Abstract
Uniparental disomy (UPD) is when all or part of the homologous chromosomes are inherited from only one of the two parents. Currently, UPD has been reported to occur for almost all chromosomes. In this study, we report two cases of UPD for chromosome 2 (UPD2) encountered during prenatal diagnosis. The ultrasound findings of the fetuses from two unrelated families showed intrauterine growth restriction. The karyotype analyses were normal. The two fetuses both had complete paternal chromosome 2 uniparental disomy detected by whole-exome sequencing, but their clinical outcomes were significantly different, with fetal arrest in case 1 and birth in case 2. In this report, we analyzed and discussed the phenotypes of the fetuses in these two cases and reviewed the literature on UPD2.
Similar content being viewed by others
Introduction
The concept of uniparental disomy (UPD) was first proposed by Engel [1] and refers to the phenomenon when all or part of an offspring’s homologous chromosome are derived from only the father or mother. UPD is a relatively rare chromosomal abnormality [2]. The pathogenic mechanism of UPD causing severe clinical phenotypes is mostly related to monogenic homozygous mutations or the disruption of imprinted gene expression [3, 4]. UPD on chromosomes 6, 7, 11, 14, 15, and 20 cause genomic imprinting disorders, resulting in disease [5]. For example, UPD15 leads to gene imprinting abnormalities in the 15q11q13 region, resulting in Prader-Willi/Angelman syndrome. Prader-Willi syndrome is a rare genetic disorder, characterized by clinical features including hypotonia and weakness, severe obesity, hypogonadism, and intellectual disability [6]. Patients with Angelman syndrome have clinical manifestations such as intellectual defects, microcephaly, ataxia, and seizures [7]. UPD of the X chromosome may lead to X-linked recessive disorders [8]. In UPD cases, the possibility of homozygous mutations in autosomal recessive genes is greatly increased. Diseases caused by this mechanism have been reported, such as LPS-responsive beige-like anchor deficiency, congenital ichthyosis, and Fanconi anemia [9–11]. The clinical phenotype of the fetus in the two cases reported here is closely associated with this mechanism.
With the development of genetic diagnostic techniques, more chromosomal abnormalities or genetic abnormalities have been detected during prenatal diagnosis, and most prenatal diagnostic techniques such as karyotyping, quantitative fluorescence PCR, copy number variant sequencing (CNV-Seq), and array comparative genomic hybridization cannot be used to screen for UPD [12, 13]. Using traditional genetic diagnosis methods, some cases of UPD may be overlooked [2]. Current genetic methods that can detect UPD with high accuracy include SNP arrays, short tandem repeat sequencing, and whole-exome sequencing (WES) [12, 13].
Here, we describe two pregnant women who had abnormal fetal development detected through ultrasound examination. Subsequent genetic diagnosis with WES found the presence of paternal uniparental disomy for chromosome 2. We analyze and discuss the inconsistent phenotypes of the fetuses in these two cases and review previous literature on UPD for chromosome 2 (UPD2).
Case presentation
Case 1
A 26-year-old pregnant woman presented to our hospital for prenatal diagnosis because the ultrasound results showed that the fetal limbs were abnormally short. She had given birth to a healthy baby boy two years before. She and her husband had no family history of congenital malformations, intellectual defects, or other genetic diseases. At 29 + 6 weeks gestation, the fetal ultrasound findings were as follows: biparietal diameter = 70 mm, − 2.55 SD; head circumference = 261 mm, − 1.99 SD; abdominal circumference = 247 mm, − 1.27 SD; femoral length = 46 mm, − 4.52 SD. Unfortunately, the fetal heartbeat stopped at 35 weeks + 1 day of gestation.
Case 2
A 33-year-old pregnant woman came to our hospital for pregnancy examination late in her pregnancy, which was her first. The prenatal ultrasound results done at other hospitals showed that the fetal growth was low, but the fetal cardiac ultrasound was not abnormal. Subsequently, the prenatal diagnosis results suggested that the fetal chromosome karyotype was normal, and the SNP array results revealed chromosome 2 UPD with unknown parentage. The pregnant woman came to our department to clarify the genetic abnormality of fetus. At 34 weeks of gestation, the fetal ultrasound results showed the following: biparietal diameter = 80 mm, − 2.27 SD; head circumference = 288 mm, − 2.15 SD; abdominal circumference = 282 mm, − 1.49 SD; femoral length = 56 mm, − 3.56 SD. At 36 weeks + 6 days of pregnancy, the fetal membrane ruptured. Considering that the fetus had intrauterine growth restriction (IUGR) and might have difficulty in normal delivery, the female baby was delivered by cesarean section.
Materials and methods
Karyotype analysis
After informed consent was obtained, fetal cord blood was collected for chromosome karyotype analysis. First, conventional cell culture was performed according to the standard procedure. Then, the cells were treated with colchicine to obtain mitotic metaphase cells. Metaphase chromosome specimens were prepared after hypotonic and fixation and were stained with Giemsa for banding display. Thirty metaphase cells with a resolution of 500 bands were screened for karyotyping using the Zeiss automated chromosome analysis system.
Genomic analysis
Parental peripheral blood samples and fetal amniotic fluid were collected after informed consent was obtained. Genomic DNA was extracted and purified using the QIAamp DNA Midi Kit (QIAGEN, Crawley, UK) according to the manufacturer’s instructions. Library preparation was performed, followed by whole-exome sequencing on the Illumina HiSeq 2500 platform (Illumina, CA, USA). After sequencing data was obtained, the sequence alignment was performed with reference to the human genome build GRCh37. GATK (v.3.8) software was used for single nucleotide variant (SNV) and insertion deletion (indel) detection. ANNOVAR software was used to annotate the variants. The annotated data from WES were screened: first, it was compared with the 1000 Genomes Project and Genome Aggregation Database to eliminate relatively common genetic variation (minor allele frequency-MAF > 1%) in the population. Then, variants predicted by Variant Effect Predictor that have only mild, moderate, and modifying effects on the phenotype and are located at non-coding regions were removed. Multiple algorithms were then used to make predictions about the deleteriousness of the remaining variants. These included SIFT, PolyPhen, ClinPred, and Mutation Taster. The mutations predicted as “harmful” and “possibly harmful” were retrieved from HGMD and Clinvar to enrich for and classify rare and potentially pathogenic mutations.
CNV-seq mainly consists of three steps: (1) Genomic DNA extraction: Genomic DNA (15 ng) was extracted from amniotic fluid cells and fragmented. (2) Library construction, purification and quality control: the DNA ends of small fragments were complemented by adding adenine deoxyribonucleotides and then ligated with the universal primer by TA ligation for sequencing to form a DNA library. The libraries were then quality controlled using quantitative fluorescent PCR. The library needed a concentration greater than 10 pmol/L, a melting temperature of 78–81 °C, and normal melting peaks without dimerization or broad peaks to pass QC. (3) Sequencing: Sequencing was performed on the Nextseq CN500 (Illumina). Approximately 5 million single-end reads of 45-bp in length were obtained. Approximately 2.8–3.2 million accurately located 36-bp reads were aligned to the human reference genome for each sample using the Burrows–Wheeler alignment algorithm and were then allocated into 20-kb bins on each of the 24 chromosomes. Then, the log2 value of the average CNV along the length of each sequencing bin on each chromosome was calculated. A log2 value of 0 represents two copies (normal), A log2 value of 1.5 represents three copies (duplication), and a log2 value of 0.5 represents one copy (deletion). The average chromosomal copy number of triploids can range from 2.05 (5%) to 2.95 (95%), while the average chromosomal copy number of monoploids can range from 1.05 (5%) to 1.95 (95%). Finally, the pathogenicity of candidate variants was evaluated according to the guidelines of the American College of Medical Genetics and Genomics (ACMG).
Results
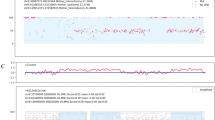
The ultrasound findings in the case 1 and 2 fetuses suggested significantly less fetal development than normal fetuses at the same age, with normal fetal karyotypes (46, XN) and no chromosomal number or structural abnormalities. CNV-seq did not show any copy number variants. The SNP genotyping results showed that there were runs of homozygosity region on chromosome 2 with a normal copy number of two (Fig. 1). Meanwhile, WES sequencing data analysis revealed that the fetal genotypes remained consistent with the father at the homozygous locus of chromosome 2 (Fig. 2). This suggested paternal UPD throughout chromosome 2. We analyzed and filtered the variants detected by WES on chromosome 2 with the following selection criteria: (a) novel or rare (MAF < 1%) variants, including missense, loss-of-function (such as frameshift, nonsense) and splice site variants with potential deleterious effects; (b) variants are heterozygous in the father and homozygous in the fetus; (c) variants follow an autosomal recessive inheritance pattern; (d) and are described in the OMIM database. In case 1, two rare missense variants were found on chromosome 2 in the fetus. Table 1 summarizes the homozygous loci on chromosome 2 that may be associated with the clinical phenotype of the case 1 fetus. Four rare homozygous nonsynonymous variants were identified on chromosome 2 in case 2 fetus. Table 2 summarizes the homozygous loci on chromosome 2 of the case 2 fetus. The harmfulness prediction results of these variants are also displayed.
A There were no heterozygous SNPs on chromosome 2 in the genotypes of fetus 1 and fetus 2. The x-axis shows the number of bases of chromosome 2 (in units of 1e8 bp). “Hom” represents homozygote and “Het” represents heterozygote. B The B-allele frequency within the red dashed box should have a distribution with a value of 0.5. However, there is an obvious absence of the 0.5 value, with only two values (0/1) present, indicating that there has been a run of homozygosity
Discussion
UPD is caused by chromosome segregation errors during meiosis and/or mitosis, which can occur independently or jointly [14, 15]. The four main formation mechanisms of UPD are often described as monosomic rescue, trisomic rescue, postfertilization division errors, and gamete complementation [5, 14]. UPD can sometimes cause homozygous mutations in recessive genes or imprinted gene expression disorders, leading to serious clinical consequences such as rib dysmorphism, mental retardation, or short stature [16–18]. So far, UPD has been reported on almost all chromosomes. Cases of UPD2 are less frequently reported [19]. Some of the UPD2 cases reported to date were found in children with developmental defects or mental abnormalities. Pathogenic mutations located on chromosome 2 were detected. UPD2 resulting in homozygosity of pathogenic mutations leads to certain diseases such as Catel-Manzke syndrome/VCRL syndrome, infantile hypotonia with psychomotor retardation and characteristic facies 2, and hepatocerebral mitochondrial DNA depletion syndrome [3, 20, 21]. Some UPD2 cases were discovered in normal individuals during paternity testing [2, 22, 23].
In this report, we conducted a study on two fetuses with abnormal intrauterine development. The limbs of fetus 1 and fetus 2 were significantly shorter than those of normal fetuses of the same age. Unfortunately, fetus 1 was stillborn, and fetus 2 was born prematurely. The results of karyotyping and CNV-seq showed no numerical or structural abnormalities of the chromosomes. The presence of chromosomal chimerism was also excluded. Paternal UPD2 in the fetuses by WES. We performed WES to look for potentially pathogenic mutations. Some variants that may be associated with IUGR were screened by WES, such as the TTN variants. TTN variants have been reported to be linked to multiple skeletal and cardiac myopathies [24]. Genetic analysis results revealed that the TTN missense variants in case 1 and case 2 were inherited from the father and were homozygous due to UPD of chromosome 2. However, TTN truncating variants are a common cause of dilated cardiomyopathy, however their penetrance for dilated cardiomyopathy in general populations is low [25, 26]. The TTN variants and other variants detected by WES were considered as variants of uncertain significance according to the guidelines of the ACMG. Considering that the fetuses’ parents were both healthy individuals and combined with the ACMG score, no potential pathogenic mutations were found. We consider that the variants detected by WES are unlikely to be involved in the intrauterine abnormal development phenotypes of the fetuses in both cases. Additionally, we speculate that there may be an imprinting region on chromosome 2 that may lead to developmental disorders or intellectual problems. UPD2 would cause this imprinting region to not be expressed, thus leading to abnormal embryonic development. The effects caused by this genetic imprinting region may potentially vary in penetrance across different populations.
This is the first report of UPD2 found in fetuses with IUGR that were eventually stillborn. After excluding genomic pathogenic mutations, we speculated whether there might be potential maternal imprinting regions on chromosome 2. Paternal UPD2 prevents the expression of the imprinting region and thus affects normal development of the embryo. There are currently no reports of genetic imprinting regions on chromosome 2 [2, 27]. It is possible that an imprinting region on chromosome 2 has not been discovered yet or has been overlooked due to the mild phenotype of the patients. We summarized the homozygous variants on chromosome 2 in fetuses 1 (Table 1) and fetus 2 (Table 2). Since we filtered out genes not included in OMIM, further studies may be conducted in the future to explore the functions of the filtered genes and determine whether they are related to the phenotypes observed in these two cases. Further validation experiments are needed to confirm whether there is an imprinting region on chromosome 2. Furthermore, our study shows that UPD might not be identified through traditional prenatal diagnosis. With the advantages of high resolution and throughput, WES technology can be used to monitor the presence of UPD in the case of microduplications, microdeletions, or single gene point mutations. The combination of WES with cytogenetics and CNV-seq has greatly improved prenatal diagnostics.
Availability of data and materials
The datasets for this article are not publicly available due to concerns regarding participant/patient anonymity. Data for this study can be requested from the corresponding author.
References
Engel E. A new genetic concept: uniparental disomy and its potential effect, isodisomy. Am J Med Genet. 1980;6(2):137–43. https://doi.org/10.1002/ajmg.1320060207.
Zhang X, Ding Z, He R, Qi J, Zhang Z, Cui B. Complete paternal uniparental disomy of chromosome 2 in an Asian female identified by short tandem repeats and whole genome sequencing. Cytogenet Genome Res. 2019;157(4):197–202. https://doi.org/10.1159/000499893.
Tao Y, Han D, Wei Y, Wang L, Song W, Li X. Case Report: Complete maternal uniparental disomy of chromosome 2 with a novel UNC80 splicing variant c.5609–4G> A in a Chinese patient with infantile hypotonia with psychomotor retardation and characteristic facies 2. Front Genet. 2021;12:747422. https://doi.org/10.3389/fgene.2021.747422.
Yamazawa K, Ogata T, Ferguson-Smith AC. Uniparental disomy and human disease: an overview. Am J Med Genet C Semin Med Genet. 2010;154C(3):329–34. https://doi.org/10.1002/ajmg.c.30270.
Benn P. Uniparental disomy: origin, frequency, and clinical significance. Prenat Diagn. 2021;41(5):564–72. https://doi.org/10.1002/pd.5837.
Kusz MJ, Gawlik AM. Adrenal insufficiency in patients with Prader-Willi syndrome. Front Endocrinol. 2022;13:1021704. https://doi.org/10.3389/fendo.2022.1021704.
Pearson E, Wilde L, Heald M, Royston R, Oliver C. Communication in Angelman syndrome: a scoping review. Dev Med Child Neurol. 2019;61(11):1266–74. https://doi.org/10.1111/dmcn.14257.
Kim JK, Jeong JE, Choi JM, Kim GH, Yoo HW. A female with typical fragile-X phenotype caused by maternal isodisomy of the entire X chromosome. J Hum Genet. 2020;65(6):551–5. https://doi.org/10.1038/s10038-020-0735-9.
Soler-Palacin P, Garcia-Prat M, Martin-Nalda A, Franco-Jarava C, Riviere JG, Plaja A, et al. LRBA deficiency in a patient with a novel homozygous mutation due to Chromosome 4 segmental uniparental isodisomy. Front Immunol. 2018;9:2397. https://doi.org/10.3389/fimmu.2018.02397.
Polubothu S, Glover M, Holder SE, Kinsler VA. Uniparental disomy as a mechanism for CERS3-mutated autosomal recessive congenital ichthyosis. Br J Dermatol. 2018;179(5):1214–5. https://doi.org/10.1111/bjd.16999.
Donovan FX, Kimble DC, Kim Y, Lach FP, Harper U, Kamat A, et al. Paternal or maternal uniparental disomy of chromosome 16 resulting in homozygosity of a mutant allele causes Fanconi anemia. Hum Mutat. 2016;37(5):465–8. https://doi.org/10.1002/humu.22962.
Vermeesch JR, Voet T, Devriendt K. Prenatal and pre-implantation genetic diagnosis. Nat Rev Genet. 2016;17(10):643–56. https://doi.org/10.1038/nrg.2016.97.
Hopkins MK, Dugoff L, Kuller JA. Exome sequencing and its emerging role in prenatal genetic diagnosis. Obstet Gynecol Surv. 2020;75(5):317–20. https://doi.org/10.1097/OGX.0000000000000787.
Eggermann T, Soellner L, Buiting K, Kotzot D. Mosaicism and uniparental disomy in prenatal diagnosis. Trends Mol Med. 2015;21(2):77–87. https://doi.org/10.1016/j.molmed.2014.11.010.
Nakka P, Pattillo Smith S, O’Donnell-Luria AH, McManus KF, Mountain JL, et al. Characterization of prevalence and health consequences of uniparental disomy in four million individuals from the general population. Am J Hum Genet. 2019;105(5):921–32. https://doi.org/10.1016/j.ajhg.2019.09.016.
Soellner L, Begemann M, Mackay DJ, Gronskov K, Tumer Z, Maher ER, et al. Recent advances in imprinting disorders. Clin Genet. 2017;91(1):3–13. https://doi.org/10.1111/cge.12827.
Kivrak Pfiffner F, Koller S, Ménétrey A, Graf U, Bähr L, Maspoli A, et al. Homozygosity for a novel DOCK7 variant due to segmental uniparental isodisomy of chromosome 1 associated with early infantile epileptic encephalopathy (EIEE) and cortical visual impairment. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms23137382.
Liu J, Chen B, Liu Y, Kong J, Zhang B, Han L, et al. Paternal uniparental disomy of chromosome 16 resulting in homozygosity of a GPT2 mutation causes intellectual and developmental disability. Eur J Med Genet. 2022;65(9):104554. https://doi.org/10.1016/j.ejmg.2022.104554.
Keller MC, McRae AF, McGaughran JM, Visscher PM, Martin NG, Montgomery GW. Non-pathological paternal isodisomy of chromosome 2 detected from a genome-wide SNP scan. Am J Med Genet A. 2009;149A(8):1823–6. https://doi.org/10.1002/ajmg.a.32973.
Borchers A, Pieler T. A homozygous deletion of exon 5 of KYNU resulting from a maternal chromosome 2 isodisomy (UPD2) causes Catel-Manzke-Syndrome/VCRL syndrome. Genes. 2010;1(3):413–26. https://doi.org/10.3390/genes12060879.
Haudry C, de Lonlay P, Malan V, Bole-Feysot C, Assouline Z, Pruvost S, et al. Maternal uniparental disomy of chromosome 2 in a patient with a DGUOK mutation associated with hepatocerebral mitochondrial DNA depletion syndrome. Mol Genet Metab. 2012;107(4):700–4. https://doi.org/10.1016/j.ymgme.2012.10.008.
Ou X, Liu C, Chen S, Yu J, Zhang Y, Liu S, et al. Complete paternal uniparental isodisomy for chromosome 2 revealed in a parentage testing case. Transfusion. 2013;53(6):1266–9. https://doi.org/10.1111/j.1537-2995.2012.03863.x.
Chen M, Jiang J, Li C, Ren H, Chen W, Liu Z, et al. Non-pathological complete paternal uniparental isodisomy of chromosome 2 revealed in a maternity testing case. Int J Legal Med. 2019;133(4):993–7. https://doi.org/10.1007/s00414-018-1857-x.
Kellermayer D, Smith JE 3rd, Granzier H. Titin mutations and muscle disease. Pflugers Arch. 2019;471(5):673–82. https://doi.org/10.1007/s00424-019-02272-5.
Schiabor Barrett KM, Cirulli ET, Bolze A, Rowan C, Elhanan G, Grzymski JJ, et al. Cardiomyopathy prevalence exceeds 30% in individuals with TTN variants and early atrial fibrillation. Genet Med. 2023;25(4):100012. https://doi.org/10.1016/j.gim.2023.100012.
Hastings R, de Villiers CP, Hooper C, Ormondroyd L, Pagnamenta A, Lise S, et al. Combination of whole genome sequencing, linkage, and functional studies implicates a missense mutation in titin as a cause of autosomal dominant cardiomyopathy with features of left ventricular noncompaction. Circ Cardiovasc Genet. 2016;9(5):426–35. https://doi.org/10.1161/CIRCGENETICS.116.001431.
Zhou S, Wang H, Wang QK, Wang P, Wang F, Xu C. Loss of heterozygosity detected at three short tandem repeat locus commonly used for human DNA identification in a case of paternity testing. Leg Med. 2017;24:7–11. https://doi.org/10.1016/j.legalmed.2016.11.001.
Acknowledgements
The authors are grateful to the two families who participated in this study.
Funding
This work was supported by the National Natural Science Foundation of China (82060284), and the Guangxi Natural Science Foundation (2020GXNSFBA297155), the Health Department Research Fund of Guangxi Zhuang Autonomous Region, Guangxi, People’s Republic of China (Z20190789), and the Guangxi Science and Technology Plan Project (Guangxi Clinical Research Center for Obstetrics and Gynecology, GuiKe AD22035223).
Author information
Authors and Affiliations
Contributions
DY, TY and DZ conceived the study. XT and BL wrote the paper. BL and YQ were involved in the counselling for case 1 and case 2. XW carried out the laboratory work. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tan, X., Liu, B., Yan, T. et al. Prenatal diagnosis of paternal uniparental disomy for chromosome 2 in two fetuses with intrauterine growth restriction. Mol Cytogenet 16, 20 (2023). https://doi.org/10.1186/s13039-023-00647-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13039-023-00647-z