Abstract
Ovarian cancer (OC) is one of the deadliest malignant tumors affecting women worldwide. The predictive value of some blood inflammatory composite markers in OC has been extensively reported. They can be used for early detection and differential diagnosis of OC and can be used for predicting survival, treatment response, and recurrence in the affected patients. Here, we reviewed the predictive values of composite inflammatory markers based on complete blood count, namely neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), monocyte-to-lymphocyte ratio, and systemic inflammation index and markers based on blood protein, namely C-reactive protein-to-albumin ratio and prognostic nutritional index in OC, with a focus on NLR and PLR. We referred to the clinical studies on these six markers, reviewed the patient population, and summarized the marker cut-off values, significance, and limitations of these studies. All these studies were retrospective and most of them were single-center clinical studies with small sample sizes. We found that the cut-off values of these markers have not been unified, and methods used to determine these values varied among studies. The predictive value of these markers on survival was mainly reflected in the postoperative patients of multiple subtypes of ovarian cancer including epithelial OC, high-grade serous ovarian carcinoma, and ovarian clear cell carcinoma. We focused on NLR and PLR and calculated their pooled hazard ratios. NLR and PLR were reliable in predicting overall and progression-free survivals in patients with OC. Therefore, it is necessary to adjust important confounding factors and conduct a long-term follow-up prospective cohort study to further clarify the cut-off values of NLR and PLR and their clinical applications.
Similar content being viewed by others
Introduction
GLOBOCAN database (2020) included 313,959 new cases and 207,252 deaths for ovarian cancer (OC) [1]; these values were worse than those predicted in 2016 [2]. OC is the eighth most common cancer, accounting for 4.7% of all female cancer-related deaths and poses a serious threat to the lives and health of women worldwide [3]. OC is often regarded as a “silent killer” because of the lack of specific symptoms in the early stages and effective early diagnostic strategies [4]. Currently, surgery and platinum-based chemotherapy are the common treatment strategies for patients with OC [5, 6]. Although the initial remission rate of patients with OC is 60%–80%, 70% of patients with advanced OC relapse within 5 years of remission, and many acquire drug resistance [7, 8]. The five-year survival rate for patients with advanced ovarian cancer (stage III or IV) is < 30% whereas that for patients in early stages is 95% [9]. Survival prediction, early diagnosis, differential diagnosis, and treatment response prediction are required for patients with OC. Therefore, reliable markers are urgently required to guide the diagnosis and treatment options for patients and doctors.
The primary challenge is the diagnosis of OC, which includes differential diagnoses from other abdominal masses. Further, patients who receive chemotherapy may develop some adverse outcomes, such as drug resistance, recurrence, and death. Currently, we are unable to accurately predict the survival of patients with OC. Even before the occurrence of ovarian cancer, tumor cells induce the body to produce an environment suitable for tumor occurrence and development, including an inflammatory microenvironment. The British surgeon Stephen Paget first put forward the “seed-soil” theory, which laid the foundation for the concept of the tumor microenvironment. This is an extremely complex cellular network, in which a variety of inflammatory factors secreted by tumor and stromal cells (such as fibroblasts) construct an inflammatory microenvironment. This inflammatory microenvironment greatly affects the malignant characteristics of the tumors by regulating the biological processes involved in their development [10, 11]. This explains why even OC patients who are diagnosed and treated at early stages achieve poor outcomes. Therefore, evaluating inflammatory responses is crucial in the prognosis of OC. Uncontrollable inflammation plays an important role in inducing and promoting tumors, and the state of inflammation is reflected in the changes in blood inflammatory markers. Measurable parameters in the blood that reflect systemic inflammation include increased levels of leukocytes and their subtypes, elevated platelets, elevated C-reactive protein (CRP), and decreased albumin (ALB) [12, 13]. This evaluation approach is minimally invasive, low-cost, and easily available.
White blood cells are the largest group of inflammatory cells, and their several subtypes including neutrophils, lymphocytes, and monocytes are important inflammatory markers. Neutrophils can promote tumor progression by releasing tumor necrosis factors, interleukin-1 and interleukin-6 [14]. Lymphocytes are crucial in tumor-specific immune responses by inducing cytotoxic cell death and inhibiting the proliferation and migration of tumor cells [10]. Monocytes are involved in tumor occurrence, growth, migration, vascularization, invasion, and metastasis [15]. Therefore, white blood cells are considered the first traditional markers of inflammation. In recent years, the role of platelets as a marker of inflammation has been gradually recognized as they have distinct roles in inflammatory responses. Platelets can induce the epithelial–mesenchymal transformation of tumor cells in circulation and promote extravasation to the metastatic site [16]. Macrophages, neutrophils, and platelets present in the chronic inflammatory environment of tumors secrete cytokines, proteases, angiogenic factors, and chemokines [17]. Inflammation in cancer, caused by neutropenia, lymphopenia, monocytosis, and thrombocytosis, accelerates cancer progression by inducing angiogenesis, invasion, metastasis, and paraneoplastic phenomena [18,19,20]. In addition, some proteins in the blood, such as CRP and ALB, can reflect the inflammatory status of the body. These proteins have a certain correlation with the prognosis of OC [21]. However, a single blood parameter as an inflammatory marker does not reflect the state of inflammation; the values may represent secretion from tumor cells of an underlying infection. Therefore, it is complicated to evaluate the predictive values of such parameters in cancer. In addition, some currently used clinical indicators, such as the palliative prognostic index, play a good prognostic role and are easy to use without any invasive tests or the help of an experienced physician [22]. Yoshida et al. reported that cancer antigen 125 (CA125) is a better parameter than other complete blood count parameters for the prediction of ovarian tumors before surgery [23]. Therefore, the predictive value of inflammatory cells such as neutrophils and inflammatory proteins such as CRP is controversial in OC, and their use in clinical practice is not preferred.
Compared with single blood parameters as the inflammatory markers, the predictive value of blood inflammatory composite markers, such as neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), monocyte-to-lymphocyte ratio (MLR), systemic inflammation index (SII), C-reactive protein albumin ratio (CAR), and prognostic nutritional index (PNI), is better because of their sensitivity and stability. They have been confirmed to predict survival, treatment response, and diagnosis in patients with different OC, including epithelial ovarian cancer (EOC), high-grade serous ovarian carcinoma (HGSOC), and ovarian clear cell carcinoma (OCCC). Cramer et al. reported that NLR, PLR, and MLR could help us in the better identification of benign and malignant tumors [24] and in guiding changes in the chemotherapy regimen [25]. NLR is significantly increased in malignant ovarian cases and was the second most sensitive marker for predicting malignant tumors after cancer antigen 19–9 [26]. PLR values of ≥ 205.4 predicted incomplete remission in patients with OC (CR, accuracy is 71.6%) [27]. NLR and PLR can also be used to predict the distant metastasis of gynecological tumors [28]. Kokcu et al. reported that NLR and PLR showed an upward trend with the increase of OC stages [29]. Polat et al. confirmed through clinical studies that it was reasonable to observe the relationship between these hematological indexes and the prognosis of the disease. A high ratio may be an early sign of micrometastasis or dominant metastasis as well as a valuable prognostic index [30]. Meerwaldt et al. found that CRP and ALB could predict the prognosis of OC [31]. However, the study has suggested that PLR has no value in monitoring the postoperative status of patients with OC [32]; it was not significant in predicting the survival of patients with OC [33,34,35,36]. Topcu et al. showed that NLR was not an effective marker for predicting the malignant characteristics of pelvic masses [37]. Therefore, although these composite markers have been studied for many years, they are still not widely used in clinical practice compared with biomarkers such as serum CA125 and human epididymal protein 4. Currently, few guidelines or consensus statements emphasize the predictive value of these markers, and studies on these markers have not been well-summarized.
The inflammatory microenvironment can promote the occurrence and development of OC; however, the clinical studies on the predictive value of these blood inflammatory composite markers for OC have not been well-reviewed. The accuracy of prediction varies with the conditions of patients, time nodes, and other factors. The biomarkers for different subtypes of OC and the timelines for recording them have not been conclusively defined. This review critically summarizes the importance of blood inflammatory composite markers in predicting the occurrence and development of OC, elaborates on the advantages of using such biomarkers, and highlights future research directions to enhance their clinical applications.
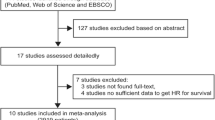
We screened PubMed, EMBASE, Web of Science, and Cochrane Library for studies that may meet our criteria until June 2022. The search terms were set to “ovarian neoplasms” OR “ovarian cancer” OR “cancer of ovary” AND “neutrophil-to-lymphocyte ratio,” “platelet-to-lymphocyte ratio,” “monocyte-to-lymphocyte ratio,” “systemic inflammation Index,” “C-reactive protein albumin ratio,” “prognostic nutritional index” (Table S1). We eliminated the repeated studies by verifying the author’s name, institution, number of participants, and baseline data. We ensured that all the studies were included in Science Citation Index for high research quality. The results were limited to humans with ovarian cancer and the language was limited to English. All results were imported into EndNote (Vision X9.2).
The data were extracted independently by Chuan-long Zhang, Xiao-chen Jiang, and Yi Li. The main extracted information included the biomarker studied, author, year, conditions of study participants, cut-off values, low/ high (number), marker significance, and limitations of the study. We also extracted the area under receiver operating characteristics curve (AUC) values from the studies that used AUC analyses to determine the biomarker cut-off values. We only extracted independent prediction outcomes from the studies that reported survival prediction. In addition, we extracted the “limitation” of the study without any subjective factors. We focused on NLR and PLR, visually analyzed the forest map of the hazard ratios (HR) of these two markers with survival data in the included studies, and calculated the pooled HRs. The quality of data extraction was ensured by Yan Chen and Bo Pang (Table S2).
Blood inflammatory composite markers based on complete blood count
NLR
We included 36 studies on NLR in our analysis, and 21 of them reported that NLR had an independent predictive value in predicting the survival of patients with OC. These studies included patients with EOC, HGSOC, and OCCC who had undergone surgery or chemotherapy. Cho et al. reported that preoperative high NLR predicted poor overall survival (OS) in patients with OC who underwent surgery [38], which was further confirmed by Li et al.[34, 36, 39,40,41,42,43,44,45,46]. Badora-Rybicka et al. observed NLR in 315 patients with EOC who received platinum-taxane chemotherapy after surgery, and found that high NLR could predict poor progression-free survival (PFS) but not OS [33]. Similar observations were reported by Feng et al. [47, 48]. Wang et al. found that the preoperative high NLR had predictive value for both poor OS and PFS in patients with OC [49,50,51,52]. Nakamura et al. suggested that higher NLR indicated higher mortality within 100 days of the failure of final-line chemotherapy [53]. Pinto et al. found that the increased NLR after surgery also predicted the poor OS of the patients [54]. Notably, similar observations were reported at different time nodes in these studies. Kim et al. noted the predictive value of NLR before treatment. Further, they also measured the dynamic changes in NLR during chemotherapy and confirmed that the increased NLR during chemotherapy was an independent predictor of PFS in patients with OC [55]. The pooled HR was 1.63 (95% CI: 1.39, 1.91; Fig. 1A) for the prediction of OS by NLR, and, the pooled HR was 1.69 (95% CI: 1.39, 2.05, Fig. 1B) for the prediction of PFS. The prediction value of NLR indicated its potential in predicting survival in patients with OC who underwent surgery. Overall, the pooled HRs showed that NLR could predict OS and PFS in patients with OC.
Several studies have focused on the importance of NLR in early diagnosis and in predicting treatment response and distant metastases of malignant tumors. Medina et al. showed that NLR was used to monitor the postoperative evolution of surgical patients, but could not be used to detect infectious complications [32]. Wang et al. stratified the value of NLR, which confirmed that NLR had a predictive value for chemotherapy response [49]. Several subsequent studies confirmed that high NLR before treatment or before surgery usually indicated poor surgical outcomes [42, 56, 57], poor efficacies of chemotherapy and immunotherapy [39, 43, 58, 59], or even drug resistance [60]. Inflammation could mediate drug resistance in cancer treatment [61]. In 2014 and 2015, Yildirim et al. demonstrated that preoperative NLR could be used for the early detection of ovarian malignant tumors, and preoperative NLR could predict the pathological diagnosis of adnexal masses [62, 63]. They concluded that the difference in preoperative NLR level could assist in the differential diagnosis of malignant and benign ovarian tumors; similar conclusions were reported in many other studies [26, 30, 64,65,66,67]. Chen et al. also confirmed the use of NLR in the differential diagnosis of OC and endometriosis [68]. Abu-Shawer et al. evaluated 264 patients with FIGO stage III and IV gynecological (endometrial, ovarian, and cervical) cancers and found that baseline NLR was a marker for predicting the presence of distant metastases [28] (Table 1). Currently, the cut-off values of NLR range from 0.89 to 6 with the most frequent values concentrated in the range from 2 to 4 (Table S3). However, Forget et al. reported similar values in healthy people (0.78 to 3.53) [69]. Therefore, the cut-value of NLR in predicting OC needs to be determined for clinical applications.
PLR
We analyzed 22 studies on PLR and found that 10 of them focused on the predictive value of PLR for predicting survival in patients with OC. Viren Asher et al. suggested, for the first time, that PLR may a new independent prognostic marker for patients with OC. Preoperative high PLR predicted poor OS [72]. Several authors [40, 49, 73, 74] had come to this conclusion. Zhang et al. [75] and Miao et al. [50] showed that PLR was also valuable in predicting PFS in addition to OS in OC. Farolfi et al. [39] observed the predictive value of PLR for PFS, whereas Jammal et al. [62] and Ramón-Rodríguez et al. [76] determined its predictive value in predicting disease-free survival (DFS). Yoshida et al. reported that elevated PLR was not useful in predicting adverse OS and PFS in patients with early-stage OCCC [36]. Jeerakornpassawat et al. confirmed high PLR is a potential independent predictive factor for poor survival outcomes of patients with EOC, fallopian tube, and primary peritoneal cancer treated with platinum-based chemotherapy [77]. In these studies, PLR was measured before surgery or before chemotherapy. For the prediction of OS by PLR, the pooled HR was 1.66 (95% CI: 1.41–1.96) (Fig. 2A), and for the prediction of PFS, the pooled HR was 1.61 (95%CI: 1.37–1.89) (Fig. 2B). This suggested that high PLR predicted poor OS and PFS in patients with OC. PLR may be less affected by infection and autoimmune diseases than NLR because platelets are used to calculate this ratio.
PLR could well predict the staging and surgical outcomes of patients with OC after surgery [78]. Several researchers [56, 57] also showed that PLR could predict surgical outcome in patients with OC. Winarno et al. determined that post-operative PLR could predict the response of patients to chemotherapy [59]. Abu-Shawer et al. showed that baseline PLR was a marker for predicting the presence of distant metastases in patients with FIGO stage III and IV gynecological (endometrial, ovarian, and cervical) cancers [28]. Yildirim et al. reported that PLR could play a predictive role in the early diagnosis of OC and could effectively predict the pathological diagnosis of adnexal masses in OC [62, 63]. Several researchers [30, 65, 79] showed that preoperative PLR was a predictive marker for ovarian malignant tumors. Wang et al. [80], and Li et al. [66] found that preoperative PLR was a predictor of the recurrence of OC. Yun et al. showed that preoperative high PLR suggested that ovarian cancer was more likely to occur than benign or borderline tumors [67] (Table 2). However, the cut-off values of PLR were different in all the studies because of the differences in methods used to obtain these values (Table S2). The cut-off values were obtained through the receiver operating characteristic (ROC) curve, log-rank test, or referring to previous studies. Therefore, standardized universal cut-off values for the blood inflammatory composite markers, including PLR, are not defined. And we found that the results of some studies did not fully support the conclusions of his study [78].
MLR and SII.
Few studies have reported the predictive value of MLR in patients with OC. Xiang et al. confirmed that preoperative MLR is a predictor of advanced stages, advanced pathologic grades, positive lymphatic metastasis, and OS in patients with OC [83]. Sastra et al. determined that higher preoperative MLR predicted worse surgical outcomes [57]. Guo et al. proposed a new diagnostic normal map model (including preoperative MLR) which predicted the degree of malignancy in patients with ovarian masses [84] (Table 3). MLR cut-off values ranged from 0.23 to 0.249 (Table S5).
Nie et al. found that preoperative high SII was an independent prognostic factor for poor OS and PFS in patients with OC [85]. Farolfi et al. [44] and Ramón-Rodríguez et al. [82] suggested that the value of high SII predicted OS in patients with OC. Farolfi et al. also showed that the baseline high SII independently indicated the poor efficacy of chemotherapy in patients with OC (Table 4). SII cut-off values ranged from 564.8 to 730 (Table S6).
Blood inflammatory composite markers based on blood protein
CAR and PNI
Liu et al. [35] and Komura et al. [86] conducted clinical studies on the CAR-based prediction of survival in patients with OC and found that high CAR before treatment was an independent marker for poor OS and disease-specific survival (DSS) (Table 5).
Miao et al. [87] suggested that PNI was an independent prognostic indicator for OS and PFS in OC patients. Some authors [88,89,90] pointed out that the decrease in PNI was an independent predictor of poor OS, but not PFS. PNI was an independent predictor of OS in patients in OC as a continuous variable [47]. Komura et al. showed that PNI was an independent prognostic factor for poor PFS and DSS [91]. Xing et al. found that postoperative PNI was an independent predictor of 1-year recurrence [90]. In patients with advanced OC, the increased PNI was not correlated with poor OS, but it helped predict the early stage of OC, and the predictive AUC for the efficacy of chemotherapy was 69%, which was an acceptable predictive value [92]. Miao et al. [73] also supported the observation that high PNI was an independent predictor of chemotherapy efficacy [87] (Table 6).
The two studies on CAR reported variable cut-off values, which may not be informative (Table S7). The cut-off values of PNI were between 42.9 and 50.4 (Table S8). Presently, there is no gold standard nutritional assessment method to predict the prognosis of patients with OC. It was difficult to compare the advantages and disadvantages of these two markers. We believed that the dynamic changes in these markers were related to the level of systemic inflammation and nutritional status, and the values changed more often because of the response to treatment. Therefore, we recommend that further research should focus on predicting the treatment response of patients with OC to provide guidance for patients and doctors on treatment choices. The dynamic values of these markers may be more significant than the baseline values.
Conclusion and Perspective
NLR, PLR, MLR, SII, CAR, and PNI have notable predictive value in predicting survival, treatment response, and diagnosis in patients with OC. Our review further emphasizes their predictive values. The analysis of these biomarkers is advantageous because of low cost, easy access, and less trauma, which can be beneficial for patients. Further, these blood inflammatory composite markers may have the potential to identify patients with high-risk OC as candidates for more intensive treatment in addition to standard treatment. The current predicted values and future research directions for these composite markers are illustrated in Fig. 3. We reviewed AUC in the existing clinical studies and found that these biomarkers had an acceptable predictive performance. However, the gap between clinical research and clinical applications of composite markers still exists because of two major reasons. First, their cut-off values have not been determined. Second, these values are easily affected by several confounding factors. Therefore, a prediction model is required to establish and verify the cut-off values of these composite biomarkers. A prospective multicenter study, including large sample size and assured follow-up, is required to generate data for building such a model.
Overview of predictive values of blood inflammatory composite markers in ovarian cancer and future research directions. NLR, neutrophil-to-lymphocyte ratio; PLR, platelet-to-lymphocyte ratio; MLR, monocyte-to-lymphocyte ratio; SII, systemic inflammation index; CAR, C-reactive protein-to-albumin ratio; PNI, prognostic nutritional index; OCP: ovarian cancer patients; EOCP: epithelial ovarian cancer patients; HGSOCP: high-grade serous ovarian carcinoma patients; OCCCP: ovarian clear cell carcinoma patients; CT, chemotherapy; NACT, neoadjuvant chemotherapy; OS, overall survival; PFS, progression-free survival; DFS, disease-free survival; DSS, disease-specific survival
Further, the dynamic changes in these markers may be of greater value and worthy of further studies. The differences in the timing of measuring these biomarkers, such as at diagnosis and before, during, and after treatment may have different implications for guiding clinical therapies. Even though neoadjuvant chemotherapy (NACT) for OC had always been controversial, its clinical efficacy is undeniable [93, 94]. However, none of the patients experienced NACT in the study population in which PLR was evaluated as a composite marker. Therefore, we have selected patients on NACT as our target group in our future study. The diagnostic values of the three markers SII, CAR, and PNI have not been determined; this is also a good direction for research. Presently, few researchers have worked on predicting the response to immunotherapy using such composite markers, and this aspect can be explored further. In the context of the study population, the number of studies focused on patients with EOC is higher than those focused on patients with OCCC and HGSOC. A comparison of the values of the same biomarker for different ovarian cancer subtypes would be immensely beneficial in guiding clinicians.
We extracted the limitations of the included studies without subjective factors and found that they had some common limitations: retrospective study design, small sample size, single-centric, and influence of confounding factors. Only one of the included studies had a prospective design [95]. These limitations biased their findings and decreased the reliability of their conclusions. In addition, we did not include studies on blood markers that can guide the prognosis of ovarian cancer, such as F-NLR [96], prognostic inflammation score [49], NLPN score (recurrent neutrophil–lymphocyte ratio × number of previous regimens) [89], and multiplication of neutrophil and monocyte counts [97], which may also be of great predictive value in OC. Clinicians urgently require better and cheaper biomarkers to predict the diagnosis and prognosis of patients with OC. However, the repetition of these studies is not advisable unless they have clinical applications. We recommend personalized medical research, higher-quality multicenter clinical studies, and more case observations for blood inflammatory composite markers to develop a comprehensive strategy for using these markers in predicting different parameters in patients with OC.
Availability of data and materials
All data are included in the manuscript.
Abbreviations
- AUC:
-
Area under the Curve
- ROC:
-
Receiver Operating Characteristic
- N:
-
Number of patients
- NA:
-
Not available
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PLR:
-
Platelet-to-lymphocyte ratio
- MLR:
-
Monocyte-to-lymphocyte ratio
- SII:
-
Systemic inflammation index
- CRP:
-
C-reactive protein
- ALB:
-
Albumin
- CAR:
-
C-reactive protein-to-albumin ratio
- PNI:
-
Prognostic nutritional index
- HR:
-
Hazard ratio
- 95% CI:
-
95% Confidence interval
- OC:
-
Ovarian cancer
- EOC:
-
Epithelial ovarian cancer
- HGSOC:
-
High-grade serous ovarian carcinoma
- OCCC:
-
Ovarian clear cell carcinoma
- OCP:
-
Ovarian cancer patients
- EOCP:
-
Epithelial ovarian cancer patients
- HGSOCP:
-
High-grade serous ovarian carcinoma patients
- OCCCP:
-
Ovarian clear cell carcinoma patients
- PDS:
-
Primary debulking surgery
- DS:
-
Debulking surgery
- CT:
-
Chemotherapy
- CTB:
-
Chemotherapy with bevacizumab
- NACT:
-
Neoadjuvant chemotherapy
- ICB:
-
Immune checkpoint blockade
- HIPEC:
-
Hyperthermic intraperitoneal chemotherapy
- CRS:
-
Cytoreductive surgery
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- DFS:
-
Disease-free survival
- DSS:
-
Disease-specific survival
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021. https://doi.org/10.3322/caac.21660.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30. https://doi.org/10.3322/caac.21332.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Atallah GA, Aziz Abd NH, Teik CK, Shafiee MN, Kampan NC. New Predictive Biomarkers for Ovarian Cancer. Diagnostics (Basel). 2021;11(3):465. https://doi.org/10.3390/diagnostics11030465.
Krzystyniak J, Ceppi L, Dizon DS, Birrer MJ. Epithelial ovarian cancer: the molecular genetics of epithelial ovarian cancer. Ann Oncol. 2016;27(Suppl 1):i4–10. https://doi.org/10.1093/annonc/mdw083.
Lee YJ, Kim HS, Rim JH, Lee JY, Nam EJ, Kim SW, et al. Germline BRCA, chemotherapy response scores, and survival in the neoadjuvant treatment of ovarian cancer. BMC Cancer. 2020;20(1):185. https://doi.org/10.1186/s12885-020-6688-8.
Palaia I, Tomao F, Sassu CM, Musacchio L, Benedetti PP. Immunotherapy For Ovarian Cancer: Recent Advances And Combination Therapeutic Approaches. Onco Targets Ther. 2020;13:6109–29. https://doi.org/10.2147/OTT.S205950.
Jayson GC, Kohn EC, Kitchener HC, Ledermann JA. Ovarian cancer. Lancet. 2014;384(9951):1376–88. https://doi.org/10.1016/S0140-6736(13)62146-7.
Prat J. Pathology of borderline and invasive cancers. Best Pract Res Clin Obstet Gynaecol. 2017;41:15–30. https://doi.org/10.1016/j.bpobgyn.2016.08.007.
Arneth B. Tumor Microenvironment. Medicina (Kaunas). 2019;56(1):15. https://doi.org/10.3390/medicina56010015.
Kulbe H, Chakravarty P, Leinster DA, Charles KA, Kwong J, Thompson RG, et al. A dynamic inflammatory cytokine network in the human ovarian cancer microenvironment. Cancer Res. 2012;72(1):66–75. https://doi.org/10.1158/0008-5472.CAN-11-2178.
Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010;6(1):149–63. https://doi.org/10.2217/fon.09.136.
Glare P. Clinical predictors of survival in advanced cancer. J Support Oncol. 2005;3(5):331–9.
Hedrick CC, Malanchi I. Neutrophils in cancer: heterogeneous and multifaceted. Nat Rev Immunol. 2022;22(3):173–87. https://doi.org/10.1038/s41577-021-00571-6.
Olingy CE, Dinh HQ, Hedrick CC. Monocyte heterogeneity and functions in cancer. J Leukoc Biol. 2019;106(2):309–22. https://doi.org/10.1002/JLB.4RI0818-311R.
Cedervall J, Hamidi A, Olsson AK. Platelets, NETs and cancer. Thromb Res. 2018;164(Suppl 1):S148–52. https://doi.org/10.1016/j.thromres.2018.01.049.
Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493-503. https://doi.org/10.1016/S1470-2045(14)70263-3.
Stone RL, Nick AM, McNeish IA, Balkwill F, Han HD, Bottsford-Miller J, et al. Paraneoplastic thrombocytosis in ovarian cancer. N Engl J Med. 2012;366(7):610–8. https://doi.org/10.1056/NEJMoa1110352.
Huang H, Liu Q, Zhu L, Zhang Y, Lu X, Wu Y, et al. Prognostic Value of Preoperative Systemic Immune-Inflammation Index in Patients with Cervical Cancer. Sci Rep. 2019;9(1):3284. https://doi.org/10.1038/s41598-019-39150-0.
Stoiber D, Assinger A. Platelet-Leukocyte Interplay in Cancer Development and Progression. Cells. 2020;9(4):855. https://doi.org/10.3390/cells9040855.
Kodama J, Miyagi Y, Seki N, Tokumo K, Yoshinouchi M, Kobashi Y, et al. Serum C-reactive protein as a prognostic factor in patients with epithelial ovarian cancer. Eur J Obstet Gynecol Reprod Biol. 1999;82(1):107–10. https://doi.org/10.1016/s0301-2115(98)00227-9.
Lee SH, Lee JG, Choi YJ, Seol YM, Kim H, Kim YJ, et al. Prognosis palliative care study, palliative prognostic index, palliative prognostic score and objective prognostic score in advanced cancer: a prospective comparison. BMJ Support Palliat Care. 2021. https://doi.org/10.1136/bmjspcare-2021-003077.
Yoshida A, Sarian LO, Marangoni MJ, Firmano IC, Derchain SF. Diagnostic Value of the Neutrophil/Lymphocyte Ratio, Platelet/Lymphocyte Ratio, and Thrombocytosis in the Preoperative Investigation of Ovarian Masses. Rev Bras Ginecol Obstet. 2020;42(7):397–403. https://doi.org/10.1055/s-0040-1712991.
Cramer DW, Benjamin Iv WJ, Vitonis AF, Berkowitz R, Goodman A, Matulonis U. Differential blood count as triage tool in evaluation of pelvic masses. Int J Gynecol Cancer. 2021;31(5):733–43. https://doi.org/10.1136/ijgc-2019-001103.
Huang CY, Yang YC, Wang KL, Chen TC, Chen JR, Weng CS, et al. Possible surrogate marker for an effective dose-dense chemotherapy in treating ovarian cancer. Taiwan J Obstet Gynecol. 2016;55(3):405–9. https://doi.org/10.1016/j.tjog.2016.04.017.
Seckin KD, Karslı MF, Yucel B, Bestel M, Yıldırım D, Canaz E, et al. The utility of tumor markers and neutrophil lymphocyte ratio in patients with an intraoperative diagnosis of mucinous borderline ovarian tumor. Eur J Obstet Gynecol Reprod Biol. 2016;196:60–3. https://doi.org/10.1016/j.ejogrb.2015.10.025.
Kim HS, Choi HY, Lee M, Suh DH, Kim K, No JH, et al. Systemic Inflammatory Response Markers and CA-125 Levels in Ovarian Clear Cell Carcinoma: A Two Center Cohort Study. Cancer Res Treat. 2016;48(1):250–8. https://doi.org/10.4143/crt.2014.324.
Abu-Shawer O, Abu-Shawer M, Hirmas N, Alhouri A, Massad A, Alsibai B, et al. Hematologic markers of distant metastases and poor prognosis in gynecological cancers. BMC Cancer. 2019;19(1):141. https://doi.org/10.1186/s12885-019-5326-9.
Kokcu A, Kurtoglu E, Celik H, Tosun M, Malatyalioglu E, Ozdemir AZ. May the platelet to lymphocyte ratio be a prognostic factor for epithelial ovarian cancer? Asian Pac J Cancer Prev. 2014;15(22):9781–4. https://doi.org/10.7314/apjcp.2014.15.22.9781.
Polat M, Senol T, Ozkaya E, Ogurlu Pakay G, Cikman MS, Konukcu B, et al. Neutrophil to lymphocyte and platelet to lymphocyte ratios increase in ovarian tumors in the presence of frank stromal invasion. Clin Transl Oncol. 2016;18(5):457–63. https://doi.org/10.1007/s12094-015-1387-7.
Meerwaldt JH, Haije WG, Cooper EH, Pidcock NB, Burg ME v d. Biochemical aids in the monitoring of patients with ovarian cancer. Gynecol Oncol. 1983;16(2):209–18. https://doi.org/10.1016/0090-8258(83)90095-1.
Medina Fernández FJ, Muñoz-Casares FC, Arjona-Sánchez A, Casado-Adam A, Gómez-Luque I, Garcilazo Arismendi DJ, et al. Postoperative time course and utility of inflammatory markers in patients with ovarian peritoneal carcinomatosis treated with neoadjuvant chemotherapy, cytoreductive surgery, and HIPEC. Ann Surg Oncol. 2015;22(4):1332–40. https://doi.org/10.1245/s10434-014-4096-5.
Badora-Rybicka A, Nowara E, Starzyczny-Slota D. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio before chemotherapy as potential prognostic factors in patients with newly diagnosed epithelial ovarian cancer. ESMO Open. 2016;1(2):e000039.
Li Z, Hong N, Robertson M, Wang C, Jiang G. Preoperative red cell distribution width and neutrophil-to-lymphocyte ratio predict survival in patients with epithelial ovarian cancer. Sci Rep. 2017;7:43001. https://doi.org/10.1038/srep43001.
Liu Y, Chen S, Zheng C, Ding M, Zhang L, Wang L, et al. The prognostic value of the preoperative c-reactive protein/albumin ratio in ovarian cancer. BMC Cancer. 2017;17(1):285. https://doi.org/10.1186/s12885-017-3220-x.
Yoshida K, Yoshikawa N, Shirakawa A, Niimi K, Suzuki S, Kajiyama H, et al. Prognostic value of neutrophil-to-lymphocyte ratio in early-stage ovarian clear-cell carcinoma. J Gynecol Oncol. 2019;30(6):e85.
Topcu HO, Guzel AI, Ozer I, Kokanali MK, Gokturk U, Muftuoglu KH, et al. Comparison of neutrophil/lymphocyte and platelet/ lymphocyte ratios for predicting malignant potential of suspicious ovarian masses in gynecology practice. Asian Pac J Cancer Prev. 2014;15(15):6239–41. https://doi.org/10.7314/apjcp.2014.15.15.6239.
Cho H, Hur HW, Kim SW, Kim SH, Kim JH, Kim YT, et al. Pre-treatment neutrophil to lymphocyte ratio is elevated in epithelial ovarian cancer and predicts survival after treatment. Cancer Immunol Immunother. 2009;58(1):15–23. https://doi.org/10.1007/s00262-008-0516-3.
Farolfi A, Petrone M, Scarpi E, Galla V, Greco F, Casanova C, et al. Inflammatory Indexes as Prognostic and Predictive Factors in Ovarian Cancer Treated with Chemotherapy Alone or Together with Bevacizumab. A Multicenter, Retrospective Analysis by the MITO Group (MITO 24). Target Oncol. 2018;13(4):469–79. https://doi.org/10.1007/s11523-018-0574-1.
Ceran MU, Tasdemir U, Colak E, Güngör T. Can complete blood count inflammatory parameters in epithelial ovarian cancer contribute to prognosis? - a survival analysis. J Ovarian Res. 2019;12(1):16. https://doi.org/10.1186/s13048-019-0491-7.
Salman L, Sabah G, Jakobson-Setton A, Raban O, Yeoshoua E, Eitan R. Neutrophil-to-lymphocyte ratio as a prognostic factor in advanced stage ovarian carcinoma treated with neoadjuvant chemotherapy. Int J Gynaecol Obstet. 2020;148(1):102–6. https://doi.org/10.1002/ijgo.12986.
Nguyen JMV, Ferguson SE, Bernardini MQ, May T, Laframboise S, Hogen L, et al. Preoperative neutrophil-to-lymphocyte ratio predicts 30 day postoperative morbidity and survival after primary surgery for ovarian cancer. Int J Gynecol Cancer. 2020;30(9):1378–83. https://doi.org/10.1136/ijgc-2020-001378.
Henriksen JR, Nederby L, Donskov F, Waldstrøm M, Adimi P, Jakobsen A, et al. Prognostic significance of baseline T cells, B cells and neutrophil-lymphocyte ratio (NLR) in recurrent ovarian cancer treated with chemotherapy. J Ovarian Res. 2020;13(1):59. https://doi.org/10.1186/s13048-020-00661-4.
Farolfi A, Scarpi E, Greco F, Bergamini A, Longo L, Pignata S, et al. Inflammatory indexes as predictive factors for platinum sensitivity and as prognostic factors in recurrent epithelial ovarian cancer patients: a MITO24 retrospective study. Sci Rep. 2020;10(1):18190. https://doi.org/10.1038/s41598-020-75316-x.
John-Olabode SO, Okunade KS, Olorunfemi G, Soibi-Harry A, Rimi G, Osunwusi B, et al. Pretreatment Neutrophil-to-Lymphocyte Ratio: A Prognostic Biomarker of Survival in Patients With Epithelial Ovarian Cancer. Cureus. 2021;13(7):e16429. https://doi.org/10.7759/cureus.16429.
Liontos M, Andrikopoulou A, Koutsoukos K, Markellos C, Skafida E, Fiste O, et al. Neutrophil-to-lymphocyte ratio and chemotherapy response score as prognostic markers in ovarian cancer patients treated with neoadjuvant chemotherapy. J Ovarian Res. 2021;14(1):148. https://doi.org/10.1186/s13048-021-00902-0.
Feng Z, Wen H, Ju X, Bi R, Chen X, Yang W, et al. The preoperative prognostic nutritional index is a predictive and prognostic factor of high-grade serous ovarian cancer. BMC Cancer. 2018;18(1):883. https://doi.org/10.1186/s12885-018-4732-8.
Komura N, Mabuchi S, Yokoi E, Kozasa K, Kuroda H, Sasano T, et al. Comparison of clinical utility between neutrophil count and neutrophil-lymphocyte ratio in patients with ovarian cancer: a single institutional experience and a literature review. Int J Clin Oncol. 2018;23(1):104–13. https://doi.org/10.1007/s10147-017-1180-4.
Wang YQ, Jin C, Zheng HM, Zhou K, Shi BB, Zhang Q, et al. A novel prognostic inflammation score predicts outcomes in patients with ovarian cancer. Clin Chim Acta. 2016;456:163–9. https://doi.org/10.1016/j.cca.2016.03.013.
Miao Y, Yan Q, Li S, Li B, Feng Y. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio are predictive of chemotherapeutic response and prognosis in epithelial ovarian cancer patients treated with platinum-based chemotherapy. Cancer Biomark. 2016;17(1):33–40. https://doi.org/10.3233/cbm-160614.
Zhou M, Li L, Wang X, Wang C, Wang D. Neutrophil-to-Lymphocyte Ratio and Platelet Count Predict Long-Term Outcome of Stage IIIC Epithelial Ovarian Cancer. Cell Physiol Biochem. 2018;46(1):178–86. https://doi.org/10.1159/000488420.
Baert T, Van Camp J, Vanbrabant L, Busschaert P, Laenen A, Han S, et al. Influence of CA125, platelet count and neutrophil to lymphocyte ratio on the immune system of ovarian cancer patients. Gynecol Oncol. 2018;150(1):31–7. https://doi.org/10.1016/j.ygyno.2018.05.004.
Nakamura K, Nagasaka T, Nishida T, Haruma T, Ogawa C, Kusumoto T, et al. Neutrophil to lymphocyte ratio in the pre-treatment phase of final-line chemotherapy predicts the outcome of patients with recurrent ovarian cancer. Oncol Lett. 2016;11(6):3975–81. https://doi.org/10.3892/ol.2016.4513.
Pinto MP, Balmaceda C, Bravo ML, Kato S, Villarroel A, Owen GI, et al. Patient inflammatory status and CD4+/CD8+ intraepithelial tumor lymphocyte infiltration are predictors of outcomes in high-grade serous ovarian cancer. Gynecol Oncol. 2018;151(1):10–7. https://doi.org/10.1016/j.ygyno.2018.07.025.
Kim YJ, Lee I, Chung YS, Nam E, Kim S, Kim SW, et al. Pretreatment neutrophil-to-lymphocyte ratio and its dynamic change during neoadjuvant chemotherapy as poor prognostic factors in advanced ovarian cancer. Obstet Gynecol Sci. 2018;61(2):227–34. https://doi.org/10.5468/ogs.2018.61.2.227.
Ashrafganjoei T, Mohamadianamiri M, Farzaneh F, Hosseini MS, Arab M. Investigating Preoperative Hematologic Markers for Prediction of Ovarian Cancer Surgical Outcome. Asian Pac J Cancer Prev. 2016;17(3):1445–8. https://doi.org/10.7314/apjcp.2016.17.3.1445.
Sastra WIG, Aditya PPK, Gradiyanto OE, Ketut S. Predictive value of preoperative inflammatory markers and serum CA 125 level for surgical outcome in Indonesian women with epithelial ovarian cancer. Cancer Biomark. 2022;34(1):123–9. https://doi.org/10.3233/cbm-201415.
Boland JL, Zhou Q, Martin M, Callahan MK, Konner J, O’Cearbhaill RE, et al. Early disease progression and treatment discontinuation in patients with advanced ovarian cancer receiving immune checkpoint blockade. Gynecol Oncol. 2019;152(2):251–8. https://doi.org/10.1016/j.ygyno.2018.11.025.
Winarno GNA, Pasaribu M, Susanto H, Nisa AS, Harsono AB, Yuseran H, et al. The Platelet to Lymphocyte and Neutrophil to Lymphocyte Ratios in Predicting Response to Platinum-based Chemotherapy for Epithelial Ovarian Cancer. Asian Pac J Cancer Prev. 2021;22(5):1561–6. https://doi.org/10.31557/apjcp.2021.22.5.1561.
Chen W, Zhong S, Shan B, Zhou S, Wu X, Yang H, et al. Serum D-dimer, albumin and systemic inflammatory response markers in ovarian clear cell carcinoma and their prognostic implications. J Ovarian Res. 2020;13(1):89. https://doi.org/10.1186/s13048-020-00693-w.
Beatty GL. Overcoming Therapeutic Resistance by Targeting Cancer Inflammation. Am Soc Clin Oncol Educ Book. 2016;35:e168–73. https://doi.org/10.14694/EDBK_15894810.1200/EDBK_158948.
Yildirim MA, Seckin KD, Togrul C, Baser E, Karsli MF, Gungor T, et al. Roles of neutrophil/lymphocyte and platelet/lymphocyte ratios in the early diagnosis of malignant ovarian masses. Asian Pac J Cancer Prev. 2014;15(16):6881–5. https://doi.org/10.7314/apjcp.2014.15.16.6881.
Yildirim M, Demir Cendek B, Filiz AA. Differentiation between benign and malignant ovarian masses in the preoperative period using neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios. Mol Clin Oncol. 2015;3(2):317–21. https://doi.org/10.3892/mco.2014.481.
Wu YY, Qin YY, Qin JQ, Zhang X, Lin FQ. Diagnostic value of derived neutrophil-to-lymphocyte ratio in patients with ovarian cancer. J Clin Lab Anal. 2019;33(4):e22833. https://doi.org/10.1002/jcla.22833.
Eo WK, Kim KH, Park EJ, Kim HY, Kim HB, Koh SB, et al. Diagnostic accuracy of inflammatory markers for distinguishing malignant and benign ovarian masses. J Cancer. 2018;9(7):1165–72. https://doi.org/10.7150/jca.23606.
Li L, Tian J, Zhang L, Liu L, Sheng C, Huang Y, et al. Utility of Preoperative Inflammatory Markers to Distinguish Epithelial Ovarian Cancer from Benign Ovarian Masses. J Cancer. 2021;12(9):2687–93. https://doi.org/10.7150/jca.51642.
Yun TH, Jeong YY, Lee SJ, Choi YS, Ryu JM. Neutrophil-Lymphocyte and Platelet-Lymphocyte Ratios in Preoperative Differential Diagnosis of Benign, Borderline, and Malignant Ovarian Tumors. J Clin Med. 2022;11(5):1355. https://doi.org/10.3390/jcm11051355.
Chen L, Wang X, Shu J, Xu S, Wu Q, Yu Y. Diagnostic value of serum D-dimer, CA125, and neutrophil-to-lymphocyte ratio in differentiating ovarian cancer and endometriosis. Int J Gynaecol Obstet. 2019;147(2):212–8. https://doi.org/10.1002/ijgo.12949.
Forget P, Khalifa C, Defour JP, Latinne D, Van Pel MC, De Kock M. What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Res Notes. 2017;10(1):12. https://doi.org/10.1186/s13104-016-2335-5.
Badora-Rybicka A, Nowara E, Starzyczny-Słota D. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio before chemotherapy as potential prognostic factors in patients with newly diagnosed epithelial ovarian cancer. ESMO Open. 2016;1(2):e000039.
Feng Z, Wen H, Bi R, Ju X, Chen X, Yang W, et al. Preoperative Neutrophil-to-Lymphocyte Ratio as a Predictive and Prognostic Factor for High-Grade Serous Ovarian Cancer. PLoS One. 2016;11(5):e0156101.
Asher V, Lee J, Innamaa A, Bali A. Preoperative platelet lymphocyte ratio as an independent prognostic marker in ovarian cancer. Clin Transl Oncol. 2011;13(7):499–503. https://doi.org/10.1007/s12094-011-0687-9.
Hu D, Lin Y, Liu F, Zeng L, Ouyang X, Wang K, et al. Elevated Preoperative Platelet to Lymphocyte Ratio Indicates Poor Survival in Patients with Resected High-grade Serous Ovarian Carcinoma. Clin Lab. 2016;62(8):1443–9. https://doi.org/10.7754/Clin.Lab.2016.151137.
Chon S, Lee S, Jeong D, Lim S, Lee K, Shin J. Elevated platelet lymphocyte ratio is a poor prognostic factor in advanced epithelial ovarian cancer. J Gynecol Obstet Hum Reprod. 2021;50(6):101849.
Zhang WW, Liu KJ, Hu GL, Liang WJ. Preoperative platelet/lymphocyte ratio is a superior prognostic factor compared to other systemic inflammatory response markers in ovarian cancer patients. Tumour Biol. 2015;36(11):8831–7. https://doi.org/10.1007/s13277-015-3533-9.
Ramon-Rodriguez J, De-Armas-Conde N, Jaen-Torrejimeno I, Prada-Villaverde A, Rojas-Holguin A, Lopez-Guerra D, et al. Prognostic value of pre-operative systemic immune-inflammation index and platelet to lymphocyte ratio in peritoneal carcinomatosis of ovarian origin. Surg Oncol. 2022;42:101750.
Jeerakornpassawat D, Suprasert P. Potential predictors for chemotherapeutic response and prognosis in epithelial ovarian, fallopian tube and primary peritoneal cancer patients treated with platinum-based chemotherapy. Obstet Gynecol Sci. 2020;63(1):55–63. https://doi.org/10.5468/ogs.2020.63.1.55.
Raungkaewmanee S, Tangjitgamol S, Manusirivithaya S, Srijaipracharoen S, Thavaramara T. Platelet to lymphocyte ratio as a prognostic factor for epithelial ovarian cancer. J Gynecol Oncol. 2012;23(4):265–73. https://doi.org/10.3802/jgo.2012.23.4.265.
Ozaksit G, Tokmak A, Kalkan H, Yesilyurt H. Value of the platelet to lymphocyte ratio in the diagnosis of ovarian neoplasms in adolescents. Asian Pac J Cancer Prev. 2015;16(5):2037–41. https://doi.org/10.7314/apjcp.2015.16.5.2037.
Wang N, Li C, Yang Y, Guan Y, Wang F, Wang Y, et al. The Use of Platelet/Lymphocyte Ratio and Cancer Antigen 125 Combined with Magnetic Resonance Diffusion-Weighted Imaging in Diagnosis of Recurrent Ovarian Cancer and Neuropathic Pain. World Neurosurgery. 2021;149:502–10. https://doi.org/10.1016/j.wneu.2020.11.117.
Jammal MP, Martins Filho A, Bandeira GH, Murta BMT, Murta EFC, Nomelini RS. Laboratory predictors of survival in ovarian cancer. Rev Assoc Med Bras (1992). 2020;66(1):61–6. https://doi.org/10.1590/1806-9282.66.1.61.
Ramón-Rodríguez J, De-Armas-Conde N, Jaén-Torrejimeno I, Prada-Villaverde A, Rojas-Holguín A, López-Guerra D, et al. Prognostic value of pre-operative systemic immune-inflammation index and platelet to lymphocyte ratio in peritoneal carcinomatosis of ovarian origin. Surg Oncol. 2022;42:101750.
Xiang J, Zhou L, Li X, Bao W, Chen T, Xi X, et al. Preoperative Monocyte-to-Lymphocyte Ratio in Peripheral Blood Predicts Stages, Metastasis, and Histological Grades in Patients with Ovarian Cancer. Transl Oncol. 2017;10(1):33–9. https://doi.org/10.1016/j.tranon.2016.10.006.
Guo Y, Jiang T, Ouyang L, Li X, He W, Zhang Z, et al. A novel diagnostic nomogram based on serological and ultrasound findings for preoperative prediction of malignancy in patients with ovarian masses. Gynecol Oncol. 2021;160(3):704–12. https://doi.org/10.1016/j.ygyno.2020.12.006.
Nie D, Gong H, Mao X, Li Z. Systemic immune-inflammation index predicts prognosis in patients with epithelial ovarian cancer: A retrospective study. Gynecol Oncol. 2019;152(2):259–64. https://doi.org/10.1016/j.ygyno.2018.11.034.
Komura N, Mabuchi S, Shimura K, Kawano M, Matsumoto Y, Kimura T. Significance of Pretreatment C-Reactive Protein, Albumin, and C-Reactive Protein to Albumin Ratio in Predicting Poor Prognosis in Epithelial Ovarian Cancer Patients. Nutr Cancer. 2021;73(8):1357–64. https://doi.org/10.1080/01635581.2020.1798479.
Miao Y, Li S, Yan Q, Li B, Feng Y. Prognostic Significance of Preoperative Prognostic Nutritional Index in Epithelial Ovarian Cancer Patients Treated with Platinum-Based Chemotherapy. Oncol Res Treat. 2016;39(11):712–9. https://doi.org/10.1159/000452263.
Zhang W, Ye B, Liang W, Ren Y. Preoperative prognostic nutritional index is a powerful predictor of prognosis in patients with stage III ovarian cancer. Sci Rep. 2017;7(1):9548. https://doi.org/10.1038/s41598-017-10328-8.
Yoshikawa N, Yoshida K, Tamauchi S, Ikeda Y, Nishino K, Niimi K, et al. The Preoperative Prognostic Nutritional Index for the Prediction of Outcomes in Patients with Early-Stage Ovarian Clear Cell Carcinoma. Sci Rep. 2020;10(1):7135. https://doi.org/10.1038/s41598-020-64171-5.
Xing L, Chen R, Qian J, Ren J, Deng X. A comparison of three preoperative nutritional assessment methods for predicting ovarian cancer patient prognosis: which is better? Support Care Cancer. 2022;30(6):5221–9. https://doi.org/10.1007/s00520-022-06941-7.
Komura N, Mabuchi S, Yokoi E, Shimura K, Kawano M, Matsumoto Y, et al. Prognostic significance of the pretreatment prognostic nutritional index in patients with epithelial ovarian cancer. Oncotarget. 2019;10(38):3605–13. https://doi.org/10.18632/oncotarget.26914.
Karakas S, Demirayak G, Onder AB, Ozdemir IA, Comba C, Suzen Caypinar S, et al. The Association between the Preoperative Prognostic Nutritional Index and the Controlling Nutritional Status Score on Tumor Stage, Chemotherapeutic Response and Overall Survival in Ovarian Cancer. Nutr Cancer. 2022;74(5):1770–9. https://doi.org/10.1080/01635581.2021.2022170.
Wright AA, Bohlke K, Armstrong DK, Bookman MA, Cliby WA, Coleman RL, et al. Neoadjuvant chemotherapy for newly diagnosed, advanced ovarian cancer: Society of Gynecologic Oncology and American Society of Clinical Oncology Clinical Practice Guideline. Gynecol Oncol. 2016;143(1):3–15. https://doi.org/10.1016/j.ygyno.2016.05.022.
Wright AA, Bohlke K, Armstrong DK, Bookman MA, Cliby WA, Coleman RL, et al. Neoadjuvant Chemotherapy for Newly Diagnosed, Advanced Ovarian Cancer: Society of Gynecologic Oncology and American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2016;34(28):3460–73. https://doi.org/10.1200/JCO.2016.68.6907.
Sanna E, Tanca L, Cherchi C, Gramignano G, Oppi S, Chiai MG, et al. Decrease in Neutrophil-to-Lymphocyte Ratio during Neoadjuvant Chemotherapy as a Predictive and Prognostic Marker in Advanced Ovarian Cancer. Diagnostics (Basel). 2021;11(1):1298. https://doi.org/10.3390/diagnostics11071298.
Yang J, Ma J, Cheng S, Wang Y. The Combination of Plasma Fibrinogen Concentration and Neutrophil Lymphocyte Ratio (F-NLR) as a Prognostic Factor of Epithelial Ovarian Cancer. Onco Targets Ther. 2020;13:7283–93. https://doi.org/10.2147/ott.S264118.
Paik ES, Shim M, Choi HJ, Lee YY, Kim TJ, Choi CH, et al. Preoperative multiplication of neutrophil and monocyte counts as a prognostic factor in epithelial ovarian cancer. Cancer Biomark. 2016;17(4):419–25. https://doi.org/10.3233/cbm-160658.
Acknowledgements
We are grateful for the reviewers’ comments and suggestions, which helped us to improve the manuscript. We also thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Funding
This research was supported by the Natural Science Foundation of Beijing (General Program, Grant no.7222296); and the Scientific and Technological Innovation Project of China Academy of Chinese Medical Sciences (Grant no.CI2021A01805).
Author information
Authors and Affiliations
Contributions
CL.Z. and B.P. developed the study concept and design. CL.Z., XC.J. and Y.L. performed the initial literature review. CL.Z., XC.J., Y.L., X.P., and MQ.G. participated in extracting data. CL.Z. and Y.C. wrote the first draft. CL.Z., XC.J., Y.L., X.P., MQ.G., Y.C., and B.P. participated in the development and revisions of the manuscript. Obtained funding and study supervision by B.P. All authors contributed to the writing of the final manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, Cl., Jiang, Xc., Li, Y. et al. Independent predictive value of blood inflammatory composite markers in ovarian cancer: recent clinical evidence and perspective focusing on NLR and PLR. J Ovarian Res 16, 36 (2023). https://doi.org/10.1186/s13048-023-01116-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13048-023-01116-2