Abstract
Objective
To report the outcomes and complications associated with prophylactic incisional gastropexy performed in dog breeds at risk for GDV.
Results
Seven hundred and sixty-six dogs underwent prophylactic incisional gastropexy of which 61 were electively performed at the time of castration or spay and 705 were adjunctively performed at the time of emergency abdominal surgery. All dogs had short-term follow-up, and 446 dogs (58.2%) had additional follow-up with a median long-term follow-up time of 876 days (range 58-4450). Only 3 dogs (0.4%) had a direct complication associated with the gastropexy site including hemorrhage causing hemoabdomen (2) and infection with partial dehiscence (1). No dogs with long-term follow-up experienced gastric dilatation (GD), gastric dilatation volvulus (GDV), or persistent GI signs following gastropexy. Results of this study found that complications directly associated with prophylactic gastropexy were rare and limited to hemorrhage causing hemoabdomen and infection with partial dehiscence. Transient postoperative GI signs may occur. Gastropexy malpositioning and bowel entrapment were not encountered. There was no occurrence of GD or GDV.
Similar content being viewed by others
Introduction
Gastric dilatation volvulus (GDV) is an acute, life-threatening condition affecting a wide variety of dog breeds, most commonly large- and giant-breed dogs. Predisposing factors associated with GDV include increasing age, being underweight, history of GDV in a first-degree relative, rapid eating, once daily feedings, exercising either before or following meals, fearful or anxious temperaments, increased thoracic depth-to-width ratio, and increased hepatogastric ligament length [1,2,3,4,5,6,7,8,9,10,11,12]. A recent history of splenectomy may be associated with GDV, but reports are conflicting [12, 13].
Mortality rates associated with GDV range from 10 to 55% [9, 14,15,16,17], so prophylactic gastropexy has been recommended due to reduced mortality up to thirty times in certain breeds at risk for GDV (e.g. Great Danes) compared with dogs that did not get a gastropexy [19]. Gastropexy is a surgical procedure involving fixation of the pyloric antrum region of the stomach to the right body wall with several techniques described [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. The incidence of gastric dilatation (GD) in patients who previously underwent prophylactic incisional gastropexy (IG) was 11.1% in one report [37]. That study included 27 dogs with postoperative complications of mild and transient GI signs including episodes of regurgitation, inappetence, and gastrointestinal (GI) upset [37]. Gastric malpositioning has also been reported as an intraoperative complication, most recently reported in 5% of dogs that underwent laparoscopically assisted gastropexy (LAIG) [38].
Concerns remain regarding the occurrence of rare but potentially life-threatening complications such as hemorrhage and bowel entrapment [40, 41]. This study aims to report the outcomes and identify the incidence of intraoperative and postoperative complications associated with prophylactic gastropexy in a large population of at risk dog breeds. We hypothesized that performing prophylactic gastropexy in dogs poses minimal risk for intraoperative and postoperative complications.
Materials and methods
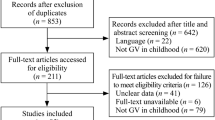
Medical records obtained from Ocean State Veterinary Specialists between 2009 and 2019 were retrospectively evaluated for dogs in which prophylactic incisional gastropexy procedure was performed, including IG, LAIG, and total laparoscopic incisional gastropexy (TLIG). Inclusion criteria were at-risk dog breeds for GDV presenting for elective prophylactic gastropexy or emergency abdominal surgery that also underwent prophylactic IG during laparotomy. Dogs were excluded if they had pre-existing GI disease such as GD, GDV, mesenteric torsion, colonic torsion, and inflammatory bowel disease (IBD) as any postoperative GI signs could not be distinguished from complications of the gastropexy. Dogs were also excluded if they died prior to discharge if cause of death was reported due to the primary disease or a complication from the primary disease (e.g. disseminated intravascular coagulopathy). Medical records were evaluated for signalment, gastropexy technique performed, and intraoperative and postoperative complications.
All dogs were treated with similar anesthetic protocols. Surgical techniques for prophylactic gastropexy included IG by open laparotomy, LAIG using the technique described by Rawlings et al. [28], and TLIG with an endoscopic suturing device (Endostitch; Covidien, Mansfield, MA) using the technique described by Deroy et al [42]. Surgery was performed by either a Diplomate of the American College of Veterinary Surgeons (DACVS), surgery resident, intern, or emergency veterinarian. Any intraoperative complications associated with the gastropexy were recorded. Postoperatively, dogs were managed and discharged based on clinician judgement.
Median follow-up times (with ranges) were reported. The overall follow-up time was defined as the time from surgery until death or last contact. Short-term follow-up involved reviewing records from discharge until incision recheck and/or suture or staple removal, either in-person or through communication with the owner, ranging from 7 days to 2 months to allow for healing of incisions and incision-related complications. Long-term follow-up involved reviewing records beyond incision recheck until death or last contact from the owner or primary care veterinarian.
The frequency of complications as well as the occurrence of GD and GDV following prophylactic gastropexy was reported. Minor complications included any superficial incisional issues that resolved with medical care. Major complications included dogs needing deep incisional and/or abdominal surgery for treatment of a life-threatening postoperative complication such as incision infection and dehiscence, body wall dehiscence, septic abdomen, hemoabdomen, etc. Complications directly associated with the gastropexy found during subsequent abdominal surgery were reported separately as well as any incidence of postoperative GI signs including hyporexia, anorexia, regurgitation, vomiting, and diarrhea and any later abdominal surgeries after discharge.
Results
Seven hundred and sixty-six (766) dogs met the criteria for inclusion. Sixty-seven different breeds were represented with Labrador Retriever (19.2%, n = 147), Golden Retriever (13.3%, n = 102), and German Shepherd Dog (6.6%, n = 51) being the most common. The sex distribution was 61% male (119 intact, 348 castrated) and 39% female (120 intact, 179 spayed). The median age was 4.9 years (range, 0.2–15.8), and the median weight was 33 kg (range, 6.4–120). Sixty-one dogs presented for elective prophylactic gastropexy at the time of castration or spay (ovariohysterectomy or ovariectomy based on clinician preference), of which there were 19 IG, 41 LAIG, and 1 TLIG. The remaining 705 dogs presented for emergency abdominal surgery where prophylactic IG was also performed. There were 165 unique combinations of abdominal and non-abdominal procedures performed with IG (see Table 1).
Seven hundred and fifty dogs had notation of suture type used for the gastropexy. The suture types used for the gastropexy were polydioxanone (PDS, Ethicon) size 0 (n = 603), 2 − 0 (n = 19), and 3 − 0 (n = 2); poliglecaprone 25 (Monocryl, Ethicon) size 2 − 0 (n = 1); polypropylene (Prolene, Ethicon) size 0 (n = 20) and 2 − 0 (n = 1); barbed glycomer 631 (V-loc, Covidien) size 0 (n = 1) and 2 − 0 (n = 103); or not specified (n = 16). The gastropexy was secured in a continuous (n = 652) or interrupted (n = 8) pattern or not available in the records (n = 106). Orientation and length of gastropexy incisions were inconsistently noted.
All 766 dogs had short-term follow-up with a median of 13 days (range 7–55). Four hundred and forty-six dogs (58.2%) had additional follow-up with a median of 876 days (range 58-4450). Postoperative complications included 88 minor wound-related complications (11.5%) and 22 major complications (2.9%) requiring surgical intervention within the hospitalization or short-term follow-up period. Minor complications included superficial incision infection (84), incision abscess (3), and draining tract (1) that resolved with antibiotic therapy. Only 3 dogs had a direct (major) complication that could be associated with the gastropexy site including hemorrhage from the gastropexy site causing hemoabdomen (2) and infection with partial dehiscence (1). Table 2 lists the other major complications. The frequency of direct gastropexy complication was 0.4%.
Of the 705 dogs that presented for abdominal emergency surgery and had IG performed, 466 dogs presented for a primary GI emergency and 239 dogs for a non-GI abdominal emergency. 145/466 dogs with a GI emergency had postoperative GI signs (144 presented for GIFB and 1 for intestinal mass resection), and 28/239 dogs with a non-GI abdominal emergency had postoperative GI signs. Table 3 lists the causes identified in the total 173 dogs that had postoperative GI signs. Of note, 11 dogs had transient postoperative GI signs that resolved with medical therapy (variable based on clinician judgment) and definitive diagnosis was not identified with an overall incidence of 1.4%. Three had persistent GI signs that did not respond to medical therapy and did not get additional diagnostic workup with an overall incidence of 0.4%.
Of the 144 dogs with GIFB obstruction, 93 dogs had subsequent abdominal surgeries, and 80 of those were confirmed to have an intact gastropexy adhesion with proper positioning (range, 15-4450 days after the initial surgery with gastropexy). The remaining 13 dogs did not mention gastropexy in the operative report. None of the 446 dogs with long-term follow-up in this study were diagnosed with GD or GDV. Gastropexy malpositioning and bowel entrapment were not encountered in any dogs that had subsequent abdominal surgery.
Discussion
The efficacy of prophylactic IG has previously been confirmed for the long-term prevention of GDV in dogs [37]. However, complications associated with IG have not been directly examined. This is the largest retrospective study to date reporting the outcomes and complications of prophylactic IG and identified two major complications including hemorrhage from the gastropexy site leading to hemoabdomen and infection and partial dehiscence of the gastropexy. Prophylactic gastropexy may also cause transient postoperative GI signs, but gastric malpositioning and bowel entrapment were not encountered.
There are 3 recent studies that reported on the long-term outcomes and complications of prophylactic IG in 27 dogs in Benitez et al. [37], LAIG in 44 dogs in Loy-Son et al. [38], and TLIG in 39 dogs in Giaconella et al [39]. In the present study, only 3/766 dogs (0.4%) were found to have complications directly associated with the gastropexy that required surgical intervention compared to a frequency of 0–5% in the other studies evaluating prophylactic IG [37], LAIG [38], and TLIG [39]. Loy-Son et al. was the only study to report the need for immediate surgical revision in 2/44 dogs (5%) due to direct gastropexy complication (gastropexy malpositioning). There was no incidence of gastropexy malpositioning in the present study.
Hemoabdomen from the gastropexy site is possible due to a neurovascular bundle frequently encountered during incision of the transversus abdominis muscle that can lead to significant hemorrhage. This may be a lateral branch of caudal superficial epigastric artery coursing alongside costoabdominalis or iliohypogastricus cranialis nerve (ventral branches of T13 and L1 spinal nerves, respectively) within the transversus abdominal muscle plane [43]. Hemorrhage is usually self-limiting, but electrocautery can be used for hemostasis or to make the gastropexy incisions as originally described by Funkquist in 1967 and 1979. Coagulopathy was considered in both dogs in this study but neither were confirmed.
Two possibilities were considered for the source of gastropexy infection and dehiscence: spread of infection from the ventral midline laparotomy incision through the linea dehiscence to the nearby gastropexy site, or penetration and contamination of suture in the gastric lumen during gastropexy suturing. The latter was considered less likely given that the bacterial loads of the canine stomach are relatively low [44]. Culture of the incision or gastropexy site was not performed. Long-term follow-up was not available for this dog.
Persistence of GI signs and occurrence of GD following gastropexy for GDV in dogs is attributed to underlying gastric motility disorder or negative effects on gastric motility from circumcostal gastropexy [45,46,47]. More recently, studies by Gazzola et al. and Coleman et al. concluded that LAIG did not influence GI motility based on data collected from a wireless motility device [48, 49]. Three dogs (0.4%) in the present study had persistent GI signs and 11 dogs (1.4%) had transient GI signs that responded to medical therapy compared to 0-7.7% of dogs with GI signs reported in other studies [37,38,39]. A previous study reported the occurrence of GD in 3/27 dogs (11.1%) after IG [37]. No dogs in the present study with long-term follow-up were diagnosed with GD or GDV.
The overall complication rate in this study was 14.4%. Minor complications (11.5%) only included incision complications as all other complications (major, 2.9%) required additional surgery for revision. Therefore, the surgical site infection rate for all abdominal surgeries in this population of dogs was 11.5%. The frequency of incision complications in this study was similar to the frequency of 5.1–20.4% in other studies evaluating prophylactic IG [37], LAIG [38], and TLIG [39].
This is the largest study to date reporting the outcomes and complications of prophylactic gastropexy. This study concludes that prophylactic gastropexy is a safe procedure that should be performed in at-risk dog breeds at the time of elective castration or spay or as an adjunctive procedure during emergency abdominal surgery. Direct risks associated with prophylactic gastropexy include hemorrhage, infection, and dehiscence. Prophylactic gastropexy may cause transient GI signs that can be medically managed but is unlikely to cause persistent GI signs. The benefits of preventing GDV seemingly far outweigh the low incidence of complications.
Limitations
-
Long-term follow-up was not available for all dogs.
-
A prospective study with a large population of healthy at-risk dog breeds without pre-existing GI signs presenting for elective incisional gastropexy at the time of castration or spay would be needed to evaluate the direct effect of gastropexy on causing postoperative GI signs or other complications.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- GI:
-
gastrointestinal
- GIFB:
-
gastrointestinal foreign body
- GD:
-
gastric dilatation
- GDV:
-
gastric dilatation volvulus
- IBD:
-
inflammatory bowel disease
- IG:
-
incisional gastropexy
- LAIG:
-
laparoscopically assisted gastropexy
- TLIG:
-
total laparoscopic gastropexy
- NSAID:
-
non-steroidal anti-inflammatory drug
References
Monnet E. Gastric dilatation-volvulus syndrome in dogs. Vet Clin North Am Small Anim Pract. 2003;33(5):987–1005.
Hall JA, Willer RL, Seim HB, et al. Gross and histologic evaluation of hepatogastric ligaments in clinically normal dogs and dogs with gastric dilatation-volvulus. Am J Vet Res. 1995;56(12):1611–4.
Theyse LF, van de Brom WE, van Sluijs FJ. Small size of food particles and age as risk factors for gastric dilatation volvulus in great danes. Vet Rec. 1998;143(2):48–50.
Schellenberg D, Yi Q, Glickman NW, et al. Influence of thoracic conformation and genetics on the risk of gastric dilatation-volvulus in Irish setters. J Am Anim Hosp Assoc. 1998;34(1):64–73.
Schaible RH, Ziech J, Glickman NW, et al. Predisposition to gastric dilatation-volvulus in relation to genetics of thoracic conformation in Irish setters. J Am Anim Hosp Assoc. 1997;33(5):379–83.
Raghavan M, Glickman NW, Glickman LT. The effect of ingredients in dry dog foods on the risk of gastric dilatation-volvulus in dogs. J Am Anim Hosp Assoc. 2006;42(1):28–36.
Glickman LT, Glickman NW, Schellenberg DB, et al. Incidence of and breed-related risk factors for gastric dilatation-volvulus in dogs. J Am Vet Med Assoc. 2000;216(1):40–5.
Glickman LT, Glickman NW, Schellenberg DB, et al. Non-dietary risk factors for gastric dilatation-volvulus in large and giant breed dogs. J Am Vet Med Assoc. 2000;217(10):1492–9.
Glickman LT, Glickman NW, Schellenberg DB, et al. Multiple risk factors for the gastric dilatation-volvulus syndrome in dogs: a practitioner/owner case-control study. J Am Anim Hosp Assoc. 1997;33(3):197–204.
Glickman L, Emerick T, Glickman N, et al. Radiological assessment of the relationship between thoracic conformation and the risk of gastric dilatation-volvulus in dogs. Vet Radiol Ultrasound. 1996;37:174–80.
Glickman LT, Glickman NW, Pérez CM, et al. Analysis of risk factors for gastric dilatation and dilatation-volvulus in dogs. J Am Vet Med Assoc. 1994;204(9):1465–71.
Millis DL, Nemzek J, Riggs C, et al. Gastric dilatation-volvulus after splenic torsion in two dogs. J Am Vet Med Assoc. 1995;207(3):314–5.
Goldhammer MA, Haining H, Milne EM, et al. Assessment of the incidence of GDV following splenectomy in dogs. J Small Anim Pract. 2010;51(1):23–8.
Glickman LT, Lantz GC, Schellenberg DB, et al. A prospective study of survival and recurrence following the acute gastric dilatation-volvulus syndrome in 136 dogs. J Am Anim Hosp Assoc. 1998;34:253–9.
Zacher LA, Berg J, Shaw SP, et al. Association between outcome and changes in plasma lactate concentration during presurgical treatment in dogs with gastric dilatation-volvulus: 64 cases (2002–2008). J Am Vet Med Assoc. 2010;236:892–7.
Mackenzie G, Barnhart M, Kennedy S, et al. A retrospective study of factors influencing survival following surgery for gastric dilatation-volvulus syndrome in 306 dogs. J Am Anim Hosp Assoc. 2010;46:97–102.
Rawlings CA, Mahaffey MB, Bement S, et al. Prospective evaluation of laparoscopic-assisted gastropexy in dogs susceptible to gastric dilatation. J Am Vet Med Assoc. 2002;221:1576–81.
Dujowich M, Reimer SB. Evaluation of an endoscopically assisted gastropexy technique in dogs. Am J Vet Res. 2008;69(4):537–41.
Ward MP, Patronek GJ, Glickman LT. Benefits of prophylactic gastropexy for dogs at risk of gastric dilatation-volvulus. Prev Vet Med. 2003;60(4):319–29.
Coolman BR, Manfra Marretta S, Pijanowski GJ, et al. Evaluation of a skin stapler for belt-loop gastropexy in dogs. J Am Anim Hosp Assoc. 1999;35(5):440–4.
Belandria GA, Pavletic MM, Boulay JP, et al. Gastropexy with an automatic stapling instrument for the treatment of gastric dilatation and volvulus in 20 dogs. Can Vet J. 2009;50(7):733–40.
Woolfson J, Kostolich M. Circumcostal gastropexy: clinical use of the technique in 34 dogs with gastric dilatation-volvulus. J Am Anim Hosp Assoc. 1986;22:825–30.
Wilson ER, Henderson RA, Montgomery RD, et al. A comparison of laparoscopic and belt-loop gastropexy in dogs. Vet Surg. 1996;25(3):221–7.
Whitney W, Scavelli T, Matthiesen D. Belt-loop gastropexy: technique and surgical results in 20 dogs. J Am Anim Hosp Assoc. 1989;25:75–83.
Schulman A, Lusk R, Lippincott C, et al. Muscular flap gastropexy: a new surgical technique to prevent recurrences of gastric dilatation-volvulus syndrome. J Am Anim Hosp Assoc. 1986;22:339–46.
Runge JJ, Mayhew P, Rawlings CA. Surgical views: laparoscopic-assisted and laparoscopic prophylactic gastropexy: indications and techniques. Compend Contin Educ Vet. 2009;31(2):58–65.
Rawlings CA, Mahaffey MB, Bement S, et al. Prospective evaluation of laparoscopic-assisted gastropexy in dogs susceptible to gastric dilatation. J Am Vet Med Assoc. 2002;221(11):1576–81.
Rawlings CA, Foutz TL, Mahaffey MB, et al. A rapid and strong laparoscopic-assisted gastropexy in dogs. Am J Vet Res. 2001;62(6):871–5.
Rawlings CA. Laparoscopic-assisted gastropexy. J Am Anim Hosp Assoc. 2002;38(1):15–9.
Pope ER, Jones BD. Clinical evaluation of a modified circumcostal gastropexy in dogs. J Am Vet Med Assoc. 1999;215(7):952–5.
Meyer-Lindenberg A, Harder A, Fehr M, et al. Treatment of gastric dilatation-volvulus and a rapid method for prevention of relapse in dogs: 134 cases (1988–1991). J Am Vet Med Assoc. 1993;203(9):1303–7.
MacCoy DM, Sykes GP, Hoffer RE, et al. A gastropexy technique for permanent fixation of the pyloric antrum. J Am Anim Hosp Assoc. 1982;18:763–8.
Degna M, Formaggini L, Fondati A, et al. Using a modified gastropexy technique to prevent recurrence of gastric dilatation-volvulus in dogs. Vet Med. 2001;96:39–50.
Eggertsdóttir AV, Stigen y Ø, Lønaas L, et al. Comparison of the recurrence rate of gastric dilatation with or without volvulus in dogs after circumcostal gastropexy versus gastrocolopexy. Vet Surg. 2001;30(6):546–51.
Eggertsdóttir AV, Langeland M, Fuglem B, et al. Long-term outcome in dogs after circumcostal gastropexy or gastrocolopexy for gastric dilatation with or without volvulus. Vet Surg. 2008;37(8):809–10.
Fallah A, Lumb W, Nelson A, et al. Circumcostal gastropexy in the dog: a preliminary study. Vet Surg. 1982;11:9–12.
Benitez ME, Schmeidt CW, Radlinsky MG, Cornell KK. Efficacy of incisional gastropexy for prevention of GDV in dogs. JAAHA. 2013;49:185–9.
Loy Son NK, Singh A, Amsellem P, et al. Long-Term Outcome and Complications Following Prophylactic Laparoscopic-Assisted Gastropexy in Dogs. Vet Surg. 2016;45:O77–O83.
Giaconella V, Grillo R, Giaconella R, et al. Outcomes and Complications in a Case Series of 39 Total Laparoscopic Prophylactic Gastropexies Using a Modified Technique. Animals. 2021;11(2):255.
Willmann M, Lorinson D, Hittmair KM. Large intestinal entrapment as a long-term complication after gastropexy in a Great Dane. Wiener Tierarztl Monatsschrift. 2004;91:23–6.
Gagnon D, Brisson B. Predisposing factors for colonic torsion/volvulus in dogs: a retrospective study of six cases (1992–2010). J Am Anim Hosp Assoc. 2013 May-Jun;49(3):169–74.
Deroy C, Hahn H, Bismuth C, et al. Simplified Minimally Invasive Surgical Approach for Prophylactic Laparoscopic Gastropexy in 21 Cases. JAAHA. 2019;55(3):152–9.
Castaneda-Herrera FE, Buritica-Gaviria EF, Echeverry-Bonilla DF. Anatomical Evaluation of the Thoracolumbar Nerves Related to the Transversus Abdominis Plane Block Technique in the Dog. Anat Histol Embryol. 2017;46(4):373–7.
Schmitz S, Suchodolski J. Understanding the canine intestinal microbiota and its modification by pro-, pre‐ and synbiotics - what is the evidence? Vet Med Sci. 2016;2(2):71–94.
Hall JA, Willer RL, Seim HB III, et al. Gastric emptying of nondigestible radiopaque markers after circumcostal gastropexy in clinically normal dogs and dogs with gastric dilatationvolvulus. Am J Vet Res. 1992;53:1961–5.
Hall JA, Willer RL, Solie TN, et al. Effect of circumcostal gastropexy on gastric myoelectric and motor activity in dogs. J Small Anim Pract. 1997;38:200–7.
Funkquist B, Garmer L. Pathogenic and therapeutic aspects of torsion of the canine stomach. J Small Anim Pract. 1967;8:523–32.
Gazzola KM, et al. Effects of prophylactic incisional gastropexy on markers of gastric motility in dogs as determined by use of a novel wireless motility device. AJVR. 2017;78(1):100–6.
Coleman KA, Boscan P, Ferguson L, et al. Evaluation of gastric motility in nine dogs before and after prophylactic laparoscopic gastropexy: a pilot study. Aust Vet J. 2019;97(7):225–30.
Acknowledgements
The authors would like to thank Joe Hauptman, DVM, MS, DACVS, for his assistance with the statistical analysis for the study and Milan Milovancev, DVM, DACVS for his advice in editing.
Funding
Funding was provided by Ocean State Veterinary Specialists as part of residency research funds, with no role in design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
de la Vega M, DVM: Conception and design of the study, acquisition of all data, data analysis and interpretation, drafting the article, critical revision of the article, and approval of the version to be published; Ralphs SC, DVM, DACVS-SA: Conception and design of the study, data analysis and interpretation, critical revision of the article, and approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in compliance with both the principles of the Basal Declaration as well as institutional guidelines. Ethical review and approval were not required for this study because only medical records were reviewed retrospectively, although the institution lacked an available ethics committee. This retrospective study involved client-owned animals; informed written consent from all canine owners was obtained for the surgical procedures performed, and practices adhered to a high standard of veterinary care.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest related to this report.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
de la Vega, M., Ralphs, S.C. Outcomes and complications of prophylactic incisional gastropexy in 766 dogs (2009–2019).. BMC Res Notes 16, 300 (2023). https://doi.org/10.1186/s13104-023-06595-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-023-06595-6