Abstract
Background
There is conflicting evidence on association between quick sequential organ failure assessment (qSOFA) and sepsis mortality in ICU patients. The primary aim of this study was to determine the association between qSOFA and 28-day mortality in ICU patients admitted for sepsis. Association of qSOFA with early (3-day), medium (28-day), late (90-day) mortality was assessed in low and lower middle income (LLMIC), upper middle income (UMIC) and high income (HIC) countries/regions.
Methods
This was a secondary analysis of the MOSAICS II study, an international prospective observational study on sepsis epidemiology in Asian ICUs. Associations between qSOFA at ICU admission and mortality were separately assessed in LLMIC, UMIC and HIC countries/regions. Modified Poisson regression was used to determine the adjusted relative risk (RR) of qSOFA score on mortality at 28 days with adjustments for confounders identified in the MOSAICS II study.
Results
Among the MOSAICS II study cohort of 4980 patients, 4826 patients from 343 ICUs and 22 countries were included in this secondary analysis. Higher qSOFA was associated with increasing 28-day mortality, but this was only observed in LLMIC (p < 0.001) and UMIC (p < 0.001) and not HIC (p = 0.220) countries/regions. Similarly, higher 90-day mortality was associated with increased qSOFA in LLMIC (p < 0.001) and UMIC (p < 0.001) only. In contrast, higher 3-day mortality with increasing qSOFA score was observed across all income countries/regions (p < 0.001). Multivariate analysis showed that qSOFA remained associated with 28-day mortality (adjusted RR 1.09 (1.00–1.18), p = 0.038) even after adjustments for covariates including APACHE II, SOFA, income country/region and administration of antibiotics within 3 h.
Conclusions
qSOFA was independently associated with 28-day mortality in ICU patients admitted for sepsis. In LLMIC and UMIC countries/regions, qSOFA was associated with early to late mortality but only early mortality in HIC countries/regions.
Graphical Abstract

Similar content being viewed by others
Introduction
Sepsis-3 consensus definitions introduced quick Sequential Organ Failure Assessment (qSOFA) as a sepsis screening tool to identify patients with higher hospital mortality [1]. The original Sepsis-3 derivation cohort showed that Sequential Organ Failure Assessment (SOFA) was superior when compared to qSOFA or systemic inflammatory response syndrome (SIRS) for prediction of mortality in the intensive care unit (ICU) [2]. Subsequent early validation studies on qSOFA from ICUs in high income settings have confirmed these limitations [3,4,5,6]. Thus, its potential role as a simple sepsis diagnostic and outcome prediction tool has been mostly evaluated in the Emergency Department [7,8,9].
Whether qSOFA has prognostic value for patients with sepsis in low resourced ICUs where Acute Physiology and Chronic Health Evaluation (APACHE) II score or SOFA may not be practical has not been robustly assessed [10, 11]. Recent evidence from low resource settings does suggest qSOFA is associated with mortality in hospitalized patients with infection [12,13,14,15,16].The addition of lactate has also been shown to improve qSOFA sepsis mortality prediction in all income settings [17,18,19,20,21].
Studies on qSOFA mortality prediction in ICU patients with sepsis have generally used all-cause hospital mortality as the endpoint. However, since calculation of qSOFA is based on physiological parameters alone, its predictive performance is likely more dependent on time from assessment than severity scores such as APACHE II that incorporate variables on chronic health. This has been demonstrated in a large retrospective study in Taiwan which showed that the association between qSOFA mortality was greater at 72 h than 28-days [22].
The Management of Severe sepsis in Asia’s Intensive Care unitS (MOSAICS) II was a prospective, observational, cross-sectional point prevalence study on sepsis epidemiology in 386 ICUs from 22 Asian countries/regions across all income settings [23]. Detailed admission physiological data was collected from a well-defined cohort of 4980 ICU patients admitted for sepsis. In this secondary analysis of MOSAICS II, our primary aim was to determine the association between qSOFA and 28-day mortality in ICU patients admitted for sepsis. Association of qSOFA with early (3-day), medium (28-day), late (90-day) mortality was assessed in low and lower middle income (LLMIC), upper middle income (UMIC) and high income (HIC) countries/regions. Predictive performance of qSOFA on 28-day mortality was compared to APACHE II, SIRS, SOFA. Additional value of lactate measurement on qSOFA sepsis mortality prediction was assessed. Lastly, we described the characteristics and outcomes of different clinical sepsis phenotypes in patients who met Sepsis-3 SOFA criteria and simultaneously fulfilled SIRS and qSOFA criteria.
Methods
Study design and score criteria
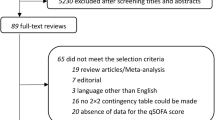
The MOSAICS II study recruited adult patients (age ≥ 18 years old) who were admitted to the ICU for treatment of sepsis. Sepsis was defined using Sepsis-3 criteria as infection with a ∆SOFA ≥ 2 from baseline [1]. They were recruited on four separate days of different quarters in 2019 [23]. All patients from the MOSAICS II cohort who had ICU admission qSOFA recorded were included in this study. Patients who had missing SOFA, APACHE II and survival status at 90 days were excluded from this analysis. Countries and regions were grouped by income according to the 2019 World Bank Classification [24].
Score criteria
Physiological data and laboratory results closest to time of ICU admission was used to calculate ∆SOFA, SIRS and qSOFA score. Change in SOFA at ICU admission from baseline SOFA (assumed to be zero if without prior organ dysfunction) was calculated to obtain ∆SOFA score (0 to 24 points) [25]. qSOFA score (0 to 3 points) was calculated by summation of individual components with 1 point each for SBP < 100 mmHg, respiratory rate ≥ 22 breaths/min and altered mental status (Glasgow Coma Scale < 15) [1, 3, 4]. SIRS (0 to 4 points) was assessed by fulfillment of four individual components: heart rate > 90 beats/min; temperature < 36 °C or > 38 °C; white blood cell count > 12,000/μL or < 4000/μL; respiratory rate > 20 breaths/min or arterial PCO2 < 32 mmHg [26]. Thresholds to fulfill score criteria were ∆SOFA ≥ 2 for SOFA, ≥ 2 for SIRS, ≥ 2 for qSOFA [1, 26].
Mortality endpoint
All patients recruited to MOSAICS II were prospectively followed up for all-cause mortality from initial time of sepsis recognition until day 90. Patients who were alive but not discharged from hospital at 90 days were classified as survivors at 90 days. Early (3-day), medium (28-day) and late (90-day) mortality was assessed.
Predictive performance of scores
Predictive performances of APACHE II, SOFA, SIRS, qSOFA and qSOFA with lactate to predict early to late mortality were assessed using area under the receiver operating characteristic curve (AUC), sensitivity and specificity. The lactate value obtained closet to time of ICU admission (within 24 h) was used for analysis. Patients who did not have lactate results were excluded in this part of the analysis. The thresholds selected for each score was determined for each mortality timepoint using Youden’s index. A subgroup analysis excluding patients who remained in hospital by day 90 was performed to evaluate the discriminatory performance of each score for hospital mortality.
Clinical sepsis phenotype
Patients were classified into four clinical sepsis phenotype groups accordingly: “SOFA only” (S), “SOFA and SIRS” (SS), “SOFA and qSOFA” (SqS) and “SOFA and SIRS and qSOFA” (SSqS). Phenotype S consisted of patients who only had SOFA without fulfilling SIRS or qSOFA criteria. Phenotype SS consisted of those who fulfilled both SOFA and SIRS criteria but had qSOFA < 2. Phenotype SqS consisted of patients with sepsis who fulfilled both SOFA and qSOFA criteria but had SIRS < 2. Those who met the thresholds for all three scores were included in the SSqS phenotype.
Statistical analysis
Shapiro–Wilk test was used to test for normality of numerical variables. Descriptive statistics using proportions and median with interquartile range were used to summarize data. Kruskal–Wallis and ϰ2 tests were used to assess the differences in characteristics between clinical phenotype groups. Pairwise ϰ2 test was used to assess differences in mortality between different clinical phenotypes. Association between overall qSOFA score and individual qSOFA components were compared within each income region/country using ϰ2 test. Fischer’s test was used instead of ϰ2 test when appropriate.
Multivariate analysis using modified Poisson regression was used to determine the adjusted relative risk (RR) of qSOFA score on mortality at 28 days. A directed acyclic graph was used to select covariates from identified confounders on hospital mortality in MOSAICS II and other illness severity scores [23]. These included income region/country, age, sex, solid malignant tumor, immunosuppression, hematological malignancy, Emergency Department admission, unscheduled surgical admission, antibiotic within 3 h of sepsis recognition, APACHE II and SOFA (see Additional file 1: Fig. S1). Additional multivariate analyzes were performed to assess the association between qSOFA and mortality at 3-days and 90-days.
Difference in AUC on 28-day mortality prediction between scores were compared using Delong’s method. McNemar’s test was used to evaluate differences in sensitivities and specificities of severity scores. Significance value was set at α < 0.05. Data analyzes were performed in R studio (v 2023.06.1 + 524) with reportROC and ggplot packages.
Results
Cohort characteristics
Among the MOSAICS II study cohort of 4980 patients, 4826 patients from 343 ICUs and 22 countries were included in this secondary analysis (see Additional file 1: Fig. S2). The baseline characteristics of included patients grouped by clinical phenotype are shown in Table 1. Overall, 696/4826 (14.4%) fulfilled only SOFA criteria, 1495/4826 (31.0%) fulfilled both SOFA and SIRS, 265/4826 (5.5%) fulfilled both SOFA and qSOFA, and 2370/4826 (49.1%) fulfilled all of SOFA, SIRS and qSOFA criteria. The proportion of individual qSOFA score components in different income countries/regions are shown in Fig. S3, Additional file 1. There were 281 patients who remained in hospital at 90 days. HIC countries/regions had the highest proportion of patients who remained in hospital by day 90 compared to LLMIC and UMIC countries/regions (p < 0.001) (see Additional file 1: Fig. S4 and Fig. S5).
qSOFA and associated mortality
Early to late mortality rates associated with range of qSOFA scores in different income countries/regions are shown in Fig. 1. Overall, 28-day mortality progressively increased with higher qSOFA (p < 0.001). However, this 28-day trend was only observed in LLMIC (p < 0.001) and UMIC (p < 0.001) and not HIC (p = 0.220) countries/regions (see Additional file 2: Table S1). Similarly, higher 90-day mortality was associated with increased qSOFA in LLMIC (p < 0.001) and UMIC (p < 0.001) only. In contrast, higher 3-day mortality with increasing qSOFA score was observed across all income countries/regions (p < 0.001). Only systolic blood pressure and altered mental status components of qSOFA were consistently associated with 28-day mortality in both LLMIC and UMIC (see Additional file 2: Table S2). In contrast, none of the qSOFA components were associated with 28-day mortality in HIC countries/regions.
Multivariate analysis showed that qSOFA remained associated with 28-day mortality (adjusted RR 1.09 [1.00–1.18], p = 0.038) even after adjustments for covariates including APACHE II, SOFA, income country/region and administration of antibiotics within 3 h (Table 2). In addition, qSOFA was associated with 3-day mortality (adjusted RR 1.52 [1.24–1.87], p < 0.001) but was not associated with 90-day mortality (adjusted RR 1.03 [0.96–1.100], p = 0.454) on multivariate analysis (see Additional file 2: Tables S3 and S4). In contrast, APACHE II and SOFA were both independently associated with mortality at 3-days, 28-days and 90-days.
Mortality prediction performance of APACHEII, SOFA, SIRS, qSOFA
Predictive performance of APACHE II, SOFA, SIRS, qSOFA, and qSOFA with lactate for mortality were evaluated in 3,863 patients after exclusion of 1091 patients who did not have lactate results within 24 h of ICU admission. The AUCs of different scores on prediction of short to long term mortality are shown in Fig. 2. The addition of lactate did not improve the AUC of qSOFA to predict 28-day mortality (qSOFA with lactate [0.644 (95%CI 0.602–0.685)] vs. qSOFA [0.642 (95%CI 0.601–0.682)], p = 0.175) (see Additional file 2: Table S5). On subgroup analysis, there was no difference between qSOFA with lactate and qSOFA alone on prediction of 28-day mortality in any of the income countries/regions (see Additional file 1: Fig. S6 and Additional file 2: Tables S6–S8).
Mortality predictive performance of different scores across income regions/countries. Heatmap showing the area under the curve (AUC) of APACHE II, SOFA, SIRS, qSOFA and qSOFA with lactate to predict mortality across all income countries/regions. APACHE, Acute Physiology And Chronic Health Evaluation; qSOFA, quick sequential organ failure assessment; SIRS, systemic inflammatory response syndrome; SOFA, sequential organ failure assessment
qSOFA had lower AUC compared to APACHE II to predict 28-day mortality in HIC region/countries (APACHE II [0.599 (95%CI 0.562–0.636)] vs. qSOFA [0.530 (95%CI 0.495–0.566)], p = 0.001) and UMIC region/countries (APACHE II [0.636 (95%CI 0.604–0.669)] vs. qSOFA [0.576 (95%CI 0.545–0.608)], p < 0.001). In contrast, qSOFA had similar AUC compared to APACHE II predicted 28-day mortality in LLMIC (APACHE II 0.637 (95%CI 0.601–0.674) vs. qSOFA 0.601 (95%CI 0.566–0.636), p = 0.077). Since qSOFA was not associated with 90-day mortality in multivariate analysis, additional testing was performed to confirm qSOFA was indeed inferior to APACHE II in 90-day mortality discrimination in LLMIC (AUC 0.591 [95%CI 0.557–0.625] vs. 0.649 [95%CI 0.614–0.683], p = 0.003). In contrast, there was no difference between the AUCs of qSOFA and SOFA to predict 28-day mortality in any of the income countries/regions.
Overall, APACHE II and qSOFA both had poor specificity for 28-day mortality, although APACHE II was slightly higher [0.566 (95%CI 0.547–0.584) vs 0.490 (95%CI 0.471–0.508), p < 0.001]. Similarly, the sensitivity of either APACHE II or qSOFA for 28-day mortality was poor for 28-day mortality [0.608 (95%CI 0.577–0.638) vs. 0.625 (95%CI 0.595–0.655), p = 0.363]. Comparatively, qSOFA had higher sensitivity (p = 0.048) but lower specificity (p < 0.001) compared to SOFA which had sensitivity of 0.586 (95%CI 0.555–0.617) and specificity of 0.549 (95%CI 0.531–0.567) to predict 28-day mortality. Predictive performance of different scores for 3-day, 28-day and 90-day mortality are shown in Tables S5–S8, Additional file 2. The predictive performances of different scores for hospital mortality in subgroup analysis excluding patients who remained in hospital by day 90 were similar to the performances of the scores for 90-day mortality in the whole study cohort (see Additional file 2: Tables S9–S12).
Clinical sepsis phenotype and associated mortality
SOFA and APACHE II scores were higher in phenotypes which fulfilled the qSOFA criteria (SqS and SSqS) compared to those that did not (S and SS) (Table 1). Use of vasopressors, mechanical ventilation and kidney replacement therapy were also higher phenotypes SqS and SSqS than S or SS. The proportions of each clinical sepsis phenotype in different income countries/regions are shown in Fig. 3. Overall, phenotype S had lower 28-day mortality (19.7%) when compared to those with phenotype SqS (26.8%, p < 0.001) or SSqS (30.7%, p < 0.001) (Fig. 4). Patients with the SSqS phenotype had higher 3-day and 90-day mortality when compared to both phenotype S or SS (p < 0.001).
Proportion of clinical sepsis phenotype in different income countries/regions. Patients with sepsis were classified into four clinical sepsis phenotype groups according to fulflilment of score criteria: “SOFA only” (S), “SOFA and SIRS” (SS), “SOFA and qSOFA” (SqS) and “SOFA and SIRS and qSOFA” (SSqS). Distribution of patients with different clinical phenotypes across all income country/region groups. APACHE, Acute Physiology And Chronic Health Evaluation; qSOFA, quick sequential organ failure assessment; SIRS, systemic inflammatory response syndrome; SOFA, sequential organ failure assessment
Clinical sepsis phenotype and associated all-cause mortality. Patients with sepsis were classified into four clinical sepsis phenotype groups according to fulflilment of score criteria: “SOFA only” (S), “SOFA and SIRS” (SS), “SOFA and qSOFA” (SqS) and “SOFA and SIRS and qSOFA” (SSqS). APACHE, Acute Physiology And Chronic Health Evaluation; qSOFA, quick sequential organ failure assessment; SIRS, systemic inflammatory response syndrome; SOFA, sequential organ failure assessment
Discussion
In this secondary analysis of the MOSAICS II study, we found that qSOFA was independently associated with 28-day mortality in ICU patients admitted for sepsis. qSOFA was associated with early to late mortality in LLMIC and UMIC but only early mortality in HIC countries/regions. The 28-day mortality prediction performance of APACHE II was superior to qSOFA in HIC and UMIC. qSOFA and APACHE II had comparable, but low discriminatory performance for 28-day sepsis mortality in LLMIC. The addition of lactate did not improve the prognostic performance of qSOFA to predict 28-day sepsis mortality. The combination of SOFA, SIRS and qSOFA at time of ICU admission identified a clinical phenotype of sepsis associated with higher severity of illness and early to late mortality.
qSOFA was originally proposed as a sepsis screening tool rather than prognostic score among patients with suspected infection [1]. Moreover, interest in qSOFA as a sepsis outcome predictor in ICU patients was limited as early studies from HIC countries/regions suggest it was not better than, or even inferior to mortality prediction of SOFA [3,4,5]. In contrast, recent data from resource limited settings showed that qSOFA may have prognostic value even for patients with sepsis in the ICU [6, 27,28,29]. Our study adds clarity to these seemingly contradictory findings. Earlier study cohorts were either large retrospective cohorts or single center prospective studies from a specific income setting. Moreover, studies from limited resource settings used early mortality endpoints such as ICU mortality or 28-day mortality, whereas those from well-resourced settings assessed hospital mortality. In this study we used a well-defined, large prospective cohort of ICU patients from all income settings who met Sepsis-3 criteria to assess association between qSOFA and early (3-day) to late (90-day) sepsis mortality. We found that qSOFA was indeed associated with early to late mortality in LLMIC and UMIC but only early mortality in HIC countries/regions for ICU patients with sepsis. Furthermore, we showed that qSOFA was independently associated with 3-day and 28-day but not 90-day mortality in sepsis after adjustment for income setting. Combined with earlier studies, we conclude that association between qSOFA and sepsis mortality is both time dependent and variable across income settings.
Surprisingly, qSOFA was independently associated with 3-day and 28-day mortality even after adjustment for APACHE II and SOFA. Of note, it is interesting that qSOFA had higher adjusted RR compared to APACHE II for 3-day and 28-day mortality. Since qSOFA scoring is based on physiological variables alone, it seems reasonable that association between qSOFA and sepsis mortality was only significant in the early to medium term. Whereas for longer term survival at 90 days, age and comorbidities (adjusted for in APACHE II calculation) likely play larger roles compared to physiology predictors alone [30].
It should be noted that APACHE II, SOFA, qSOFA and SIRS all had limited discriminatory performance, sensitivity and specificity to predict sepsis mortality in ICU patients across all income settings in this study. The predictive performance of SOFA (AUC 0.569–0.630) for 28-day mortality in ICU patients with sepsis was lower in this study compared to previous reports from Thailand (AUC 0.839) or Australia and New Zealand (AUC 0.753) [3, 31]. Similarly, the mortality discrimination of APACHE II in this study (AUC 0.599–0.637) was lower than those reported from Saudi Arabia (AUC 0.782) or United States (AUC 0.80) [32, 33]. There are several reasons which may explain the observed differences. First, we calculated SOFA based on parameters closest to time of ICU admission. Instead, most studies used the worst clinical parameters within the first 24 h to calculate admission SOFA score. However, this does not explain why APACHE II also had comparatively lower predictive performance for mortality in this study. Second, our study evaluated predictive performance for 28-day mortality whereas comparative studies assessed hospital mortality. Yet, even when patients who remained in hospital at day 90 were excluded in subgroup analysis to avoid bias from censorship, discriminatory performance for hospital mortality of APACHE II and SOFA were still lower when compared to previous studies (Supplementary Table 9–12, Additoinal File 2). Third, the MOSAICS II cohort was constructed from ICU patients admitted for sepsis who all met SOFA criteria of Sepsis-3, whereas other cohorts used diagnostic coding or SIRS criteria [3, 31]. Since the discordance between SOFA, qSOFA and SIRS on diagnosis and outcomes of sepsis has been well documented, differences in study inclusion criteria for sepsis alone may have altered cohort characteristics and outcomes [14, 31, 34,35,36,37].
Although qSOFA’s predictive performance for mortality in ICU patients with sepsis was generally limited, its practical utility may differ according to income setting. Similar to data from Austrailia, we found that qSOFA was inferior to APACHE II in HIC and UMIC countries/regions on prediction of 28-day mortality [19]. In these settings, qSOFA will unlikely be used for prognostication in the ICU. However, qSOFA was comparable to APACHE II in LLMIC. Although APACHE II is widely used as a severity score for benchmarking, full calculation of APACHE II is not universally available in low resource settings [10, 11]. However, justifying use of qSOFA in low resource ICUs to provide early sepsis prognostication based on its comparable mortality discrimination to APACHE II has its own caveats. First, APACHE II was developed in HIC with limited calibration for LLMIC, and alternate scoring systems with better performance tailored for low resource settings have been proposed [11, 38]. In fact, APACHE II itself had relatively lower 28-day mortality discrimination performance (AUC 0.612) in the LLMIC cohort compared to UMIC or HIC. Severity scores may perform differently in LLMICs because of difference in case-mix with younger and minimal comorbidities when compared to HIC settings [38, 39]. These differences in patient characteristics were highlighted in the original MOSAICS II study [23]. Furthermore, MOSAICS II also showed sepsis mortality was higher in ICUs from LLMIC and UMIC when compared to HIC even after adjustment for confounders. Second, APACHE II was originally validated for predicting hospital mortality rather than specific day of mortality [40]. Alternatively, SIRS is relatively easy to compute by the bedside even in low resourced ICUs. But our results are consistent with other studies that showed SIRS underperforms when compared to qSOFA and other severity scores for mortality prediction [2, 3, 31, 41, 42].
In contrast to previous studies, addition of lactate measurement did not improve qSOFA sepsis mortality prediction [17,18,19,20,21]. Our discrepant results do not discount the utility of lactate measurement as there are several methodological and cohort differences between this study and previous reports. First, MOSAICS II only included ICU patients, whereas other studies were mostly focused on patients outside the ICU [18, 20, 21]. In addition, the mortality rate was much higher in this study compared to other studies. Second, the median lactate score was higher in this study. This suggests lactate may be better at discriminating patients who have very low risk of death against those with any elevated risks of death than discriminating those with moderate from very high risk of death from infection. In practice, lactate measurement is likely most useful outside the ICU setting to identify patients with sepsis at risk of higher mortality.
Value of combining SOFA, qSOFA and SIRS criteria to identify clinical phenotypes of sepsis has not been robustly evaluated. A retrospective study from China showed that hospitalized patients with sepsis who met both SOFA and qSOFA had higher hospital mortality when compared to those who only fulfilled SOFA alone [14]. We found that fulfillment of qSOFA criteria in addition to SOFA or in combination with SOFA and SIRS identified a clinical sepsis phenotype associated with higher requirements for mechanical ventilation, vasopressors and kidney replacement therapy. The SSqS phenotype which fulfilled all three criteria was associated with higher early to late mortality across all income countries/regions when compared to S phenotype (SOFA only).
The major strength our study was inclusion of prospectively collected data on patients with sepsis from 343 ICUs representing all income regions with minimal missing data and lost to follow up at 90 days. This facilitated granular comparisons on the association of qSOFA with sepsis mortality from different resource settings. This builds on the limited data supporting use of qSOFA for ICU patients in low resource settings which have been studies that were single center, had small sample sizes or included patients who only had suspected sepsis [12, 13, 29]. However, our study also has several limitations. First, because recruitment into MOSAICS II was by SOFA criteria, this study did not include patients who may have sepsis but did not meet Sepsis-3 criteria. Second, MOSAICS II was an epidemiological study and treatment was not protocolized. Third, we assessed all-cause mortality and reasons for early mortality were not documented.
Conclusion
qSOFA was independently associated with 28-day mortality in ICU patients admitted for sepsis. In LLMIC and UMIC countries/regions, qSOFA was associated with early to late mortality but only early mortality in HIC countries/regions. Combination of SOFA, SIRS and qSOFA identified a clinical phenotype of sepsis which is associated with early to late mortality.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):762–74.
Raith EP, Udy AA, Bailey M, McGloughlin S, MacIsaac C, Bellomo R, et al. Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017;317(3):290–300.
Nakayama I, Izawa J, Mouri H, Kitamura T, Shiotsuka J. Mortality and detailed characteristics of pre-ICU qSOFA-negative patients with suspected sepsis: an observational study. Ann Intensive Care. 2018;8(1):44.
Probst L, Schalk E, Liebregts T, Zeremski V, Tzalavras A, von Bergwelt-Baildon M, et al. Prognostic accuracy of SOFA, qSOFA and SIRS criteria in hematological cancer patients: a retrospective multicenter study. J Intensive Care. 2019;7:41.
Savarimuthu SM, Cairns C, Allorto NL, Weissman GE, Kohn R, Wise RD, et al. qSOFA as a predictor of ICU outcomes in a resource-limited setting in KwaZulu-Natal Province, South Africa. South Afr J Crit Care. 2020;36(2):92–5.
Brink A, Alsma J, Verdonschot R, Rood PPM, Zietse R, Lingsma HF, et al. Predicting mortality in patients with suspected sepsis at the emergency department; a retrospective cohort study comparing qSOFA, SIRS and national early warning score. PLoS ONE. 2019;14(1): e0211133.
Freund Y, Lemachatti N, Krastinova E, Van Laer M, Claessens YE, Avondo A, et al. Prognostic accuracy of sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. JAMA. 2017;317(3):301–8.
Jiang J, Yang J, Mei J, Jin Y, Lu Y. Head-to-head comparison of qSOFA and SIRS criteria in predicting the mortality of infected patients in the emergency department: a meta-analysis. Scand J Trauma Resusc Emerg Med. 2018;26(1):56.
Haniffa R, Pubudu De Silva A, Weerathunga P, Mukaka M, Athapattu P, Munasinghe S, et al. Applicability of the APACHE II model to a lower middle income country. J Crit Care. 2017;42:178–83.
Haniffa R, Mukaka M, Munasinghe SB, De Silva AP, Jayasinghe KSA, Beane A, et al. Simplified prognostic model for critically ill patients in resource limited settings in South Asia. Crit Care. 2017;21(1):250.
Khan AM, Aslam SM. Comparison of qSOFA Score, SIRS Criteria, and SOFA Score as predictors of mortality in patients with sepsis. Ghana Med J. 2022;56(3):191–7.
Pairattanakorn P, Angkasekwinai N, Sirijatuphat R, Wangchinda W, Tancharoen L, Thamlikitkul V. Diagnostic and prognostic utility compared among different sepsis scoring systems in adult patients with sepsis in Thailand: a prospective cohort study. Open Forum Infect Dis. 2021;8(1):ofaa573.
Tian H, Zhou J, Weng L, Hu X, Peng J, Wang C, et al. Accuracy of qSOFA for the diagnosis of sepsis-3: a secondary analysis of a population-based cohort study. J Thorac Dis. 2019;11(5):2034–42.
Huson MAM, Katete C, Chunda L, Ngoma J, Wallrauch C, Heller T, et al. Application of the qSOFA score to predict mortality in patients with suspected infection in a resource-limited setting in Malawi. Infection. 2017;45(6):893–6.
Adegbite BR, Edoa JR, Ndzebe Ndoumba WF, Dimessa Mbadinga LB, Mombo-Ngoma G, Jacob ST, et al. A comparison of different scores for diagnosis and mortality prediction of adults with sepsis in Low-and-Middle-Income Countries: a systematic review and meta-analysis. EClinicalMedicine. 2021;42: 101184.
Hu H, Jiang JY, Yao N. Comparison of different versions of the quick sequential organ failure assessment for predicting in-hospital mortality of sepsis patients: a retrospective observational study. World J Emerg Med. 2022;13(2):114–9.
Wright SW, Hantrakun V, Rudd KE, Lau CY, Lie KC, Chau NVV, et al. Enhanced bedside mortality prediction combining point-of-care lactate and the quick Sequential Organ Failure Assessment (qSOFA) score in patients hospitalised with suspected infection in southeast Asia: a cohort study. Lancet Glob Health. 2022;10(9):e1281–8.
Ho KM, Lan NS. Combining quick Sequential Organ Failure Assessment with plasma lactate concentration is comparable to standard Sequential organ failure assessment score in predicting mortality of patients with and without suspected infection. J Crit Care. 2017;38:1–5.
Shetty A, MacDonald SP, Williams JM, van Bockxmeer J, de Groot B, Esteve Cuevas LM, et al. Lactate >/=2 mmol/L plus qSOFA improves utility over qSOFA alone in emergency department patients presenting with suspected sepsis. Emerg Med Australas. 2017;29(6):626–34.
Machado FR, Cavalcanti AB, Monteiro MB, Sousa JL, Bossa A, Bafi AT, et al. Predictive accuracy of the quick sepsis-related organ failure assessment score in Brazil. A prospective multicenter study. Am J Respir Crit Care Med. 2020;201(7):789–98.
Chen FC, Kung CT, Cheng HH, Cheng CY, Tsai TC, Hsiao SY, et al. Quick sepsis-related organ failure assessment predicts 72-h mortality in patients with suspected infection. Eur J Emerg Med. 2019;26(5):323–8.
Li A, Ling L, Qin H, Arabi YM, Myatra SN, Egi M, et al. Epidemiology, management, and outcomes of sepsis in ICUs among countries of differing national wealth across Asia. Am J Respir Crit Care Med. 2022;206(9):1107–16.
World Bank Operational Income Category. World Bank Country and Lending Groups; 2018
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–55.
Do SN, Luong CQ, Nguyen MH, Pham DT, Nguyen NT, Huynh DQ, et al. Predictive validity of the quick Sequential Organ Failure Assessment (qSOFA) score for the mortality in patients with sepsis in Vietnamese intensive care units. PLoS ONE. 2022;17(10): e0275739.
Bishop LA, Wilson DPK, Wise RD, Savarimuthu SM, Anesi GL. Prognostic value of the quick sepsis-related organ failure assessment (qSOFA) score among critically ill medical and surgical patients with suspected infection in a resource-limited setting. Afr J Thorac Crit Care Med. 2021;27(4):145–50.
Rudd KE, Seymour CW, Aluisio AR, Augustin ME, Bagenda DS, Beane A, et al. Association of the quick sequential (Sepsis-Related) Organ Failure Assessment (qSOFA) score with excess hospital mortality in adults with suspected infection in low- and middle-income countries. JAMA. 2018;319(21):2202–11.
Haas B, Wunsch H. How does prior health status (age, comorbidities and frailty) determine critical illness and outcome? Curr Opin Crit Care. 2016;22(5):500–5.
Khwannimit B, Bhurayanontachai R, Vattanavanit V. Comparison of the performance of SOFA, qSOFA and SIRS for predicting mortality and organ failure among sepsis patients admitted to the intensive care unit in a middle-income country. J Crit Care. 2018;44:156–60.
Arabi Y, Al Shirawi N, Memish Z, Venkatesh S, Al-Shimemeri A. Assessment of six mortality prediction models in patients admitted with severe sepsis and septic shock to the intensive care unit: a prospective cohort study. Crit Care. 2003;7(5):R116–22.
Sadaka F, EthmaneAbouElMaali C, Cytron MA, Fowler K, Javaux VM, O’Brien J. Predicting mortality of patients with sepsis: a comparison of APACHE II and APACHE III scoring systems. J Clin Med Res. 2017;9(11):907–10.
Prasad PA, Fang MC, Abe-Jones Y, Calfee CS, Matthay MA, Kangelaris KN. Time to recognition of sepsis in the emergency department using electronic health record data: a comparative analysis of systemic inflammatory response syndrome, sequential organ failure assessment, and quick sequential organ failure assessment. Crit Care Med. 2020;48(2):200–9.
Dykes LA, Heintz SJ, Heintz BH, Livorsi DJ, Egge JA, Lund BC. Contrasting qSOFA and SIRS criteria for early sepsis identification in a veteran population. Fed Pract. 2019;36(Suppl 2):S21–4.
Kilinc Toker A, Kose S, Turken M. Comparison of SOFA Score, SIRS, qSOFA, and qSOFA + L criteria in the diagnosis and prognosis of sepsis. Eurasian J Med. 2021;53(1):40–7.
Williams JM, Greenslade JH, McKenzie JV, Chu K, Brown AFT, Lipman J. 2017 Systemic Inflammatory Response Syndrome Quick Sequential Organ Function Assessment and Organ Dysfunction Insights From a Prospective Database of ED Patients With Infection. Chest. 151(3):586–96.
Gupta R, Arora VK. Performance evaluation of APACHE II score for an Indian patient with respiratory problems. Indian J Med Res. 2004;119(6):273–82.
Aryal D, Thakur A, Gauli B, Paneru HR, Koirala K, Khanal K, et al. Epidemiology of critically ill patients in intensive care units in Nepal. Wellcome Open Research. 2023;8:180.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29.
Finkelsztein EJ, Jones DS, Ma KC, Pabon MA, Delgado T, Nakahira K, et al. Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit. Crit Care. 2017;21(1):73.
Costa RT, Nassar AP Jr, Caruso P. Accuracy of SOFA, qSOFA, and SIRS scores for mortality in cancer patients admitted to an intensive care unit with suspected infection. J Crit Care. 2018;45:52–7.
Acknowledgements
MOSAICS II Study Group: The study sites and investigators who contributed to recruitment and data collection are listed in Appendix 1, Additional file 3.
Funding
This was not a funded study.
Author information
Authors and Affiliations
Consortia
Contributions
AL and LL designed the study. AL, LL, HQ, YMA, SNN, ME, JEK, MBMN, DNS, WF, BW, MH, MOF, BP, MJAB, BRS, US, KMKN, KKS, JEMP, NM, AK, KD, YHC, BD, JVD, YK, CD, JP and other MOSCAICS II investigators collected the data. LL performed the data analysis. AL and LL wrote the first draft of the manuscript. All authors provided critique of the manuscript and approved it for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The National Healthcare Group Domain-Specific Review Board approved the study (2018/00354), with a waiver informed consent as this was an observational study. In addition this study was approved by institutional review boards according to local regulations at participating ICUs, with most waiving the need for informed consent.
Competing interest
All authors declare no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary Figures 1–6.
Additional file 2.
Supplementary Tables 1–12.
Additional file 3.
Appendix 1: Contributing centers listed alphabetically per country/region with Lead Investigators and Co-Investigators.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, A., Ling, L., Qin, H. et al. Prognostic evaluation of quick sequential organ failure assessment score in ICU patients with sepsis across different income settings. Crit Care 28, 30 (2024). https://doi.org/10.1186/s13054-024-04804-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-024-04804-7