Abstract
Background
An appropriate diagnostic process is crucial for managing patients with acute heart failure (AHF) in emergency department (ED). Our study aims to describe the characteristics and therapeutic management of patients admitted to the ED for dyspnea suspected to have AHF, their in-hospital pathway of care and their in-hospital outcome.
Methods
Consecutive patients admitted in 26 French ED for dyspnea suspected to be the consequence of AHF, prior to in hospital diagnostic test, were prospectively included at the time of their admission in the DeFSSICA Survey. Clinical characteristics at admission were recorded by the ED physicians. At discharge from ED, patients were categorized as AHF or non-AHF based on the final diagnosis reported in the discharge summary. The completeness of the data was controlled by the local investigator.
Results
From 16/6/2014 to 7/7/2014, 699 patients were included, of whom 537 (77 %) had a final diagnosis of AHF at discharge. Patients with AHF were older (median 83 vs 79 years, p = 0.0007), more likely to have hypertension (71 % vs 57 %, p = 0.002), chronic HF (54 % vs 37 %, p = 0.0004), atrial fibrillation (45 % vs 34 %, p = 0.02) and history of hospitalization for AHF in the previous year (40 % vs 18 %, p < 0.0001) when compared to patients without AHF. Furosemide and oxygen were used in approximately 2/3 of the patients in the ED (respectively 75 and 68 %) whereas nitrates were in 19 % of the patients. Diagnostic methods used to confirm AHF included biochemistry (100 %), pro-B-type natriuretic peptide (90 %), electrocardiography (98 %), chest X-ray (94 %), and echography (15 %) which only 18 % of lung ultrasound.
After the ED visit, 13 % of AHF patients were transferred to the intensive care unit, 28 % in cardiology units and 12 % in geriatric units. In-hospital mortality was lower in AHF vs non-AHF patients (5.6 % vs 14 %, p = 0.003).
Discussion
DeFSSICA, a large French observational survey of acute HF, provides information on HF presentation and the French pathway of care. Patients in DeFSSICA were elderly, with a median age of 83 years. Compared with the French OFICA study, patients in DeFSSICA were more likely to have hypertension (71 % vs 62 %) and atrial fibrillation (45 % vs 38 %). As atrial fibrillation and a rapid heart rate have been closely linked to mortality, detection of atrial fibrillation should be considered systematically.The limited use of nitrates in DeFSSICA may be related to the median SBP of 140 (121–160) mmHg. However, our use of nitrates was similar to those in the EAHFE (20.7 %) and OPTIMIZE-HF (14.3 %) registries. In line with guidelines, the proportions of patients who underwent ECG, biological analysis, or chest X-ray were all >90 % in DeFSSICA. Similarly, BNP or pro-BNP was measured in 93 % of patients, compared with 82 % of patients in the OFICA study. Although BNP may be helpful when the diagnosis of HF is in doubt, ultrasound remains the gold standard. The use of ultrasound in the ED has been reported to accelerate the diagnosis of HF and the initiation of treatment, and shorten the length of stay. In-hospital mortality of HF patients in DeFSSICA was 6.4 %, slightly lower than in the OFICA study (8.2 %). Improved interdisciplinary cooperation has been highlighted as a key factor for the improvement of HF patient care.
Conclusions
DeFSSICA shows that patients admitted for dyspnea suspected to be the consequence of AHF are mostly elderly. The diagnosis of AHF is difficult to ascertain based on clinical presentation in patients with dyspnea. Novel diagnostic techniques such as thoracic ultrasound are warranted to provide the right treatment to the right patients in the ED as early as possible.
Similar content being viewed by others
Background
Heart failure (HF) has been estimated to affect approximately 2 % of adults in developed countries [1], and 9 % of those aged 80–89 years [2]. HF is the cause of over 150,000 hospitalizations in France each year, and the costs of treating patients with HF have been estimated to consume around 1 % of the total healthcare costs [2]. Patients with HF often present in acute or subacute decompensation in acute HF, but various other conditions can also cause dyspnea, raising the problem of differential diagnosis.
Importance
An appropriate diagnostic process is crucial for starting the patient on the right care pathway and to avoid loss of time in care. However, no trial or survey has described the current management of acute HF syndromes in the French emergency medical system.
Goals of this investigation
The main objective was to assess the diagnostic and therapeutic management of emergency patients with suspected heart failure dyspnea. Secondary objectives were to define the pathway of care according to the Emergency Department (ED) diagnosis and evaluate mortality.
Methods
Study design and setting
DeFSSICA (Description de la Filière de Soins dans les Syndromes d’Insuffisance Cardiaque Aigue) is a French prospective survey that recruited consecutive patients presenting with suspected heart failure dyspnea in 26 emergency departments (EDs) in academic hospitals and community and regional hospitals. The study was promoted by the French Society of Cardiology (Société Française de Cardiologie [SFC]), the French Society of Emergency Medicine (Société Française de Médecine d'Urgence [SFMU]) and RESCUe (an emergency cardiovascular network).
DeFSSICA received approval from the National Commission for Liberties and Data Protection (Commission Nationale de l’Informatique et des Libertés [CNIL]) (number DR-2014-543) and the Advisory Committee on the Treatment of Information in the field of Health Research (Comité Consultatif sur le Traitement de l’Information en matière de Recherche dans le domaine de la Santé [CCTIRS]) (number 14-291). All patients received written information about the survey objectives.
Selection of participants
Consecutive patients aged above 18 years admitted to the ED with dyspnea compatible with acute HF were included in the survey by the emergency physician on charge and prior to chest X-ray and laboratory test. Dyspnea compatible with HF was defined as dyspnea associated with peripheral edema and/or pulmonary crackles and/or excessive weight gain and/or use of furosemide.
Methods and measurements
Data concerning baseline characteristics, medical history, social factors, in-hospital diagnostic tests and treatment, final diagnosis, destination after ED discharge, and in-hospital mortality and length of stay were recorded by emergency physicians in a case report form (CRF). The CRF was structured according to the progress of care. Cardiac sonographic evaluations were judged at the sole discretion of emergency physician. Abnormal chest ray was defined by the presence of cardiomegaly and/or alveolar edema and/or interstitial opacity and/or pleural effusion. The choice of treatment was at the emergency physician’s discretion, according to their usual practice. Final diagnosis of acute HF was retained by emergency physician as a combination of a clinical history, an abnormal chest x-ray, an elevated BNP/proBNP and ultrasound signs. Data were entered into a secured database located at the RESCUe Coordination Center.
Local investigators monitored the data to check for any errors or inconsistencies. They were also in charge of trying to recover missing data. At discharge from ED, patients were categorized as AHF or non-AHF based on the final diagnosis reported in the discharge summary. A hotline staffed by a clinical research assistant was dedicated to the survey (during the daytime).
Outcomes
This study examined the pathway of care (from transportation to the ED to discharge destination); the use of various diagnostic methods (biological and imaging) and treatments; clinical signs and symptoms; causes of HF; and mortality.
Analysis
All patients with suspected heart failure dyspnea were included. Comparisons between those with and without a final diagnosis of HF were undertaken. Data are medians and interquartile ranges (IQRs) for continuous variables, and numbers and percentages for qualitative variables. Comparative analyses were performed using the χ 2 or Fisher’s test for binary variables and the Wilcoxon test for analysis of variance for continuous variables. Differences were considered to be statistically significant when the P value was <0.05. Analysis were performed using the R statistical package.
Results
Characteristics of study subjects
Between June 16 and July 7, 2014, DeFSSICA recorded 699 cases of suspected cardiac dyspnea, of whom 537 (77 %) were ultimately identified as having HF. During the same period, 64,281 emergency visits were recorded, thus HF accounted for 0.8 % of ED visits.
Thirteen (50 %) investigators centers were academic hospitals, 11 (42 %) were community hospitals and 2 (8 %) of them were regional hospitals. The academic hospitals included 349 (50 %) patients, community hospitals included 243 (35 %) patients and regional hospitals included 107 (15 %).
Baseline characteristics of patients with and without an ED diagnosis of HF are shown in Table 1. HF patients were older than those without HF, and just under half of each group were male. HF patients were significantly more likely to have hypertension, chronic heart failure, and atrial fibrillation than patients without HF, but the prevalence of other comorbidities did not differ between the two groups. HF patients were more likely to be taking furosemide, angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin II receptor blockers (ARBs), β-blockers, anticoagulants, and insulin than those without HF. Compared to those without HF, those with HF were more likely to have been hospitalized for HF at least once during the past year; they were also more likely to be under the care of a cardiologist.
Most patients, with or without HF, were living at home (Table 1). However, patients with HF were less likely to be self-sufficient, and more likely to be in receipt of home assistance.
Hospitalization and clinical status
Among all DeFSSICA patients, 63 % made their own way to the ED (Table 2). For the remaining patients, medical dispatch centers (Centres 15 or services d’aide médicale urgente [SAMUs]) mobilized appropriate prehospital assistance. There was no difference in the distribution of transport modes between patients with and without HF.
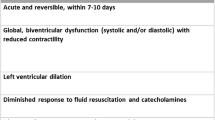
Clinical signs were mainly similar between patients with and without HF, but HF patients were more likely to present with signs of right heart failure (Table 2). Vital signs were also mainly similar between patients with and without HF, although pulse oximetry was lower among those with HF. Only 3.2 % of patients with or without HF presented signs of cardiogenic shock, while 54 and 18 % of HF patients were Killip 2 or 3, respectively, versus 29 and 9.4 %, respectively of patients without HF (P < .0001).
Early management and diagnosis
At admission, all patients (100 %) underwent biological analysis. Patients with HF had lower creatinine clearance and higher B-type natriuretic peptide (BNP) and pro-BNP (Table 3). Troponin was positive in 66 % of HF patients versus 46 % in non-HF patients (P = .0001).
Most patients (98 %) underwent an ECG. HF patients were more likely to have atrial fibrillation and left bundle branch block (LBBB) (Table 4). The majority of patients underwent chest X-ray (94 %), which was more often abnormal in HF patients (95 % vs 71 %; P < .0001).
Echocardiography was performed in 104 patients (15 %) of which 19 have received pulmonary echography. Cardiologists conducted 60 % of echographies while emergency physicians performed 40 % of them (Table 4).
Echographies performed by cardiologists were more likely to be self-rated as satisfactory than those by emergency physicians. Left ventricular ejection fraction (LVEF) did not differ significantly between those with and without HF.
Patients with HF were more likely to receive furosemide, oxygen, and nitrates, but other emergency measures occurred similarly in both groups (Table 4).
Among the 158 patients in whom the diagnosis of HF was not retained, emergency physician reported pulmonary disease in 51.3 % of them (mainly pulmonary infection, pulmonary embolism, and chronic obstructive pulmonary disease (COPD) exacerbation), cardiac disease in 29.1 % (mainly acute coronary syndrome), unspecific diagnosis (discomfort, stress, panting or palpitation) in 10.7 %, renal failure in 5.1 % and gastric disease in 3.8 %.
Outcomes
Most patients with suspected heart failure dyspnea had acute HF (77 %). ED diagnosis (i.e. HF or NHF) was made at the end of hospitalization by consulting the medical record. Precipitating factors were not determined in 43 % of cases (Table 5). The most common determined precipitating factors were infection (25 %) and arrhythmia (15 %).
After the ED admission, HF patients were most likely to be hospitalized in a cardiology ward, and only 13 % required treatment in an intensive care unit (Table 5). The destination unit was judged by the emergency physician as appropriate in 76 % of cases.
Only 1 % of patients died in the ED. In-hospital mortality was lower among those with versus without HF (5.6 % vs 14 %; P = .003), but length of stay was longer (Table 5).
Discussion
This large French observational survey of acute HF coordinated by emergency medicine investigators has successfully collected epidemiologic, diagnostic, and therapeutic data, from emergency admission to hospital discharge. As such, DeFSSICA provides information on HF presentation and the French pathway of care.
Not surprisingly, patients in DeFSSICA were elderly, with a median age of 83 years. However, DeFSSICA patients were generally older than those in other HF registries from France (Observatoire Français de l’Insuffisance Cardiaque Aiguë [OFICA]) [4], Switzerland (Acute Heart Failure Global Survey of Standard Treatment [ALARM-HF]) [5], Spain (Epidemiology of Acute Heart Failure in Emergency Departments [EAHFE]) [6], and the US (Acute Decompensated Heart Failure National Registry Emergency Module [ADHERE-EM] [7], Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure [OPTIMIZE-HF]) [8]. Mean ages in these studies ranged from 73 to 79 years (details of these registries can be found in the Additional file 1). Compared with these registries [4–8], patients in DeFSSICA were less likely to have chronic respiratory failure or chronic HF, but more likely to have chronic renal failure (Web Appendix). Compared with the French OFICA study [4], patients in DeFSSICA were more likely to have hypertension (71 % vs 62 %) and atrial fibrillation (45 % vs 38 %). As atrial fibrillation and a rapid heart rate have been closely linked to mortality [9], detection of atrial fibrillation should be considered systematically.
Furosemide, oxygen, and nitrates were the most commonly used treatments in DeFSSICA patients with HF (75, 68, and 19 %, respectively). The limited use of nitrates may be related to the median (IQR) SBP of 140 (121–160) mmHg. However, our use of nitrates was similar to those in the EAHFE [6] (20.7 %) and OPTIMIZE-HF [8] (14.3 %) registries. Only 10 % of our HF patients received non-invasive ventilation or Boussignac continuous positive airway pressure (CPAP), similar to in the OFICA study (12.4 %) [4]. This ventilation assistance improves outcome in acute HF patients, especially those with pulmonary edema [10, 11]. However, it requires patient compliance and cooperation, which is not necessarily obvious in elderly [12, 13].
Current recommendations for diagnostic investigations in patients with suspected HF include first the assessment of HF probability related to the clinical history (history of coronary artery diseases, or hypertension, or use of diuretics…), the physical examination (bilateral ankle oedema, jugular venous dilatation…) and the ECG (Class I, Level C) [14].
If one of these symptoms or abnormal ECG signs are present, the measurement of BNP or NT-proBNP is the second step in the algorithm of the diagnosis (Class IIa, Level C) with also blood chemistry, and complete blood count (Class I, Level C). Finally, comprehensive assessment of patients with HF comprises, chest X-Ray, transthoracic echocardiography (Class I, Level C), and lung ultrasound (Classe IIb, Level C) [14]. However, in DeFSSICA, only 15 % of all patients underwent echography, due to a lack of equipment and training of emergency physicians. When echography was performed by a cardiologist (60 % of cases), most considered the results to be satisfactory (66 %), but when it was performed by emergency physicians (40 % of cases), only 21 % considered the results to be satisfactory. Therefore, we have identified a need for additional effort for training emergency physicians and providing equipment, as prompt use of echography in the ED has been shown to improve the diagnosis of HF [15].
In line with guidelines, the proportions of patients who underwent ECG, biological analysis, or chest X-ray were all >90 % in DeFSSICA. Similarly, BNP or pro-BNP was measured in 93 % of patients, compared with 82 % of patients in the OFICA study [4]. Not surprisingly, BNP and pro-BNP values were significantly higher among those with versus without HF in DeFSSICA. Several studies have shown the diagnostic and prognostic values of BNP (and troponin) in HF [16–18]; however, they have limited specificity and may be elevated secondary to a variety of causes [9]. Two recent papers have also suggested that neprilysin [19] and soluble CD146 [20] may have a role in the diagnosis of acute HF. Although BNP may be helpful when the diagnosis of HF is in doubt [21], ultrasound remains the gold standard. [22] The use of ultrasound in the ED has been reported [23] to accelerate the diagnosis of HF and the initiation of treatment, and shorten the length of stay. For example, in this study [24] the use of ultrasound could help early diagnosis and therapy for the patient who may need to transfer to the intensive care unit and reduce the length of stay for in-hospital patients. Several others studies have shown the feasibility of ultrasound in the ED and prehospital emergency management of HF patients [24–27]. As the diagnosis of acute HF remains difficult, ultrasound enables emergency physicians to improve their diagnostic performance, optimize their therapeutic strategy, and improve prognosis [28].. In the DeFSSICA survey, only 19 patients received lung ultrasound (LUS) evaluation in the ED. This result clearly shows that, for now, lung ultrasound is scarcely used by French emergency physicians. This fact is really different from the American or Italian practices where LUS is being used frequently. Lung ultrasound is an excellent differential diagnostic tool for distinguishing cardiac causes from pulmonary causes of dyspnea [29].
Pivetta et al. [30] definitively confirmed the excellent diagnostic performance of lung ultrasound to detect acute HF in an ED setting. In their multicenter study that included 1005 patients admitted with acute dyspnea, LUS sensitivity and specificity were respectively 97 % [95 % CI, 95–98.3 %] and 97.4 % [95 % CI, 95.7–98.6 %], and were superior to the one observed with clinical evaluation, chest X-ray and natriuretic peptides. Importantly, the net reclassification index of the LUS-implemented approach compared with standard workup was 19.1 % [30], which suggest the high diagnostic value of LUS in this setting. This performance of LUS has been confirmed in a prehospital setting by Prosen et al. (100 % sensitivity, 95 % specificity) [31]. So it’s probably a key to extend the training facilities for LUS in Europe, especially in France.
To date, the HF pathway of care has been poorly examined in the literature, in particular, patient destinations after ED discharge. It has been suggested that up to half of patients with HF may not require hospitalization [32]. However, in DeFSSICA, 95 % of HF patients were hospitalized, most commonly (28 %) in cardiology units. Approximately 14 % of HF patients were moved to ED hospitalization units, which provide close observation in the absence of a bed in the appropriate unit, or for patients due to be discharged the following day. Over one third of HF patients were hospitalized in non-cardiology units, particularly geriatric units (12 %). If the demonstration was made that the management of HF patients is more optimal in cardiology units [3], the choice of another destination may have been governed by a lack of beds in cardiology and/or the advanced age of some patients requiring a geriatric unit. Considering that majority of patients with AHF should be hospitalized in cardiology or ICU, we asked emergency physicians to assess whether the final destination was appropriate. In more than 75 % of cases they considered it adapted based on the diagnosis and the patient’s clinical status in ED. In 24 % of cases, the ED physician considered that the destination unit was not appropriate, mainly due to lack of beds availability in the unit perceived as appropriate.
In DeFSSICA, 18 % of HF patients had creatinine clearance <30 mL/min. Close cooperation with nephrologists is necessary in these patients, to determine whether dialysis is indicated [28, 33].
Although the incidence of HF decreased between 2000 and 2010 in relation to improvements in the management of myocardial infarction. Regarding to mortality, we have different data between Europe and the United States. While the mortality rate appears stable in the United States between the years 2000-2010 [34], there is a decrease between the years 1987–2008 in Europe [35]. In-hospital mortality of HF patients in DeFSSICA was 6.4 %, slightly lower than in the OFICA study [4] (8.2 %). At 30 days, 6.8 % of DeFSSICA HF patients were still hospitalized, while the median (IQR) length of stay was 7 (3–12) days. In the same idea, the length of stay in DeFSSICA is 7 days in median, like in EAHFE registry [3] and ALARM-HF [5] study which include the patients from the Emergency Department. However in OFICA [4] registry the length of stay is twice. This is probably explained by the inclusion of the patients admitted in intensive cardiac unit who are probably more serious.
Improved interdisciplinary cooperation has been highlighted as a key factor for the improvement of HF patient care [36]. An acute HF syndromes clinical trials network has been set up to improve clinical trials in this patient population [37]. Telemedicine [38] and wireless monitoring could also offer opportunities for improved HF management.
Limitations
First, the DeFSSICA study was focused only on patients in the ED. Additional prehospital data would be very valuable.
Our study has the strength and the limitation regarding internal and external validity of its multicenter national design. We believe that data collection at different settings, including academic, community, and regional hospitals, makes the result of this study largely applicable to the French healthcare system.
We acknowledge that BNP was not available in every patient despite the IIa European recommendation [14], which is suboptimal. However, it is likely to reflect the “real-life” use of BNP.
One of the limitations of our survey is that we only included dyspneic patients with suspected HF origin, instead of considering all dyspneic patients admitted to the ED. Thus, we found that 23 % of patients don’t have HF.
Finally, a limitation of this survey is that the discharge summary was not subject to expertise for the final diagnosis.
Conclusion
In conclusion, DeFSSICA has provided insights into the characteristics, diagnosis, treatment pathway, and outcomes of patients with acute HF in French emergency departments. As the diagnosis of AHF remains difficult, Ultrasound enables emergency physicians to improve their diagnostic performance, optimize their therapeutic strategy and improve prognosis. Our study highlights the need for the development of networks, such as those that exist for acute coronary syndromes, for improving the implementation of guidelines.
Abbreviations
- ACEIs:
-
Angiotensin-converting enzyme inhibitors
- ADHERE-EM:
-
Acute Decompensated Heart Failure National Registry Emergency Module
- ALARM-HF:
-
Acute Heart Failure Global Survey of Standard Treatment
- ARBs:
-
Angiotensin II receptor blockers
- BNP:
-
B-type natriuretic peptide
- CCTIRS:
-
Comité Consultatif sur le Traitement de l’Information en matière de Recherche dans le domaine de la Santé
- CNIL:
-
Commission Nationale de l’Informatique et des Libertés (National Commission for Liberties and Data Protection)
- COPD:
-
Chronic obstructive pulmonary disease
- CPAP:
-
Continuous positive airway pressure
- CRF:
-
Case report form
- DeFSSICA:
-
Description de la Filière de Soins dans les Syndromes d’Insuffisance Cardiaque Aigue
- EAHFE:
-
Epidemiology of Acute Heart Failure in Emergency Departments
- ED:
-
Emergency Department
- HF:
-
Heart failure
- IQRs:
-
Interquartile ranges
- LBBB:
-
Left bundle branch block
- LVEF:
-
Left ventricular ejection fraction
- OFICA:
-
Observatoire Français de l’Insuffisance Cardiaque Aiguë
- OPTIMIZE-HF:
-
Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure
- RESCUe:
-
Réseau Cardiologie Urgences (emergency cardiovascular network)
- SAMU:
-
Medical dispatch center (Service d’Aide Médicale Urgente)
- SFC:
-
Société Française de Cardiologie (French Society of Cardiology)
- SFMU:
-
Société Française de Médecine d’Urgence (French Society of Emergency Medicine)
References
Sayago-Silva I, Garcia-Lopez F, Segovia-Cubero J. Epidemiology of heart failure in Spain over the last 20 years. Rev Esp Cardiol (Engl Ed). 2013;66:649–56.
Malaquin D, Tribouilloy C. Epidemiology of heart failure. Rev Prat. 2010;60:911–5.
Collins SP, Storrow AB, Levy PD, et al. Early management of patients with acute heart failure: state of the art and future directions--a consensus document from the SAEM/HFSA acute heart failure working group. Acad Emerg Med. 2015;22:94–112.
Logeart D, Isnard R, Resche-Rigon M, et al. Current aspects of the spectrum of acute heart failure syndromes in a real-life setting: the OFICA study. Eur J Heart Fail. 2013;15:465–76.
Follath F, Yilmaz MB, Delgado JF, et al. Clinical presentation, management and outcomes in the Acute Heart Failure Global Survey of Standard Treatment (ALARM-HF). Intensive Care Med. 2011;37:619–26.
Llorens P, Escoda R, Miró Ò, et al. Characteristics and clinical course of patients with acute heart failure and the therapeutic measures applied in Spanish emergency departments: based on the EAHFE registry (Epidemiology of Acute Heart Failure in Emergency Departments). Emergencias. 2015;27:11–22.
Diercks DB, Fonarow GC, Kirk JD, et al. Risk stratification in women enrolled in the Acute Decompensated Heart Failure National Registry Emergency Module (ADHERE-EM). Acad Emerg Med. 2008;15:151–8.
Abraham WT, Fonarow GC, Albert NM, et al. Predictors of in-hospital mortality in patients hospitalized for heart failure: insights from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF). J Am Coll Cardiol. 2008;52:347–56.
Laskey WK, Alomari I, Cox M, et al. Heart rate at hospital discharge in patients with heart failure is associated with mortality and rehospitalization. J Am Heart Assoc. 2015;4:e001626.
Goodacre S, Stevens JW, Pandor A, et al. Prehospital noninvasive ventilation for acute respiratory failure: systematic review, network meta-analysis, and individual patient data meta-analysis. Acad Emerg Med. 2014;21:960–70.
Ducros L, Logeart D, Vicaut E, et al. CPAP for acute cardiogenic pulmonary oedema from out-of-hospital to cardiac intensive care unit: a randomised multicentre study. Intensive Care Med. 2011;37:1501–9.
Masip J, Roque M, Sanchez B, Fernandez R, Subirana M, Exposito JA. Noninvasive ventilation in acute cardiogenic pulmonary edema: systematic review and meta-analysis. JAMA. 2005;294:3124–30.
Carratalá JM, Masip J. Noninvasive ventilation in acute heart failure: use of continuous positive airway pressure in the emergency department. Emergencias. 2010;22:49–55.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, et al. 2016 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC)Developed with the Special Contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–200.
Pirozzi C, Numis FG, Pagano A, Melillo P, Copetti R, Schiraldi F. Immediate versus delayed integrated point-of-care-ultrasonography to manage acute dyspnea in the emergency department. Crit Ultrasound J. 2014;6:5.
Januzzi Jr JL, Peacock WF, Maisel AS, et al. Measurement of the interleukin family member ST2 in patients with acute dyspnea: results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) study. J Am Coll Cardiol. 2007;50:607–13.
Maisel AS, McCord J, Nowak RM, et al. Bedside B-Type natriuretic peptide in the emergency diagnosis of heart failure with reduced or preserved ejection fraction. Results from the Breathing Not Properly Multinational Study. J Am Coll Cardiol. 2003;41:2010–7.
Lassus J, Gayat E, Mueller C, et al. Incremental value of biomarkers to clinical variables for mortality prediction in acutely decompensated heart failure: the Multinational Observational Cohort on Acute Heart Failure (MOCA) study. Int J Cardiol. 2013;168:2186–94.
Seronde MF, Mebazaa A. Neprilysin: biotarget and biomarker in heart failure. JACC Heart Fail. 2015;3:645–6.
Gayat E, Caillard A, Laribi S, et al. Soluble CD146, a new endothelial biomarker of acutely decompensated heart failure. Int J Cardiol. 2015;199:241–7.
Vodovar N, Seronde MF, Laribi S, et al. Post-translational modifications enhance NT-proBNP and BNP production in acute decompensated heart failure. Eur Heart J. 2014;35:3434–41.
Mebazaa A, Yilmaz MB, Levy P, et al. Recommendations on pre-hospital & early hospital management of acute heart failure: a consensus paper from the Heart Failure Association of the European Society of Cardiology, the European Society of Emergency Medicine and the Society of Academic Emergency Medicine. Eur J Heart Fail. 2015;17:544–58.
Al Deeb M, Barbic S, Featherstone R, Dankoff J, Barbic D. Point-of-care ultrasonography for the diagnosis of acute cardiogenic pulmonary edema in patients presenting with acute dyspnea: a systematic review and meta-analysis. Acad Emerg Med. 2014;21(8):843–52.
Wang X, Liu D, He H, Du W, Zhang H, Liu Y, Chai W, Zhang Q, Zhou X. Using critical care chest ultrasonic examination in emergency consultation: a pilot study. Ultrasound Med Biol. 2015;41(2):401–6. doi:10.1016/j.ultrasmedbio.2014.09.010.
Prosen G, Klemen P, Strnad M, Grmec S. Combination of lung ultrasound (a comet-tail sign) and N-terminal pro-brain natriuretic peptide in differentiating acute heart failure from chronic obstructive pulmonary disease and asthma as cause of acute dyspnea in prehospital emergency setting. Crit Care. 2011;15:R114.
Hoyer HX, Vogl S, Schiemann U, Haug A, Stolpe E, Michalski T. Prehospital ultrasound in emergency medicine: incidence, feasibility, indications and diagnoses. Eur J Emerg Med. 2010;17:254–9.
Heegaard W, Hildebrandt D, Spear D, Chason K, Nelson B, Ho J. Prehospital ultrasound by paramedics: results of field trial. Acad Emerg Med. 2010;17:624–30.
Seronde MF, Laribi S, Collins SP, et al. Heart failure diagnosis in acute conditions has high agreement with inpatient diagnosis. Eur J Emerg Med. 2015. Epub ahead of print.
Liteplo AS, Marill KA, Villen T, Miller RM, Murray AF, Croft PE, Capp R, Noble VE. Emergency Thoracic Ultrasound in the Differentiation of the Etiology of Shortness of Breath (ETUDES): Sonographic B-Lines and N-Terminal Pro-Brain-Type Natriuretic Peptide in Diagnosing Congestive Heart Failure. Acad Emerg Med. 2009;16:201–10.
Pivetta E, Goffi A, Lupia E, Tizzani M, Porrino G, Ferreri E, Volpicelli G, et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED. Chest. 2015;148:202–10.
Prosen G, Klemen P, Strnad M, Grmec Š. Combination of Lung Ultrasound (a Comet-Tail Sign) and N-Terminal pro-Brain Natriuretic Peptide in Differentiating Acute Heart Failure from Chronic Obstructive Pulmonary Disease and Asthma as Cause of Acute Dyspnea in Prehospital Emergency Setting. Crit Care. 2011;15:R114.
Collins SP, Pang PS, Fonarow GC, Yancy CW, Bonow RO, Gheorghiade M. Is hospital admission for heart failure really necessary? The role of the emergency department and observation unit in preventing hospitalization and rehospitalization. J Am Coll Cardiol. 2013;61:121–6.
Nieminen MS, Brutsaert D, Dickstein K, et al. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006;27:2725–36.
Gerber Y, Weston SA, Redfield MM, et al. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern Med. 2015;175:996–1004.
Laribi S, Aouba A, Nikolaou M, et al. Trends in death attributed to heart failure over the past two decades in Europe. Eur J Heart Fail. 2012;14:234–9.
Mueller C, Christ M, Cowie M, et al. European Society of Cardiology-Acute Cardiovascular Care Association Position paper on acute heart failure: A call for interdisciplinary care. Eur Heart J Acute Cardiovasc Care. 2015. Epub ahead of print.
Collins SP, Levy PD, Lindsell CJ, et al. The rationale for an acute heart failure syndromes clinical trials network. J Card Fail. 2009;15:467–74.
Zannad F, Maugendre P, Audry A, et al. Telemedicine: what framework, what levels of proof, implementation rules. Therapie. 2014;69:339–54.
Acknowledgements
We would like to thank the emergency physicians and cardiologists who participated in this survey (CHU Toulouse, CHU Rouen, CHU Clermont Ferrand, CHU Nancy, CHR Metz-Thionville-Hôpital de Mercy, Hôpital Lariboisière-Paris, CHR Annecy Genevois, CHU Lyon-Hôp, Edouard Herriot, CHRU de Lille, Chu De Caen, CHU Nice-Hôpital Saint-Roch, CHU de Grenoble, Hôpital Bicêtre-Paris, Hôpital St Louis Paris, CH I Meulan, CH d’Avignon, CH Jacques Lacarin–Vichy, CH d’Aix En Provence, CH Fleyriat –Bourg En Bresse, CH Bourgoin Jallieu, CHU de Saint Etienne, CH du Forez Montbrison-Feurs, CH de Firminy, CH Villefranche-Sur-Saône, CHU De Brest, CH Henri Mondor, CH de Vienne). We also thank the RESCUe Network for the practical implementation of this survey and statistical analysis and Novartis France for its financial support. Editorial support for this paper was provided by Medlink Healthcare Communications Ltd. and was funded by the authors.
Funding and support
This work was supported by Novartis France, but the sponsor was not involved in the study protocol, methods, or choice of centers.
Availability of data and supporting materials
The database supporting the results of this article can be shared on reasonable request.
Authors’ contributions
CEK, SM-S, NP, SC, ME, DS, EB-C, SL, PH and TC conceived the study, designed the trial, and obtained research funding. CEK and TC supervised the conduct of the trial and data collection. CEK, NP, SC, DS and TC undertook recruitment of participating centers and patients and managed the data, including quality control. CEK and TC provided statistical advice on study design and analyzed the data; CEK chaired the data oversight committee. CEK and TC drafted the manuscript, and all authors contributed substantially to its revision. CEK and TC take responsibility for the paper as a whole. All authors read and approved the final manuscript.
Competing interests
Dr. El Khoury reports grants from NOVARTIS, outside the submitted work, Dr. Peschanski reports other from VYGON SA, from null, outside the submitted work; and Consultant for VYGON SA, manufacturer of the Boussignac© continuous positive airway pressure (CPAP) device. Dr. Charpentier reports personal fees from Novartis, outside the submitted work. Dr. Manzo-Silberman, Dr. Elbaz, Dr. Savary, Dr. Bonnefoy-Cudraz, Dr. Laribi, Dr. Henry, Dr. Girerd, Dr. Zannad and Dr Tahar Chouihed have nothing to disclose.
Consent for publication
Not applicable.
Ethics approval and consent to participate
DeFSSICA received approval from the National Commission for Liberties and Data Protection (Commission Nationale de l’Informatique et des Libertés [CNIL]) (number DR-2014-543) and the Advisory Committee on the Treatment of Information in the field of Health Research (Comité Consultatif sur le Traitement de l’Information en matière de Recherche dans le domaine de la Santé [CCTIRS]) (number 14–291). All patients received written information about the survey objectives.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Comparison of DeFSSICA survey and data of the main registers of heart failure. (DOCX 17.5 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chouihed, T., Manzo-Silberman, S., Peschanski, N. et al. Management of suspected acute heart failure dyspnea in the emergency department: results from the French prospective multicenter DeFSSICA survey. Scand J Trauma Resusc Emerg Med 24, 112 (2016). https://doi.org/10.1186/s13049-016-0300-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-016-0300-x