Abstract
Introduction
We conducted the present study to assess the validity of mortality prediction systems in patients admitted to the intensive care unit (ICU) with severe sepsis and septic shock. We included Acute Physiology and Health Evaluation (APACHE) II, Simplified Acute Physiology Score (SAPS) II, Mortality Probability Model (MPM) II0 and MPM II24 in our evaluation. In addition, SAPS II and MPM II24 were customized for septic patients in a previous study, and the customized versions were included in this evaluation.
Materials and method
This cohort, prospective, observational study was conducted in a tertiary care medical/surgical ICU. Consecutive patients meeting the diagnostic criteria for severe sepsis and septic shock during the first 24 hours of ICU admission between March 1999 and August 2001 were included. The data necessary for mortality prediction were collected prospectively as part of the ongoing ICU database. Predicted and actual mortality rates, and standardized mortality ratio were calculated. Calibration was assessed using Lemeshow–Hosmer goodness of fit C-statistic. Discrimination was assessed using receiver operating characteristic curves.
Results
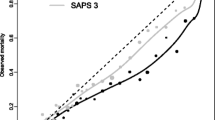
The overall mortality prediction was adequate for all six systems because none of the standardized mortality ratios differed significantly from 1. Calibration was inadequate for APACHE II, SAPS II, MPM II0 and MPM II24. However, the customized version of SAPS II exhibited significantly improved calibration (C-statistic for SAPS II 23.6 [P = 0.003] and for customized SAPS II 11.5 [P = 0.18]). Discrimination was best for customized MPM II24 (area under the receiver operating characteristic curve 0.826), followed by MPM II24 and customized SAPS II.
Conclusion
Although general ICU mortality system models had accurate overall mortality prediction, they had poor calibration. Customization of SAPS II and, to a lesser extent, MPM II24 improved calibration. The customized model may be a useful tool when evaluating outcomes in patients with sepsis.
Similar content being viewed by others
Introduction
Severe sepsis and septic shock are major reasons for intensive care unit (ICU) admission and leading causes of mortality in noncoronary ICUs [1–3]. Apart from in the West, little is known about outcomes of patients admitted to the ICU with severe sepsis and septic shock, despite the seriousness of sepsis as a public health problem in developing countries. According to the 1996 World Health Organization Health Report [4], infectious and parasitic diseases caused 17 million out of 50 million deaths globally, including 3.4 million deaths from acute lower respiratory infections, 3 million from tuberculosis, 2.5 million from diarrhoeal diseases, 1.5–2.7 million from malaria and 1.5 million from HIV/AIDS. Infectious and parasitic diseases accounted for 43% of the 40 million deaths occurring in the developing countries in 1996.
With increasing international travel and the trend toward globalization, an international perspective on the outcome following sepsis is becoming increasingly important. The Kingdom of Saudi Arabia has some unique features in this regard. First, the Kingdom hosts the annual Islamic pilgrimage (Hajj), when 2 million Muslims from more than 100 countries gather in Makkah [5]. Many of these pilgrims are elderly with underlying chronic illnesses, making them especially susceptible to infectious illnesses. Second, the health care system in the Kingdom grew rapidly to state-of-the-art levels over the past two decades, and this development has brought with it the challenges that face modern medicine, including transplantation complications, cancer therapy and advanced surgery.
Understanding sepsis outcome studies is hampered by two factors. First is the inconsistency in the definition of sepsis. This led to a consensus statement that defined systemic inflammatory response syndrome (SIRS), sepsis, severe sepsis and septic shock [6]. More recently, these definitions were revisited; the concept of SIRS was challenged, and the definitions of sepsis, severe sepsis and septic shock were maintained [7]. The second factor was the lack of an agreed severity of illness scoring system for sepsis patients. In the absence of such a system, it would be difficult to interpret sepsis outcome studies [8]. Mortality prediction systems have been introduced as tools for assessing the performance of ICUs [9–12]. Some of these systems have been customized for patients with specific conditions such as sepsis, and liver transplantation and long-stay ICU patients [13, 14]. If these systems are proved to predict accurately mortality in severe sepsis and septic shock, then they will have the advantage of being readily available and easily incorporated into general ICU databases without additional data collection. Customized versions of SAPS II and MPM II24 for septic patients were introduced by the European–North American Study of Severity Systems [15]. That study included 1130 patients who met the criteria for severe sepsis.
The objective of the present study is to assess the validity of six mortality prediction systems for the severe sepsis and septic shock patient population. This was, to our knowledge, the first study of its kind to be conducted on an independent database. It is also the first study to describe the outcome of severe sepsis and septic shock using standardized definitions in a non-Western country.
Materials and method
King Fahad National Guard Hospital is a 550-bed tertiary care teaching centre in Riyadh, Saudi Arabia. It is a transplant centre, and it therefore receives a large number of referrals of patients with end-stage liver disease. The 21-bed medical/surgical ICU has 700–800 admissions per year and is run by full-time, on-site, board-certified intensivists. The ICU database was established in March 1999 to record all ICU admissions. We included information on all consecutive admissions between 1 March 1999 and 31 August 2001 meeting the definitions of severe sepsis and septic shock in the first 24 hours of ICU admission. Severe sepsis is defined as the presence of sepsis associated with organ dysfunction. Septic shock is defined as sepsis-induced hypotension and perfusion abnormalities despite fluid resuscitation, necessitating vasopressor support. At the time of the study, these definitions were based on the 1992 American College of Chest Physicians and Society of Critical Care Medicine consensus statement [6]. In the more recent statement, published in 2003 [7], the definition of SIRS was challenged and was replaced by new diagnostic criteria. The definitions of severe sepsis and septic shock were maintained, as mentioned above. Therefore, the new definitions do not affect our patient population.
Patients younger than 16 years, and burn and brain-dead patients were excluded. For patients admitted to the ICU more than once during a hospitalization episode, only data from the first admission were used. Approval from the hospital ethics committee was not required because the information was already being collected for clinical purposes. The following data were collected: demographics, Acute Physiology and Chronic Health Evaluation (APACHE) II scores, Simplified Acute Physiology Score (SAPS) II scores, and Mortality Probability Model (MPM) variables. MPM II0 data were obtained for all admissions, whereas MPM II24, APACHE II and SAPS II data were obtained in patients who stayed 24 hours or longer in the ICU. The original methodology for data collection was followed [10–12, 15]. The main reason for ICU admission, whether the admission was following emergency surgery, and the presence of severe chronic illness were documented according to the definitions used in the original APACHE II article [10]. Severe chronic illnesses included cirrhosis, New York Heart Association class IV heart failure, chronic respiratory failure, end-stage renal disease and immunosuppression. ICU and hospital duration of stay, and vital status at discharge both from the ICU and from the hospital was documented. Hospital mortality is used as the primary end-point for all mortality predictions.
Statistics
Predicted mortality was calculated using the logistic regression formulae described in the original articles [10–12, 15]. The formula used for calculation of predicted mortality in the customized SAPS II system is as follows:

where β0 is -3.5524 and β1 is 0.0694.
A similar approach was used in calculating predicted mortality for the customized MPM II24:

where β0 is 0.0157 and β1 is 0.7971 [15].
Standardized mortality ratio (SMR) was calculated by dividing observed mortality by the predicted mortality. The 95% confidence intervals for SMRs were calculated using the observed mortality as a Poisson variable, and then dividing its 95% confidence interval by the predicted mortality [16].
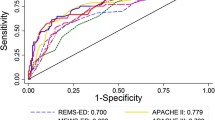
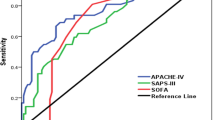
System validation was tested by assessing both calibration and discrimination values. Calibration (the ability to provide a risk estimate that corresponds to the observed mortality) was assessed using Lemeshow–Hosmer goodness of fit C-statistics [17]. In order to calculate the C-statistic, the study population was divided into 10 groups of approximately equal numbers of patients. The predicted and actual number of survivors and nonsurvivors were compared statistically using formal goodness of fit testing to determine whether the discrepancy between predicted and actual values was statistically insignificant (P > 0.05). Discrimination was tested using receiver operating characteristic (ROC) curves. ROC curves were constructed using 10% stepwise increments in predicted mortality [18, 19]. A comparison of the six curves was done by computing the areas under the ROC curves.
Continuous variables were expressed as means ± standard deviation and were compared using standard t-test. Categorical values were expressed in absolute and relative frequencies, and were analyzed using χ2 test. P ≤ 0.05 was considered statistically significant.
Results
Demographics
During the period of study 250 patients met the diagnostic criteria for severe sepsis/septic shock in the first 24 hours of ICU admission. Demographic data for these patients are summarized in Table 1. Of note is the high proportion of patients (54.80%) with underlying chronic illness. ICU mortality was 46% (115 patients) and hospital mortality was 61% (152 patients). The differences between hospital survivors and nonsurvivors are also shown. Nonsurvivors were older, had higher APACHE II and SAPS II scores, had shorter hospital duration of stay and were more likely to have chronic illnesses, especially liver disease and immunosuppression. The most common source of infection was the respiratory system (41%), followed by abdominal (32%) and then urinary (17%) sites. A total of 93 patients (37%) had positive blood cultures, with Gram-negative bacilli being the most common (53 patients [57%]), followed by Gram-positive cocci (36 patients [39%]) and fungi (3 patients [3%]), and Gram-negative cocci (1 patient [1%]).
Predicted mortalities
Table 2 shows actual and predicted hospital mortality for each of the six prediction systems. There was no significant difference between the SMR for any of the systems and 1, as evident from the confidence intervals; this indicates that all the six systems gave overall accurate mortality estimates.
Calibration
Calibration, as tested by C-statistics, was poor for the four standard ICU mortality prediction systems (C-statistics: MPM II0 29.79 [P < 0.001]; MPM II24 24.82 [P = 0.002]; APACHE II 34.89 [P < 0.001]; SAPS II 23.60 [P = 0.003]). Customization of SAPS II and MPM II24 was associated with improvement in calibration, but this was statistically adequate only for customized SAPS II (C-statistic 11.48 [P = 0.18]; Table 3).
Discrimination
The ROC curves are shown in Fig. 1. The corresponding areas under the ROC curves were as follows (in descending order to reflect decreasing levels of discrimination): customized MPM II24 0.826; MPM II24 0.823; MPM II0 0.806; customized SAPS II 0.799; SAPS II 0.797; and APACHE II 0.782.
Discussion
The main findings of this study can be summarized as follows. First, the overall mortality prediction for all six systems was accurate, as reflected by the SMRs. Second, calibration was inadequate for the general (noncustomized) systems and was improved by customization, particularly for the SAPS II. Third, discrimination was good for all systems, especially for the customized versions.
Mortality risk stratification in severe sepsis and septic shock is commonly used in clinical trials and in practice [20], which helps to improve accuracy when evaluating new therapies and refining indications. By facilitating comparison of the actual with predicted mortalities, the use of such systems can also provide valuable information about the performance of individual ICUs in treating septic patients.
Several approaches in risk stratification have been utilized, including the use of severity of illness scoring systems and the use of certain inflammatory markers (e.g. interleukin-1, interleukin-6, tumour necrosis factor-α) [20]. The use of illness severity systems has several advantages, including their relative simplicity and wide availability. However, there is as yet no ideal system for this group of patients. Most of the systems were developed for general ICU patients, and when applied to a particular group of patients, such as those with sepsis, their accuracy declines. Customization of these systems to predict sepsis outcome is an attractive option. Compared with the introduction of a system specific to sepsis, the customized versions require little if any extra data collection by units already using general ICU systems.
There are several advantages to having an internationally valid mortality prediction system for patients with severe sepsis and septic shock. First, it would be useful in comparing the outcomes of such patients between different ICUs and countries. In research it would help by grouping patients in a clinical trial – an approach used recently in the Recombinant human protein C Worldwide Evaluation in Severe Sepsis (PROWESS) trial [21, 22]. The use of these systems will be of particular value when conducting large international multicentre studies.
There is a good body of literature addressing ICU outcomes of septic patients in Western ICUs, including USA [3], France [23], Italy [24], and the UK [25]. However, apart from in the West, very little is reported in this field, despite the seriousness of sepsis as a public health problem in these countries. The present study sheds some light on ICU outcomes of patients admitted with severe sepsis and septic shock in a Middle Eastern country.
Our study has the strength of being prospective, using standardized definitions of severe sepsis and septic shock. The study also has some limitations. First, it was conducted at only one centre. The results therefore reflect the outcome of septic patients in a tertiary care centre and they may not be generalizeable to all hospitals in the country. However, the study gives some insight into this issue, at least from a tertiary care perspective.
In conclusion, the present study shows that customized version of SAPS II (and to lesser extent the customized MPM II24) performed well in predicting mortality in patients with severe sepsis and septic shock. As such, the customized versions are better options for mortality prediction in septic patients than are the general ICU mortality prediction systems.
Abbreviations
- APACHE:
-
= Acute Physiology and Chronic Health Evaluation
- ICU:
-
= intensive care unit
- MPM:
-
= Mortality Probability Model
- ROC:
-
= receiver operating characteristic
- SAPS:
-
= Simplified Acute Physiology Score
- SIRS:
-
= systemic inflammatory response syndrome
- SMR:
-
= standardized mortality ratio.
References
Rangel-Frausto MS: The epidemiology of bacterial sepsis. Infect Dis Clin North Am. 1999, 13: 299-312.
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR: Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001, 29: 1303-1310. 10.1097/00003246-200107000-00002.
Angus DC, Wax RS: Epidemiology of sepsis: an update. Crit Care Med. 2001, suppl: S109-S116. 10.1097/00003246-200107001-00035.
The World Health Orgnization: The world health report archives 1995–2000. [http://www.who.int/whr/2001/archives/1997/factse.htm]
Memish ZA, Ahmed QA: Mecca bound: the challenges ahead. J Travel Med. 2002, 9: 202-210.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ: American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992, 101: 1644-1655.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G: 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003, 31: 1250-1256. 10.1097/01.CCM.0000050454.01978.3B.
Friedman G, Silva E, Vincent JL: Has the mortality of septic shock changed with time?. Crit Care Med. 1998, 26: 2078-2086. 10.1097/00003246-199812000-00045.
Lemeshow S, Le Gall Jr: Modeling the severity of illness of ICU patients. JAMA. 1994, 272: 1049-1055. 10.1001/jama.272.13.1049.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE: APACHE II. A severity of disease classification system. Crit Care Med. 1985, 13: 818-829.
Le Gall J-R, Lemeshow S, Saulnier F: A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multi center study. JAMA. 1993, 270: 2957-2962. 10.1001/jama.270.24.2957.
Lemeshow S, Teres D, Klar J, Avrunin JS, Gehlbach SH, Rapoport J: Mortality Probability Models (MPM II) based on an international cohort of intensive care unit patients. JAMA. 1993, 270: 2478-2486. 10.1001/jama.270.20.2478.
Suistomaa M, Niskanen M, Kari A, Hynynen M, Takala J: Customized prediction models based on APACHE II and SAPS II scores in patients with prolonged length of stay in the ICU. Intensive Care Med. 2002, 28: 479-485. 10.1007/s00134-002-1214-9.
Angus DC, Clermont G, Kramer DJ, Linde-Zwirble WT, Pinsky MR: Short-term and long-term outcome prediction with the Acute Physiology and Chronic Health Evaluation II in System after orthotopic liver transplantation. Crit Care Med. 2000, 28: 150-156. 10.1097/00003246-200001000-00025.
LeGall JR, Lemeshow S, Leleug , Klar J, Huillard J, Rui M, Teres D, Artigas A: Customized probability models for early severe sepsis in adult intensive care patients. JAMA. 1995, 273: 644-650.
Goldhill DR, Sumner A: Outcome of intensive care patients in a group of British intensive care units. Crit Care Med. 1998, 26: 1337-1345. 10.1097/00003246-199808000-00017.
Lemeshow S, Hosmer DW: A Review of goodness of fit statistics for use in the development of logistic regression models. Am J Epidemiol. 1982, 115: 92-106.
Metz CE: Basic Principles of ROC analysis. Semin Nucl Med. 1978, 8: 283-298.
Hanley JA, McNeil BJ: The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982, 143: 29-36.
Barriere SL, Lowry SF: An overview of mortality risk prediction in sepsis. Crit Care Med. 1995, 23: 376-393. 10.1097/00003246-199502000-00026.
Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD, Ely EW, Fisher CJ: Recombinant human protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study group. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001, 344: 699-709. 10.1056/NEJM200103083441001.
Warren HS, Suffredini AF, Eichacker PQ, Munford RS: Risks and benefits of activated protein C treatment for severe sepsis. N Eng J Med. 2002, 347: 1027-1030. 10.1056/NEJMsb020574.
Brun-Buisson C, Doyon F, Carlet J, Dellamonica P, Gouin F, Lep-outre A, Mercier JC, Offenstadt G, Regnier B: Incidence, risk factors, and outcome of severe sepsis and septic shock in adults. A multicenter prospective study in intensive care units. French ICU Group for Severe Sepsis. JAMA. 1995, 274: 968-974. 10.1001/jama.274.12.968.
Salvo I, de Cian W, Musicco M, Langer M, Piadena R, Wolfler A, Montani C, Magni E: The Italian SEPSIS study: preliminary results on the incidence and evolution of SIRS, sepsis, severe sepsis and septic shock. Intensive Care Med. 1995, suppl 2: S244-S249.
Edbrooke DL, Hibbert CL, Kingsley JM, Smith S, Bright NM, Quinn JM: The patient-related costs of care for sepsis patients in a United Kingdom adult general intensive care unit. Crit Care Med. 1999, 27: 1760-1767. 10.1097/00003246-199909000-00010.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Arabi, Y., Shirawi, N.A., Memish, Z. et al. Assessment of six mortality prediction models in patients admitted with severe sepsis and septic shock to the intensive care unit: a prospective cohort study. Crit Care 7, R116 (2003). https://doi.org/10.1186/cc2373
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc2373