Abstract
Background
To date, no studies on the feasibility or outcomes of cardiac rehabilitation (CR) after percutaneous mitral valve reconstruction using clipping procedures have been published. The aim of this study was to report on our first experiences with this special target group.
Methods
Monocentric retrospective analysis of 27 patients (72 ± 12 years old, 52% female) who underwent multimodal inpatient CR in the first 2 month after MitraClip™ implantation. A six-minute-walking-test, a handgrip-strength-test and the Berg-Balance-Scale was conducted at the beginning and end of CR. Echocardiography was performed to rule out device-related complications.
Results
Adapted inpatient CR started 16 ± 13 days after clipping intervention and lasted 22 ± 4 days. In 4 patients (15%) CR had to be interrupted or aborted prematurely due to cardiac decompensations. All other patients (85%) completed CR period without complications. Six-minute-walking-distance improved from 272 ± 97 to 304 ± 111 m (p < .05) and dependence on rollator walker or walking aids was significantly reduced (p < .05). Results of handgrip-strength-test and Berg-Balance-Scale increased (p < .05). Overall, social-medical and psychological consultations were well received by the patients and no device-related complications occurred during rehabilitation treatments.
Conclusions
The results indicate that an adapted inpatient CR in selected patients after MitraClip™ implantation is feasible. Patients benefited from treatments both at functional and social-medical level and no device-related complications occurred. Larger controlled studies are needed.
Similar content being viewed by others
Introduction
Valvular heart disease (VHD) is common in elderly patients, and its importance will increase in the coming decades due to demographic change [1, 2]. In the OxVALVE cohort study (2500 individuals, ≥ 65 years), 51% of participants were diagnosed with previously undetected VHD, with 11.3% having moderate or severe manifestations [2]. Data from Germany show that the number of hospital admissions due to VHD has been steadily increasing for many years [3]. The second most common VHD (after aortic sclerosis) is Mitral insufficiency (MI) [2] with frequent occurrence especially in ageing heart failure (HF) patients. According to current guidelines [4, 5], treatment of secondary mitral regurgitation may also be considered via percutaneous mitral valve interventions in patients at high surgical risk. Therefore, clipping procedures (e.g. MitraClip™, Abbott, Fig. 1) have become an established method in recent years [6, 7].
However, despite an increasing number of patients, no studies on the feasibility or outcomes of cardiac rehabilitation (CR)—whether performed in an inpatient or outpatient setting—after MitraClip™ implantation have been published to date, with the exception of one theoretical draft paper [8]. One reason could be that physical rest is often recommended immediately after implantation to prevent dislocation of the clip, and that patients are therefore not prescribed CR.
In our opinion, this is not ideal (at least not as a general precaution) since the often multimorbid patients already suffer from physical inactivity. Common comorbidities are for example arterial hypertension, coronary artery disease, HF, atrial fibrillation, diabetes mellitus or renal failure. Patients are typically old (> 70 years) and many of them had previous cardiac interventions (e.g. coronary bypass grafting) or cardiac decompensations (> 50% within 6 months and > 30% within 21 days) prior to clipping procedure with prolonged hospital stay and physical inactivity periods [9, 10]. Consequently, impaired peripheral adaptive mechanisms and progressive skeletal muscle deconditioning (sarcopenia, frailty) are widely suspected [11]. From our point of view, especially these patients could benefit from multimodal CR in many different ways, since the essential role of physical and rehabilitation medicine (PMR) in the secondary prevention of cardiovascular diseases is evident [12, 13]. This is particularly important given that the long-term results of the COAPT trial show that the six-minute walking distance (6MWD) and its improvement in the first month after MitraClip™ implantation are associated with lower mortality and HF hospitalization, at least for the first 2 years [6, 14].
It is the aim of this study to report our experience with this patient group during inpatient CR program in terms of safety and feasibility in order to start discussions and improve the treatment situation.
Materials and methods
We conducted a monocentric retrospective analysis of patients who underwent inpatient CR at our hospital within the first 2 months after percutaneous mitral valve intervention between October 2017 and February 2020. The prerequisite for admission and adequate participation in inpatient CR was a stable clinical state and a barthel index of ≥ 65 points.
Inpatient CR program and diagnostics
The patients received a 3-week multimodal standard inpatient CR program in line with their requirements and condition. The duration of 3 weeks is the typical length for inpatient CR in Germany and is covered by public health insurance.
Therapeutic treatments were agreed with the cardiologist and often included the following:
-
aerobic exercise training on a cycle ergometer with monitoring or (if indicated) an assisted cycle therapy (5 times a week/30 min)
-
gymnastics in small groups using small equipment like elastic bands or dumbbells (3 times a week/30 min)
-
resistance exercise training on weight machines e.g. leg curl or leg extension (2 times a week/30 min)
-
outdoor walking training (2 times a week/30 min)
-
mechanically guided inhalation training (3 times a week/10 min)
-
physiotherapist-guided inspiratory muscle training (3 times a week/20 min)
-
arm baths (3 times a week/20 min)
-
mud packs (2 times a week, 20 min)
-
ergotherapy (3 times a week/30 min)
-
individually adapted education (e.g. about HF or VHD)
-
socio-medical care
-
and also further therapies if indicated.
One specific restriction of CR program was that blood pressure peaks should be avoided during treatments (systolic target value ≤ 120 mmHg). For this reason, no maximum cardiopulmonary exercise test (CPET) was performed during CR. Physical exercise units (e.g. aerobic cycle ergometer training or resistance training) were only performed at a low intensity level and incorporated blood pressure monitoring. During the 3-week CR stay, intensity levels were carefully increased depending on the blood pressure values and the perception of the experienced therapists. As part of our standard functional diagnostics, a six-minute-walking-test (6MWT) [15, 16], a handgrip-strength-test [17] (Fig. 2) and the Berg-Balance-Scale (BBS) [18] were performed at the start and end of CR in standardized approach. Likewise, rehabilitation routines included 24-h electrocardiogram (ECG) and 24-h blood pressure measurement. At the end of CR, echocardiography was performed in order to test both MI and the position of the MitraClip™ to rule out possible clip detachments.
Study population
A total of 27 patients after percutaneous mitral valve interventions via clipping procedures could be included into the study. All patients underwent MitraClip™ implantation and other clipping devices were not observed. Patients were mean 72 ± 12 years old, 52% female and started inpatient CR on average 16 ± 13 days after percutaneous intervention (min 3 days, max 55 days). Before admission, patients achieved a Barthel index of mean 92 ± 9 points (min 70, max 100), indicating sufficient functional independence and the ability to follow inpatient CR program adequately. Detailed patient characteristics are summarized in Table 1.
Data collection and analyses
Within this evaluation, clinical data from rehabilitation stay and discharge reports from acute hospital stay were examined retrospectively and anonymously. Processing and statistical analysis were performed using the IBM SPSS Statistics software (Version 26, IBM). Comparisons of two nominal variables were conducted using the Fisher’s exact test. For dependent comparisons of mean values, a dependent t-test and/or Wilcoxon rank sum test was used. All statistical comparisons were two-tailed, and the level of significance was set at alpha 5%.
According to our local ethics committee (German Sports University Cologne) specific approval for this study was not needed due to the retrospective and anonymous internal single-centre design and informed consent could be waived.
Results
Inpatient CR completion
Of the 27 patients admitted, 23 (85%) completed CR without complications. One patient (4%) had to interrupt rehabilitation due to cardiac decompensation, but was able to continue successfully after percutaneous coronary intervention (PCI). In 3 patients (11%) CR had to be stopped in the first week, in two cases due to cardiac decompensation, in one due to cardiac decompensation and renal failure. The following results refer to the 24 patients who completed CR.
Inpatient CR treatments
Patients were admitted for inpatient CR at an average of 16 ± 13 days after MitraClip™ implantation. The mean CR duration was 22 ± 4 days. In 7 patients (26%) the 3-week CR was extended by one week to meet their needs. Core components of exercise-based CR were individually adapted gymnastics in small groups (100%, 7 ± 2 units), low-intensity aerobic exercise training on a cycle ergometer with monitoring (96%, 11 ± 3 units), low-dose resistance exercises (92%, 6 ± 2 units), mechanically guided inhalation training (96%, 6 ± 2 units) and physiotherapist-guided inspiratory muscle training (50%, 7 ± 2 units). If indicated, especially to improve and stabilize perfusion, patients also received physical therapy, such as mud packs (58%, 5 ± 1 units) or arm baths (54%, 3 ± 2 units). Other core components of CR were individually adapted education and socio-medical care.
Diagnostic values and outcomes
The 24-h diagnostics showed that during a standard rehabilitation day a mean heart rate of 71 ± 9 bpm and a systolic blood pressure of mean 117 ± 10 mmHg were achieved. The maximum daily values were 100 ± 21 bpm and 142 ± 18 mmHg. Main changes during CR in exercise intensities, functional performance values and device-related echocardiography parameters are summarized in Table 2.
During CR, exercise intensity started at a low intensity level and carefully increased over the course (p < 0.01). The mean 6MWD improved significantly from 272 ± 97 to 304 ± 111 m (p < 0.05), corresponding to an improvement from 60 ± 26% to 67 ± 29% of predicted values [19]. At the beginning of CR, 14 patients were below the critical prognostic threshold [20, 21] of 300 m, by the end only 8 patients. Dependence on a rollator walker or walking aids was significantly reduced from 9 to 4 patients (p < .05). Values of BBS improved significantly (p < .05), whereas handgrip strength values only improved for the non-dominant hand (p < .05). At the end of CR, no device-related problems were observed echocardiographically: no clip detachments, no changes regarding MI or related gradient, and even slightly improved left ventricular ejection fraction (p < .05).
At a socio-medical level, patients also profited: during CR, 4 patients could apply for household help and 3 patients for an official disability level.
Discussion
Feasibility and outcomes
To the best of our knowledge, this is the first published report on feasibility and outcomes of CR (whether performed inpatient or outpatient) immediately after percutaneous mitral valve reconstruction using clipping procedures. This is surprising since the positive effects of rehabilitation programs in other cardiac patient populations (e.g. coronary artery disease, HF, transcatheter aortic valve replacement, heart transplantation) are already well-known [12, 22] and CR should be recommended especially in older and frail patients [23].
One reason for a low level of CR utilization after MitraClip™ implantation could be that the risk of clip dislocation appears to be highest in the first period after implantation [24] and therefore physically rest is often recommended. As a consequence, it can be assumed that CR is rarely prescribed and appears to be underused in this patient population (even less than for “normal” HF patients [25]).
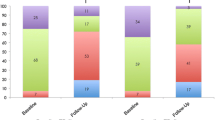
However, our experience shows that adapted inpatient CR in selected patients is definitively possible, and that patients can profit from multimodal CR at both a functional and a socio-medical level (Fig. 3). In our hospital, physical exercise training was purposely conducted at a low intensity level, with mean systolic blood pressure values of below 120 mmHg and maximum values of about 140 mmHg. The treatments led to no device-related complications, and functional capacity could be significantly improved during the rehabilitation period. Dependence on a rollator walker or walking aids could be reduced, indicating improved prerequisites for activities of daily living.
Potential benefits for participating in multimodal cardiac rehabilitation program after percutaneous mitral valve reconstruction using clipping procedures: a prolonged observation period and possibility for supplementary diagnostics, b individualised exercise interventions to improve functional capacity, c personalised preparation for activities of daily living
The 6MWD achieved of mean 304 (± 111) m was just above the critical prognostic threshold of 300 m [20] and the reached improvements during CR can be classified as moderate clinically important changes [26]. The observed functional capacity is approximately within the range measured in elderly patients undergoing CR after atrioventricular valve interventions [27] and in line with published MitraClip™ studies [28, 29]. Albeit compared with other special cardiological patient cohorts (e.g. PCI, transcatheter aortic valve replacement, left ventricular assist device implantation, heart transplantation), a reduced functional capacity must be assumed [27, 30, 31].
Potential benefits of inpatient CR
Prolonged observation period
A main advantage of participating in an inpatient CR program after clip implantation is the significantly extended observation period (in Germany by 3 weeks) compared to a discharge directly home. During this time span supplementary diagnostic and therapies (e.g. 24-h ECG, 24-h blood pressure measurement, echocardiography, treatment of possible transcatheter complications, treatment of possible HF symptoms) can be performed in a clinical setting in order to adjust/optimize therapy and prevent complications that might go undetected/untreated at home [23]. Thus, in our study 4 patients (15%) with a worsening clinical condition could be identified and referred to acute HF department timely, with 1 patient able to continue inpatient CR after PCI.
Physical therapy and exercise interventions
The special needs of this often old and frail patient population can be addressed in an adequate manner by implementing individualized physical therapy and tailored exercise interventions during CR period [11, 23]. In addition to the treatment of possible orthopedic comorbidities, the achievement of sufficient coordinative and motoric functions should be aimed in order to prepare the patients for discharge home and the activities of daily living (e.g. balance training and fall prevention by physiotherapy and/or ergotherapy if needed). Patients are also introduced to moderate aerobic endurance and resistance training in a supervised clinical setting to counteract muscle deconditioning without causing blood pressure peaks.
Education, socio-medical care and psychological support
The transition from the clinic to the home environment is crucial and can often be accompanied by uncertainties, especially after a long hospital stay. With individual educational courses, socio-medical and psychological consultations, patients can be supported by specialized staff during CR period. The aim of these treatments is to prevent potential problems at home or to detect and eliminated them in time to prepare patients for the challenges of everyday life. Thus, in our study 4 patients (15%) were able to apply for household help at the health insurance companies and also 3 patients (11%) were able to apply for an official disability level at the local authority. These applications were all initiated and guided by socio-medical personnel during the CR period, and it is uncertain whether the applications would have been made without our external support.
Study limitations and future investigastions
This is a retrospective pilot study with only a small sample size and without comparison of exercise values before and after implantation. Further studies are required to confirm and supplement our experience. These studies should systematically examine the special needs of this often frail patient population in order to develop specific rehabilitation programs. Likewise, prospective and controlled studies (e.g. CR vs, geriatric rehabilitation vs.no rehabilitation; inpatient vs. outpatient) would be highly desirable to examine the effect of CR on functional capacity, quality of life, readmissions and survival over the long-term course.
Conclusions
The results of this study indicate that an adapted inpatient CR is feasible in selected patients after percutaneous mitral valve clipping procedure. MitraClip™ patients are usually a multimorbid patient group with many comorbidities (also orthopaedic) and a high need for care. However, our first results are encouraging: during therapeutic treatments no device-related complications occurred and functional capacity and dependence on rollator walker was significantly improved. Larger controlled studies should be aimed to improve evidence on exercise-related questions in MitraClip™ patients to allow for optimized recovery and aftercare after transcatheter mitral valve procedure.
Availability of data and materials
The datasets used and/or analysed during the current study are not publicly available due to our internal hospital policy but are available from the corresponding author on reasonable request.
Abbreviations
- BBS:
-
Berg-Balance-Scale
- CPET:
-
Cardiopulmonary exercise test
- CR:
-
Cardiac rehabilitation
- ECG:
-
Electrocardiogram
- HF:
-
Heart failure
- MI:
-
Mitral insufficiency
- PCI:
-
Percutaneous coronary intervention
- PMR:
-
Physical medicine and rehabilitation
- VHD:
-
Valvular heart disease
- 6MWD:
-
Six-minute walking distance
- 6MWT:
-
Six-minute walking test
References
Rostagno C. Heart valve disease in elderly. World J Cardiol. 2019;11:71–83. https://doi.org/10.4330/wjc.v11.i2.71.
d’Arcy JL, Coffey S, Loudon MA, Kennedy A, Pearson-Stuttard J, Birks J, et al. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: the OxVALVE Population Cohort Study. Eur J Heart Fail. 2016;37:3515–22. https://doi.org/10.1093/eurheartj/ehw229.
German Heart Foundation. German Heart Report 2020. 2021. https://www.herzstiftung.de/system/files/2021-06/Deutscher-Herzbericht-2020.pdf. Accessed 17 Jan 2022.
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Fleisher LA, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135:e1159–95. https://doi.org/10.1161/CIR.0000000000000503.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891–975. https://doi.org/10.1002/ejhf.592.
Stone GW, Lindenfeld J, Abraham WT, Kar S, Lim DS, Mishell JM, et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018;379:2307–18. https://doi.org/10.1056/NEJMoa1806640.
Obadia J-F, Messika-Zeitoun D, Leurent G, Iung B, Bonnet G, Piriou N, et al. Percutaneous repair or medical treatment for secondary mitral regurgitation. N Engl J Med. 2018;379:2297–306. https://doi.org/10.1056/NEJMoa1805374.
Schlitt A, Lubos E, Guha M, Hegeler-Molkewehrum C, Sudau M, Schmidt H. Aftercare of patients after MitraClip® implantation. Herz. 2017;42:176–85. https://doi.org/10.1007/s00059-016-4448-y.
Ledwoch J, Franke J, Lubos E, Boekstegers P, Puls M, Ouarrak T, et al. Prognostic value of preprocedural 6-min walk test in patients undergoing transcatheter mitral valve repair-insights from the German transcatheter mitral valve interventions registry. Clin Res Cardiol. 2018;107:241–8. https://doi.org/10.1007/s00392-017-1177-z.
Eggebrecht H, Schelle S, Puls M, Plicht B, von Bardeleben RS, Butter C, et al. Risk and outcomes of complications during and after MitraClip implantation: Experience in 828 patients from the German TRAnscatheter mitral valve interventions (TRAMI) registry. Catheter Cardiovasc Interv. 2015;86:728–35. https://doi.org/10.1002/ccd.25838.
Kitzman DW, Whellan DJ, Duncan P, Pastva AM, Mentz RJ, Reeves GR, et al. Physical rehabilitation for older patients hospitalized for heart failure. N Engl J Med. 2021;385:203–16. https://doi.org/10.1056/NEJMoa2026141.
Winnige P, Vysoky R, Dosbaba F, Batalik L. Cardiac rehabilitation and its essential role in the secondary prevention of cardiovascular diseases. World J Clin Cases. 2021;9:1761–84. https://doi.org/10.12998/wjcc.v9.i8.1761.
Papathanasiou J, Troev T, Ferreira AS, Tsekoura D, Elkova H, Kyriopoulos E, Ilieva E. Advanced role and field of competence of the physical and rehabilitation medicine specialist in contemporary cardiac rehabilitation. Hellenic J Cardiol. 2016;57:16–22. https://doi.org/10.1016/s1109-9666(16)30013-6.
Arnold SV, Stone GW, Jain SS, Mack MJ, Saxon JT, Zhang Z, et al. Prognostic importance of health status versus functional status in heart failure and secondary mitral regurgitation. JACC Heart Fail. 2021;9:684–92. https://doi.org/10.1016/j.jchf.2021.04.012.
Papathanasiou JV, Ilieva E, Marinov B. Six-minute walk test: an effective and necessary tool in modern cardiac rehabilitation. Hellenic J Cardiol. 2013;54:126–30.
American Thoracic Society. ATS Statement: guidelines for the six-minute walk test. Am J respir Crit Care Med. 2002;166:111–7. https://doi.org/10.1164/ajrccm.166.1.at1102.
Mathiowetz V, Kashman N, Volland G, Weber K, Dowe M, Rogers S. Grip and pinch strength: normative data for adults. Arch Phys Med Rehabil. 1985;66:69–74.
Scherfer E, Bohls C, Freiberger E, Heise K-F, Hogan D. Berg-Balance-Scale-German Version—translation of a standardized instrument for the assessment of balance and risk of falling. Physioscience. 2006;2:59–66. https://doi.org/10.1055/s-2006-926833.
Enright PL, Sherrill DL. Reference equations for the six-minute walk in healthy adults. Am J respir Crit Care Med. 1998;158:1384–7. https://doi.org/10.1164/ajrccm.158.5.9710086.
Metra M, Ponikowski P, Dickstein K, McMurray JJV, Gavazzi A, Bergh C-H, et al. Advanced chronic heart failure: a position statement from the Study Group on Advanced Heart Failure of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2007;9:684–94. https://doi.org/10.1016/j.ejheart.2007.04.003.
Arslan S, Erol MK, Gundogdu F, Sevimli S, Aksakal E, Senocak H, Alp N. Prognostic value of 6-minute walk test in stable outpatients with heart failure. Tex Heart Inst J. 2007;34:166–9.
Epstein E, Rosander A, Pazargadi A, Taub P. Cardiac rehab for functional improvement. Curr Heart Fail Rep. 2020;17:161–70. https://doi.org/10.1007/s11897-020-00462-2.
Schopfer DW, Forman DE. Growing relevance of cardiac rehabilitation for an older population with heart failure. J Card Fail. 2016;22:1015–22. https://doi.org/10.1016/j.cardfail.2016.10.010.
Toggweiler S, Zuber M, Sürder D, Biaggi P, Gstrein C, Moccetti T, et al. Two-year outcomes after percutaneous mitral valve repair with the MitraClip system: durability of the procedure and predictors of outcome. Open Heart. 2014;1: e000056. https://doi.org/10.1136/openhrt-2014-000056.
Park LG, Schopfer DW, Zhang N, Shen H, Whooley MA. Participation in cardiac rehabilitation among patients with heart failure. J Card Fail. 2017;23:427–31. https://doi.org/10.1016/j.cardfail.2017.02.003.
Jain SS, Cohen DJ, Zhang Z, Uriel N, Sayer G, Lindenfeld J, et al. Defining a clinically important change in 6-minute walk distance in patients with heart failure and mitral valve disease. Circ Heart Fail. 2021;14: e007564. https://doi.org/10.1161/CIRCHEARTFAILURE.120.007564.
Eichler S, Hadzic M, Völler H, Salzwedel A. Octogenarians in interventional cardiology: feasibility and safety of functional and nutritional assessments for a new patient group in cardiac rehabilitation. Eur J Prev Cardiol. 2020. https://doi.org/10.1177/2047487319899194.
Iliadis C, Lee S, Kuhr K, Metze C, Matzik A-S, Michels G, et al. Functional status and quality of life after transcatheter mitral valve repair: a prospective cohort study and systematic review. Clin Res Cardiol. 2017;106:1005–17. https://doi.org/10.1007/s00392-017-1150-x.
Barth S, Hautmann MB, Kerber S, Gietzen F, Reents W, Zacher M, et al. Left ventricular ejection fraction of < 20%: too bad for MitraClip©? Cathether Cardiocvasc Interv. 2017;90:1038–45. https://doi.org/10.1002/ccd.27159.
Schmidt T, Bjarnason-Wehrens B, Bartsch P, Deniz E, Schmitto J, Schulte-Eistrup S, et al. Exercise capacity and functional performance in heart failure patients supported by a left ventricular assist device at discharge from inpatient rehabilitation. Artif Organs. 2018;42:22–30. https://doi.org/10.1111/aor.12936.
Schmidt T, Bjarnason-Wehrens B, Predel H-G, Reiss N. Exercise after heart transplantation: typical alterations, diagnostics and interventions. Int J Sports Med. 2021;42:103–11. https://doi.org/10.1055/a-1194-4995.
Acknowledgements
The authors wish to thank Anita Nitters-Daske, Britta Kattlun and Cornelia Marques for their helpful support regarding data acquisition.
Funding
No specific grant from any funding agency in the public, commercial or not-for-profit sectors was received to carry out the work.
Author information
Authors and Affiliations
Contributions
TS, BBW and NR contributed to the conception of the study. TS, MK, FR, GM and NR contributed to data acquisition. TS and BBW drafted the first version of the manuscript. MK, FR, GM and NR critically revised the manuscript. All authors gave their final approval for its publication. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods performed during this study were carried out in accordance with relevant guidelines and regulations. The ethics committee of German Sports University Cologne waived the need for specific approval and informed consent due to the retrospective and anonymous internal single-centre design.
Consent for publication
Figure 2: Patient permission obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Schmidt, T., Kowalski, M., Bjarnason-Wehrens, B. et al. Feasibility of inpatient cardiac rehabilitation after percutaneous mitral valve reconstruction using clipping procedures: a retrospective analysis. BMC Sports Sci Med Rehabil 14, 120 (2022). https://doi.org/10.1186/s13102-022-00517-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13102-022-00517-y