Abstract
Objective
To describe the disease course of patients with early arthritis without rheumatoid factor (RF) and anti-citrullinated protein auto-antibodies (ACPA) in an inception cohort. To determine baseline predictors of fulfilling 2010 ACR/EULAR criteria for rheumatoid arthritis (RA) for these patients within 3 years.
Method
Patients included in the multicenter ESPOIR cohort were compared at baseline and 3 years by whether they were negative for RF and ACPA (“seronegative”) or positive for RF and/or ACPA (“seropositive”). Univariate analysis was used to determine the association between baseline variables in seronegative patients and RA classification. Stepwise multiple logistic regression was used to identify predictors of RA classification within 3 years, estimating odds ratios (ORs).
Results
Among 354 seronegative patients, 224/340 with available data (65.9%) fulfilled RA classification at baseline and 189/233 (81.1%) at 3 years. As compared with seropositive patients, seronegative patients had lower DAS28 (p = 0.002) and lower modified total Sharp score (mTSS; p = 0.026) at baseline; DAS28 remission was similar (p = 0.634), but radiographic progression rate was lower in seronegative patients (p < 0.001) at 3 years. In seronegative patients, factors predicting RA classification within 3 years were additive (OR = 3.61), bilateral (OR = 2.59) and hand, wrist or forefeet involvement (OR = 3.87); presence of a trigger event (OR = 3.57); pain at rest (OR = 2.76); morning stiffness (OR = 2.62); number of tender joints (OR = 23.73); and mTSS (OR = 2.56).
Conclusion
“Seronegative” patients have less active disease at baseline and less radiographic progression during follow-up than “seropositive” patients. With inflammatory pain, symmetric involvement of numerous small joints and erosive disease, a classification of RA is likely.
Similar content being viewed by others
Background
Diagnosing rheumatoid arthritis (RA) at an early stage remains a challenge for clinicians. Indeed, no test is sufficiently specific to identify RA with certainty. The diagnosis is based on a spectrum of clinical, biological, and radiographic features, although the latter, despite a high specificity when typical erosions are observed, are rarely present at an early stage of the disease. Thus, testing for auto-antibodies such as rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPA) is useful to diagnose RA among patients with early arthritis [1].
ACPA such as anti-cyclic-citrullinated peptide (anti-CCP) antibodies are highly specific to RA [2, 3], have good predictive validity for RA in patients with early arthritis [4], and are associated with radiographic progression in early RA [5, 6]. Although RF is considered less specific [3], it is also associated with worst radiographic outcome [7, 8]. ACPA and RF have the same weight in the 2010 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) classification criteria for RA [9] and have a major impact in the diagnosis and prognosis of RA. In clinical practice, the decision to start a disease-modifying anti-rheumatic drug (DMARD) is more difficult in the absence of RF and ACPA [10] since these auto-antibodies are important features both for diagnosis and for risk of persistency and erosiveness. Nevertheless, 20 to 30% of RA patients do not have ACPA [2] or RF, and erosive RA may exist without these two auto-antibodies.
Distinct genetic risk factors are associated with ACPA-positive or ACPA-negative disease. Anti-CCP–positive RA was found associated with HLA-DRB1, HLA-DP, PTPN22, C5-TRAF1, and TNFAIP3-OLIG3 polymorphisms [11,12,13], whereas anti-CCP–negative RA was found associated with genes such as HLA-DR3 and IRF-5 [13, 14], two genes that are also associated with systemic lupus erythematosus and Sjögren syndrome. These data might indicate distinct pathogenic mechanisms underlying ACPA-positive and ACPA-negative RA, with the last entity not well defined. Whether ACPA-negative RA features auto-antibodies binding to other citrullinated proteins (vimentin etc.) not detected in routine care or whether it is true RA without auto-antibodies is unknown. Because the clinical presentation of early arthritis is not specific, we do not know whether RA without ACPA or RF is “true” RA or another undifferentiated inflammatory arthritis. The literature contains few data specifically regarding the follow-up of “seronegative” early arthritis (i.e., negative for RF and ACPA).
The objectives of this study were first to describe the disease course of patients without RF and ACPA in an inception cohort of early inflammatory arthritis patients and second to determine baseline predictors of fulfilling 2010 ACR/EULAR criteria for RA within 3 years in these patients.
Patients and methods
Study population
The ESPOIR cohort included 813 patients with early arthritis from 14 French rheumatology centers between 2002 and 2005 [15]. Patients were eligible if they had a definitive or probable clinical diagnosis of RA or polyarthritis not better explained by another etiology; had two or more swollen joints for more than 6 weeks and less than 6 months; and did not receive DMARDs or steroids for more than 2 weeks, and if administered, steroids were stopped at least 2 weeks before inclusion. We excluded patients with a definite diagnosis different from RA. Patients were evaluated every 6 months for 2 years and then once a year and were cared for as routine by their rheumatologist. The protocol of the ESPOIR cohort was approved by the ethics committee of Montpellier, France (no. 020307, CNIL 02-1293), and all patients gave their signed informed consent before inclusion.
Auto-antibodies
Patients were tested for RF and anti-CCP antibodies. Anti-CCP antibodies were analyzed by Elecsys assay (Roche Diagnostics, Switzerland), with titers > 17 U/ml considered positive. IgM-RF was analyzed by using an ELISA kit (Ménarini, France), with titers > 9 IU/ml considered positive. The analyses of RF and anti-CCP status were centralized and performed in the Department of Immunology, Bichat University Hospital, Paris.
Baseline assessment
The following data were collected at baseline and at each visit: demographic data, comorbidities, current tobacco use, current alcohol consumption, family history of RA, duration of symptoms at first visit (defined by the date of the first fixed swollen joint), presence of a trigger event (death of a relative/loved one, trauma, vaccination, hormonal medication, delivery), clinical features of arthritis (duration of morning stiffness, pain at rest and on mobility on a 0–100 mm visual analog scale), number of tender and swollen joints in 28 joints, initial joint topography (additive, bilateral, distal (hands, wrists or forefeet), or proximal (elbows, shoulders, ankles, knees) involvement), extra-articular manifestations (Sicca syndrome, nodules, Raynaud syndrome), Disease Activity Score in 28 joints–erythrocyte sedimentation rate (DAS28-ESR), functional disability evaluated by the Stanford Health Assessment Questionnaire Disability Index (HAQ-DI), biological features (including ESR, [mm/h], C-reactive protein [CRP; mg/l] level by standard laboratory methods, auto-antibodies previously described, anti-nuclear antibodies (ANA), HLA-DRB1* genotype), and radiographs of hands, wrists, and forefeet in the posteroanterior view.
Follow-up assessment
All patients were followed up for 3 years. A clinical evaluation and blood test for acute phase reactants were performed every year using the technique previously described. RF and anti-CCP antibodies were tested at each visit. Treatments (conventional synthetic [cs] or biological [b] DMARDs, steroids) were reported. Radiographs were obtained every year by using the same technique.
Radiographic evaluation
Radiographs were stored in the Department of Rheumatology, Brest Hospital (Brest, France), and blindly scored for presence of erosions and joint space narrowing according to the van der Heijde-modified total Sharp score (mTSS) [16] by an experienced imaging reader (CL) who was blinded to patients’ other data. Radiographs were scored in a chronological order. Typical RA erosion was defined as previously described [17]. Radiographic progression was defined by an increase of at least 1 unit in the mTSS.
Outcome
We considered a diagnosis of RA as the ability of each patient to fulfill the 2010 ACR/EULAR classification criteria [9]. The patients were classified as RA or not according to the 2010 ACR/EULAR criteria at any visit during the first 3 years of follow-up. Alternative diagnoses were reported among patients who did not fulfill the 2010 ACR/EULAR criteria.
Statistical analysis
Descriptive statistics are presented as mean (SD), median (IQR), or number (%) as appropriate. Comparisons between patients with RF and/or ACPA positivity and without RF and ACPA positivity (as defined above) were performed at baseline and at 3 years by chi-square test or Fisher’s exact test as appropriate for qualitative variables and Wilcoxon test for quantitative variables. Similarly, comparisons between all baseline values and outcome measures involved use of the chi-square test or Fisher’s exact test for categorical data and Wilcoxon test for continuous variables. For the multivariate analysis, continuous variables were transformed into categorical variables with the median or a predetermined threshold used as the cut-off. The explanatory variables included in the multiple regression model had p < 0.20 on univariate analysis. Stepwise logistic regression analysis was used to determine relevant independent baseline variables to predict RA classification during the first 3 years. Significance was defined as p < 0.05 for variables in the multivariate model. SAS v9.4 was used for analysis (SAS Institute, Cary, NC, USA).
Results
Baseline characteristics
Among the 813 included patients, serology data were missing for one patient and 64 were excluded because of another definite diagnosis than RA or undifferentiated arthritis finally made during the 3 years of follow-up: psoriatic arthritis (n = 11), spondyloarthritis (n = 10), osteoarthritis (n = 9), connective tissue disease and vasculitis (n = 16), polymyalgia rheumatica and RS3PE syndrome (n = 3), fibromyalgia (n = 6), or other (n = 9).
Among the 748 remaining patients, 354 (47.3%) were negative for both IgM-RF and anti-CCP2 antibodies and 394 (52.7%) were positive for IgM-RF and/or anti-CCP2 antibodies. The flow-chart of patients is presented in Fig. 1. The baseline characteristics of the 748 patients are in Table 1. Seronegative patients had less active disease than seropositive patients (mean DAS28-ESR 5.0 [SD 1.3] vs 5.3 [SD 1.3], p = 0.002) and had slightly less structural damage (mean mTSS 4.3 [6] vs 5.7 [8.2], p = 0.026) and less disability (mean HAQ-DI 0.9 [0.7] vs 1 [0.7], p = 0.030). HLA-DRΒ1*01 or 04 gene was less frequent in seronegative than seropositive patients (31.6% vs 61.2%, p < 0.001), and the opposite was found for HLA-DRB1*03 (21.7% vs 15.2%, p = 0.021). ANA were more frequent in seropositive than seronegative patients (28.5% vs 12.8%, p < 0.001). Extra-articular manifestations were similar in both groups (Table 1).
Overall, 224/340 (65.9%) seronegative patients with all available data fulfilled 2010 ACR/EULAR criteria for RA at baseline as compared with 386/394 (98%) seropositive patients (p < 0.001). Among them, 60/318 (18.9%) seronegative patients had typical RA erosions [17] as compared with 113/362 (31.2%) seropositive patients (p < 0.001). Other baseline characteristics did not differ between the two groups.
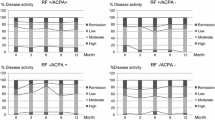
RA outcome at 3 years
Data were available for 617 (242 seronegative and 375 seropositive) patients followed up at 3 years (Table 2). A total of 38 patients who were seronegative at baseline showed RF (n = 30), anti-CCP2 (n = 7), or both auto-antibodies (n = 1) during the 3 years of follow-up and were considered seropositive. Baseline characteristics of these 617 patients were similar to the whole cohort. Baseline HAQ-DI and mTSS data were numerically lower for seronegative compared to seropositive patients reaching 3 years follow-up, but did not reach significance (Additional file 1: Table S1), whereas the difference was significant when considering the whole population (Table 1), probably due to a higher sample size. Finally, 189/233 (81.1%) seronegative and 369/371 (99.4%) seropositive patients with data available were classified as having RA during the 3 years of follow-up (p < 0.001); 71 (29.3%) and 235 (62.7%) had typical RA erosions (p < 0.001) (Table 2).
Seronegative patients had similar mean DAS28-ESR and mean HAQ-DI as seropositive patients (Table 2). The proportion of patients achieving DAS28 remission was similar. The mean mTSS and radiographic progression at 3 years were lower in the seronegative group. These patients also less frequently had csDMARDs or bDMARDs or used corticosteroids than seropositive patients.
The 38 patients who switched from seronegative to seropositive did not show a significantly different outcome as compared with patients who were seropositive at baseline (data not shown).
Predictors of RA classification within 3 years
On univariate analysis, RA classification by 3 years was significantly associated with several baseline parameters among seronegative patients (Table 3). In particular, at baseline, patients fulfilling 2010 ACR/EULAR criteria for RA within 3 years had higher values than those without an RA classification for the following: median (IQR) number of tender joints (9 [5–16] vs 2 [0–4], p < 0.001) and swollen joints (7 [4–12] vs 3 [2–5], p < 0.001), and mean (SD) DAS28 (5.3 [1.2] vs 3.8 [1.1], p < 0.001), HAQ-DI (1 [0.7] vs 0.6 [0.6], p = 0.008), and mTSS (5 [6.6] vs 2.4 [3.1], p = 0.008). A trigger event (p = 0.004), in particular the death of a relative or loved one (p = 0.0253), was more frequent in patients with than without an RA classification during the follow-up. However, some other factors such as presence of anti-nuclear antibodies or harboring HLA-DRΒ1*03 were less frequent in patients with than without RA although not significantly. Mean ESR or CRP level was not significantly higher in RA patients.
Stepwise logistic regression analysis showed that in the seronegative cohort, RA classification within 3 years was associated with the baseline factors additive, bilateral, and distal (i.e., hands, wrists, or forefeet) involvement; presence of a trigger event; pain at rest; morning stiffness; number of tender joints; and mTSS (Table 3), with no association between extra-articular manifestations, harboring HLA- DRΒ1*03 and RA classification.
Discussion
When patients present inflammatory arthritis, physicians must identify disease that will progress to RA. Because auto-antibodies such as RF or ACPA are key in the diagnosis, their weight is important (up to 3 of 10 points) in the 2010 ACR/EULAR classification criteria for RA. Thus, obtaining 6 of 10 points required for such a classification of RA in the absence of these 2 auto-antibodies may be difficult in the early phases of the disease, since it requires the involvement of more than 10 involved joints. Although this situation is frequently encountered, especially in early RA, the initial clinical presentation and disease course of seronegative RA is not well known. We first compared the initial features of patients with early arthritis according to positivity for RF and/or ACPA. We used a large, prospective, early-arthritis cohort from the community. This situation reflects clinical practice and allowed us to study the clinical value of RF and ACPA in patients selected by symptoms, not diagnosis. The patients in our 2 seronegative and seropositive groups were well balanced, thus confirming that almost half of the patients were negative for RF and ACPA at inclusion in this primary care–based cohort. The disease was less active based on DAS28-ESR and also less severe in terms of functional index and radiographic score at baseline in seronegative versus seropositive group. These results agree with those of the Norfolk Arthritis Register (NOAR) [18, 19] but not with the Canadian early-arthritis cohort (CATCH), showing seronegative patients with higher mean swollen joint count, DAS28, and erosive disease [20], which suggests that these patients are more frequently referred to rheumatology if they have more active and severe disease. The disease progression was less severe and DMARD or steroid use less frequent in seronegative versus seropositive group during follow-up in the ESPOIR cohort, which agrees with other early-arthritis cohorts [18, 20]. In our cohort, about 10% of patients developed de novo auto-antibodies (RF or anti-CCP2) during the 3 years of follow-up. This proportion was less in another Dutch early-arthritis cohort, in which the switch from negative to positive occurred in 2% for ACPA and 3% for IgM-RF during the first year of follow-up [21].
The secondary objective of our study was to determine baseline predictors of fulfilling the 2010 ACR/EULAR criteria for RA within 3 years in these patients. We were looking for factors other than auto-antibodies that suggest the development of RA. The best independent predictive factors were additive, bilateral, and distal involvement; presence of a trigger event; pain at rest; morning stiffness; number of tender joints; and mTSS. In the prediction model for persistent erosive arthritis published by Visser et al., similar baseline variables were selected, including morning stiffness for at least 1 h, arthritis in at least three joint groups, IgM-RF, and anti-CCP2 positivity, in addition to erosions on hand and foot radiographs that were not selected in our model [22].
ACR/EULAR classification criteria were used to guide the diagnosis of RA, which may lead to incorporation bias, because explanatory variables were part of the reference standard. This observation may suggest overestimation of the discriminative ability of the model [23]. To partly solve this problem, we could have added expert opinion to the ACR/EULAR criteria, although incorporation bias still exists in this case. This bias can explain the important weight of the number of tender joints in the model. Of note, the area under the receiver operating characteristic curve for the stepwise logistic regression analyses was high (0.905), which suggests that these predictors are efficient to differentiate early in the disease between RA and other forms of arthritis in clinical practice. ACR/EULAR classification criteria were built based on cohorts of real-world patients with early arthritis, to identify factors and their relative weights, which were associated with the subsequent decision by a physician to start methotrexate. Consequently, they were better adapted to the classification of patients with early arthritis. Nevertheless, performance of these criteria have also been studied in patients with established disease and had the same sensitivity, but higher specificity than the 1987 ACR criteria for predicting a diagnosis of RA after 10 years, mainly due to the use of exclusion criteria [24].
Nevertheless, some limitations in our study should be noted. First, patients were defined as seronegative if they did not have IgM-RF and anti-CCP2 antibodies. Some seronegative patients may have had other RA-associated antibodies, such as IgA-RF or anticarbamylated antibodies, which were not tested in our study. However, based on currently available studies, these patients likely represent a small proportion of the seronegative population [25]. Among 318 patients with anti-CCP-negative RA (1987 ACR criteria) included in the Leiden early-arthritis cohort, a cluster analysis performed to evaluate whether patients resemble each other revealed no grouping of patients, which suggests that anti-CCP–negative RA patients may be homogeneous [26]. Second, more patients were lost to follow-up in the seronegative group, even after accounting for the 38 patients with auto-antibodies during follow-up. This finding can be explained by patients with severe RA more likely to be followed up. Previous data noted that anti-CCP antibodies were the best predictor of remaining in the ESPOIR cohort for 5 years [27].
Conclusion
Patients with early arthritis and without RF and ACPA have less active disease at baseline and less severe disease during follow-up. They are more likely to fulfill RA classification at 3 years if they have RA typical inflammatory characteristics of pain, symmetric involvement of numerous small joints, and initial erosive disease.
Abbreviations
- ACPA:
-
Anti-citrullinated protein antibodies
- ACR:
-
American College of Rheumatology
- ANA:
-
Anti-nuclear antibodies
- Anti-CCP:
-
Anti-cyclic-citrullinated peptide
- APHP:
-
Assistance publique – hôpitaux de Paris
- b DMARD:
-
Biological DMARD
- CATCH:
-
Canadian early-arthritis cohort
- CHU:
-
Centre hospitalier universitaire
- CNIL:
-
Commission nationale de l'informatique et des libertés
- CRP:
-
C-reactive protein
- cs DMARD:
-
Conventional synthetic DMARD
- DAS28:
-
Disease activity score in 28 joints
- DMARD:
-
Disease-modifying anti-rheumatic drug
- EA:
-
équipe d’accueil
- ESPOIR:
-
Etude et Suivi des POlyarthrites Indifferenciées Récentes
- ESR:
-
Erythrocyte sedimentation rate
- EULAR:
-
European League Against Rheumatism
- HAQ-DI:
-
Stanford Health Assessment Questionnaire Disability Index
- HLA:
-
Human leucocyte antigen
- Ig:
-
Immunoglobulin
- INSERM:
-
Institut national de la santé et de la recherche médicale
- IQR:
-
Interquartile range
- IRF-5:
-
Interferon regulatory factor 5
- mTSS:
-
Modified total Sharp score
- NOAR:
-
Norfolk Arthritis Register
- ORs:
-
Odds ratios
- PTPN22:
-
Protein tyrosine phosphatase, non receptor type 22
- RA:
-
Rheumatoid arthritis
- RF:
-
Rheumatoid factor
- RS3PE syndrome:
-
Remitting seronegative symmetrical synovitis with pitting edema
- SAS:
-
Statistical Analysis System
- SD:
-
Standard deviation
- TNFAIP3-OLIG3:
-
Tumor necrosis factor Alpha Induced Protein 3 - oligodendrocyte transcription factor 3
- TRAF1/C5:
-
Tumor necrosis factor-receptor associated factor 1/complement component 5
- UMR:
-
unité mixte de recherche
- Univ:
-
University
- Vs:
-
Versus
References
Gossec L, Combescure C, Rincheval N, Saraux A, Combe B, Dougados M. Relative clinical influence of clinical, laboratory, and radiological investigations in early arthritis on the diagnosis of rheumatoid arthritis. Data from the French Early Arthritis Cohort ESPOIR. J Rheumatol. 2010;37(12):2486–92.
Avouac J, Gossec L, Dougados M. Diagnostic and predictive value of anti-cyclic citrullinated protein antibodies in rheumatoid arthritis: a systematic literature review. Ann Rheum Dis. 2006;65(7):845–51.
Nishimura K, Sugiyama D, Kogata Y, Tsuji G, Nakazawa T, Kawano S, et al. Meta-analysis: diagnostic accuracy of anti-cyclic citrullinated peptide antibody and rheumatoid factor for rheumatoid arthritis. Ann Intern Med. 2007;146(11):797–808.
Aggarwal R, Liao K, Nair R, Ringold S, Costenbader KH. Anti-citrullinated peptide antibody assays and their role in the diagnosis of rheumatoid arthritis. Arthritis Rheum. 2009;61(11):1472–83.
van Gaalen FA, van Aken J, Huizinga TW, Schreuder GM, Breedveld FC, Zanelli E, et al. Association between HLA class II genes and autoantibodies to cyclic citrullinated peptides (CCPs) influences the severity of rheumatoid arthritis. Arthritis Rheum. 2004;50(7):2113–21.
Mewar D, Coote A, Moore DJ, Marinou I, Keyworth J, Dickson MC, et al. Independent associations of anti-cyclic citrullinated peptide antibodies and rheumatoid factor with radiographic severity of rheumatoid arthritis. Arthritis Res Ther. 2006;8(4):R128.
Mattey DL, Hassell AB, Dawes PT, Cheung NT, Poulton KV, Thomson W, et al. Independent association of rheumatoid factor and the HLA-DRB1 shared epitope with radiographic outcome in rheumatoid arthritis. Arthritis Rheum. 2001;44(7):1529–33.
Vittecoq O, Pouplin S, Krzanowska K, Jouen-Beades F, Menard JF, Gayet A, et al. Rheumatoid factor is the strongest predictor of radiological progression of rheumatoid arthritis in a three-year prospective study in community-recruited patients. Rheumatology (Oxford). 2003;42(8):939–46.
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69(9):1580–8.
Zink A, Listing J, Niewerth M, Zeidler H, German Collaborative Arthritis C. The national database of the German Collaborative Arthritis Centres: II. Treatment of patients with rheumatoid arthritis. Ann Rheum Dis. 2001;60(3):207–13.
Ding B, Padyukov L, Lundstrom E, Seielstad M, Plenge RM, Oksenberg JR, et al. Different patterns of associations with anti-citrullinated protein antibody-positive and anti-citrullinated protein antibody-negative rheumatoid arthritis in the extended major histocompatibility complex region. Arthritis Rheum. 2009;60(1):30–8.
Plenge RM, Seielstad M, Padyukov L, Lee AT, Remmers EF, Ding B, et al. TRAF1-C5 as a risk locus for rheumatoid arthritis--a genomewide study. N Engl J Med. 2007;357(12):1199–209.
van der Helm-van Mil AH, Huizinga TW. Advances in the genetics of rheumatoid arthritis point to subclassification into distinct disease subsets. Arthritis Res Ther. 2008;10(2):205.
Verpoort KN, van Gaalen FA, van der Helm-van Mil AH, Schreuder GM, Breedveld FC, Huizinga TW, et al. Association of HLA-DR3 with anti-cyclic citrullinated peptide antibody-negative rheumatoid arthritis. Arthritis Rheum. 2005;52(10):3058–62.
Combe B, Benessiano J, Berenbaum F, Cantagrel A, Daures JP, Dougados M, et al. The ESPOIR cohort: a ten-year follow-up of early arthritis in France: methodology and baseline characteristics of the 813 included patients. Joint Bone Spine. 2007;74(5):440–5.
van der Heijde DM, van Riel PL, Nuver-Zwart IH, Gribnau FW, vad de Putte LB. Effects of hydroxychloroquine and sulphasalazine on progression of joint damage in rheumatoid arthritis. Lancet. 1989;1(8646):1036–8.
van der Heijde D, van der Helm-van Mil AH, Aletaha D, Bingham CO, Burmester GR, Dougados M, et al. EULAR definition of erosive disease in light of the 2010 ACR/EULAR rheumatoid arthritis classification criteria. Ann Rheum Dis. 2013;72(4):479–81.
Farragher TM, Lunt M, Plant D, Bunn DK, Barton A, Symmons DP. Benefit of early treatment in inflammatory polyarthritis patients with anti-cyclic citrullinated peptide antibodies versus those without antibodies. Arthritis Care Res (Hoboken). 2010;62(5):664–75.
Bukhari M, Thomson W, Naseem H, Bunn D, Silman A, Symmons D, et al. The performance of anti-cyclic citrullinated peptide antibodies in predicting the severity of radiologic damage in inflammatory polyarthritis: results from the Norfolk Arthritis Register. Arthritis Rheum. 2007;56(9):2929–35.
Barra L, Pope JE, Orav JE, Boire G, Haraoui B, Hitchon C, et al. Prognosis of seronegative patients in a large prospective cohort of patients with early inflammatory arthritis. J Rheumatol. 2014;41(12):2361–9.
Ursum J, Bos WH, van Dillen N, Dijkmans BA, van Schaardenburg D. Levels of anti-citrullinated protein antibodies and IgM rheumatoid factor are not associated with outcome in early arthritis patients: a cohort study. Arthritis Res Ther. 2010;12(1):R8.
Visser H, le Cessie S, Vos K, Breedveld FC, Hazes JM. How to diagnose rheumatoid arthritis early: a prediction model for persistent (erosive) arthritis. Arthritis Rheum. 2002;46(2):357–65.
Visser H, Hazes JM. The diagnosis and prognosis of early arthritis: comment on the editorial by Scott. Arthritis Rheum. 2003;48(3):856–7 author reply 7-8.
Cornec D, Varache S, Morvan J, Devauchelle-Pensec V, Berthelot JM, Le Henaff-Bourhis C, et al. Comparison of ACR 1987 and ACR/EULAR 2010 criteria for predicting a 10-year diagnosis of rheumatoid arthritis. Joint Bone Spine. 2012;79(6):581–5.
Shi J, Knevel R, Suwannalai P, van der Linden MP, Janssen GM, van Veelen PA, et al. Autoantibodies recognizing carbamylated proteins are present in sera of patients with rheumatoid arthritis and predict joint damage. Proc Natl Acad Sci U S A. 2011;108(42):17372–7.
De Rooy DP, Willemze A, Mertens B, Huizinga TW, Van der Helm-van Mil AH. Can anti-cyclic citrullinated peptide antibody-negative RA be subdivided into clinical subphenotypes? Arthritis Res Ther. 2011;13(5):R180.
Combe B, Rincheval N, Benessiano J, Berenbaum F, Cantagrel A, Daures JP, et al. Five-year favorable outcome of patients with early rheumatoid arthritis in the 2000s: data from the ESPOIR cohort. J Rheumatol. 2013;40(10):1650–7.
Acknowledgements
We thank S. Martin (Paris Bichat) who analyzed all the central dosages of CRP, IgM-RF, and anti-CCP antibodies and all investigators who recruited and followed patients (F. Berenbaum, Paris- Saint Antoine, MC. Boissier, Paris-Bobigny, A. Cantagrel, Toulouse, B. Combe, Montpellier, M. Dougados, Paris-Cochin, P Fardelone et P Boumier Amiens, B. Fautrel, Paris-La Pitié, RM. Flipo, Lille, Ph. Goupille, Tours, F. Liote, Paris- Lariboisière, O Vittecoq, Rouen, X Mariette, Paris Bicetre, O Meyer et Ph Dieude, Paris Bichat, A. Saraux, Brest, Th Schaeverbeke, Bordeaux, J. Sibilia, Strasbourg).
Funding
An unrestricted grant from Merck Sharp and Dohme (MSD) was allocated for the first 5 years of the ESPOIR cohort study. Two additional grants from INSERM were obtained to support part of the biological database. The French Society of Rheumatology, Pfizer, Abbvie, and more recently Roche-Chugai and Lilly also supported the ESPOIR cohort study.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article and its additional files.
Author information
Authors and Affiliations
Contributions
GM conceived of the study and drafted the manuscript, NR performed the statistical analysis, CL participated in the design of the study, CD participated in the design of the study, AS participated in the design of the study, PD participated in the design of the study, JM participated in the design of the study, BC conceived of the study, and participated in its design and coordination, and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol of the ESPOIR cohort was approved by the ethics committee of Montpellier, France (no. 020307, CNIL 02-1293), and all patients gave their signed informed consent before inclusion.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Table S1. Baseline characteristics of patients with “seronegative” and “seropositive” early arthritis with data available at 3 years (n = 617). (DOCX 115 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mouterde, G., Rincheval, N., Lukas, C. et al. Outcome of patients with early arthritis without rheumatoid factor and ACPA and predictors of rheumatoid arthritis in the ESPOIR cohort. Arthritis Res Ther 21, 140 (2019). https://doi.org/10.1186/s13075-019-1909-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-019-1909-8