Abstract
Background
The characteristics of muscle degeneration in individual quadriceps in early knee osteoarthritis (OA) and the association of muscle quantity and quality on knee dysfunction remain unclear. This study aimed to clarify the characteristics of muscle degeneration in individual quadriceps muscles in early knee OA and elucidate the association of muscle volume and intramuscular adipose tissue (intraMAT) with knee dysfunction, including functional disabilities, symptoms, and joint morphology.
Methods
Fifty participants were categorized into early knee OA and healthy control groups. 3.0 T magnetic resonance imaging (MRI) using T1-weighted and Dixon methods and 3D SPACE in the thigh muscle and knee joint regions was performed. Quadriceps muscle volume, intraMAT, and whole-organ MRI score (WORMS) were assessed. The Knee Society Score (KSS) was used to evaluate functional disabilities and knee symptoms. Univariate analysis of variance was conducted with covariates to clarify the differences in muscle volume and intraMAT between the two groups. Multiple linear regression analyses were performed using the KSS function and symptom subcategories and WORMS as dependent variables and muscle volume, intraMAT, and the presence of early knee OA as independent variables, such as potential confounders.
Results
The quadriceps intraMAT, especially in the vastus medialis (VM), was significantly higher in patients with early knee OA than in healthy controls. The VM intraMAT, not muscle volume, was significantly associated with KSS function [B = − 3.47; 95% confidence interval [CI], − 5.24 to − 1.71; p < 0.001] and symptom scores [B = − 0.63; 95% CI, − 1.09 to − 0.17; p = 0.008], but not with WORMS.
Conclusion
These findings suggest that higher VM intraMAT is characteristic of quadriceps muscle degeneration in early knee OA and its increase is associated with functional disabilities and symptoms.
Similar content being viewed by others
Introduction
Knee osteoarthritis (OA) is one of the most common musculoskeletal disorders that worsen functional ability in older people. Early detection of knee OA pathology is important for preventing cartilage degeneration and worsening of symptoms. Since the definition of early-stage knee OA (early knee OA) was published in the 2010s [1, 2], clinical studies have used the classification criteria for early knee OA based on radiographic Kellgren-Lawrence (KL) grade 0–1 and clinical signs including poor function and pain. The development and progression of early knee OA by evaluating intra-articular lesions using magnetic resonance imaging (MRI) is an active area of research [3, 4]. A previous study [5] indicated that medial meniscal extrusion is a known risk factor for the progression of early knee OA, but the modifiable factors that could change with therapeutic intervention remain unclear. Recently, some studies [6,7,8] have suggested that intramuscular adipose tissue (intraMAT) infiltration into the quadriceps in patients with advanced knee OA is associated with muscle weakness and functional disabilities; thus, quantification of intraMAT has attracted attention for detecting knee OA pathology. As an increase in quadriceps intraMAT occurs earlier than loss of muscle quantity (i.e., muscle atrophy) in age-related changes [6, 9], assessment of intraMAT infiltration may also be useful in detecting early knee OA.
Chemical shift-based 2-point Dixon water-fat separation MRI techniques can be used for the quantification of intraMAT in localized regions [10, 11]. Dixon-MRI has high spatial resolution and is more advantageous for extracting intraMAT than T1-weighted methods, as measured by pixel intensity [12].
Only one study [6] has evaluated intraMAT in knee OA using the Dixon-MRI technique has been reported.
To the best of our knowledge, only one previous study [6], by Kumar et al., has evaluated intraMAT in knee OA using the Dixon-MRI technique. Their study [6] showed that intraMAT infiltration was significantly higher in the quadriceps of patients with knee OA than in healthy controls, whereas no significant difference was observed in other thigh muscles. Additionally, no difference between groups was observed in the anatomical cross-sectional area of all thigh muscles, implying that muscle atrophy in the quadriceps was not observed in knee OA [6]. Although these results are interesting, it is still unknown whether these changes occur in early knee OA and whether there are differences in these changes between the four individual quadriceps muscles.
Several previous studies [7, 13] have shown that a high intraMAT in the vastus medialis (VM) muscle is associated with the worsening of cartilage damage. Other previous studies [9, 14] evaluated intraMAT using B-mode ultrasound images and suggested that an increase in VM intraMAT was confirmed in knee OA patients, and higher fat content was associated with poor functional abilities and worsening symptoms. In summary, although the number of previous reports is limited, there is a close interaction between VM intraMAT and structural changes and functional disabilities in knee OA patients. Considering that an increase in intraMAT occurs earlier than muscle atrophy [9, 15], a higher VM intraMAT may characterize quadriceps muscle degeneration in early knee OA patients. However, to the best of our knowledge, no study has investigated both muscle volume and intraMAT of individual quadriceps muscles and clarified the relationship between muscle degeneration characteristics and knee dysfunction in early knee OA.
The present study aimed to determine (1) the characteristics of muscle degeneration in individual quadriceps in early knee OA and (2) the association of muscle volume and intraMAT on knee dysfunction, such as functional disabilities, symptoms, and joint morphology. We hypothesized that (1) the intraMAT in the VM muscle was increased in early knee OA patients compared to healthy controls, and (2) a higher VM intraMAT was associated with knee dysfunction.
Patients and methods
Study participants
A total of 52 older adults aged > 60 years (women, n = 23; mean age, 73.5 ± 6.6 years) residing in local communities in Kyoto and neighboring cities participated in this cross-sectional observational study. Before starting the study, the study procedures and aims were explained verbally, and all individuals provided written informed consent. The protocol was approved by the Ethics Committee of Kyoto University Graduate School and Faculty of Medicine (R1746).
The inclusion criteria were as follows: (1) no diagnosis of advanced knee OA (KL grade ≥ 2), (2) ability to walk without an assistive device, and (3) no general contraindications for MRI. The exclusion criteria were rheumatoid arthritis, knee osteonecrosis, neuromuscular disorders, history of lower-limb surgery, and cognitive impairment. Thereafter, according to the classification criteria, the participants were divided into early knee OA and healthy control groups. Early knee OA was defined as a KL grading scale of 1 or less, tenderness and/or stiffness around the knee, and symptomatic knee assessed using the Knee Society Score (KSS) symptom subcategory. The healthy control group included patients who did not meet the definition of early knee OA and those without knee symptoms.
MRI acquisition
MRI scans of the right knee joint and thigh muscle were obtained using a 3.0 T MRI scanner (MAGNETOM Verio; Siemens AG, Germany). After resting for more than 15 min in a relaxed supine position, MRIs of the whole knee joint were acquired with a sequence corresponding to 3D SPACE with proton-density variable contrast using a body matrix coil and spine coil. The parameters were set as follows: slice thickness, 0.7 mm; repetition time (TR), 1000 ms; echo time (TE), 35 ms; field of view, 150 mm × 150 mm; voxel size, 0.59 mm × 0.59 mm × 0.7 mm. Additionally, MRIs of the entire thigh were obtained from the pelvis to the right tibial tuberosity and divided into three parts with a body matrix coil and a spine coil. Multi-slice T1-weighted MRIs of the thigh muscles were performed with the following parameters: [16] slice thickness, 4 mm; TR, 2820 ms; TE, 16 ms; optimized field of view, 320 mm × 240 mm; flip angle, 129°; voxel size, 0.5 mm × 0.5 mm × 4.0 mm. Two-point Dixon images with a slice thickness of 3 mm were acquired using the following sequences [17]: TR, 4.33 ms; TE1, 1.31 ms; TE2, 2.54 ms; optimized field of view, 286.4 mm × 365 mm; flip angle, 9°. Based on the water/fat chemical shift difference and consequently on their phase difference in signal intensity, water and fat images were produced using the two-point Dixon sequence. IntraMAT was calculated based on the signal intensities using the following equation: IntraMAT (%) = mean signal intensity of fat × 100/(mean signal intensity of fat + mean signal intensity of water) [17].
Quantification of muscle volume and intraMAT
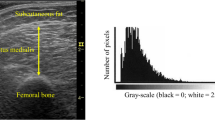
The region of interest (ROI) in individual quadriceps muscles was registered in T1-weighted and two-point Dixon images using Osirix MD (version 11.0; OsiriX, Geneva, Switzerland). To measure the muscle volume, the ROIs in the rectus femoris (RF), vastus intermedius (VI), vastus lateralis (VL), and VM were traced on each slice throughout the entire muscle length and measured as the muscle cross-sectional area (CSA, cm2). Then, the volume (cm3) of each slice was obtained by multiplying the muscle CSA by the slice thickness of 4 mm, and the muscle volume was calculated by summing the volume of each slice throughout the entire muscle length. The muscle volumes of the four individual quadriceps and total quadriceps were determined. IntraMAT was measured using two-point Dixon imaging. ROIs were carefully traced within the fascial borders of each muscle using a well-trained analyzer. The ROIs for RF, VI, and VL were constructed at the mid-thigh between the anterior superior iliac spine and the proximal end of the patella, and those for VM were at the distal 30% between the greater trochanter and the lateral femoral tuberosity. The intraMAT (%) was calculated from every 10 consecutive images with the measurement point mentioned above as the center, and the average value was obtained for the four individual quadriceps. The mean intraMAT of the quadriceps was determined as the average value of the four individual muscles.
Assessment of the Kellgren-Lawrence grading scale and knee OA joint morphology
After obtaining 3D SPACE MRIs of the right knee, one orthopedic surgeon judged the OA severity of the tibiofemoral joint and then confirmed the criteria for radiographic early knee OA. The KL grade based on knee MRIs was evaluated using a grading system with the Noyes classification, adding the status of osteophytes, bone marrow edema, and subchondral cyst, and it was strongly correlated with that of X-ray evaluation [18].
Knee joint morphology was assessed using the whole-organ magnetic resonance imaging score (WORMS), a semi-quantified scoring method based on knee imaging [19]. Five features of the articular surface, such as cartilage, subarticular bone marrow, bone cyst, subarticular bone attrition, and osteophyte, were scored by a well-trained examiner. Fifteen regions of the patella, femur, and tibia were assessed using the original WORMS. The total WORMS was obtained by adding the scores for each feature, and a higher WORMS indicated greater severity of morphological degeneration.
Self-reported knee function and symptom
Functional disabilities and symptoms were measured using the KSS 2011 Japanese edition, a self-administered assessment tool. The KSS comprises functional activities, symptoms, expectations, and satisfaction. This battery has demonstrated validity in the Japanese population, and two subcategories of functional activities and symptoms were used in the present study [20]. The KSS function score evaluates the activity status during daily living, such as standing, walking, and standard/advanced/discretionary activities. The maximum score on the KSS function was 100 points, and a higher score reflected better functional activities. Additionally, KSS symptoms, with a maximum score of 25 points, quantify knee stiffness and the degree of pain during walking and climbing stairs. Lower KSS symptoms indicate worsening knee pain, and a score of less than 23 is defined as a symptomatic knee [21].
Clinical features of physical function and amount of physical activity
Gait speed (m/s) during the participant’s comfortable walking measured the time it took to pass the gait way at a distance of 10 m and was converted to speed by dividing by the time taken. The chair stand-30 test measured the number of repetitions with sit-to-stand for 30 s as much as possible. The knee extension strength test was performed twice using an isometric dynamometer (Isoforce GT-330; OG GIKEN Co., Japan) with knee flexion of 60°, and the maximum value was obtained by converting into a ratio of torque to body weight (Nm/kg). The average number of steps per day for 14 days was measured as the amount of physical activity in daily life using a pedometer with a triaxial accelerometer (ES-500; YAMASA, Japan).
Statistical analysis
Continuous variables are shown as the mean ± standard deviation (SD), and categorical variables are presented as counts and percentages (n, %). Outcome measures and covariates were compared between the early knee OA and healthy control groups using an unpaired t-test or a chi-square test. Univariate analysis of variance (ANOVA) was conducted to clarify the differences in muscle volume and intraMAT between the early knee OA and healthy control groups. The adjusted mean differences between the two groups for each parameter were estimated by adjusting for age, sex, and body mass index (BMI). To determine the cut-off value of muscle degeneration parameters in early knee OA, receiver operating characteristic (ROC) curve analysis with the Youden index was conducted on the significant variable confirmed by group difference analysis. We performed three multiple linear regression analyses with the KSS function, symptoms, and WORMS as dependent variables. The regression analyses included quadriceps muscle volume, intraMAT, and the presence of early knee OA as independent variables, with adjustment variables for age, sex, and BMI. For secondary analyses, we also conducted another multiple linear regression as the independent variable with VM muscle volume and intraMAT to test our hypothesis. All statistical tests were performed using the SPSS software (version 25.0 for Windows, IBM Japan Inc., Japan). Statistical significance was set at p < 0.05.
Results
Besides two excluded participants with blurred MRIs (obvious artifacts in images) or missing clinical data, 50 participants were divided into the early knee OA (n = 19) and healthy control groups (n = 31). The demographic characteristics are shown in Table 1. KSS function and symptom scores in the early knee OA group were significantly lower than those in the healthy control group, while there was no significant difference in WORMS scores between groups. There were no significant differences in muscle volume and intraMAT between the two groups, except for the VM intraMAT, which was higher in early knee OA than in healthy controls. Physical function and amount of physical activity were also not significantly different between the two groups.
The characteristics of muscle degeneration in the early knee OA group
Based on the results of univariate ANOVA with adjustment for covariates (Table 2), we observed that quadriceps intraMAT, not muscle volume, was significantly higher in the early knee OA group than in the healthy control (adjusted mean difference, 1.0%; 95% confidence interval [CI], 0.1 to 1.9%; p = 0.035). Further, for individual quadriceps muscles, the VM intraMAT in the early knee OA group was significantly higher than that in the healthy control (adjusted mean difference, 2.2%; 95% CI, 1.2 to 3.3%; p < 0.001), while intraMAT of the RF, VI, and VL did not confirm group differences. The volume of all four muscles also showed no significant differences between the two groups. ROC curve analysis indicated that the optimal cut-off point of the VM intraMAT for detecting early knee OA was 7.2%. This model on VM intraMAT had moderate prediction accuracy, with an area under the curve of 0.80, sensitivity of 0.63, and specificity of 0.81.
Association of muscle volume and intraMAT on KSS function, symptom, and WORMS
Associations of quadriceps muscle volume, intraMAT, and the presence of early knee OA with KSS function, symptoms, and WORMS are presented in Table 3. In the multiple regression analysis, quadriceps intraMAT and the presence of early knee OA were selected as significant variables for the KSS function score. A 1% increase in quadriceps intraMAT was significantly associated with a 3.88-point reduction in the KSS function score (95% CI, 1.82 to 5.93 points, p < 0.001) after adjusting for covariates, but the muscle volume was not. In contrast, the presence of early knee OA, but not quadriceps muscle volume or intraMAT, was associated with the KSS symptom score. There were no significant variables associated with WORMS.
Table 4 presents the results of the secondary analyses which entered VM muscle volume, intraMAT, and the presence of early knee OA as the independent variables. VM intraMAT was selected as a significant variable for the KSS function score, whereas VM intraMAT and the presence of early knee OA were selected for the KSS symptom score. A higher VM intraMAT was significantly associated with KSS function (B = − 3.47; 95% CI, − 5.24 to − 1.71; p < 0.001) and symptoms (B = − 0.63; 95% CI, − 1.09 to − 0.17; p = 0.008). In the secondary analyses, there were no significant variables associated with WORMS.
Discussion
To the best of our knowledge, this study is the first to clarify the characteristics of muscle degeneration in early knee OA. In agreement with our hypothesis, quadriceps intraMAT, especially in the VM, was significantly higher in the early knee OA group than in healthy controls. Moreover, multiple regression analysis indicated that a higher quadriceps intraMAT was associated with worsening KSS function, partially supporting our hypothesis. Notably, this association was remarkably confirmed in VM intraMAT, and a higher VM intraMAT was associated with both functional disabilities and worse symptoms but not with joint morphology. These findings suggest that VM intraMAT is characteristic of quadriceps muscle degeneration in early knee OA and its increase is associated with functional disabilities and symptoms.
The current study found that the VM intraMAT increased even in early knee OA, and the ROC analysis showed a VM intraMAT of 7.2% for detecting early knee OA. Although the sensitivity was slightly low, specificity was high; thus, it was suggested that evaluation of the VM intraMAT among the four individual quadriceps muscles was useful for differentiating early knee OA. There is already evidence in advanced knee OA that intraMAT infiltration occurs prior to muscle atrophy in the quadriceps [6, 9, 22] and that the loss of muscle quality in the VM, such as higher intraMAT, characterizes quadriceps degeneration [8]. Some factors may contribute to the higher VM intraMAT. One factor is the mesenchymal progenitor cells, which are associated with ectopic adipogenesis of the VM in patients with advanced knee OA [23]. A previous study in mice showed that chronic inflammation within the muscles also promotes muscle degeneration [24]. The inflammatory cytokine IL-6 is amplified in patients with knee OA, and higher IL-6 levels are associated with worsened knee pain [25, 26]. Considering that patients with early knee OA have pain and slight knee degeneration, the aforementioned response may have arisen even in early knee OA. Additionally, the VM is a dynamic stabilizer of the knee and attaches closer to the painful site than to other quadriceps muscles [27, 28]. Therefore, biomechanical and anatomical factors and added biological factors are associated with a higher VM intraMAT. This mechanism is currently unknown; therefore, further studies are needed to elucidate why VM intraMAT increases in early knee OA.
An increase in VM intraMAT was associated with lower KSS function and symptoms, but not WORMS, in early knee OA. Although a higher VM intraMAT was reported to be one of the risk factors for cartilage damage in a longitudinal study [6], VM intraMAT was not related to WORMS in this study. This discrepancy could be due to differences in the severity of knee OA; previous studies [7, 13] included patients with advanced knee OA, but the current study targeted participants with early knee OA. The association of VM intraMAT with KSS function scores was consistent with a previous study in advanced knee OA [14]. Given that the minimum clinically significant difference in KSS function scores after total knee arthroplasty was 4.1 points [29], our findings that quadriceps 1% higher intraMAT was associated with a 3.88-point reduction in KSS functional score appear to be clinically significant. Notably, our findings suggested that VM intraMAT had a stronger relationship with KSS scores than quadriceps intraMAT. As the presence of early OA was not significant in the regression model using VM intraMAT, a higher VM intraMAT seemed to play a mediating role in the relationship between early knee OA and functional disabilities. Our results also showed that a higher VM intraMAT was associated with the worsening of KSS symptoms. Although it is known that an increase in intraMAT of the VM is associated with knee pain in advanced knee OA [14], the current study is the first to confirm similar associations in the pre-stage of knee OA development. As this study had a cross-sectional design, the causal relationship between knee symptoms and VM intraMAT infiltration in early knee OA could not be determined. As a clinical suggestion, it seems likely that VM intraMAT is meaningful for preventing functional disability and symptoms of knee osteoarthritis because, with muscle strength training, a higher intraMAT infiltration improves.
There are several limitations to this study. First, KL grade was converted based on the MRI grading system, such as the Noyes classification, to define early knee OA. Although the validity of this classification has been demonstrated, it may differ from the classification of early knee OA based on the anteroposterior weight-bearing X-ray view [18]. Second, the participants of this study were community-dwelling older adults. Thus, we assumed that our study participants were functionally better than individuals with early knee OA who visited an orthopedic clinic. No differences in WORMS or physical function were observed between the early knee OA and healthy control groups. Nonetheless, it is important to note that a higher intraMAT was identified in early knee OA.
Conclusions
The intraMAT of the quadriceps, especially the VM, was significantly increased in patients with early knee OA compared with that in healthy controls. Furthermore, higher VM intraMAT was associated with poor functional abilities and symptoms. Therefore, these findings suggest that higher VM intraMAT is characteristic of quadriceps muscle degeneration in early knee OA and its increase is associated with functional disabilities and symptoms.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available due to ethical restrictions but are available from the corresponding author upon reasonable request.
Abbreviations
- ANOVA:
-
Analysis of variance
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CSA:
-
Cross-sectional area
- IntraMAT:
-
Intramuscular adipose tissue
- KL:
-
Kellgren-Lawrence
- KSS:
-
Knee Scoring System
- MRI:
-
Magnetic resonance imaging
- OA:
-
Osteoarthritis
- RF:
-
Rectus femoris
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- TE:
-
Echo time
- TR:
-
Repetition time
- VI:
-
Vastus intermedius
- VL:
-
Vastus lateralis
- VM:
-
Vastus medialis
- WORMS:
-
Whole-organ magnetic resonance imaging score
References
Luyten FP, Denti M, Filardo G, Kon E, Engebretsen L. Definition and classification of early osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):401–6. https://doi.org/10.1007/s00167-011-1743-2.
Luyten FP, Bierma-Zeinstra S, Dell’Accio F, Kraus VB, Nakata K, Sekiya I, Arden NK, et al. Toward classification criteria for early osteoarthritis of the knee. Semin Arthritis Rheum. 2018;47(4):457–63. https://doi.org/10.1016/j.semarthrit.2017.08.006.
Hada S, Kaneko H, Sadatsuki R, Liu L, Futami I, Kinoshita M, Yusup A, et al. The degeneration and destruction of femoral articular cartilage shows a greater degree of deterioration than that of the tibial and patellar articular cartilage in early stage knee osteoarthritis: a cross-sectional study. Osteoarthritis Cartilage. 2014;22(10):1583–9. https://doi.org/10.1016/j.joca.2014.07.021.
Tsai PH, Wong CC, Chan WP, Lu TW. The value of MR T2* measurements in normal and osteoarthritic knee cartilage: effects of age, sex, and location. Eur Radiol. 2019;29(8):4514–22. https://doi.org/10.1007/s00330-018-5826-z.
Liu Y, Joseph GB, Foreman SC, Li X, Lane NE, Nevitt MC, McCulloch CE, et al. Determining a threshold of medial meniscal extrusion for prediction of knee pain and cartilage damage progression over 4 years: data from the osteoarthritis initiative. AJR Am J Roentgenol. 2021;216(5):1318–28. https://doi.org/10.2214/AJR.20.23864.
Kumar D, Karampinos DC, Macleod TD, Lin W, Nardo L, Li X, Link TM, et al. Quadriceps intramuscular fat fraction rather than muscle size is associated with knee osteoarthritis. Osteoarthritis Cartilage. 2014;22(2):226–34. https://doi.org/10.1016/j.joca.2013.12.005.
Raynauld JP, Pelletier JP, Roubille C, Dorais M, Abram F, Li W, Wang Y, et al. Magnetic resonance imaging-assessed vastus medialis muscle fat content and risk for knee osteoarthritis progression: relevance from a clinical trial. Arthritis Care Res (Hoboken). 2015;67(10):1406–15. https://doi.org/10.1002/acr.22590.
Taniguchi M, Fukumoto Y, Yagi M, Yamagata M, Kobayashi M, Yamada Y, Kimura M, et al. Enhanced echo intensity and a higher extracellular water-to-intracellular water ratio are helpful clinical signs for detecting muscle degeneration in patients with knee osteoarthritis. Clin Rheumatol. 2021;40(10):4207–15. https://doi.org/10.1007/s10067-021-05763-y.
Taniguchi M, Fukumoto Y, Kobayashi M, Kawasaki T, Maegawa S, Ibuki S, Ichihashi N. Quantity and quality of the lower extremity muscles in women with knee osteoarthritis. Ultrasound Med Biol. 2015;41(10):2567–74. https://doi.org/10.1016/j.ultrasmedbio.2015.05.014.
Azzabou N, Hogrel JY, Carlier PG. NMR based biomarkers to study age-related changes in the human quadriceps. Exp Gerontol. 2015;70:54–60. https://doi.org/10.1016/j.exger.2015.06.015.
Hogrel JY, Barnouin Y, Azzabou N, Butler-Browne G, Voit T, Moraux A, Leroux G, et al. NMR imaging estimates of muscle volume and intramuscular fat infiltration in the thigh: variations with muscle, gender, and age. Age. 2015;37(3):9798. https://doi.org/10.1007/s11357-015-9798-5.
Schick F, Machann J, Brechtel K, Strempfer A, Klumpp B, Stein DT, Jacob S. MRI of muscular fat. Magn Reson Med. 2002;47(4):720–7. https://doi.org/10.1002/mrm.10107.
Kumar D, Link TM, Jafarzadeh SR, LaValley MP, Majumdar S, Souza RB. Association of quadriceps adiposity with an increase in knee cartilage, meniscus, or bone marrow lesions over three years. Arthritis Care Res (Hoboken). 2021;73(8):1134–9. https://doi.org/10.1002/acr.24232.
Taniguchi M, Fukumoto Y, Yagi M, Motomura Y, Okada S, Okada S, Kobayashi M, et al. Enhanced echo intensity in vastus medialis is associated with worsening of functional disabilities and symptoms in patients with knee osteoarthritis: a 3 years longitudinal study. Rheumatol Int. 2022. https://doi.org/10.1007/s00296-022-05246-6.
Fukumoto Y, Ikezoe T, Yamada Y, Tsukagoshi R, Nakamura M, Takagi Y, Kimura M, et al. Age-related ultrasound changes in muscle quantity and quality in women. Ultrasound Med Biol. 2015;41(11):3013–7. https://doi.org/10.1016/j.ultrasmedbio.2015.06.017.
Yagi M, Taniguchi M, Tateuchi H, Hirono T, Fukumoto Y, Yamagata M, Nakai R, et al. Age- and sex-related differences of muscle cross-sectional area in iliocapsularis: a cross-sectional study. BMC Geriatr. 2022;22(1):435. https://doi.org/10.1186/s12877-022-03127-y.
Fukumoto Y, Taniguchi M, Hirono T, Yagi M, Yamagata M, Nakai R, Asai T, et al. Influence of ultrasound focus depth on the association between echo intensity and intramuscular adipose tissue. Muscle Nerve. 2022;66(5):568–75. https://doi.org/10.1002/mus.27677.
Park HJ, Kim SS, Lee SY, Park NH, Park JY, Choi YJ, Jeon HJ. A practical MRI grading system for osteoarthritis of the knee: association with Kellgren-Lawrence radiographic scores. Eur J Radiol. 2013;82(1):112–7. https://doi.org/10.1016/j.ejrad.2012.02.023.
Peterfy CG, Guermazi A, Zaim S, Tirman PF, Miaux Y, White D, Kothari M, et al. Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004;12(3):177–90. https://doi.org/10.1016/j.joca.2003.11.003.
Taniguchi N, Matsuda S, Kawaguchi T, Tabara Y, Ikezoe T, Tsuboyama T, Ichihashi N, et al. The KSS 2011 reflects symptoms, physical activities, and radiographic grades in a Japanese population. Clin Orthop Relat Res. 2015;473(1):70–5. https://doi.org/10.1007/s11999-014-3650-6.
Taniguchi M, Ikezoe T, Kamitani T, Tsuboyama T, Ito H, Matsuda S, Tabara Y, et al. Extracellular-to-intracellular water ratios are associated with functional disability levels in patients with knee osteoarthritis: results from the Nagahama Study. Clin Rheumatol. 2021;40(7):2889–96. https://doi.org/10.1007/s10067-021-05591-0.
Teoli A, Martel-Pelletier J, Abram F, Pelletier JP, Robbins SM. Vastus medialis intramuscular fat is associated with reduced quadriceps strength, but not knee osteoarthritis severity. Clin Biomech (Bristol, Avon). 2022;96:105669. https://doi.org/10.1016/j.clinbiomech.2022.105669.
Ikemoto-Uezumi M, Matsui Y, Hasegawa M, Fujita R, Kanayama Y, Uezumi A, Watanabe T, et al. Disuse atrophy accompanied by intramuscular ectopic adipogenesis in vastus medialis muscle of advanced osteoarthritis patients. Am J Pathol. 2017;187(12):2674–85. https://doi.org/10.1016/j.ajpath.2017.08.009.
Saito Y, Chikenji TS, Matsumura T, Nakano M, Fujimiya M. Exercise enhances skeletal muscle regeneration by promoting senescence in fibro-adipogenic progenitors. Nat Commun. 2020;11(1):889. https://doi.org/10.1038/s41467-020-14734-x.
Levinger I, Levinger P, Trenerry MK, Feller JA, Bartlett JR, Bergman N, McKenna MJ, et al. Increased inflammatory cytokine expression in the vastus lateralis of patients with knee osteoarthritis. Arthritis Rheum. 2011;63(5):1343–8. https://doi.org/10.1002/art.30287.
Shimura Y, Kurosawa H, Sugawara Y, Tsuchiya M, Sawa M, Kaneko H, Futami I, et al. The factors associated with pain severity in patients with knee osteoarthritis vary according to the radiographic disease severity: a cross-sectional study. Osteoarthritis Cartilage. 2013;21(9):1179–84. https://doi.org/10.1016/j.joca.2013.05.014.
Hoy MG, Zajac FE, Gordon ME. A musculoskeletal model of the human lower extremity: the effect of muscle, tendon, and moment arm on the moment-angle relationship of musculotendon actuators at the hip, knee, and ankle. J Biomech. 1990;23(2):157–69. https://doi.org/10.1016/0021-9290(90)90349-8.
Waligora AC, Johanson NA, Hirsch BE. Clinical anatomy of the quadriceps femoris and extensor apparatus of the knee. Clin Orthop Relat Res. 2009;467(12):3297–306. https://doi.org/10.1007/s11999-009-1052-y.
Nishitani K, Yamamoto Y, Furu M, Kuriyama S, Nakamura S, Ito H, Fukuhara S, et al. The minimum clinically important difference for the Japanese version of the new Knee Society Score (2011KSS) after total knee arthroplasty. J Orthop Sci. 2019;24(6):1053–7. https://doi.org/10.1016/j.jos.2019.09.001.
Acknowledgements
We would like to thank Editage (www.editage.jp) for English language editing.
Funding
This study was supported by JSPS KAKENHI Grant-in-Aid for Scientific Research (18H03164 and 20K19376). This grant was used for data collection, data analysis, and manuscript writing.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the conception and design of the study. MT measured, analyzed, interpreted the data, and wrote the manuscript. YF, MaY, and NI measured, analyzed, interpreted the data, and revised the manuscript. TH, MoY, AA, SO, and RN measured and analyzed. MK was responsible for diagnosis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All study procedures were approved by the Ethics Committee of the Kyoto University Graduate School of Medicine and conducted in accordance with the principles of the Declaration of Helsinki (protocol identification number R1746). All patients were informed of the aim and procedures of the study, and all the patients provided written informed consent before participation.
Consent for publication
Written informed consent was obtained from all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Taniguchi, M., Fukumoto, Y., Yagi, M. et al. A higher intramuscular fat in vastus medialis is associated with functional disabilities and symptoms in early stage of knee osteoarthritis: a case–control study. Arthritis Res Ther 25, 61 (2023). https://doi.org/10.1186/s13075-023-03048-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-023-03048-0