Abstract
Objective
This study proposes to identify and validate weighted sensor stream signatures that predict near-term risk of a major depressive episode and future mood among healthcare workers in Kenya.
Approach
The study will deploy a mobile application (app) platform and use novel data science analytic approaches (Artificial Intelligence and Machine Learning) to identifying predictors of mental health disorders among 500 randomly sampled healthcare workers from five healthcare facilities in Nairobi, Kenya.
Expectation
This study will lay the basis for creating agile and scalable systems for rapid diagnostics that could inform precise interventions for mitigating depression and ensure a healthy, resilient healthcare workforce to develop sustainable economic growth in Kenya, East Africa, and ultimately neighboring countries in sub-Saharan Africa. This protocol paper provides an opportunity to share the planned study implementation methods and approaches.
Conclusion
A mobile technology platform that is scalable and can be used to understand and improve mental health outcomes is of critical importance.
Similar content being viewed by others
Introduction
According to the World Health Organization (WHO), mental disorders account for the largest burden of illness among all types of health problems [1]. Major depressive disorder is the second leading cause of disability, affecting more than 350 million people worldwide [2]. In low-and-middle-income countries (LMICs), resources are particularly limited for surveillance, diagnosis, and treatment. In Kenya, a report prepared by a national mental health taskforce [3] highlighted the fact that the severe state of neglect of mental health services, infrastructure and research has led to a “national crisis” and implored the mobilization of immediate and effective solutions to address mental health issues. The Taskforce highlighted that research institutions and universities should: (1) collect relevant data to better define the mental illness gaps (in detection and interventions), burden and determinants; (2) focus particular attention on escalating interventions to reduce depression and suicidal acts. We propose a novel mobile infrastructure in Kenya that has previously been deployed in the United States of America (USA), to test its validity and predictive capability in a different cultural setting [4, 5].
The proposed study builds up on the Intern Health Study which is a prospective longitudinal cohort study of stress and depression among training physicians in the USA and China [6, 7]. This model allows for the same individuals to be followed, first under normal conditions and then under high-stress conditions [8]. The Intern Health Study employs a unique mobile app platform, the Intern App, specifically designed for healthcare workers to collect and integrate active and passive data on mood, sleep, and activity. Intern Health Study has demonstrated that mobile monitoring can facilitate the prospective, real-time monitoring of continuous, passive measures and effectively predict short-term risk for depressive episodes in a large group of individuals (See Tables 1and Fig. 1). Mobile technology coupled with predictive models can help in triggering early warning systems e.g., signs of depression [8]. We would like to adapt the App and make it contextually relevant and deploy it among healthcare workers within Kenyan urban and semi-urban settings.
The objective of the proposed study is to demonstrate the feasibility of deploying a novel methodology for developing predictive models for mood changes and depression among Kenyan healthcare workers. The specific objectives of the research are:
-
i)
To adapt, validate and refine previously developed Artificial Intelligence/Machine Learning (AI/ML) based prediction models of depression and mood among Kenyan healthcare workers; and.
-
ii)
To collect and evaluate individual active and passive data that may predict depression and mood among Kenyan healthcare workers.
Main text
Methods
Design
This will be a longitudinal cohort study.
Study settings
The setting will be in five urban and semi-urban healthcare facilities in the Kenyan capital city, Nairobi, where healthcare workers from diverse cadres are directly involved with the patient’s care.
Facility 1
The Aga Khan University Hospital Nairobi, which is a private facility with a bed capacity of 254 with 14 different specialty departments.
Facility 2
Pumwani Hospital, which is a public maternity facility with 396 healthcare staff spread across 13 different cadres (physicians, nurses, nutritionists, and medical students) and 25 different departments [9].
Facility 3
Mama Lucy Hospital, which is a public facility with 700 healthcare workers who attend to more than 800 outpatients daily and has an ever-growing bed capacity.
Facility 4
Kenyatta National Hospital, which is a public facility which has a bed capacity of 1800 and a staff population of 6000 [10]. These staff give medical care to patients in 50 inpatient wards, 24 theaters, 22 outpatient clinics and 1 accident and emergency center.
Facility 5
Kenyatta University Teaching Referral and Research Hospital, which is a public facility which has an over 650 bed capacity and there are around 665 hospital staff [11].
Sample size determination
The Cochran formula to estimate a representative sample for proportions is utilized [12]. Using a 95% confidence level, proportion = 0.5 (maximum variability) of +/- 5%, the minimum sample size required will be 462 participants after an attrition rate of 20%. n= (Z^2 p q)/e^2 where n is the sample size, Z is the statistic corresponding to 95% level of confidence, P is expected proportion, and d is precision (corresponding to effect size). Thus, we will recruit 500 participants, which will translate to 100 participants from each of the five healthcare facilities.
Instruments description
A socio-demographic questionnaire in the App incorporates elements such as age, gender and education background.
The app is the platform utilized to electronically capture all the tools within the participant questionnaire. Utilizing the app in this way enables us to have skip logistics in the questionnaire, making it shorter for the participants. For example, where a participant responds and says that they have never had a COVID-19 vaccination, they will not encounter questions on whether and when they got their first, second and third dose, experience with the vaccine, and type of vaccine. In line with this response process, it will be difficult to identify the total number items in the questionnaire that each participant will attend to. However, we can estimate the time for completion in one sitting as 20–30 min.
Each participant will complete the following standardized instruments/tools:
-
1)
Neuroticism - NEO-Five Factor Inventory [13] is a 60-item measurement that is designed to assess personality in the domains of neuroticism, extraversion, openness, consciousness, and agreeableness. Each item is scored with a 5-point Likert scale ranging from “strongly disagree, disagree, neutral, agree and strongly agree. Internal consistency reliability [13] of the tool has been found to be good α = .86.
-
2)
Positive and Negative Suicide Inventory (PANSI) [14] will measure suicidal ideation. PANSI evaluates both the protective and risk factors associated with suicidal ideation and comprises two dimensions (14 items total): positive ideation (PANSI-PI, 6 items) and negative suicide ideation (PANSI-NSI; 8 items). PANSI-NSI and PANSI-PI examine the frequency of specific negative thoughts (e.g., failure to accomplish something important) or positive thoughts (e.g., excited about doing well at school or work) related to suicidal behavior [14]. Participants will use a Likert scale ranging from 1 (i.e., “none of the time”) to 5 (i.e., “most of the time”) to assess the frequency they experience suicidal ideation. Higher scores indicate more positive or negative suicide ideation, depending on the item’s particular subscale.
-
3)
Patient Health Questionnaire (PHQ-9) [15]. It consists of nine major depression diagnostic items of DSM-V: anhedonia, depressed mood, trouble sleeping, feeling tired, guilt or worthlessness, concentration difficulties, feeling restless and suicidal thoughts. Each item is scored from 0 (not all) to 3 (nearly every day). The final score indicates depressive symptoms: minimal (0–4), mild (5–9), moderate (10–14), moderately severe (15–19) and severe (20–27). PHQ-9 has good reliability and convergent validity [16]. The Swahili PHQ-9 is validated in Kenya and has demonstrated good reliability α = 0.84 [17].
-
4)
Pittsburgh Sleep Quality Index [18] will assess sleep quality in relation to a range of subjective estimations component scores. The scores range 0–21 with higher scores indicating an increased dissatisfaction with sleep and a greater severity of sleep disturbance. Though not validated in Kenya, it has been validated in other African settings such as Ethiopia moderate internal consistency α = 0.59 [19] and Nigeria α = 0.55 [20].
-
5)
Risky Families Questionnaire [21] will be utilized to assess the degree of risk of physical, mental, and emotional distress that participants faced in their homes during childhood and adolescence. Participants will rate the frequency with which certain events or situations occurred in their homes during the ages of 5–15 years, using a 5-Point Likert scale (1 = Not at All, 5 = Very Often). Internal consistency reliability of the tool has been found to be good α = 0.86 [13].
-
6)
Generalized Anxiety Disorder – 7 (GAD-7) [22] will measure anxiety based on seven items which are scored from 0 to 3. The scale score can range from 0 to 21 and cut-off scores for mild, moderate and severe anxiety symptoms are 5, 10 and 15 respectively [22]. GAD-7 has demonstrated good internal consistency and convergent validity in heterogeneous samples [23] and has been used within Kenyan settings [24, 25].
-
7)
MyDataHelps App – Online Survey.
MyDataHelps is an application (available on iOS, Android, and web) developed by CareEvolution which provides step-by-step instructions for collecting data from participants via their smartphones [26]. The app acts as a tool for consent, data collection, delivery of study questionnaires, automated notifications, and reminders.
-
8)
Mobile Monitoring.
In addition to completing surveys, the participants will also be asked to wear Fitbit Inspire 2™ (www.fitbit.com) which is a wearable fitness tracker wristband to track daily activity levels, daily mood rating and sleep. The device automatically connects via Bluetooth and transfers data to a mobile platform via a dedicated App. Fitbit Inspire 2™ allows tracking of sleep stages (minutes spent awake, in “light”, “deep”, and “REM” [Rapid Eye Movement] sleep) in addition to sleep/wake states. During set-up, the participants will be prompted to allow MyDataHelps to send them notifications. A notification will be automatically generated on their phone daily and will appear as follows: “On a scale of 1 to 10 what was your average mood today?” They will then respond in the App. We will ask them to complete this daily rating for a period of one year. After completing the consenting process and initial survey via the study App, participants will be given Fitbit Inspire 2. They will be asked to sync the fitness tracker with their phone and wear it daily through to the end of their study year for the purpose of collecting objective data on their daily activity. On the App activities page, participants will be able to track their recent activity data (e.g., how many days they entered mood over the past week, last fitness tracker sync) (see “MyDataHelps App – Dashboard-Activities Screen”). Healthcare workers will also be able to view graphs of their mood, sleep, and step data at any time on the App dashboard. (See Fig. 1)
Sampling Procedure
The healthcare workers will be sampled using random sampling technique on the basis that they meet the following inclusion criteria: voluntary consent to participate in the study; enrolled at the sampled facility as a healthcare worker (including residents) and own a smart phone. Exclusion criteria will be: decline consent to participate in study; has a non-smartphone and HCW’s on locum. This sampling technique is preferred due to the large number of healthcare workers who rotate in these sites. Moreover, though there is as high as 117.2% mobile connections in the country, some participants may not have phones with app access and latest operating systems that are compatible with our data collection devices. The country has been, however, reporting an increase in mobile phone access which may support scalability of the study in future as newer phones come with updated features. Potential participants will be randomly selected from a list with staff names and contacts. They will then be contacted via email or smartphone.
Data collection procedure
We will administer surveys and collect active and passive mobile data on mood and affect over a 12-month period in a Kenyan cohort of 500 healthcare workers, recruited from five health facilities. The frequency of the data collection will vary i.e., daily, monthly and quarterly. The initial data collection day will be the same as the consenting day. Right after the participants give consent through the App (MyDataHelps), a unique identifier will be generated. All consented healthcare workers will then be encouraged to complete the baseline survey. In addition to demographic and baseline psychological information (Neuroticism using the NEO-FFI and Early Family Environment using the Risk Family Questionnaire), the baseline survey will assess anxiety symptoms using GAD-7, suicidal symptoms using PANSI and depressive symptoms using PHQ-9 [14,15,16,17,18]. Participants will also be asked for permission for us to collect active and passive data through their smartphone. On submission of the survey, the healthcare workers will receive a message directing them where they will pick Fitbit Inspire 2.
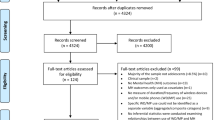
During the 12-month data collection period, participants will respond daily to a validated one-question measure of mood valence via the mobile App (scale of 1 to 10). At 3-month intervals (quarterly) they will also be assessed via the App using a shorter questionnaire designed to assess: (1) current depressive symptoms measured by the PHQ-9, (2) current suicidal symptoms measured by the PANSI, (3) current anxiety symptoms measured by the GAD-7, (4) non-work life stress, (5) COVID-19 experiences, (6) work hours, and (7) perceived medical errors (Table 1). If participants do not respond to the surveys and have not indicated that they do not wish to participate in the study, a reminder will be sent after 3 days of no response (See Fig. 2). The healthcare workers will be compensated (Kenya Shillings 500.00 or USD $4.06 equivalent) for each quarterly survey. Compensation has been shown to reduce attrition rate [27] which may be felt in this study due to lack of resources to buy internet access tokens. In a country where internet access is intermittent and not always freely available, the compensation will aid in having ready internet access during data upload.
Data analysis and presentation
Data will be collected, stored in the cloud database, and checked for completeness daily. Whenever we come across missing data, a reminder will be sent to the respondents after three consecutive days of missed entries, urging them to complete the data entry process. When they opt out of the study, reminders will no longer be sent. Once the study is over, the data will be stored in accordance with guidelines from Kenya’s Data Protection Act 2019 [28], National Institute of Mental Health and Aga Khan University Hospital. For aim 2, we will adapt and test models using mobile data in the domains that are most promising as predictors (sleep behaviors, mood, anxiety) of depression and future mood from the Intern Health Study. This will be used to determine if the predictors identified in the Intern Health Study dataset suggest similar correlates in our Kenyan sample, which would be essential in adapting, developing, and validating individualized risk prediction models for depression and mood. We will identify data driven behavioral phenotypes, derived from mobile data elements, which predict short-term risk for mood changes and depressive episodes.
Modeling approach. The framework for this model was built in 1999 [29, 30], and has been constantly updated.
Circadian phase, sleep drive and performance. We will use our modeling framework to estimate circadian phase and sleep drive in individual subjects. We will compare the Fitbit estimates of individual’s asleep and awake durations, with our predicted sleep drive. The predicted relationship between these variables by our mathematical models will be compared with these datasets, aggregated over the population to refine parameters for the mathematical model, which will represent the behavior of a typical individual. These estimates of circadian and sleep drive have the potential to inform shift work.
Behavioral phenotyping for Mood Prediction. We will make inferences about which behavioral phenotypes are most predictive and evaluate their time-delayed impact upon mood at different time lags. Granger causality [31] is a quantitative framework for assessing the relationship between time series, and has been widely used in econometrics, neuroscience, and genomics to study the temporal causal relations among multiple economic events [31, 32] directional interactions of neurobiological signals [33,34,35] and gene time-course expression levels [36,37,38], respectively. Given two time series \(\text{X}\) and \(\text{Y}\), the temporal structure of the data is used to assess whether the past values of \(\text{X}\), are predictive of future values of \(\text{Y}\), beyond what the past of \(\text{Y}\) can predict alone; if so, \(\text{X}\) is said to Granger cause\(\text{Y}\). Consider the two regression models: (a) \({\text{Y}}_{\text{T}}=\text{A}{\text{Y}}_{1:\text{T}-1}+\text{B}{\text{X}}_{1:\text{T}-1}+{\text{?}}_{\text{t}}\) and (b) \({\text{Y}}_{\text{T}}=\text{A}{\text{Y}}_{1:\text{T}-1}+{\text{?}}_{\text{t}}\), where A is a vector with j-th element is the lag-j effect upon \({\text{Y}}_{\text{T}}\) and B is a vector with j-th element representing the effect of j-th lag of X upon Y. Then X is said to be Granger-causal for Y only if model (a) results in significant improvement over model (b). We will use the multivariate extension of the notion of Granger causality between two variables to p variables, referred to as graphical Granger models (GGM) [39]. GGM uncovers a sparse set of Granger causal relationships amongst the individual univariate time series, for example, to establish the temporal relationship between the daily sleep hours and mood scores. In the GGM, on a given day, a behavioral phenotype is said to be Granger causal for another if the corresponding coefficient for this phenotype and day is significant.
Feature and temporal order selection. We will estimate the strength of association among the mobile phenotypes and their respective associations with the daily mood scores. For example, we will construct the sequence of sleep hours averaged over the past 1, 2 or 7 days and study their respective association with self-reported mood scores. These estimates will directly address two questions: (1) “Which phenotypes and their temporal features predict the daily mood scores?”, and (2) “If a phenotype is predictive of daily mood scores, at what time lags do we observe the strongest predictive strength?” We address these questions via Lasso-type estimates in the context of Granger causality to estimate the effects of variables on each other in a sparse graphical model framework [37]. Important questions including the direction (positive/negative) and the strength of the effect of, say sleep hours on mood scores, can then be answered. Such methods have been known to reduce false positive and false negative rates [37] in inferring the relations among mobile phenotypes and between the mobile phenotypes and the daily mood scores.
Nonlinearity extensions. We will also likely observe nonlinear relationships between the mobile phenotypes and the daily mood scores. We will use kernel-based regression methods to explicitly relax the linear dependence of the outcome upon predictors [40].
Latent variable model for integrating mood scores and PHQ-9 responses. In addition to the daily mood scores, we will also use PHQ-9 scores to assess the study participants’ depressive symptoms. We will use dynamic latent variable models [41] to address the different frequencies at which daily mood scores and PHQ-9 data are collected. We will introduce a daily latent variable that represents the true mood for every subject. The true daily mood will then be informed by both the self-reported mood score and the proximal PHQ-9 survey responses. This approach has been applied to the study of complex disease etiology where multiple measurements with different errors and frequencies are integrated to provide extra statistical precision [39, 42]. The integrated analysis has the advantage of increasing the power of identifying important mobile phenotypes that are predictive of the true mood represented by the latent variable.
Study limitations
Selection and Missing Data Bias. As with in any longitudinal study, missing data may be a problem. We will perform a secondary analysis after accounting for missing data to ensure the absence of missing data biases and to maximize power [43].
Self-Reported Depressive Symptoms. We cannot diagnose major depressive disorders (MDD) using self-reported assessments. However, our self-reporting assessment has several advantages. For instance, the PHQ-9 instrument that we will utilize to measure depressive symptoms has a sensitivity of 88% and a specificity of 88% for a MDD diagnosis with a cut-off of 10 points or higher [15, 44]. Further, there is evidence that in the population of young healthcare workers, maintaining anonymity is of paramount importance to the accurate assessment of sensitive personal information such as depressive symptoms, suggesting that self-reporting may be the most accurate ascertainment method in this population [45].
Accuracy of Mobile Data. The smartphone and wearable devices utilized in this study rely on emerging technology and do not measure parameters of sleep and activity as accurately as gold-standard laboratory tests [46, 47]. While these mobile tools can be used at a scale and in settings that traditional assessment cannot, preliminary evidence suggests that mobile tools produce meaningful and important data [48], we will rigorously monitor their accuracy and upgrade to better technology as it becomes available.
Generalizability: The study healthcare workers are domiciled in hospitals within Nairobi which is a setting characterized by urban and semi-urban dwellings. The results may not depict the mental health status of healthcare workers in rural settings, hence limiting generalizability of our findings. We have however made efforts to enlist participation from the different hospital levels to include public and private hospitals and diverse cadres in ensuring generalizability in respect to hospital infrastructure and staffing and potential scalability in similar health facilities and staffing in urban and semi-urban settings.
Response Bias
We anticipate Hawthorne effects when participants change patterns of behavior due to having devices that they can utilize in monitoring and improving their own wellbeing. There is also a possibility of participants choosing not to wear their Fitbits at certain times due to fatigue or discomfort during sleep. Some of these response behaviors will be difficult to mitigate. However, we have integrated adherence schedules that will help us in following up participants with missing data points for more than a week.
Data Availability
There is no data for sharing now as no data sets have been generated or analyzed.
Change history
12 March 2024
A Correction to this paper has been published: https://doi.org/10.1186/s13104-024-06731-w
Abbreviations
- UM:
-
University of Michigan
- USA:
-
United States of America
- MDD:
-
Major Depressive Disorders IHS:Intern Health Study
- PANSI:
-
Positive and Negative Suicidality Inventory
- GAD 7:
-
Generalized Anxiety Disorder version 7
- PHQ-9:
-
Patient Health Questionnaire version 9
- AI/ML:
-
Artificial Intelligence and Machine Learning
- KNH/UON-ERC:
-
Kenyatta National Hospital and University of Nairobi Ethics Review Board
- NACOSTI:
-
National Commission for Science, Technology and Innovation
- FIC:
-
Fogarty International Center
- AKU:
-
Aga Khan University
- NIBIB:
-
National Institute of Biomedical Imaging and Bioengineering
- NIMH:
-
National Institute of Mental Health
- OD:
-
Office of The Director, National Institutes of Health
- LMICs:
-
Low-and-Middle-Income Countries
References
https://www.who.int/news-room/fact-sheets/detailMental disorders (who.int) [Accessed 25, September 2022].
Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet. 2017;390(10100):1211–59. https://doi.org/10.1016/S0140-6736(17)32154-2.
Mental Health and Wellbeing. Towards happiness and National Prosperity. Ministry of Health; 2020.
Kalmbach DA, Fang Y, Arnedt JT, Cochran AL, Deldin PJ, Kaplin AI, Sen S. Effects of Sleep, Physical Activity, and Shift Work on Daily Mood: a prospective Mobile Monitoring Study of Medical Interns. J Gen Intern Med. 2018;33(6):914–20. https://doi.org/10.1007/s11606-018-4373-2.
Sen S, Kranzler HR, Krystal JH, Speller H, Chan G, Gelernter J, Guille C. A prospective cohort study investigating factors associated with depression during medical internship. Arch Gen Psychiatry. 2010;67(6):557–65. https://doi.org/10.1001/archgenpsychiatry.2010.41.
Lihong C, Zhuo Z, Zhen W, Ying Z, Xin Z, Hui P, Fengtao S, Suhua Z, Xinhua S, Elena F, Srijan S, Weidong L. & Margit B. Prevalence and risk factors for depression among training physicians in China and the United States. 2022;12:8170 https://doi.org/10.1038/s41598-022-12066-y.
Weidong L, Elena F, Zhuo Z, Lihong C, Zhen W, Margit B, Srijan S. Mental Health of Young Physicians in China during the Novel Coronavirus Disease 2019. Outbreak. 2020;3(6):e2010705. 10.1001.
Srijan S, Henry RK, John HK, Heather S, Grace C, Joel G, Constance G. A prospective cohort study investigating factors associated with depression during medical internship. Arch Gen Psychiatry. 2010;67(6):557–65.
Nairobi City Council. Pumwani Maternity Hospital. Retrieved from https://nairobi.go.ke/pumwani-maternity-hospital/. 2021.
Kenyatta National Hospital. History: Kenyatta National Hospital. Retrieved from https://knh.or.ke/index.php/history/ 2017.
Kenyatta University Teaching and Referral Hospital. HOSPITAL PROFILE: Quality-Patient Centred Care. Retrieved from https://kutrrh.go.ke/wp-content/uploads/2021/01/kutrrh-profile-jan-2021.pdf.
Cochran WG. Sampling techniques. New York: John Wiley and Sons, Inc; 1963.
Rice GI, Forte GM, Szynkiewicz M, Chase DS, Aeby A, Abdel-Hamid MS, Crow YJ. Assessment of interferon-related biomarkers in Aicardi-Goutieres syndrome associated with mutations in TREX1, RNASEH2A, RNASEH2B, RNASEH2C, SAMHD1, and ADAR: a case-control study. Lancet Neurol. 2013;12(12):1159–69. https://doi.org/10.1016/S1474-4422(13)70258-8.
Osman A, Gutierrez PM, Kopper BA, Barrios FX, Chiros CE. The positive and negative suicide ideation inventory: development and validation. Psychol Rep. 1998;82(3):783–93. https://doi.org/10.2466/pr0.1998.82.3.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
Cameron IM, Crawford JR, Lawton K, Reid IC. Psychometric comparison of PHQ-9 and HADS for measuring depression severity in primary care. Br J Gen Pract. 2008;58:32–6. https://doi.org/10.3399/bjgp08X263794.
Mwangi P, Nyongesa MK, Koot HM, Cuijpers P, Newton CRJC, Abubakar A. Validation of a Swahili version of the 9-item Patient Health Questionnaire (PHQ-9) among adults living with HIV compared to a community sample from Kilifi, Kenya. J Affect Disorders Rep. 2020;1:100013. https://doi.org/10.1016/j.jadr.2020.100013.
Buysse D, Reynolds C III, Monk T, Berman S, Kupfer D. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Salahuddin M, Maru TT, Kumalo A, Pandi-Perumal SR, Bahammam AS, Manzar MD. Validation of the pittsburgh sleep quality index in community dwelling ethiopian adults. Health Qual Life Outcomes. 2017;15:58. https://doi.org/10.1186/s12955-017-0637-5.
Aloba OO, Adewuya AO, Ola BA, Mapayi BM. Validity of the pittsburgh sleep quality index (psqi) among nigerian university students. Sleep Med. 2007;5:266–70. https://doi.org/10.1016/j.sleep.2007.08.003.
Taylor SE, et al. Early family environment, current adversity, the serotonin transporter promoter polymorphism, and depressive symptomatology. Biol Psychiatry. 2006;60:671–6. https://doi.org/10.1016/j.biopsych.2006.04.019.
Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317–25. pmid:17339617.
Johnson SU, Ulvenes PG, Øktedalen T, Hoffart A. Psychometric properties of the general anxiety disorder 7-Item (GAD-7) scale in a heterogeneous psychiatric sample. Front Psychol. 2019;10:1713. https://doi.org/10.3389/fpsyg.2019.01713.
Nyongesa MK, Mwangi P, Koot HM, Cuijpers P, Newton CRJC, Abubakar A. The reliability, validity and factorial structure of the Swahili version of the 7-item generalized anxiety disorder scale (GAD-7) among adults living with HIV from Kilifi, Kenya. Ann Gen Psychiatry. 2020;19:62. https://doi.org/10.1186/s12991-020-00312-4.
Osborn TL, Venturo-Conerly KE, Wasil AR, Schleider JL, Weisz JR. Depression and anxiety symptoms, social support, and demographic factors among kenyan high school students. J Child Fam Stud. 2020;29:1432–43. https://doi.org/10.1007/s10826-019-01646-8.
www.support.mydatahelps.org/hc/en-us.MyDataHelps™ Designer Help Center [Accessed 16, September 2022].
Appleby L, Morriss R, Gask L, Roland M, Perry B, Lewis A, Faragher B. An educational intervention for front-line health professionals in the assessment and management of suicidal patients (the STORM Project). Psychol Med. 2000;30(4):805–12. https://doi.org/10.1017/s0033291799002494.
www.kenyalaw.org/kl/fileadmin/pdfdownloads/Acts/2019/TheDataProtectionAct__No24of2019.pdf(kenyalaw.org)TheDataProtectionAct__No24of2019.pdf (kenyalaw.org) [Accessed 16, September 2022]
Forger DB, Jewett ME, Kronauer RE. A simpler model of the human circadian pacemaker. J Biol Rhythms. 1999;14(6):532–7. https://doi.org/10.1177/074873099129000867.
Walch OJ, Cochran A, Forger DB. A global quantification of normal sleep schedules using smartphone data. Sci Adv. 2016;2(5):e1501705. https://doi.org/10.1126/sciadv.1501705.
Cross-Disorder Group of the Psychiatric Genomics Consortium. Electronic address, p. m. h. e., & Cross-Disorder Group of the Psychiatric Genomics, C. Genomic Relationships, Novel Loci, and Pleiotropic Mechanisms across Eight Psychiatric Disorders. Cell,. 2019; 179(7), 1469–1482 e1411. https://doi.org/10.1016/j.cell.2019.11.020.
Jacob KS, Sharan P, Mirza I, Garrido-Cumbrera M, Seedat S, Mari JJ, Saxena S. Mental health systems in countries: where are we now? Lancet. 2007;370(9592):1061–77. https://doi.org/10.1016/S0140-6736(07)61241-0.
Marques DF, Ota VK, Santoro ML, Talarico F, Costa GO, Spindola LM, Belangero S. I. LINE-1 hypomethylation is associated with poor risperidone response in a first episode of psychosis cohort. Epigenomics. 2020;12(12):1041–51. https://doi.org/10.2217/epi-2019-0350.
Sharan P, Gallo C, Gureje O, Lamberte E, Mari JJ, Mazzotti G, World Health Organization-Global Forum for Health Research - Mental Health Research Mapping Project, G. Mental health research priorities in low- and middle-income countries of Africa, Asia, Latin America and the Caribbean. Br J Psychiatry. 2009;195(4):354–63. https://doi.org/10.1192/bjp.bp.108.050187.
Thornicroft G, Alem A, Antunes Dos Santos R, Barley E, Drake RE, Gregorio G, Wondimagegn D. WPA guidance on steps, obstacles and mistakes to avoid in the implementation of community mental health care. World Psychiatry. 2010;9(2):67–77. https://doi.org/10.1002/j.2051-5545.2010.tb00276.x.
Ota VK, Santoro ML, Spindola LM, Pan PM, Simabucuro A, Xavier G, Belangero S. I. Gene expression changes associated with trajectories of psychopathology in a longitudinal cohort of children and adolescents. Transl Psychiatry. 2020;10(1):99. https://doi.org/10.1038/s41398-020-0772-3.
Pan PM, Sato JR, Salum GA, Rohde LA, Gadelha A, Zugman A, Stringaris A. Ventral striatum functional connectivity as a predictor of adolescent depressive disorder in a Longitudinal Community-Based sample. Am J Psychiatry. 2017;174(11):1112–9. https://doi.org/10.1176/appi.ajp.2017.17040430.
Synofzik M, Gonzalez MA, Lourenco CM, Coutelier M, Haack TB, Rebelo A, Zuchner S. PNPLA6 mutations cause Boucher-Neuhauser and Gordon Holmes syndromes as part of a broad neurodegenerative spectrum. Brain. 2014;137(Pt 1):69–77. https://doi.org/10.1093/brain/awt326.
Boukhris A, Schule R, Loureiro JL, Lourenco CM, Mundwiller E, Gonzalez MA, Stevanin G. Alteration of ganglioside biosynthesis responsible for complex hereditary spastic paraplegia. Am J Hum Genet. 2013;93(1):118–23. https://doi.org/10.1016/j.ajhg.2013.05.006.
Thomas PK, Marques W Jr, Davis MB, Sweeney MG, King RH, Bradley JL, Harding AE. The phenotypic manifestations of chromosome 17p11.2 duplication. Brain. 1997;120(Pt 3):465–78. https://doi.org/10.1093/brain/120.3.465.
Cortese A, Tozza S, Yau WY, Rossi S, Beecroft SJ, Jaunmuktane Z, Reilly MM. Cerebellar ataxia, neuropathy, vestibular areflexia syndrome due to RFC1 repeat expansion. Brain. 2020;143(2):480–90. https://doi.org/10.1093/brain/awz418.
Sen S, Nesse RM, Stoltenberg SF, Li S, Gleiberman L, Chakravarti A, Burmeister M. A BDNF coding variant is associated with the NEO personality inventory domain neuroticism, a risk factor for depression. Neuropsychopharmacology. 2003;28(2):397–401. https://doi.org/10.1038/sj.npp.1300053.
Raghunathan TE. What do we do with missing data? Some options for analysis of incomplete data. Annu Rev Public Health. 2004;25:99–117. https://doi.org/10.1146/annurev.publhealth.25.102802.124410.
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of Mental Disorders. Patient Health Questionnaire JAMA. 1999;282(18):1737–44. https://doi.org/10.1001/jama.282.18.1737.
Myers M. On the importance of anonymity in surveying medical student depression. Acad Psychiatry. 2003;27(1):19–20. https://doi.org/10.1176/appi.ap.27.1.19.
Chow JJ, Thom JM, Wewege MA, Ward RE, Parmenter BJ. Accuracy of step count measured by physical activity monitors: the effect of gait speed and anatomical placement site. Gait Posture. 2017;57:199–203. https://doi.org/10.1016/j.gaitpost.2017.06.012.
Kang SG, Kang JM, Ko KP, Park SC, Mariani S, Weng J. Validity of a commercial wearable sleep tracker in adult insomnia disorder patients and good sleepers. J Psychosom Res. 2017;97:38–44. https://doi.org/10.1016/j.jpsychores.2017.03.009.
Steinhubl SR, Muse ED, Topol EJ. The emerging field of mobile health. Sci Transl Med. 2015;7(283):283rv283. https://doi.org/10.1126/scitranslmed.aaa3487.
Acknowledgements
We would like to acknowledge the healthcare facilities and administration who have already provided permission to set up the study.
Funding
Research reported in this publication was supported by the Office of The Director, National Institutes of Health (OD), the National Institute of Biomedical Imaging and Bioengineering (NIBIB), the National Institute of Mental Health (NIMH), and the Fogarty International Center (FIC) of the National Institutes of Health under award number U54TW012089 (AA* and AK*). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
LA, AA*, ZM*, AKW* AKN, WA, ZW, FE, WJ and SS conceptualized the study. WN, AA, LK, MNK, and RM carried out community engagement meetings to align the potential participants needs to study procedures. LA, AA*, AKW*, ZM*, AKN, ZW, EMWH, JAB, FE, JW, SS, JO, SW, JS, and RM designed the study and ensured alignment to ethics guidelines. WN and RM wrote the first draft of the manuscript. All authors critically reviewed subsequent versions of the manuscript and approved the final version for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study ethical approval will be sought from the Institutional Review Boards of the University of Michigan and Aga Khan University. We recognize that a country’s legal and ethical requirements may differ. We will, therefore, apply for ethics review and approval from Kenyan institutional review boards. Aga Khan University Hospital’s - Institutional Review Ethics Committee (IREC), Kenyatta University - Ethics Review Committee (KU-ERC) and Kenyatta National Hospital - University of Nairobi Ethics Review Committee (KNH-UON ERC) approval will be sought before commencement of the study. In addition, we will seek regulatory approvals from the National Commission for Science Technology and Innovation (NACOSTI) as well as Nairobi County and Nairobi Metropolitan Services. The study protocol will be conducted in accordance with the declaration of Helsinki and a written informed consent will be obtained from all the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised to correct co-author Elena Frank’s name.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Njoroge, W., Maina, R., Frank, E. et al. Use of mobile technology to identify behavioral mechanisms linked to mental health outcomes in Kenya: protocol for development and validation of a predictive model. BMC Res Notes 16, 226 (2023). https://doi.org/10.1186/s13104-023-06498-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-023-06498-6