Abstract
Background
Activated phosphoinositide3-kinase (PI3K) δ syndrome 1 (APDS1) is a novel inborn errors of immunity (IEIs) caused by heterozygous gain of function mutations in PI3Kδ catalytic p110δ (PIK3CD). APDS1 has a spectrum of clinical manifestations. Recurrent respiratory infections, lymphoproliferation, hepatosplenomegaly, hyper-IgM syndrome and autoimmunity are the common symptoms of this disease.
Case Presentation
Patient 1 presented with recurrent respiratory infections, hepatosplenomegaly and hyper-IgM syndrome. Patient 2 developed early onset systemic lupus erythematosus (SLE)-like disease with resistant thrombocytopenia. c.3061 G > A and c.2314G > A variants in the PIK3CD gene were detected by whole exome sequencing in two patients respectively. c.2314G > A variant in PIK3CD gene of patient 2 is a newly report. After genetic diagnosis, two patients received sirolimus treatment and sirolimus alleviated clinical manifestations, including hepatosplenomegaly in patient 1 and thrombocytopenia in patient 2.
Conclusion
Genetics diagnosis should be considered in patients with complicated clinical manifestations with no or insufficient response to the conventional therapies. If whole exome sequencing suggests a variant in PIK3CD gene, sirolimus may relieve hepatosplenomegaly and resistant thrombocytopenia. This is the first report of c.2314G > A variant in PIK3CD gene.
Similar content being viewed by others
Background
Human inborn errors of immunity (IEIs) are rare diseases caused by damaging genetic variants. IEI can be dominant or recessive, autosomal or X-linked inheritance, and the clinical phenotype can be complete or incomplete penetrance. The main clinical manifestations of these rare diseases are susceptibility to infection, as well as combining with autoimmune, autoinflammatory, allergic and/or malignant diseases. They now comprise 485 genetic disorders listed in the 2022 International Union of Immunological Societies (IUIS) classical classification [1].
Activated phosphoinositide3-kinase-δ (PI3Kδ) syndrome (APDS) is a recently reported IEI. PI3K molecules are composed of a p110 catalytic subunit and a regulatory subunit. Autosomal dominant gain-of-function (GOF) mutation in the PIK3CD gene encoding the PI3Kδ catalytic subunit p110δ cause APDS1, whereas autosomal dominant loss-of-function (LOF) mutation in the PIK3R1 gene encoding the regulatory subunit p85α cause APDS2 [2]. The hyperactivation of PI3Kδ results in the activation of the AKT-mTOR pathway, which further phosphorifies AKT and ribosomal S6 kinases in lymphocytes. The hyperactivated PI3K-AKT-mTOR pathway leads to functional defects of B lymphocytes, T lymphocytes and natural killer (NK) cells [3,4,5]. APDS1 patients develop a wide spectrum of clinical phenotypes, including recurrent respiratory tract infections, chronic epstein barr virus (EBV) and/or cytomegalovirus (CMV) viremia, benign lymphoproliferation, increased risk of lymphoma and autoimmunity [6]. Immunological features of these patients include low/normal serum level of immunoglobulin A (IgA) and IgG, normal or increased IgM [7], reduced class-switched memory B cells and CD4+ lymphopenia [8].
To date, 12 different activating missense mutations of PIK3CD gene have been revealed in APDS1, such as c.3061G > A, c.1002C > A, c.1246 T > C, c.1573G > A, and et al., of which c.3061G > A appears to be the most prevalent, accounting for approximately 85% [9,10,11,12,13]. Herein, we presented the clinical features and genotypes of two pediatric patients to show the diversity of APDS1 and to discuss the effect of sirolimus in curing APDS1. Especially, a novel variant in PIK3CD was reported.
Case presentation
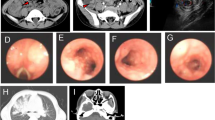
Patient 1 was a 1 year and 5 months old male that presented with hepatosplenomegaly for more than one year and vomiting and diarrhea for one week. The medical history included recurrent respiratory tract infections, but no recurrent abdominal pain or diarrhea. When admitted to our hospital, the patient weighed 8.5 kg (< 3rd percentile) and had enlarged axilla lymph nodes. Abdominal ultrasonography showed hepatosplenomegaly, such that the liver was 2 cm below the right subcostal and the spleen was 3 cm below the umbilicus. Complete blood count values were as follows: white blood cells (WBC) 6.27 × 109/L (normal, 4–10 × 109/L), hemoglobin (Hb) 109 g/L (normal, 110–140 g/L), platelets (PLT) 76 × 109/L (normal, 85–303 × 109/L), and C-reactive protein (CRP) 3.04 mg/L (normal, 0–8 mg/L). Immunological values were as follows: CD3 919/μl (normal, 744–879/μl), CD4 422/μl (normal, 349–469/μl), CD8 496/μl (normal, 240–341/μl), CD4/CD8 0.9 (normal, 1.0–1.9), and CD19 61/μl (normal, 85–211/μl). Serum IgG, A, and M levels were 3.75 g/L (normal, 3.82–10.58 g/L), 0.8 g/L (normal, 0.14–1.14 g/L), and 1.59 g/L (normal, 0.4–1.28 g/L), respectively (Table 1). The EBV and CMV DNA load in the plasma were negative. Bone marrow biopsy excluded the possibility of malignancy. Computed tomography (CT) findings showed enlargement of multiple axilla nodes and hepatosplenomegaly. The whole exome sequencing of venous blood was performed on the child and his parents. A heterozygous missense mutation c.3061G > A (p.E1021K, Fig. 1, Table 2) of PIK3CD gene was revealed in this patient and his mother. His mother has not any clinical symptoms. After treatment with piperacillin and glucocorticoids for one week, symptoms of vomiting and diarrhea improved, but hepatosplenomegaly persisted. Subsequently, sirolimus (1 mg/m2) was started and sirolimus levels were maintained around 5.6–6.2 ng/mL. During follow-up, diarrheal episodes decreased, body weight increased, and hepatosplenomegaly significantly improved. However, the low IgG level and high IgM level have not fully recovered. Other serious adverse events were not noted.
Patient 2 was a 4-month-old male that presented with coughing for two days. He had a history of recurrent respiratory tract infections since birth. Complete blood count values were as follows: WBC 10.46 × 109/L (normal, 4–10 × 109/L), Hb 117 g/L (normal, 110–140 g/L), PLT 10 × 109/L (normal, 85–303 × 109/L), and CRP 0.81 mg/L (normal, 0–8 mg/L). Immunological values were as follows: CD3 3749/μl (normal, 4275–5056/μl), CD4 1614/μl (normal, 2008–2695/μl), CD8 1647/μl (normal, 1381–1961/μl), CD4/CD8 1.00 (normal, 1.0–1.9), and CD19 1427/μl (normal, 487–1214/μl). Serum IgG, A, and M levels were 13.31 g/L (normal, 3.22–7.18 g/L), 0.44 g/L (normal, 0.13–0.35 g/L), and 1.96 g/L (normal, 0.23–0.91 g/L), respectively. Serum C3 and C4 were 0.60 g/L (normal, 0.79–1.52 g/L) and 0.01 g/L (normal, 0.16–0.38 g/L), respectively (Table 1). Coombs test was positive, antinuclear antibodies (ANA) were positive (1:1000), and anti-dsDNA showed negative. The EBV and CMV DNA load in the plasma were negative. After treatment with glucocorticoids (1 mg/kg) and immunoglobulin (2 g/kg), significant improvement of thrombocytopenia and respiratory infections were noted after five months. However, over the next year, the patient was hospitalized twice for thrombocytopenia and was given tacrolimus (0.5 g, qd) and mycophenolate mofetil (0.25 g, bid) orally during treatment. Four months ago, the patient was referred to our clinic for thrombocytopenia again. Complete blood count values were as follows: WBC 8.36 × 109/L (normal, 4–10 × 109/L), Hb 112 g/L (normal, 120–140 g/L), PLT 5 × 109/L (normal, 100–300 × 109/L), and CRP 2.33 mg/L (normal, 0–8 mg/L). Serum C3 and C4 were 0.62 g/L (normal, 0.85–1.93 g/L) and 0.08 g/L (normal, 0.12–0.36 g/L), respectively. ANA was positive (1:100) and anti-dsDNA showed positive (+ + +) (Table 1). According to the EULAR/ACR 2019 SLE classification standard, the patient was diagnosed with SLE. The whole exome sequencing of venous blood was performed on the child and his parents. A heterozygous missense mutation c.2314G > A (p.G772S, Fig. 1, Table 2) of PIK3CD gene was revealed in this patient and his father. His father has not any clinical symptoms. His father has the identical mutation to the child. However, there is not any family history of APDS1 or of other immune deficiency (Fig. 2). Subsequently, tacrolimus was discontinued and sirolimus was started. Sirolimus level was maintained approximately 4 ng/mL at a dose of 1 mg/m2. Upon treatment, thrombocytopenia significantly improved and maintained stability. Currently, the patient has shown no signs of complications.
Discussion and conclusions
We herein report two cases of different variants in PIK3CD gene, presenting with sirolimus relieving hepatosplenomegaly and resistant thrombocytopenia. Our presented case is worth reporting due to the novelty of one of the variants. Besides, the clinical manifestations in two patients with APDS1 are heterogeneous and they are well aligned with known phenotypic data for the disease, which will be reviewed in the following lines.
APDS1 patients typically present with recurrent sinopulmonary infections and increased susceptibility to EBV and/or CMV [9]. In a large pediatric cohort, Almost all APDS1 patients suffered benign lymphoproliferation, including lymphadenopathy, hepatomegaly, splenomegaly or nodular mucosal lymphoid hyperplasia [14]. In accordance with previously studies, recurrent sinopulmonary infections, lymphadenopathy and splenomegaly were the prominent signs in patient 1. Meanwhile, patient 1 had the most frequently reported variant c.3061G > A. The p.E1021K mutation enhances the overactivation of PI3K signaling [15]. The hyperactivation of PI3Kδ plays a crucial role in the pathogenesis of inflammatory and autoimmune diseases. Autoimmune presentations are the features of APDS1 in 28 to 42% of cases [16]. Among these, autoimmune hemolytic anemia (AIHA) and immune thrombocytopenic purpura (ITP) were the most frequent manifestations, followed by Evans syndrome, type 1 diabetes mellitus, enteropathy, arthritis, SLE, autoimmune thyroiditis, sclerosing cholangitis, sjogren syndrome, and autoimmune hepatitis also have been previously reported [17,18,19,20,21]. To date, only a few cases of SLE phenotype have been described in patients with APDS1 [8, 22]. Our patient 2 met classification criteria of SLE due to thrombocytopenia, low level of complement, positive coombs test, and dsDNA. In particular, she had a novel variant c.2314G > A.
A cohort study showed that clinical features of APDS1 patients were incomplete penetrance and highly variable, even in the family carrying the same mutation, ranging from asymptomatic adults to those with primary immunodeficiency, and those with a serious immunodeficiency resulting in early death, to others suffering from lymphoproliferation and malignancy [23]. In accordance with the study, our patient's parents have the same heterozygous missense mutation as their children, but they have not any clinical symptoms. Heurtier L et al. found rare variants c.241G > A and c.371G > A in PIK3CD and confirmed these variants can produce similar phenotypes [24]. Moreover, the novel variants c.1339 + 4G > A and c.2027 + 5C > T have been reported, but no functional assay has been performed [25]. Herein, we have reported a patient with SLE-like phenotype that is in line with the diagnosis of APDS1, who has a novel c.2314G > A variant in PIK3CD gene. Previous studies have suggested that PIK3CD mutations increase PI3Kδ activity resulting in the hyperactivation of the PI3K/AKT/mTOR/S6 signally pathway [26, 27]. Furthermore, studies have indicated that the activity of PI3K and mTOR were implicated in the upregulation of protein S6 phosphorylation induced by IL2 [28]. Several studies have reported that the activation of the PI3K pathway breaks pregerminal center B cell self-tolerance [29]. As shown in the supplement figure, the protein expression levels of pAKT and pS6 were significantly increased (p < 0.05, Additional file 1: Fig. S1a, b). Furthermore, elevated expression of IL2 was observed (p < 0.01, Additional file 1: Fig. S1c). These results demonstrated hyperactivation of the PI3K/AKT/mTOR/S6 signal pathway. However, no in-depth immune studies have been shown.
The treatment of APDS1 revolves around preventing recurrent infection, reducing lymphoproliferation, and suppressing autoimmunity [30]. In the setting of hypogammaglobulinemia or recurrent infections (even if total IgG is normal), immunoglobulin replacement therapy should be initiated. However, immunoglobulin replacement therapy does not improve autoimmunity and lymphoproliferation. Sirolimus is a mTOR inhibitor that directly targets mTOR and inhibits the PI3K pathway downstream. When sirolimus binds to mTOR it blocks activation of IL-2 induced proliferation of T cells [31]. Currently, sirolimus as the first-line drug for the treatment of APDS1 [5], which is effective in the treatment of lymphocytosis and hepatosplenomegaly [2], but less effective for cytopenia. In a retrospective study, 3 of 14 patients with cytopenia had complete remission with sirolimus and 2 of 14 patients had a partial remission with cytopenia [18, 23]. In addition, 69% of patients did not respond to sirolimus treatment in other studies [32]. Herein, two pediatric patients with APDS1 have received sirolimus treatment after genetic diagnosis. Symptoms, such as hepatosplenomegaly, respiratory infections, and resistant thrombocytopenia, have been effectively controlled, and no obvious adverse reactions have been observed. Leniolisib (CDZ173), an oral p110δ inhibitor, was engineered to decrease PI3Kδ pathway hyperactivity [33]. Currently available studies demonstrated that treatment with leniolisib was well tolerated and reduced lymphadenopathy in patients with APDS1 [34]. In addition to oral mTOR inhibitor or p110δ inhibitor, allogeneic hematopoietic stem cell transplantations (HSCT) is an option for those APDS patients with severe complications and poor responses to currently available conventional therapies [35, 36].
We experienced two patients with APDS1 presenting with diverse clinical phenotypes and different variants in PIK3CD gene. Early genetic diagnosis is essential for providing better treatment for children with APDS1. If whole exome sequencing reveals a variant in PIK3CD gene, sirolimus may be considered to alleviate clinical manifestations such as hepatosplenomegaly and resistant thrombocytopenia. This is a newly report of c.2314G > A variant in PIK3CD gene. Further functional immune studies are needed to explore the mechanisms related to the variant in APDS1.
Availability of data and materials
The original contributions presented in the study are included in the article.
Abbreviations
- PI3K:
-
Activated phosphoinositide3-kinase
- APDS1:
-
Activated phosphoinositide3-kinase δ syndrome 1
- IEI:
-
Inborn errors of immunity
- PI3Kδ:
-
Phosphoinositide3-kinase
- SLE:
-
Systemic lupus erythematosus
- EBV:
-
Epstein barr virus
- CMV:
-
Cytomegalovirus
- WBC:
-
White blood cells
- Hb:
-
Hemoglobin
- PLT:
-
Platelets
- CRP:
-
C-reactive protein
- ANA:
-
Antinuclear antibodies
- AIHA:
-
Autoimmune hemolytic anemia
- ITP:
-
Immune thrombocytopenic purpura
- HSCT:
-
Allogeneic hematopoietic stem cell transplantations
References
Bousfiha A, Moundir A, Tangye SG, Picard C, Jeddane L, Al-Herz W, et al. The 2022 Update of IUIS Phenotypical Classification for Human Inborn Errors of Immunity. J Clin Immunol. 2022;42(7):1508–20.
Lucas CL, Kuehn HS, Zhao F, Niemela JE, Deenick EK, Palendira U, et al. Dominant-activating germline mutations in the gene encoding the PI(3)K catalytic subunit p110δ result in T cell senescence and human immunodeficiency. Nat Immunol. 2014;15(1):88–97.
Edwards ESJ, Bier J, Cole TS, Wong M, Hsu P, Berglund LJ, et al. Activating PIK3CD mutations impair human cytotoxic lymphocyte differentiation and function and EBV immunity. J Allergy Clin Immunol. 2019;143(1):276-291.e6.
Preite S, Gomez-Rodriguez J, Cannons JL, Schwartzberg PL. T and B-cell signaling in activated PI3K delta syndrome: from immunodeficiency to autoimmunity. Immunol Rev. 2019;291(1):154–73.
Ruiz-García R, Vargas-Hernández A, Chinn IK, Angelo LS, Cao TN, Coban-Akdemir Z, et al. Mutations in PI3K110δ cause impaired natural killer cell function partially rescued by rapamycin treatment. J Allergy Clin Immunol. 2018;142(2):605-617.e7.
Singh A, Joshi V, Jindal AK, Mathew B, Rawat A. An updated review on activated PI3 kinase delta syndrome (APDS). Genes Dis. 2020;7(1):67–74.
Fekrvand S, Mozdarani H, Delavari S, Sohani M, Nazari F, Kiaee F, et al. Evaluation of radiation sensitivity in patients with hyper IgM syndrome. Immunol Invest. 2021;50(5):580–96.
Li GM, Liu HM, Guan WZ, Xu H, Wu BB, Feng JY, et al. A mutation in PIK3CD gene causing pediatric systemic lupus erythematosus: a case report. Medicine. 2019;98(18): e15329.
Lucas CL, Chandra A, Nejentsev S, Condliffe AM, Okkenhaug K. PI3Kδ and primary immunodeficiencies. Nat Rev Immunol. 2016;16(11):702–14.
Jamee M, Moniri S, Zaki-Dizaji M, Olbrich P, Yazdani R, Jadidi-Niaragh F, et al. Clinical, immunological, and genetic features in patients with activated PI3Kδ syndrome (APDS): a systematic review. Clin Rev Allergy Immunol. 2020;59(3):323–33.
Lougaris V, Baronio M, Moratto D, Tampella G, Gazzurelli L, Facchetti M, et al. A novel monoallelic gain of function mutation in p110δ causing atypical activated phosphoinositide 3-kinase δ syndrome (APDS-1). Clin Immunol. 2019;200:31–4.
Rae W, Gao Y, Ward D, Mattocks CJ, Eren E, Williams AP. A novel germline gain-of-function variant in PIK3CD. Clin Immunol. 2017;181:29–31.
Takeda AJ, Zhang Y, Dornan GL, Siempelkamp BD, Jenkins ML, Matthews HF, et al. Novel PIK3CD mutations affecting N-terminal residues of p110δ cause activated PI3Kδ syndrome (APDS) in humans. J Allergy Clin Immunol. 2017;140(4):1152-1156.e10.
Qiu L, Wang Y, Tang W, Yang Q, Zeng T, Chen J, et al. Activated phosphoinositide 3-kinase delta syndrome: a large pediatric cohort from a single center in China. J Clin Immunol. 2022;42(4):837–50.
Dornan GL, Siempelkamp BD, Jenkins ML, Vadas O, Lucas CL, Burke JE. Conformational disruption of PI3Kδ regulation by immunodeficiency mutations in PIK3CD and PIK3R1. Proc Natl Acad Sci USA. 2017;114(8):1982–7.
Schworer SA, Francis OL, Johnson SM, Smith BD, Gold SH, Smitherman AB, et al. Autoimmune cytopenia as an early and initial presenting manifestation in activated PI3 kinase delta syndrome: case report and review. J Pediatr Hematol Oncol. 2021;43(8):281–7.
Bacalao MA, Satterthwaite AB. Recent advances in lupus B cell biology: PI3K, IFNγ, and chromatin. Front Immunol. 2020;11: 615673.
Maccari ME, Abolhassani H, Aghamohammadi A, Aiuti A, Aleinikova O, Bangs C, et al. Disease evolution and response to rapamycin in activated phosphoinositide 3-Kinase δ syndrome: The European Society for Immunodeficiencies-Activated Phosphoinositide 3-Kinase δ Syndrome Registry. Front Immunol. 2018;9:543.
Hartman HN, Niemela J, Hintermeyer MK, Garofalo M, Stoddard J, Verbsky JW, et al. Gain of function mutations of PIK3CD as a cause of primary sclerosing cholangitis. J Clin Immunol. 2015;35(1):11–4.
Ren Y, Cui G, Gao Y. Research progress on inflammatory mechanism of primary Sjögren syndrome. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2021;50(6):783–94.
Wang S, Huang Z, Lei Y, Han X, Tian D, Gong J, et al. Celastrol alleviates autoimmune hepatitis through the PI3K/AKT signaling pathway based on network pharmacology and experiments. Front Pharmacol. 2022;13: 816350.
Wang Y, Yang Q, Chen X, Tang W, Zhou L, Chen Z, et al. Phenotypic characterization of patients with activated PI3Kδ syndrome 1 presenting with features of systemic lupus erythematosus. Genes Dis. 2021;8(6):907–17.
Coulter TI, Chandra A, Bacon CM, Babar J, Curtis J, Screaton N, et al. Clinical spectrum and features of activated phosphoinositide 3-kinase δ syndrome: a large patient cohort study. J Allergy Clin Immunol. 2017;139(2):597-606.e4.
Heurtier L, Lamrini H, Chentout L, Deau MC, Bouafia A, Rosain J, et al. Mutations in the adaptor-binding domain and associated linker region of p110δ cause Activated PI3K-δ Syndrome 1 (APDS1). Haematologica. 2017;102(7):e278–81.
Fekrvand S, Delavari S, Chavoshzadeh Z, Sherkat R, Mahdaviani SA, Sadeghi Shabestari M, et al. The first Iranian cohort of pediatric patients with activated phosphoinositide 3-Kinase-δ (PI3Kδ) syndrome (APDS). Immunol Invest. 2022;51(3):644–59.
Jung S, Gámez-Díaz L, Proietti M, Grimbacher B. “Immune TOR-opathies,” a Novel Disease Entity in Clinical Immunology. Front Immunol. 2018;9:966.
Thouenon R, Moreno-Corona N, Poggi L, Durandy A, Kracker S. Activated PI3Kinase delta syndrome-a multifaceted disease. Front Pediatr. 2021;9: 652405.
Tuhácková Z, Sloncová E, Vojtechová M, Sovová V. IL2-dependent phosphorylation of 40S ribosomal protein S6 is controlled by PI-3K/mTOR signalling in CTLL2 cells. Int J Mol Med. 2004;13(4):601–5.
Lau A, Avery DT, Jackson K, Lenthall H, Volpi S, Brigden H, et al. Activated PI3Kδ breaches multiple B cell tolerance checkpoints and causes autoantibody production. J Exp Med. 2020; 217(2).
Coulter TI, Cant AJ. The treatment of activated PI3Kδ syndrome. Front Immunol. 2018;9:2043.
Lee VW, Chapman JR. Sirolimus: its role in nephrology. Nephrology. 2005;10(6):606–14.
Nunes-Santos CJ, Uzel G, Rosenzweig SD. PI3K pathway defects leading to immunodeficiency and immune dysregulation. J Allergy Clin Immunol. 2019;143(5):1676–87.
Hoegenauer K, Soldermann N, Zécri F, Strang RS, Graveleau N, Wolf RM, et al. Discovery of CDZ173 (Leniolisib), representing a structurally novel class of PI3K delta-selective inhibitors. ACS Med Chem Lett. 2017;8(9):975–80.
Rao VK, Webster S, Šedivá A, Plebani A, Schuetz C, Shcherbina A, et al. A randomized, placebo-controlled phase 3 trial of the PI3Kδ inhibitor leniolisib for activated PI3Kδ syndrome. Blood. 2023;141(9):971–83.
Nademi Z, Slatter MA, Dvorak CC, Neven B, Fischer A, Suarez F, et al. Hematopoietic stem cell transplant in patients with activated PI3K delta syndrome. J Allergy Clin Immunol. 2017;139(3):1046–9.
Okano T, Imai K, Tsujita Y, Mitsuiki N, Yoshida K, Kamae C, et al. Hematopoietic stem cell transplantation for progressive combined immunodeficiency and lymphoproliferation in patients with activated phosphatidylinositol-3-OH kinase δ syndrome type 1. J Allergy Clin Immunol. 2019;143(1):266–75.
Acknowledgements
We thank the Department of Nephrology and Immunology in Children's Hospital of Soochow University, Suzhou, China for their support. We also thank the native English speaking scientists of Elixigen Company (Huntington Beach, California) for editing our manuscript.
Funding
This work was supported by the Suzhou Key Discipline Project of Pediatric Immunology (grant number SZXK202106); the Suzhou Science and Technology Development Plan Project (grant number SS202067); and the Suzhou Science and Technology Development Program Medical Devices and New Medicine (grant number SLT201941).
Author information
Authors and Affiliations
Contributions
LJ conceived and prepared the manuscript. QY X, YY S, YZ, QL diagnosed the patient and drafted the initial manuscript. LJ, RY C and XH H wrote the presentation of cases and contributed to the discussion section. XZ L edited and coordinated the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of Children's Hospital of Soochow University (No. 2022031).
Consent for publication
Written informed consents were obtained from the patient’s parents for the publication of this case report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information

Additional file 1: Figure S1.
The protein expression levels of pAKT, pS6 and IL2 in patient 2. Phosphorylation of AKT, S6 and IL2 in patient 2 were significantly higher than in the control group. All data are presented as mean ± SD (n = 3). *p < 0.05, **p < 0.01.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, L., Hu, X., Lin, Q. et al. Two cases of successful sirolimus treatment for patients with activated phosphoinositide 3-kinase δ syndrome 1. Allergy Asthma Clin Immunol 19, 86 (2023). https://doi.org/10.1186/s13223-023-00840-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13223-023-00840-0