Abstract
Background
Observational studies have indicated an association between diabetes mellitus (DM), glycemic traits, and the occurrence of Parkinson’s disease (PD). However, the complex interactions between these factors and the presence of a causal relationship remain unclear. Therefore, we aim to systematically assess the causal relationship between diabetes, glycemic traits, and PD onset, risk, and progression.
Method
We used two-sample Mendelian randomization (MR) to investigate potential associations between diabetes, glycemic traits, and PD. We used summary statistics from genome-wide association studies (GWAS). In addition, we employed multivariable Mendelian randomization to evaluate the mediating effects of anti-diabetic medications on the relationship between diabetes, glycemic traits, and PD. To ensure the robustness of our findings, we performed a series of sensitivity analyses.
Results
In our univariable Mendelian randomization (MR) analysis, we found evidence of a causal relationship between genetic susceptibility to type 1 diabetes (T1DM) and a reduced risk of PD (OR = 0.9708; 95% CI: 0.9466, 0.9956; P = 0.0214). In our multivariable MR analysis, after considering the conditions of anti-diabetic drug use, this correlation disappeared with adjustment for potential mediators, including anti-diabetic medications, insulin use, and metformin use.
Conclusion
Our MR study confirms a potential protective causal relationship between genetically predicted type 1 diabetes and reduced risk of PD, which may be mediated by factors related to anti-diabetic medications.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM) and Parkinson’s disease (PD) are disorders associated with aging, and their prevalence is increasing worldwide. In the past few decades, the global number of adult diabetes patients has increased from 108 million in 1980 to 422 million in 2014 [1]. At the same time, the age-standardized prevalence of diabetes in men increased from 4.3 to 9.0% and in women from 5.0–7.9% [1]. It is estimated that by 2045, the number of diabetes patients will increase to 783 million [2]. Parkinson’s disease (PD) is also a rapidly developing neurodegenerative disease, with a global average prevalence of 1–2‰ [3]. With the exacerbation of population aging, the burden of PD will become even heavier [4]. According to statistics, from 1990 to 2016, the incidence, disability burden, and mortality related to Parkinson’s disease have more than doubled. Furthermore, a global survey of neurological diseases shows that PD may be the fastest-growing neurological disease globally [5]. In recent years, the role of DM in neurodegeneration has grown special interest not only as a contributing factor to disease onset but also as a modifying factor of motor and nonmotor symptoms [6].
Some epidemiological studies suggest an association between diabetes and PD, but the results are not entirely consistent with some positive correlation studies [7]. A recent meta-analysis included 15 cohort studies (including over 86,000 PD cases and nearly 30 million participants), reporting a 27% increased risk of PD in patients with diabetes [8]. An earlier meta-analysis included 7 cohort studies (including 1,761,632 patients) and found that the risk of PD in patients with diabetes also increased by 38% [9]. It is worth noting that the results of a few case-control studies suggest that diabetes may reduce the risk of PD [10, 11]. This difference may be attributed to heterogeneity, confounding factors, and biases between studies (such as inclusion and recall biases) [10]. Therefore, the causal relationship between diabetes and PD is still controversial.
Factors such as ethical and moral constraints, methodological confounding, and reverse causality contribute to the lack of high-quality randomized controlled trial (RCT) data in observational studies. However, Mendelian randomization (MR) provides a promising alternative. MR, which conceptually resembles a randomized controlled trial, is based on the principle of random allocation of genetic variations during meiosis. This random allocation makes genetic variations independent of many factors influencing observational studies. To investigate the causal relationship between genetic liability to diabetes and glycemic traits with Age at onset (AAO), risk of PD, and progression (UPDRS3/MMSE/MOCA), we conducted univariable Mendelian randomization (UVMR). UVMR allows us to examine the potential causal effects of genetic variations on these outcomes. Considering the everyday use of clinical anti-diabetic medications in diabetes management, we implemented multivariable Mendelian randomization (MVMR) to account for biases induced by the concomitant use of anti-diabetic drugs. This approach allows us to control for the potential confounding effects of these medications on the observed associations.
Materials and methods
Study design
We used the two-sample MR method to investigate the potential causal relationship between diabetes, blood glucose traits, and PD. Specifically, we retrieved summary genetic data for exposure and outcome from two independent samples based on strict genetic instrumental variables (IVs) criteria, avoiding bias caused by overlap [12]. Finally, we used rigorously selected SNPs for our final MR analysis. Currently, the GWAS database of the European population is the largest publicly available, so we focused on studying participants of European ancestry.
All MR analyses in our study need to meet three fundamental assumptions: (I) Instrumental variables are closely related to the exposure; (II) Instrumental variables are independent of confounding factors; (III) Instrumental variables only affect the outcome through the exposure (see Fig. 1) [13]. The analysis was conducted using the TwoSampleMR package (version 0.5.6) in R software (version 4.2.2).
Data source
All data for this study were based on publicly available GWAS summary results (see Table 1). The T1DM data were obtained from a large GWAS summary dataset with a sample size of 520,580 (18,942 cases and 501,638 controls) [14]. The T2DM data were obtained from the Diabetes Genetics Replication and Meta-analysis (DIAGRAM) consortium, one of the most extensive collaborative efforts focused on characterizing the genetic basis of T2DM. This GWAS study involved 933,970 individuals of European ancestry, including 80,154 T2DM cases and 853,816 controls [15]. Additionally, data for other relevant traits such as glycated hemoglobin levels [14] (N~146,806), fasting glucose [14] (N~200,622), two-hour glucose [14](N~63,396), insulin fold change during an oral glucose tolerance test (adjusted for BMI) [16] (N~53,287), modified Stumvoll insulin sensitivity index (adjusted for BMI) [16] (N~53,657), fasting insulin [17] (N~151,013), and proinsulin [18] (N~45,861) were obtained from The Meta-Analyses of Glucose and Insulin-related traits Consortium (MAGIC).
PD-related phenotypic data AAO [19] (N~28,568), PD risk [20] (N~482,730), UPDRS3/MMSE/ MOCA [21] (N~4093) were obtained from the International Parkinson’s Disease Genomics Consortium (IPDGC) [22].
The phenotype data related to anti-diabetic drugs were obtained from the IEU Open GWAS project (https://gwas.mrcieu.ac.uk/), including Drugs used in diabetes [23](N~305,913), Diabetes, insulin treatment [24] (N~218,792), Metformin [24] (N~462,933).
All studies have obtained ethical approval from their respective institutional review boards and include written informed consent from the participants and strict quality control. Since all analyses in this paper are based on publicly available summary data, ethical approval from institutional review boards is not required for this study.
Selection of genetic instruments and data harmonization
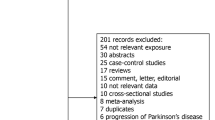
Select genetic instruments based on the following criteria (see Table S1): I. Choose genetic variants that are closely associated with the exposure (P < 5 × 10− 8, F-statistic > 10) and are independent [linkage disequilibrium (LD) r2 < 0.001, Window size = 1 Mb]. II. Remove SNPs closely associated with the outcome (p < 5 × 10− 8). III;. Apply the MR Pleiotropy RESidual Sum and Outlier (MR-PRESSO) test to remove potential outliers before each MR analysis (P < 0.05). III;. To determine whether SNPs are associated with potential risk factors, we searched all SNPs in PhenoScanner (Version 2, http://www.phenoscanner.medschl.cam.ac.uk/) [25, 26]. We removed SNPs associated with the disease or potential risk factors related to PD, including neurotoxins, smoking, coffee drinking, use of anti-inflammatory drugs, high plasma urate, physical activity, and obesity (see Table S2) [27]. The remaining SNPs were used in the MR analysis.
MR analysis
To avoid potential pleiotropic effects, we employed three different MR methods (inverse-variance weighted (IVW), MR-Egger regression, weighted median, and weighted mode) to assess the bidirectional causal effects between diabetes and PD. The results from the IVW method were used as the primary outcome. MR-Egger and weighted median complemented the IVW estimates (P < 0.05 indicating a causal relationship between exposure and outcome). IVW is a commonly used primary method in MR studies, which combines all Wald ratios of each SNP to obtain an overall estimate [28]. IVW assumes that all genetic variations are valid, making it the most efficient MR estimation method, but it is also prone to pleiotropic bias. Conversely, MR-Egger believes the instrument strength is independent of the direct effect (internal) and negligible measurement error (NOME) [29]. Weighted median assumes that at least half of the instruments are valid [30].
To demonstrate the reliability of our results, we conducted a series of sensitivity analyses to assess potential confounding factors. These factors include horizontal pleiotropy, heterogeneity, and reverse causality in the study. We utilized Cochran’s Q test and a funnel plot to measure potential heterogeneity. Cochran’s Q statistic evaluates heterogeneity among genetic variations, with a significance level of P < 0.05, indicating the presence of heterogeneity. To estimate horizontal pleiotropy, we performed the MR-Egger Intercept test. A significance level of P < 0.05 indicates the presence of horizontal pleiotropy [31]. We employed Steiger’s directional test to detect variations that are more strongly associated with the outcome than the exposure [32]. If the Steiger test provides evidence of a stronger association for specific genetic instruments, we repeated the analysis after excluding these variations [33]. To assess potential directional pleiotropy, we utilized a funnel plot. Additionally, we conducted a leave-one-out study to evaluate whether the causal relationship depends on or is biased by any individual SNP. Furthermore, we performed reverse MR analysis on results with PIVW < 0.05 to assess whether or not the results are influenced by reverse causality.
To address potential confounding caused by the combined use of diabetes, blood glucose traits, and anti-diabetic medication in assessing Parkinson’s disease-related phenotypes, we employed the Multivariable MR (MVMR) method [34]. Overall, these sensitivity analyses enhance the reliability of our findings by accounting for potential confounding factors and providing a more comprehensive assessment of the relationship between the variables of interest.
Results
Univariate conventional MR analysis showed a correlation between the genetic prediction of T1DM and a reduced risk of PD (IVW OR = 0.9708; 95% CI: 0.9466, 0.9956; P = 0.0214) (see Figs. 2 and 3; Table 2, S3). The estimated associations from MR Egger and Weighted median analyses were consistent with the observed associations in the primary study, but the confidence intervals were often imprecise. It is worth noting that these sensitivity methods have lower statistical power than IVW because they rely on more stringent assumptions; thus, their results are expected to provide weaker statistical evidence but cannot offer effect sizes. There is no statistical evidence for an impact of T2DM on the risk of PD (IVW OR = 1.0292; 95% CI: 0.9714, 1.0905; P = 0.3284). Furthermore, there is no statistical evidence to suggest an association between diabetes, glycemic traits, and other phenotypes of PD.
IVW estimates from Diabetes Mellitus, Glycemic traits on PD phenotypes. The color of each block represents the IVW-derived P-values for each MR analysis, examining the association between Diabetes mellitus, Glycemic traits, and PD (red indicates a positive association, and blue indicates a negative association). PD refers to Parkinson’s disease, AAO stands for Age at onset, UPDRS3 stands for Unified Parkinson’s Disease Rating Scale part III, MMSE stands for Mini-Mental State Examination, and MoCA stands for Montreal Cognitive Assessment
Mendelian randomization (MR) analysis results for T1DM and its impact on Parkinson’s disease (PD) risk. (A) A scatter plot illustrating the potential effects of single nucleotide polymorphisms (SNPs) on T1DM and PD risk using IVW, MR-Egger, and weighted median methods. The slope of the fitted lines represents the estimated MR effect per method, while the 95% CI for the effect size on T1DM is shown as vertical lines, and the 95% CI for PD risk is shown as horizontal lines. (B) A funnel plot for T1DM shows the estimation using the inverse of the standard error of the causal estimate with each SNP as a tool. The vertical line depicts the estimated causal effect obtained using IVW and MR-Egger methods. (C) A forest plot demonstrating the impact of each SNP in the MR analysis. (D) A forest plot presenting the results of the leave-one-out sensitivity analysis, where each SNP in the instrument was iteratively removed to check the stability of the result
We conducted a series of sensitivity tests to assess the accuracy of the optimistic estimates. These tests included Cochran’s Q-test, MR-Egger intercept, leave-one-out analysis, and funnel plot. The results of Cochran’s Q-test indicated no heterogeneity (P = 0.3968), suggesting that the studies included in our calculation were consistent. Additionally, the MR-Egger intercept test (P = 0.9704) did not detect potential horizontal pleiotropy, further supporting the reliability of our findings. Furthermore, the leave-one-out analysis results indicated that the causal effect was not driven by a single instrumental variable, suggesting that the observed association was robust. The symmetrical funnel plot also stated the results’ reliability, suggesting minimal publication bias. We conducted directionality checks using Steiger’s analysis to validate our findings further. These checks did not indicate a violation of the observed causal relationship, strengthening the evidence for our significant associations. Moreover, we performed reverse MR analysis to assess the influence of reverse causality on our results. The analysis showed that the results were unlikely to be influenced by reverse causality (IVW OR = 0.9347; 95% CI: 0.8657, 1.0092; P = 0.0844), providing additional support for the robustness of our findings(see Table S4).
In the context of MVMR, we evaluated the genetic risk of T1DM in combination with anti-diabetic drugs (see Table 3, 5). After adjusting for phenotypes related to anti-diabetic medications, such as drugs used in diabetes (IVW OR = 0.9812; 95% CI: 0.9324, 1.0325; P = 0.4740), diabetes, insulin treatment (IVW OR = 0.9822; 95% CI: 0.9463, 1.0194; P = 0.3380), and Metformin (IVW OR = 1.0000; 95% CI: 0.9825, 1.0178; P = 0.9930), the correlation between T1DM and PD risk was no longer significant. This suggests that the observed association between T1DM and PD risk may be confounded by the use of anti-diabetic drugs. The estimated associations from MR Egger and Weighted median analyses consistently aligned with the associations observed in IVW. Moreover, Cochran’s Q-test and MR-Egger intercept test did not reveal potential heterogeneity and pleiotropy, further supporting the robustness of our findings.
Discussion
In this analysis, we have demonstrated the potential protective effect of T1DM on PD risk. Our MVMR analysis suggests that this observed causal relationship may be driven by drug-related features of specific anti-diabetic medications. We thoroughly examined the data using various sensitivity methods in the MR analysis and found no significant pleiotropy or heterogeneity. Moreover, no evidence supports a causal relationship between genetically predicted T2DM and PD. To delve deeper into the topic, we further analyzed the causal relationship between glycemic traits and PD. However, the results of this analysis do not support a causal relationship between the two.
There has been a long-standing controversy regarding the association between DM and PD. Epidemiological evidence suggests an association between DM and PD, but the results are inconsistent, ranging from significant negative correlations to significant positive correlations [35,36,37,38,39,40]. Biological evidence demonstrates that both conditions are characterized by abnormal protein accumulation, lysosomal and mitochondrial dysfunction, and chronic systemic inflammation [41, 42]. Moreover, hypoinsulinemia in T1DM patients or insulin resistance (IR) in T2D patients leads to hyperglycemia, exposing neurons to increased metabolic stress, neuronal dysfunction, and death, thereby directly contributing to the development of PD [43]. Furthermore, several anti-diabetic drugs have been shown to have anti-PD effects, such as DPP-4 inhibitors and GLP-1 receptor agonists [44,45,46]. However, these studies often have relatively small sample sizes, which may introduce confounding, selection bias, and reverse causality, further limiting the interpretability of the results [47]. Additionally, case-control studies do not adequately address the temporal relationship between diabetes and PD since they rely on retrospective data and often fail to specify the time window for exposure assessment. Although large-scale prospective studies hold promise in overcoming these limitations, conducting such research requires significant human, financial, and time resources.
Although clinical trials have various limitations, early identification of risk factors for PD is crucial. Early intervention targeting relevant risk factors is currently the most effective approach to delay or prevent the onset of PD [48]. However, there is currently no effective cure once PD occurs. Compared to traditional epidemiology, MR analysis reveals the causal relationship between DM and PD cost-effectively, reducing confounding biases in epidemiological studies, including reverse causation [49, 50]. Three Mendelian randomization studies have recently been reported, investigating the causal inference of DM on PD in different populations. Chohan et al.‘s MR study on the European population reveals that genetically predicted T2DM leads to an increased risk and faster progression of PD, particularly in motor impairment [51]. Park et al.‘s MR study based on the Korean (East Asian) population suggests no evidence of a causal association between T2DM and PD. The authors explain this seemingly contradictory result as being due to a small sample size and ethnic differences [51, 52]. Additionally, Senkevich et al.‘s MR study on the European population suggests a potential protective association between genetically predicted T1DM and the risk and progression of PD, possibly driven by latent pleiotropy [53].
There is ongoing controversy regarding the relationship between DM and PD; given the complex association and significant clinical implications between the two, it is imperative to robustly replicate this association in larger GWAS study cohorts and explore potential underlying mechanisms. Consistent with the findings of Senkevich et al., our results confirm the causal relationship between T1DM and reduced risk of PD, and we further discovered that the use of anti-diabetic medications may mediate this causal relationship. Some traditional epidemiological approaches have also reported a lower risk of PD incidence in DM patients [37, 38, 54]. It has been reported that long-term use of anti-diabetic medications such as GLP-2 receptor agonists and DPP1 inhibitors may potentially reduce the risk of PD [45]. In recent years, an increasing body of research evidence supports the potential of anti-diabetic medications in reducing the risk of PD [55]. Using commonly used anti-diabetic drugs targeting the insulin signaling pathway has induced neuroprotective effects in preclinical studies and clinical trials. A longitudinal study of 5,528 veterans with T2DM showed that treatment with metformin for more than four years can reduce the risk of AD and PD [56]. The neuroprotective effect of metformin is mediated through the regulation of AMP-activated protein kinase (AMPK) activity, which modulates several critical cellular processes such as autophagy, cell growth, and mitochondrial function, as well as inhibiting microglial activation and inflammation [57,58,59,60]. Some studies have explored the neuroprotective potential of intranasal insulin. Preclinical data indicate that intranasal delivery of recombinant human insulin can reach deep brain structures, including the hippocampus and nigrostriatal pathway [61]. The study by Novak et al. showed that intranasal short-acting (regular) insulin treatment improved motor performance and function compared to placebo, resulting in lower disability scores (HY scale) and improved UPDRS motor scores compared to placebo [46].
Furthermore, other drugs, such as glucagon-like peptide 1 (GLP-1) agonists, can provide neuroprotection. Liraglutide and lixisenatide, both GLP-1 analogs, have been shown to induce neuroprotection in PD animal models [62]. These drugs can cross the blood-brain barrier (BBB), enhance hippocampal neurogenesis, and increase brain-derived neurotrophic factor (BDNF) expression, promoting neuroprotection in AD and PD [63, 64].
Our study highlights the potential protective effect of genetic prediction of T1DM on PD, suggesting that anti-diabetic drugs may play a crucial role in reducing PD risk. However, the exact mechanism underlying this protective effect remains unclear. Therefore, it is necessary to gather further direct evidence to validate our findings and develop effective PD prevention and management strategies.
We want to acknowledge certain limitations in our study. Firstly, it is essential to note that the associations observed through MR analysis do not provide information about temporal patterns but rather reflect lifelong effects on specific risk factors. Secondly, the sample size used for analyzing PD progression (UPDRS3/MMSE/MOCA) is relatively small, which may reduce the analytical power and potentially lead to false-negative results. Conducting larger-scale MR analyses will be essential to ensure the robustness of our findings. Additionally, it should be considered that genetic variations associated with T1DM may be correlated with multiple factors, which could represent alternative pathways through which these genetic variations influence PD. This potential horizontal pleiotropy should be taken into account when interpreting our results. Lastly, it is worth mentioning that our study primarily focuses on individuals of European ancestry. Further research is needed to determine whether our findings can be generalized to other ethnicities.
Conclusion
In summary, our study discovered a direct causal relationship between genetic predictions of T1DM and a decreased risk of PD in individuals of European ancestry. Moreover, there is indirect evidence indicating that anti-diabetic drugs may mediate the protective effect of T1DM against PD. However, further research is needed to fully understand the mechanisms by which anti-diabetic drugs exert their anti-PD effects and to identify potential therapeutic targets.
Data availability
The summary statistics analyzed in the study are included in the article. MAGIC investigators have contributed data on glycaemic traits and have been downloaded from www.magicinvestigators.org
References
Worldwide trends in diabetes. Since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–30.
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, Stein C, Basit A, Chan JCN, Mbanya JC, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119.
Tysnes OB, Storstein A. Epidemiology of Parkinson’s disease. J Neural Transm (Vienna). 2017;124(8):901–5.
The Lancet N. Parkinson’s disease needs an urgent public health response. Lancet Neurol. 2022;21(9):759.
Global regional, national burden of neurological disorders. 1990–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459–80.
Labandeira CM, Fraga-Bau A, Arias Ron D, Alvarez-Rodriguez E, Vicente-Alba P, Lago-Garma J, Rodriguez-Perez AI. Parkinson’s disease and diabetes mellitus: common mechanisms and treatment repurposing. Neural Regen Res. 2022;17(8):1652–8.
Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017., et al. Lancet. 2018;392(10159):1923–94.
Aune D, Schlesinger S, Mahamat-Saleh Y, Zheng B, Udeh-Momoh CT, Middleton LT. Diabetes mellitus, prediabetes and the risk of Parkinson’s disease: a systematic review and meta-analysis of 15 cohort studies with 29.9 million participants and 86,345 cases. Eur J Epidemiol. 2023;38(6):591–604.
Yue X, Li H, Yan H, Zhang P, Chang L, Li T. Risk of Parkinson Disease in Diabetes Mellitus: an updated Meta-analysis of Population-based Cohort studies. Med (Baltim). 2016;95(18):e3549.
Cereda E, Barichella M, Pedrolli C, Klersy C, Cassani E, Caccialanza R, Pezzoli G. Diabetes and risk of Parkinson’s disease: a systematic review and meta-analysis. Diabetes Care. 2011;34(12):2614–23.
Lu L, Fu DL, Li HQ, Liu AJ, Li JH, Zheng GQ. Diabetes and risk of Parkinson’s disease: an updated meta-analysis of case-control studies. PLoS ONE. 2014;9(1):e85781.
Burgess S, Davies NM, Thompson SG. Bias due to participant overlap in two-sample mendelian randomization. Genet Epidemiol. 2016;40(7):597–608.
Emdin CA, Khera AV, Kathiresan S. Mendelian randomization. JAMA. 2017;318(19):1925–6.
Chiou J, Geusz RJ, Okino ML, Han JY, Miller M, Melton R, Beebe E, Benaglio P, Huang S, Korgaonkar K, et al. Interpreting type 1 diabetes risk with genetics and single-cell epigenomics. Nature. 2021;594(7863):398–402.
Mahajan A, Spracklen CN, Zhang W, Ng MCY, Petty LE, Kitajima H, Yu GZ, Rüeger S, Speidel L, Kim YJ, et al. Multi-ancestry genetic study of type 2 diabetes highlights the power of diverse populations for discovery and translation. Nat Genet. 2022;54(5):560–72.
Williamson A, Norris DM, Yin X, Broadaway KA, Moxley AH, Vadlamudi S, Wilson EP, Jackson AU, Ahuja V, Andersen MK, et al. Genome-wide association study and functional characterization identifies candidate genes for insulin-stimulated glucose uptake. Nat Genet. 2023;55(6):973–83.
Chen J, Spracklen CN, Marenne G, Varshney A, Corbin LJ, Luan J, Willems SM, Wu Y, Zhang X, Horikoshi M, et al. The trans-ancestral genomic architecture of glycemic traits. Nat Genet. 2021;53(6):840–60.
Broadaway KA, Yin X, Williamson A, Parsons VA, Wilson EP, Moxley AH, Vadlamudi S, Varshney A, Jackson AU, Ahuja V, et al. Loci for insulin processing and secretion provide insight into type 2 diabetes risk. Am J Hum Genet. 2023;110(2):284–99.
Blauwendraat C, Heilbron K, Vallerga CL, Bandres-Ciga S, von Coelln R, Pihlstrøm L, Simón-Sánchez J, Schulte C, Sharma M, Krohn L, et al. Parkinson’s disease age at onset genome-wide association study: defining heritability, genetic loci, and α-synuclein mechanisms. Mov Disord. 2019;34(6):866–75.
Nalls MA, Blauwendraat C, Vallerga CL, Heilbron K, Bandres-Ciga S, Chang D, Tan M, Kia DA, Noyce AJ, Xue A, et al. Identification of novel risk loci, causal insights, and heritable risk for Parkinson’s disease: a meta-analysis of genome-wide association studies. Lancet Neurol. 2019;18(12):1091–102.
Iwaki H, Blauwendraat C, Leonard HL, Kim JJ, Liu G, Maple-Grødem J, Corvol JC, Pihlstrøm L, van Nimwegen M, Hutten SJ, et al. Genomewide association study of Parkinson’s disease clinical biomarkers in 12 longitudinal patients’ cohorts. Mov Disord. 2019;34(12):1839–50.
Ten Years of the International Parkinson Disease Genomics Consortium. Progress and next steps. J Parkinsons Dis. 2020;10(1):19–30.
Wu Y, Byrne EM, Zheng Z, Kemper KE, Yengo L, Mallett AJ, Yang J, Visscher PM, Wray NR. Genome-wide association study of medication-use and associated disease in the UK Biobank. Nat Commun. 2019;10(1):1891.
Kurki MI, Karjalainen J, Palta P, Sipilä TP, Kristiansson K, Donner KM, Reeve MP, Laivuori H, Aavikko M, Kaunisto MA, et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature. 2023;613(7944):508–18.
Sleiman PM, Grant SF. Mendelian randomization in the era of genomewide association studies. Clin Chem. 2010;56(5):723–8.
Staley JR, Blackshaw J, Kamat MA, Ellis S, Surendran P, Sun BB, Paul DS, Freitag D, Burgess S, Danesh J, et al. PhenoScanner: a database of human genotype-phenotype associations. Bioinformatics. 2016;32(20):3207–9.
Bloem BR, Okun MS, Klein C. Parkinson’s disease. Lancet. 2021;397(10291):2284–303.
Pierce BL, Burgess S. Efficient design for mendelian randomization studies: subsample and 2-sample instrumental variable estimators. Am J Epidemiol. 2013;178(7):1177–84.
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512–25.
Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in mendelian randomization with some Invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40(4):304–14.
Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from mendelian randomization between complex traits and diseases. Nat Genet. 2018;50(5):693–8.
Hemani G, Tilling K, Davey Smith G. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet. 2017;13(11):e1007081.
Burgess S, Davey Smith G, Davies NM, Dudbridge F, Gill D, Glymour MM, Hartwig FP, Kutalik Z, Holmes MV, Minelli C, et al. Guidelines for performing mendelian randomization investigations: update for summer 2023. Wellcome Open Res. 2019;4:186.
Sanderson E, Davey Smith G, Windmeijer F, Bowden J. An examination of multivariable mendelian randomization in the single-sample and two-sample summary data settings. Int J Epidemiol. 2019;48(3):713–27.
Becker C, Brobert GP, Johansson S, Jick SS, Meier CR. Diabetes in patients with idiopathic Parkinson’s disease. Diabetes Care. 2008;31(9):1808–12.
Powers KM, Smith-Weller T, Franklin GM, Longstreth WT Jr., Swanson PD, Checkoway H. Diabetes, smoking, and other medical conditions in relation to Parkinson’s disease risk. Parkinsonism Relat Disord. 2006;12(3):185–9.
Scigliano G, Musicco M, Soliveri P, Piccolo I, Ronchetti G, Girotti F. Reduced risk factors for vascular disorders in Parkinson disease patients: a case-control study. Stroke. 2006;37(5):1184–8.
D’Amelio M, Ragonese P, Callari G, Di Benedetto N, Palmeri B, Terruso V, Salemi G, Famoso G, Aridon P, Savettieri G. Diabetes preceding Parkinson’s disease onset. A case-control study. Parkinsonism Relat Disord. 2009;15(9):660–4.
Hu G, Jousilahti P, Bidel S, Antikainen R, Tuomilehto J. Type 2 diabetes and the risk of Parkinson’s disease. Diabetes Care. 2007;30(4):842–7.
Simon KC, Chen H, Schwarzschild M, Ascherio A. Hypertension, hypercholesterolemia, diabetes, and risk of Parkinson disease. Neurology. 2007;69(17):1688–95.
Athauda D, Foltynie T. Insulin resistance and Parkinson’s disease: a new target for disease modification? Prog Neurobiol. 2016;145–146:98–120.
Cheong JLY, de Pablo-Fernandez E, Foltynie T, Noyce AJ. The Association between type 2 diabetes Mellitus and Parkinson’s Disease. J Parkinsons Dis. 2020;10(3):775–89.
Morsi M, Maher A, Aboelmagd O, Johar D, Bernstein L. A shared comparison of diabetes mellitus and neurodegenerative disorders. J Cell Biochem. 2018;119(2):1249–56.
Bayram E, Litvan I. Lowering the risk of Parkinson’s disease with GLP-1 agonists and DPP4 inhibitors in type 2 diabetes. Brain. 2020;143(10):2868–71.
Brauer R, Wei L, Ma T, Athauda D, Girges C, Vijiaratnam N, Auld G, Whittlesea C, Wong I, Foltynie T. Diabetes medications and risk of Parkinson’s disease: a cohort study of patients with diabetes. Brain. 2020;143(10):3067–76.
Novak P, Pimentel Maldonado DA, Novak V. Safety and preliminary efficacy of intranasal insulin for cognitive impairment in Parkinson disease and multiple system atrophy: a double-blinded placebo-controlled pilot study. PLoS ONE. 2019;14(4):e0214364.
Boyko EJ. Observational research–opportunities and limitations. J Diabetes Complications. 2013;27(6):642–8.
Ascherio A, Schwarzschild MA. The epidemiology of Parkinson’s disease: risk factors and prevention. Lancet Neurol. 2016;15(12):1257–72.
Davey Smith G, Ebrahim S. What can mendelian randomisation tell us about modifiable behavioural and environmental exposures? BMJ. 2005;330(7499):1076–9.
Skrivankova VW, Richmond RC, Woolf BAR, Yarmolinsky J, Davies NM, Swanson SA, VanderWeele TJ, Higgins JPT, Timpson NJ, Dimou N, et al. Strengthening the reporting of Observational studies in Epidemiology using mendelian randomization: the STROBE-MR Statement. JAMA. 2021;326(16):1614–21.
Chohan H, Senkevich K, Patel RK, Bestwick JP, Jacobs BM, Bandres Ciga S, Gan-Or Z, Noyce AJ. Type 2 diabetes as a determinant of Parkinson’s Disease Risk and Progression. Mov Disord. 2021;36(6):1420–9.
Park KW, Hwang YS, Lee SH, Jo S, Chung SJ. The effect of blood lipids, type 2 diabetes, and body Mass Index on Parkinson’s disease: a Korean mendelian randomization study. J Mov Disord. 2023;16(1):79–85.
Senkevich K, Alipour P, Chernyavskaya E, Yu E, Noyce AJ, Gan-Or Z. Potential protective link between type I diabetes and Parkinson’s Disease Risk and Progression. Mov Disord. 2023;38(7):1350–5.
Miyake Y, Tanaka K, Fukushima W, Sasaki S, Kiyohara C, Tsuboi Y, Yamada T, Oeda T, Miki T, Kawamura N, et al. Case-control study of risk of Parkinson’s disease in relation to hypertension, hypercholesterolemia, and diabetes in Japan. J Neurol Sci. 2010;293(1–2):82–6.
Mullard A. Diabetes drug shows promise in Parkinson disease. Nat Rev Drug Discov. 2017;16(9):593.
Shi Q, Liu S, Fonseca VA, Thethi TK, Shi L. Effect of metformin on neurodegenerative disease among elderly adult US veterans with type 2 diabetes mellitus. BMJ Open. 2019;9(7):e024954.
Wang Y, An H, Liu T, Qin C, Sesaki H, Guo S, Radovick S, Hussain M, Maheshwari A, Wondisford FE, et al. Metformin improves mitochondrial respiratory activity through activation of AMPK. Cell Rep. 2019;29(6):1511–1523e1515.
Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, Wu M, Ventre J, Doebber T, Fujii N, et al. Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest. 2001;108(8):1167–74.
Wen Z, Zhang J, Tang P, Tu N, Wang K, Wu G. Overexpression of miR–185 inhibits autophagy and apoptosis of dopaminergic neurons by regulating the AMPK/mTOR signaling pathway in Parkinson’s disease. Mol Med Rep. 2018;17(1):131–7.
Tayara K, Espinosa-Oliva AM, García-Domínguez I, Ismaiel AA, Boza-Serrano A, Deierborg T, Machado A, Herrera AJ, Venero JL, de Pablos RM. Divergent effects of Metformin on an inflammatory model of Parkinson’s Disease. Front Cell Neurosci. 2018;12:440.
Fan LW, Carter K, Bhatt A, Pang Y. Rapid transport of insulin to the brain following intranasal administration in rats. Neural Regen Res. 2019;14(6):1046–51.
Liu W, Jalewa J, Sharma M, Li G, Li L, Hölscher C. Neuroprotective effects of lixisenatide and liraglutide in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model of Parkinson’s disease. Neuroscience. 2015;303:42–50.
Hunter K, Hölscher C. Drugs developed to treat diabetes, liraglutide and lixisenatide, cross the blood brain barrier and enhance neurogenesis. BMC Neurosci. 2012;13:33.
Hölscher C. The incretin hormones glucagonlike peptide 1 and glucose-dependent insulinotropic polypeptide are neuroprotective in mouse models of Alzheimer’s disease. Alzheimers Dement. 2014;10(1 Suppl):47–54.
Acknowledgements
The authors thank all the relevant consortiums and investigators for the management and sharing of summary-level data.
Funding
This work was supported by Hainan Provincial Natural Science Foundat ion of China823MS133823MS133; Hainan Key Scientific Research Projects (14A110060), Key R&D Plan Projects of Hainan Province (ZDYF2021SHFZ091), Hainan Natural Science Foundation Innovative Research Team Projects (2016CXTD010), Key Educational Reform Projects of Hainan Province (Hnjg2019ZD-15), and High-level Talents of the Hainan Natural Science Foundation (820RC759). This work was Supported by the Construction Project of Hainan Province Clinical Medical Center and Science, Innovation Platform for Academicians of Hainan Province. The funding bodies had no role in the design of the study; the collection, analysis, or interpretation of the data; or the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
QW: Conceptualization, Writing– original draft, Formal analysis. BC: Writing– original draft, Formal analysis. LZ: Writing– original draft, Formal analysis. JI: Writing– original draft, Formal analysis. TC: Conceptualization, Writing– review & editing, Formal analysis. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Q., Cai, B., Zhong, L. et al. Causal relationship between diabetes mellitus, glycemic traits and Parkinson’s disease: a multivariable mendelian randomization analysis. Diabetol Metab Syndr 16, 59 (2024). https://doi.org/10.1186/s13098-024-01299-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-024-01299-8