Abstract
Background
In males with end stage renal disease biochemical hypogonadism is a frequent finding. Testosterone and sex hormone binding globulin (SHBG) have been associated with insulin resistance, a well-known condition in uremia. The aim of the present study was to investigate in males on chronic hemodialysis the relationship of testosterone and SHBG serum levels with insulin resistance.
Methods
In a cross-sectional study we enrolled men treated with chronic hemodialysis who did not suffer from an acute illness or other endocrinopathy, as well as primary hypogonadism, and were not hospitalised. Diabetes mellitus, diabetic nephropathy or previous transplantation were not exclusion criteria. As controls we used a community-based group of healthy males matched for age and Body Mass Index (BMI). We assessed the BMI (kg/m2) from body weight and height, the body fat content (%) by bioelectrical impedance and serum testosterone (ng/ml), SHBG (nmol/L) and estradiol (pg/ml) by standard methods. Testosterone < 3.25 ng/ml defined biochemical hypogonadism. In non-diabetic males, we calculated the homeostasis model assessment index (HOMA-R), an estimate of insulin resistance, from serum fasting insulin and glucose.
Results
27 men (age 54.4 ± 19 years) on chronic hemodialysis (treatment duration 29.1 ± 14.4 months) and 51 healthy men (age 47.1 ± 9.6 years) were included. In men on hemodialysis vs. healthy men there were increased serum levels of SHBG (40.9 ± 26.9 vs. 27.6 ± 11.9 nmol/L; p = 0.031) and a significantly enhanced frequency of biochemical hypogonadism (22.2 vs. 3.9%; p = 0.011). In cases without diabetes (n = 22) a significant correlation was observed between the HOMA-R (r = -0.586, p = 0.004) and the fasting insulin levels (r = -0.650, p = 0.001) on the one hand and the serum SHBG levels on the other.
Conclusions
Our findings confirm enhanced prevalence of biochemical hypogonadism in males on chronic hemodialysis. In non-diabetic cases the serum levels of SHBG correlated with serum insulin and insulin resistance.
Similar content being viewed by others
Background
Insulin resistance is the impaired ability of plasma insulin to promote tissue glucose disposal adequately and is accompanied frequently by hyperinsulinemia and glucose intolerance. In chronic kidney disease and uremia insulin resistance is very common [1, 2]. Hemodialysis treatment, by significantly improving uremia, ameliorates insulin resistance [3]. Previous clinical and experimental studies suggest that in kidney disease the main site of insulin resistance is the skeletal muscle, where a defect of the post-receptor pathway is involved [4, 5]. However, the exact pathogenic mechanism of insulin resistance in kidney disease remains still unresolved.
In men with severe chronic kidney disease there is frequently a biochemical primary and a concurrent secondary hypogonadism [6, 7]. Low serum testosterone in men has been associated with the metabolic syndrome, diabetes mellitus and insulin resistance [8,9,10]. In the same context, sex hormone binding globulin (SHBG), a plasma transporter of sex steroids, is also associated with the metabolic syndrome and with insulin resistance [11, 12]. SHBG plasma concentration, independently from sex steroids, is inversely correlated with glycosylated hemoglobin in both men and women without diabetes mellitus. In women with polycystic ovarian syndrome, a condition associated with insulin resistance and an increased risk of type 2 diabetes mellitus, SHBG concentrations are decreased [13]. Furthermore, hypogonadism is a recognised factor predisposing to increased mortality and cardiovascular morbidity both in males undergoing chronic hemodialysis and in males of the general population [14].
SHBG is a 90-kD glycoprotein composed of two 373-amino-acid subunits, each with a single steroid binding site. SHBG is synthesized mainly in hepatocytes, and its clearance from the intravascular compartment is dependent on glycosylation, which prolongs half life. The kidneys, however, are not involved either in synthesis or in catabolism and clearance of the molecule. Traditionally, it has been considered to function merely as a sex steroid transporter, controlling circulating free sex steroids in blood. However, today certain findings suggest that SHBG has additional functions [15]. The existence of a plasma membrane receptor binding unliganded SHBG was previously demonstrated. Liganded SHBG does not bind to the SHBG-receptor on the cellular plasma membrane, suggesting that there are SHBG cellular effects, which are independent of sex steroids. In addition, binding of a sex steroid on the SHBG bound on its receptor leads to an activation of a G-protein-linked second-messenger system. The resulting cellular reactions depend on the sex steroid ligand. The presence of an SHBG receptor in the plasma membrane and of a second messenger system provides a probable explanation for the non-genomic actions of sex hormones [16].
The aim of the present cross-sectional study in men with end stage renal disease on chronic hemodialysis was to address the hypothesis that testosterone and SHBG serum levels may relate to insulin resistance, a very common condition in uremia and investigate a probable relationship of biochemical hypogonadism with insulin resistance in this group.
Methods
Subjects
In this cross-sectional study the inclusion criteria were male patients with end-stage renal disease treated with chronic hemodialysis in the Renal Unit at the University Hospital of Larissa. All were enrolled if they were on treatment with chronic hemodialysis treatment for more than three months, did not suffer from an acute illness or other endocrinopathy, as well as primary hypogonadism, and were not hospitalised. Patients were excluded if they were receiving hemodialysis treatment transiently, i.e. for acute renal failure, and if they were unable to provide informed consent. None of the patients was previously transplanted. Tre presence of diabetes mellitus/diabetic nephropathy was not exclusion criteria.
Relevant clinical and laboratory data as well as 5-years mortality data were recorded from the medical records kept in the renal unit. If this was not possible mortality data were acquired from the national end stage renal disease registry. A community based control group of healthy males matched for age (± 5 years) and Body Mass Index (BMI; ±2 kg/m2) was used.
The purpose and the procedure of the study were clearly explained to the participants, who then all provided informed consent. Before initiation, the study presented here was approved by the Ethics Review Board of the University Hospital of Larissa.
Clinical and laboratory data
We assessed Body Mass Index (BMI; kg/m2) according to the Quetelet’s formula from body weight (W; kg) and height (H; m) [17]: \(BMI = {W \over {{H^2}}}\). For body fat content (%) we applied a bioelectrical impedance analysis by means of a commercially available bio-impedance analyser (Omron HBF 302 Body Fat Analyser, Omron Healthcare Inc., Vernon Hills, IL, USA) with the participant in standing position. Waist circumference (cm) was measured according to the World Health Organisation (WHO) stepwise approach to surveillance (STEPS) [18] using a plastic non-stretchable tailor’s measuring tape, at the approximate midpoint between the lower margin of the last palpable rib margin and the top of the iliac crest to the nearest centimetre, as previously described. In hemodialysis patients waist circumference (cm), body weight (kg) and body fat content (%) were assessed after the end of the hemodialysis session [19].
The protein catabolic rate (PCR) was calculated from the pre-dialysis BUN concentration (C0; mg/dl) and the Kt/V [20], based on a two-BUN measurement, single-pool, variable-volume model by the following formula, for patients dialysed thrice weekly and especially for a C0 measured after the long dialysis-free interval at the beginning of the week:
Hemodialysis adequacy was assessed by the urea clearance ratio (Kt/V), which was calculated from the urea reduction ratio (R), the ultrafiltration volume (UF) and the post-dialysis body weight (W) via the second generation natural logarithmic formula, also based on the single pool urea kinetic model, namely:
Blood samples were always collected after an overnight fast in the morning (8–10 am) and in hemodialysis patients, especially, before commencement of the middle week (Wednesday or Thursday) hemodialysis session. All parameters in serum samples were measured with commercially available assays. Total testosterone (ng/ml) and total estradiol serum levels (pg/ml) were assessed by a coat-a-count solid phase radioimmunoassay (RIA; Diagnostic System Laboratories Inc., Webster, TX, USA). The assay sensitivity for serum testosterone was 0.08 ng/ml and for serum estradiol 0.6 pg/ml. The interassay coefficient of variation (CV) was 8% for serum testosterone and 4% for serum oestradiol measurements. Serum levels of sex hormone binding globulin (SHBG; nmol/L) were measured using an immunoradiometric assay (IRMA; Radim SpA, Roma, Italy). The assay sensitivity was 2.5 nmol/L and the interassay CV 5%. Free androgen index (FAI) was the ratio of serum total testosterone (nmol/L) to serum SHBG (nmol/L). According to previous reports, biochemical hypogonadism was defined either as serum total testosterone ≤ 3.25 ng/ml or as FAI ≤ 0.153 [21].
In non-diabetic men serum glucose levels were determined by means of the Glucoanalyzer II (Beckmann, Munich, Germany) and the serum insulin concentrations by an IRMA (Immunotech, Beckman Counter Company, Marseille, France). From the serum fasting levels of glucose (Glucose; mg/dl) and insulin (Insulin; µIU/ml) the homeostasis model assessment ratio (HOMA-R) was calculated according to the following formula: \(HOMA - R = {{Glu\cos e \cdot Insulin} \over {405}}\). The HOMA-R (mmol·µIU/ml) was previously validated in 888 healthy Caucasian subjects and the values in the top quintile of the distribution (> 2.77 mmol·µIU/ml) were defined as insulin resistant state, while lower values were considered to represent an insulin sensitive state.
Statistical analysis
Data were expressed as mean values (\(\bar {\rm X}\)) with standard deviation (SD). The normality of continuous variables was tested by the Kolmogorov-Smirnov test. Variables not following normal distribution were logarithmically transformed for implementation in linear regression. Pair-wise comparisons of continuous variables were performed with the t-test or the Mann-Whitney U test for unpaired data, as appropriate. For comparison of categorical variables among the two groups we used the χ2 test. Interdependence of the different continuous variables was checked by means of a Pearson or a Spearman correlation analysis and a linear regression analysis, as appropriate. Based on the results of the univariate analysis and respective scatter-plots we set up a multiple linear regression model. In the model, we included HOMA-R (mmol·µIU/ml) as the dependent variable on the one hand and age (years), testosterone (ng/ml) as well as all parameters that significantly correlated with HOMA-R (mmol·µIU/ml) as predictor variables on the other.
Overall, statistical analyses were carried out using the Statistic Package for Social Sciences 13.0 (SPSS® 13.0) for Windows (SPSS Inc., Chicago, IL, USA). P-values < 0.05 were considered statistically significant.
Results
The flowchart of the study participation among hemodialysis patients is shown in Fig. 1. We enrolled 27 men (age 54.4 ± 19 years) on chronic hemodialysis (treatment duration 29.1 ± 14.4 months) and 51 healthy men (age 47.1 ± 9.6 years). On Table 1 primary diseases of men on chronic hemodialysis, enrolled in the study, is shown.
Prevalence of biochemical hypogonadism (testosterone < 3.25 ng/ml) was increased in men on hemodialysis vs. healthy men (22.2 vs. 3.9%; p = 0.011). Furthermore, in men on hemodialysis there were significantly increased serum levels of SHBG (nmol/L; p = 0.031) along with increased free testosterone index values and significantly reduced testosterone (ng/ml) and estradiol levels (pg/ml). All these findings are presented in detail on Table 2.
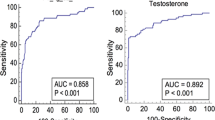
In cases without diabetes mellitus (n = 22) a significant negative correlation was observed between insulin resistance expressed as the HOMA-R (mmol·µIU/ml; r = -0.586, p = 0.004) and the fasting insulin levels (µIU/L; r =-0.650, p < 0.001) on the one hand and the serum SHBG levels (nmol/L) on the other. In healthy males (n = 51) correlation analysis showed similar results (Table 3). The significant relationship between serum levels of SHBG (nmol/ml) and the Homeostasis Model Assessment Ratio (HOMA-R; mmol·µIU/ml) both in non-diabetic males on chronic hemodialysis treatment (n = 22) and in healthy men (n = 51) is presented graphically in Fig. 2. In addition, in non-diabetic hemodialysis patients (n = 22) there was significant correlation between the HOMA-R (mmol·µIU/ml) on the one hand and the BMI (kg/m2), the body fat content (%), the hemodialysis treatment duration (months) and the SHBG (nmol/L) on the other (Table 3).
The significant relationship between the SHBG levels (nmol/L) and insulin resistance, i.e. the HOMA-R (mmol·µIU/ml), persisted in multiple regression analysis. Concretely, both BMI (kg/m2) and SHBG levels (nmol/L) statistically significantly predicted HOMA-R (mmol·µIU/ml), F(4, 18) = 9.565, p < 0.001, r2 = 0.692. Each independent variable, i.e. BMI and SHBG levels, added statistically significantly to the prediction of HOMA-R (p < 0.05). Detailed findings of the multiple linear regression analysis including SHBG (nmol/L), age (years), dialysis duration (months), BMI (kg/m2), fat content (%), waist circumference (cm) as predictor variables and HOMA-R (mmol·µIU/ml) as dependent variable are shown on Table 4. Further multivariate models of regression analysis dealing with the relationship of the SHBG levels (nmol/L) with HOMA-R (mmol·µIU/ml) are shown on Table 5.
Discussion
Our study examines whether testosterone and SHBG serum levels may relate to insulin resistance in men on chronic hemodialysis. Findings, in agreement with previous studies, showed an enhanced prevalence of biochemical hypogonadism with significantly decreased total testosterone levels and free androgen index (FAI) in men on chronic hemodialysis in comparison to healthy males [22]. Primary hypogonadism is predominant in end stage renal disease, most probably due to local accumulation of uremic toxins causing testicular dysfunction [23]. The pathogenic role of uremia is obvious from studies showing a rapid recovery of hypogonadism in males after receiving a kidney transplant [24]. This notion is strongly supported by findings of significantly decreased testosterone and enhanced LH and FSH levels, which parallel the progression of CKD, which failed to correct after human chorionic gonadotropin (hCG) administration both in uremic rats and humans [24].
In our study, serum SHBG levels were significantly higher in men on chronic hemodialysis than in healthy men. This finding is in agreement with previous studies, although evidence may be contradicting. Furthermore, neither kidney transplantation nor worsening kidney function in chronic kidney disease had been shown to influence SHBG levels. However, according to recent lines of evidence, there are also indications of potential connections between androgens and SHBG levels and kidney dysfunction in both men and women [25]. Men exhibiting lower SHBG levels face an increased likelihood of having a low estimated glomerular filtration rate (eGFR), indicating diminished kidney function [26].
Furthermore, the SHBG levels in our study negatively correlated with the measures of insulin resistance – HOMA-R and serum insulin – both in healthy men and in non-diabetic men on chronic hemodialysis. In contrast, the levels of total testosterone did not correlate with measures of insulin resistance. In the multiple regression-analysis independent predictors of insulin resistance were both SHBG levels and BMI. The relationship between SHBG levels and insulin resistance was independent from total testosterone and from the free androgen index (FAI). In addition, the enhanced levels of SHBG in hemodialysis patients were inversely related to HOMA-R supporting the hypothesis that SHBG is pathogenetically involved, ameliorating uremic insulin resistance.
In this context, SHBG seems to be independently associated with insulin resistance in our study. In both men and women without diabetes mellitus SHBG concentrations were previously shown to be, independently from sex steroids, inversely correlated with glycated hemoglobin.
In a post-hoc analysis of the Evaluation of Cinacalcet Therapy to Lower Cardiovascular Events (EVOLVE) randomized controlled trial serum levels of total testosterone, free testosterone, and SHBG were examined in relation to cardiovascular outcomes. Reduced serum levels of free testosterone and elevated levels of SHBG in men undergoing chronic hemodialysis were linked to an increased risk for mortality and cardiovascular morbidity [27].
In a recent meta-analysis of cohort studies low levels of both total and free testosterone were prognostic indicators for adverse clinical events in male patients with CKD [28]. More specifically, for every 1-standard deviation (SD) decrease in total testosterone, there was an independent increase in the risk of all-cause mortality by 27%, cardiovascular mortality by 100%, cardiovascular events by 20%, and infectious events by 41%. Additionally, a 1-SD decrease in free testosterone corresponded to a 66% increase in the risk of overall adverse events. Subgroup analysis demonstrated that the inverse association between total testosterone and the risk of all-cause death remained significant regardless of factors such as age, race, body mass index, diabetes, hypertension, C-reactive protein, creatinine, and sex hormone binding globulin [28]. Similarly in an additional recent meta-analysis low levels of endogenous testosterone could independently predict adverse clinical outcomes among male patients with CKD [29].
Chronic kidney disease (CKD) is an inflammatory condition, and inflammation exhibits a negative correlation with circulating testosterone levels, which tends to intensify in advanced CKD. It remains uncertain however whether the reduced testosterone levels are a cause or a consequence of inflammation in CKD. In agreement with this finding, inflammation and insulin resistance might serve as mediators in the connection between SHBG and CKD according to the results of a recent Mendelian randomization study [30]. In addition, based on the findings of another Mendelian randomization study in UK Biobank data, genetically predicted higher levels of SHBG were linked to reduced CKD risk and improved kidney function in men, but not in women [31]. This indicates a potential gender-specific role of SHBG in CKD. It has also been found that testosterone levels had a positive correlation with insulin resistance in men with Type 1 diabetes [32].
Weak points of the study presented here are both its cross-sectional design and the relative low sample size, a significant limitation which may obscure other contributing factors, such as the duration of dialysis. In this context, the post hoc power analysis gave a power of 80% for non-parametric comparisons and for correlation analyses.
Conclusions
Our findings confirm enhanced prevalence of biochemical hypogonadism in males on chronic hemodialysis. In non-diabetic cases the serum levels of SHBG correlated with serum insulin and insulin resistance. However, larger studies are needed to gain a deeper understanding of how androgens and SHBG might serve as modifiable risk factors for kidney function and CKD. Understanding the factors influencing SHBG levels and the underlying mechanisms could offer valuable insights into preventing and treating cardiovascular complications and CKD itself.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- BMI:
-
Body Mass Index
- BUN:
-
Blood urea nitrogen
- CKD:
-
Chronic kidney disease
- eGFR:
-
Estimated glomerular filtration rate
- FAI:
-
Free androgen index
- HOMA-R:
-
Homeostasis model assessment index
- IRMA:
-
Immunoradiometric assay
- PCR:
-
Protein catabolic rate
- SHBG:
-
Sex hormone binding globulin
- UF:
-
Ultrafiltration volume
- WHO:
-
World Health Organisation
References
Nakashima A, Kato K, Ohkido I, Yokoo T. Role and Treatment of Insulin Resistance in patients with chronic kidney disease: a review. Nutrients. 2021;13.
Schrauben SJ, Jepson C, Hsu JY, Wilson FP, Zhang X, Lash JP, et al. Insulin resistance and chronic kidney disease progression, cardiovascular events, and death: findings from the chronic renal insufficiency cohort study. BMC Nephrol. 2019;20:60.
Lambie M, Bonomini M, Davies SJ, Accili D, Arduini A, Zammit V. Insulin resistance in cardiovascular disease, uremia, and peritoneal dialysis. Trends Endocrinol Metabolism. 2021;32:721–30.
Carré JE, Affourtit C. Mitochondrial activity and Skeletal Muscle Insulin Resistance in kidney disease. Int J Mol Sci. 2019;20.
Uchiyama K, Wakino S, Irie J, Miyamoto J, Matsui A, Tajima T, et al. Contribution of uremic dysbiosis to insulin resistance and sarcopenia. Nephrol Dial Transpl. 2020;35:1501–17.
Romejko K, Rymarz A, Sadownik H, Niemczyk S. Testosterone Deficiency as one of the Major Endocrine disorders in chronic kidney disease. Nutrients. 2022;14.
Garibotto G, Esposito P, Picciotto D, Verzola D. Testosterone disorders and male hypogonadism in kidney disease. Semin Nephrol. 2021;41:114–25.
Yassin A, Haider A, Haider KS, Caliber M, Doros G, Saad F, et al. Testosterone therapy in Men with Hypogonadism prevents Progression from prediabetes to type 2 diabetes: eight-Year Data from a Registry Study. Diabetes Care. 2019;42:1104–11.
Amiri M, Ramezani Tehrani F, Rahmati M, Amanollahi Soudmand S, Behboudi-Gandevani S, Sabet Z, et al. Low serum testosterone levels and the incidence of chronic kidney disease among male adults: a prospective population-based study. Andrology. 2020;8:575–82.
Pivonello R, Menafra D, Riccio E, Garifalos F, Mazzella M, de Angelis C, et al. Metabolic disorders and male hypogonadotropic hypogonadism. Front Endocrinol (Lausanne). 2019;10:345.
Gyawali P, Martin SA, Heilbronn LK, Vincent AD, Jenkins AJ, Januszewski AS, et al. Higher serum sex hormone-binding globulin levels are Associated With Incident Cardiovascular Disease in men. J Clin Endocrinol Metab. 2019;104:6301–15.
O’Reilly MW, Glisic M, Kumarendran B, Subramanian A, Manolopoulos KN, Tahrani AA, et al. Serum testosterone, sex hormone-binding globulin and sex-specific risk of incident type 2 diabetes in a retrospective primary care cohort. Clin Endocrinol (Oxf). 2019;90:145–54.
Zhu J-L, Chen Z, Feng W-J, Long S-L, Mo Z-C. Sex hormone-binding globulin and polycystic ovary syndrome. Clin Chim Acta. 2019;499:142–8.
Leśniak K, Rymarz A, Sobol M, Dymus J, Woźniak-Kosek A, Niemczyk S. Testosterone Deficiency and Nutritional Parameters as Predictors of All-Cause Mortality among Male Dialysis Patients. Nutrients [Internet]. 2022;14. https://www.scopus.com/inward/record.uri?eid=2-s2.0-85141628895&doi=10.3390%2fnu14214461&partnerID=40&md5=0ae0bb0f179a3161d264e3fd1e1c7929
Basualto-Alarcón C, Llanos P, García-Rivas G, Troncoso MF, Lagos D, Barrientos G, et al. Classic and Novel Sex hormone binding globulin effects on the Cardiovascular System in men. Int J Endocrinol. 2021;2021:5527973.
Guadarrama-García C, Bello M, Soriano-Ursúa M. Molecular insights into how SHBG dimerization exerts changes on ligand molecular recognition. J Steroid Biochem Mol Biol. 2020;197:105502.
Aguas-Ayesa M, Yárnoz-Esquiroz P, Perdomo CM, Olazarán L, Vegas-Aguilar IM, García-Almeida JM, et al. Revisiting the beyond BMI paradigm in excess weight diagnosis and management: a call to action. Eur J Clin Invest. 2024;54:e14218.
Issaka A, Cameron AJ, Paradies Y, Kiwallo JB, Bosu WK, Houehanou YCN, et al. Associations between obesity indices and both type 2 diabetes and impaired fasting glucose among west African adults: results from WHO STEPS surveys. Nutr Metabolism Cardiovasc Dis. 2021;31:2652–60.
Loutradis C, Sarafidis PA, Ekart R, Papadopoulos C, Sachpekidis V, Alexandrou ME, et al. The effect of dry-weight reduction guided by lung ultrasound on ambulatory blood pressure in hemodialysis patients: a randomized controlled trial. Kidney Int. 2019;95:1505–13.
Casino FG, Deira J, Roblero MFS, González-Sanchidrian S, Dominguez SG, Bilbao IC, et al. Validation of formulas calculating normalized protein catabolic rate in patients undergoing home hemodialysis. J Nephrol. 2023;36:1965–74.
Singh J, Sahoo AK, Swain J, Mangaraj S, Kanwar JB, Manglunia A. Assessment of hypogonadism and its determinants among adult men with type 2 diabetes mellitus. Prim Care Diabetes. 2023;17:348–53.
Marcelli M, Mediwala SN. Male hypogonadism: a review. J Investig Med. 2020;68:335–56.
Oueslati I, Ounissi M, Talbi E, Azaiez S, Bacha MM, Ben Abdallah T. Prevalence and risk factors of hypogonadism in men with chronic renal failure. Tunis Med. 2020;98:138–43.
Kazemeini SM, Mogharabian N, Asadpour A, Naderi G, Kasaeian A, Mousavi A. The Effect of Renal Transplant on Hypogonadism and Erectile Dysfunction due to End-stage Renal Disease. Saudi Journal of Kidney Diseases and Transplantation [Internet]. 2021;32. https://journals.lww.com/sjkd/fulltext/2021/32040/the_effect_of_renal_transplant_on_hypogonadism_and.4.aspx.
Lau LHY, Nano J, Prehn C, Cecil A, Rathmann W, Zeller T, et al. Associations of endogenous androgens and sex hormone-binding globulin with kidney function and chronic kidney disease. Front Endocrinol (Lausanne). 2022;13:1000650.
Zhang H, Chen C, Zhang X, Wang Y, Wan H, Chen Y et al. Association between sex hormone-binding globulin and kidney function in men: results from the SPECT-China study. Chinese Medical Journal [Internet]. 2022;135. https://journals.lww.com/cmj/fulltext/2022/09050/association_between_sex_hormone_binding_globulin.9.aspx.
Nilsson E, Stenvinkel P, Liu S, Stedman MR, Chertow GM, Floege J. Serum testosterone concentrations and outcomes in hemodialysis patients enrolled in the EVOLVE trial. Nephrol Dial Transpl. 2023;38:1519–27.
Li L, Ju H, Jin H, Chen H, Sun M, Zhou Z. Low testosterone level and risk of adverse clinical events among male patients with chronic kidney disease: a systematic review and Meta-analysis of Cohort studies. J Healthc Eng. 2022;2022:3630429.
van der Burgh AC, Khan SR, Neggers SJCMM, Hoorn EJ, Chaker L. The role of serum testosterone and dehydroepiandrosterone sulfate in kidney function and clinical outcomes in chronic kidney disease: a systematic review and meta-analysis. Endocr Connect. 2022;11.
Zhao S, Li Y, Su C. Assessment of common risk factors of diabetes and chronic kidney disease: a Mendelian randomization study. Frontiers in Endocrinology [Internet]. 2023;14. https://www.frontiersin.org/journals/endocrinology/articles/https://doi.org/10.3389/fendo.2023.1265719.
Zhao JV, Schooling CM. Sex-specific Associations of Sex Hormone Binding Globulin with CKD and Kidney Function: A Univariable and Multivariable Mendelian Randomization Study in the UK Biobank. Journal of the American Society of Nephrology [Internet]. 2021;32. https://journals.lww.com/jasn/fulltext/2021/03000/sex_specific_associations_of_sex_hormone_binding.19.aspx.
Šimonienė D, Platūkiene A, Prakapienė E, Radzevičienė L, Veličkiene D. Insulin Resistance in type 1 diabetes Mellitus and its Association with Patient’s Micro- and macrovascular complications, sex hormones, and other Clinical Data. Diabetes Ther. 2020;11:161–74.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualization, I.S.; methodology, I.S, T.E., G.N.K., P.R.M.; software, M.T.; formal analysis, E.N., M.T., S.G.,G.F., A.B.; data curation, E.N., M.T.; writing—original draft preparation, M.T. and I.S. P.D. G.M.H.; visualization, M.T., I.S.; supervision, I.S. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Τhe study was approved by the Ethics Review Board of the University Hospital of Larissa.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nikolaou, E., Tziastoudi, M., Gougoura, S.G. et al. Sex hormone binding globulin (SHBG) serum levels and insulin resistance in men on chronic hemodialysis. Diabetol Metab Syndr 16, 166 (2024). https://doi.org/10.1186/s13098-024-01406-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-024-01406-9