Abstract
Objectives
Different noninvasive imaging methods to predict the chance of malignancy of ovarian tumors are available. However, their predictive value is limited due to subjectivity of the reviewer. Therefore, more objective prediction models are needed. Computer-aided diagnostics (CAD) could be such a model, since it lacks bias that comes with currently used models. In this study, we evaluated the available data on CAD in predicting the chance of malignancy of ovarian tumors.
Methods
We searched for all published studies investigating diagnostic accuracy of CAD based on ultrasound, CT and MRI in pre-surgical patients with an ovarian tumor compared to reference standards.
Results
In thirty-one included studies, extracted features from three different imaging techniques were used in different mathematical models. All studies assessed CAD based on machine learning on ultrasound, CT scan and MRI scan images. Per imaging method, subsequently ultrasound, CT and MRI, sensitivities ranged from 40.3 to 100%; 84.6–100% and 66.7–100% and specificities ranged from 76.3–100%; 69–100% and 77.8–100%. Results could not be pooled, due to broad heterogeneity. Although the majority of studies report high performances, they are at considerable risk of overfitting due to the absence of an independent test set.
Conclusion
Based on this literature review, different CAD for ultrasound, CT scans and MRI scans seem promising to aid physicians in assessing ovarian tumors through their objective and potentially cost-effective character. However, performance should be evaluated per imaging technique. Prospective and larger datasets with external validation are desired to make their results generalizable.
Key points
-
Computer-aided diagnostics has potential to predict the nature of ovarian tumors.
-
Literature shows heterogeneous sensitivity and specificity of machine learning on ultrasound images, CT-scan images and MRI-scan images.
-
More prospective studies on other computer-aided techniques and imaging modalities should be performed with an external validation set.
Similar content being viewed by others
Introduction
An accurate preoperative diagnosis of an ovarian tumor into either benign, borderline or malignant is important for multiple reasons: (1) for the patients’ surgical workup and treatment planning, (2) for the patients’ mental wellbeing and (3) for correct use of diagnostic algorithms [1]. Currently, most women diagnosed with an ovarian tumor are initially evaluated with transvaginal ultrasound and serum CA125. For a more objective approach, different ultrasound-based models, to discriminate between benign, borderline and malignant ovarian tumors, have been constructed over time. One of the first widely used models is the risk of malignancy index (RMI) which combines five ultrasound variables with serum CA125 and postmenopausal status [2]. Other models have been developed by the International Ovarian tumor analysis (IOTA) group, such as the Assessment of Different NEoplasias in the adneXa (ADNEX) model, which combines six ultrasound features together with patients age, serum CA125 and type of center (oncology referral center vs other) [3, 4]. However, for both models the reported sensitivity lies around 98% and 71%, and the specificity around 85% and 62% [5]. In addition, two other classification models were introduced by radiologists and gynecologists: (1) the GI-RADs (Gynecologic Imaging Reporting and Data System) score, for diagnosis of adnexal masses by pelvic ultrasound, and (2) the O-RADS (Ovarian-adnexal reporting and data system) data system, both showing a sensitivity of 92.7% and 93.6% and a specificity of 96.8% and 92.8% [6, 7]. Nevertheless, research has shown that ultrasound features are often misclassified by unexperienced examiners [8].
Nowadays, preoperative computer tomography (CT) and/or magnetic resonance imaging (MRI) is performed to pre-surgically assess the nature of an ovarian tumor and to predict the presence of metastatic disease. MRI has proven to be able to discriminate between benign and malignant ovarian tumors with a sensitivity of 96% and a specificity of 91%. The O-RADs MRI has a sensitivity of 93% and a specificity of 91% for score 5 (malignant) with a comparable reading between senior and junior radiologists [7, 9, 10]. However, for spiral CT scans no diagnostic studies are available. Research conducted with multidetector CT scans shows an accuracy of 90 to 93% in adnexal mass characterization [11].
For clinicians, ideally, when using any test a 100% sensitivity and specificity is desired. For imaging prediction models, this means that no malignant tumors are missed and no benign tumors are classified as malignant to prevent unnecessary surgical procedures on benign ovarian tumors [12, 13]. Hence, diagnostic accuracy with a higher sensitivity at the detriment of the specificity is favorable. The currently used imaging prediction models show high performance in ovarian tumor classification; nevertheless, they are greatly affected by subjective assessment and users’ experience. Therefore, evaluation of more independent strategies to determine the nature of ovarian tumors among these different imaging modalities is needed.
Over the past three decades, several computer-aided diagnostics (CADs) have been developed for accurate ovarian cancer prediction, mainly on ultrasound, all using predefined hand-selected features to build their classifiers [14,15,16]. Computer-aided diagnostics is used to assist clinical professionals within different medical specialties, such as dermatology, neurology and pathology [17,18,19,20]. Furthermore, it can aid radiologists’ image interpretations and extract features from medical images, which are not visible for the human eye, giving it a cost-effective potential as well [21]. Still, within the field of gynecologic oncology it is relatively new compared to other medical specialties [22].
In this study, we assess the available literature on CAD in preoperatively predicting the chance of an ovarian malignancy.
Materials and methods
We searched for all published studies investigating diagnostic accuracy of CAD based on ultrasound, CT and MRI in patients with an ovarian tumor. Search terms used were: ‘ovaria,’ ‘ovarian neoplasms,’ ‘ovarian neoplasm,’ ‘ovarian masses,’ ‘ovarian lesion,’ ‘ovarian tumor,’ ‘adnexal,’ ‘adnexal mass,’ ‘ovarian cancer,’ ‘ovarian malignancy,’ ‘ovary,’ ‘classification of ovarian,’ ‘machine learning,’ ‘computer aided,’ ‘Diagnosis Computer-Assisted,’ ‘computer assisted-diagnosis,’ ‘artificial intelligence,’ ‘Neural Networks, Computer,’ ’convolutional neural network,’ ‘radiomics,’ ‘decision support system,’ ‘decision support technique,’ ‘decision support techniques,’ ‘machine learning classifier,’ ‘machine learning classifiers,’ ‘diagnosis,’ ‘diagnostic accuracy,’ ‘presurgical,’ ‘preoperative,’ ‘preoperative diagnosis,’ ‘preoperative evaluation,’ ‘Tomography, X-ray Computed,’ ‘ct-scan,’ ‘ultrasound,’ ‘echography,’ ‘gynecological ultrasound,’ ‘ultrasonography,’ ‘magnetic resonance imaging,’ ‘nuclear magnetic resonance imaging’ and ‘MRI.’ We used ‘title abstract’ (tiab) and ‘Mesh’ added to each search term. The exact search syntax per database is provided in Additional file 1: Appendix 1.
The search was last performed on 9th 2022 by two independent reviewers and a research librarian was consulted for support in this matter.
We searched for papers published in English in Cochrane Central Register of Controlled Trials, MEDLINE, Embase, Scopus and PubMed. Additionally, we searched trial registries for ongoing and registered trials on Clinicaltrials.gov. To identify additional trials, references of all included studies by the initial search were hand searched to add relevant trials.
All studies that investigated diagnostic accuracy of CAD based on ultrasound, CT and MRI images in patients with an adnexal mass were included. Case reports, summaries, animal studies, meta-analyses, comments, editorials, conference abstracts and other irrelevant article types were excluded.
Selection of studies
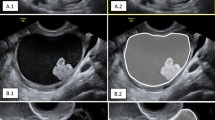
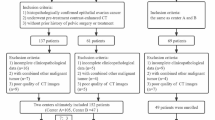
Titles and abstracts retrieved by the search were imported into the reference manager database Covidence [23]. Duplicates were removed and two reviewers independently screened the records. Subsequently, full-text versions of potentially relevant studies were obtained and assessed for eligibility by the same researchers. Studies were qualified if the following criteria were met: (1) accurate disease type, e.g., benign, borderline or malignant ovarian tumors, (2) appropriate clinical setting, for example, no ex vivo studies, (3) description of overfitting techniques and reference standard, (4) use of correct classifier, e.g., none of the features selected to construct the CAD were manually measured, as done by Timmerman et al., Biagiotti et al. or Zimmerman et al. [14,15,16] and (5) diagnostic accuracy had to be reported, namely sensitivity, specificity or area under the curve (AUC). Disagreements were resolved through discussion until consensus was reached, or by consulting a third member of the review team. The selection process was visualized in a PRISMA flowchart (Fig. 1).
PRISMA flowchart [32]
Data extraction and management
Two reviewers independently extracted the following data from each included study: study design, year of publication, country where the study was conducted, inclusion and exclusion criteria or population description, number of participants, menopausal status, mean CA125 serum levels of included participants, number of images, intervention compared to histology, type of classifier and features used to develop the CAD, duration of follow-up, reference standard and results. When multiple classifiers were described, the best performing one was selected. Supplementary appendices were assessed for additional study details and corresponding authors were contacted by email on study details if necessary. Discrepancies were resolved through discussion and consensus, or by consulting a third member of the review team. Study outcomes were type of classifier, whether an external validation set was used, if CAD was compared to or combined with other models or subjective assessment (SA), sensitivity, specificity, accuracy and AUC, when mentioned in the included study. Other diagnostic accuracy values were also considered. We aimed to perform a meta-analysis of the CAD methods that used an external validation set, for which Review Manager (RevMan) software (v5.4.1) and Meta-DiSc software were utilized [24]. Heterogeneity was assessed by using the I2 statistics, which describes the percentage of variability due directly to heterogeneity, with > 50% representing moderate heterogeneity and > 75% indicating high heterogeneity and Moses-Littenberg SROC (summary receiver operating curve) plot [25, 26].
Assessment of risk of bias of included studies
Two independent reviewers assessed the methodological quality of each included study by using the Prediction Model Study Risk of Bias Assessment Tool (PROBAST) together with additional questions from the quality assessment of diagnosis accuracy study (QUADAS-2) tool and the quality in prognostic studies (QUIPS) tool. Discrepancies were resolved through discussion and consensus, or by consulting a third member of the review team. Different risk of bias assessment tools were used because different types of study designs were included. Studies that evaluated multivariable diagnostic or prognostic prediction models were reviewed using PROBAST. PROBAST assesses four key domains: participants, predictors, outcome and analysis. Studies that evaluated diagnostic tests of prognostic factors were reviewed by a few questions from the QUADAS-2 tool and the QUIPS tool [27,28,29,30]. Furthermore, seven signaling questions were composed by independent technical members of the study team to assess risk of bias based on the used CAD model, called ‘CAD model risk of bias screening questions.’ These two members were not aware of the content of the articles included. These signaling questions are described in Additional file 1: Appendix 2.
The signaling questions were used to determine whether risk of bias was low, high or unclear.
The extraction of study data, comparisons in data tables and preparation of a ‘Summary of findings’ table were performed before writing the results and conclusions of this review.
The protocol of this systematic review was registered with PROSPERO (Registration number CRD42020189910).
Results
After the search was performed and cross-reference articles were added, a total of 532 articles were retrieved. Subsequently, duplicates were removed and 331 articles remained for screening on title and abstract. Seventy-one articles were eligible for full-text reading. Two studies on CAD and ovarian tumors were found on ClinicalTrial.gov. Both trials are open for accrual and are using CAD in diagnosing (1) malignant ovarian tumor with CT (NCT05174377) and (2) endometriosis-related ovarian cancer (NCT05161949). Most articles were excluded because they were not using CAD, not assessing ovarian tumors or because a wrong type of classifier was used. A summary of the selection process is shown in a PRISMA flowchart (Fig. 1) [31, 32].
After screening the title, abstract and full-text thirty-one studies were included in this systematic review.
Description of included studies
Thirty-one studies were included in this review, of which twenty-two ultrasound-based studies [33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53, 62], three CT-based studies [54,55,56] and six MRI-based studies [57,58,59,60,61,62]. A detailed overview of the included studies is presented in Additional file 2: Table 1a–c. There were twenty-two retrospective studies of which nineteen are case–control studies and two are cohort studies. Six studies have a prospective case–control design, and one is a cohort study. Women of all ages were included in the studies. Only seven studies used external validation datasets to assess the performance of their classifier: four ultrasound, one CT and two MRI studies [33, 35, 51, 53, 56, 59, 61]. The same dataset was used in ten studies to develop and test different classifiers [43, 45, 49, 50, 52, 54, 56, 59, 61, 62]. In most studies, the region of interest (ROI) was annotated manually. Two studies did not mention histology as definite diagnosis [41, 42]. Only three studies combined CAD with clinical features. Eleven studies compared the CAD with subjective assessment (SA) of a reviewer or combined the CAD model with SA performance of the reviewer [33, 35,36,37,38, 48, 50, 58, 60,61,62]. Table 1a–c presents the results of each study.
In the included studies, fourteen different machine learning modalities were employed: Seventeen were different types of deep machine learning, and the remaining were conventional machine learning. Fourteen studies used classification [34, 39,40,41,42,43,44,45,46,47, 50, 51, 53, 63], and remaining studies used segmentation to predict the nature of the ovarian tumor. With classification, a class label (e.g., benign or malignant) is predicted by analyzing its input, which is often numerical data (e.g., images). With segmentation, each pixel in an image is assigned to a predefined category (e.g., malignant or non-malignant), whereby certain image characteristics are shared by pixels with identical labels [64]. The input for the segmentation studies was usually different types of grayscale patterns, e.g., gray-level size zone matrix or wavelet features. The input for the classification studies was global images with or without clinical variables added.
Pooling of diagnostic accuracy
A meta-analysis on the seven studies that used an external validation set to test their CAD model was attempted; however, due to heterogeneity, missing diagnostic accuracy rates and unclear data, this could not be executed [33, 35, 51, 53, 56, 59, 61]. An additional sub-analysis of studies using CAD on ultrasound imaging was performed, which showed great heterogeneity as well. The remaining twenty-four studies without an independent validation per imaging modality were not pooled due to heterogeneity at forehand.
Risk of bias in studies per imaging modality
A general overview of risk of bias of per imaging modality of the included studies is presented in the ‘Risk of bias’ summary (Table 2a–c).
Ultrasound:
Participants
Risk of bias based on selection of participants was considered low in ten studies. In five studies, risk of selection bias was unclear, because inclusion of participants was not clearly described. Seven studies were graded with high risk of selection bias because they described neither little information about baseline patient characteristics nor inclusion or exclusion criteria.
Predictors
Risk of bias based on predictors was considered low for twenty studies, because predictors were defined and assessed in the same way for all participants and predictor assessments were made before results were known. For two studies, this was unclear due to missing information on this matter.
Outcome
Risk of bias based on outcome or its determination was considered low for eightteen studies, because in these studies the outcome was predetermined appropriately. Risk of bias was scored unclear in in one study, because there was no clear description of the reference standards used and high in three studies, since reference standards were not described.
Analysis
Risk of bias based on analysis was considered low for eight studies, because analysis was properly performed. In three studies, risk of bias based on analysis was unclear, because analysis was not clearly described. Eleven studies described very little of the analysis process, and therefore, these studies were considered containing high risk of bias.
CAD model
Risk of bias based on CAD model bias screening questions was considered low in four studies. In nine studies, the risk of bias based on CAD model bias screening questions was assessed as unclear, because it was unclear how overfitting mitigation techniques and cross-validation were used or if the data were reproducible or validated in other centers. Risk of bias based on CAD model bias screening questions was reckoned high in nine studies. This was due to overfitting mitigation techniques which were not used or incorrectly used, the training set was not independent from the test set or did not have enough power, or no cross-validation was used and data were not reproducible or not validated in other settings.
CT and MRI
Participants
Risk of bias based on selection of participants was considered low in all nine studies, because of transparent description of patient selection.
Predictors
Risk of bias based on predictors was regarded low for eight studies, because the researchers were clear on how predictors were determined and characterized before outcome was known. Only one study reported that the outcome was known at forehand when assessing the predictors.
Outcome
Risk of bias based on outcome or its determination was considered low for eight studies, because it was predetermined appropriately. For one study, this was high because outcome differed among participants.
Analysis
Risk of bias based on analysis was considered low for six studies, because analysis was accurately carried out. In two studies, risk of bias based on analysis was high, because analysis was not properly performed. In one study, the sub-results were inconclusive and therefore the study was considered containing an unclear risk of bias.
CAD model
Risk of bias based on CAD model bias screening questions was assessed low in six studies. In three studies, risk of bias based on CAD model bias screening questions was considered unclear, because the use of overfitting mitigation techniques was not mentioned or they were not executed correctly, and it was unclear if executed correctly it was unclear if the dataset was reproducible or validated in other settings.
Discussion
This systematic review shows numerous studies that use CAD to assess the nature of an ovarian tumor. Due to the large heterogeneity, we were not able to pool data. However, highest performance as measured by AUC was seen in both CT- and MRI-based CAD models.
A meta-analysis was endeavored for the seven studies that used an external dataset for validation. However, this could not be executed for multiple reasons. One study, describing a CAD-MRI model for differentiating borderline from malignant ovarian tumors, only mentioned the sensitivity and specificity for radiologists’ performance and for the model only the AUC [61]. Another study was unclear about which data were used to calculate the diagnostic performance of their model [56]. Consequently, for both studies it was not possible to calculate diagnostic accuracy rates, such as true positive (TP), true negative (NT) values and to use them in the meta-analysis.
For the five remaining studies, heterogeneity proved to be too large with an I2 of 92.8% and 90.7%. In an additional subgroup analysis of only ultrasound CAD models, this was also apparent with an I2 of 94.3% and 83.5%. These analyses can be found in Additional file 1: Appendix 3. This heterogeneity can be explained by (1) different types of CAD models using either conventional or deep learning techniques, (2) different inclusion and exclusion criteria and (3) type of imaging modality used. Among the twenty-four studies without an independent dataset, pooling of the results was not viable since the data were too diverse. This was illustrated by differences in imaging techniques used, e.g., 2D or 3D ultrasound and CT, or 2D, 3D or pharmacokinetic MRI. Furthermore, different CAD techniques were applied, e.g., conventional and deep learning machine learning models. Moreover, some studies combined clinical features such as patients’ age, menopausal status or serum CA125 to support the classifiers. Finally, different outcome measurements per classifier were found, such as benign, malignant and borderline in combination with a different tumor subtype, such as mucinous ovarian tumors.
All studies assessed computer-aided diagnostics based on machine learning. We found that classifying the nature of an ovarian tumor by CAD on ultrasound images results in sensitivities of 40.3% to 100% and specificities of 76.3% to 100%. For CT, sensitivities of 84.6% to 100% and specificities of 69% to 100% were described. For MRI, sensitivities and specificities ranged between 66.7% and 100% and 77.8% and 100%, respectively. Even though some studies report high performances, they are at risk for overfitting due to the lack of an independent test set. Twenty-three studies lacked an independent test set for evaluating model performance.
With conventional machine learning techniques, features extracted from medical imagery are used to optimize a mathematical model for predicting new, unseen data. A model should be built based on a training set of images and validated in a test set. If the model is too tightly fitted to the training data and does not generalize toward new data, it is called overfitting. Overfitting occurs more often with conventional machine learning, where many parameters are hand-selected instead of being learned from the data, especially when the model is not validated on an independent test set [64].
Ultrasound
Earlier published studies assessing ultrasound prediction models show reasonable sensitivity (72–77%) and specificity (85–89%) for the RMI [65, 66]. An external validation of the IOTA ADNEX model showed a better performance, with a sensitivity of 98% (95% CI 93–100%), but with low specificity of 62% at a cutoff value for malignancy of 10% (95% CI 55%–68%) [5]. The GI-RADs and the O-RADs perform better with a sensitivity of 92.7% and 93.6% and a specificity of 97.5% and 92.8%, subsequently [6]. However, all these models depend on specific terminology and expertise of their users. Furthermore, interpretation of ultrasound imaging regarding ovarian tumors has shown to be difficult for novel clinicians and for clinicians who do not perform ultrasonography on a regular basis [8, 9]. Based on the amount of studies included in this review assessing the CAD technique for ultrasound, CAD can be a promising tool to aid clinicians in determining the origin of ovarian tumors. Moreover, when comparing CAD models’ performances with experienced clinicians or existing models they achieve similar or even better diagnostic accuracy. Nevertheless, this performance comparison was performed in only three studies. Even though overfitting mitigation techniques were applied in twenty-one ultrasound studies, only four studies used external validation. Thus, a high risk of overfitting is present, which could lead to an unreliable performance.
CT
The diagnostic performance of CT in preoperatively classifying the origin of an ovarian tumor is primary known for multidetector computer tomography (MDCT), with a diagnostic accuracy of 90–93% [11]. Therefore, no fair comparison on CAD for CT can be made. However, the performance of CAD for CT is indeed promising based on the included studies in this review. The models show a high diagnostic accuracy and low selection bias. Nonetheless, only three studies in total assessed CAD for CT of which only one study utilized an independent validation, thus risking overfitting.
For CAD on CT scans, more research is needed to further evaluate its potential benefits.
MRI
The diagnostic accuracy for MRI in ovarian tumor classification has a sensitivity and specificity of 96% and 91%, respectively [7, 9]. For the O-RADs MRI score, this is comparable with a sensitivity of 93% and a specificity of 91% and it shows a similar performance among junior and senior radiologists (κ = 0.784; 95% CI, 0.743–0824) [9, 10]. CAD for MRI as an additional diagnostic method for ovarian tumors has the potential to aid radiologists due to its high diagnostic performance as a single model or when compared to SA of radiologists. However, caution is needed when using MRI-CAD as a supplementary tool. First, due to the absence of international guidelines when to conduct an MRI for ovarian tumors classification a selection bias is being created. Moreover, the performance of the MRI has no further clinical consequences for the patient. However, if radiologists are trained with MRI O-RADs classification model, the usage of MRI can have an additional beneficial effect on ovarian tumor classification, especially when classifying benign and or possibly malignant lesions [67]. However, for the O-RADs MRI familiarity and expertise are essential to use the scoring system [7, 10].
Second, only one out of six studies showed a low overall risk of bias on using MRI CAD [59]. Unfortunately, the authors did not compare their CAD to ovarian tumor characterization by radiologists or to other models, such as the O-RADs model. Hence, one study alone cannot support clinical implementation of MRI CAD. Moreover, although in three studies CAD outperformed the radiologists’ performance, no external validation sets were used in these studies and risk of bias was mostly unclear [58, 59, 60, 61]. Furthermore, only two of the six studies used an external validation set [59, 61]. Another study used 3D MRI for their model building, showing good results; however, this is a rather expensive MRI technique [57]. Finally, two studies used the same dataset. Therefore, only limited evidence to support the usage of MRI-CAD additionally is available [59, 63].
Hence, more studies should be undertaken with external validation sets in order to be able to implement these CAD-MRI models in clinical practice.
Trends among publications
Over the last three decades, different trends among included studies in the CAD field are observed.
An increasing number of publications presented clear inclusion and exclusion criteria for data before using it to construct a CAD model [33,34,35,36,37,38,39, 44, 48,49,50, 52, 54,55,56,57,58,59,60,61,62,63]. In addition, more studies used statistical tests to select the most promising features to include into the CAD model and in most articles this was precisely described [34, 37, 41, 43,44,45,46, 48,49,50,51, 54,55,56,57,58, 60,61,62,63]. Furthermore, study cohorts became substantially larger [33]. Finally, clinicians are more involved in the CAD model construction, e.g., for the delineation of the images. Thus, uniformity among studies is improved, making studies more comparable.
Regarding the outcomes, almost all studies used the same outcome measurements, i.e., sensitivity, specificity, accuracy and area under the curve (AUC). More connection with the clinical setting is observed. In particular, the comparison of the CAD model to either assessment of scans by clinicians such as radiologists, sonographists or gynecologists or to commonly used models in ultrasound (RMI or LR1-2) is now included [33, 35,36,37,38, 48, 51, 60, 61, 68].
Hence, the difficult technical matter of a CAD model development is made more comprehensible for clinicians.
Finally, more deep learning models have been developed in recent years, showing the potential of this new type of CAD. If these trends continue, it could substantially contribute to patient care.
Previous studies have shown that depending on the imaging technique used the interobserver agreement is low for many features and are prone to contain significant measurement errors when used by inexperienced clinicians. Therefore, more uncertainties in measured features within these imaging techniques can lead to diminished accuracies of a model. It is therefore important to develop new techniques with less inter- and intra-observer variability to reach higher test performances to prevent unnecessary referrals to tertiary centers and unnecessary stress for the patient. Based on this literature review, computer-aided ultrasound, CT and MRI techniques based on different (deep) neural networks and conventional machine learning techniques such as support vector machines are promising. They can either be used as a single entity or combined with SA or with other prediction models. They could potentially offer a noninvasive and cost-effective method in the future. However, this is only shown in eight studies of which five are ultrasound studies and three MRI studies. Of these studies, four used independent validation sets, of which three within ultrasound CAD and one within an MRI CAD. For the remaining studies, lack of a validation cohort might cause a high risk of overfitting. The CT CAD models seem to perform fairly but they consist of small datasets and are in the absence of a SA and only one study used an external validation set; therefore, risk of overfitting is present.
Furthermore, CAD as a technique within the gynecology–oncology is slowly gaining field in comparison with other oncology specialties. Combining datasets with larger test sets is needed in prospective cohorts [22, 33, 69].
It is likely that deep learning in assessing the nature of an ovarian tumor will reach higher test performances than traditional machine learning. For MRI and CT, the number of studies in this review is limited and needs to be broadened [22].
Strengths and weaknesses
To the best of our knowledge, this is the most comprehensive review on computer-aided diagnostics for differentiating benign from borderline and malignant ovarian tumors on ultrasound, MRI and CT scans. We have worked by a clearly defined protocol that was first submitted to PROSPERO, to provide transparency in the review process and avoid reporting bias. There was no substantial disagreement in inclusion of articles by the authors, and this can be regarded as a strong point in the review process. A meta-analysis of the studies with an external validation set was attempted. A limitation of this review is the heterogeneity between studies, the lack of independent validation sets and comparison with SA.
Conclusions
In conclusion, this review shows that CAD certainly has potential as a noninvasive model to preoperatively predict whether an ovarian tumor is benign, borderline or malignant and thus can aid the physician with assessment of ovarian tumors. However, this depends on the type of imaging modality assessed and thus should be evaluated per imaging technique. CAD for CT displays the best performance overall. However, the three studies included are all lacking an external validation. The results of CAD for MRI were similar; however, more studies used external validation to test their CAD. Nevertheless, the risk of bias for the domain ‘CAD model’ for half of the studies was found to be unclear. Furthermore, it is important to take into account that MRI is clinically less relevant for detecting and classifying ovarian tumors. Finally, most research has been done on CAD for ultrasound, of which the results are reasonable in comparison with existing models, but has limited external validation and risks overfitting. Moreover, included studies per image modality show great heterogeneity, and thus, results most likely cannot be generalized to other data.
Studies in which all methods are validated in the same population should be performed in order to prove which techniques demonstrate the best diagnostic performance. Above all, it is important that new CAD techniques are tested and validated with an independent, prospectively collected dataset.
Future perspectives
In the near future, it is likely that CAD will facilitate diagnostics and will be used as a decision support system by clinicians, depending on the imaging modality the CAD is developed for. The performance of CAD for discriminating the nature of an ovarian tumor on CT and MRI is good, and studies assessing these two imaging techniques show a low risk of bias. Consequently, a majority of research should focus on these two imaging modalities. Particularly, since both MRI and CT are more standardized than ultrasound imaging and therefore more suitable for CAD development. However, it should be taken into account that MRI is less clinically relevant in diagnosing ovarian tumors. In addition, in order to increase accuracy, CAD for CT or MRI could be combined with clinical markers, e.g., menopausal age or liquid biopsies, such as circulating cell free tumor DNA (ct-DNA). Implementation of CAD for ultrasound in clinical practice will presumably take longer due to the dynamic character of this imaging method and the high and unclear risk of bias.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- ADNEX model:
-
Assessment of different NEoplasias in the adneXa
- CA125:
-
Cancer antigen 125
- CAD:
-
Computer-aided diagnostics
- CT:
-
Computer tomography
- ct-DNA:
-
Circulating cell-free tumor DNA
- GI-RADs:
-
Gynecologic imaging reporting and data system for diagnosis of adnexal masses (AMs) by pelvic ultrasound (US)
- MDCT:
-
Multidetector computer tomography
- MRI:
-
Magnetic resonance imaging
- O-RADs:
-
Ovarian-adnexal reporting and data system
- PROBAST:
-
Prediction Model Study Risk of Bias Assessment Tool
- QUADAS-2:
-
Quality Assessment of Diagnosis Accuracy Study
- QUIPS:
-
Quality in prognostic studies
- RMI:
-
Risk of malignancy index
- ROI:
-
Region of interest
- SA:
-
Subjective assessment
- SROC:
-
Summary receiver operating curve
- TP:
-
True positive
- TN:
-
True negative
References
Geomini PM, Kruitwagen RF, Bremer GL, Massuger L, Mol BW (2011) Should we centralise care for the patient suspected of having ovarian malignancy? Gynecol Oncol 122(1):95–99. https://doi.org/10.1016/j.ygyno.2011.03.005
Jacobs I, Oram D, Fairbanks J, Turner J, Frost C, Grudzinskas JG (1990) A risk of malignancy index incorporating CA 125, ultrasound and menopausal status for the accurate preoperative diagnosis of ovarian cancer. Br J Obstet Gynaecol 97:922–929. https://doi.org/10.1111/j.1471-0528.1990.tb02448.x
Van Calster B, Van Hoorde K, Valentin L et al (2014) Evaluating the risk of ovarian cancer before surgery using the ADNEX model to differentiate between benign, borderline, early and advanced stage invasive, and secondary metastatic tumours: prospective multicentre diagnostic study. BMJ 349:g5920. https://doi.org/10.1136/bmj.g5920
Van Calster B, Valentin L, Froyman W et al (2020) Validation of models to diagnose ovarian cancer in patients managed surgically or conservatively: multicentre cohort study. BMJ 370:m2614. https://doi.org/10.1136/bmj.m2614
Meys EMJ, Jeelof LS, Achten NMJ et al (2017) Estimating risk of malignancy in adnexal masses: external validation of the ADNEX model and comparison with other frequently used ultrasound methods. Ultrasound Obstet Gynecol 49(6):784–792. https://doi.org/10.1002/uog.17225
Basha MAA, Metwally MI, Gamil SA et al (2021) Comparison of O-RADS, GI-RADS, and IOTA simple rules regarding malignancy rate, validity, and reliability for diagnosis of adnexal masses. Eur Radiol 31(2):674–684. https://doi.org/10.1007/s00330-020-07143-7
Timmerman D, Planchamp F, Bourne T et al (2021) ESGO/ISUOG/IOTA/ESGE Consensus Statement on pre-operative diagnosis of ovarian tumors. Int J Gynecol Cancer 31(7):961–982. https://doi.org/10.1136/ijgc-2021-002565
Meys E, Rutten I, Kruitwagen R, et al. Simple Rules, Not So Simple: The Use of International Ovarian Tumor Analysis (IOTA) Terminology and Simple Rules in Inexperienced Hands in a Prospective Multicenter Cohort Study. Ultraschall Med. 2017;38(6):633–641. "Simple Rules" - nicht so einfach: Anwendung der "International Ovarian Tumor Analysis" (IOTA)- Terminologie und der "Simple Rules" in unerfahrenen Handen in einer prospektiven multizentrischen Kohortenstudie. doi:https://doi.org/10.1055/s-0043-113819
Shimada K, Matsumoto K, Mimura T et al (2018) Ultrasound-based logistic regression model LR2 versus magnetic resonance imaging for discriminating between benign and malignant adnexal masses: a prospective study. Int J Clin Oncol 23(3):514–521. https://doi.org/10.1007/s10147-017-1222-y
Thomassin-Naggara I, Poncelet E, Jalaguier-Coudray A et al (2020) Ovarian-adnexal reporting data system magnetic resonance imaging (O-RADS MRI) score for risk stratification of sonographically indeterminate adnexal masses. JAMA Netw Open. 3(1):e1919896. https://doi.org/10.1001/jamanetworkopen.2019.19896
Mukhtar S, Khan SA, Hussain M, Adil SO (2017) Role of multidetector computed tomography in evaluation of ovarian lesions in women clinically suspected of malignancy. Asian Pac J Cancer Prev 18(8):2059–2062. https://doi.org/10.22034/apjcp.2017.18.8.2059
Walker SP, The ROC (2019) Curve redefined—optimizing sensitivity (and specificity) to the lived reality of cancer. N Engl J Med 380(17):1594–1595. https://doi.org/10.1056/NEJMp1814951
Lange RT, Lippa SM (2017) Sensitivity and specificity should never be interpreted in isolation without consideration of other clinical utility metrics. Clin Neuropsychol 31(6–7):1015–1028. https://doi.org/10.1080/13854046.2017.1335438
Biagiotti R, Desii C, Vanzi E, Gacci G (1999) Predicting ovarian malignancy: application of artificial neural networks to transvaginal and color Doppler flow US. Radiology 210(2):399–403. https://doi.org/10.1148/radiology.210.2.r99fe18399
Timmerman D, Verrelst H, Bourne TH et al (1999) Artificial neural network models for the preoperative discrimination between malignant and benign adnexal masses. Ultrasound Obstet Gynecol 13(1):17–25. https://doi.org/10.1046/j.1469-0705.1999.13010017.x
Zimmer Y, Tepper R, Akselrod S (1999) Computerized quantification of structures within ovarian cysts using ultrasound images. Ultrasound Med Biol 25(2):189–200. https://doi.org/10.1016/s0301-5629(98)00150-1
Chilamkurthy S, Ghosh R, Tanamala S et al (2018) Deep learning algorithms for detection of critical findings in head CT scans: a retrospective study. Lancet 392(10162):2388–2396. https://doi.org/10.1016/s0140-6736(18)31645-3
Esteva A, Kuprel B, Novoa RA et al (2017) Dermatologist-level classification of skin cancer with deep neural networks. Nature 542(7639):115–118. https://doi.org/10.1038/nature21056
Ehteshami Bejnordi B, Veta M, Johannes van Diest P et al (2017) Diagnostic assessment of deep learning algorithms for detection of lymph node metastases in women with breast cancer. JAMA 318(22):2199–2210. https://doi.org/10.1001/jama.2017.14585
Lakhani P, Sundaram B (2017) Deep learning at chest radiography: automated classification of pulmonary tuberculosis by using convolutional neural networks. Radiology 284(2):574–582. https://doi.org/10.1148/radiol.2017162326
Lambin P, Leijenaar RTH, Deist TM et al (2017) Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol 14(12):749–762. https://doi.org/10.1038/nrclinonc.2017.141
Mysona DP, Kapp DS, Rohatgi A et al (2021) Applying artificial intelligence to gynecologic oncology: a review. Obstet Gynecol Surv 76(5):292–301. https://doi.org/10.1097/ogx.0000000000000902
Veritas Health Innovation M, Australia. Covidence systematic review software. website. Covidence systematic review software, Veritas Health Innovation. Updated 2022. Accessed 09–05–2022, https://www.covidence.org/
Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A (2006) Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 6:31. https://doi.org/10.1186/1471-2288-6-31
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Moses LE, Shapiro D, Littenberg B (1993) Combining independent studies of a diagnostic test into a summary ROC curve: data-analytic approaches and some additional considerations. Stat Med 12(14):1293–1316. https://doi.org/10.1002/sim.4780121403
Wolff RF, Moons KGM, Riley RD et al (2019) PROBAST: a tool to assess the risk of bias and applicability of prediction model studies. Ann Intern Med 170(1):51–58. https://doi.org/10.7326/m18-1376
Moons KGM, Wolff RF, Riley RD et al (2019) PROBAST: a tool to assess risk of bias and applicability of prediction model studies: explanation and elaboration. Ann Intern Med 170(1):W1–W33. https://doi.org/10.7326/M18-1377
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C (2013) Assessing bias in studies of prognostic factors. Ann Intern Med 158(4):280–286. https://doi.org/10.7326/0003-4819-158-4-201302190-00009
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 339:b2535. https://doi.org/10.1136/bmj.b2535
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Gao Y, Zeng S, Xu X et al (2022) Deep learning-enabled pelvic ultrasound images for accurate diagnosis of ovarian cancer in China: a retrospective, multicentre, diagnostic study. Lancet Digit Health 4(3):e179–e187. https://doi.org/10.1016/s2589-7500(21)00278-8
Chiappa V, Bogani G, Interlenghi M et al (2021) The Adoption of Radiomics and machine learning improves the diagnostic processes of women with Ovarian MAsses (the AROMA pilot study). J Ultrasound 24(4):429–437. https://doi.org/10.1007/s40477-020-00503-5
Chiappa V, Interlenghi M, Bogani G et al (2021) A decision support system based on radiomics and machine learning to predict the risk of malignancy of ovarian masses from transvaginal ultrasonography and serum CA-125. Eur Radiol Exp. 5(1):28. https://doi.org/10.1186/s41747-021-00226-0
Christiansen F, Epstein EL, Smedberg E, Akerlund M, Smith K, Epstein E (2021) Ultrasound image analysis using deep neural networks for discriminating between benign and malignant ovarian tumors: comparison with expert subjective assessment. Ultrasound Obstet Gynecol 57(1):155–163. https://doi.org/10.1002/uog.23530
Qi L, Chen D, Li C et al (2021) Diagnosis of ovarian neoplasms using nomogram in combination with ultrasound image-based radiomics signature and clinical factors. Front Genet 12:753948. https://doi.org/10.3389/fgene.2021.753948
Wang H, Liu C, Zhao Z et al (2021) Application of deep convolutional neural networks for discriminating benign, borderline, and malignant serous ovarian tumors from ultrasound images. Front Oncol. https://doi.org/10.3389/fonc.2021.770683
Martinez-Mas J, Bueno-Crespo A, Khazendar S et al (2019) Evaluation of machine learning methods with Fourier Transform features for classifying ovarian tumors based on ultrasound images. PLoS One 14(7):e0219388. https://doi.org/10.1371/journal.pone.0219388
Zhang L, Huang J, Liu L (2019) Improved deep learning network based in combination with cost-sensitive learning for early detection of ovarian cancer in color ultrasound detecting system. J Med Syst. 43(8):251. https://doi.org/10.1007/s10916-019-1356-8
Acharya UR, Akter A, Chowriappa P et al (2018) Use of nonlinear features for automated characterization of suspicious ovarian tumors using ultrasound images in fuzzy forest framework. Int J Fuzzy Syst 20(4):1385–1402. https://doi.org/10.1007/s40815-018-0456-9
Acharya UR, Mookiah MR, Vinitha Sree S et al (2014) Evolutionary algorithm-based classifier parameter tuning for automatic ovarian cancer tissue characterization and classification. Ultraschall Med 35(3):237–245. https://doi.org/10.1055/s-0032-1330336
Acharya UR, Sree SV, Krishnan MM et al (2012) Ovarian tumor characterization using 3D ultrasound. Technol Cancer Res Treat 11(6):543–552. https://doi.org/10.7785/tcrt.2012.500272
Acharya UR, Sree SV, Kulshreshtha S et al (2014) GyneScan: an improved online paradigm for screening of ovarian cancer via tissue characterization. Technol Cancer Res Treat 13(6):529–539. https://doi.org/10.7785/tcrtexpress.2013.600273
Acharya UR, Sree SV, Saba L, Molinari F, Guerriero S, Suri JS (2013) Ovarian tumor characterization and classification using ultrasound-a new online paradigm. J Digit Imaging 26(3):544–553. https://doi.org/10.1007/s10278-012-9553-8
Aramendia-Vidaurreta V, Cabeza R, Villanueva A, Navallas J, Alcazar JL (2016) Ultrasound image discrimination between benign and malignant adnexal masses based on a neural network approach. Ultrasound Med Biol 42(3):742–752. https://doi.org/10.1016/j.ultrasmedbio.2015.11.014
Khazendar S, Sayasneh A, Al-Assam H et al (2015) Automated characterisation of ultrasound images of ovarian tumours: the diagnostic accuracy of a support vector machine and image processing with a local binary pattern operator. Facts Views Vis Obgyn 7(1):7–15
Faschingbauer F, Beckmann MW, Weyert Goecke T et al (2013) Automatic texture-based analysis in ultrasound imaging of ovarian masses. Ultraschall Med 34(2):145–150. https://doi.org/10.1055/s-0031-1299331
Vaes E, Manchanda R, Autier P et al (2012) Differential diagnosis of adnexal masses: sequential use of the risk of malignancy index and HistoScanning, a novel computer-aided diagnostic tool. Ultrasound Obstet Gynecol 39(1):91–98. https://doi.org/10.1002/uog.9079
Vaes E, Manchanda R, Nir R et al (2011) Mathematical models to discriminate between benign and malignant adnexal masses: potential diagnostic improvement using ovarian HistoScanning. Int J Gynecol Cancer 21(1):35–43. https://doi.org/10.1097/IGC.0b013e3182000528
Lu C, Van Gestel T, Suykens JA, Van Huffel S, Vergote I, Timmerman D (2003) Preoperative prediction of malignancy of ovarian tumors using least squares support vector machines. Artif Intell Med 28(3):281–306. https://doi.org/10.1016/s0933-3657(03)00051-4
Lucidarme O, Akakpo JP, Granberg S et al (2010) A new computer-aided diagnostic tool for non-invasive characterisation of malignant ovarian masses: results of a multicentre validation study. Eur Radiol 20(8):1822–1830. https://doi.org/10.1007/s00330-010-1750-6
Zimmer Y, Tepper R, Akselrod S (2003) An automatic approach for morphological analysis and malignancy evaluation of ovarian masses using B-scans. Ultrasound Med Biol 29(11):1561–1570. https://doi.org/10.1016/j.ultrasmedbio.2003.08.013
Li S, Liu J, Xiong Y et al (2022) Application values of 2D and 3D radiomics models based on CT plain scan in differentiating benign from malignant ovarian tumors. Biomed Res Int 2022:5952296. https://doi.org/10.1155/2022/5952296
Park H, Qin L, Guerra P, Bay CP, Shinagare AB (2021) Decoding incidental ovarian lesions: use of texture analysis and machine learning for characterization and detection of malignancy. Abdom Radiol (NY) 46(6):2376–2383. https://doi.org/10.1007/s00261-020-02668-3
Li S, Liu J, Xiong Y et al (2021) A radiomics approach for automated diagnosis of ovarian neoplasm malignancy in computed tomography. Sci Rep 11(1):8730. https://doi.org/10.1038/s41598-021-87775-x
Liu X, Wang T, Zhang G et al (2022) Two-dimensional and three-dimensional T2 weighted imaging-based radiomic signatures for the preoperative discrimination of ovarian borderline tumors and malignant tumors. J Ovarian Res 15(1):22. https://doi.org/10.1186/s13048-022-00943-z
Song XL, Ren JL, Zhao D, Wang L, Ren H, Niu J (2021) Radiomics derived from dynamic contrast-enhanced MRI pharmacokinetic protocol features: the value of precision diagnosis ovarian neoplasms. Eur Radiol 31(1):368–378. https://doi.org/10.1007/s00330-020-07112-0
Jian J, Li Y, Xia W et al (2021) MRI-based multiple instance convolutional neural network for increased accuracy in the differentiation of borderline and malignant epithelial ovarian tumors. J Magn Reson Imaging. https://doi.org/10.1002/jmri.28008
Zhang H, Mao Y, Chen X et al (2019) Magnetic resonance imaging radiomics in categorizing ovarian masses and predicting clinical outcome: a preliminary study. Eur Radiol 29(7):3358–3371. https://doi.org/10.1007/s00330-019-06124-9
Li Y, Jian J, Pickhardt PJ et al (2020) MRI-based machine learning for differentiating borderline from malignant epithelial ovarian tumors: a multicenter study. J Magn Reson Imaging 52(3):897–904. https://doi.org/10.1002/jmri.27084
Jian J, Xia W, Zhang R et al (2021) Multiple instance convolutional neural network with modality-based attention and contextual multi-instance learning pooling layer for effective differentiation between borderline and malignant epithelial ovarian tumors. Artif Intell Med 121:102194. https://doi.org/10.1016/j.artmed.2021.102194
Ștefan P-A, Lupean R-A, Mihu CM et al (2021) Ultrasonography in the diagnosis of adnexal lesions: the role of texture analysis. Diagnostics 11(5):812
van der Sommen F, de Groof J, Struyvenberg M et al (2020) Machine learning in GI endoscopy: practical guidance in how to interpret a novel field. Gut 69(11):2035–2045. https://doi.org/10.1136/gutjnl-2019-320466
Chacon E, Dasi J, Caballero C, Alcazar JL (2019) Risk of ovarian malignancy algorithm versus risk malignancy index-I for preoperative assessment of adnexal masses: a systematic review and meta-analysis. Gynecol Obstet Invest 84(6):591–598. https://doi.org/10.1159/000501681
Mulder EE, Gelderblom ME, Schoot D, Vergeldt TF, Nijssen DL, Piek JM (2020) External validation of risk of malignancy index compared to IOTA simple rules. Acta Radiol. 62:673–678. https://doi.org/10.1177/0284185120933990
Sadowski EA, Maturen KE, Rockall A et al (2021) Ovary: MRI characterisation and O-RADS MRI. Br J Radiol 94(1125):20210157. https://doi.org/10.1259/bjr.20210157
Song H, Bak S, Kim I et al (2021) An application of machine learning that uses the magnetic resonance imaging metric, mean apparent diffusion coefficient, to differentiate between the histological types of ovarian cancer. J Clin Med 11(1):229. https://doi.org/10.3390/jcm11010229
Forstner R (2020) Early detection of ovarian cancer. Eur Radiol 30(10):5370–5373. https://doi.org/10.1007/s00330-020-06937-z
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Contributions
JMJP and JN contributed to conceptualization; CLPM, NMK, JL and JMJP were involved in protocol finalization; CLPM and TB contributed to bias screening questions; TB and FvdS were involved in technical contributions; AHK, TAG, NMK, LJ and JMJP contributed to article selection; JMJP was involved in article consensus; AHK, CLPM and LJ contributed to manuscript writing; AHK and TAG were involved in visualization; CLPM, LJ and JMJP contributed to writing—review and editing; JMJP and FvdS were involved in supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Appendix 1. Search syntax. Appendix 2. Signaling questions. Appendix 3. Meta-analysis results.
Additional file 2
. Tables 1a–c.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koch, A.H., Jeelof, L.S., Muntinga, C.L.P. et al. Analysis of computer-aided diagnostics in the preoperative diagnosis of ovarian cancer: a systematic review. Insights Imaging 14, 34 (2023). https://doi.org/10.1186/s13244-022-01345-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-022-01345-x