Abstract
Introduction/objectives
To test the hypothesis that greater extracellular-to-intracellular water (ECW/ICW) ratios in lower-limb muscles are associated with worsened functional abilities in patients with knee osteoarthritis (OA).
Methods
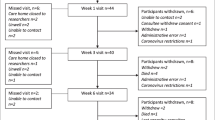
We analyzed data from 787 participants (82.2% female; mean age, 69.6 ± 5.3 years) from the Nagahama Prospective Cohort who were ≥60 years old and had radiographically confirmed bilateral knee OA. The Knee Scoring System (KSS) was used to assess functional abilities. Lower-limb ECW/ICW ratios and skeletal mass index values were determined with multi-frequency bioelectrical impedance analysis (BIA). Multiple linear regression analysis was used to test for associations between ECW/ICW ratios and functional abilities. Subgroup analyses based on OA severities and symptomaticity were also conducted.
Results
Increased ECW/ICW ratios were associated with a 4.38-point decrease in the KSS function scores (95% confidence interval [CI], 3.15–5.62 points) after adjusting for covariates. This association varied according to the degree of knee symptoms, especially in individuals with radiologically mild OA. ECW/ICW ratios in individuals with asymptomatic mild OA were associated with a 2.14-point decrease in the KSS function score (95% CI, 0.32–3.96 points), whereas those in individuals with severe symptomatic mild OA were associated with a 6.16-point decrease (95% CI, 2.13–10.19 points).
Conclusions
Our findings indicate that higher ECW/ICW ratios are associated with greater functional disability in patients with knee OA. Therefore, ECW/ICW ratio measurements with multi-frequency BIA can serve as valuable indicators for functional disability in patients with knee OA.
Key Points • Higher extracellular-to-intracellular water (ECW/ICW) ratios are associated with greater functional disability levels in patients with knee osteoarthritis (OA). • ECW/ICW ratios are useful clinical signs as a biomarker for poor functional abilities in patients with knee OA. |

Similar content being viewed by others
Data availability
Data not available due to ethical restrictions
References
Oiestad BE, Juhl CB, Eitzen I, Thorlund JB (2015) Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthritis Cartilage 23:171–177. https://doi.org/10.1016/j.joca.2014.10.008
Ruhdorfer A, Wirth W, Eckstein F (2015) Relationship between isometric thigh muscle strength and minimum clinically important differences in knee function in osteoarthritis: data from the osteoarthritis initiative. Arthritis Care Res 67:509–518. https://doi.org/10.1002/acr.22488
Wada O, Kurita N, Kamitani T, Nakano N, Mizuno K (2018) Influence of the severity of knee osteoarthritis on the association between leg muscle mass and quadriceps strength: the SPSS-OK study. Clin Rheumatol 38:719–725. https://doi.org/10.1007/s10067-018-4337-2
Gur H, Cakin N (2003) Muscle mass, isokinetic torque, and functional capacity in women with osteoarthritis of the knee. Arch Phys Med Rehabil 84:1534–1541. https://doi.org/10.1016/s0003-9993(03)00288-0
Delmonico MJ, Harris TB, Visser M, Park SW, Conroy MB, Velasquez-Mieyer P, Boudreau R, Manini TM, Nevitt M, Newman AB, Goodpaster BH, Health A, Body (2009) Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr 90:1579–1585. https://doi.org/10.3945/ajcn.2009.28047
Pedroso MG, de Almeida AC, Aily JB, de Noronha M, Mattiello SM (2019) Fatty infiltration in the thigh muscles in knee osteoarthritis: a systematic review and meta-analysis. Rheumatol Int. 39:627–635. https://doi.org/10.1007/s00296-019-04271-2
Kumar D, Karampinos DC, Macleod TD, Lin W, Nardo L, Li X, Link TM, Majumdar S, Souza RB (2014) Quadriceps intramuscular fat fraction rather than muscle size is associated with knee osteoarthritis. Osteoarthritis Cartilage 22:226–234. https://doi.org/10.1016/j.joca.2013.12.005
Raynauld JP, Pelletier JP, Roubille C, Dorais M, Abram F, Li W, Wang Y, Fairley J, Cicuttini FM, Martel-Pelletier J (2015) Magnetic resonance imaging-assessed vastus medialis muscle fat content and risk for knee osteoarthritis progression: relevance from a clinical trial. Arthritis Care Res 67:1406–1415. https://doi.org/10.1002/acr.22590
Dannhauer T, Ruhdorfer A, Wirth W, Eckstein F (2015) Quantitative relationship of thigh adipose tissue with pain, radiographic status, and progression of knee osteoarthritis: longitudinal findings from the osteoarthritis initiative. Invest Radiol 50:268–274. https://doi.org/10.1097/RLI.0000000000000113
Segal KR, Burastero S, Chun A, Coronel P, Pierson RN Jr, Wang J (1991) Estimation of extracellular and total body water by multiple-frequency bioelectrical-impedance measurement. Am J Clin Nutr 54:26–29. https://doi.org/10.1093/ajcn/54.1.26
Gudivaka R, Schoeller DA, Kushner RF, Bolt MJ (1999)Single- and multifrequency models for bioelectrical impedance analysis of body water compartments. J Appl Physiol 87:1087–1096. https://doi.org/10.1152/jappl.1999.87.3.1087
Mingrone G, Bertuzzi A, Capristo E, Greco AV, Manco M, Pietrobelli A, Salinari S, Heymsfield SB (2001) Unreliable use of standard muscle hydration value in obesity. Am J Physiol Endocrinol Metab 280:E365–E371. https://doi.org/10.1152/ajpendo.2001.280.2.E365
Yamada Y, Buehring B, Krueger D, Anderson RM, Schoeller DA, Binkley N (2017) Electrical properties assessed by bioelectrical impedance spectroscopy as biomarkers of age-related loss of skeletal muscle quantity and quality. J Gerontol A Biol Sci Med Sci 72:1180–1186. https://doi.org/10.1093/gerona/glw225
Lee S, Kim TN, Kim SH (2012) Sarcopenic obesity is more closely associated with knee osteoarthritis than is non-sarcopenic obesity: a cross-sectional study. Arthritis Rheum 64:3947–3954. https://doi.org/10.1002/art.37696
Taniguchi N, Matsuda S, Kawaguchi T, Tabara Y, Ikezoe T, Tsuboyama T, Ichihashi N, Nakayama T, Matsuda F, Ito H (2015) The KSS 2011 reflects symptoms, physical activities, and radiographic grades in a Japanese Population. Clin Orthop Relat Res 473:70–75. https://doi.org/10.1007/s11999-014-3650-6
Schoeller DA (2000) Bioelectrical impedance analysis. What does it measure? Ann N Y Acad Sci 904:159–162. https://doi.org/10.1111/j.1749-6632.2000.tb06441.x
Yamada Y, Ikenaga M, Takeda N, Morimura K, Miyoshi N, Kiyonaga A, Kimura M, Higaki Y, Tanaka H, Nakagawa S (2014) Estimation of thigh muscle cross-sectional area by single- and multifrequency segmental bioelectrical impedance analysis in the elderly. J Appl Physiol 116:176–182. https://doi.org/10.1152/japplphysiol.00772.2013
Janssen I, Baumgartner RN, Ross R, Rosenberg IH, Roubenoff R (2004) Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. Am J Epidemiol 159:413–421. https://doi.org/10.1093/aje/kwh058
Misra D, Fielding RA, Felson DT, Niu J, Brown C, Nevitt M, Lewis CE, Torner J, Neogi T, study M (2019) Risk of knee osteoarthritis with obesity, sarcopenic obesity, and sarcopenia. Arthritis Rheum 71:232–237. https://doi.org/10.1002/art.40692
Visser AW, de Mutsert R, Loef M, le Cessie S, den Heijer M, Bloem JL, Reijnierse M, Rosendaal FR, Kloppenburg M, NEO Study Group (2014) The role of fat mass and skeletal muscle mass in knee osteoarthritis is different for men and women: the NEO study. Osteoarthritis Cartilage 22:197–202. https://doi.org/10.1016/j.joca.2013.12.002
Conde J, Gomez R, Bianco G, Scotece M, Lear P, Dieguez C, Gomez-Reino J, Lago F, Gualillo O (2011) Expanding the adipokine network in cartilage: identification and regulation of novel factors in human and murine chondrocytes. Ann Rheum Dis 70:551–559. https://doi.org/10.1136/ard.2010.132399
Harding GT, Hubley-Kozey CL, Dunbar MJ, Stanish WD, Astephen Wilson JL (2012) Body mass index affects knee joint mechanics during gait differently with and without moderate knee osteoarthritis. Osteoarthritis Cartilage 20:1234–1242. https://doi.org/10.1016/j.joca.2012.08.004
Le Graverand MP, Brandt K, Mazzuca SA, Raunig D, Vignon E (2009) Progressive increase in body mass index is not associated with a progressive increase in joint space narrowing in obese women with osteoarthritis of the knee. Ann Rheum Dis 68:1734–1738. https://doi.org/10.1136/ard.2007.085530
Batsis JA, Zbehlik AJ, Barre LK, Bynum JP, Pidgeon D, Bartels SJ (2015) Impact of obesity on disability, function, and physical activity: data from the Osteoarthritis Initiative. Scand J Rheumatol 44:495–502. https://doi.org/10.3109/03009742.2015.1021376
Jeanmaire C, Mazieres B, Verrouil E, Bernard L, Guillemin F, Rat AC (2018) Body composition and clinical symptoms in patients with hip or knee osteoarthritis: results from the KHOALA cohort. Semin Arthritis Rheum 47:797–804. https://doi.org/10.1016/j.semarthrit.2017.10.012
Levinger I, Levinger P, Trenerry MK, Feller JA, Bartlett JR, Bergman N, McKenna MJ, Cameron-Smith D (2011) Increased inflammatory cytokine expression in the vastus lateralis of patients with knee osteoarthritis. Arthritis Rheum 63:1343–1348. https://doi.org/10.1002/art.30287
Ikemoto-Uezumi M, Matsui Y, Hasegawa M, Fujita R, Kanayama Y, Uezumi A, Watanabe T, Harada A, Poole AR, Hashimoto N (2017) Disuse atrophy accompanied by intramuscular ectopic adipogenesis in vastus medialis muscle of advanced osteoarthritis patients. Am J Pathol 187:2674–2685. https://doi.org/10.1016/j.ajpath.2017.08.009
Yamada Y, Yoshida T, Yokoyama K, Watanabe Y, Miyake M, Yamagata E, Yamada M, Kimura M, Kyoto-Kameoka Study (2016) The extracellular to intracellular water ratio in upper legs is negatively associated with skeletal muscle strength and gait speed in older people. J Gerontol A Biol Sci Med Sci 72:293–298. https://doi.org/10.1093/gerona/glw125
Lee I, Cho J, Jin Y, Ha C, Kim T, Kang H (2016) Body fat and physical activity modulate the association between sarcopenia and osteoporosis in elderly Korean women. J Sports Sci Med 15:477–482
Malavolti M, Mussi C, Poli M, Fantuzzi AL, Salvioli G, Battistini N, Bedogni G (2003)Cross-calibration of eight-polar bioelectrical impedance analysis versus dual-energy X-ray absorptiometry for the assessment of total and appendicular body composition in healthy subjects aged 21-82 years. Ann Hum Biol 30:380–391. https://doi.org/10.1080/0301446031000095211
Yamada Y, Schoeller DA, Nakamura E, Morimoto T, Kimura M, Oda S (2010) Extracellular water may mask actual muscle atrophy during aging. J Gerontol A Biol Sci Med Sci 65:510–516. https://doi.org/10.1093/gerona/glq001
Yamada Y, Matsuda K, Bjorkman MP, Kimura M (2014) Application of segmental bioelectrical impedance spectroscopy to the assessment of skeletal muscle cell mass in elderly men. Geriatr Gerontol Int 14:129–134. https://doi.org/10.1111/ggi.12212
Taniguchi M, Yamada Y, Fukumoto Y, Sawano S, Minami S, Ikezoe T, Watanabe Y, Kimura M, Ichihashi N (2017) Increase in echo intensity and extracellular-to-intracellular water ratio is independently associated with muscle weakness in elderly women. Eur J Appl Physiol 117:2001–2007. https://doi.org/10.1007/s00421-017-3686-x
Acknowledgements
We are extremely grateful to the Nagahama City Office and a non-profit organization called the Zeroji Club for their help in conducting the Nagahama Study. We would like to thank Editage (www.editage.cn) for English language editing.
Funding
The work was supported by a university grant, the Center of Innovation Program, the Global University Project, and a Grant-in-Aid for Scientific Research (25293141, 26670313, 26293198, 17H04182, 17H04126, 17H04123, 18K18450, and 19K17634) from the Ministry of Education, Culture, Sports, Science and Technology of Japan; the Practical Research Project for Rare/Intractable Diseases (ek0109070, ek0109070, ek0109196, and ek0109348), the Comprehensive Research on Aging and Health Science Research Grants for Dementia R&D (dk0207006, dk0207027), the Program for an Integrated Database of Clinical and Genomic Information (kk0205008), the Practical Research Project for Lifestyle-related Diseases including Cardiovascular Diseases and Diabetes Mellitus (17ek0210066, 18ek0210096, and 19ek0210116), and the Research Program for Health Behavior Modification by Utilizing IoT (le0110005, le0110013) from the Japan Agency for Medical Research and Development (AMED); the Takeda Medical Research Foundation, the Mitsubishi Foundation, the Daiwa Securities Health Foundation, and the Sumitomo Foundation; the Comprehensive Research on Aging and Health Science Research Grants for Dementia R&D from Japan Agency for Medical Research and Development (H26-Choju-Ippan-001, 15dk0107007h0003, 16dk0110007h0003); and the JSPS KAKENHI Grant-in-Aid for Research Activity Start-up (19K21493).
Author information
Authors and Affiliations
Consortia
Contributions
All authors have made substantial contributions to (1) the conception and design of the study, (2) revising it critically for important intellectual content, and (3) final approval of the version to be submitted. The specific contributions of each author are as follows:
1. Analysis and interpretation of the data: MT, TI, TK, and NI.
2. Drafting of the article: MT, TI, TK, and NI.
3. Statistical expertise: MT and TK.
Corresponding author
Ethics declarations
Code availability
Not applicable
Disclosures
None.
Ethics approval consent to participate
All study procedures were approved by the Ethics Committee of the Kyoto University Graduate School of Medicine and the Nagahama Municipal Review Board (G278) and were conducted in accordance with the principles of the Declaration of Helsinki.Written informed consent for the use of data was obtained from all participants in the Nagahama Study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 19.5 kb)
Rights and permissions
About this article
Cite this article
Taniguchi, M., Ikezoe, T., Kamitani, T. et al. Extracellular-to-intracellular water ratios are associated with functional disability levels in patients with knee osteoarthritis: results from the Nagahama Study. Clin Rheumatol 40, 2889–2896 (2021). https://doi.org/10.1007/s10067-021-05591-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-05591-0