Abstract
Background
Most studies initiated basal-bolus insulin in a ratio of 1:1 and titrated based on glucose. This study aimed to investigate the effectiveness and safety of a weight-based and ratio of 1:1.5 basal-bolus insulin using an algorithm for both initiation and titration in hospitalized patients with type 2 diabetes (T2D).
Methods
Hospitalized patients with T2D were randomly assigned to two groups in equal numbers to receive 1:1.5 and 1:1 ratios of basal-bolus insulin using a weight-based algorithm for both initiation and titration. The primary outcome was the time taken to reach the fasting blood glucose (FBG) target and 2-h postprandial blood glucose (2hBG) targets after three meals. The secondary outcome included insulin dosage to achieve glycemic control and the incidence of hypoglycemia during hospitalization.
Results
250 patients were screened between October 2021 and June 2022, 220 were randomly grouped, and 182 completed the trial (89 in the 1:1.5 and 93 in the 1:1 groups). The time taken to reach FBG targets was comparable between the two groups (3.4 ± 1.7 vs. 3.0 ± 1.3 days, p = 0.137) within about 3 days. The 2hBG after three meals was shorter in the 1:1.5 group than in the 1:1group (2.9 ± 1.5 vs. 3.4 ± 1.4 days, p = 0.015 for breakfast, 3.0 ± 1.6 vs. 3.6 ± 1.4 days, p = 0.005 for lunch, and 3.1 ± 2.1 vs. 4.0 ± 1.5 days, p = 0.002 for dinner). No significant difference in insulin dosages was found between the two groups at the end of the study. The incidence of hypoglycemia was similar in both groups.
Conclusions
We demonstrated that fixed dose-ratio basal-bolus insulin at 1:1.5 calculated using a weight-based initiation and titration algorithm was simple, as effective, and safe as ratio at 1:1 in managing T2D in hospitalized patients.
Trial Registration ChiCTR 2,100,050,963. Date of registration: September 8, 2021.
Similar content being viewed by others
Background
Hospitalized patients with hyperglycemia require a longer hospital stay and face several complications [1, 2]. The glycemic level at fasting (fasting blood glucose, FBG) and 2-h postprandial blood glucose (2hBG) targeting 7.8 and 10.0 mmol/L, respectively, in non-critically ill patients with hyperglycemia, could prevent adverse outcomes [2, 3].
Insulin is superior to other medications for the rapid control of hyperglycemia in hospitalized patients. The normal physiological pattern of insulin secretion by the pancreas consists of basal release and burst of bolus insulin. American Association of Clinical Endocrinologists (AACE) and American Diabetes Association (ADA) recommend basal-bolus insulin instead of slide-scale insulin for glycemic control due to its effectiveness and safety [4]. However, the latest survey revealed that more than 30% of physicians still prefer to use slide-scale insulin in clinical practice because the administration of bolus insulin is complex [5,6,7]. Many studies simplified the insulin administration regimen, for example, by using basal plus [7], reducing correction insulin administration [8, 9], using premixed insulin [10], or only using basal insulin [11].
In healthy individuals, the ratio of basal and bolus insulin levels is 50:50 [12]. Therefore, when initiating insulin therapy in hospitalized patients with type 2 diabetes (T2D) one-half of the total daily dose (TDD) was given as a basal dose (glargine or determir) once daily at bedtime, and the other half was given as a bolus (aspart, lispo, or glulisine) in equally divided doses before breakfast, lunch, and dinner regardless of TDD calculation based on body mass index (BMI) or random glucose level [2, 13, 14]. At the end of the corresponding clinical trials, Umpierrez found that the ratio of basal-bolus was about 1:1 in their two clinical trials (glargine to glulisine, 22:20 units/day and 43:42 units/day) and Meyer et al. found the ratio as about 1:1 (glargine to glulisine 33:36 units/day) [13,14,15].
Currently, the initial and final ratio of basal-bolus are kept at 1:1. We also designed a study that had a titrating ratio of 1:1 during the middle period. Surprisingly, when FBG and three 2hBG reached the target levels, the ratio was 1:1.5 (glargine to aspart, 25:36 units/day) [16]. Liu et al. used a continuous subcutaneous infusion of titrated insulin and the study found a ratio of 1:1.5 when the target glucose level was attained [17]. A study with the Latin American non-intensive care unit patients with T2D used basal-bolus and had a ratio of about 1:1.5 (glargine to glulisine, 22:31 units/day) [18].
This multicenter, randomized, controlled clinical study aimed to investigate whether the weight-based, 1:1.5 basal-bolus insulin initiation and titration using an algorithm is superior to 1:1.
Patients
This multicenter, randomized prospective study was performed in the department of endocrinology of four medical centers (The Second Affiliated Hospital of Guangzhou Medical University, The Third Affiliated Hospital of Southern Medical University, the Fifth Affiliated Hospital of Guangzhou Medical University, and the First Affiliated Hospital of Shenzhen University) between October 2021 and June 2022. Informed consent was obtained from each participant. This study was approved by the ethics Committee of our hospital.
Inclusion/exclusion criteria
Patients who were aged between 18 and 75 years and diagnosed previously or newly with T2D, with a blood glucose (BG) level of > 10.0 mmol/L on admission were randomly selected for the current study. The patients were excluded if they were in one of the following criteria: (i) patients who received insulin therapy at a daily dosage of > 0.4 U/kg before admission. This is because one of our group initiated insulin 0.4 U/kg, if patient had used a daily dosage of > 0.4 U/kg before admission, their glucose maybe worsen ; (ii) patients who were unable to eat; (iii) patients who received corticosteroid therapy; (iv) patients who had renal insufficiency with the plasma creatinine concentration of ≥ 130 µmol/L or liver insufficiency (aspartate aminotransferase or alanine aminotransferase concentration of ≥ two-fold normal range), this is because insulin was metabolized in liver and kidney; (v) patients who were pregnant; (vi) patients with a previous or current history of malignant tumors.
Randomization
Randomization codes were generated using a computer program (SPSS V.25.0). Patients were randomly assigned at a ratio of 1:1 to the two treatment groups on the first day of admission at the four medical centers. Neither patients nor investigators were masked to the treatment group.
Study protocol
Basal insulin bolus consisting of a subcutaneous injection of glargine (Sanofi Aventis Deutschland GmbH, Frankfurt, Germany) at bedtime and aspart (Novo Nordisk, Bagsværd, Denmark) before each of three meals. The blood glucose levels of the patients were checked during the round at 09:00 h and insulin titration dose was determined by physicians based on FBG in the morning and 2hBG after breakfast from the same day and 2hBG after lunch and dinner from the previous day.
All other antidiabetic agents were discontinued on the day of admission. Insulin was initiated at a TDD of 0.5 units/kg in the 1:1.5 group and 0.4 units/kg in the 1:1 group. The 1:1.5 group received 40% (0.2 units/kg) of the TDD as glargine and 60% (0.3 units/kg) as aspart. The 1:1 group received 50% (0.2 units/kg) of the TDD as glargine and 50% as aspart (0.2 units/kg). Glargine was administered as a single daily dose while aspart was divided into three equal parts.
Both glargine and aspart were titrated using a weight-based algorithm. In the 1:1.5 and 1:1 groups, glargine was titrated at 0.1 units/kg/day. In the 1:1.5 group, aspart was titrated at 0.05 units/kg/day, and in the 1:1 group, aspart was titrated at 1/3 of 0.1 units/kg/day before each meal. When one 2hBG level reached the target, the aspart was not titrated further (Table 1). The FBG and 2hBG target levels were set at 7.8 mmol/L and 10.0 mmol/L, respectively, as recommended by the American Endocrine Society, respectively (Table 1) [2]. If hypoglycemia was seen, the corresponding insulin titration was held.
Blood glucose levels at five points were measured, including FBG, 2hBG after three meals, and BG at 03:00 h using a glucose meter (Accu-Chek Advantage; Roche Diagnostics, Basel, Switzerland). Additionally, the glucose levels were measured when patients reported symptoms of hypoglycemia. Hypoglycemia was classified into three categories (level 1:3.0 ≤ BG < 3.9 mmol/L; level 2: BG < 3.0 mmol/L; level 3: a severe event that requires assistance from another person for treatment of hypoglycemia). Hemoglobin A1c (HbA1c) was tested in all patients on day 2 of hospitalization.
All centers ordered dietary profile according to our textbook. First, we calculated ideal weight (kg) which is height (cm) minus 105. Second, we calculated total energy between 25 (overweight or obese) and 30 (normal weight or lean) kcal/kg/day. Third, in our diet, protein was given 1.0 g/kg ideal weight, fat was given 0.8 g/kg ideal weight, and left energy was given as carbohydrate which account for about 50–55% of total energy. Total calories were divided in a ratio of 1:2:2 across the three daily meals.
Outcome measures
The primary outcome of the study was the time for achieving FBG and 2hBG target levels. The secondary outcome was the incidence of hypoglycemia during hospitalization.
Statistical analysis
The primary endpoint was considered on the day when 2hBG reached the target level after three meals. Based on our previous study [9], a significant difference in the time was considered when 2hBG reached the target level on any 1 day between the two groups. Assuming significant differences of three points with α = 0.05% and 90% power, the required number of patients for each group was 86. To allow a 20% dropout rate, it needed 215 patients and we recruited 220 patients. The basic characteristics of subjects and outcome variables were compared using an independent t-test or χ2 test as appropriate. Statistical analyses were performed using the SPSS version 25.0 (SPSS, Chicago, IL). The p-value of < 0.05 was considered statistically significant. Data were provided as means ± SD or median (range).
Results
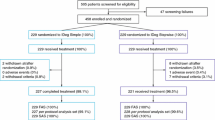
Figure 1 shows the patients’ selection. Between October 2021 and June 2022 the number of patients screened was 250. Among them, 220 were selected to randomly assign in equal numbers to the 1:1.5 and 1:1 of glargine to aspart groups. During hospitalization, 21 patients from the 1:1.5 group and 17 from the 1:1 group dropped out of the study. Therefore, 89 patients in the 1:1.5 group and 93 patients in the 1:1 group were analyzed. As shown in Table 2, both groups were well-matched for age, sex, BMI, and initial BG levels. The distribution of previous antidiabetic treatments was also similar in the two groups. The diagnoses on admission included isolated hyperglycemia, diabetic ketoacidosis, and infections.
Length of time for reaching BG target levels
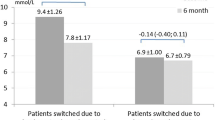
The length of time for reaching the FBG and 2hBG target levels after breakfast, lunch, and dinner in the 1:1.5 group and the 1:1 group were 3.4 ± 1.7 vs. 3.0 ± 1.3 days (p = 0.137), 2.9 ± 1.5 vs. 3.4 ± 1.4 days (p = 0.015), 3.0 ± 1.6 vs. 3.6 ± 1.4 days (p = 0.005), and 3.1 ± 2.1 vs. 4.0 ± 1.5 days (p = 0.002), respectively (Fig. 2A).
A The number of days taken to reach FBG and 2hBG target levels. B, breakfast; L, lunch; D, dinner. The time taken to reach the FBG target level was not significant between the two groups. The time taken to reach three 2hBG target levels was significant between the two groups. B Insulin dosage at the end of treatment. B, breakfast; L, lunch; D, dinner. The dosage of glargine, pre-breakfast, pre-lunch, and pre-dinner aspart were not significant between the two groups. C The percentage of hypoglycemia episode in the 1:1.5 and 1:1 basal-bolus groups
Figure 2 A. The number of days taken to reach FBG and 2hBG target levels. B, breakfast; L, lunch; D, dinner. The time taken to reach the FBG target level was not significant between the two groups. The time taken to reach three 2hBG target levels was significant (p = 0.015, 0.005, and 0.002, respectively) between the two groups.
In the 1:1.5 group, 4 patients had two BG levels and 3 patients had one BG level that did not reach the targets. In the 1:1 group, 4 patients had three BG levels and 5 patients had one BG level that did not reach the targets.
Insulin dosage
The dose of glargine, pre-breakfast aspart, pre-lunch aspart, and pre-dinner aspart in the 1:1.5 group and the 1:1group were 27.5 ± 11.7 vs. 26.1 ± 9.9 units/day (p = 0.339), 13.2 ± 5.6 vs. 11.9 ± 5.0 units/day (p = 0.113), 13.7 ± 6.2 vs. 12.4 ± 4.9 units/day (p = 0.133), and 14.1 ± 6.9 vs. 12.8 ± 5.0 units/day (p = 0.169), respectively (Fig. 2B).
Hypoglycemia
The percentage of hypoglycemia episodes in the morning (6:30 − 12:00), afternoon (12:00–17:30), evening (17:30 − 23:00), and night (23:00–6:30) in the 1:1.5 group and the 1:1group were 11.2% (10/89. level 1, 8(9.0%); level 2, 2(2.2%)) vs. 14.0% (13/93. level 1, 11(11.8%); level 2, 2(2.2%)), p = 0.578; 9.0% (8/89. level 1, 7(7.9%); level 2, 1(1.1%)) vs. 4.3% (4/93. level 1, 3(3.2%); level 2, 1(1.1%)), p = 0.203; 5.6% (5/89. level 1, 5(5.6%); level 2, 0(0.0%)) vs. 5.4% (5/93, level 1, 4(4.3%); level 2, 1(1.1%)), p = 0.943; and 1.1% (1/89. level 1, 1(1.1%); level 2, 0(0.0%)) vs. 3.2% (3/93. level 1, 3(3.2%); level 2, 0(0.0%)), p = 0.328, respectively (Fig. 2C).
Discussion
Our previous studies found that weight-based basal and bolus insulin treatment had the same effectiveness and safety as the glucose level-based treatment calculated using an algorithm [16, 19]. Through the present study, using an insulin initiation and titration by weight-based algorithm, a basal-bolus insulin regimen with a fixed dose and ratio of 1:1.5 achieved the BG target levels in a shorter period compared with the 1:1 ratio in hospitalized patients with T2D. The dosages at initiation were 0.2 units/kg for glargine and 0.1 units/kg for aspart to each meal, and those at titration were 0.1 units/kg for glargine and 0.05 units/kg for aspart to each meal daily. Both FBG and 2hBG achieved the target levels in about 3 days. This efficacy was similar to a famous trial that used basal-bolus correction and a glucose-based regimen and achieved mean glucose levels of less than 10.0 mmol/L by day 2 and of less than 8.9 mmol/L by day 4 [13]. The effectiveness of the ratio 1:1.5 could be justified by several explanations. First, patients in this study all had T2D which might have had different pathophysiology compared to the physiological insulin secretion. Also, glargine and aspart are all exogenous insulins. Second, although aspart is considered short-acting insulin, it is sufficient for more than 5 h [20], and the tapering level contributes to the basal insulin. Third, although hospitalized patients in this study had a fixed calorie and fixed proportion of carbohydrates, the Chinese might have preferred more carbohydrates to others [21]. A study conducted with the Latin American non-intensive care unit patients with T2D who used basal-bolus showed a ratio of about 2:3 (glargine 22 units/day and glulisine 31 units/day) to reach a target blood glucose level [18].
In literature and practice, most physicians initiate basal-bolus insulin with a ratio of 1:1 [13,14,15,16]. Only in the Johns Hopkins hospital, insulin is initiated in a basal-bolus ratio of 1:1.5 in hospitalized patients [22]. However, the John Hopkins hospital titrates basal bolus based on glucose level which is different from ours which was based on body weight.
Although AACE and ADA recommend basal-bolus insulin instead of slide-scale insulin for glycemic control in hospitalized patients [4], the slide-scale dosage remains the most popular regimen in the majority of hospitals because of its convenience, simplicity, and rapid response [4]. In contrast, the basal-bolus approach requires subcutaneous administration of basal insulin given once daily in combination with prandial and corrective dosages of rapid-acting insulin given before meals. The adoption of the three scales of insulin administration and seven scales of glucose level detection with a correction dosage is very challenging which limits the use by physicians [23]. To overcome inertia, many electronic instruments are designed to assist hospital-based insulin management by clinicians [24,25,26,27,28]. Compared to glucose-based basal-bolus correction regimens and electronic instruments assisting hospital-based insulin management [24,25,26,27,28], our algorithm was cost-effective, simple, and convenient to use.
The present study used glargine other than detemir or degludec. Though detemir was found in an observational study have similar inpatient glycemic control compared with glargine, it was associated with higher daily dose and number of injections [29]. Degludec was non-inferiority to glargine in hospitalized patients with T2D [30]. However, in some studies, due to its prolonged effect of more than 24 h, the quantity was adjusted every 2 days instead of once daily which may prolong the length of stay [31]. Short-acting insulin, though there is no head-to-head trial, glulisine, aspart and lispro had been widely studied as effective and safe using basal-bolus algorism in inpatients [13, 16, 19, 32, 33]. Faster aspart and faster lispro need evidence for inpatients.
Hypoglycemia is one of the main concerns during antidiabetic treatment, especially insulin treatment. Our hypoglycemia episode rate of 26.9% in the 1:1.5 group was similar to other basal-bolus randomized control trials which had 16.0–35.0% [13, 18, 33,34,35,36]. A clinical trial conducted in China using basal-bolus insulin also showed a similar hypoglycemia rate of 28.0% [36]. No severe hypoglycemia was found in this trial. In this regard, 1:1.5 basal-bolus insulin initiation and titration using a weight-based algorithm were safe for hospitalized patients with T2D.
Nevertheless, the present open-label study also had several limitations. First, all patients included in the study were on regular diets and had normal renal and liver functions. Therefore, whether the algorithm is applicable to patients with parenteral nutrition, and renal and liver dysfunction remains to be elucidated. Second, the subjects included in this study came from the same ethnic origin and the mean BMI values of these patients were relatively low (< 25 kg/m2). Third, most patients in this study had higher hyperglycemia on admission (mean HbA1c > 10%). Therefore, clinical trials with other populations and patients with relatively lower glycemic levels are required to determine the efficacy and safety in those groups using the new algorithm.
Conclusion
We demonstrated that fixed dose-ratio basal-bolus insulin at 1:1.5 calculated using a weight-based initiation and titration algorithm was simple, as effective, and safe as ratio at 1:1 in managing T2D in hospitalized patients.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an Independent marker of in-hospital mortality in patients with undiagnosed Diabetes. J Clin Endocrinol Metab. 2002;87(3):978–82. https://doi.org/10.1210/jcem.87.3.8341.
Umpierrez GE, Hellman R, Korytkowski MT, Kosiborod M, Maynard GA, Montori VM, et al. Management of hyperglycemia in hospitalized patients in non-critical care setting: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(1):16–38. https://doi.org/10.1210/jc.2011-2098.
American Diabetes Association. Economic costs of Diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033–46. https://doi.org/10.2337/dc12-2625.
Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman R, Hirsch IB, et al. American association of clinical endocrinologists; American diabetes association. American association of clinical endocrinologists and American diabetes association consensus statement on inpatient glycemic control. Diabetes Care. 2009;32(6):1119–31. https://doi.org/10.2337/dc09-9029.
Migdal AL, Fortin-Leung C, Pasquel F, Wang H, Peng L, Umpierrez GE. Inpatient glycemic control with sliding scale insulin in noncritical patients with type 2 Diabetes: who can slide? J Hosp Med. 2021;16(8):462–8. https://doi.org/10.12788/jhm.3654.
Sadhu AR, Patham B, Vadhariya A, Chikermane SG, Johnson ML. Outcomes of real-world insulin strategies in the management of hospital hyperglycemia. J Endocr Soc. 2021;5(8):bvab101. https://doi.org/10.1210/jendso/bvab101.
Umpierrez GE, Smiley D, Hermayer K, Khan A, Olson DE, Newton C, et al. Randomized Study comparing a basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 Diabetes. Diabetes Care. 2013;36(8):2169–74. https://doi.org/10.2337/dc12-1988.
Vellanki P, Bean R, Oyedokun FA, Pasquel FJ, Smiley D, Farrokhi F, et al. Randomized controlled trial of insulin supplementation for correction of bedtime hyperglycemia in hospitalized patients with type 2 Diabetes. Diabetes Care. 2015;38(4):568–74. https://doi.org/10.2337/dc14-1796.
Vellanki P, Cardona S, Galindo RJ, Urrutia MA, Pasquel FJ, Davis GM, et al. Efficacy and safety of intensive versus nonintensive supplemental insulin with a basal-bolus insulin regimen in hospitalized patients with type 2 Diabetes: a randomized clinical study. Diabetes Care. 2022;45(10):2217–23. https://doi.org/10.2337/dc21-1606.
Bellido V, Suarez L, Rodriguez MG, Sanchez C, Dieguez M, Riestra M, et al. Comparison of basal-bolus and premixed insulin regimens in hospitalized patients with type 2 Diabetes. Diabetes Care. 2015;38(12):2211–6. https://doi.org/10.2337/dc15-0160.
Pérez-Belmonte LM, Osuna-Sánchez J, Millán-Gómez M, López-Carmona MD, Gómez-Doblas JJ, Cobos-Palacios L, et al. Glycaemic efficacy and safety of linagliptin for the management of non-cardiac Surgery patients with type 2 Diabetes in a real-world setting: Lina-Surg study. Ann Med. 2019;51(3–4):252–61. https://doi.org/10.1080/07853890.2019.1613672.
Polonsky KS, Given BD, Van Cauter E. Twenty-four-hour profiles and pulsatile patterns of insulin secretion in normal and obese subjects. J Clin Invest. 1988;81(2):442–8. https://doi.org/10.1172/JCI113339.
Umpierrez GE, Smiley D, Zisman A, Prieto LM, Palacio A, Ceron M, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 Diabetes (RABBIT 2 trial). Diabetes Care. 2007;30(9):2181–6. https://doi.org/10.2337/dc07-0295.
Meyer C, Boron A, Plummer E, Voltchenok M, Vedda R. Glulisine versus human regular insulin in combination with glargine in noncritically ill hospitalized patients with type 2 Diabetes: a randomized double-blind study. Diabetes Care. 2010;33(12):2496–501. https://doi.org/10.2337/dc10-0957.
Pasquel FJ, Lansang MC, Khowaja A, Urrutia MA, Cardona S, Albury B, et al. A randomized controlled trial comparing glargine U300 and glargine U100 for the inpatient management of medicine and Surgery patients with type 2 Diabetes: glargine U300 hospital trial. Diabetes Care. 2020;43(6):1242–8. https://doi.org/10.2337/dc19-1940.
Zhang X, Zhang T, Xiang G, Wang W, Li Y, Du T, et al. Comparison of weight-based insulin titration (WIT) and glucose-based insulin titration using basal-bolus algorithm in hospitalized patients with type 2 Diabetes: a multicenter, randomized, clinical study. BMJ Open Diab Res Care. 2020;8(1):e001261. https://doi.org/10.1136/bmjdrc-2020-001261.
Liu L, Ke W, Wan X, Zhang P, Cao X, Deng W, et al. Insulin requirement profiles of short-term intensive insulin therapy in patients with newly diagnosed type 2 Diabetes and its association with long-term glycemic remission. Diabetes Res Clin Pract. 2015;108(2):250–7. https://doi.org/10.1016/j.diabres.2015.02.011.
Bueno E, Benitez A, Rufinelli JV, Figueredo R, Alsina S, Ojeda A, et al. BASAL-BOLUS regimen with insulin analogues versus human insulin in medical patients with type 2 Diabetes: a randomized controlled trial in Latin America. Endocr Pract. 2015;21(7):807–13. https://doi.org/10.4158/EP15675.OR.
Li X, Du T, Li W, Zhang T, Liu H, Xiong Y. Efficacy and safety of weight-based insulin glargine dose titration regimen compared with glucose level- and current dose-based regimens in hospitalized patients with type 2 Diabetes: a randomized, controlled study. Clin Ther. 2014;36(9):1269–75. https://doi.org/10.1016/j.clinthera.2014.06.032.
Heise T, Pieber TR, Danne T, Erichsen L, Haahr H. A pooled analysis of clinical pharmacology trials investigating the pharmacokinetic and pharmacodynamic characteristics of fast-acting insulin aspart in adults with type 1 Diabetes. Clin Pharmacokinet. 2017;56(5):551–9. https://doi.org/10.1007/s40262-017-0514-8.
Yang W, Liu J, Shan Z, Tian H, Zhou Z, Ji Q, et al. Acarbose compared with metformin as initial therapy in patients with newly diagnosed type 2 Diabetes: an open-label, non-inferiority randomised trial. Lancet Diabetes Endocrinol. 2014;2(1):46–55. https://doi.org/10.1016/S2213-8587(13)70021-4.
https://www.hopkinsmedicine.org/endocrinology_diabetes_metabolism/_documents/Total_Daily_Insulin_Dose_and_JHH_Formulary_Insulins.pdf (hopkinsmedicine.org). Accessed 29 Nov 2022.
Cook CB, Castro JC, Schmidt RE, Gauthier SM, Whitaker MD, Roust LR, et al. Diabetes care in hospitalized noncritically ill patients: more evidence for clinical inertia and negative therapeutic momentum. J Hosp Med. 2007;2(4):203–11. https://doi.org/10.1002/jhm.188.
Wexler DJ, Shrader P, Burns SM, Cagliero E. Effectiveness of a computerized insulin order template in general medical inpatients with type 2 Diabetes: a cluster randomized trial. Diabetes Care. 2010;33(10):2181–3. https://doi.org/10.2337/dc10-0964.
Helmle KE, Chacko S, Chan T, Drake A, Edwards AL, Moore GE, et al. Knowledge translation to optimize adult inpatient glycemic management with basal bolus insulin therapy and improve patient outcomes. Can J Diabetes. 2018;42(5):505–13. https://doi.org/10.1016/j.jcjd.2017.12.010.
Neubauer KM, Mader JK, Höll B, Aberer F, Donsa K, Augustin T, et al. Standardized glycemic management with a computerized workflow and decision support system for hospitalized patients with type 2 Diabetes on different wards. Diabetes Technol Ther. 2015;17(10):685–92. https://doi.org/10.1089/dia.2015.0027.
Mathioudakis N, Jeun R, Godwin G, Perschke A, Yalamanchi S, Everett E, et al. Development and implementation of a sbcutaneous insulin clinical decision support tool for hospitalized patients. J Diabetes Sci Technol. 2019;13(3):522–32. https://doi.org/10.1177/1932296818798036.
Toyoshima MTK, Brandes PHR, da Paz Lauterbach G, Moraes JRA, de Paiva EF, Umpierrez GE, et al. Insulin APP application protocol for the inpatient management of type 2 Diabetes on a hospitalist-managed ward: a retrospective study. Arch Endocrinol Metab. 2022;66(4):498–505. https://doi.org/10.20945/2359-3997000000496.
Galindo RJ, Davis GM, Fayfman M, Reyes-Umpierrez D, Alfa D, Peng L, et al. Comparison of efficacy and safety of glargine and detemir insulin in the management of inpatient hyperglycemia and diabetes. Endocr Pract. 2017;23(9):1059–66. https://doi.org/10.4158/EP171804.OR.].
Galindo RJ, Pasquel FJ, Vellanki P, Alicic R, Lam DW, Fayfman M, et al. Degludec hospital trial: a randomized controlled trial comparing insulin degludec U100 and glargine U100 for the inpatient management of patients with type 2 Diabetes. Diabetes Obes Metab. 2022;24(1):42–9. https://doi.org/10.1111/dom.14544.
Suzuki J, Yamakawa T, Oba M, Nagakura J, Shigematsu E, Tamura H, et al. Efficacy and safety of insulin degludec U100 and insulin glargine U100 in combination with meal-time bolus insulin in hospitalized patients with type 2 Diabetes: an open-label, randomized controlled study. Endocr J. 2019;66(11):971–82. https://doi.org/10.1507/endocrj.EJ18-0309.
Leahy JL. Insulin management of diabetic patients on general medical and surgical floors. Endocr Pract. 2006;12(Suppl 3):86–90. https://doi.org/10.4158/EP.12.S3.86.
Umpierrez GE, Smiley D, Jacobs S, Peng L, Temponi A, Mulligan P, et al. RAndomized study of basal Bolus insulin therapy in the inpatient management of patients with type 2 Diabetes undergoing general Surgery (RABBIT Surgery). Diabetes Care. 2011;34(2):256–61. https://doi.org/10.2337/dc10-1407.
Umpierrez GE, Smiley D, Hermayer K, Khan A, Olson DE, Newton C, et al. Randomized study comparing a basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 Diabetes: basal plus trial. Diabetes Care. 2013;36(8):2169–74. https://doi.org/10.2337/dc10-1407.
Vellanki P, Rasouli N, Baldwin D, Alexanian S, Anzola I, Urrutia M, et al. Glycaemic efficacy and safety of linagliptin compared to a basal-bolus insulin regimen in patients with type 2 diabetes undergoing non-cardiac surgery: a multicentre randomized clinical trial. Diabetes Obes Metab. 2019;21(4):837–43. https://doi.org/10.1111/dom.13587.
Weng J, Li Y, Xu W, Shi L, Zhang Q, Zhu D, et al. Effect of intensive insulin therapy on beta-cell function and glycaemic control in patients with newly diagnosed type 2 Diabetes: a multicentre randomised parallel-group trial. Lancet. 2008;371(9626):1753–60. https://doi.org/10.1016/S0140-6736(08)60762-X.
Funding
This work was supported by National Natural Science Foundation of China (Grants Number: 81800682 to Yanli Li), the Medical and Health Project of Guangzhou (Grants Number: 20201A011079 to Yanli Li), Guangzhou Science and Technology Project (Grants Number: 202201020550 to Yanli Li), and National Natural Science Foundation of China (Grants Number 81800726 to Xiaodan Zhang).
Author information
Authors and Affiliations
Contributions
WL and YL contributed to the study design and interpretation of data. YL prepared all figures. WL wrote the main manuscript text. All authors contributed to study protocol discussion, data collection, and reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics Committee of the Second Affiliated Hospital of Guangzhou Medical University. Informed consent was obtained from each participant.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, X., Yan, D., Du, T. et al. Efficacy and safety of basal-bolus insulin at 1:1.5 ratio compared to 1:1 ratio using a weight-based initiation and titration (WIT2) algorithm in hospitalized patients with type 2 Diabetes: a multicenter, randomized, clinical study. Diabetol Metab Syndr 15, 243 (2023). https://doi.org/10.1186/s13098-023-01193-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-023-01193-9