium [8].
Several studies have reported remote myocardium alterations in patients with AMI, both in animal and clinical studies [9,10,11,12]. A study by Carrick et al. [13] showed that in remote zone native T1 mapping, early changes may be associated with the occurrence of early post-infarction remodeling, and in a secondary analysis, adverse outcome. However, it was not evaluated whether independent and incremental prognostic information was provided by the remote zone native T1 values over established CMR markers of infarct severity. Reinstadler et al. [14] reported that in addition to clinical risk factors and traditional CMR outcome markers, independent and incremental prognostic information was provided by remote zone alterations by native T1 mapping. The reproducibility of native T1 mapping is excellent with significant regional differences [15]. Thus, T1 of remote zone alterations may become a novel therapeutic target and a useful parameter for optimized risk stratification. Previous studies mainly focused on remote myocardium alterations in acute phase and do not evaluate the impact of MVO on remote myocardium alterations [14, 16]. Consequently, the promising role of dynamic remote myocardium alterations with MVO for the prediction of hard clinical events, and especially its potential incremental prognostic value compared with other markers of infarct severity, remains uncertain.
We designed a longitudinal clinical study in which patients with STEMI successfully treated by primary angioplasty were prospectively recruited, and a CMR was performed within the first week post-reperfusion, on day 30, and at 6 months. The impact of the dynamic change on post-MI CMR measures of remote myocardium was evaluated in reperfused MI by performing T1 mapping and a comprehensive serial CMR imaging study. Our study aimed to investigate the correlations between T1 mapping in remote myocardium and microvascular impairment and to comprehensively assess the value of T1 mapping as a prognostic indicator in patients with STEMI treated by primary percutaneous coronary intervention (PPCI).
Materials and methods
Study population and clinical endpoints
This was a prospective observational investigator-led study conducted at the Renji Hospital between June 2015 and December 2018. Patients with STEMI, who underwent PPCI within 12 h of symptom onset, were prospectively enrolled in our study.
Our study protocol was approved by the institutional ethics committee and was also in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants. Fifty age-matched normal participants were recruited as the control group to acquire the normal reference range. Exclusion criteria for participants included the commonly accepted contraindications to CMR, such as the usage of devices (implantable cardioverter-defibrillators, pacemakers, and cerebral aneurysm clips), non-ischemic cardiomyopathy (amyloidosis, cardiomyopathy due to iron deposition, valvular heart disease, evidence of inflammatory processes or Anderson–Fabry disease, and so on), coronary artery bypass grafting, previous AMI, severe claustrophobia, estimated glomerular filtration rate < 30 ml/min/1.73 m2, and/or significant arrhythmias. The clinical endpoint was major adverse cardiac events (MACE) composite of death, myocardial reinfarction, malignant arrhythmia, and hospitalization for heart failure within 3 years.
CMR imaging
CMR examinations were performed within 1 week, 30 days, and 6 months after STEMI with a 3.0 T scanner (Ingenia, Philips, Best, The Netherlands). The parameters of CMR sequences (SSFP, steady-state free-precession; T2WI-STIR, T2-weighted short-tau triple inversion recovery; native T1 mapping; T2* mapping; and first pass perfusion and LGE) are described in Additional file 1: Table S1.
Analysis of CMR images
Cardiac MR images were analyzed by two radiologists from our team with at least 5 years’ experience (Lian-Ming Wu and Bing-Hua Chen, with over 10 and 7 years) in CMR diagnostic imaging. The LV functional parameters (volumes, mass, and function) and morphology were qualified and quantified with commercial software Cvi42 Version 5.11.3 (Circle Cardiovascular Imaging Inc., Calgary, Canada). We defined remote myocardium as myocardium without evidence of infarction, edema, or enhancement [13]. The ROI of T1 mapping was placed in the territory of non-culprit vessel, which located in the myocardial segment 180°from the infarcted territory [17]. ROI in the remote myocardium was taken in the same place across the 3 scans.
Transmurality was estimated by using the centerline chord method as previous study proposed during the acute stage [18]. Microvascular obstruction (MVO) refers to a dark hypointense core within the regions of hyperenhancement on LGE during the first week after reperfusion. Intramyocardial hemorrhage (IMH) is defined as a hypointense core within the myocardial infarction zone on T2* mapping [17, 19]. Special care should be taken to have sufficient distance from adjacent tissue, such as the lungs or blood, to avoid partial volume artifacts [20]. The infarct volume fraction was quantified in LGE with full-width at half-maximum (FWHM) technique [21].
Statistical analysis
Statistical analysis was performed using SPSS Statistics version 23.0, (IBM SPSS Inc., Chicago, Illinois, USA) and MedCalc Software version 11.4.2.0 (MedCalc Software, Ostend, Belgium). Normality of variable distribution was determined by the Kolmogorov–Smirnov test and qualitative inspection of Q–Q plots. Continuous variables with normal distribution, expressed as mean ± SD, were compared using the independent t test of two samples. Non-normally distributed variables, expressed as median and inter-quartile ranges, were compared with Kruskal–Wallis test. Frequency (percentage) for categorical data of different groups was compared using the chi-square test or Fisher exact test. The optimal cutoff values of remote myocardial T1 for the prediction of MACE were calculated by the Youden index value. MACE-free survival was described by the Kaplan–Meier method. To identify predictors of MACE, we performed univariable and multivariable Cox regression analyses. To determine independent associations with MACE during follow-up (adjusted hazard ratio [95% CI]), we performed multivariable analysis with the forward selection (likelihood ratio) modeling. Five separate models were performed to ensure statistical robustness of the Cox regression analysis. C-statistics were used to compare different parameters for predicting MACE. A 2-tailed p < 0.05 was considered statistically significant.
Results
Study population
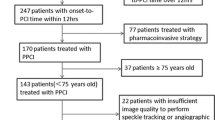
Of 152 patients with STEMI included in our prospective observational study, 135 patients (mean age 60.72 years; 12.70% female, median follow-up of 510 days) underwent the standardized CMR protocol at least twice (Fig. 1). Overall, 86 patients with MVO and 49 patients without MVO were followed up for three years. Participants were dichotomized according to whether they were complicated with MVO (86 patients with MVO).
Baseline characteristics
The patients’ baseline characteristics are summarized in Table 1. Patients with MVO tended to have higher peaks of CK-MB (p = 0.006), cTnI (p < 0.001), BNP (p = 0.020), and CRP (p < 0.001) and were more likely to have MACE (25.60% vs. 8.20%, p = 0.013). The obstruction of culprit vessels occurred more often in the proximal segments in patients with MVO than without MVO (p = 0.002). TIMI flow grade was lower in patients with MVO during pre (p = 0.030)- and post-PCI (p = 0.040).
CMR findings
Patients with MVO tended to have lower LVEF on three occasions: within 1 week (p = 0.001), 30 days (p = 0.001), and 6 months (p = 0.003). They were also more likely to have higher LGE volume on three occasions: within 1 week (p < 0.001), 30 days (p < 0.001), and 6 months (p = 0.002) (Table 2). Transmural infarction (p < 0.001), pericardial effusion (p < 0.001), and IMH (p < 0.001) occurred more often in patients with MVO.
Native T1 values of remote myocardium in patients with and without MVO changed from 1 week to 6 months after MI dynamically. The native T1 value of remote myocardium in the first week was higher than those of 1 month. Compensatory thickening of the basal left ventricular septum was greater in patients with MVO than those without MVO (Fig. 2). At 1 week and 30 days, remote myocardium T1 values of group with MVO were higher than those without MVO (p = 0.030 and p = 0.001, respectively), while differences were not significant at 6 months (p = 0.09). In patients with and without MVO, remote T1 values were lowest at 30 days and highest at 6 months (Fig. 3A). In patients with and without MACE, remote T1 values were lowest at 30 days (Fig. 3B). Patients with MACE tended to have higher native T1 values (Additional file 1: Table S2).
Native T1 values of remote myocardium in patients with and without MVO changed from 1 week to 6 months after MI dynamically. The native T1 value of remote myocardium in the first week was higher than those of 1 month. Inflammation of remote myocardium increased in the acute phase while diminished gradually during follow-up, and fibrosis of remote myocardium increased gradually. Native T1 values were determined by myocardial fibrosis in the chronic stage. The first patient had mural thrombosis in the apical during the first week. Compensatory thickening of the basal left ventricular septum was greater in patients with MVO than those without MVO
The box-plots (25th percentile, median, and 75th percentile) represent dynamic changes in native T1 values of remote myocardium on three occasions. In patients with and without MVO, remote T1 values were lowest at 30 days and highest at 6 months (A). In patients with and without MACE, remote T1 values were lowest at 30 days (B)
Endpoints and clinical outcome
During a median (510 days) follow-up, a total of 26 (19.26%) MACE (death, n = 2 [1.48%]; myocardial reinfarction, n = 4 [2.96%]; ventricular tachycardia, n = 1 [0.74%]; and hospitalization for heart failure, n = 19 [14.07%]) were observed.
In the univariable Cox regression analysis (Table 3), patients with the following characteristics were significantly associated with MACE: higher Killip class (HR 2.47, 95%CI 1.53–4, p < 0.001), higher cTnImax (HR 1.01, 95%CI 1.001–1.02, p = 0.030), higher CRPmax (HR 1.02, 95%CI 1.01–1.03, p = 0.004), lower TIMI flow grade of post-PCI (HR 0.37, 95%CI 0.20–0.70, p = 0.002), lower LVEF1w (HR 0.93, 95%CI 0.90–0.97, p < 0.001), lower LVEF6M (HR 0.95, 95%CI 0.92–0.99, p = 0.013), higher LGE1w (HR 1.10, 95%CI 1.06–1.14, p < 0.001), higher LGE30D (HR 1.12, 95%CI 1.08–1.17, p < 0.001), higher LGE6M (HR 1.05, 95%CI 1.01–1.09, p < 0.001), higher remote native1w T1 (HR 1.02, 95%CI 1.004–1.03, p = 0.009), higher remote native30D T1 (HR 1.04, 95%CI 1.03–1.05, p < 0.001), higher remote native6M T1 (HR 1.02, 95%CI 1.01–1.03, p = 0.004), higher frequency of transmural infarction (HR 5.26, 95%CI 1.24–22.27, p = 0.024), IMH (HR 3.57, 95%CI 1.07–11.93, p = 0.038), and MVO (HR 2.95, 95%CI 1.01–8.56, p = 0.047).
For univariable Cox regression analysis, p ≤ 0.1 was included into stepwise multivariable Cox regression analysis. Native1w T1 (HR 1.03, 95%CI 1.01–1.04, p = 0.002), Native30D T1 (HR 1.05, 95%CI 1.03–1.07, p < 0.001), and LGE (HR 1.10, 95%CI 1.05–1.15, p < 0.001) were joint independent predictors of MACE during mid-term follow-up for all patients with STEMI after PPCI (Table 4). In multivariable cox regression analysis of 86 patients with MVO, native30D T1 (HR 1.05, 95%CI 1.04–1.07, p < 0.001) and LGE (HR 1.10, 95%CI 1.05–1.15, p < 0.001) were joint independent predictors of MACE (Additional file 1: Table S4). Native T1 of remote myocardium surpasses predictive value of MVO or LGE in C-statistics of all patients (p < 0.001). And native30D T1 value was stronger independent predictor than native1w T1 in C-statistics of patients with MVO (p < 0.001) (Fig. 4).
Discussion
Our comprehensive, longitudinal CMR investigation demonstrated that T1 mapping of remote myocardium changed during periods of approximately 1 week, 30 days, and 6 months. Patients with MVO following reperfused STEMI showed a substantial correlation with changes in T1 mapping of the remote myocardium. The principal findings included: (1) The severity of microvascular impairment after reperfusion is correlated with the evolution of native T1 values in remote myocardium. Patients who suffered from severe microvascular impairment display higher T1 values, which is consistent with fibrosis expansion. (2) Native1w T1 value, native30D T1 value, and LGE were joint independent predictors of MACE during mid-term follow-up for patients with STEMI after PPCI. (3) In reperfused STEMI patients with MVO, native30D T1 and LGE were joint independent predictors of MACE.
Accurate noninvasive quantification and detection of remote myocardium alteration in reperfused STEMI patients are scientifically and clinically invaluable for their usefulness in prognosis prediction. Carrick et al. [13] found that early inflammation post-MI is associated with native T1 mapping. Several studies have confirmed that the native T1 of remote myocardium in the acute stage provided independent prognostic information for cardiac recovery and MACE [13, 14, 16]. However, none of the former studies revealed differences in native T1 values between STEMI patients with and without MVO. MVO after STEMI has a trend of dynamic change, which appears in the first week and disappears by day 30. MBF of infarcted myocardium significantly increased at 6 months compared with 1 to 3 days after STEMI [22]. Our findings unequivocally demonstrate that the dynamic changes in native T1 mapping from the acute stage to approximately 30 days, and approximately 6 months.
Local and systemic inflammatory responses were triggered due to ischemia and reperfusion in the acute stage after STEMI. Aggregation of neutrophil and platelets will further obliterate the microvascular lumen, which will then induce further microvascular impairment, ultimately leading to the production of vasoconstrictors and inflammatory mediators [23]. Acute STEMI will trigger a spectrum of alterations in the remote vessels, including upregulation of the platelet-endothelial adhesion from endothelial-associated von Willebrand factor multimers and endothelial inflammatory adhesion molecules [24]. The activation of leukocyte infiltration and proinflammatory pathways is related to the response of the remote myocardium [25]. The remodeling process post-infarction has been increasingly recognized as a cause of inflammatory response [26]. Native T1 values were determined by myocardial water content and cellularity [27]. Increased T1 of myocardium with inflammatory cell infiltration was confirmed by histopathology in patients with the features of acute rejection who underwent cardiac transplant [28]. Therefore, myocardial edema and hypercellularity, due to the inflammation during the acute phase post-STEMI, are the reasons why there has been an increase in the remote myocardial native T1 in the acute stage [13, 14]. Most patients with MVO also had IMH implicated severe microvascular impairment. Persistent crystallized iron deposition from MVO complicated with IMH is directly associated with left ventricular adverse remodeling in the chronic stage after MI, infarct resorption, and proinflammatory burden [29].
Inflammation of remote myocardium increased in the acute phase while diminished gradually during follow-up, and fibrosis of remote myocardium increased gradually. Native T1 values were determined by myocardial fibrosis in the chronic stage [30]. These may be the main reasons for the bimodal behavior of the T1 value in the remote myocardium. Diffuse myocardial fibrosis can cause the increase in native T1 [11]. In the chronic phase, prolonged T1 values correlate with the severity of myocardial interstitial fibrosis [31], which has been advocated as the sensitive marker to differentiate between fibrosis and healthy myocardium [32].
Microvascular dilation and increased blood volume may cause T1 values to increase after myocardial ischemia [33]. Another key explanation for the higher T1 values at first week, compared to values at one month, may be that myocardial blood flow of remote regions increased after MI, reflecting the hyperdynamic performance of remote myocardium [34]. Coronary microvascular injury and obstruction occur in approximately half of patients after successful primary PCI and is associated with worse outcomes compared to those without microvascular injury [3]. Severe microvascular impairment will cause a stronger systemic response, including both the infarcted and non-infarcted myocardium. Compensatory enhancement of systolic function in remote myocardium leads to compensatory cellular hypertrophy, hyperkinesis after STEMI, and cellular dysfunction [11].
Our study has several limitations. First, our sample size was small. However, a total of 341 CMR scans were performed (within 1 week = 135, 30 days = 134, 6 months = 72) on 135 patients, with each patient undergoing at least two scans. Thus, it is necessary to confirm our findings in a large-scale study. Nevertheless, our data—baseline characteristics, CMR results on infarct severity, and incidence of MACE—are comparable with other recent CMR studies [4]. In light of the fact that patients were scanned successively, we kept our CMR protocol as short as possible. Instead, both myocardium edema and hemorrhage were assessed by T2W-STIR imaging, a sequence validated and used in many published papers for these purposes. Patients with anterior STEMI, and also patients with inferolateral wall STEMI, were included in our clinical study. This may possibly induce magnetic-field non-homogeneity associated with the inferolateral wall. Additionally, care should be taken when extrapolating results to lateral MI locations, especially when attempting to adequately visualize the phenomenon, as signal loss attributable to through-plane cardiac motion may occur [35]. Wall stress may affect the pathophysiology of the remote zone in STEMI. Future studies are needed to examine wall stress and determine the clinical significance of native T1 changes in the longer-term follow-up.
To summarize, our study is the first longitudinal pathophysiological study of remote myocardium that evaluated mid-term outcomes through CMR. Native T1 mapping could detect myocardial abnormalities in remote myocardium that may be neglected by conventional LGE. The early detection of diffuse myocardial pathological alterations in the remote myocardium among survivors of STEMI allows for a more timely and individualized treatment and disease-specific therapy. The assessment of dynamic evolution of remote myocardium and the adjudication of outcome events are other strengths of the study.
Conclusion
The evolution of native T1 in remote myocardium associated with the extent of microvascular impairment after reperfusion injury. Native1w T1 value, native30D T1 value, and LGE were joint independent predictors of MACE during mid-term follow-up for all patients with STEMI after PPCI. In reperfused STEMI patients with MVO, native30D T1 and LGE were joint independent predictors of MACE. These findings may provide insight into the assessment of LV remodeling and prognosis after myocardial infarction.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AMI:
-
Acute myocardial infarction
- BNPmax :
-
Peak brain natriuretic peptide
- CK-MBmax :
-
Peak creatinine kinase-MB
- CMR:
-
Cardiac magnetic resonance
- CRPmax :
-
Peak C-creative protein
- cTnImax :
-
Peak troponin I
- iLVEDV:
-
Indexed left ventricular end-diastolic volume
- IMH:
-
Intramyocardial hemorrhage
- LAD:
-
Left anterior descending
- LGE:
-
Late gadolinium enhancement
- LVEDV:
-
Left ventricular end-diastolic volume
- LVEF:
-
Left ventricular ejection fraction
- LVESV:
-
Left ventricular end-systolic volume
- MACE:
-
Major adverse cardiac events
- MVO:
-
Microvascular obstruction
- NT-proBNP:
-
N-terminal pro-brain natriuretic peptide
- PPCI:
-
Primary percutaneous coronary intervention
- SSFP:
-
Steady-state free-precession
- STEMI:
-
ST-segment elevation myocardial infarction
- T2WI-STIR:
-
T2-weighted short-tau triple inversion recovery
References
Rodriguez-Palomares JF, Gavara J, Ferreira-Gonzalez I, et al. (2019) Prognostic value of initial left ventricular remodeling in patients with reperfused STEMI. JACC Cardiovasc Imaging 12(12):2445–2456
Yellon DM, Hausenloy DJ (2007) Myocardial reperfusion injury. N Engl J Med 357(11):1121–1135
Niccoli G, Scalone G, Lerman A, Crea F (2016) Coronary microvascular obstruction in acute myocardial infarction. Eur Heart J 37(13):1024–1033
Eitel I, de Waha S, Wohrle J, et al. (2014) Comprehensive prognosis assessment by CMR imaging after ST-segment elevation myocardial infarction. J Am Coll Cardiol 64(12):1217–1226
de Waha S, Desch S, Eitel I, et al. (2012) Relationship and prognostic value of microvascular obstruction and infarct size in ST-elevation myocardial infarction as visualized by magnetic resonance imaging. Clin Res Cardiol 101(6):487–495
Hadamitzky M, Langhans B, Hausleiter J, et al. (2014) Prognostic value of late gadolinium enhancement in cardiovascular magnetic resonance imaging after acute ST-elevation myocardial infarction in comparison with single-photon emission tomography using Tc99m-Sestamibi. Eur Heart J Cardiovasc Imaging 15(2):216–225
Robbers L, Nijveldt R, Beek AM, et al. (2018) The influence of microvascular injury on native T1 and T2* relaxation values after acute myocardial infarction: implications for non-contrast-enhanced infarct assessment. Eur Radiol 28(2):824–832
Pfeffer MA, Braunwald E (1990) Ventricular remodeling after myocardial infarction. Exp Observ Clin Implic Circ 81(4):1161–1172
Cleutjens JP, Verluyten MJ, Smiths JF, Daemen MJ (1995) Collagen remodeling after myocardial infarction in the rat heart. Am J Pathol 147(2):325–338
Kramer CM, Rogers WJ, Theobald TM, Power TP, Geskin G, Reichek N (1997) Dissociation between changes in intramyocardial function and left ventricular volumes in the eight weeks after first anterior myocardial infarction. J Am Coll Cardiol 30(7):1625–1632
Bogaert J, Bosmans H, Maes A, Suetens P, Marchal G, Rademakers FE (2000) Remote myocardial dysfunction after acute anterior myocardial infarction: impact of left ventricular shape on regional function: a magnetic resonance myocardial tagging study. J Am Coll Cardiol 35(6):1525–1534
Husser O, Chaustre F, Sanchis J, et al. (2012) Function of remote non-infarcted myocardium after STEMI: analysis with cardiovascular magnetic resonance. Int J Cardiovasc Imaging 28(8):2057–2064
Carrick D, Haig C, Rauhalammi S, et al. (2015) Pathophysiology of LV remodeling in survivors of STEMI: inflammation remote myocardium, and prognosis. JACC Cardiovasc imaging 8(7):779–789
Reinstadler SJ, Stiermaier T, Liebetrau J, et al. (2018) Prognostic significance of remote myocardium alterations assessed by quantitative noncontrast T1 mapping in ST-segment elevation myocardial infarction. JACC Cardiovasc Imaging 11(3):411–419
Bottcher B, Lorbeer R, Stocklein S, et al. (2021) Global and regional test-retest reproducibility of native T1 and T2 mapping in cardiac magnetic resonance imaging. J Magn Reson Imaging 54(6):1763–1772
Puntmann VO, Carr-White G, Jabbour A, et al. (2018) International TMCMROS, native T1 and ECV of noninfarcted myocardium and outcome in patients with coronary artery disease. J Am Coll Cardiol 71(7):766–778
Bulluck H, Dharmakumar R, Arai A, Berry C, Hausenloy D (2018) Cardiovascular magnetic resonance in acute ST-segment-elevation myocardial infarction: recent advances, controversies, future directions. Circulation 137(18):1949–1964
Amado LC, Gerber BL, Gupta SN, et al. (2004) Accurate and objective infarct sizing by contrast-enhanced magnetic resonance imaging in a canine myocardial infarction model. J Am Coll Cardiol 44(12):2383–2389
Kandler D, Lucke C, Grothoff M, et al. (2014) The relation between hypointense core, microvascular obstruction and intramyocardial haemorrhage in acute reperfused myocardial infarction assessed by cardiac magnetic resonance imaging. Eur Radiol 24(12):3277–3288
Puntmann VO, Peker E, Chandrashekhar Y, Nagel E (2016) T1 mapping in characterizing myocardial disease: a comprehensive review. Circ Res 119(2):277–299
Mikami Y, Kolman L, Joncas S, et al. (2014) Accuracy and reproducibility of semi-automated late gadolinium enhancement quantification techniques in patients with hypertrophic cardiomyopathy. J Cardiovasc Magn Reson 16:85. https://doi.org/10.1186/s12968-12014-10085-x
Borlotti A, Jerosch-Herold M, Liu D et al (2019) Acute microvascular impairment post-reperfused STEMI is reversible and has additional clinical predictive value: a CMR OxAMI study. JACC Cardiovasc Imaging 12(9):1783–1793
Bekkers SC, Yazdani SK, Virmani R, Waltenberger J (2010) Microvascular obstruction: underlying pathophysiology and clinical diagnosis. J Am Coll Cardiol 55(16):1649–1660
Moccetti F, Brown E, Xie A, et al. (2018) Myocardial infarction produces sustained proinflammatory endothelial activation in remote arteries. J Am Coll Cardiol 72(9):1015–1026
Lee WW, Marinelli B, van der Laan AM, et al. (2012) PET/MRI of inflammation in myocardial infarction. J Am Coll Cardiol 59(2):153–163
Seropian IM, Toldo S, Van Tassell BW, Abbate A (2014) Anti-inflammatory strategies for ventricular remodeling following ST-segment elevation acute myocardial infarction. J Am Coll Cardiol 63(16):1593–1603
Mathur-De Vre R (1984) Biomedical implications of the relaxation behaviour of water related to NMR imaging. Br J Radiol 57(683):955–976
Miller CA, Naish JH, Shaw SM, et al. (2014) Multiparametric cardiovascular magnetic resonance surveillance of acute cardiac allograft rejection and characterisation of transplantation-associated myocardial injury: a pilot study. J Cardiovasc Magn Reson 16:52. https://doi.org/10.1186/s12968-014-0052-6
Kali A, Cokic I, Tang R, et al. (2016) Persistent microvascular obstruction after myocardial infarction culminates in the confluence of ferric iron oxide crystals, proinflammatory burden, and adverse remodeling. Circ Cardiovasc Imaging. https://doi.org/10.1161/CIRCIMAGING.115.004996
French BA, Kramer CM (2007) Mechanisms of post-infarct left ventricular remodeling. Drug Discov Today Dis Mech 4(3):185–196
Bull S, White SK, Piechnik SK, et al. (2013) Human non-contrast T1 values and correlation with histology in diffuse fibrosis. Heart 99(13):932–937
Puntmann VO, Voigt T, Chen Z, et al. (2013) Native T1 mapping in differentiation of normal myocardium from diffuse disease in hypertrophic and dilated cardiomyopathy. JACC Cardiovasc Imaging 6(4):475–484
Mahmod M, Piechnik SK, Levelt E, et al. (2014) Adenosine stress native T1 mapping in severe aortic stenosis: evidence for a role of the intravascular compartment on myocardial T1 values. J Cardiovasc Magn Reson 16:92. https://doi.org/10.1186/s12968-014-0092-y
Rechavia E, de Silva R, Nihoyannopoulos P, Lammertsma AA, Jones T, Maseri A (1995) Hyperdynamic performance of remote myocardium in acute infarction. Correlation between regional contractile function and myocardial perfusion. Eur Heart J 16(12):1845–1850
Fernandez-Friera L, Garcia-Ruiz JM, Garcia-Alvarez A, et al. (2017) Accuracy of area at risk quantification by cardiac magnetic resonance according to the myocardial infarction territory. Rev Esp Cardiol (Engl Ed) 70(5):323–330
Acknowledgements
We thank Lian-Ming Wu, whose important contributions to this study were indispensable to its success.
Funding
This study was supported by National Natural Science Foundation of China (Nos. 81873886, 81873887, and 82171884); National Natural Science Foundation of China Youth project (No. 82101981); Shanghai Science and technology innovation action plan, technology standard project Grant numbers (No. 19DZ2203800); Shanghai Science and technology innovation action plan, technology standard project (No. 19DZ2203800); Shanghai Municipal Education Commission-Gao feng Clinical Medicine Grant: Shanghai Jiao Tong University school of medicine Double hundred outstanding person project (No. 20191904); and Shanghai Jiao Tong University medical engineering cross project (No. YG2022QN016).
Author information
Authors and Affiliations
Contributions
B-HC and L-MW contributed to conceptualization, methodology, writing, and funding acquisition. MB, EO, and JH contributed to review and editing. D-AA and C-WW were involved in statistical analysis and data collection. TY was involved in literature search. JP and YZ were involved in investigation and funding acquisition and supervision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Our study protocol was approved by the institutional ethics committee and was also in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants.
Consent for publication
This manuscript is approved by all patients for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The supplementary file provides a detailed description of research methods and results.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, BH., An, DA., Wu, CW. et al. Prognostic significance of non-infarcted myocardium correlated with microvascular impairment evaluated dynamically by native T1 mapping. Insights Imaging 14, 50 (2023). https://doi.org/10.1186/s13244-022-01360-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-022-01360-y