Abstract
Background
The national antiretroviral therapy in the Republic of Chad provides free of charge antiretroviral regimens and therapeutic monitoring for patients receiving antiretroviral therapy nationwide. For a successful programmatic uptake, these efforts merit to be supported by thorough assessments of antiretroviral therapy response and HIV-1 drug resistance surveillance, especially with risks of cross-resistance due to the gradual stavudine phasing out in such national settings. We therefore evaluated the virological response to antiretroviral therapy, HIV-1 drug resistance emergence and circulating HIV-1 clades in a Chad context. A cross-sectional and prospective study was conducted among 116 patients (41 [δ ± 6.87] years, 59% female) receiving first-line antiretroviral therapy for ≥ 6 months in Ndjamena, Chad, in 2011–2012, enrolled consecutively. To ensure accuracy, plasma viral load was concomitantly measured using Abbott Real-Time and Cobas AmpliPrep/TaqMan (v2.0), and virological failure defined as ≥ 1000 HIV-1 RNA copies/ml. Plasma from patients experiencing virological failure were processed for sequencing of HIV-1 protease-reverse transcriptase using the ANRS-AC.11 resistance testing protocol; drug resistant mutations were interpreted using the ANRS-AC11 algorithm; and phylogenetic analysis was performed using MEGA.v.6.
Results
Majority of patients was receiving zidovudine plus lamivudine plus nevirapine (46%), stavudine plus lamivudine plus nevirapine (41%) and tenofovir plus emtricitabine plus efavirenz (11%), for a median time-on-treatment of 5 [IQR 4–7] years. The rate of virological failure was 43% (50/116), with 86% (43/50) sequencing performance. Overall, 32% (37/116) patients presented ≥ one major drug resistant mutation(s), with 29% (34/116) to nucleos(t)ide reverse transcriptase inhibitors (67% [29/43] M184V/I, 30% [13/43] T215Y/F, 19% [8/43] V75A/F/I/L/M, 9% [4/43] K70P/R/W, 9% [4/43] K219E/N/Q and 5% [2/43] A62V); 86% (37/43) to non-nulceos(t)ide reverse transcriptase inhibitors (30% [13/43] K103N/S/E, 26% [11/43] Y181C/V/F/L, 2% [1/43] L100I, 2% [1/43] F227L, 2% [1/43] P225H); and 2% (1/43) to protease inhibitors (M46I, I54V, V82S). Six HIV-1 subtypes were found: 30% circulating recombinant form (CRF02_AG), 30% J, 16% G, 9% A, 9% D, 5% F.
Conclusions
In Chad, almost half of patients are failing first-line antiretroviral therapy after 5 years, with considerable drug resistant mutations at failure. Absence of K65R supports the use of tenofovir-containing regimens as preferred first-line and as suitable drug for second-line combinations, in this setting with significant HIV-1 genetic diversity.
Similar content being viewed by others
Background
HIV/AIDS remains a major cause of death worldwide, and especially in sub-Saharan Africa (SSA) where over 71% of the global AIDS epidemic is concentrated in only 12% of the world population. In spite of a reduction in HIV-associated morbidity and mortality in SSA, about half of people living with HIV (PLHIV) still ignore their status, suggesting a potential growing burden of HIV in this region of the world [1,2,3].
Located in central Africa, Chad is a country with 3.3% of HIV prevalence in the sexually active population (i.e. 15–45 years) for a national population of 11.4 million inhabitants [4,5,6]. Interestingly, Chad is the fifth largest African country, partly bordered by Cameroon, a country known as the epicenter of HIV with a broad genetic diversity that includes several HIV-1 groups M, N, O and P, and HIV-2, as well as several subtypes and recombinants [7,8,9,10,11]. HIV-1 group-M predominates the molecular epidemiology in Chad (subtypes A, D, F, G, CRF01_AE, CRF02_AG and CRF11_cpx); few cases of group O have been reported while groups N and P, while HIV-2 have never been identified [10, 12, 13]. Exploring the extent of HIV diversity in Chad would therefore provide updates and related impact on the dynamics of national AIDS epidemics for relevant policy-making [14].
ART management and laboratory monitoring are effective and free-of-charge in the national AIDS program in Chad since 2007, with first-line regimens consisting of two nucleoside reverse transcriptase inhibitor (NRTI) and one non-NRTI (NNRTI). As per the World Health Organization (WHO) recommended guidelines, preferred first-line regimens since 2012 consist of “tenofovir (TDF), emtricitabine (FTC) and efavirenz (EFV)” or “zidovudine (AZT), lamivudine (3TC) and nevirapine (NVP)”; following phasing-out of Triomune due to lipodistrophy/lipoatrophy and peripheral neuropathy significantly associated with “stavudine” (d4T)-containing regimens [5, 8, 14]. However, at the moment of the study, viral load testing was implemented only at the national reference hospital laboratory. Viral load was mainly performed as needed, after treatment failure based on immunological and/or clinical parameters, thus indicating a limited accessibility to virological monitoring nationwide during the study period. Thus, mastering HIVDR profile in such context will help in predicting potential cross-resistance to currently used regimens [14, 15].
As first-line regimens used in Chad mainly consist of drugs with low-genetic barriers to resistance, risks of HIV-1 drug resistance (HIVDR) emergence are concerning. Of note, over 60% of ART failure was previously reported [14, 16], supporting the need for local HIVDR surveillance to sustain the effectiveness of first-line ART, to inform on the selection of active NRTI for second-line combinations, to generate evidence on the dynamics of HIV-1 genetic diversity and potential relevance on therapeutic response for patients receiving ART according to the current national treatment program [5, 6].
In this study, we sought to ascertain the rate of virological failure (VF), the level of drug resistance mutations and HIV-1 genetic diversity among people living with HIV (PLHIV) receiving first-line ART as per the Chadian AIDS program in N’Djamena.
Methods
Study design and population
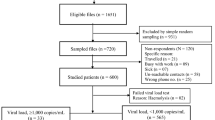
A prospective and cross-sectional study was conducted in PLHIV receiving first-line ART at the National Reference General Hospital of N’djamena (Hôpital Général de Référence National de Ndjaména) in Chad, between 2011 and 2012. This hospital was selected as sentinel site based on its role as the national reference center in Chad, its long-term experience on ART and its technical capacity in providing reference laboratory monitoring for ARV management. Participants were eligible if: (a) receiving first-line ART for ≥ 6 months, (b) self-reported adherent to prescribed ARV medications, (c) registered and followed-up on ART at the study clinic, and (d) providing consent as study participants.
Sampling method
A non-probability sampling was used, by which patients were conveniently enrolled based on accessibility throughout the study period.
Following informed consent, participants were interviewed and assessed for eligibility criteria, then enrolled as study participants if eligible.
Whole blood was collected in two EDTA tubes of 4 ml each, through venipuncture, and plasma was collected following centrifugation at 2000g for 10 min. Plasma aliquots of 1 ml were prepared and stored at − 80 °C.
Measurement of TCD4 lymphocytes
To evaluate the stage of disease progression, CD4 T lymphocytes were measured for all patients at baseline and at 6 [± 2] months of ART, based on the fluorescent activated cell sorting approach, using the commercially available FACS Count as per the manufacturer’s instructions (Becton–Dickinson Immunocytometry Systems, USA).
Measurement of plasma viral load
Plasma viral load (PVL) was performed at the AIDS Reference Laboratory of the University Health Center (Laboratoire de Référence Sida du CHU) in Liege, Belgium, using two different approaches purposely to ensure accuracy on these non-B viral populations: (1) COBAS® AmpliPrep/CobasTaqman® HIV-1 version 2.0 (v2.0) which is based on in vitro amplification of HIV-1 RNA from plasma with detection thresholds ranging from 20 (lower) to 10,000,000 (upper) RNA copies/ml designed specifically for HIV-1 groups M and O; (2) the Abbott RealTime HIV-1 test Ref 2G3190 which is based on in vitro amplification by RT-PCR for the quantification of HIV-1 in plasma. Both PVL tests were performed as per manufacturers’ instructions.
VF was defined as PVL ≥ 1000 HIV-1 RNA copies/ml; plasma samples from study participants experiencing VF were designated for HIV-1 sequencing for the detection of DRMs and for viral subtyping.
RNA extraction, amplification and sequencing
RNA extraction
RNA extraction was performed on plasma using the QIAamp mini kit (Qiagen, Courtaboeuf, France), as per the manufacturer’s instructions. Briefly, 140 µl plasma samples stored at − 80 °C was extracted using lysis and wash buffers, followed by elution of 60 µl RNA.
Amplification and Sequencing reactions
The ANRS AC11 protocol was used for amplification and sequencing of the protease (PR) and reverse transcriptase (RT) regions of HIV-1, using GeneAmp PCR System 9700 thermal cycler [17]. Briefly, amplification was performed using Titan One tube RT-PCR Kit version 13 (Boehringer Mannheim, Manneheim, Germany), with a first-round PCR using primers amplifying 941 bp of RT (MJ3/MJ4) and 653 bp that encompasses the entire PR (5′Prot1/3′Prot1) region. Second-round (nested) PCR was performed with primers A35/NE(1)35 covering 731 bp of RT and primers 5′prot2/3′prot2 covering 507 bp that encompasses the entire PR. Alternative outer primers used for RT were RT18/RT21 and for PR 5′eprB/3′eprB, while alternative nested primers were RT1/RT4 for RT and 5′prB/3′prB for PR regions. Primer sequences are provided in Additional file 1.
Revelation of PCR products was done using 4% ethidium bromide agarose gel electrophoresis, with an expected size of 731 pb for RT and 507 for PR, including positive and negative controls alongside a molecular ladder (Tacklt ™ ΦX174 RF DNA/Hae III Fragment). Amplicons were purified PCR using NucleoFast® 96 PCR (Macherey–Nagel).
As per the ANRS AC11 protocol, HIV-1 PR-RT was sequenced using overlapping primers by deoxyterminators [17]. Sequences were purified using resin Sephadex G-50, and identified following capillary electrophoresis on a “3730” genetic analyzer of Applied Biosystem (ABI).
Interpretation of HIV-1 drug resistance
Following the sequencing protocol used [17], HIV-1 DRMs were interpreted according to the ANRS AC11 algorithm (http://www.hivfrenchresistance.org/). Viruses with a mutant or a mixture of wild type and mutant, at an amino acid’s position, were considered to have the resistant variant. Patients were considered as harbouring wild type viruses if their viral load was < 1000 RNA copies/ml (virological success) or with a non-amplifiable sample.
HIV-1 phylogenetic analysis
Sequence alignment was done using CLUSTAL W version 1.7, then sequences were trimmed and gaps closed [18]. Phylogenetic inference was performed with MEGA version 6 [19], using Neighbor Joining with 1000 replicates and Kimura two-parameter [20, 21]. Subtypes were assigned for bootstrap ≥ 70% with a reference sequences from a pure HIV-1 subtype or recombinant strain obtained from Genbank (http://www.hiv.lanl.gov/).
Statistical analysis
Data were processed using EPI INFO version 3.3.2. Chi square test was used for analysing categorical data on VF according to ART regimens, including 95% CI, with a P < 0.05 considered statistically significant. Spearman correlation was used for quantitative data on PVL results obtained from the two different instruments, with R ≥ 0.8 considered as a strong positive correlation.
Results
Profile of study participants
Overall, 116 PLHIV treated at the National Reference General Hospital of N’djamena were enrolled in the study, divided into 59% (68) female versus 41% (48) male. Mean age of these participants was 41 (± 6.87) years, min–max: 17–84 years (Additional file 2). Median CD4 was 248 [interquartile range (IQR) 145; 504] cells/mm3, min–max: 11–684 cells/mm3.
Among study participants, the median time-on-ART was 5 [IQR 4; 7] years. In terms of first-line drug regimens commonly prescribed at the study period, 87% (101/116) were receiving nevirapine (NVP) plus lamivudine (3TC) plus zidovudine (AZT) or stavudine (d4T), followed by 11% on a tenofovir-containing regimen (Table 1).
Viral measurements and virological response to first-line ART
All one hundred and sixteen study participants were tested for PVL using both described quantitation assays (Cobas AmpliPrep/TaqManv2.0 and Abbott Real time HIV-1), and 109 samples yield comparable levels of HIV-1 RNA copies between both assays. A strong positive correlation (R2 = 0.96016) was observed between both PVL assays (Fig. 1), with only two samples reported “not detected” with Abbott Real time HIV-1 and detected as low-levels (2.23 and 2.68 Log10 RNA copies/ml) viremia with Cobas AmpliPrep/TaqMan v2.0. Overall, both PVL assays accurately detect all patients with VF (≥ 1000 HIV-1 RNA copies/ml). Further characteristics of the two assays are provided in Additional file 3.
Out of 116 participants, 50 (43%) experienced VF. Between the two most prescribed regimens, VF was higher with d4T-containing (49% [24/49]) compared to other regimens (39% [26/67]), odd ratio (OR): 1.514 [95% CI 0.672–3.417), P = 0.274 (see Table 2).
The low number of participants on the other regimens could not allow a relevant statistical evaluation of response to ART.
HIV-1 drug resistance mutations
Sequencing performance
All 50 samples from patients classified as VF (PVL ≥ 1000 HIV-1 RNA copies/ml) were processed for HIV-1 genotypic resistance testing (GRT), resulting to 86% (43/50) sequencing performance with the ANRS AC11 genotyping protocol [17].
HIV-1 mutations associated with resistance to reverse transcriptase inhibitors
The overall rate of patients with DRMs to reverse transcriptase inhibitors was 32% (37/116), including both nucleoside and non-nucleoside inhibitors.
Thirty-four participants had at least one major DRM to nucleoside reverse transcriptase inhibitors (NRTIs), resulting to 29% (34/116) prevalence of NRTI DRMs in the entire study population. Out of the 43 sequences generated, the most prevalent DRMs were: (67% [29/43] M184V/I, 30% [13/43] T215Y/F, 19% [8/43] V75A/F/I/L/M, 9% [4/43] K70P/R/W, 9% [4/43] K219E/N/Q and 5% [2/43] A62V, followed by other DRMs observed at low rates (Fig. 2).
Thirty-seven participants had at least one major DRM to non-nucleoside reverse transcriptase inhibitors (NNRTIs), resulting to 32% (37/116) prevalence in the entire study population. Out of the 43 sequences generated, the most prevalent DRMs were: 30% [13/43] K103N/S/E, 26% [11/43] Y181C/V/F/L, 2% [1/43] L100I, 2% [1/43] F227L and 2% [1/43] P225H, followed by other DRMs observed at lower rates. Of note, Y181C/F and K103N were observed concomitantly in three (7%) cases. Thus, in the entire study population, NNRTI DRMs exhibit 28% (32/116) and 21% (24/116) high-level resistance to nevirapine and efavirenz respectively (Fig. 3).
OF note, six (12%) patients, classified as VF, were reported without any DRMs, suggesting possible poor adherence in spite of the self-reported adherence registered prior to enrolment. The list of genotypic scores associated to each RTI is provided in Additional file 4.
HIV-1 mutations associated with resistance to protease inhibitors
Only one patient (< 1%) was reported with major DRMs to protease inhibitors (PI/r), among which M46I, I54V, and V82S, indicating either an event of transmitted PI-associated DRMs or unknown past-exposure to PIs. Minor mutations found were mainly polymorphisms: K20I/M (21), L10I/V (15), L90W (1), L76S (1), N88D (1), V11I (1), V32L (1) and G48R (1).
HIV-1 genetic diversity
The 43 protease-RT sequences generated clustered within six clades (five pure subtypes and one recombinant). Of note, the two equally most prevailing were subtype J (30%) and CRF02_AG (30%), followed by subtypes G (16%), A (9%), D (9%) and F (5%), as shown in Fig. 4.
Phylogenetic tree. The evolutionary history was inferred using the Neighbor-Joining method in the protease-reverse transcriptase regions (Saitou and Nei [20]). The tree is drawn to scale, with branch lengths in the same units as those of the evolutionary distances used to infer the phylogenetic tree. The evolutionary distances were computed using the Kimura 2-parameter method (Kimura [21]) and are in the units of the number of base substitutions per site. The analysis involved 43 query nucleotide sequences. All positions containing gaps and missing data were eliminated. Evolutionary analyses were conducted in MEGA6 (Tamura et al. [19])
Discussion
The success of combination ART has remarkably changed the paradigm in the AIDS epidemics globally. However, such achievements could rapidly be hampered in settings where ART is mainly based on drugs with low genetic barrier to resistance [14, 22, 23]. Since PLHIV in Chad are treated with RTI- or PI/r-containing regimens, evaluating the virological response, acquired HIVDR and circulating strains are of great programmatic asset in sustaining ART performance in a medium-long run [6, 15, 16].
Our findings indicated that, about 5 years after ART initiation, almost half of PLHIV on first-line NRTI/NNRTI regimens in Chad would be experiencing VF, suggesting close virological monitoring is needed in the country ART program [15, 24,25,26,27]. More importantly, as higher (though non-significant) rate of VF was observed with d4T-containing regimens (49% vs. 39% for other regimens, OR = 1.514), added to the known adverse effects of this, our findings support effective phasing-out of d4T from first-line ART regimens from this setting, while monitoring for cross-resistance to AZT and other NRTIs commonly used in first- and second-line combinations [6, 14, 28].
The high rate of VF in our cohort could be attributed to infrequent PVL measurement in 2011–2012 due to the centralized system, thus resulting to delayed testing and suboptimal monitoring. At the moment of the study, VL was possible only at the National Reference General Hospital of N’djamena, the only facility nationwide whereby VL is routinely offered since 2005 to date. Presently, the Entre-aide 92 team from Paris is assessing the feasibility of using GeneXpert for point-of-care VL in the cities of Moundou and Am Timan, in order to scale-up access to VL in Chad [29]. Therefore, although based on a limited sample, our findings could be representative of the general country situation.
Amongst those experiencing VF, relatively lower rates of NRTI and NNRTI mutations were found, possibly due to suboptimal adherence, in the frame of poor ART monitoring. This calls for an improved adherence support to enhance and sustain viral suppression in the country [29].
For an accurate evaluation of virological response, a strong positive correlation in PVL was reported for samples tested concomitantly with two different platforms, which in turns confirms assay reliability in settings where non-B HIV-1 prevails [23]. Of note, the two discrepant cases were patients with low-level PVL (< 1000 copies/ml), both clinically classified as virological success [3], or blips (transient rebound in PVL returning to undetectable levels with adherence) [8].
As levels of acquired HIVDR are higher to NNRTIs (32%) compared to NRTIs (29%), conferring high-level resistance to NVP and EFV (mainly due to K103N and Y181C), NRTIs are more prone for use in second-line combinations in such ART program [30,31,32]. Of note, K65R, the main DRM to TDF was not detected, supporting TDF-containing NRTIs as preferred combinations to second-line LPV/r, as globally recommended [3, 14]. Moreover, our data also support using the combination of TDF plus (FTC or 3TC) plus EFV as the most prominently active first-line regimen in such RLS, at the moment [9, 14]. Even though 3TC and FTC are highly hampered by M184V (~ 29%) in the overall study population, the ability of this mutation in decreasing viral replicative fitness and in improving susceptibility to thymidine analogs suggest maintaining these drugs (3TC and FTC) within current treatment guidelines [3, 9, 33, 34]. Very low resistance to ABC also favors this drug as a suitable NRTI substitute for second-line combination, especially in case of counter indication to TDF [3, 35, 36]. Most importantly, the very low-level of HIVDR to PI/r confirms the suitability to LPV/r, ATV/r and other PI/r as backbone for second-line ART, in combination with potentially active NTRIs [3, 6, 9, 13].
A higher prevalence of CRF02_AG was found in Chad as compared to previous findings [10, 12], possibly due the ability of AG-recombinant in being more infectious but with less cytopathic effect [37,38,39,40]. Our small sample (43 sequences) therefore calls for enlarged molecular epidemiology studies to better understand the HIV-1 genetic diversity, its evolution overtime and related clinical relevance in the country [41].
A study limitation would be the “self-reported” adherence, making it difficult to verify the reliability of recalls. Phasing out of D4T may suggest not representativeness of the data on current ART regimens. However, D4T is the same drug class with AZT (analogs of TAMs), and several patients have been exposed to these drugs. Our findings are therefore useful for all patients with past-exposure to the drug class of TAMs [42, 43].
Complementary studies are needed to ascertain response after switch from first- to second-line [9, 44, 45], to evaluate the feasibility of point-of-care resistance testing designed with commonly found mutations (M184V/I, T215mutants, K103N, Y181C) for greater cost-effectiveness [46, 47], and monitoring HIVDR early warning indicators [48].
Programmatic implications for the ART program in Chad
Our findings address issues that could be translated into policies. Of note, in addition to the need for closed viral load monitoring for timely detection of treatment failures, the high failure rate of ART in Chad also indicates a rapid switch of patients from first- to second-line ART regimens. Rapid switch to second-line ART lead to increased costs of ARVs provision for the national HIV program in Chad, thus representing a major programmatic challenge for such RLS. Interestingly, the unusually low rate of DRMs, developing after significant periods of treatment failure, suggests suboptimal adherence, thereby underscores the usefulness to closely monitor ART adherence and the need for confirming VF (i.e. a second viral load after counselling and adherence support) before deciding on ART switch. Such measure would help clinicians in distinguishing elevated viremia due to non-adherence, thereby limiting unnecessary switch to second-line regimens while saving related-costs in the national ART program of Chad.
Conclusions
About half of Chadian PLHIV experienced VF by medium-term after ART initiation, suggesting closed virological monitoring using commonly available commercial assays. For successful phasing-out of d4T, DRMs supports using current WHO-recommended TDF plus TFC (or 3TC) plus EFV as preferred first-line regimen in Chad, while LPV/r is potentially active as second-line backbone, alongside “TDF” or “ABC”, in association with NRTIs. The predominant rate of recombinant AG is a quest for further investigation within the sub-region.
Abbreviations
- 3TC:
-
lamivudine
- ABI:
-
applied biosystem
- AIDS:
-
acquired immunodeficiency syndrome
- ANRS:
-
agence nationale pour la recherche sur le SIDA et les hépatitis virales
- ARV:
-
antiretroviral
- ART:
-
antiretroviral therapy
- AZT:
-
zidovudine
- CHU:
-
centre hospitalier universitaire
- D4T:
-
stavudine
- DRM:
-
drug resistance mutation
- EDTA:
-
ethidium diamine tetra acetate
- EFV:
-
efavirenz
- FACS:
-
fluorescent activated cell sorting
- FTC:
-
emtricitabine
- HIVDR:
-
HIV-1 drug resistance
- HIV:
-
human immunodeficiency virus
- MEGA:
-
molecular evolutionary genetics analysis
- NNRTI:
-
non-nucleoside reverse transcriptase inhibitor
- NRTI:
-
nucleoside reverse transcriptase inhibitor
- NVP:
-
nevirapine
- PCR:
-
polymerase chain reaction
- PLHIV:
-
people living with HIV
- PVL:
-
plasma viral load
- PR:
-
protease
- RLS:
-
resource-limited setting
- RNA:
-
ribonucleic acid
- RT:
-
reverse transcriptase
- RT-PCR:
-
reverse-transcriptase polymerase chain reaction
- SSA:
-
sub-Saharan Africa
- TAM:
-
thymidine analog mutation
- TDF:
-
tenofovir
- WHO:
-
World Health Organization
References
Joint United Nations Programme on HIV/AIDS. The Gap Report. Geneva: UNAIDS; 2014. http://www.unaids.org/en/resources/documents/2014/name,97466,en.asp. Accessed 15 Jun 2015.
World Health Organisation. Global summary of the HIV/AIDS epidemic. Geneva: World Health Organisation; 2014. http://www.who.int/hiv/data/epi_core_dec2014.png?ua=1. Accessed 15 Jun 2015.
World Health Organisation. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach. Geneva: World Health Organisation; 2013. http://www.who.int/hiv/pub/guidelines/arv2013/en/. Accessed 15 Jun 2015.
Sigaloff KC, Hamers RL, Menke J, Labib M, Siwale M, Ive P, et al. Early warning indicators for population-based monitoring of HIV drug resistance in 6 African countries. Clin Infect Dis. 2012;54(Suppl 4):S294–9. https://doi.org/10.1093/cid/cir1015.
Republique du Tchad. Programme National de Lutte contre le Sida. Cadre strategique national de lutte contre le VIH/Sida et les IST 2007-2011; Ndjamena, Mai 2007. http://www.africanchildforum.org/clr/policy%20per%20country/chad/chad_aids_2007-2011_fr.pdf.
Adawaye C, Kamangu E, Djibrine SI, Mahamat MA, Tchombou HZ, Vaira D, et al. Immunovirologic Evaluation of Triomune (Lamivudine, Stavudine and Nevirapine) Antiretroviral Therapy in first line HIV-1 adult patients in N’Djamena, Chad. World J AIDS. 2014;4:3.
Plantier J-C, Leoz M, Dickerson JE, De Oliveira F, Cordonnier F, Lemée V, et al. A new human immunodeficiency virus derived from gorillas. Nat Med. 2009;15(8):871–2.
World Health Organisation. HIV drug resistance report 2012. Geneva: World Health Organisation; 2012. http://www.who.int/hiv/pub/drugresistance/report2012/en/. Accessed 15 Jun 2015.
Fokam J, Salpini R, Santoro MM, Cento V, Perno CF, Colizzi V, et al. Drug resistance among drug-naive and first-line antiretroviral treatment-failing children in Cameroon. Pediatr Infect Dis J. 2011;30(12):1062–8. https://doi.org/10.1097/INF.0b013e31822db54c.
Lihana RW, Ssemwanga D, Abimiku A, Ndembi N. Update on HIV-1 diversity in Africa: a decade in review. AIDS Rev. 2012;14(2):83–100.
Billong SC, Fokam J, Aghokeng AF, Milenge P, Kembou E, Abessouguie I, et al. Population-based monitoring of emerging HIV-1 drug resistance on antiretroviral therapy and associated factors in a sentinel site in Cameroon: low levels of resistance but poor programmatic performance. PLoS ONE. 2013;8(8):e72680. https://doi.org/10.1371/journal.pone.0072680 (eCollection 2013).
Vidal N, Koyalta D, Richard V, Lechiche C, Ndinaromtan T, Djimasngar A, Delaporte E, Peeters M. High genetic diversity of HIV-1 strains in Chad, West Central Africa. J Acquir Immune Defic Syndr. 2003;33(2):239–46.
Doualla-bell F, Turner D, Loemba H, Petrella M, Brenner B, Wainberg MA. Résistance du VIH aux antirétroviraux: conséquences pour les pays à faibles revenus. MS Rev. 2004;20(10):835–940.
Tang MW, Rhee SY, Bertagnolio S, Ford N, Holmes S, Sigaloff KC, et al. Nucleoside reverse transcriptase inhibitor resistance mutations associated with first-line stavudine-containing antiretroviral therapy: programmatic implications for countries phasing out stavudine. J Infect Dis. 2013;15(207 Suppl 2):S70–7. https://doi.org/10.1093/infdis/jit114.
Koyalta D, Charpentier C, Beassamda J, Rey E, Si-Mohamed A, Djemadji-Oudjeil N, Bélec L. High frequency of antiretroviral drug resistance among HIV-infected adults receiving first-line highly active antiretroviral therapy in N’Djamena, Chad. Clin Infect Dis. 2009;49(1):155–9.
Wojewoda CM, Spahlinger T, Harmon ML, Schnellinger B, Li Q, Dejelo C, et al. Comparison of Roche Cobas AmpliPrep/Cobas TaqMan HIV-1 test version 2.0 (CAP/CTM v2.0) with other real-time PCR assays in HIV-1 monitoring and follow-up of low-level viral loads. J Virol Methods. 2013;187(1):1–5.
ANRS AC11 Resistance Study Group. PCR and sequencing procedures : HIV-1 version February 2008. ANRS. 2008. p. 3–7.
Thompson JD, Higgins DG, Gibson TJ. CLUSTAL W: improving the sensitivity of progressive multiple sequence alignment through sequence weighting, position-specific gap penalties and weight matrix choice. Nucleic Acids Res. 1994;22:4673–80.
Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. MEGA6: molecular evolutionary genetics analysis version 6.0. Mol Biol Evol. 2013;30:2725–9.
Saitou N, Nei M. The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol Biol Evol. 1987;4:406–25.
Kimura M. A simple method for estimating evolutionary rate of base substitutions through comparative studies of nucleotide sequences. J Mol Evol. 1980;16:111–20.
Hanna GJ, Johnson VA, Kuritzkes DR, Richman DD, Brown AJ, et al. Patterns of resistance mutations selected by treatment of human immunodeficiency virus type 1 infection with zidovudine, didanosine, and nevirapine. J Infect Dis. 2000;181(3):904–11.
Adjé JNC, Cheingsong R, Roels TH, Maurice C, Djomand G, Verbiest W, et al. High prevalence of genotypic and phenotypic HIV-1 drug-resistant strains among patients receiving antiretroviral therapy in Abidjan, Côte d’Ivoire. J Acquir Immune Defic Syndr. 2001;26:501–6.
Kamangu KE, Zakayi K, Georges ML, Lunganza K, Gauthier MK. Genetic diversity of human immunodeficiency virus type 1 in the Democratic Republic of Congo : a review of available data. Int J Collab Res Intern Med Public Health. 2013;5(5):295–309.
Malick ZF, Tchiakpe E, Soufiane SAO, Diop-ndiaye H, Baye AM, Ould A, Babana H, Toure C. Drug Resistance mutations and genetic diversity in adults treated for HIV type 1 infection in Mauritania. J Med Virol. 2014;410:404–10.
Yahi N, Tamalet C, Tourrès C, Tivoli N, Fantini J. Mutation L210W of HIV-1 reverse transcriptase in patients receiving combination therapy. Incidence, association with other mutations, and effects on the structure of mutated reverse transcriptase. J Biomed Sci. 2000;7(6):507–13.
Calvez V, Costagliola D, Descamps D, Yvon A, Collin G, Cécile A, et al. Impact of stavudine phenotype and thymidine analogues mutations on viral response to stavudine plus lamivudine in ALTIS 2 ANRS trial. Antivir Ther. 2002;7(3):211–8.
Cozzi-Lepri A, Ruiz L, Loveday C, Phillips AN, Clotet B, Reiss P, et al. Thymidine analogue mutation profiles: factors associated with acquiring specific profiles and their impact on the virological response to therapy. Antivir Ther. 2005;10:791–802.
Ensemble pour la Solidarite Therapeutique En Reseaux. Rapport d’activite 2014: Partenariat, innovation, solidarite. Paris: ESTHER; 2015.
Richman DD, Havlir D, Corbeil J, Looney D, Ignacio C, Spector SA, et al. Nevirapine resistance mutations of human immunodeficiency virus type 1 selected during therapy. J Virol. 1994;68:1660–6.
Bacheler L, Jeffrey S, Hanna G, D’Aquila R, Wallace L, Logue K, et al. Genotypic correlates of phenotypic resistance to efavirenz in virus isolates from patients failing nonnucleoside reverse transcriptase inhibitor therapy. J Virol. 2001;75(11):4999–5008.
Torti C, Pozniak A, Nelson M, Hertogs K, Gazzard BG. Distribution of K103 N and/or Y181C HIV-1 mutations by exposure to zidovudine and non-nucleoside reverse transcriptase inhibitors. J Antimicrob Chemother. 2001;48:113–6.
Kuritzkes DR, Bassett RL, Hazelwood JD, Barrett H, Rhodes RA, Young RK, et al. Rate of thymidine analogue resistance mutation accumulation with zidovudine- or stavudine-based regimens. J Acquir Immune Defic Syndr. 2004;36(1):600–3.
De Luca A, Giambenedetto SD, Romano L, Gonnelli A, Corsi P, Baldari M, et al. Frequency and treatment-related predictors of thymidine-analogue mutation patterns in HIV-1 isolates after unsuccessful antiretroviral therapy. J Infect Dis. 2006;193:1219–22.
Brun-Vézinet F, Descamps D, Ruffault A, Masquelier B, Calvez V, Peytavin G, Morand-Joubert L, Meynard JL, Vray M, Costagliola D, et al. Clinically relevant interpretation of genotype for resistance to abacavir. AIDS. 2003;17:1795–802.
Lanier ER, Ait-Khaled M, Scott J, Stone C, Melby T, Sturge G, et al. Antiviral efficacy of abacavir in antiretroviral therapy-experienced adults harbouring HIV-1 with specific patterns of resistance to nucleoside reverse transcriptase inhibitors. Antivir Ther. 2004;9:37–45.
Montavon C, Toure-Kane C, Liegeois F, Mpoudi E, Bourgeois A, Vergne L, et al. Most env and gag subtype A HIV-1 viruses circulating in west and West Central Africa are similar to the prototype AG recombinant virus IBNG. J Acquir Immune Defic Syndr. 2000;23(5):363–74.
Roquebert B, Damond F, Brun-Vézinet F, Descamps D. HIV genetic diversity and its consequences. Pathol Biol (Paris). 2009;57(2):142–8.
Laurent C, Bourgeois A, Faye MA, Mougnutou R, Seydi M, Gueye M, et al. No difference in clinical progression between patients infected with the predominant human immunodeficiency virus type 1 circulating recombinant form (CRF) 02_AG strain and patients not infected with CRF02_AG, in western and west-central Africa: a four-year study. J Infect Dis. 2002;186(4):486–92.
Atlas A, Granath F, Lindström A, Lidman K, Lindbäck S, Alaeus A. Impact of HIV type 1 genetic subtype on the outcome of antiretroviral therapy. AIDS Res Hum Retroviruses. 2005;21:221–7.
Armenia D, Gori C, Di Carlo D, Bertoli A, Borghi V, Fabeni L, et al. Patients infected with CRF02_AG are more likely to experience virological rebound under first line PI/r based HAART. Paper presented at: The 13th European HIV & Hepatitis Workshop; 2015; Barcelona. http://www.virology-education.com/wp-content/uploads/2014/11/13th-EU_program_2015_5-212.pdf.
Manasa J, Danaviah S, Lessells R, Elshareef M, Tanser F, Wilkinson E, Pillay S, Mthiyane H, Mwambi H, Pillay D, Oliveira T. Increasing HIV-1 drug resistance between 2010 and 2012 in adults participating in population-based HIV surveillance in rural KwaZulu-Natal, South Africa. AIDS Res Hum Retroviruses. 2016;32:763–9.
Manasa J, Lessells RJ, Skingsley A, Naidu KK, Newell ML, McGrath N, de Oliveir T. Southern African Treatment and Resistance Network. High-levels of acquired drug resistance in adult patients failing first-line antiretroviral therapy in a rural HIV treatment programme in KwaZulu-Natal, South Africa. PLoS ONE. 2013;8(8):e72152. https://doi.org/10.1371/journal.pone.0072152 (eCollection 2013).
Aghokeng AF, Kouanfack C, Eymard-Duvernay S, Butel C, Edoul GE, Laurent C, et al. Virological outcome and patterns of HIV-1 drug resistance in patients with 36 months’ antiretroviral therapy experience in Cameroon. J Int AIDS Soc. 2013;31(16):18004. https://doi.org/10.7448/IAS.16.1.18004.
Aghokeng AF, Kouanfack C, Laurent C, Ebong E, Atem-Tambe A, Butel C, et al. Scale-up of antiretroviral treatment in sub-Saharan Africa is accompanied by increasing HIV-1 drug resistance mutations in drug-naive patients. AIDS. 2011;25(17):2183–8. https://doi.org/10.1097/QAD.0b013e32834bbbe9.
Fokam J, Salpini R, Santoro MM, Cento V, D’Arrigo R, Gori C, et al. Performance evaluation of an in-house human immunodeficiency virus type-1 protease-reverse transcriptase genotyping assay in Cameroon. Arch Virol. 2011;156(7):1235–43. https://doi.org/10.1007/s00705-011-0982-3.
Nanfack AJ, Agyingi L, Noubiap JJ, Ngai JN, Colizzi V, Nyambi PN. Use of amplification refractory mutation system PCR assay as a simple and effective tool to detect HIV-1 drug resistance mutations. J Clin Microbiol. 2015;53(5):1662–71. https://doi.org/10.1128/JCM.00114-15.
Fokam J, Elat JB, Billong SC, Kembou E, Nkwescheu AS, Obam NM, Essiane A, Torimiro JN, Ekanmian GK, Ndjolo A, Shiro KS, Bissek AC. Monitoring HIV drug resistance early warning indicators in cameroon: a study following the revised world health organization recommendations. PLoS One. 2015;10(6):e0129210. https://doi.org/10.1371/journal.pone.0129210.
Authors’ contributions
CA, JF, EK, HMA, DV and MM analysed and interpreted the patient data regarding CD cell count, plasma viral load and HIV sequence data. CA, JF, AMC, FS, AMM, THB and AT were the major contributor in writing the manuscript. All authors read and approved the final manuscript.
Authors’ informations
CA is a Micrbiologist, Senior Lecturer and Head of Department of Microbiology at the Institut National Supérieur des Sciences et Techniques d’Abéché, in Abéché, the republic of Chad. JF is a Virologist, Senior Scientist and Head of Virology laboratory at the Chantal BIYA International Reference Centre for research on HIV/AIDS prevention and management, in Yaounde, Cameroon. He completed a postdoctoral fellowship in Medical Virology at the University of Rome Tor Vergata in Rome, Italy. He also serves as adjunct lecturer of virology and molecular biology. EK is a Head of Laboratory and Senior Lecturer at the Faculty of Medicine of the University de Kinshasa, in the Democratic Republic of Congo. HMA, AMM, THZB and AT are health professionals and lecturers of the Faculty of Health Sciences, and of the National Reference General Hospital laboratory in Ndjamena, Chad. AMC is a Lecturer of the Institut National Supérieur des Sciences et Techniques d’Abéché, in Abéché, the Republic of Chad. FS and DV are health professionals of the AIDS Reference Laboratory at the Centre Hospitalier et Universitaire of Liège, in Liège, Belgium. MM is a health professional managing the infectious diseases and internal medicine service at the Centre Hospitalier et Universitaire of Liège, in Liège, Belgium.
Acknowledgements
We are thankful to Giussépina Olivéri, Sebastien Bontems, Caroline Adjetey, Raphaël Boreux of the Microbiology and AIDS Reference Laboratory at the University Health Center (CHU) of Liège, for their technical assistance. We are appreciative to laboratory personnel of the Chad National Reference General Hospital, for facilitating data collection locally.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data supporting the findings are provided in the manuscript text and additional files.
Consent to publish
Not applicable.
Ethics approval and consent to participate
Ethical clearance for the present study was obtained from the National ethics committee of Chad. Written informed consent was obtained from each participant and data were processed using specific identity codes to ensure protection of privacy and confidentiality. PVL and resistance testing results were returned, free of charge, to study participants for benefit in their respective clinical management. All participants were legally old enough to give informed consent.
Funding
This study was funded by the Commission Nationale de formations de Formateurs (CONFOFOR).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding authors
Additional files
13104_2017_2893_MOESM1_ESM.docx
Additional file 1. PCR and sequencing Primers (ANRS AC 11). The primer sequences are designed for amplification and sequencing reactions of protease and reverse transcriptase regions.
13104_2017_2893_MOESM2_ESM.docx
Additional file 2. Study participants by age range. The table details the study population by range age from 17 to over 60 years old, divided by male and female.
13104_2017_2893_MOESM3_ESM.docx
Additional file 3. Characteristics of assays used for plasma viral load. The table reports the minimal and maximal values, as well as mean and median of viral loads, obtained on one hand with Cobas and on the other hand with Abbott.
13104_2017_2893_MOESM4_ESM.docx
Additional file 4. Level of resistance to reverse transcriptase inhibitors. The table presents the proportion of patients with levels of genotypic susceptibility score following the Stanford algorithm.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Adawaye, C., Fokam, J., Kamangu, E. et al. Virological response, HIV-1 drug resistance mutations and genetic diversity among patients on first-line antiretroviral therapy in N’Djamena, Chad: findings from a cross-sectional study. BMC Res Notes 10, 589 (2017). https://doi.org/10.1186/s13104-017-2893-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-017-2893-1