Abstract
Background
There is no consensus exists regarding the association between oxygen exposure (arterial oxygen tension or fraction of inspired oxygen) and outcomes for patients with mechanical ventilation. Additionally, whether the association remains persistent over time is unknown. We aimed to explore the association between exposure to different intensities of oxygen exposure over time and 28-day mortality in patients with mechanical ventilation.
Methods
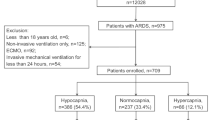
We obtained data from the Medical Information Mart for Intensive Care IV (MIMIC-IV), which included adult (≥ 18 years) patients who received invasive mechanical ventilation for at least 48 h. We excluded patients who received extracorporeal membrane oxygenation (ECMO) or who initiated ventilation more than 24 h after ICU admission. The primary outcome was 28-day mortality. Piece-wise exponential additive mixed models were employed to estimate the strength of associations over time.
Results
A total of 7784 patients were included in the final analysis. Patients had a median duration of invasive mechanical ventilation of 8.1 days (IQR: 3.8–28 days), and the overall 28-day mortality rate was 26.3%. After adjustment for baseline and time-dependent confounders, both daily time-weighted average (TWA) arterial oxygen tension (PaO2) and fraction of inspired oxygen (FiO2) were associated with increased 28-day mortality, and the strength of the association manifested predominantly in the early-middle course of illness. A significant increase in the hazard of death was found to be associated with daily exposure to TWA-PaO2 ≥ 120 mmHg (Hazard ratio 1.166, 95% CI 1.059–1.284) or TWA-FiO2 ≥ 0.5 (Hazard ratio 1.496, 95% CI 1.363–1.641) during the entire course. A cumulative effect of harmful exposure (TWA-PaO2 ≥ 120 mmHg or TWA-FiO2 ≥ 0.5) was also observed.
Conclusion
PaO2 and FiO2 should be carefully monitored in patients with mechanical ventilation, especially during the early-middle course after ICU admission. Cumulative exposure to higher intensities of oxygen exposure was associated with an increased risk of death.
Similar content being viewed by others
Introduction
The administration of supplemental oxygen is a standard treatment in mechanically ventilated patients in Intensive Care Units (ICU). Oxygen therapy can reverse tissue hypoxia and can be lifesaving on many occasions, while its overzealous use might result in hyperoxemia with supraphysiological levels of the arterial oxygen tension (PaO2) [1]. Additionally, most patients with mechanical ventilation frequently required a higher fraction of inspired oxygen (FiO2) to maintain an adequate PaO2.
PaO2 and FiO2 outside the normal physiological range can be detrimental and exacerbate systemic organ injury in critically ill patients [2,3,4,5], while numerous studies provided conflicting evidence concerning the impact of PaO2 and FiO2 on clinical outcomes of critically ill patients [6,7,8,9,10]. The cut-off values of PaO2 and FiO2 associated with increased risk of death were various, and still uncertain. Meanwhile, previous studies focused on only the association between PaO2 or FiO2 during the early onset of illness and mortality, usually within 24 h after ICU admission, and many of these studies are limited by using only a single measure of PaO2 or FiO2 to define oxygen exposure for entire ICU admission. Whether the association between time-varying oxygen exposure and mortality is significant and remains persistent over time is unknown. Besides, high FiO2 can increase PaO2 and impair lung tissues simultaneously [11, 12], while the direct and indirect effects (mediated by hyperoxemia) of high FiO2 on mortality in the real world have never been explored.
Therefore, our primary objective was to estimate the effect of time-varying exposure to different intensities of oxygen exposure (as measured either by PaO2 or FiO2) on 28-day mortality in patients with mechanical ventilation. We also examined whether the strength of the effect changed over time, and whether there was a cumulative effect of exposure over time. Finally, we aimed to identify the direct and indirect effects of high FiO2 on mortality.
Methods
Study design and participants
We conducted a retrospective cohort study using electronic health records data from the Medical Information Mart for Intensive Care IV (MIMIC-IV) [13]. The MIMIC-IV database contains comprehensive and high-quality data of well-defined and characterized ICU patients admitted to ICUs at the Beth Israel Deaconess Medical Center between 2008 and 2019. One author (HC) obtained access to the database and was responsible for data extraction (certification number 27252652). Our study complied with the Reporting of Studies Conducted using Observational Routinely Collected Health Data (RECORD) statement.
All patients in the MIMIC-IV who received invasive mechanical ventilation were eligible for inclusion in the present study. The exclusion criteria included (1) Patients who were younger than 18 years; (2) Patients ventilated for less than 48 h; (3) Patients who received extracorporeal membrane oxygenation (ECMO); (4) Patients who initiated ventilation more than 24 h after ICU admission. Additionally, we analyzed only the first ICU stay for patients who were admitted to the ICU more than once.
Variable extraction
We collected age, sex, weight, height, ethnicity, admission type, and severity at admission, as measured by the Sequential Organ Failure Assessment (SOFA) score, the Simplified Acute Physiology Score II (SAPS II), and Oxford Acute Severity of Illness Score (OASIS). Comorbidities were also collected to calculate the Elixhauser comorbidity score. Initial diagnoses were extracted according to the recorded ICD-9 and ICU-10 codes in the database. Longitudinal data including SOFA score, blood gas, ventilation parameters, and laboratory measurements were collected for each 24 h. If a variable was recorded more than once in the 24 h, we used the value related to the greatest severity of illness. Specifically, PaO2 and FiO2 were extracted per each time frame of 4 h after ICU admission. For each 24 h, the time-weighted average (TWA) PaO2 or FiO2 was calculated as the area under the PaO2 or FiO2 versus the time plot. All included patients were followed up from inclusion until death, ICU discharge, or 28 days in the ICU, whichever occurred first.
Exposures and outcomes
The primary exposures in the present study were time-varying TWA-PaO2 and TWA-FiO2. Since our research indicated that there is a consistent increase in the risk of death with TWA-PaO2 higher than or equal to 120 mmHg and TWA-FiO2 higher than or equal to 0.5, we defined hyperoxemia and high FiO2 as TWA-PaO2 ≥ 120 mmHg, and TWA-FiO2 ≥ 0.5, respectively, and employed three approaches to quantifying the effect of harmful exposure: (1) Any exposure to hyperoxemia or high FiO2 during the entire course of ICU admission; (2) The proportion of time spent in hyperoxemia or high FiO2; (3) The area under the longitudinal profiles for either TWA-PaO2 of 120 mmHg or more, or TWA-FiO2 of 0.5 or more.
The primary outcome was 28-day mortality. Secondary outcomes included in-hospital mortality, ventilation-free days (VFDs) in 28 days, length of ICU, and hospital stay. Patients who died before day 28 were considered to have zero VFDs.
Statistical analysis
Values are presented as the mean (standard deviation) or median [interquartile range (IQR)] for continuous variables as appropriate and as the total number (percentage) for categorical variables. Comparisons between groups were made using the X2 test or Fisher’s exact test for categorical variables and Student’s t test or Mann–Whitney U test for continuous variables as appropriate.
We first used piece-wise exponential additive mixed models (PAMMs) [14,15,16] to estimate the association of subject-specific longitudinal profiles of either TWA-PaO2 or TWA-FiO2 with 28-day mortality. PAMMs allow one to examine the time-varying effect of a time-varying exposure (time-varying TWA-PaO2 or TWA-FiO2 in the present study) on a time-to-event outcome (Additional file 1). Based on prior knowledge, baseline variables were purposefully selected to be used in the PAMMs as time-fixed confounders and included age, gender, admission type, weight, and Elixhauser comorbidity score. Considering that the confounders may change over time during the follow-up period, and that the effect of such confounders on outcomes is time-varying, we treated longitudinal data including the use of mechanical ventilation and vasopressor, SOFA score, and PaCO2 during follow-up as time-varying confounders in the PAMMs. To investigate whether the association between TWA-PaO2 or TWA-FiO2 and 28-day mortality changed over time, we included an interaction term with time and exposures in the model. To avoid bias induced by missing data, we used multiple imputations by chained equation (MICE) to account for the missing data.
We identified the approximate PaO2 and FiO2 threshold above which the risk of 28-day mortality began to increase based on PAMMs. And then, three secondary analyses were performed. We included any hyperoxemia or high FiO2 as time-varying exposure variables and explored the impact of any exposure to hyperoxemia or high FiO2 on mortality; we also estimated the association between the proportion of time spent in harmful exposure (TWA-PaO2 ≥ 120 mmHg or TWA-FiO2 ≥ 0.5) and mortality. Furthermore, we investigated the relationship between cumulative dose and 28-day mortality using the area under the longitudinal profiles for either TWA-PaO2 of 120 mmHg or more, or TWA-FiO2 of 0.5 or more.
Based on the additive hazards model, we conduct a causal mediation analysis (CMA) to explore whether the effect of time-varying high FiO2 (TWA-FiO2 ≥ 0.5) on the primary outcome is mediated by the time-varying hyperoxemia. The additive hazards model allows for a time-varying mediator in survival analysis [17]. CMA separates the total effect of exposure into direct and indirect effects. The indirect impact on the outcome is mediated via a mediator. Our study used time-varying high FiO2 as a harmful exposure and time-varying hyperoxemia as a mediator variable.
Several subgroup analyses were performed according to exposure window (up to 3 days, 5 days, 7 days, 14 days, and 21 days), admission type, gender, and initial diagnosis. Since patients could liberate from mechanical ventilation during the follow-up period, we duplicated the analysis after changing the follow-up period. Specifically, patients were followed up from inclusion until death, liberated from mechanical ventilation, ICU discharge, or 28 days in the ICU, whichever occurred first. We also conducted sensitivity analyses after excluding missing values of daily TWA-PaO2 or TWA-FiO2 during follow-up.
All statistical analyses were performed using R (version 4.0.3), and p < 0.05 was considered statistically significant.
Results
Patients in study
After reviewing the data of 29,119 patients with mechanical ventilation, a total of 7784 patients were included in the final analysis. The flow diagram of patient selections is presented in Additional file 2: Figure S1. Baseline characteristics are shown in Table 1. The patients had a median age of 65.0 years (IQR: 54.0–76.0), and 57.2% of them were men. Of the study cohort, 89.5% of patients had sepsis and 50.6% had acute respiratory failure. Patients had a median duration of invasive mechanical ventilation of 8.1 days (IQR: 3.8–28) and the overall 28-day mortality rate was 26.3%.
A total of 6544 (84.1%) patients had complete data of TWA-PaO2 on Day 1, and 58.1% of patients were exposed to hyperoxemia (TWA-PaO2 ≥ 120 mmHg), while 7778 (99.9%) patients had complete data of TWA-FiO2 on Day 1, and 52.7% of patients were exposed to TWA-FiO2 ≥ 0.5. There were lots of differences in patient characteristics and outcomes based on their level of TWA-PaO2 (Additional file 2: Table S1) and TWA-FiO2 (Additional file 2: Table S2) on Day 1.
Primary analysis
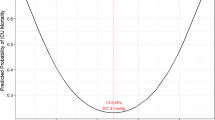
Based on the PAMMs, we identified a U-shaped relationship between time-varying TWA-PaO2 or TWA-FiO2 (Figs. 1 and 2) and the risk of 28-day mortality. There was a consistent increase in the risk of death with TWA-PaO2 higher than or equal to 120 mmHg and TWA-FiO2 higher than or equal to 0.5 (Figs. 1A and 2A). After adjusting for age, gender, admission type, weight, Elixhauser comorbidity score, use of mechanical ventilation, use of vasopressor, SOFA score, and PaCO2, both the time-varying TWA-PaO2 (Hazard ratio (HR) per 5 mmHg 1.801, 95% CI 1.585–2.046) and TWA-FiO2 (HR per 0.05 2.688, 95% CI 2.407–3.002) were associated with an increased risk of 28-day mortality (Additional file 2: Table S3).
Association between daily TWA-PaO2 and 28-day mortality over time using piece-wise exponential additive mixed models. A Adjusted relationship between TWA-PaO2 over time and 28-day mortality; B Adjusted relationship between TWA-PaO2 over time and 28-day mortality stratified by exposure window; C Time-varying effect of TWA-PaO2 on 28-day mortality; D Time-varying effect of TWA-PaO2 on 28-day mortality stratified by level of PaO2. TWA: Time-weighted average; PaO2: Arterial oxygen tension
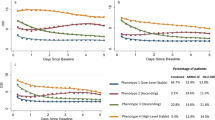
Association between daily TWA-FiO2 and 28-day mortality over time using piece-wise exponential additive mixed models. A Adjusted relationship between TWA-FiO2 over time and 28-day mortality; B Adjusted relationship between TWA-FiO2 over time and 28-day mortality stratified by exposure window; C Time-varying effect of TWA-FiO2 on 28-day mortality; D Time-varying effect of TWA-FiO2 on 28-day mortality stratified by level of FiO2. TWA: Time-weighted average; FiO2: Fraction of inspired oxygen
The strength of the association between the intensity of oxygen exposure (as measured by either TWA-PaO2 or TWA-FiO2) and 28-day mortality was not persistent across the entire course of ICU admission (Additional file 2: Figure S2). TWA-PaO2 significantly impacts mortality in the early-middle course of illness (approximately 4–12 days after ICU admission) (Fig. 1C), regardless of the level of TWA-PaO2 (Fig. 1D). While the impacts of TWA-FiO2 predominantly in the early-middle course of illness (approximately 4–16 days after ICU admission) (Fig. 2C), and for the high level of TWA-FiO2, the impact on mortality remained persistent across the entire course of ICU admission (Fig. 2D).
Secondary analysis
Three secondary analyses were performed after we identified the approximate PaO2 and FiO2 threshold above which the risk of 28-day mortality began to increase. First, PAMMs demonstrated that both time-varying hyperoxemia (HR 1.166, 95% CI 1.059–1.284) and high FiO2 (HR 1.496, 95% CI 1.363–1.641) were associated with an increased risk of 28-day mortality (Table 2). Likewise, both the proportion of time spent in hyperoxemia (HR per 5% 1.412 95% CI 1.302–1.531) and high FiO2 (HR per 5% 1.284, 95% CI 1.204–1.369) significantly impact mortality (Additional file 2: Table S4 and Fig. 3). Third, a higher cumulative dose of the potentially injurious intensity of oxygen exposure was associated with an increased hazard of death for hyperoxemia (HR 1.0014, 95% CI 1.001–1.0017) and high FiO2 (HR 1.003, 95% CI 1·0023–1.0036) (Additional file 2: Table S5).
Causal mediation analysis
Any exposure to hyperoxemia (TWA-PaO2 ≥ 120 mmHg) was significantly associated with the 28-day mortality in patients with TWA-FiO2 ≥ 0.5 (HR 1.203, 95% CI 1.088–1.331), but not in patients with TWA-FiO2 < 0.5 (HR 1.056, 95% CI 0.760–1.469). Meanwhile, the association between any exposure to TWA-FiO2 ≥ 0.5 and 28-day mortality was significant both in patients with hyperoxemia (HR 1.60, 95% CI 1.40–1.874) and non-hyperoxemia (HR 1.556, 95% CI 1.389–1.742). To explore whether the effect of time-varying high FiO2 (TWA-FiO2 ≥ 0.5) on the primary outcome was mediated by the time-varying hyperoxemia. We treated time-varying high FiO2 as a harmful exposure and time-varying hyperoxemia as a mediator variable, and visual inspection showed that both the direct effect of high FiO2 (p < 0.001) and an indirect effect via hyperoxemia (p < 0.001) on mortality were significant (Fig. 4).
The direct effect and indirect effect of high FiO2 on 28-day mortality over time using the additive hazards model. A Direct effect of high FiO2 on 28-day mortality over time; B Indirect effect (mediated by hyperoxemia) of high FiO2 on 28-day mortality over time; C Total effect of high FiO2 on 28-day mortality over time
Subgroup analyses and sensitivity analyses
Subgroup analyses of the association between time-varying hyperoxemia and high FiO2 with 28-day mortality are shown in Fig. 5. Accomplished by the increase in exposure window, the hazard of death for hyperoxemia was decreased, while the hazard of death for high FiO2 was persistent. Two sensitivity analyses were performed. First, after excluding missing values of daily TWA-PaO2 or TWA-FiO2, any exposure to hyperoxemia (HR 1.232, 95% CI 1.059–1.435) or high FiO2 (HR 1.744, 95% CI 1.355–2.245) was associated with an increased risk of 28-day mortality (Additional file 2: Table S6). Second, we changed the follow-up period to ensure all patients were ventilated during follow-up and found that hyperoxemia was associated with a 1.207-fold increase risk of death (HR 1.207, 95% CI 1.098–1.327), while high FiO2 was associated with 1.242-fold increase risk of death (HR 1.242, 95% CI 1.133–1.363) (Additional file 2: Table S7).
Discussion
Time-varying intensity of oxygen exposure, as measured by daily TWA-PaO2 or TWA-FiO2, was associated with the increased 28-day mortality for patients with mechanical ventilation, and the strength of the association manifested predominantly in the early-middle course of illness. Importantly, we observed a cumulative effect of harmful exposure (TWA-PaO2 ≥ 120 mmHg or TWA-FiO2 ≥ 0.5) over time. The impact of high FiO2 on mortality was partly mediated by hyperoxemia, meanwhile, high FiO2 can also impact mortality directly.
Our findings that oxygen exposure is associated with mortality is generally in accordance with the results of previous studies [6, 18, 19], although some differences exist. First, the assessment period of oxygen exposure was different. Prior retrospective studies exploring the association between oxygen exposure and outcome are limited by using a single measure of PaO2 or FiO2, usually taken within 24 h after ICU admission. It is biologically implausible that a single measure of oxygen exposure could shift outcomes so dramatically. To address this limitation, we evaluated the oxygen exposure throughout the entire course of ICU admission (up to 28 days) and treated daily oxygen exposure as a time-varying exposure in PAMMs to explore the time-varying effects over time. Second, the threshold to define hyperoxemia and high FiO2 varied in previous studies, the threshold ranges from 100 to 200 mmHg for hyperoxemia and 0.5–1.0 for high FiO2 [20, 21], which simply from an empirical or biological standpoint, and remains unclear whether these values could provide the best measure to elucidate harm. From another aspect, we identified the PaO2 and FiO2 threshold above which the risk of 28-day mortality began to increase. Third, in previous observational studies, the multivariable regression model only adjusted for baseline confounders, which could lead to residual confounders, such as the postbaseline time-dependent patient differences. The difference in present study is that we employed PAMMs to account for both baseline and time-dependent confounders.
We visualized the longitudinal association between TWA-PaO2 or TWA-FiO2 and 28-day mortality throughout the entire course of ICU admission and suggested that clinicians should pay more attention to PaO2 and FiO2 during the early-middle course of illness (approximately 4–16 days after ICU admission). While for the high level of FiO2, the impact on mortality was persistent over time. Visual inspection showed that the optimum range for PaO2 was approximately 80–120 mmHg, and FiO2 should be kept as low as possible to sustain the target PaO2.
The current study has implications for interpreting recent randomized control trials (RCTs) evaluating the association between conservative oxygen targets and clinical outcomes. The Oxygen-ICU trial [22] found that oxygen supplementation titrated to more conservative oxygen targets (targeting a PaO2 of 70–100 mmHg during the ICU stay) was associated with improved outcomes compared with conventional oxygen targets (allowing a PaO2 up to 150 mmHg during the ICU stay), with no mention about the proportion of patients exposed to hyperoxemia. The LOCO2 trial [23] assigned patients with acute respiratory distress syndrome to receive either conservative oxygen therapy (target PaO2, 50–70 mmHg) or liberal oxygen therapy (target PaO2, 90–105 mmHg) for 7 days and found that conservative oxygen therapy did not increase survival at 28 days, while was associated with mesenteric ischemic events. Recently, a Dutch RCT conducted in ICU patients fulfilling the systemic inflammatory response syndrome criteria found no significant difference between high-normal (14–18 kPa) and low-normal (targeting a PaO2 of 8–12 kPa) oxygenation targets for non-respiratory organ dysfunction over the first 14 days [24]. The HOT-ICU trial [25] randomly assigned patients with acute hypoxemic respiratory failure to receive oxygen therapy targeting a PaO2 of either 60 mmHg (lower-oxygenation group) or 90 mmHg (higher-oxygenation group) for a maximum of 90 days and declared that a lower-oxygenation target did not result in lower mortality than a higher target at 90 days. These RCTs are unlikely to represent the frequency and persistence of hyperoxemia in clinical practice. In our research, the median TWA-PaO2 was 130.5 mmHg, and it seems that a more conservative strategy in the early phase of disease would demonstrate a clinical benefit. However, a PaO2 target that is too conservative may expose patients to harmful hypoxemia, as was likely the case in the LOCO2 trial.
Oxygen exposure-induced oxidative stress was time- and dose-dependent [26, 27], and the assessment of cumulative exposure was equally important. We concluded that a time- and dose-dependent exposure to hyperoxemia were both associated with harm, which was consistent with two studies [19, 28] and at odds with one prior study. Palmer et al. [29] defined hyperoxemia dose as the area between the PaO2 time curve and a boundary of 100 mmHg divided by the hours of potential exposure (24, 72, 120, or 168 h) and did not observe a dose–response relationship. The inconsistencies are probably attributable, at least partly, to the different threshold values of hyperoxemia and exposure window used.
Limited data was available regarding the cumulative effect of exposure to high FiO2 on mortality, which was also restricted by a single measurement or a shorter exposure window [30,31,32]. According to 73,992 patients undergoing non-cardiothoracic surgery, Staehr-Rye et al. [33] found that high intraoperative FiO2 (0.79, range 0.64–1.0) was associated in a dose-dependent manner with major respiratory complications and 30-day mortality. In the present study, the cumulative effect of exposure to high FiO2 (TWA-FiO2 ≥ 0.5) on mortality during the entire course of ICU admission was significant. Besides, we also found that the higher FiO2 could directly impact the mortality, independently from PaO2, which supports the causal relationship between higher FiO2 and mortality.
Several limitations to the present study should be considered. First, the design of our study is a retrospective observational study, we considered only segmental measured confounders, and the residual measured confounders and unmeasured confounders cannot be fully included. Second, we included all patients who received mechanical ventilation, which makes the results more generalizable. Consequently, significant heterogeneity might exist between groups [34]. We performed several subgroup analyses based on initial admission diagnosis to account for this limitation. Further research is required to explore the impact of time-varying oxygen exposure on mortality in specific patients. Finally, the MIMIV-IV, like all databases with routinely collected data, comprises records with missing values. However, the results from our primary analysis were robust in sensitivity analyses after excluding the missing data.
Conclusion
In conclusion, PaO2 and FiO2 should be carefully monitored in patients with mechanical ventilation, especially during the early-middle course after ICU admission. Cumulative exposure to higher intensities of oxygen exposure was associated with an increased risk of death. Additionally, high FiO2 can impact mortality directly, independently from hyperoxemia.
Availability of data and materials
The datasets presented in the current study are available in the MIMIC-IV database (https://physionet.org/content/mimiciv/2.0/).
Abbreviations
- ICU:
-
Intensive care units
- PaO2 :
-
Arterial oxygen tension
- FiO2 :
-
Fraction of inspired oxygen
- MIMIC-IV:
-
Medical information mart for intensive care IV
- ECMO:
-
Extracorporeal membrane oxygenation
- SOFA:
-
Sequential organ failure assessment
- SAPS II:
-
Simplified acute physiology score II
- OASIS:
-
Oxford acute severity of illness score
- TWA:
-
Time-weighted average
- VFDs:
-
Ventilation-free days
- PAMMs:
-
Piece-wise exponential additive mixed models
- MICE:
-
Multiple imputations by chained equation
- CMA:
-
Causal mediation analysis
- RCTs:
-
Randomized control trials
References
Siemieniuk RAC, Chu DK, Kim LH, Guell-Rous MR, Alhazzani W, Soccal PM, Karanicolas PJ, Farhoumand PD, Siemieniuk JLK, Satia I, et al. Oxygen therapy for acutely ill medical patients: A clinical practice guideline. BMJ. 2018;363: k4169.
Hochberg CH, Semler MW, Brower RG. Oxygen toxicity in critically Ill adults. Am J Respir Crit Care Med. 2021;204(6):632–41.
Jackson RM. Pulmonary oxygen toxicity. Chest. 1985;88(6):900–5.
Brueckl C, Kaestle S, Kerem A, Habazettl H, Krombach F, Kuppe H, Kuebler WM. Hyperoxia-induced reactive oxygen species formation in pulmonary capillary endothelial cells in situ. Am J Respir Cell Mol Biol. 2006;34(4):453–63.
Smit B, Smulders YM, van der Wouden JC, Oudemans-van Straaten HM, Spoelstra-de Man AME. Hemodynamic effects of acute hyperoxia: systematic review and meta-analysis. Crit Care. 2018;22(1):45.
Schjorring OL, Jensen AKG, Nielsen CG, Ciubotariu A, Perner A, Wetterslev J, Lange T, Rasmussen BS. Arterial oxygen tensions in mechanically ventilated ICU patients and mortality: a retrospective, multicentre, observational cohort study. Br J Anaesth. 2020;124(4):420–9.
Eastwood G, Bellomo R, Bailey M, Taori G, Pilcher D, Young P, Beasley R. Arterial oxygen tension and mortality in mechanically ventilated patients. Intensive Care Med. 2012;38(1):91–8.
Page D, Ablordeppey E, Wessman BT, Mohr NM, Trzeciak S, Kollef MH, Roberts BW, Fuller BM. Emergency department hyperoxia is associated with increased mortality in mechanically ventilated patients: a cohort study. Crit Care. 2018;22(1):9.
Madotto F, Rezoagli E, Pham T, Schmidt M, McNicholas B, Protti A, Panwar R, Bellani G, Fan E, van Haren F, et al. Hyperoxemia and excess oxygen use in early acute respiratory distress syndrome: insights from the LUNG SAFE study. Crit Care. 2020;24(1):125.
Martin-Fernandez M, Heredia-Rodriguez M, Gonzalez-Jimenez I, Lorenzo-Lopez M, Gomez-Pesquera E, Poves-Alvarez R, Alvarez FJ, Jorge-Monjas P, Beltran-DeHeredia J, Gutierrez-Abejon E, et al. Hyperoxemia in postsurgical sepsis/septic shock patients is associated with reduced mortality. Crit Care. 2022;26(1):4.
Baleeiro CE, Wilcoxen SE, Morris SB, Standiford TJ, Paine R 3rd. Sublethal hyperoxia impairs pulmonary innate immunity. J Immunol. 2003;171(2):955–63.
Aggarwal NR, D’Alessio FR, Tsushima K, Files DC, Damarla M, Sidhaye VK, Fraig MM, Polotsky VY, King LS. Moderate oxygen augments lipopolysaccharide-induced lung injury in mice. Am J Physiol Lung Cell Mol Physiol. 2010;298(3):L371-381.
Johnson AE, Pollard TJ, Shen L, Lehman LW, Feng M, Ghassemi M, Moody B, Szolovits P, Celi LA, Mark RG. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3: 160035.
Bender A, Scheipl F, Hartl W, Day AG, Kuchenhoff H. Penalized estimation of complex, non-linear exposure-lag-response associations. Biostatistics. 2019;20(2):315–31.
Hartl WH, Kopper P, Bender A, Scheipl F, Day AG, Elke G, Kuchenhoff H. Protein intake and outcome of critically ill patients: analysis of a large international database using piece-wise exponential additive mixed models. Crit Care. 2022;26(1):7.
Ramjith J, Roes KCB, Zar HJ, Jonker MA. Flexible modelling of risk factors on the incidence of pneumonia in young children in South Africa using piece-wise exponential additive mixed modelling. BMC Med Res Methodol. 2021;21(1):17.
Aalen OO, Stensrud MJ, Didelez V, Daniel R, Roysland K, Strohmaier S. Time-dependent mediators in survival analysis: Modeling direct and indirect effects with the additive hazards model. Biom J. 2020;62(3):532–49.
de Jonge E, Peelen L, Keijzers PJ, Joore H, de Lange D, van der Voort PH, Bosman RJ, de Waal RA, Wesselink R, de Keizer NF. Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients. Crit Care. 2008;12(6):R156.
Tyagi S, Brown CA, Dickson RP, Sjoding MW. Outcomes and predictors of severe hyperoxemia in patients receiving mechanical ventilation: A single-center cohort study. Ann Am Thorac Soc; 2022.
Rachmale S, Li G, Wilson G, Malinchoc M, Gajic O. Practice of excessive F(IO(2)) and effect on pulmonary outcomes in mechanically ventilated patients with acute lung injury. Respir Care. 2012;57(11):1887–93.
Demiselle J, Wepler M, Hartmann C, Radermacher P, Schortgen F, Meziani F, Singer M, Seegers V, Asfar P, Investigators HS. Hyperoxia toxicity in septic shock patients according to the Sepsis-3 criteria: a post hoc analysis of the HYPER2S trial. Ann Intensive Care. 2018;8(1):90.
Girardis M, Busani S, Damiani E, Donati A, Rinaldi L, Marudi A, Morelli A, Antonelli M, Singer M. Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit: the oxygen-ICU randomized clinical trial. JAMA. 2016;316(15):1583–9.
Barrot L, Asfar P, Mauny F, Winiszewski H, Montini F, Badie J, Quenot JP, Pili-Floury S, Bouhemad B, Louis G, et al. Liberal or conservative oxygen therapy for acute respiratory distress syndrome. N Engl J Med. 2020;382(11):999–1008.
Gelissen H, de Grooth HJ, Smulders Y, Wils EJ, de Ruijter W, Vink R, Smit B, Rottgering J, Atmowihardjo L, Girbes A, et al. Effect of low-normal vs high-normal oxygenation targets on organ dysfunction in critically Ill patients: a randomized clinical trial. JAMA. 2021;326(10):940–8.
Schjorring OL, Klitgaard TL, Perner A, Wetterslev J, Lange T, Siegemund M, Backlund M, Keus F, Laake JH, Morgan M, et al. Lower or higher oxygenation targets for acute hypoxemic respiratory failure. N Engl J Med. 2021;384(14):1301–11.
Helmerhorst HJF, Schouten LRA, Wagenaar GTM, Juffermans NP, Roelofs J, Schultz MJ, de Jonge E, van Westerloo DJ. Hyperoxia provokes a time- and dose-dependent inflammatory response in mechanically ventilated mice, irrespective of tidal volumes. Intensive Care Med Exp. 2017;5(1):27.
Bak Z, Sjoberg F, Rousseau A, Steinvall I, Janerot-Sjoberg B. Human cardiovascular dose-response to supplemental oxygen. Acta Physiol Oxf. 2007;191(1):15–24.
Helmerhorst HJ, Arts DL, Schultz MJ, van der Voort PH, Abu-Hanna A, de Jonge E, van Westerloo DJ. Metrics of arterial hyperoxia and associated outcomes in critical care. Crit Care Med. 2017;45(2):187–95.
Palmer E, Post B, Klapaukh R, Marra G, MacCallum NS, Brealey D, Ercole A, Jones A, Ashworth S, Watkinson P, et al. The association between supraphysiologic arterial oxygen levels and mortality in critically Ill patients. A multicenter observational cohort study. Am J Respir Crit Care Med. 2019;200(11):1373–80.
Barbateskovic M, Schjorring OL, Russo Krauss S, Jakobsen JC, Meyhoff CS, Dahl RM, Rasmussen BS, Perner A, Wetterslev J. Higher versus lower fraction of inspired oxygen or targets of arterial oxygenation for adults admitted to the intensive care unit. Cochrane Database Syst Rev. 2019. https://doi.org/10.1002/14651858.CD012631.pub2.
Lassen ML, Risgaard B, Baekgaard JS, Rasmussen LS. Determining a safe upper limit of oxygen supplementation for adult patients: a systematic review. BMJ Open. 2021;11(7): e045057.
de Jonge S, Egger M, Latif A, Loke YK, Berenholtz S, Boermeester M, Allegranzi B, Solomkin J. Effectiveness of 80% vs 30–35% fraction of inspired oxygen in patients undergoing surgery: an updated systematic review and meta-analysis. Br J Anaesth. 2019;122(3):325–34.
Staehr-Rye AK, Meyhoff CS, Scheffenbichler FT, Vidal Melo MF, Gatke MR, Walsh JL, Ladha KS, Grabitz SD, Nikolov MI, Kurth T, et al. High intraoperative inspiratory oxygen fraction and risk of major respiratory complications. Br J Anaesth. 2017;119(1):140–9.
Singer M, Young PJ, Laffey JG, Asfar P, Taccone FS, Skrifvars MB, Meyhoff CS, Radermacher P. Dangers of hyperoxia. Crit Care. 2021;25(1):440.
Acknowledgements
None.
Funding
The present study is supported by Yilu “Gexin”—Fluid Therapy Research Fund Project (YLGX-ZZ-2020002).
Author information
Authors and Affiliations
Contributions
HC and YW had the idea of the study, conceptualized the research aims, ZZ and HC design the study and take responsibility for the integrity of the data and the accuracy of the data analysis. MZ, ZZ, and YW contributed to the acquisition of data, HC doing the statistical analysis. ZZ and MZ wrote the first draft of the paper and other authors provided comments and approved the final manuscript.
Corresponding author
Ethics declarations
Ethic approval and consent to participate
The establishment of this database was approved by the Massachusetts Institute of Technology (Cambridge, MA) and Beth Israel Deaconess Medical Center (Boston, MA), and consent was obtained for the original data collection. Therefore, the ethical approval statement and the need for informed consent were waived for this manuscript.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
: Codes for piece-wise exponential additive mixed models
Additional file 2. Table S1
: Baseline characteristics and outcomes of patients stratified by TWA-PaO2 on Day 1; Table S2: Baseline characteristics and outcomes of patients stratified by TWA-FiO2 on Day 1; Table S3: Effect of time-varying TWA-PaO2 and TWA-FiO2 on 28-day mortality of 7784 patients with mechanical ventilation; Table S4: Effect of time spent with hyperoxemia and high FiO2 on 28-day mortality of 7784 patients with mechanical ventilation; Table S5: Effect of cumulative exposure of hyperoxemia and high FiO2 on 28-day mortality of 7784 patients with mechanical ventilation; Table S6: Effect of time-varying hyperoxemia and high FiO2 on 28-day mortality after excluding missing data of daily TWA-PaO2 or TWA-FiO2; Table S7: Effect of time-varying hyperoxemia and high FiO2 on 28-day mortality in patients with mechanical ventilation, patients were followed up from inclusion until death, liberated from mechanical ventilation, ICU discharge, or 28 days in the ICU, whichever occurred first; Figure S1: Study flow diagram in present study. Figure S2: Time-varying effect of TWA-PaO2 (A) or TWA-FiO2 (B) on 28-day mortality
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhu, Z., Zhou, M., Wei, Y. et al. Time-varying intensity of oxygen exposure is associated with mortality in critically ill patients with mechanical ventilation. Crit Care 26, 239 (2022). https://doi.org/10.1186/s13054-022-04114-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04114-w