Abstract
Background
The Improving Mental Health Literacy Among Children and Young People in Indonesia (IMPeTUs) intervention is a co-produced, evidence-based digital intervention designed to improve anxiety and depression focused mental health literacy and self-management among people aged 11–15 in Java, Indonesia. This study aimed to evaluate the usability, feasibility and preliminary impact of our intervention.
Methods
Mixed methods, multi-site case studies based on a theory of change. Pre-and post-assessments of a range of outcomes and qualitative interviews/focus groups with children and young people (CYP), parents and facilitators. The intervention was implemented in 8 health, school and community sites across Java, Indonesia (Megelang, Jakarta and Bogor).
Quantitative data designed to understand the impact of and feasibility of evaluating the intervention collected from 78 CYP who used the intervention were analysed descriptively. Qualitative data from interviews and focus groups collected from 56 CYP, 49 parents/caregivers and 18 facilitators were analysed using framework analysis.
Results
Qualitative data analysis indicated high levels of usability and acceptability for the interface aesthetic, personalisation, message presentation and navigation. Participants reported minimal burden and no negative outcomes associated with the intervention. CYP, parents and facilitators identified a range of direct and spill over effects of interventions engagement, some of which were not anticipated at study outset. Quantitative data highlighted the feasibility of intervention evaluation, with high levels of recruitment and retention across study time points. Minimal changes were identified in outcomes pre-to-post intervention, which may in part be due to a lack of scale relevance and/or sensitivity to the intervention mechanisms indicated in the qualitative data.
Conclusions
Digital mental health literacy applications are potentially an acceptable and feasible way to prevent burdens of common mental health problems amongst CYP in Indonesia. Our intervention and evaluative processes will be further refined prior to definitive evaluation.
Similar content being viewed by others
Introduction
Mental health difficulties are significant contributors to the global burden of disease and affect between 10–20% of children and young people (CYP) across the world [1]. 50% of mental health problems are established by the age of 14 [2]. Depression, in particular, is considered a leading cause of mental health disability, estimated to affect between 4 and 8% of adolescents globally each year [3]. A recent meta-analysis estimated global prevalence of anxiety amongst CYP to be 20.5% which is considered to have doubled since the Covid-19 pandemic [4].
Evidence has demonstrated an individual’s risk of experiencing commnon mental health problems increases significantly after puberty and that approximately two-thirds of CYP with depression will have a recurrent episode within five years [5, 6]. The long-term negative effects of childhood mental health difficulties are well documented. Experiencing mental health difficulties in childhood is linked to co-morbid physical health problems, more serious and persistent mental health episodes later in life and an increased risk of suicide [7, 8].
Indonesia, an archipelago in Southeast Asia, meets World Bank criteria for a lower-middle income country (LMIC). Recent evidence suggests that nearly 50% of high school students living in Indonesia experience depressive symptoms and suicidal ideation has a 12-month prevalence of 6.8% [9]. The United Nations Sustainable Development plan sets down targets for reducing mortality by 33% by 2020, to be driven by the prevention and treatment of non-communicable diseases and the promotion of mental health and wellbeing [10, 11]. Like most LMICs, treatment gaps in Indonesia are significant and often exceed 75%, highlighting an urgent need to scale up effective and acceptable support. Mental health is a national priority in Indonesia; however, recent decentralisation of mental health care means community provision is still in the early stages of development and significant challenges remain [12].
Long standing treatment demands have been exacerbated by recent global events. For example, Covid-19 has significantly impacted on the mental health of CYP. There has been a myriad of government/policy, third sector and academic reports published signalling the concern for mental health and wellbeing among adults and CYP [13]. While the focus on transforming services to meet the needs of CYP with poor mental health is a global policy imperative [14], the pandemic has highlighted and exacerbated the gap between the needs of CYP and the solutions on offer. The current pandemic presents an opportunity to develop preventative solutions which are cost-effective in the short- and longer term. Such solutions have the potential to support CYP today to become healthier future generations of adults [15, 16].
Mental health literacy (MHL), the ‘knowledge and belief about mental disorders which aid their recognition, management or prevention’ is a promising development in global mental health research [17]. The MHL framework originally developed by Jorm and colleagues comprises of a range of skills clustered within four components:
-
the ability to identify mental health difficulties
-
recognising the causes of mental health difficulties
-
understanding of effective help-seeking
-
perceptions of the factors that impact on help-seeking [17].
This original conceptualisation has since been expanded to include perceptions of positive mental health and wellbeing, self-efficacy and stigma [18,19,20].
Mental health literacy skills have consistently been shown to be associated with improved health outcomes and social determinants of health. The available evidence suggests improved recognition and knowledge about mental illness and appropriate support can improve help-seeking in CYP [21]. This is important given that studies show as little as one third of adolescents seek appropriate treatment for mental health problems. Timely and appropriate help seeking in early adolescence is critical for recovery, and for reducing the likelihood of mental disorder in later adolescence and life [22]. Poorer mental health literacy has been associated with increasing mental illness among CYP [23].
This paper reports on the feasibility evaluation of the IMPeTuS intervention which was co-designed to improve mental health literacy amongst CYP aged 11–15 in Java, Indonesia [24].
The IMPEtUS intervention
Stepped care prevention and treatment approaches, where psychological interventions are delivered according to need, are considered an optimal solution to reduce the burden on health systems [25]. Our solution is a mental health intervention designed to improve self-management of mental health and timely intervention through improved mental health literacy, recognition and effective help-seeking [26].
The IMPeTUs intervention was co-designed with CYP, parents, professionals and games designers in Java, Indonesia [26]. Systematic reviews were undertaken in preparation for this co-production which demonstrated a dearth of culturally sensitive MHL interventions which were appropriate for use in Indonesia, which required the co-design of a novel intervention [26,27,28]. Intervention development adhered to the recommendations outlined in the Medical Research Council’s guidelines for the development of complex interventions [29] and links to the WHO strategy for improving resources in schools to support CYP mental health [11].
Drawing on principles of Experience Based Co-design [30], our intervention co-production comprised three phases. The first phase involved an initial needs assessment in the form of systematic reviews [26,27,28] and in-depth qualitative data obtained from CYP, parents, and health and education professionals [31, 32]. These data informed phase 2 which centred on a stakeholder consensus exercise and 3-day co-production workshop with 50 attendees (CYP, parents, health and education professionals, researchers and games designers). This decided a design brief for the format and provisional content of the intervention along with implementation strategies. In the third and final phase the games designers worked closely with our patient and public involvement group in ongoing group work to ensure the intervention was developed and refined in line with the original co-produced brief [26].
The IMPeTUs intervention includes a digital application and facilitated group discussion sessions for CYP before and after engagement with the intervention. Group discussions were considered necessary to enable CYP to be suitably oriented to the intervention and to provide a space in which CYP could discuss issues raised with the game and discuss any issues which arose during game play. The digital application takes the form of an immersive storyline design in which CYP take on the role of a central, customisable character and navigate the character through a series of mental health related challenges. There is one chapter of the game which focuses on depression and one chapter that focuses on anxiety. The immersive storyline design is broken up with interactive games and exercises to promote engagement with the applications. Screen art from the digital application can be found in Fig. 1 and a preliminary theory of change developed by the authors can be found in Fig. 2.
Example artwork from the IMPeTUs intervention (originally published in [24]
Preliminary theory of change originally published in [26]
Aims
In line with the WHO guidelines for the evaluation of prototype mHealth interventions, our case studies aimed to understand the usability, feasibility and preliminary imact of our prototype intervention [33]. In the WHO guidelines, efficacy relates to the extent to which an intervention is thought to bring about intended outcomes in a research setting:
-
To qualitatively examine the usability, feasibility and impact of our co-produced intervention.
-
To quantitatively explore the preliminary impact of our co-produced intervention on a range of user-focussed outcome measures.
-
To explore the feasibility of evaluating our co-produced intervention.
Methods
Study design
The study was designed to evaluate a prototype digital mental health literacy and depression and anxiety focussed self-management intervention. Our evaluation was informed by the User Focussed Evaluation approach developed by Patton (1997) [34]. This approach is based on a fundamental principle that an evaluation should be assessed on its perceived utility to its intended beneficiaries. Our previous endeavours to include relevant stakeholders in the design of the intervention are described previously [26]. We also worked closely with patient and public involvement groups comprised of CYP and adults with lived experience of mental health difficulties in Indonesia to design the initial theory of change and to design evaluation processes.
In order to address the study aims, a collective mixed-methods case study design was employed which incorporated multiple cases undertaken concurrently [35]. With equal weight given to both types of study design [36], quantitative and qualitative data were used to answer different elements of the study aims. Therefore, it was not necessary to integrate the two types of study data; however, synergies between the findings are considered in the discussion [37].
Setting
Our case study evaluations were undertaken in three geographical areas of Java, Indonesia. These were Jakarta, Magelang and Bogor. Sites were selected on their differences in culture, urbanisation and level of health service provision. These sites also had specific child and adolescent mental health service provision which was considered useful in terms of supporting the research and evaluating the prototype intervention [24]. We aimed to recruit one school, one community organisation and one health service setting in each geographical site resulting in a total of 9 case study evaluations. However, the evaluative period coincided with the global Covid-19 pandemic and the health service site in Jakarta did not have capacity to undertake the case study evaluation due to ongoing pressures relating to coronavirus. This resulted in 8 case study evaluations being completed.
Participants
Children and young people
CYP were eligible to take part if they were aged 11–15 and in contact with one of the recruitment sites across our 8 case study evaluation locations. Participants were required to provide assent and parental consent prior to participation in study activities. A total of 78 CYP were recruited to the quantitative element, 56 also took part in an interview or focus group. Further demographic information can be found in Table 1.
Parents/caregivers
Caregivers were eligible to take part in the study if they had a CYP they provided care for aged 11–15 who had agreed to take part in the prototype evaluation. Caregivers were required to give written and informed consent to take part in study activities. A total of 78 parents/caregivers provided consent for they CYP to take part in the study and 49 provided informed consent and took part in an interview or focus group. Further demographic details are provided in Table 1.
Facilitators/professionals
All facilitators who were involved in implementing the IMPeTUs intervention were invited to participate in the case study evaluations. Other professionals were eligible to participate in the case study evaluations if they were working at the sites that CYP taking part in the case study evaluations attended and had some experience of the intervention. A total of 18 facilitators/professionals were recruited to the study. Facilitators were professionals working within study sites.
Procedures
CYP were recruited to the study through direct invitation from the organisations they attended (school, health service or community venue) in each case study site. Staff within participating organisations identified CYP aged 11–15 who were eligible to take part in the evaluation. Study information packs containing an invitation letter, information sheets for both CYP and parents, a consent form and contact details form with return envelope were distributed to all eligible CYP. These were distributed to eligible participants on behalf of the research team by post, email or in person during routine contacts. CYP received a age-appropriate version of the information sheet. Parents/caregivers completed and returned consent forms and completed contact details if their child was happy to take part and had given their verbal assent.
Parents/caregivers of those children who agreed to take part in the study also received a separate invitation letter, participant information sheet, consent form and contact details form in order to invite them to take part in an individual interview or focus group to discuss their child’s experience of using the prototype intervention.
Invitation packs containing an invitation letter, participant information sheet, consent to contact form and consent form were sent by post or email directly from the research team to eligible facilitators/professionals.
Those interested in taking part returned the consent form/consent to contact form and contact details form to the research team who contacted them to discuss the study further, answer any questions and to facilitate access to an upcoming focus group or arrange a one-to-one interview, depending on individual preference. All participants (CYP, parents and professionals) were offered a small cash payment in recognition of their time taking part.
Quantitative data
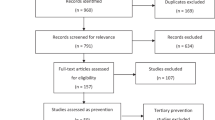
As shown in Fig. 3, CYP were invited to complete a set of questionnaires at three timepoints: prior to using the game (baseline), on a second occasion after playing the game for one month (post-intervention) and a final time six months after baseline. The measures included in the pack are detailed in Table 2 and included a range of self-complete questionnaires developed for CYP which were relevant to the initial ToC and chosen by the lived experience panel.
Qualitative data
After playing the game over approximately a one-month period, CYP took part in a one-time qualitative interview or focus group depending on participant preference lasting up to one-hour, guided by a topic guide exploring 56 CYP experiences and perceptions of the intervention. 49 parents of children who had tried the intervention and 18 professionals involved in the evaluation took part in a one-time interview or focus group lasting 60–90 min. Interviews/focus groups explored parental views about the intervention and perceptions of their child’s experiences whereas professional interviews explored their perceptions of the intervention based on their experience of delivering the intervention. 21/56 CYP, 2/49 parents and 18/18 facilitators took part in in-person interviews and focus groups and the rest were undertaken via zoom. Interviews/focus groups were digitally audio-recorded, transcribed verbatim and translated into English for the purposes of analysis.
Data analysis
Quantitative data
Scores on each of the questionnaires at each of the three time-points are summarised in Tables 4 and 5. As all of the questionnaires give a score on a continuous scale, the mean, standard deviation and range of each was calculated. To determine whether the game showed signs of preliminary efficacy (e.g., improving quality-of-life, etc.), ‘change’ scores between baseline and one-month post-intervention and baseline and six-months post-intervention were calculated and summarised as above.
Parents reported the CYP played with the intervention on average 5 times, ranging from 1–15 times.
Qualitative data
Qualitative data were analysed using a framework approach incorporating deductive and inductive coding. Deductive coding was informed by Theoretical Framework of Acceptability (TFA) [38] and inductive coding was utilised to ensure data was captured that fell outwith this framework (Table 3).
The process of analysis followed the stages outlined by Gale et al. [39]. After transcription and anonymisation, transcripts were allocated to one of 8 coders. Each analyst familiarised themselves with the data through active reading. Next, researchers moved to charting the data in an a priori matrix which was developed using the TFA. This involved writing written summaries of the data pertaining to each TFA component in each transcript. Supporting quotes were inputted into the relevant matrix cells to support the write-up process. There were areas of the Excel sheet where additional data that fell outside the TFA framework could also be captured. Researchers were asked to keep analytical memos and document any emerging thoughts/feelings about the data as this process was undertaken.
Once all the transcripts had been analysed, two authors (HBrooks/PBee) met to verify the allocation of data to the various TFA components and to identify key issues relating to acceptability of the IMPeTUS intervention within each component. This was done collaboratively with consensus reached for each TFA component before sharing with the wider team for further verification. Each component was then written up with sufficient detail provided for each section and direct quotations provided to support interpretations.
Results
Quantitative results
78 CYP provided consent to take part in the study and completed baseline data collection. 76 provided demographic data. 71/78 (91%) completed assessments at one month post intervention and 70/78 (90%) at six-months post intervention. Those who dropped out were either non-contactable or declined to take part in further data collection. Where assessments were completed, they were done so in full. Thus, no data imputation for partial non-response was required. Change scores were only calculated where there was baseline and follow-up data for participants.
Table 1 shows that the average age of the 76 participants who provided data was nearly 13 years. Thirty-nine (51.3%) were male. The male participants were marginally older, primarily due to a relatively larger percentage of 14 year-olds.
Exactly one-quarter (n = 19) reported experiencing at least one mental health problem. The most commonly reported problem was anxiety (n = 13), with depression and other mental health problems being relatively less common (both reported by five participants). The median duration of the reported problems was 12 months (range = 6 to 36 months). Nearly all of those reporting a mental health problem had sought help from their family (n = 17) and/ or a health professional (n = 15). Other sources of help seeking were much less common.
Table 4 shows that the mean changes from baseline on all outcome measures were small at both one month and six months post-intervention. Table 5 outlines the average changes from baseline on all outcome measures for the 19 participants currently experiencing mental health problems vs those who were not currently experiencing mental health problems.
Qualitative results
Participants across all stakeholder groups demonstrated a shared interest in the game prior to engagement with the intervention. Excitement was a dominant emotion in CYP narratives which focussed on experiential and interactive elements. CYP described expectations relating to wanting an interesting and challenging intervention. This excitement appeared driven by a desire to improve mental health. Supporting quotes are provided in Additional file 1 with summary description of TFA components provided below.
Parents’ perceptions mirrored those of CYP but they were more likely to focus on education and mental health outcomes rather than experiential aspects. Facilitators also expressed a desire for a solution focused intervention which was challenging for CYP and had the potential to improve CYP abilities to communicate with parents. One CYP participant and one facilitator expressed concerns about the potential for digital games to become addictive.
Affective attitude
Affective attitude relates to participants’ feelings about taking part in an intervention. The general consensus amongst CYP was that the game was fun, exciting and enjoyable and not overly complicated. These feelings were endorsed by parents and facilitators who described CYP as curious and eager to engage with the intervention and felt the game was well aligned to the needs of CYP. For most participants, their experiences with the intervention either met or exceeded their expectations. Parents described how they also enjoyed the game and had played together with their children on occasion. Facilitators further highlighted the uniqueness of the digital application in the Indonesian context and valued the focus on self-management and independence given parents/professional were often hesitant to talk about mental illness due to the prevailing stigma in Indonesia.
There were shared concerns raised by all three stakeholder groups about the game becoming boring after long periods or repeated engagement with the digital element of intervention. When played multiple (in excess of five) times, the game was considered to become less challenging which decreased CYP enthusiasm for the game over time. Parents highlighted rival games (non-health) that were more challenging and competed for CYP attention. Facilitators acknowledged this but appeared to better understand the intended use in the short-term and as a health intervention.
Such concerns; however, did not appear to impact on the perceived usefulness of the intervention. The positive feelings associated with the game appeared to relate to the storyline design, interactive elements, CYP’s ability to identify with the characters, the storylines reflecting real life experiences and the utility of the practical strategies which could be incorporated into their everyday life.
Suggested improvements to improve affective attitude included having more customisation, additional levels within the game, less text and more interactive elements. See Additional file 2 for more detail on suggested improvements to the prototype intervention.
Burden
The burden component within the TFA relates to the amount of effort that is required to be invested by participants in order to engage with the intervention. Most participants across stakeholder groups did not report any burden and those were identified within this component were relatively minor.
Stakeholders across groups described initial problems downloading the game in terms of the length of time required, technical issues relating to gameplay or challenges with compatibility with their personal devices. Others described the effort to motivate themselves (CYP) or others (facilitators/parents) to play the game which was exacerbated after prolonged engagement with the intervention and when facilitation was undertaken remotely. This perceived burden appeared related to the amount of text that needed to be read within the app and the length of time required to complete chapters.
Perceived effectiveness
Perceived effectiveness relates to participants’ perspectives about whether an intervention can achieve its intended purposes or not. Participants across all stakeholder groups described elements of the potential and actual utility of the intervention and valued the combination of group sessions and one-to-one engagement with the digital game. No participants reported any negative outcomes. Participants described the timeliness of the intervention and most reported some form of direct benefit as a result of taking part. Some felt that with further improvements to the intervention benefits could be further maximised (see Additional file 2). Figure 2 outlines the hypothesised impacts and mechanisms of change developed prior to undertaking the case study evaluation.
Whilst initially finding it difficult to articulate benefits, CYP described some positive impacts of the intervention on current mental health literacy and self-management. They also described an increased readiness to engage in self-management in the future if problems arose. These impacts appeared to be related to both increased knowledge about mental health and self-management strategies but also increased self-efficacy in terms of undertaking these activities. These included being able to control their emotions better, increased understanding about their own and others’ mental health, reduced stigma around mental health and feeling more confident to tackle problems directly. Other benefits identified by CYP included greater social confidence and improved general and mental health specific communication within families and friendship groups. Parents and facilitators supported these attributed benefits and identified additional ones which included improved mood, thinking more positively about things, increased independence, improved behaviour, enhanced problem solving abilities, less stress, being more respectful of and polite to others and being more attentive to siblings. Some felt this had been particularly useful during the pandemic because ongoing lock-downs had led to CYP becoming more introverted but others felt that the pandemic had limited opportunities to demonstrate their learning.
Benefits were also identified for facilitators, parents and families. These included better understanding of mental health and how to manage it within their families or within professional roles, improved self-management, increasing their awareness that CYP want to and can help themselves, reflecting on their parenting/professional role in relation to mental health and improved relationships with CYP. Parents and facilitators described examples of using the character and their experiences to talk to CYP about mental health and how CYP often mirrored the behaviour of characters within the intervention. A small number of parents and facilitators also described how CYP were able to challenge parents' behaviour towards their own mental health after the intervention using the characters within the digital application.
Facilitators thought the intervention might work best for those currently experiencing mental health problems and that the solution focussed nature of the game was useful as it provided insight that could be applied in daily life which increased the relevance and potential effectiveness of the intervention. Parents; however, raised the issue of long-term effectiveness when engagement with the intervention stopped. One parent retained their concern about the potential for CYP to become addicted to this type of intervention.
Ethicality
Ethicality relates to the extent to which the values underpinning an intervention align with the participants’ own value systems. Encouragingly, the IMPeTUs intervention appeared well aligned to the values of all three stakeholder groups. Facilitators also described how the intervention responded well to recent societal shifts in Indonesia which has meant that there is greater recognition of the importance of the need to promote positive mental health and wellbeing. There were no negative aspects or outcomes identified.
Participants across groups described how children in Indonesia are familiar with engaging with digital games generally and that this was their preferred way to learn about mental health. This was perceived to increase the accessibility of the intervention in Indonesian contexts. The IMPeTUs game was compared favourably by parents and facilitators to other non-health games that CYP played because it had a more useful purpose. One parent suggested the digital game should include more religious content.
Intervention coherence
Intervention coherence relates to the face validity of the intervention to relevant stakeholders. Generally speaking, there was good intervention coherence reported across all three stakeholder groups. CYP, parents and facilitators described the intervention to be straightforward and clear and the study documentation/processes prepared participants well for facilitating or using the intervention. This coherence appeared to be enhanced by the perception that the intervention met an unmet need for CYP in Indonesia and it was suitably different from existing interventions with similar aims.
There was acknowledgement amongst facilitators that there needed to be sufficient time built into the implementation process in order to achieve intervention coherence amongst parents and CYP. This was considered more difficult to achieve when facilitation was undertaken remotely due to Covid-19 related restrictions. Introducing the game and clarifying understanding amongst study participants was considered easier to achieve if undertaken face-to-face.
Some facilitators felt that coherence was more readily achieved amongst CYP and required more sustained effort to achieve in parents. This appeared to be due to parental concerns about CYP engagement with digital games generally, a lack of understanding about how a game could improve mental health amongst parents and concerns about digital literacy amongst some adults when compared to children.
Facilitators reported this could be mitigated against through having regular meetings/contact with parents and all participants having the opportunity to ask questions and raise concerns. This worked best where facilitators took responsibility for driving these activities.
One CYP reported finding the storyline and sentences confusing and a small number of parents endorsed this whilst highlighting that understanding was more of an issue for younger participants. This was a view that was also acknowledged by some facilitators.
Opportunity costs
Opportunity costs relate to the benefits, profits or values that need to be relinquished in order to engage with an intervention. Participants across all three stakeholder groups coalesced in their views that there were no identifiable opportunity costs related to engagement with the IMPeTUS interventions. One parent reported that the cost-free access to the current intervention was a comparative strength compared to other pay to play digital applications.
Self-efficacy
Self-efficacy is defined at the participants' confidence that they can perform the behaviours required to engage in the intervention. Self-efficacy was not reported as a major component of intervention acceptability in the parent data, most likely reflecting their more peripheral role as a support rather than direct participant in the intervention.
Facilitators received training to deliver the IMPeTUS intervention and considered this training fit for purpose. They felt that the intervention aligned well with their existing roles, and that their previous experience and existing skills had prepared them well. A minority of facilitators suggested increasing the level of training to ease any necessary transition from face to face to remote facilitation. Some also acknowledged that competing occupational responsibilities and time pressures had impacted their ability to fully familiarise themselves with the app, and advised that sufficient opportunity should be available to enable facilitators to engage with the intervention themselves before introducing it to CYP.
Despite facilitators requiring time to orientate themselves to the game, and explain it to parents, they believed that the digital IMPeTUS intervention was intuitive for CYP and required little preparation. This view was upheld by the CYP themselves; some of whom explicitly acknowledged that they were able to engage in the impetus intervention during periods of low mood, when participation in other gaming applications was more difficult.
Distinguishing between the IMPeTUS app and the group facilitation components of the intervention, some CYP reported that, due to a lack of confidence, they initially found the group discussions challenging. However, there was no evidence that these feelings impacted on CYP’s participation and group discussion was still considered a beneficial part of the intervention. Group discussion was reported to increase CYP’s ability to initiate and engage with the game, as well as increasing their mental health knowledge and understanding.
Discussion
In line with WHO guidelines for evaluating prototype mHealth interventions, our mixed methods case study evaluation aimed to examine the usability, feasibility and preliminary impact of our co-produced intervention [33]. We recruited 56 CYP, 49 parents and 18 facilitators to understand user perspectives on these criteria and underpinned our study with a co-produced theory of change to ensure a theory-driven evaluation.
The data analysis revealed that usability was strongly impacted by the perceived function of the intervention and whether its primary function was considered to be an interactive game or a mental health intervention. Our qualitative analysis indicates that our intervention fits best in the mental health intervention landscape. In this context, our intervention has an explicit purpose (mental health education and self-management), and thus a potentially targeted and time-bounded duration of use, partially offsetting user concerns about longer term use and gaming sustainability more critical to a digital entertainment context. While gaming innovations may help to maximise the uptake and interactivity of digital health resources, further consideration may need to be given to the development and evaluation of products capable of performing well in both markets.
Through consultation with our PPI advisory group and study team, we envisaged that participants would need to engage for a minimum of one hour in each storyline chapter of our intervention to confer benefit in line with our co-produced theory of change. However, some participants reported using the intervention primarily as a recreational game and played it multiple times over sustained periods of time. This unintended usage could lead to participants reporting repetition and/or boredom and highlights a need for clear explanation of the aims of the intervention and expected engagement.
Engagement in digital health interventions is likely to be a function of both the intervention and user characteristics. Participants across stakeholder groups felt that there was potential for further intervention development, through the addition of extra chapters and improvements to existing content, to increase future sustainability (See Additional file 2). Examples for additional chapters included self-harm and suicidal ideation, bullying, and substance abuse. There were also some indications that in its existing form, our intervention might work best for: older children, those with less gaming experience, those currently experiencing mental health problems and those with very limited existing mental health literacy.
Our data identified good levels of acceptability with our intervention across stakeholder groups. Using a checklist of design features which are known to enhance user experience, our intervention performed well terms of interface aesthetic, personalisation, navigation, reinforcement and message presentation [40]. There were no concerns reported about credibility which was considered to be as a result of the implementation route (via a trusted organisation) but participants described a preference for enhanced communication within the game (e.g. with others using the app) in future iterations [40]. Encouragingly, there were minimal burdens identified and no negative outcomes reported. This is likely to be a consequence of our iterative co-productive design approach which drew on principles of experience-based co-design with no a priori restrictions in terms of intervention content or delivery [30]. Our substantial needs assessment in the form of two systematic reviews [27, 28] and qualitative research with CYP, parents and health and education professionals [31, 32] was used to inform initial co-design workshops with the games designers and CYP, parents and professionals who together agreed upon a brief for our prototype intervention [26]. Games designers and researchers then worked closely with patient and public involvement contributors to implement the brief with two opportunities for initial user testing and iteration. This appears to have contributed to the perceived timeliness and relevance of the intervention and the close alignment of the intervention with CYP needs, values and real word experiences [41]. It also likely reflects a wider social shift in Indonesia from preferences for traditional practitioners to evidence-based interventions and alternative forms of service provision [42]. Our analysis demonstrates stakeholder preferences for mHealth interventions which focus on empowerment and recovery (i.e. solution-focussed) interventions rather than paternalistic problem-focussed support and resources. This highlights the opportunity for harnessing the drive for global movements that prioritise self-management and strengths-based initiatives, for the development of mental health interventions in Indonesia [43].
Our qualitative data identified some initial concerns about the addictiveness of computer games and digital applications more generally which have been identified in Indonesian contexts previously [26]. These concerns appeared to be allayed for the most part by direct experience with our intervention; we identified some important attitudinal shifts which appeared to be driven by engagement with the intervention and the range of benefits identified.
Our preliminary theory of change which was co-produced with relevant stakeholders during the initial co-design process identified a range of theorised benefits [26]. However, our qualitative data identified a more nuanced range of benefits that were not adequately captured in our original theory of change or quantitative outcome measures. These included improved conceptualisations of mental health and readiness to disclose difficulties, increased confidence to communicate with others and increased likelihood of engaging in positive mental health self-management. Our quantitative outcome measures focussed on current mental health symptoms/difficulties which may not have been sufficiently relevant to our participants (of whom only 19/78 were currently experiencing mental health difficulties) or sensitive to capture these more nuanced benefits.
Our quantitative data tentatively supported the qualitative data by indicating an increased utility of intervention for those currently experiencing mental health problems. These CYP (n = 19) had lower quality of life scores, lower family adaptability and cohesion and higher anxiety and depression scores at all three assessment points compared to children who did not report experiencing a mental health problem. There was some evidence that these children exhibited a greater change from baseline, particularly in quality of life and family adaptability and cohesion (both of which improved). However, only 19 CYP reported experiencing a mental health problem, so these findings must be viewed cautiously until data from a much larger sample is obtained.
The qualitative data also identified a range of spill over impacts which were unanticipated at study outset. For example, parents and facilitators reported benefiting directly from their experience with the intervention but also acknowledged wider family benefits, not incorporated in our initial theory of change. These benefits included CYP helping parents with their own mental health, enhanced understanding of and empathy towards the challenges CYP currently face and increased mental health literacy amongst parents, families and facilitators. There has been a step change towards increasing the availability of lower intensity, scalable interventions for depression and anxiety globally [44]. However, in the current study facilitators described limited awareness of the use of mhealth interventions to support self-management for mild-moderate mental health difficulties prior to using the intervention.
WHO guidelines for evaluating interventions in the later stages of the intervention maturity life-cycle recommend evaluation in terms of effectiveness, cost-effectiveness and implementation [33]. While our findings are limited in their capacity to directly evidence population health change, they have important implications for future evaluation. Revising the intervention’s theory of change and ensuring the selection of meaningful quantitative measures and the recruitment and inclusion of potential beneficiaries are important activities in future evaluation processes. Public involvement in the design of future evaluations will further support the choice of relevant and appropriate outcome measures and evaluation processes. Future implementation will also require effective collaboration with relevant ministries and institutions in Indonesia such as the Ministry of Health, the Ministry of National Education and the Ministry of Communication and Informatics. See Fig. 4 for a revised theory of change.
Initial findings from our prototype evaluation highlight the value of the use of our digital intervention in conjunction with the pre-and post group sessions despite these sessions being initially viewed as challenging by CYP in both on and offline settings. These appeared particularly important in the implementation of the intervention in Indonesian contexts given the concerns parents raised about not feeling comfortable discussing mental health with their children and because they offset the increased curiousness as reported by CYP [31]. There were no differences in study data between different implementation sites (schools, health services and community venues or geographical locations) suggesting our intervention is setting agnostic and can be used on or offline. However, the data highlighted the importance of facilitation and of recruiting facilitators from existing contexts with pre-existing positive relationships with CYP. Facilitators also suggested developing supporting training materials such as information videos and manuals to further support future implementation. Our mixed methods case study evaluation thus provides important learning for definitive clinical and cost-effectiveness studies and opportunities for optimising future implementation strategies.
Limitations
Our mixed methods study recruited from three study sites in Java, Indonesia (Jakarta, Bogor and Magelang). Indonesia has high levels of geographical, economic and cultural diversity and as such, our findings might not be transferable to other areas of Indonesia. Participants in the current study self-selected to participate in the study. It may be that those with an interest in mental health and digital interventions were more likely to volunteer to take part. Future research is required to evaluate our intervention with other groups including those with lower levels of digital literacy.
Our quantitative data collection processes were not powered to detect statistical difference and the aim was instead to assess the feasibility of the future evaluation of our intervention and interrogate our theory of change. While completion levels indicate high levels of feasibility in terms of future evaluation, robust randomised controlled trials are required to adequately assess clinical and cost effectiveness. The largest absolute changes are in the PedSQL at one month (+ 2.5 points). A clinically important change for a quality-of-life measure is considered to be in the region of 5 points. For example, if such data were used to inform a power calculation for a subsequent RCT to test the effectiveness of the game (versus, say, usual care), it would likely result in a very large sample size being required.
Conclusion
Our co-produced digital anxiety and depression focussed mental health literacy and self-management intervention was considered acceptable and easily implementable by CYP, parents and facilitators even in the context of the Covid-19 pandemic. The intervention is currently being culturally adapted for CYP in the UK demonstrating its flexibility for use in high and low resource settings. The chapter focussed design easily allows for expansion of our intervention which can be developed specifically for the needs of local populations, maximising its relevance and scope to include additional conditions, including comorbid non-communicable diseases and integrated care. Future research should explore equity in access to digital interventions in Indonesia and consider the impact of the digital literacy on engagement with our intervention.
Digital applications to support mental health literacy and self-management are potentially an acceptable and feasible way in which health, community and education settings can attempt to prevent future, and treat existing, burdens of common mental health problems amongst CYP in Indonesia. The results will be used to further refine our co-produced intervention prior to definitive evaluation of its clinical and cost effectiveness.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to ethical restrictions but are available from the corresponding author on reasonable request.
Abbreviations
- CYP:
-
Children and young people
- EBCD:
-
Experience based co-design
- LMIC:
-
Low and middle income country
- MHL:
-
Mental health literacy
- MHP:
-
Mental health problems
- PPI:
-
Patient and public involvement
- ToC:
-
Theory of change
- TFA:
-
Theoretical framework of acceptability
- UK:
-
United Kingdom
References
Gore FM, Bloem PJN, Patton GC, Ferguson J, Joseph V, Coffey C, et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. The Lancet. 2011;377(9783):2093–102.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602.
Jane Costello E, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? J Child Psychol Psychiatry. 2006;47(12):1263–71.
Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175(11):1142–50.
Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry. 2000;157(10):1584–91.
Haller SP, Cohen Kadosh K, Scerif G, Lau JY. Social anxiety disorder in adolescence: how developmental cognitive neuroscience findings may shape understanding and interventions for psychopathology. Dev Cogn Neurosci. 2015;13:11–20.
Lewinsohn PM, Rohde P, Seeley JR. Major depressive disorder in older adolescents: prevalence, risk factors, and clinical implications. Clin Psychol Rev. 1998;18(7):765–94.
Johnson AL. Changes in mental health and treatment, 1997–2017. J Health Soc Behav. 2021;62(1):53–68.
Damaiyanti M, editor Indonesia Prevalence of depression amongst Indonesian high school adolescents. 13th International Conference on Psychiatric-Mental Health Nursing 2016. London.
Lim SS, Allen K, Bhutta ZA, Dandona L, Forouzanfar MH, Fullman N, et al. Measuring the health-related sustainable development goals in 188 countries: a baseline analysis from the global burden of disease study 2015. Lancet. 2016;388(10053):1813–50.
World Health Organisation. Transforming our world: the 2030 agenda for sustainable development. New York: World Health Organisation; 2015.
Sari OK, Ramdhani N, Subandi S. Mental health in the digital age: psychologist professional services development opportunities. Media Health Res Dev. 2020;30(4):337–48.
Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health. 2020;17(22):8479.
World Health Organisation. WHO Mental Health Gap Action Programme (mhGAP). Geneva. Contract No.: 25 April 2023.
McDaid D, Park AL, Wahlbeck K. The economic case for the prevention of mental illness. Annu Rev Public Health. 2019;40:373–89.
Power E, Hughes S, Cotter D, Cannon M. Youth mental health in the time of COVID-19. Irish J Psychol Med. 2020;37(4):301–5.
Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. “Mental health literacy”: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust. 1997;166(4):182–6.
Kutcher S, Bagnell A, Wei Y. Mental health literacy in secondary schools: a Canadian approach. Child Adolesc Psychiatr Clin N Am. 2015;24(2):233–44.
Kutcher S, Wei Y, Coniglio C. Mental health literacy: past, present, and future. Can J Psychiatry. 2016;61(3):154–8.
Jorm A. We need to move from ‘mental health literacy’ to ‘mental health action.’ Mental Health Prev. 2020;18: 200179.
Weare K, Nind M. Mental health promotion and problem prevention in schools: what does the evidence say? Health Promot Int. 2011;26(Suppl 1):i29-69.
Neufeld SAS, Dunn VJ, Jones PB, Croudace TJ, Goodyer IM. Reduction in adolescent depression after contact with mental health services: a longitudinal cohort study in the UK. Lancet Psychiatry. 2017;4(2):120–7.
Lam LT. Mental health literacy and mental health status in adolescents: a population-based survey. Child and Adolescent Psychiatry and Mental Health. 2014. https://doi.org/10.1186/1753-2000-8-26
Brooks H, Irmansyah I, Lovell K, Savitri I, Utomo B, Prawira B, et al. Improving mental health literacy among young people aged 11–15years in Java, Indonesia: co-development and feasibility testing of a culturally-appropriate, user-centred resource (IMPeTUs)—a study protocol. Bmc Health Serv Res. 2019. https://doi.org/10.1186/s12913-019-4328-2.
Richards DA, Bower P, Pagel C, Weaver A, Utley M, Cape J, et al. Delivering stepped care: an analysis of implementation in routine practice. Implement Sci. 2012;7(1):3.
Brooks H, Syarif AK, Pedley R, Irmansyah I, Prawira B, Lovell K, et al. Improving mental health literacy among young people aged 11–15 years in Java, Indonesia: the co-development of a culturally-appropriate, user-centred resource (The IMPeTUs intervention). Child Adolesc Psychiatry Ment Health. 2021;15(1):56.
Renwick L, Pedley R, Johnson I, Bell V, Lovell K, Bee P, et al. Conceptualisations of positive mental health and wellbeing among children and adolescents in low- and middle-income countries: a systematic review and narrative synthesis. Health Expect. 2021. https://doi.org/10.1007/s00787-022-01997-6.
Renwick L, Pedley R, Johnson I, Bell V, Lovell K, Bee P, et al. Mental health literacy in children and adolescents in low- and middle-income countries: a mixed studies systematic review and narrative synthesis. Eur Child Adolesc Psychiatry. 2022. https://doi.org/10.1007/s00787-022-01997-6.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of medical research council guidance. BMJ. 2021;374: n2061.
Donetto S, Pierri P, Tsianakas V, Robert G. Experience-based co-design and healthcare improvement: realizing participatory design in the public sector. Des J. 2015;18(2):227–48.
Brooks H, Prawira B, Windfuhr K, Irmansyah I, Lovell K, Syarif AK, et al. Mental health literacy amongst children with common mental health problems and their parents in Java, Indonesia: a qualitative study. Global Mental Health. 2022. https://doi.org/10.1017/gmh.2022.5.
Brooks H, Windfuhr K, Irmansyah PB, Desyadi Putriningtyas DA, Lovell K, et al. Children and young people’s beliefs about mental health and illness in Indonesia: a qualitative study informed by the common sense model of self-regulation. PLoS One. 2022;17(2):e0263232.
World Health Organisation. Monitoring and evaluating digital health interventions. Switzerland: World Health Organisation; 2016.
Patton MQ. Essentials of Utilization-Focused Evaluation. London: Sage Publications Ltd.; 2012.
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach. BMC Med Res Methodol. 2011;11:100.
Schoonenboom J, Johnson RB. How to construct a mixed methods research design. Kolner Z Soz Sozpsychol. 2017;69(Suppl 2):107–31.
Teddlie C, Tashakkori A. A general typology of research designs featuring mixed methods. Res Sch. 2006;13(1):12–28.
Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17(1):88.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(1):117.
Wei Y, Zheng P, Deng H, Wang X, Li X, Fu H. Design features for improving mobile health intervention user engagement: systematic review and thematic analysis. J Med Internet Res. 2020;22(12): e21687.
Curtis BL, Ashford RD, Magnuson KI, Ryan-Pettes SR. Comparison of smartphone ownership, social media use, and willingness to use digital interventions between generation Z and millennials in the treatment of substance use: cross-sectional questionnaire study. J Med Internet Res. 2019;21(4): e13050.
Arjadi R, Nauta MH, Bockting CLH. Acceptability of internet-based interventions for depression in Indonesia. Internet Interv. 2018;13:8–15.
Best D, De Alwis SJ, Burdett D. The recovery movement and its implications for policy, commissioning and practice. Nordic Stud Alcohol Drugs. 2017;34(2):107–11.
Bockting CLH, Williams AD, Carswell K, Grech AE. The potential of low-intensity and online interventions for depression in low- and middle-income countries. Global Mental Health. 2016;3:e25.
Simkiss NJ, Gray NS, Dunne C, Snowden RJ. Development and psychometric properties of the knowledge and attitudes to mental health scales (KAMHS): a psychometric measure of mental health literacy in children and adolescents. BMC Pediatr. 2021;21(1):508.
Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care. 1999;37(2):126–39.
Setyowati A, Chung M, Yusuf A. Development of self-report assessment tool for anxiety among adolescents: indonesian version of the Zung self-rating anxiety scale. J Public Health Africa. 2019. https://doi.org/10.4081/jphia.2019.1172.
Reynolds WM. The Reynolds adolescent depression scale-second edition (RADS-2). Comprehensive handbook of psychological assessment, personality assessment, vol. 2. Hoboken: John Wiley & Sons, Inc; 2004. p. 224–36.
Olson D. FACES IV and the circumplex model: validation study. J Marital Fam Ther. 2011;37(1):64–80.
Acknowledgements
We would like to thank all the study sites, contributors and participants who took the time to support this study. The authors would like to thank the Patient and Public Advisory Panel for their ongoing contributions to the programme of work.
Funding
This project is funded by the MRC/DFID/NIHR/ESRC programme of research to improve adolescent health in low and middle income countries. (MR/R022151/1). The funders and sponsor have no role in study design, data collection and analysis, decision to publish, or preparation of manuscripts.
Author information
Authors and Affiliations
Contributions
HBrooks, PB, II, KL, LR, BP conceptualised the study. II, AKS, APR, CM contributed to study recruitment and data collection. HB, II, AK, RP, LR, APR, CM, MH, HBrieley, PB contributed to data analysis. BP led the patient and public involvement in the study. The drafting of the manuscript was led by HBrooks and PB. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Our study gained ethical approval from the University of Manchester Research Ethics Committee (REF: 8870) and The Ministry of Health Indonesia (Ref: LB:02.01/2/KE.201/2019). All adult participants provided written, informed consent to participate. For the CYP who participated in the study, assent was obtained along with written consent from their parents/guardian.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Example quotes.
Additional file 2:
Suggestions for future iterations of the digital application.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Brooks, H., Irmansyah, I., Syarif, A.K. et al. Evaluating a prototype digital mental health literacy intervention for children and young people aged 11–15 in Java, Indonesia: a mixed methods, multi-site case study evaluation. Child Adolesc Psychiatry Ment Health 17, 79 (2023). https://doi.org/10.1186/s13034-023-00608-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13034-023-00608-9