Abstract
Background
Acute respiratory distress syndrome (ARDS) has different phenotypes and distinct short-term outcomes. Patients with non-focal ARDS have a higher short-term mortality than focal ones. The aim of this study was to assess the impact of the morphological phenotypes of ARDS on long-term outcomes.
Methods
This was a secondary analysis of the LIVE study, a prospective, randomised control trial, assessing the usefulness of a personalised ventilator setting according to lung morphology in moderate-to-severe ARDS. ARDS was classified as focal (consolidations only in the infero-posterior part of the lungs) or non-focal. Outcomes were assessed using mortality and functional scores for quality of life at the 1-year follow-up.
Results
A total of 124 focal ARDS and 236 non-focal ARDS cases were included. The 1-year mortality was higher for non-focal ARDS than for focal ARDS (37% vs. 24%, p = 0.012). Non-focal ARDS (hazard ratio, 3.44; 95% confidence interval, 1.80–6.59; p < 0.001), age, McCabe score, haematological cancers, SAPS II, and renal replacement therapy were independently associated with 1-year mortality. This difference was driven by mortality during the first 90 days (28 vs. 16%, p = 0.010) but not between 90 days and 1 year (7 vs. 6%, p = 0.591), at which point only the McCabe score was independently associated with mortality. Morphological phenotypes had no impact on patient-reported outcomes.
Conclusion
Lung morphologies reflect the acute phase of ARDS and its short-term impact but not long-term outcomes, which seem only influenced by comorbidities.
Trial registration: NCT 02149589; May 29, 2014.
Similar content being viewed by others
Background
Since its first description up to its association with COVID-19, acute respiratory distress syndrome (ARDS) continues to represent a challenging feature in the intensive care unit (ICU) [1]. Mortality due to ARDS remains high without any decrease since the late 1990s [2]. Multiple therapeutics have failed to enhance survival, and quality of life is highly impacted in ARDS survivors [3]. The lack of promising interventions calls for a better targeting of interventions to a subset of patients [4]. Thus, ARDS research has moved from a simple syndromic clinical description to a more complex and broader field of subphenotypes [5].
Various ARDS phenotypes have been described over the past 10 years based on a range of pulmonary physiologic abnormalities [5]. Important investigations focusing on inflammatory biomarkers have been reported using latent class analysis [6]. Hyper- and hypo-inflammatory phenotypes have been described with worse outcomes for the hyper-inflammatory phenotype. Furthermore, post hoc analysis of negative randomised clinical trials found improved outcomes in the treatment arm for patients with hyper-inflammatory phenotype [7]. Similarly, analysis of lung morphology identified two subgroups—focal and non-focal ARDS—with major differences in lung physiology. Non-focal ARDS is associated with worse respiratory mechanics, and morphological phenotypes may influence the response to positive end-expiratory pressure, recruitment manoeuvres, and prone position [8, 9]. Recently, the LIVE study assessed the use of personalised ventilation based on lung morphology [10]. Although the trial was negative, post-hoc analysis suggested promising results for better personalised mechanical ventilation based on lung morphology.
Aside from important in-hospital mortality rates, 1-year mortality is high, and ARDS-related markers of severity are not associated with mortality among ARDS survivors. However, comorbidities and not living at home prior to admission were reported as independent predictors of 1-year mortality [11]. A recent study by Hashem and colleagues assessing long-term outcomes in inflammatory subphenotypes found that those phenotypes largely reflect the acute phase of illness and its short-term impact, with little to no impact on survival beyond 90 days [12]. Although the association between non-focal ARDS and higher 90-day mortality was previously reported, longer-term survival and quality of life have never been investigated in focal and non-focal ARDS. Therefore, our main objective was to assess the long-term outcomes (1 year) of focal and non-focal ARDS. Our secondary objective was to assess the impact of personalised ventilation protocol using a secondary analysis of the prospective LIVE trial after a 1-year follow-up.
Methods
Design and patients
We conducted a secondary preplanned analysis on the long-term outcomes of patients enrolled in the LIVE study, as described in the original protocol [13]. The LIVE study was a prospective, multicentre, stratified, parallel-group, single-blind randomised controlled trial in 20 university and non-university French ICUs [10]. Patients with moderate-to-severe ARDS, according to the Berlin definition, were characterised by local site investigators as having focal ARDS (presence of consolidations localised only in the lower and back parts of the lungs) or non-focal ARDS [14]. Lung morphology was assessed before randomisation using a CT scan of the whole lung or chest X-ray when the severity of the patient was not compatible with transport. Patients were randomly assigned to a ventilation protocol adjusted on the basis of lung morphology (personalised group) or to a standard strategy in line with traditional care (control group). The detailed protocol is available in the online supplement.
In the LIVE trial, 24% of patients were misclassified as focal or non-focal ARDS before randomisation (see LIVE trial for more explanation [10]). We performed an intention-to-treat analysis that included all participants who were randomly assigned to treatment, except those who withdrew consent and those who were found to be ineligible because they met the exclusion criteria. Next, we performed a per-protocol analysis in which misclassified patients in the personalised group were excluded due to a breakdown in the ventilation protocol. Misclassified patients in the control group were not excluded because they were not misaligned with ventilator strategy, which, by definition, is not related to lung morphology.
The study took place in two steps. First, long-term outcomes were assessed based on lung morphology phenotypes: focal versus non-focal ARDS. Then, the impact of a personalised ventilation protocol (i.e. personalised vs. control group) was assessed on the same outcomes. Only the per-protocol analysis was used to compare focal and non-focal ARDS to avoid any bias induced by misclassified patients. However, both the intention-to-treat and the per-protocol analyses were used to compare the personalised and control groups. The results of the personalised and control groups are reported in the Supplemental Data available online.
Ethics
According to current French law, the original trial was approved by the “Institutional Review Board of Clermont-Ferrand, France” (ID RCB 2013-A01756-39) and registered on ClinicalTrials.gov (NCT 02149589) [15]. Before any inclusion, written informed consent was obtained from patients or their relatives. They could refuse to participate at any time, and their decisions were recorded in patient files.
Outcomes
Patient’s survival was assessed, after a 1-year follow-up, between focal and non-focal ARDS and between personalised and control groups. Early mortality was defined as mortality in the first 90 days. Late mortality was defined as mortality between day 90 and 1 year. Further, at the 1-year follow-up, survivors were evaluated by trained research staff who were blinded to treatment allocation. Patient-reported outcome measurements included age- and sex-adjusted physical function and mental health domain scores of the Medical Outcomes Study Short Form 36 (SF-36) instrument [16]; anxiety and depression symptoms from the Hospital Anxiety and Depression Scale (HAD) subscale scores [17]; and effects of fatigue on quality of life from the Modified Fatigue Impact Scale (MFIS) [18]. SF-36 ranges from 0 to 100 with 8 categories and sums up into the physical component summary and the mental component summary. HAD score is divided into anxiety and depression subscales, both ranging from 0 to 21. The presence of anxiety or depression was defined as a subscale over 7 [19]. MFIS total score ranges from 0 to 84 with three subscales: physical (range 0–36), cognitive (range 0–40), and psychosocial (range 0–8). Based on previous studies, patients with an MFIS of over 38 were described as having fatigue [20].
Statistical analysis
Given that this was a secondary analysis of the LIVE study, no sample size calculation was required a priori. A descriptive analysis was performed on all patients and survivors. Quantitative variables are expressed as mean (standard derivation [SD]) or median (interquartile range [IQR], 25–75%) and compared using Student’s t test or the Mann–Whitney U test, as appropriate. Categorical variables are expressed as numbers (%) and compared using the chi-square test or the Fisher’s exact test as appropriate.
Survival curves were plotted using the Kaplan–Meyer method, and comparisons were made using the log-rank test and a Cox model. To assess the impact of lung morphology phenotypes (focal vs. non-focal ARDS) on mortality, significant variables during the univariable analysis (threshold of p < 0.10) or any variable known to be associated with mortality during ARDS were included in a Cox model. Multivariable analysis was performed on complete cases. A sensitivity analysis with multiple imputations was conducted to deal with missing data. Additional information about the process use for multiple imputations is reported in Additional file 1.
Statistical analyses used to assess the impact of a personalised ventilation protocol adjusted on the basis of lung morphology (personalised vs. control group) are reported in Additional file 1.
To compare the functional outcomes of the SF-36 instrument with previous reports [3, 21, 22], z-scores were created by standardising the values (mean = 50, standard deviation = 10; range 0–100, with a higher score indicating better function) using previously described methods [23] and a French cohort of healthy patients [24]. A Mann–Whitney U test was used to assess the difference between the z-scores and 50. Because 35% of patients missed the functional outcomes assessment, a sensitivity analysis with imputation was conducted to deal with missing data. Additional information about the process use for imputation is reported in Additional file 1. A P value of ≤ 0.05 was considered to be statistically significant. Statistical analyses were carried out using R version 4.1.2 for macOS® (https://www.r-project.org, accessed November 2021).
Results
Population
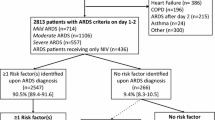
From June 2014 to February 2017, 420 patients were included in the LIVE study. Flow charts of the study are reported in Fig. 1 and Additional file 1: Fig. S1. Sixty patients were excluded from the per-protocol analysis, as described in Additional file 1: Fig. S1. Of the remaining 360 patients, 124 (34%) and 236 (66%) had focal and non-focal ARDS, respectively (Fig. 1). Information for survival at 1 year was available for 334 patients (93%) (114 and 220 patients with focal and non-focal ARDS, respectively). Data on the population included to compare the personalised and control groups are reported in the online supplement.
Flow chart: Shown is the recruitment of the cohort for analysis comparing focal and non-focal ARDS. *Misclassified patients (focal ARDS characterised as non-focal ARDS or non-focal ARDS characterised as focal ARDS) in the intervention arm of the LIVE study (patients with a personalised ventilation protocol based on the morphological phenotypes) were excluded due to a breakdown in the ventilation protocol. ARDS: Acute respiratory distress syndrome
Mortality according to lung morphology
Patient baseline data for the per-protocol cohort and for the focal and non-focal ADRS groups are summarised in Table 1. There were more males, and BMI was higher in the focal ARDS group. Plateau pressure, PEEP, and driving pressure were higher in non-focal ARDS. Ventilator-free days to day 28 and ICU length of stay were not different between the groups.
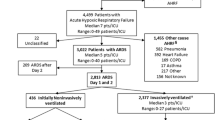
The 1-year mortality was higher in non-focal ARDS patients compared with focal ARDS patients (81 [37%] vs. 27 [24%], respectively; log-rank test: p = 0.012) (Fig. 2A). In the multivariate analysis, non-focal ARDS (hazard ratio (HR), 3.44; 95% confidence interval (95%CI), 1.80–6.59; p < 0.001), age (HR, 1.04; 95%CI, 1.02–1.06; p < 0.001), McCabe score (HR, 1.51; 95%CI, [1.04–2.19]; p = 0.029), haematological cancers (HR, 2.24; 95%CI, 1.02–4.97; p = 0.045), SAPS II (HR, 1.02; 95%CI, 1.00–1.04; p = 0.047), and renal replacement therapy (HR, 1.71; 95%CI, 1.04–2.79; p = 0.033) were independently associated with 1-year mortality (Additional file 1: Table S1).
Mortality assessment during a 1-year follow-up between focal and non-focal ARDS. A Survival analyses in the per-protocol cohort by morphological phenotypes during a 1-year follow-up (log-rank test: p = 0.012, HR = 3.44 [1.80–6.59] p < 0.001, with higher mortality among non-focal ARDS), B Early and late mortality defined as mortality during the first 90 days and between day 90 and 1 year, respectively. One-year mortality was driven by early mortality (log-rank test: p = 0.010, HR = 4.40 [1.93–10.01] p < 0.001) but not by late mortality (log-rank test: p = 0.591, HR = 2.79 [0.81–9.63] p = 0.106). Survival curves were realised using the Kaplan–Meyer methods. ARDS: acute respiratory distress syndrome
The difference in 1-year mortality was driven by early mortality (65 non-focal ARDS patients [28%] vs. 19 focal ARDS patients [16%]; log-rank test: p = 0.010) but not by late mortality (16 non-focal ARDS patients [7%] vs. 8 focal ARDS patients [6%]; log-rank test: p = 0.591) (Fig. 2B). Non-focal ARDS, age, SAPS II, and renal replacement therapy were independent predictors of early mortality (Table 2). Only the McCabe score was associated with late mortality (Table 2). During the first 90 days, death was directly related to ARDS in 35% and 37% of patients with focal and non-focal ARDS, respectively (p = 0.89). Underlying disease was accountable for 65% and 63% of deaths in focal and non-focal ARDS, respectively.
There were no missing data for the included variables, except for plateau pressure, PEEP, and driving pressure, which were unavailable for 83 (23%), 14 (4%), and 88 (24%) patients, respectively. A sensibility analysis with multiple imputations for missing data confirmed the previous multivariate analysis. (Additional file 1: Table S2).
Quality of life according to lung morphology
A total of 226 patients survived after a 1-year follow-up and were eligible for functional outcomes assessment. We noted that 79 patients (35%) missed the functional outcomes assessment (27 [31%] and 52 [37%] patients with focal and non-focal ARDS, respectively) (Fig. 1). There was no difference between patients who did and did not complete the functional outcomes assessment at the 1-year follow-up except for age and McCabe score (Additional file 1: Table S3). Focal ARDS patients who completed the functional outcomes assessment were older (62 [14] vs. 54 [16] years; p = 0.005) and had a lower McCabe score (p = 0.027) than those who did not. However, there was no difference between focal and non-focal ARDS among patients who completed the functional outcomes assessment.
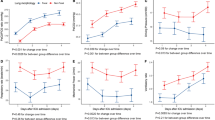
After a 1-year follow-up, the per-protocol cohort had significant impairment in patient-reported outcomes when compared against an age- and sex-matched population (Table 3) [24]. The median values for the standardised SF-36 physical and mental component summary were 37 (p < 0.001) and 41 (p < 0.001), respectively. Compared against an age- and sex-matched population [24], both focal (p < 0.001) and non-focal ARDS (p < 0.001) had impairment in the SF-36 physical component summary, with no differences between both groups (p = 0.201).
Regarding the HAD scale, 41% and 35% of the per-protocol cohort had anxiety and depression, respectively. The median MFIS component summary of the per-protocol cohort was 43 (Table 3), and 91 (62%) patients experienced fatigue. There was no difference in anxiety and depression symptoms and rate of fatigue between the focal and non-focal ARDS groups (Table 3).
A sensitivity analysis dealing with patients that missed the 1-year functional assessment confirmed the previous analysis (Additional file 1: Table S4).
Personalised ventilation protocol
At the 1-year follow-up, there was no difference in survival and quality of life between the personalised and the control groups regarding both the intention to treat and per-protocol analysis (Additional file 1: Fig. S2 and Tables S5 to S8).
Discussion
To our knowledge, this is the first prospective study to assess the impact of morphological phenotypes on long-term outcomes among ARDS patients. We demonstrated a difference in survival over a 1-year follow-up between focal and non-focal ARDS, which is only driven by early mortality without any consequences of lung morphology beyond the first 90 days. Among survivors, physical and mental health, anxiety, depression, and fatigue were all impaired but independently of ARDS phenotypes.
Impact of lung morphology phenotype on long-term outcomes
A prior study demonstrated a significant difference in early mortality between focal and non-focal ARDS without assessing long-term outcomes [8]. Beyond confirming these results, our study found that the difference in survival after a 1-year follow-up is only explained by short-term mortality. The impact of morphological phenotypes on mortality may be explained by differences in respiratory mechanics, with a higher driving pressure and elastance in non-focal ARDS [25]. Indeed, in our study, non-focal ARDS had higher plateau and driving pressures at baseline.
As with other intensive care variables (i.e. SAPS II, renal replacement therapy), which are independently associated with short-term mortality (90-day mortality), morphological phenotypes had no impact on mortality thereafter. Only comorbidities and previous health status seemed to impact long-term survival. These results are consistent with previous studies reporting that the severity of illness is a strong predictor of hospital and short-term mortality, whereas age, serious comorbidities, and previous health status are associated with long-term mortality in ARDS [11, 26]. Nevertheless, morphological phenotypes may be considered one of baseline intensive care variables, along with others such as respiratory mechanics and renal replacement therapy, which may only impact short-term mortality [27, 28]. These findings are consistent with a recent study that focused on the impact of the inflammatory phenotype on long-term survival in ARDS patients [12]. In that study, the inflammatory phenotype had an impact on short-term survival, with little implication after 90 days.
In our trial, beyond survival, quality of life was altered after a 1-year follow-up. Physical and mental health were impaired compared with a healthy population [24] which is consistent with previous studies [3, 21, 22]. Age and previous comorbidities have been reported to be associated with impairment of the SF-36 instrument [3]. Even though the specific contribution of ARDS is contested [29], the severity of the initial ARDS, the rapidity of its resolution, and the pulmonary dysfunction thereafter were all correlated with long-term outcomes [21, 30]. Anxiety and depression affected one-third of the ARDS survivors in our study. These results were similar to those of previous trials that reported between 11 and 42% of anxiety and 9 to 39% of depression using the HAD scale [22, 31]. Female sex, unemployment, alcohol misuse, and greater opioid use in the ICU were significantly associated with psychiatric symptoms [32]. Baseline intensive care variables, severity of illness, and mechanical ventilation duration were not associated with anxiety or depression. Eventually, fatigue was reported in 62% of ARDS survivors using the MFIS score in our study. Using another fatigue scale, a recent study reported 70% and 66% of ARDS survivors with significant symptoms of fatigue at 6-month and 1-year follow-ups, respectively [31]. Worse physical, cognitive, and mental health but not baseline critical care variables were associated with greater fatigue. Thus, one could wonder about the impact of morphological phenotypes on survivors’ later quality of life. However, in our study, there was no influence of morphological phenotypes on any functional score.
Impact of a personalised ventilation protocol based on phenotypes on long-term outcomes
In the age of personalised medicine, a personalised ventilation protocol adjusted on the basis of morphological phenotypes was of concern. The LIVE trial failed to show any effect on 90-day mortality [10]. Similarly, we could not find any improvement in mortality or functional outcomes even with the exclusion of patients with a ventilation protocol break. The LIVE trial was unfortunately biased by a high number of misclassified patients who had worse outcomes than the control group. Morphological phenotyping of ARDS patients is a major problem because the misclassification of some patients makes it impossible to determine the value of phenotyping over the standard of care. Recently, some machine learning algorithms have been inconsistent in their ability to identify clusters of ARDS patients involved in significant heterogeneity of treatment effects [33]. Future studies may be needed to provide physicians with effective solutions to avoid misclassification, with or without the help of new technologies.
Strengths and limits
The prospective and multicentre aspects of this study are some of its strengths. Compared with most studies, phenotyping was performed before randomisation, and the large cohort allowed the use of multivariable analysis in the statistical protocol, providing a more detailed interpretation of the data. However, this study has some limitations. First, it is a secondary analysis of a previous trial with an a priori sample size calculation based on the primary outcome and with numerous misclassified patients. This might have induced an underpower analysis, which can explain the absence of differences induced by the personalised ventilation protocol. Second, 24% of patients were misclassified into the focal and non-focal ARDS groups in the LIVE study, which may influence the different analyses and their interpretations. Indeed, misclassified patients have worse outcomes than correctly classified patients in both the LIVE trial and study [10]. Third, there were about 20% of missing data concerning plateau pressure, PEEP, and driving pressure. Given that we used a complete case analysis in our multivariable models, this may have induced a selection bias. However, our results were confirmed by a sensitive analysis with multiple imputations for missing data. Eventually, about 30% of survivors missed the functional outcome assessment after a 1-year follow-up. This may have induced a bias, especially as the patients were not similar in terms of age and McCabe score. However, our results are similar to those of previous studies, and there was no difference between the two phenotypes.
Conclusion
Morphological phenotypes and 1-year mortality were associated with a higher mortality in patients with non-focal ARDS. This difference in survival was driven only by mortality before day 90. Our findings indicate that between day 90 and 1 year, none of the ICU parameters (severity scores, ventilator setting, lung morphology) had an impact on mortality and long-term outcomes. Yet, this study suggests that ARDS morphological phenotypes and related therapeutic approaches largely reflect the acute phase of the syndrome and its short-term impact on mortality; they do not impact the long-term outcomes of patients, which are only influenced by underlying comorbidities.
Availability of data and materials
Data collected for the study, including individual participant data, data dictionary defining each field in the set, and study protocol will be made available to others. Data will be communicated as de-identified participant data according to French law and will be available after publication of the manuscript. Data were stored at the Direction de la Recherche Clinique, University Hospital of Clermont-Ferrand, Clermont-Ferrand, France. Data requests should be addressed to Pr Jean-Michel Constantin (jean-michel.constantin@aphp.fr) who will send the data after receipt of a signed data access agreement.
References
Thompson BT, Chambers RC, Liu KD. Acute respiratory distress syndrome. New Engl J Med. 2017;377:562–72.
Phua J, Badia JR, Adhikari NKJ, Friedrich JO, Fowler RA, Singh JM, et al. Has mortality from acute respiratory distress syndrome decreased over time? Am J Resp Crit Care. 2009;179:220–7.
Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. New Engl J Med. 2011;364:1293–304.
Laffey JG, Kavanagh BP. Negative trials in critical care: why most research is probably wrong. Lancet Respir Med. 2018;6:659–60.
Matthay MA, Arabi YM, Siegel ER, Ware LB, Bos LDJ, Sinha P, et al. Phenotypes and personalized medicine in the acute respiratory distress syndrome. Intens Care Med. 2020;46:2136–52.
Calfee CS, Delucchi K, Parsons PE, Thompson BT, Ware LB, Matthay MA, et al. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med. 2014;2:611–20.
Famous KR, Delucchi K, Ware LB, Kangelaris KN, Liu KD, Thompson BT, et al. Acute respiratory distress syndrome subphenotypes respond differently to randomized fluid management strategy. Am J Resp Crit Care. 2016;195:331–8.
Rouby J-J, Puybasset L, Cluzel P, Richecoeur J, Lu Q, Grenier P. Regional distribution of gas and tissue in acute respiratory distress syndrome. II. Physiological correlations and definition of an ARDS Severity Score. Intens Care Med. 2000;26:1046–56.
Constantin J-M, Grasso S, Chanques G, Aufort S, Futier E, Sebbane M, et al. Lung morphology predicts response to recruitment maneuver in patients with acute respiratory distress syndrome. Crit Care Med. 2010;38:1108–17.
Constantin J-M, Jabaudon M, Lefrant J-Y, Jaber S, Quenot J-P, Langeron O, et al. Personalised mechanical ventilation tailored to lung morphology versus low positive end-expiratory pressure for patients with acute respiratory distress syndrome in France (the LIVE study): a multicentre, single-blind, randomised controlled trial. Lancet Respir Med. 2019;7:870–80.
Wang CY, Calfee CS, Paul DW, Janz DR, May AK, Zhuo H, et al. One-year mortality and predictors of death among hospital survivors of acute respiratory distress syndrome. Intens Care Med. 2014;40:388–96.
Hashem MD, Hopkins RO, Colantuoni E, Dinglas VD, Sinha P, Friedman LA, et al. Six-month and 12-month patient outcomes based on inflammatory subphenotypes in sepsis-associated ARDS: secondary analysis of SAILS-ALTOS trial. Thorax. 2022;77:22–30.
Jabaudon M, Godet T, Futier E, Bazin J-É, Sapin V, Roszyk L, et al. Rationale, study design and analysis plan of the lung imaging morphology for ventilator settings in acute respiratory distress syndrome study (LIVE study): Study protocol for a randomised controlled trial. Anaesth Crit Care Pa. 2017;36:301–6.
Force ADT, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–33.
Toulouse E, Masseguin C, Lafont B, McGurk G, Harbonn A, Roberts JA, et al. French legal approach to clinical research. Anaesth Crit Care Pa. 2018;37:607–14.
Ware J, Sherbourne C. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiat Scand. 1983;67:361–70.
Téllez N, Río J, Tintoré M, Nos C, Galán I, Montalban X. Does the modified fatigue impact scale offer a more comprehensive assessment of fatigue in MS? Mult Scler. 2005;11:198–202.
Snaith RP. The hospital anxiety and depression scale. Health Qual Life Out. 2003;1:29.
Flachenecker P, Kümpfel T, Kallmann B, Gottschalk M, Grauer O, Rieckmann P, et al. Fatigue in multiple sclerosis: a comparison of different rating scales and correlation to clinical parameters. Mult Scler. 2002;8:523–6.
Schelling G, Stoll C, Vogelmeier C, Hummel T, Behr J, Kapfhammer H-P, et al. Pulmonary function and health-related quality of life in a sample of long-term survivors of the acute respiratory distress syndrome. Intens Care Med. 2000;26:1304–11.
Pfoh ER, Chan KS, Dinglas VD, Cuthbertson BH, Elliott D, Porter R, et al. The SF-36 offers a strong measure of mental health symptoms in survivors of acute respiratory failure. A tri-national analysis. Ann Am Thorac Soc. 2016;13:1343–50.
The SF-36 [Internet]. Available from: https://alswh.org.au/wp-content/uploads/2020/08/DDSSection2.3SF36.pdf.
Leplège A, Ecosse E, Verdier A, Perneger TV. The French SF-36 health survey translation, cultural adaptation and preliminary psychometric evaluation. J Clin Epidemiol. 1998;51:1013–23.
Puybasset L, Cluzel P, Gusman P, Grenier P, Preteux F, Rouby J-J. Regional distribution of gas and tissue in acute respiratory distress syndrome. I. Consequences for lung morphology. Intens Care Med. 2000;26:857–69.
Chiumello D, Coppola S, Froio S, Gotti M. What’s next after ARDS: long-term outcomes. Respir Care. 2016;61:689–99.
Chiumello D, Taccone P, Berto V, Marino A, Migliara G, Lazzerini M, et al. Long-term outcomes in survivors of acute respiratory distress syndrome ventilated in supine or prone position. Intens Care Med. 2012;38:221–9.
Khandelwal N, Hough CL, Bansal A, Veenstra DL, Treggiari MM. Long-term survival in patients with severe acute respiratory distress syndrome and rescue therapies for refractory hypoxemia. Crit Care Med. 2014;42:1610–8.
Granja C, Morujão E, Costa-Pereira A. Quality of life in acute respiratory distress syndrome survivors may be no worst than in other ICU survivors. Intens Care Med. 2003;29:1744–50.
Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. New Engl J Med. 2003;348:683–93.
Neufeld KJ, Leoutsakos JMS, Yan H, Lin S, Zabinski JS, Dinglas VD, et al. Fatigue symptoms during the first year following ARDS. Chest. 2020;158:999–1007.
Huang M, Parker AM, Bienvenu OJ, Dinglas VD, Colantuoni E, Hopkins RO, et al. Psychiatric symptoms in acute respiratory distress syndrome survivors. Crit Care Med. 2016;44:954–65.
Sinha P, Spicer A, Delucchi KL, McAuley DF, Calfee CS, Churpek MM. Comparison of machine learning clustering algorithms for detecting heterogeneity of treatment effect in acute respiratory distress syndrome: a secondary analysis of three randomised controlled trials. EBioMedicine. 2021;74: 103697.
Acknowledgements
Not applicable.
Funding
French Ministry of Health (Programme Hospitalier de Recherche Clinique InterRégional 2013: 13–014). The funding had no role in the study design, collection, analysis, or interpretation of data.
Author information
Authors and Affiliations
Contributions
J-MC and EF conceived and designed the study. FB, J-MC, MJ, AM, and EF acquired, analysed, or interpreted the data. FB and J-MC created the first draft of the manuscript. FB, J-MC, TG, SP, NK, MJ, VD, AB, AM, EF, and AJ provided crucial revisions for important intellectual content and gave final approval of the manuscript. LB was charged with data management. FB performed the statistical analysis. J-MC and LB were tasked with administrative, technical, or material support. J-MC supervised the study. All authors reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in the present study were in accordance with the Declaration of Helsinki, and the study was reviewed and approved by Institutional Review Board of Clermont-Ferrand, France (N°EudraCT 2013-A01756-39) and registered on ClinicalTrials.gov (NCT02149589, May 29, 2014). Written informed consent was obtained from the patients when possible. Otherwise, informed consent was firstly asked to next to kin and later confirmed by patients if feasible.
Consent for publication
Not applicable
Competing interests
MJ reports grants from the European Union, French Ministry of Health (Direction Générale de l’Offre de Soins), Auvergne Regional Council, Agence Nationale de la Recherche, CHU Clermont-Ferrand, European Society of Anesthesiology, and Sedana Medical; personal fees from Sedana Medical, General Electrics Healthcare, Abbvie, and the Société Française d’Anesthésie et Réanimation; and non-financial support from General Electrics Healthcare, outside the submitted work. EF reports personal fees from Edwards Lifesciences, Drager, General Electric Healthcare, Fresenius Kabi, Fisher and Paykel Healthcare, and Baxter, outside of the submitted work. J-MC reports personal fees and non-financial support from Drager, GE Healthcare, Sedana Medical, Baxter, and Amomed; personal fees from Fisher and Paykel Healthcare, Orion, Philips Medical, and Fresenius Medical Care; and non-financial support from LFB and Bird Corporation, outside of the submitted work. All other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Method and Result supplements.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Blanchard, F., Godet, T., Pons, S. et al. One-year patient outcomes based on lung morphology in acute respiratory distress syndrome: secondary analysis of LIVE trial. Crit Care 26, 159 (2022). https://doi.org/10.1186/s13054-022-04036-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04036-7