Abstract
In this narrative review, we reported un up-to-date on the role of radiomics to assess prognostic features, which can impact on the liver metastases patient treatment choice. In the liver metastases patients, the possibility to assess mutational status (RAS or MSI), the tumor growth pattern and the histological subtype (NOS or mucinous) allows a better treatment selection to avoid unnecessary therapies. However, today, the detection of these features require an invasive approach. Recently, radiomics analysis application has improved rapidly, with a consequent growing interest in the oncological field. Radiomics analysis allows the textural characteristics assessment, which are correlated to biological data. This approach is captivating since it should allow to extract biological data from the radiological images, without invasive approach, so that to reduce costs and time, avoiding any risk for the patients. Several studies showed the ability of Radiomics to identify mutational status, tumor growth pattern and histological type in colorectal liver metastases. Although, radiomics analysis in a non-invasive and repeatable way, however features as the poor standardization and generalization of clinical studies results limit the translation of this analysis into clinical practice. Clear limits are data-quality control, reproducibility, repeatability, generalizability of results, and issues related to model overfitting.
Similar content being viewed by others
Background
There is no doubt that from a radiologist point of view, the liver is probably the most insidious target, given the considerable amount of benign and malignant processes that can involve it [1,2,3,4,5,6,7,8]. Moreover, different pathologies can be synchronous or metachronous, so radiologists dedicated to the study of the liver should be experts and collaborate with a multidisciplinary team [9,10,11,12,13,14,15,16,17,18,19,20]. In a such complex situation, the radiological management of liver metastases patient requires great skill considering, also, the different management phases [21,22,23,24], as in terms of the most suitable radiological tools to use [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43], as in term of response assessment after different therapies [44,45,46,47,48,49,50].
In addition, the radiologist role has profoundly changed, having to answer increasingly critical questions. In fact, compared to the characterization and evaluation of lesion resectability, today a prognostic assessment is also required, for the identification of several features that can impact on the therapeutic choice [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38].
Among metastatic patients, the overall survival (OS) is profoundly related to different features, such as the stage of the disease, the lesion mutational status as well as the patient physical condition and it has been reported that although about 70–75% of patients survive within 1 year, fewer than 20% outside 5 years [51]. The main treatment for unfit surgical resection lesions is systemic therapy, based on the combination of cytotoxic chemotherapies, biologic therapies and or immunotherapy. Several clinical experiments have proven that modifying treatments according to tumor molecular and pathologic profiling could improve OS. Genomic characteristics are a critical point since these allow to identify the therapies that should be efficient. It has been proven that about the 50% of patients with KRAS/NRAS/BRAF wild-type lesions, can be treated with monoclonal antibodies to the epithelial growth factor receptor (EGFR) in combination with conventional cytotoxic treatments, with an OS improvement of 2 to 4 months compared to chemotherapy alone [51]. So as, immunotherapy could be utilized as upfront treatment, in patients with microsatellite instability or mismatch repair deficiency, improving OS of 31.4 months [51].
In addition, directed therapy, including hepatectomy, radiofrequency or microwave ablation, and/or hepatic artery infusion chemotherapy (HAIC), can be associated with 5-year OS as high as 60% [52, 53]. The definition for resectability of liver metastases in recent years has developed to comprise any patient in whom all liver lesions can be surgically eradicated with negative margins (R0) and an adequate future liver remnant can be preserved [54, 55]. However, about 60% of patients will have recurrence in the liver even after a complete surgical removal of all primary liver metastases.
At this time, it is complicated to exactly predict clinical outcome considering patient and primary lesion features. Clinical risk scores of Fong and Nordlinger were usually adopted to assess clinical outcome in this context [56, 57]. However, the validity of these risk scores is doubted, since these are considering outcomes of patients in the 1990’s, when the approach to treat liver metastases patients was overall more conservative [56, 57]. Another pre-surgical score, the Genetic And Morphologic Evaluation (GAME) score was improved, but is still not utilized in clinical setting [58]. Biomarkers correlated to the outcome can help the patient management. To this end, several prognostic biomarkers have been proposed, mainly focused on clinic-pathological characteristics as KRAS and BRAF mutational status, histopathological features (mucinous), and surgical resection margin [59,60,61,62,63,64,65,66,67].
Recently, the idea that imaging studies contain a great quantity of data, in form of grey level patterns, which are imperceptible to the human eyes, has become more and more interesting [68,69,70,71,72,73,74,75,76,77,78,79,80]. These texture features, when correlated with clinical-pathological data and outcomes [81,82,83,84,85,86,87,88,89,90,91,92,93], theoretically allow diagnostic and prognostic assessment [94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115]. The assessment of textural characteristics, obtained by radiological images, which depend on mathematical analysis, as histogram analysis, is called radiomics [116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133]. This approach is captivating since it should allow to extract biological data from the radiological images [134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156], without invasive approach, so that to reduce costs and time, avoiding any risk for the patients. For several tumors, radiomics analysis has already demonstrated an accurate biological features evaluation [157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174].
In this narrative review, we reported un up-to-date on the role of radiomics to assess prognostic features, which can impact on the liver metastases patient treatment choice.
RAS mutational status and radiomics
Advances in surgery and systemic therapy have improved the percentage of patients with liver metastases, which are technically resectable [175]. Although the number of technically resectable lesions was increasing, surgeons recognized the importance of tumor biology beyond technical resectability alone [175]. Even if the molecular studies initiated in the 2000s, only in 2013, Vauthey et al [176] demonstrated the prognostic role of molecular data (RAS mutation) in patients with colorectal liver metastases, so that RAS mutational status was routinely tested by determining the eligibility for anti-EGFR treatment. Consequently, Johns Hopkins Hospital (JHH) team [177] and The University of Texas MD Anderson Cancer Center team [178] combined RAS status with several clinic-pathologic features to develop the first two hybrid clinical and genetic risk scores. In addition, it has been demonstrated the negative effect of RAS mutations in patients re-treated with hepatectomy for recurrent liver metastases, so that RAS mutational status may impact on selection for a second hepatectomy [179].
KRAS, NRAS, and HRAS are the RAS oncogenes to encode a family of guanidine triphosphates (GTP)-adjusted switches [180,181,182]. KRAS gene is correlated to the colorectal cancer development and progression, representing an independent prognostic risk factor. Usually, the assessment of gene mutation status is based on the examination of specimens obtained from surgery or biopsy, which are expensive and invasive approaches. Since Lambin et al, first proposed the concept of Radiomics in 2012, this high-throughput, non-invasive strategy has been shown to provide addition data that can offer assistance for clinical decision making in several settings and different tumors [183,184,185,186,187,188,189,190,191,192,193,194,195,196,197,198,199,200,201,202,203,204,205,206,207,208,209,210,211,212,213,214,215,216,217,218,219,220]. Several previous studies have assessed the role of radiomics and RAS status in the primary colorectal lesions [221,222,223].
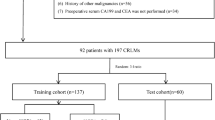
With regard to liver mutational status, the opportunity to compare RAS status and radiomic features provide significant advantages compare to quality evaluation, since this analysis allows a better patient selection for treatment, to predict response to therapies, discriminating favorable and unfavorable subsets of patients, including patients which could benefit from surgical resection [224,225,226,227,228,229,230,231,232,233,234,235,236,237,238,239,240,241,242,243,244,245,246,247,248,249,250,251,252,253,254,255,256,257,258,259]. Yang et al. [225] evaluated KRAS/NRAS/BRAF mutation in 117 untreated primary lesions (61 in the training and 56 in the validation set), obtaining 346 radiomics features from portal phase of CT studies. They demonstrated that radiomics features were significantly correlated with KRAS/NRAS/ BRAF mutation.
Lubner et al. [226] assessed texture features obtained from liver metastasis CT studies in 77 untreated patients, showing that entropy, mean positive pixels and standard deviation of medium filtration were correlated to tumor stage. In addition, skewness was negatively correlated to KRAS, while the coarse filtration entropy was correlated to OS.
Shi et al [227], in a multi-centric retrospective study, evaluated 159 untreated patients, which underwent CT studies. Radiomics features were obtained from the portal phase of the contrast studies. Seven machine learning algorithms were utilized to establish three scores based on the semantic, radiomics and the combination of both features. Two semantic and 851 radiomics features were used to predict the mutation status of RAS and BRAF using an artificial neural network method (ANN). They showed that this score can allow to distinguish wild type and mutant patients with an AUC of 0.95 in the training set and 0.79 in the validation set.
Granata et al [228] evaluated the association of RAS status and radiomics metrics by Contrast Enhanced (CE)-Magnetic Resonance Imaging (MRI). Significant results were obtained only for texture features using multivariate analysis, while the univariate analysis did not allow RAS status assessment.
Microsatellite instability and radiomics
Several types of genomic instability can drive tumor initiation and development. The main frequent type in colorectal cancer (about 85%) is chromosomal instability, while microsatellite instability (MSI) is found in 15% of lesions. MSI lesion is a kind of tumor in which the failure of mismatch repair genes (MMR), causes errors in short tandem repetitive DNA sequences known as microsatellites [260,261,262]. About the 5% of metastatic colorectal patients had MSI or deficient MMR [262].
Assessment of MSI status in colorectal cancer patients has prognostic and therapeutic effects. It has been shown that patients with MSI have longer OS compared to patients without MSI [263]. The reason is due to the fact that lesions with MSI have greater numbers of tumor-infiltrating lymphocytes that are activated and cytotoxic [263], so that the detection of MSI in a patient with colorectal cancer is a positive prognostic feature, particularly among young patients [263].
Today, it is clear the role of the host immune system in controlling tumor progression and new biomarkers have been included as a tool for the prediction of prognosis and response to therapy. MSI colorectal tumors display highly up-regulated expression of multiple immune checkpoints, including Programmed Death 1 (PD-1), Programmed Death-ligand 1 (PD-L1) and CTLA-4. It has been theorized that strategies involving the blockade of these immunoregulatory mechanisms might be selectively effective in this critical subset of patients [264,265,266,267,268,269,270,271].
Knowing the patients MSI status is critical since it should be correlated to immunotherapy response or resistance to fluorouracil-based therapies [272]. However, the diagnosis of MSI status is obtained by polymerase chain reaction (PCR) and immunohistochemistry achieved on pathological tissues from biopsies or surgical procedures. Therefore, it is mandatory to introduce a non-invasive and cost-effective procedure to assess MSI status. Golia Pernicka et al [273], by evaluating 254 radiomics features obtained by CT studies of 198 patients (134 patients without MSI and 64 with MSI tumors) developed 3 prognostication models based on clinical data alone, radiomics data alone, and combined radiomics and clinical data. The combined model outperformed the other two, with an AUC of 0.80 and 0.79 for the training and validation set, respectively [273]. Similar results were obtained by Fan et al. in the assessment of 119 stage II tumor patients [274]. Six radiomics features, obtained from pre-treatment CT studies, and 11 clinical data were utilized for predicting MSI status model. The combined model achieved the overall best performance obtaining an AUC, sensitivity, and specificity of 0.752, 0.663, and 0.841, respectively [274].
Wu et al. [275] developed a model by using several features to evaluate the diagnostic accuracy of dual-energy CT for discriminating MSI from MSS colorectal cancer. The AUC of the model provided relatively high diagnostic accuracy with an AUC value of 0.886, sensitivity 81.6%, and specificity of 81.6%.
At the best of our knowledge no studies assessed liver colorectal metastases MSI status and radiomics and the studies evaluating primary lesions should be interpreted with caution since the results are based on a limited number of patients. Further multicentric studies are required using a larger sample size in order to introduce this approach into everyday clinical practice [276,277,278,279].
Mucinous histological subtypes and radiomics
With regard to histological subtypes, there are inadequate data on the role of histological subtypes in colorectal cancer patient outcomes [128]. The most common histological type is adenocarcinoma not otherwise specified (NOS), followed by mucinous adenocarcinoma, which represents 5–15% of all lesions. A greater number of BRAF and KRAS mutations and higher rate of MSI characterize mucinous subtype, so that, compared to the NOS type, the mucinous lesion is correlated to a higher risk of metastases, worse OS and a weakness response to standard chemotherapy [280,281,282].
In this contest, it is evident that a proper detection and characterization of liver mucinous metastases allows a better patient selection to avoid unnecessary therapies.
At the best of our knowledge, few studies have assessed the ability of Radiomics features, obtained by CT or MRI, in mucinous liver metastases characterization [105, 108, 283,284,285]. Granata et al evaluated radiomics data obtained from CT studies of untreated patients and from MRI studies of pre-surgical patients compared to mucinous subtype [105, 108, 283,284,285].
With regard to data obtained from MRI studies with hepatospecific contrast agent (EOB) [105], the univariate analysis showed a variable number of metrics, which allow to discriminate mucinous subtype: 15 significant features extracted from T2W SPACE; 13 extracted from the arterial phase; 12 extracted from the portal phase; 12 extracted from the EOB-phase. The best results at univariate analysis were reached by the wavelet_LLH_glcm_JointEntropy extracted by T2W SPACE sequence with accuracy of 92%, a sensitivity of 83%, a specificity of 94%, a PPV and a NPV of 78 and 95%, respectively, with a cut-off value of 4.61. Linear regression model increased the performance obtained respect to the univariate analysis. The best results were obtained by a linear regression model of 15 significant features extracted by the T2W SPACE sequence with accuracy of 94%, a sensitivity of 92%, a specificity of 95%, a PPV and a NPV of 83 and 98%, respectively. This study has some limits: (1) small sample size, although the analysis was done on homogeneous subset and considering all lesions; (2) the retrospective nature, (3) a manual segmentation so as (4) the impact of chemotherapy on the results [105]. The main advantage was related to the assessment of all protocol study sequences [105].
Colorectal liver metastases growth pattern and radiomics
The majority of liver metastases have one of three common distinct histopathological growth patterns (HGPs), known as desmoplastic HGP, pushing HGP or replacement HGP, and two rare HGPs [286]. These HGPs are distinguishable because the interface between the tumor and the surrounding normal parenchymal is distinct in each growth pattern [286]. Moreover, the distinct topography of cancer cells in each HGP predicts HGP-specific interactions with parenchymal (hepatocytes and cholangiocytes) and non-parenchymal cells (sinusoidal endothelial cells, stellate cells and immune cells). However, despite these clear differences in the biology of these metastases, the molecular drivers of the distinct HGPs remain unknown. It is also currently unclear whether these distinct HGPs require different clinical management strategies, since these different patterns have shown to have prognostic significance [286]. Both Van den Eynden et al and Nielsen et al assessed the impact of the HGPs on OS in patients with liver metastases. In both studies, the desmoplastic HGP represented superior OS [287, 288]. The replacement HGP indicates not only worse OS but also resistance to systemic therapy [289]. Moreover, the HGP sub-types have diverse immune-phenotypes that are correlated to different responses to immunotherapy. Evidence showed a lower immune cells or inflammatory cells infiltration rate in the replacement sub-type while desmoplastic type is frequently surrounded by many lymphocytes [289].
The gold standard for HGP diagnosis is the histopathological analysis of the untreated resected specimen [289]. Considering the low fraction of primarily resectable metastases and the wide use of preoperative chemotherapy, clinical relevance is limited [289,290,291,292,293,294,295]. Therefore, a non-invasive strategy is needed to improve the prognosis and facilitate the treatment strategy [289]. In addition, a non-invasive approach would also allow for longitudinal response evaluation during treatment [289, 296,297,298,299,300,301,302,303,304,305,306].
Several researches have assessed the role of radiomics in the HGP pattern [109, 113, 141, 143, 145, 307], showing that HGPs of liver metastases can be effectively characterized using CT or/and MRI- radiomics data. Cheg et al [143] evaluated 126 metastatic patients who had undergone CT studies and surgical resection with histopathologically confirmed HGPs (desmoplastic HGP in 68 patients and replacement HGP in 58). The authors showed that combined, clinical-radiomics signature had the best performance in differentiating replacement from desmoplastic type [143]. Han et al. [141] assessed MRI radiomics features of 182 resected untreated metastases (desmoplastic HGPs in 59 patients and replacement HGPs in 123), using a decision tree algorithm and a combined clinical and radiomics model. They found that the combined model had good discriminating capability, with the AUC of 0.971, 0.909, and 0.905, respectively, in the training, internal validating, and external validating set [141]. Granata et al [307], analyzing a training set of 51 patients (121 metastases) and an external validation set of 30 patients (30 lesions), obtained 851 radiomics features from MRI studies in pre-surgical phase. They showed that, at univariate analysis, the best results to discriminate expansive versus infiltrative HGPs were obtained by the wavelet_LHH_glrlm_ShortRunLowGray Level Emphasis from portal phase. In addition, by using a linear regression model, the performance was higher for all sequences except that for hepatobiliary phase. Furthermore, using pattern recognition approaches, the diagnostic performance increased again and the best classifier was a weighted KNN trained [307].
The main limits of assessed studies are related to the retrospective nature, the type of segmentation and the sample size.
Prospects and limits
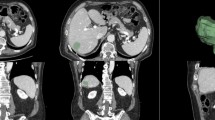
Recently, the radiomics field has developed rapidly, and the pattern recognition approaches introduction has supported faster quantitative data extraction processes [308,309,310]. By extracting a great deal of quantitative features from conventional medical imaging, radiomics analysis (Fig. 1) allows to obtain biological information without invasive approach. Compared with conventional and qualitative analysis, this approach should, hypothetically, improve cancer diagnosis, grading and staging, treatment response and prognosis prediction, providing professional guidance for treatment planning [311,312,313,314,315,316].
Even if there is a great interest on Radiomic as a very promising tool, however the poor standardization and generalization of studies results limit the translation of this analysis into clinical practice. Clear limits are data-quality control, reproducibility, repeatability, generalizability of results, and issues related to model overfitting [317,318,319,320,321].
The main critical issues are the necessity of images of high quality, so as the standardization of studies protocol and reconstruction algorithms [322, 323]. In addition, ample size and comprehensiveness of datasets, separate training and validation sets, class imbalances and overfitting are critical points. Beyond randomized trials, class inequalities are usual. So that, not only overall accuracy but also class wise accuracy, or sensitivity or specificity, should be assessed [322, 323]. When a model is not well balanced in terms of function approximation, one may encounter overfitting or, to a lesser degree, underfitting. Overfitting is due to the assessment of a large number of input parameters, which not are all relevant. To avoid overfitting, it is necessary to apply smoothing model feature, or to reduce the number of input features by reducing the number of model parameters required. Validation using a separate dataset helps detect overfitting. Underfitting arises or when a model is not able to appropriately classify data in the training and validation datasets, or if it is excessively simplistic [324,325,326,327,328,329,330,331,332,333,334].
Therefore, radiomics analysis should be performed considering all these aspects in order to obtain robust and reproducible data which could be generalized in other patient classes.
Conclusion
Recently, radiomics analysis application has improved rapidly, with a consequent growing interest in the oncological field. In addition, the possibility to analyse with faster processes large amount of data with pattern recognition approaches is significantly changing the idea of radiology.
In the liver metastases clinical setting, the possibility to assess mutational status (RAS or MSI), the tumour growth pattern and the histological subtype (NOS or mucinous) allows a better patient selection to avoid unnecessary treatment. Although, radiomics analysis in a non-invasive and repeatable way, also during treatment, by using imaging tools used in clinical practice, however features as the poor standardization and generalization of clinical studies results limit the translation of this analysis into clinical practice. Clear limits are data-quality control, reproducibility, repeatability, generalizability of results, and issues related to model overfitting.
Data availability
All data are available in the manuscript and at https://zenodo.org/record/7741988#.ZBNQm3bMK3A.
Change history
05 May 2023
A Correction to this paper has been published: https://doi.org/10.1186/s13027-023-00508-9
References
Arai Y, Helmberger T, White S, Zech J. C. The challenge of liver tumors for interventional oncology: past, present and future - introductory editorial. Br J Radiol. 2022 Sep 1;95(1138):20229005. doi: https://doi.org/10.1259/bjr.20229005.
Xiao Y, Zheng X, Zhou C, Huang P, Wu F, Yang C, Zeng M. Combined hepatocellular carcinoma-cholangiocarcinoma with a predominant HCC component: better survival and MRI-based prediction. Eur Radiol. 2022 Sep;16. https://doi.org/10.1007/s00330-022-09131-5. Epub ahead of print.
Granata V, Fusco R, Catalano O, Avallone A, Leongito M, Izzo F, Petrillo A. Peribiliary liver metastases MR findings. Med Oncol. 2017 Jul;34(7):124. https://doi.org/10.1007/s12032-017-0981-7.
Yang Z, Zhang C, Li Z, Wu L, Li M. Comparison of Hepatectomy and Hemangiomas Stripping on Patients with Giant Hepatic Hemangiomas.Contrast Media Mol Imaging. 2022 Aug31;2022:1350826. doi: https://doi.org/10.1155/2022/1350826.
Cholangiocarcinoma Working Group. Italian Clinical Practice Guidelines on Cholangiocarcinoma - Part II: Treatment. Dig Liver Dis. 2020 Dec;52(12):1430–1442. doi: https://doi.org/10.1016/j.dld.2020.08.030.
Granata V, Fusco R, Venanzio Setola S, Mattace Raso M, Avallone A, De Stefano A, Nasti G, Palaia R, Delrio P, Petrillo A, Izzo F. Liver radiologic findings of chemotherapy-induced toxicity in liver colorectal metastases patients. Eur Rev Med Pharmacol Sci. 2019 Nov;23(22):9697–706. https://doi.org/10.26355/eurrev_201911_19531.
Granata V, Fusco R, Avallone A, Cassata A, Palaia R, Delrio P, Grassi R, Tatangelo F, Grazzini G, Izzo F, Petrillo A. Abbreviated MRI protocol for colorectal liver metastases: How the radiologist could work in pre surgical setting.PLoS One. 2020 Nov19;15(11):e0241431. doi: https://doi.org/10.1371/journal.pone.0241431.
Schooler GR, Infante JC, Acord M, Alazraki A, Chavhan GB, Davis JC, Khanna G, Morani AC, Morin CE, Nguyen HN, Rees MA, Shaikh R, Srinivasan A, Squires JH, Tang E, Thacker PG, Towbin AJ. Imaging of pediatric liver tumors: a COG Diagnostic Imaging Committee/SPR Oncology Committee White Paper. Pediatr Blood Cancer. 2022 Sep;14:e29965. https://doi.org/10.1002/pbc.29965.
Papaconstantinou D, Tsilimigras DI, Pawlik TM. Recurrent Hepatocellular Carcinoma: Patterns, Detection, Staging and Treatment.J Hepatocell Carcinoma. 2022 Sep3;9:947–957. doi: https://doi.org/10.2147/JHC.S342266.
Granata V, Fusco R, Petrillo A. Additional considerations on use of abbreviated liver MRI in patients with colorectal liver metastases. AJR Am J Roentgenol. 2021 Jul;217(1):W1. https://doi.org/10.2214/AJR.21.25652.
Granata V, Grassi R, Fusco R, Setola SV, Belli A, Ottaiano A, Nasti G, La Porta M, Danti G, Cappabianca S, Cutolo C, Petrillo A, Izzo F. Intrahepatic cholangiocarcinoma and its differential diagnosis at MRI: how radiologist should assess MR features. Radiol Med. 2021 Dec;126(12):1584–600. https://doi.org/10.1007/s11547-021-01428-7.
Granata V, Fusco R, Avallone A, Catalano O, Piccirillo M, Palaia R, Nasti G, Petrillo A, Izzo F. A radiologist’s point of view in the presurgical and intraoperative setting of colorectal liver metastases. Future Oncol. 2018 Sep;14(21):2189–206. https://doi.org/10.2217/fon-2018-0080.
Granata V, Fusco R, Catalano O, Avallone A, Palaia R, Botti G, Tatangelo F, Granata F, Cascella M, Izzo F, Petrillo A. Diagnostic accuracy of magnetic resonance, computed tomography and contrast enhanced ultrasound in radiological multimodality assessment of peribiliary liver metastases.PLoS One. 2017 Jun20;12(6):e0179951. doi: https://doi.org/10.1371/journal.pone.0179951.
Aboutaleb M, Kheirkhah N, Samani A, Sadeghi-Naini A. An Enhanced Method for Full-Inversion-Based Ultrasound Elastography of the Liver.Annu Int Conf IEEE Eng Med Biol Soc. 2022Jul;2022:3887–3890. doi: https://doi.org/10.1109/EMBC48229.2022.9871656.
Izzo F, Piccirillo M, Albino V, Palaia R, Belli A, Granata V, Setola S, Fusco R, Petrillo A, Orlando R, Tosone G, Scordino F, Curley SA. Prospective screening increases the detection of potentially curable hepatocellular carcinoma: results in 8,900 high-risk patients. HPB (Oxford). 2013 Dec;15(12):985–90. https://doi.org/10.1111/hpb.12080.
Avallone A, Pecori B, Bianco F, Aloj L, Tatangelo F, Romano C, Granata V, Marone P, Leone A, Botti G, Petrillo A, Caracò C, Iaffaioli VR, Muto P, Romano G, Comella P, Budillon A, Delrio P. Critical role of bevacizumab scheduling in combination with pre-surgical chemo-radiotherapy in MRI-defined high-risk locally advanced rectal cancer: Results of the BRANCH trial. Oncotarget. 2015 Oct 6;6(30):30394-407. doi: https://doi.org/10.18632/oncotarget.4724.
Bimonte S, Leongito M, Barbieri A, Del Vecchio V, Barbieri M, Albino V, Piccirillo M, Amore A, Di Giacomo R, Nasto A, Granata V, Petrillo A, Arra C, Izzo F. Inhibitory effect of (-)-epigallocatechin-3-gallate and bleomycin on human pancreatic cancer MiaPaca-2 cell growth.Infect Agent Cancer. 2015 Jul29;10:22. doi: https://doi.org/10.1186/s13027-015-0016-y.
Ottaiano A, Scala S, Santorsola M, Trotta AM, D’Alterio C, Portella L, Clemente O, Nappi A, Zanaletti N, De Stefano A, Avallone A, Granata V, Notariello C, Luce A, Lombardi A, Picone C, Petrillo A, Perri F, Tatangelo F, Di Mauro A, Albino V, Izzo F, Rega D, Pace U, Di Marzo M, Chiodini P, De Feo G, Del Prete P, Botti G, Delrio P, Caraglia M, Nasti G. Aflibercept or bevacizumab in combination with FOLFIRI as second-line treatment of mRAS metastatic colorectal cancer patients: the ARBITRATION study protocol. Ther Adv Med Oncol. 2021 Mar;24:13:1758835921989223. https://doi.org/10.1177/1758835921989223.
Ottaiano A, Caraglia M, Di Mauro A, Botti G, Lombardi A, Galon J, Luce A, D’Amore L, Perri F, Santorsola M, Hermitte F, Savarese G, Tatangelo F, Granata V, Izzo F, Belli A, Scala S, Delrio P, Circelli L, Nasti G. Evolution of Mutational Landscape and Tumor Immune-Microenvironment in Liver Oligo-Metastatic Colorectal Cancer. Cancers (Basel). 2020 Oct 21;12(10):3073. doi: https://doi.org/10.3390/cancers12103073.
Izzo F, Granata V, Fusco R, D’Alessio V, Petrillo A, Lastoria S, Piccirillo M, Albino V, Belli A, Tafuto S, Avallone A, Patrone R, Palaia R. Clinical Phase I/II Study: Local Disease Control and Survival in Locally Advanced Pancreatic Cancer Treated with Electrochemotherapy. J Clin Med. 2021 Mar 22;10(6):1305. doi: https://doi.org/10.3390/jcm10061305.
Izzo F, Granata V, Fusco R, D’Alessio V, Petrillo A, Lastoria S, Piccirillo M, Albino V, Belli A, Nasti G, Avallone A, Patrone R, Grassi F, Leongito M, Palaia R. A Multicenter Randomized controlled prospective study to assess efficacy of laparoscopic Electrochemotherapy in the treatment of locally Advanced Pancreatic Cancer. J Clin Med. 2021 Sep;5(17):4011. https://doi.org/10.3390/jcm10174011.
Avallone A, Piccirillo MC, Nasti G, Rosati G, Carlomagno C, Di Gennaro E, Romano C, Tatangelo F, Granata V, Cassata A, Silvestro L, De Stefano A, Aloj L, Vicario V, Nappi A, Leone A, Bilancia D, Arenare L, Petrillo A, Lastoria S, Gallo C, Botti G, Delrio P, Izzo F, Perrone F, Budillon A. Effect of Bevacizumab in Combination With Standard Oxaliplatin-Based Regimens in Patients With Metastatic Colorectal Cancer: A Randomized Clinical Trial. JAMA Netw Open. 2021 Jul 1;4(7):e2118475. doi: https://doi.org/10.1001/jamanetworkopen.2021.18475.
Ottaiano A, Petito A, Santorsola M, Gigantino V, Capuozzo M, Fontanella D, Di Franco R, Borzillo V, Buonopane S, Ravo V, Scipilliti E, Totaro G, Serra M, Ametrano G, Penta R, Tatangelo F, Scognamiglio G, Di Mauro A, Di Bonito M, Napolitano M, Scala S, Rea G, Santagata S, Lombardi A, Grimaldi A, Caputo C, Crispo A, Celentano E, De Feo G, Circelli L, Savarese G, Ruggiero R, Perri F, Granata V, Botti G, Caraglia M, Nasti G, Muto P. Prospective Evaluation of Radiotherapy-Induced Immunologic and Genetic Effects in Colorectal Cancer Oligo-Metastatic Patients with Lung-Limited Disease: The PRELUDE-1 Study. Cancers (Basel). 2021 Aug 23;13(16):4236. doi: https://doi.org/10.3390/cancers13164236.
Ottaiano A, de Vera d’Aragona RP, Trotta AM, Santorsola M, Napolitano M, Scognamiglio G, Tatangelo F, Grieco P, Zappavigna S, Granata V, Perri F, Luce A, Savarese G, Ianniello M, Casillo M, Petrillo N, Belli A, Izzo F, Nasti G, Caraglia M, Scala S. Characterization of KRAS Mutational Regression in Oligometastatic Patients. Front Immunol. 2022 Jul;22:13:898561. https://doi.org/10.3389/fimmu.2022.898561.
Argalia G, Tarantino G, Ventura C, Campioni D, Tagliati C, Guardati P, Kostandini A, Marzioni M, Giuseppetti GM, Giovagnoni A. Shear wave elastography and transient elastography in HCV patients after direct-acting antivirals. Radiol Med. 2021 Jun;126(6):894–9. https://doi.org/10.1007/s11547-020-01326-4.
Giovagnoni A. A farewell from the “old” editor-in-Chief. Radiol Med. 2021 Jan;126(1):1–2. https://doi.org/10.1007/s11547-020-01325-5.
Cicero G, Mazziotti S, Silipigni S, Blandino A, Cantisani V, Pergolizzi S, D’Angelo T, Stagno A, Maimone S, Squadrito G, Ascenti G. Dual-energy CT quantification of fractional extracellular space in cirrhotic patients: comparison between early and delayed equilibrium phases and correlation with oesophageal varices. Radiol Med. 2021 Jun;126(6):761–7. https://doi.org/10.1007/s11547-021-01341-z.
Granata V, Fusco R, Setola SV, Avallone A, Palaia R, Grassi R, Izzo F, Petrillo A. Radiological assessment of secondary biliary tree lesions: an update. J Int Med Res. 2020 Jun;48(6):300060519850398. https://doi.org/10.1177/0300060519850398.
Granata V, Grassi R, Fusco R, Belli A, Palaia R, Carrafiello G, Miele V, Grassi R, Petrillo A, Izzo F. Local ablation of pancreatic tumors: State of the art and future perspectives. World J Gastroenterol. 2021 Jun 21;27(23):3413–3428. doi: https://doi.org/10.3748/wjg.v27.i23.3413.
Fusco R, Simonetti I, Ianniello S, Villanacci A, Grassi F, Dell’Aversana F, Grassi R, Cozzi D, Bicci E, Palumbo P, Borgheresi A, Giovagnoni A, Miele V, Barile A, Granata V. Pulmonary Lymphangitis Poses a Major Challenge for Radiologists in an Oncological Setting during the COVID-19 Pandemic. J Pers Med. 2022 Apr 12;12(4):624. doi: https://doi.org/10.3390/jpm12040624.
Granata V, Fusco R, Salati S, Petrillo A, Di Bernardo E, Grassi R, Palaia R, Danti G, La Porta M, Cadossi M, Gašljević G, Sersa G, Izzo F. A systematic review about imaging and histopathological findings for detecting and evaluating Electroporation based treatments response. Int J Environ Res Public Health. 2021 May;24(11):5592. https://doi.org/10.3390/ijerph18115592.
Tafuto S, von Arx C, De Divitiis C, Maura CT, Palaia R, Albino V, Fusco R, Membrini M, Petrillo A, Granata V, Izzo F, ENETS Center of Excellence Multidisciplinary Group for Neuroendocrine Tumors in Naples (Italy). Electrochemotherapy as a new approach on pancreatic cancer and on liver metastases. Int J Surg. 2015 Sep;21(Suppl 1):78–82. https://doi.org/10.1016/j.ijsu.2015.04.095.
Semaan S, Vietti Violi N, Lewis S, Chatterji M, Song C, Besa C, Babb JS, Fiel MI, Schwartz M, Thung S, Sirlin CB, Taouli B. Hepatocellular carcinoma detection in liver cirrhosis: diagnostic performance of contrast-enhanced CT vs. MRI with extracellular contrast vs. gadoxetic acid. Eur Radiol. 2020 Feb;30(2):1020–30. https://doi.org/10.1007/s00330-019-06458-4.
Lee DH, Lee JM, Baek JH, Shin CI, Han JK, Choi BI. Diagnostic performance of gadoxetic acid-enhanced liver MR imaging in the detection of HCCs and allocation of transplant recipients on the basis of the Milan criteria and UNOS guidelines: correlation with histopathologic findings. Radiology. 2015 Jan;274(1):149–60. https://doi.org/10.1148/radiol.14140141.
Granata V, Fusco R, Maio F, Avallone A, Nasti G, Palaia R, Albino V, Grassi R, Izzo F, Petrillo A. Qualitative assessment of EOB-GD-DTPA and Gd-BT-DO3A MR contrast studies in HCC patients and colorectal liver metastases.Infect Agent Cancer. 2019 Nov27;14:40. doi: https://doi.org/10.1186/s13027-019-0264-3.
Zech CJ, Ba-Ssalamah A, Berg T, Chandarana H, Chau GY, Grazioli L, Kim MJ, Lee JM, Merkle EM, Murakami T, Ricke J, Sirlin B, Song C, Taouli B, Yoshimitsu B, Koh K. Consensus report from the 8th International Forum for Liver magnetic resonance imaging. Eur Radiol. 2020 Jan;30(1):370–82. https://doi.org/10.1007/s00330-019-06369-4.
Granata V, Catalano O, Fusco R, Tatangelo F, Rega D, Nasti G, Avallone A, Piccirillo M, Izzo F, Petrillo A. The target sign in colorectal liver metastases: an atypical Gd-EOB-DTPA “uptake” on the hepatobiliary phase of MR imaging. Abdom Imaging. 2015 Oct;40(7):2364–71. https://doi.org/10.1007/s00261-015-0488-7.
Stefanini M, Simonetti G. Interventional magnetic resonance imaging suite (IMRIS): how to build and how to use. Radiol Med. 2022 Aug;26. https://doi.org/10.1007/s11547-022-01537-x.
Granata V, Fusco R, Setola SV, Castelguidone ELD, Camera L, Tafuto S, Avallone A, Belli A, Incollingo P, Palaia R, Izzo F, Petrillo A. The multidisciplinary team for gastroenteropancreatic neuroendocrine tumours: the radiologist’s challenge.Radiol Oncol. 2019 Oct25;53(4):373–387. doi: https://doi.org/10.2478/raon-2019-0040.
Nakamura Y, Higaki T, Honda Y, Tatsugami F, Tani C, Fukumoto W, Narita K, Kondo S, Akagi M, Awai K. Advanced CT techniques for assessing hepatocellular carcinoma. Radiol Med. 2021 Jul;126(7):925–35. https://doi.org/10.1007/s11547-021-01366-4.
Perl RM, Portugall J, Hinterleitner C, Hinterleitner M, Kloth C, Walter SS, Bitzer M, Horger MS. Differences Between CT-Perfusion and Biphasic Contrast-enhanced CT for Detection and Characterization of Hepatocellular Carcinoma: Potential Explanations for Discrepant Cases.Anticancer Res. 2021Mar;41(3):1451–1458. doi: https://doi.org/10.21873/anticanres.14903.
Kurucay M, Kloth C, Kaufmann S, Nikolaou K, Bösmüller H, Horger M, Thaiss WM. Multiparametric imaging for detection and characterization of hepatocellular carcinoma using gadoxetic acid-enhanced MRI and perfusion-CT: which parameters work best?Cancer Imaging. 2017 Jun28;17(1):18. doi: https://doi.org/10.1186/s40644-017-0121-9.
Fusco R, Setola SV, Raiano N, Granata V, Cerciello V, Pecori B, Petrillo A. Analysis of a monocentric computed tomography dosimetric database using a radiation dose index monitoring software: dose levels and alerts before and after the implementation of the adaptive statistical iterative reconstruction on CT images. Radiol Med. 2022 Jul;127(7):733–42. https://doi.org/10.1007/s11547-022-01481-w.
De Muzio F, Cutolo C, Dell’Aversana F, Grassi F, Ravo L, Ferrante M, Danti G, Flammia F, Simonetti I, Palumbo P, Bruno F, Pierpaoli L, Fusco R, Giovagnoni A, Miele V, Barile A, Granata V. Complications after Thermal Ablation of Hepatocellular Carcinoma and Liver Metastases: Imaging Findings. Diagnostics (Basel). 2022 May 5;12(5):1151. doi: https://doi.org/10.3390/diagnostics12051151.
Ierardi AM, Stellato E, Pellegrino G, Bonelli C, Cellina M, Renzulli M, Biondetti P, Carrafiello G. Fluid-dynamic control microcatheter used with glue: preliminary experience on its feasibility and safety. Radiol Med. 2022 Mar;127(3):272–6. https://doi.org/10.1007/s11547-022-01461-0.
Granata V, Fusco R, Catalano O, Filice S, Amato DM, Nasti G, Avallone A, Izzo F, Petrillo A. Early Assessment of Colorectal Cancer Patients with Liver Metastases Treated with Antiangiogenic Drugs: The Role of Intravoxel Incoherent Motion in Diffusion-Weighted Imaging. PLoS One. 2015 Nov 13;10(11):e0142876. doi: https://doi.org/10.1371/journal.pone.0142876.
Izzo F, Palaia R, Albino V, Amore A, di Giacomo R, Piccirillo M, Leongito M, Nasto A, Granata V, Petrillo A, Lastoria S. Hepatocellular carcinoma and liver metastases: clinical data on a new dual-lumen catheter kit for surgical sealant infusion to prevent perihepatic bleeding and dissemination of cancer cells following biopsy and loco-regional treatments.Infect Agent Cancer. 2015 Apr10;10:11. doi: https://doi.org/10.1186/s13027-015-0006-0.
Granata V, Fusco R, Setola SV, Piccirillo M, Leongito M, Palaia R, Granata F, Lastoria S, Izzo F, Petrillo A. Early radiological assessment of locally advanced pancreatic cancer treated with electrochemotherapy. World J Gastroenterol. 2017 Jul 14;23(26):4767–4778. doi: https://doi.org/10.3748/wjg.v23.i26.4767.
Granata V, Fusco R, Piccirillo M, Palaia R, Petrillo A, Lastoria S, Izzo F. Electrochemotherapy in locally advanced pancreatic cancer: preliminary results. Int J Surg. 2015 Jun;18:230–6. https://doi.org/10.1016/j.ijsu.2015.04.055.
Granata V, Fusco R, de Lutio di Castelguidone E, Avallone A, Palaia R, Delrio P, Tatangelo F, Botti G, Grassi R, Izzo F, Petrillo A. Diagnostic performance of gadoxetic acid-enhanced liver MRI versus multidetector CT in the assessment of colorectal liver metastases compared to hepatic resection. BMC Gastroenterol. 2019 Jul;24(1):129. https://doi.org/10.1186/s12876-019-1036-7.
Biller LH, Schrag D. Diagnosis and treatment of metastatic colorectal Cancer: a review. JAMA. 2021 Feb;16(7):669–85. https://doi.org/10.1001/jama.2021.0106.
Kopetz S, Chang GJ, Overman MJ, et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol. 2009;27(22):3677–83.
Pawlik TM, Scoggins CR, Zorzi D et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005;241(5):715–722, discussion 722–714.
Pawlik TM, Schulick RD, Choti MA. Expanding criteria for resectability of colorectal liver metastases. Oncologist. 2008;13(1):51–64.
Aquina CT, Brown ZJ, Beane JD, Ejaz A, Cloyd JM, Tsung A, Adam MO, Pawlik TM, Kim AC. Disparities in Care Access to Liver-Directed Therapy among Medicare beneficiaries with colorectal Cancer Liver Metastasis. Ann Surg Oncol. 2022 Sep;23:1–10. https://doi.org/10.1245/s10434-022-12513-0.
Fong Y, et al. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230(3):309–18. discussion 318 – 21.
Nordlinger B, et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients, Association Francaise de Chirurgie. Cancer. 1996;77(7):1254–62.
Margonis GA, et al. Genetic and morphological evaluation (GAME) score for patients with colorectal liver metastases. Br J Surg. 2018;105(9):1210–20.
Fusco R, Granata V, Rega D, Russo C, Pace U, Pecori B, Tatangelo F, Botti G, Izzo F, Cascella M, et al. Morphological and functional features prognostic factor of magnetic resonance imaging in locally advanced rectal cancer. Acta Radiol. 2018;60:815–25.
Fusco R, Petrillo M, Granata V, Filice S, Sansone M, Catalano O, Petrillo A. Magnetic resonance imaging evaluation in neoadjuvant therapy of locally advanced rectal cancer: a systematic review. Radiol Oncol. 2017;51:252–62.
Van den Eynden GG, Bird NC, Majeed AW, Van Laere S, Dirix LY, Vermeulen PB. The histological growth pattern of colorectal cancer liver metastases has prognostic value. Clin Exp Metastasis. 2012;29:541–9.
Eefsen RL, Vermeulen PB, Christensen IJ, Laerum OD, Mogensen MB, Rolff HC, Van Den Eynden GG, Høyer-Hansen G, Osterlind K, Vainer B, et al. Growth pattern of colorectal liver metastasis as a marker of recurrence risk. Clin Exp Metastasis. 2015;32:369–81.
Moro CF, Bozóky B, Gerling M. Growth patterns of colorectal cancer liver metastases and their impact on prognosis: a systematic review. BMJ Open Gastroenterol. 2018;5:e000217.
Chiloiro G, Cusumano D, de Franco P, Lenkowicz J, Boldrini L, Carano D, Barbaro B, Corvari B, Dinapoli N, Giraffa M, et al. Does restaging MRI radiomics analysis improve pathological complete response prediction in rectal cancer patients? A prognostic model development. Radiol Med. 2022;127:11–20.
Hof J, Kok K, Sijmons RH, De Jong KP. Systematic review of the Prognostic Role of the Immune System after surgery of Colorectal Liver Metastases. Front Oncol. 2019;9:148.
Park SH, Kim YS, Choi J. Dosimetric analysis of the effects of a temporary tissue expander on the radiotherapy technique. Radiol Med. 2021 Mar;126(3):437–44. https://doi.org/10.1007/s11547-020-01297-6.
Bozkurt M, Eldem G, Bozbulut UB, Bozkurt MF, Kılıçkap S, Peynircioğlu B, Çil B, Lay Ergün E, Volkan-Salanci B. Factors affecting the response to Y-90 microsphere therapy in the cholangiocarcinoma patients. Radiol Med. 2021 Feb;126(2):323–33. https://doi.org/10.1007/s11547-020-01240-9.
Dercle L, Lu L, Schwartz LH, Qian M, Tejpar S, Eggleton P, Zhao B, Piessevaux H. Radiomics Response Signature for Identification of Metastatic Colorectal Cancer Sensitive to Therapies Targeting EGFR Pathway. J Natl Cancer Inst. 2020 Sep 1;112(9):902–912. doi: https://doi.org/10.1093/jnci/djaa017.
Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009 May;50(Suppl 1):122S–50S. https://doi.org/10.2967/jnumed.108.057307.
Spinczyk D. Measuring Respiratory Motion for Supporting the Minimally Invasive Destruction of Liver Tumors. Sensors (Basel). 2022 Aug 26;22(17):6446. doi: https://doi.org/10.3390/s22176446.
Bera K, Braman N, Gupta A, Velcheti V, Madabhushi A. Predicting cancer outcomes with radiomics and artificial intelligence in radiology. Nat Rev Clin Oncol. 2022 Feb;19(2):132–46. https://doi.org/10.1038/s41571-021-00560-7.
Taghavi M, Trebeschi S, Simões R, Meek DB, Beckers RCJ, Lambregts DMJ, Verhoef C, Houwers JB, van der Heide UA, Beets-Tan RGH, Maas M. Machine learning-based analysis of CT radiomics model for prediction of colorectal metachronous liver metastases. Abdom Radiol (NY). 2021 Jan;46(1):249–56. https://doi.org/10.1007/s00261-020-02624-1.
Granata V, de Lutio di Castelguidone E, Fusco R, Catalano O, Piccirillo M, Palaia R, Izzo F, Gallipoli AD, Petrillo A. Irreversible electroporation of hepatocellular carcinoma: preliminary report on the diagnostic accuracy of magnetic resonance, computer tomography, and contrast-enhanced ultrasound in evaluation of the ablated area. Radiol Med. 2016 Feb;121(2):122–31. https://doi.org/10.1007/s11547-015-0582-5. Epub 2015 Sep 7. PMID: 26345332.
Rocca A, Brunese MC, Santone A, Avella P, Bianco P, Scacchi A, Scaglione M, Bellifemine F, Danzi R, Varriano G, Vallone G, Calise F, Brunese L. Early diagnosis of Liver Metastases from Colorectal Cancer through CT Radiomics and formal methods: a pilot study. J Clin Med. 2021 Dec;22(1):31. https://doi.org/10.3390/jcm11010031.
Merlotti A, Bruni A, Borghetti P, Ramella S, Scotti V, Trovò M, Chiari R, Lohr F, Ricardi U, Bria E, Pappagallo GL, D’Angelillo RM, Arcangeli S. Sequential chemo-hypofractionated RT versus concurrent standard CRT for locally advanced NSCLC: GRADE recommendation by the Italian Association of Radiotherapy and Clinical Oncology (AIRO). Radiol Med. 2021 Aug;126(8):1117–28. https://doi.org/10.1007/s11547-021-01362-8.
Wei J, Cheng J, Gu D, Chai F, Hong N, Wang Y, Tian J. Deep learning-based radiomics predicts response to chemotherapy in colorectal liver metastases.Med Phys. 2021 Jan;48(1):513–522. doi: https://doi.org/10.1002/mp.14563.
Dias AG, Pinto DFS, Borges MF, Pereira MH, Santos JAM, Cunha LT, Lencart J. Optimization of skin dose using in-vivo MOSFET dose measurements in bolus/non-bolus fraction ratio: a VMAT and a 3DCRT study. J Appl Clin Med Phys. 2019 Feb;20(2):63–70. https://doi.org/10.1002/acm2.12525.
Falcinelli L, Mendichi M, Chierchini S, Tenti MV, Bellavita R, Saldi S, Ingrosso G, Reggioli V, Bini V, Aristei C. Pulmonary function in stereotactic body radiotherapy with helical tomotherapy for primary and metastatic lung lesions. Radiol Med. 2021 Jan;126(1):163–9. https://doi.org/10.1007/s11547-020-01223-w.
Arslan A, Aktas E, Sengul B, Tekin B. Dosimetric evaluation of left ventricle and left anterior descending artery in left breast radiotherapy. Radiol Med. 2021 Jan;126(1):14–21. https://doi.org/10.1007/s11547-020-01201-2.
Barra S, Guarnieri A, di Monale E, Bastia MB, Marcenaro M, Tornari E, Belgioia L, Magrini SM, Ricardi U, Corvò R. Short fractionation radiotherapy for early prostate cancer in the time of COVID-19: long-term excellent outcomes from a multicenter italian trial suggest a larger adoption in clinical practice. Radiol Med. 2021 Jan;126(1):142–6. https://doi.org/10.1007/s11547-020-01216-9.
Cellini F, Di Franco R, Manfrida S, Borzillo V, Maranzano E, Pergolizzi S, Morganti AG, Fusco V, Deodato F, Santarelli M, Arcidiacono F, Rossi R, Reina S, Merlotti A, Jereczek-Fossa BA, Tozzi A, Siepe G, Cacciola A, Russi E, Gambacorta MA, Scorsetti M, Ricardi U, Corvò R, Donato V, Muto P, Valentini V. Palliative radiotherapy indications during the COVID-19 pandemic and in future complex logistic settings: the NORMALITY model. Radiol Med. 2021 Dec;126(12):1619–56. https://doi.org/10.1007/s11547-021-01414-z.
Lancellotta V, Del Regno L, Di Stefani A, Fionda B, Marazzi F, Rossi E, Balducci M, Pampena R, Morganti AG, Mangoni M, Lebbe C, Garbe C, Longo C, Schinzari G, Tagliaferri L, Peris K. The role of stereotactic radiotherapy in addition to immunotherapy in the management of melanoma brain metastases: results of a systematic review. Radiol Med. 2022 Jul;127(7):773–83. https://doi.org/10.1007/s11547-022-01503-7.
Hewitt DB, Pawlik TM, Cloyd JM. Who will benefit? Using Radiomics to predict response to oxaliplatin-based chemotherapy in patients with colorectal liver metastases. Ann Surg Oncol. 2021 Jun;28(6):2931–3. https://doi.org/10.1245/s10434-020-09586-0.
Creasy JM, Cunanan KM, Chakraborty J, McAuliffe JC, Chou J, Gonen M, Kingham VS, Weiser MR, Balachandran VP, Drebin JA, Kingham TP, Jarnagin WR, D’Angelica MI, Do RKG, Simpson AL. Differences in Liver Parenchyma are measurable with CT Radiomics at initial Colon resection in patients that develop hepatic metastases from stage II/III Colon cancer. Ann Surg Oncol. 2021 Apr;28(4):1982–9. https://doi.org/10.1245/s10434-020-09134-w.
Hussein MAM, Cafarelli FP, Paparella MT, Rennie WJ, Guglielmi G. Phosphaturic mesenchymal tumors: radiological aspects and suggested imaging pathway. Radiol Med. 2021 Dec;126(12):1609–18. https://doi.org/10.1007/s11547-021-01412-1.
Danti G, Flammia F, Matteuzzi B, Cozzi D, Berti V, Grazzini G, Pradella S, Recchia L, Brunese L, Miele V. Gastrointestinal neuroendocrine neoplasms (GI-NENs): hot topics in morphological, functional, and prognostic imaging. Radiol Med. 2021 Dec;126(12):1497–507. https://doi.org/10.1007/s11547-021-01408-x.
Petrillo A, Fusco R, Petrillo M, Granata V, Sansone M, Avallone A, Delrio P, Pecori B, Tatangelo F, Ciliberto G. Standardized Index of Shape (SIS): a quantitative DCE-MRI parameter to discriminate responders by non-responders after neoadjuvant therapy in LARC. Eur Radiol. 2015 Jul;25(7):1935–45. https://doi.org/10.1007/s00330-014-3581-3. Epub 2015 Jan 11. PMID: 25577525.
Laurelli G, Falcone F, Gallo MS, Scala F, Losito S, Granata V, Cascella M, Greggi S. Long-Term Oncologic and Reproductive Outcomes in Young Women with Early Endometrial Cancer conservatively treated: a prospective study and literature update. Int J Gynecol Cancer. 2016 Nov;26(9):1650–7. https://doi.org/10.1097/IGC.0000000000000825.
Taghavi M, Staal F, Gomez Munoz F, Imani F, Meek DB, Simões R, Klompenhouwer LG, van der Heide UA, Beets-Tan RGH, Maas M. CT-Based Radiomics Analysis before Thermal ablation to Predict Local Tumor Progression for Colorectal Liver Metastases. Cardiovasc Intervent Radiol. 2021 Jun;44(6):913–20. https://doi.org/10.1007/s00270-020-02735-8.
Fiz F, Costa G, Gennaro N, la Bella L, Boichuk A, Sollini M, Politi LS, Balzarini L, Torzilli G, Chiti A, Viganò L. Contrast Administration Impacts CT-Based Radiomics of Colorectal Liver Metastases and Non-Tumoral Liver Parenchyma Revealing the “Radiological” Tumour Microenvironment. Diagnostics (Basel). 2021 Jun 25;11(7):1162. doi: https://doi.org/10.3390/diagnostics11071162.
Fiz F, Viganò L, Gennaro N, Costa G, La Bella L, Boichuk A, Cavinato L, Sollini M, Politi LS, Chiti A, Torzilli G. Radiomics of Liver Metastases: A Systematic Review. Cancers (Basel). 2020 Oct 7;12(10):2881. doi: https://doi.org/10.3390/cancers12102881.
Saini A, Breen I, Pershad Y, Naidu S, Knuttinen MG, Alzubaidi S, Sheth R, Albadawi H, Kuo M, Oklu R. Radiogenomics and Radiomics in Liver Cancers. Diagnostics (Basel). 2018 Dec 27;9(1):4. doi: https://doi.org/10.3390/diagnostics9010004.
Becker AS, Schneider MA, Wurnig MC, Wagner M, Clavien PA, Boss A. Radiomics of liver MRI predict metastases in mice. Eur Radiol Exp. 2018;2(1):11. https://doi.org/10.1186/s41747-018-0044-7.
Staal FCR, Taghavi M, van der Reijd DJ, Gomez FM, Imani F, Klompenhouwer EG, Meek D, Roberti S, de Boer M, Lambregts DMJ, Beets-Tan RGH, Maas M. Predicting local tumour progression after ablation for colorectal liver metastases: CT-based radiomics of the ablation zone. Eur J Radiol. 2021 Aug;141:109773. https://doi.org/10.1016/j.ejrad.2021.109773.
Rizzetto F, Calderoni F, De Mattia C, Defeudis A, Giannini V, Mazzetti S, Vassallo L, Ghezzi S, Sartore-Bianchi A, Marsoni S, Siena S, Regge D, Torresin A, Vanzulli A. Impact of inter-reader contouring variability on textural radiomics of colorectal liver metastases.Eur Radiol Exp. 2020 Nov10;4(1):62. doi: https://doi.org/10.1186/s41747-020-00189-8.
Kobe A, Zgraggen J, Messmer F, Puippe G, Sartoretti T, Alkadhi H, Pfammatter T, Mannil M. Prediction of treatment response to transarterial radioembolization of liver metastases: Radiomics analysis of pre-treatment cone-beam CT: A proof of concept study.Eur J Radiol Open. 2021 Aug30;8:100375. doi: https://doi.org/10.1016/j.ejro.2021.100375.
Maclean D, Tsakok M, Gleeson F, Breen DJ, Goldin R, Primrose J, Harris A, Franklin J. Comprehensive Imaging Characterization of Colorectal Liver Metastases.Front Oncol. 2021 Dec7;11:730854. doi: https://doi.org/10.3389/fonc.2021.730854.
Granata V, Fusco R, Barretta ML, Picone C, Avallone A, Belli A, Patrone R, Ferrante M, Cozzi D, Grassi R, Grassi R, Izzo F, Petrillo A. Radiomics in hepatic metastasis by colorectal cancer.Infect Agent Cancer. 2021 Jun2;16(1):39. doi: https://doi.org/10.1186/s13027-021-00379-y.
Yuan ZG, Zeng TM, Tao CJ. Current and emerging immunotherapeutic approaches for biliary tract cancers. Hepatobiliary Pancreat Dis Int. 2022 Sep 7:S1499-3872(22)00201-6. doi: https://doi.org/10.1016/j.hbpd.2022.08.015.
Taieb J, Svrcek M, Cohen R, Basile D, Tougeron D, Phelip JM. Deficient mismatch repair/microsatellite unstable colorectal cancer: Diagnosis, prognosis and treatment.Eur J Cancer. 2022 Sep14;175:136–157. doi: https://doi.org/10.1016/j.ejca.2022.07.020.
Granata V, Fusco R, Costa M, Picone C, Cozzi D, Moroni C, La Casella GV, Montanino A, Monti R, Mazzoni F, Grassi R, Malagnino VG, Cappabianca S, Grassi R, Miele V, Petrillo A. Preliminary Report on Computed Tomography Radiomics Features as Biomarkers to Immunotherapy Selection in Lung Adenocarcinoma Patients. Cancers (Basel). 2021 Aug 7;13(16):3992. doi: https://doi.org/10.3390/cancers13163992.
Fushimi Y, Yoshida K, Okawa M, Maki T, Nakajima S, Sakata A, Okuchi S, Hinoda T, Kanagaki M, Nakamoto Y. Vessel wall MR imaging in neuroradiology.Radiol Med. 2022 Jul30:1–14. doi: https://doi.org/10.1007/s11547-022-01528-y.
Granata V, Simonetti I, Fusco R, Setola SV, Izzo F, Scarpato L, Vanella V, Festino L, Simeone E, Ascierto PA, Petrillo A. Management of cutaneous melanoma: radiologists challenging and risk assessment. Radiol Med. 2022 Aug;127(8):899–911. https://doi.org/10.1007/s11547-022-01522-4.
Cirillo L, Rustici A, Toni F, Zoli M, Bartiromo F, Gramegna LL, Cicala D, Tonon C, Caranci F, Lodi R. Vessel Wall MRI: clinical implementation in cerebrovascular disorders-technical aspects. Radiol Med. 2022 Jun;127(6):645–51. https://doi.org/10.1007/s11547-022-01484-7.
Granata V, Fusco R, De Muzio F, Cutolo C, Setola SV, Dell’Aversana F, Grassi F, Belli A, Silvestro L, Ottaiano A, Nasti G, Avallone A, Flammia F, Miele V, Tatangelo F, Izzo F, Petrillo A. Radiomics and machine learning analysis based on magnetic resonance imaging in the assessment of liver mucinous colorectal metastases. Radiol Med. 2022 Jul;127(7):763–72. https://doi.org/10.1007/s11547-022-01501-9.
Tagliafico AS, Campi C, Bianca B, Bortolotto C, Buccicardi D, Francesca C, Prost R, Rengo M, Faggioni L. Blockchain in radiology research and clinical practice: current trends and future directions. Radiol Med. 2022 Apr;127(4):391–7. https://doi.org/10.1007/s11547-022-01460-1.
Chiti G, Grazzini G, Flammia F, Matteuzzi B, Tortoli P, Bettarini S, Pasqualini E, Granata V, Busoni S, Messserini L, Pradella S, Massi D, Miele V. Gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs): a radiomic model to predict tumor grade. Radiol Med. 2022 Aug 2. doi: https://doi.org/10.1007/s11547-022-01529-x.
Granata V, Fusco R, De Muzio F, Cutolo C, Setola SV, Grassi R, Grassi F, Ottaiano A, Nasti G, Tatangelo F, Pilone V, Miele V, Brunese MC, Izzo F, Petrillo A. Radiomics textural features by MR imaging to assess clinical outcomes following liver resection in colorectal liver metastases. Radiol Med. 2022 May;127(5):461–70. https://doi.org/10.1007/s11547-022-01477-6.
Starmans MPA, Buisman FE, Renckens M, Willemssen FEJA, van der Voort SR, Groot Koerkamp B, Grünhagen DJ, Niessen WJ, Vermeulen PB, Verhoef C, Visser JJ, Klein S. Distinguishing pure histopathological growth patterns of colorectal liver metastases on CT using deep learning and radiomics: a pilot study. Clin Exp Metastasis. 2021 Oct;38(5):483–94. https://doi.org/10.1007/s10585-021-10119-6.
Giannini V, Defeudis A, Rosati S, Cappello G, Mazzetti S, Panic J, Regge D, Balestra G. An innovative radiomics approach to predict response to chemotherapy of liver metastases based on CT images. Annu Int Conf IEEE Eng Med Biol Soc. 2020 Jul;2020:1339–42. https://doi.org/10.1109/EMBC44109.2020.9176627.
Bao H, Chen T, Zhu J, Xie H, Chen F. CEUS-Based Radiomics Can Show Changes in Protein Levels in Liver Metastases After Incomplete Thermal Ablation.Front Oncol. 2021 Aug26;11:694102. doi: https://doi.org/10.3389/fonc.2021.694102.
Qin H, Wu YQ, Lin P, Gao RZ, Li X, Wang XR, Chen G, He Y, Yang H. Ultrasound Image-Based Radiomics: an innovative method to identify primary tumorous sources of liver metastases. J Ultrasound Med. 2021 Jun;40(6):1229–44. https://doi.org/10.1002/jum.15506.
Wei S, Han Y, Zeng H, Ye S, Cheng J, Chai F, Wei J, Zhang J, Hong N, Bao Y, Zhou J, Ye Y, Meng X, Zhou Y, Deng Y, Qiu M, Tian J, Wang Y. Radiomics diagnosed histopathological growth pattern in prediction of response and 1-year progression free survival for colorectal liver metastases patients treated with bevacizumab containing chemotherapy. Eur J Radiol. 2021 Sep;142:109863. https://doi.org/10.1016/j.ejrad.2021.109863.
Giannini V, Rosati S, Defeudis A, Balestra G, Vassallo L, Cappello G, Mazzetti S, De Mattia C, Rizzetto F, Torresin A, Sartore-Bianchi A, Siena S, Vanzulli A, Leone F, Zagonel V, Marsoni S, Regge D. Radiomics predicts response of individual HER2-amplified colorectal cancer liver metastases in patients treated with HER2-targeted therapy. Int J Cancer. 2020 Dec;147(1):3215–23. https://doi.org/10.1002/ijc.33271.
Viganò L, Jayakody Arachchige VS, Fiz F. Is precision medicine for colorectal liver metastases still a utopia? New perspectives by modern biomarkers, radiomics, and artificial intelligence. World J Gastroenterol. 2022 Feb;14(6):608–23. https://doi.org/10.3748/wjg.v28.i6.608.
Fusco R, Granata V, Sansone M, Rega D, Delrio P, Tatangelo F, Romano C, Avallone A, Pupo D, Giordano M, Grassi R, Ravo V, Pecori B, Petrillo A. Validation of the standardized index of shape tool to analyze DCE-MRI data in the assessment of neo-adjuvant therapy in locally advanced rectal cancer. Radiol Med. 2021 Aug;126(8):1044–54. https://doi.org/10.1007/s11547-021-01369-1.
Latacz E, van Dam PJ, Vanhove C, Llado L, Descamps B, Ruiz N, Joye I, Grünhagen D, Van Laere S, Dirix P, Mollevi DG, Verhoef C, Dirix L, Vermeulen P. Can medical imaging identify the histopathological growth patterns of liver metastases?Semin Cancer Biol. 2021 Jun;71:33–41. doi: https://doi.org/10.1016/j.semcancer.2020.07.002.
Wang L, Tan J, Ge Y, Tao X, Cui Z, Fei Z, Lu J, Zhang H, Pan Z. Assessment of liver metastases radiomic feature reproducibility with deep-learning-based semi-automatic segmentation software. Acta Radiol. 2021 Mar;62(3):291–301. https://doi.org/10.1177/0284185120922822.
Ye S, Han Y, Pan X, Niu K, Liao Y, Meng X. Association of CT-Based Delta Radiomics Biomarker With Progression-Free Survival in Patients With Colorectal Liver Metastases Undergo Chemotherapy.Front Oncol. 2022 May27;12:843991. doi: https://doi.org/10.3389/fonc.2022.843991.
Liu M, Ma X, Shen F, Xia Y, Jia Y, Lu J. MRI-based radiomics nomogram to predict synchronous liver metastasis in primary rectal cancer patients. Cancer Med. 2020 Jul;9(14):5155–63. https://doi.org/10.1002/cam4.3185.
Hegde PS, Chen DS. Top 10 Challenges in Cancer Immunotherapy. Immunity. 2020 Jan 14;52(1):17–35. doi: https://doi.org/10.1016/j.immuni.2019.12.011.
Renzulli M, Brandi N, Argalia G, Brocchi S, Farolfi A, Fanti S, Golfieri R. Morphological, dynamic and functional characteristics of liver pseudolesions and benign lesions. Radiol Med. 2022 Feb;127(2):129–44. https://doi.org/10.1007/s11547-022-01449-w.
Li N, Wakim J, Koethe Y, Huber T, Schenning R, Gade TP, Hunt SJ, Park BJ. Multicenter assessment of augmented reality registration methods for image-guided interventions. Radiol Med. 2022 Aug;127(8):857–65. https://doi.org/10.1007/s11547-022-01515-3.
Ledda RE, Silva M, McMichael N, Sartorio C, Branchi C, Milanese G, Nayak SM, Sverzellati N. The diagnostic value of grey-scale inversion technique in chest radiography. Radiol Med. 2022 Mar;127(3):294–304. https://doi.org/10.1007/s11547-022-01453-0.
Sansone M, Marrone S, Di Salvio G, Belfiore MP, Gatta G, Fusco R, Vanore L, Zuiani C, Grassi F, Vietri MT, Granata V, Grassi R. Comparison between two packages for pectoral muscle removal on mammographic images. Radiol Med. 2022 Aug;127(8):848–56. https://doi.org/10.1007/s11547-022-01521-5.
Granata V, Fusco R, Belli A, Danti G, Bicci E, Cutolo C, Petrillo A, Izzo F. Diffusion weighted imaging and diffusion kurtosis imaging in abdominal oncological setting: why and when.Infect Agent Cancer. 2022 Jun9;17(1):25. doi: https://doi.org/10.1186/s13027-022-00441-3.
Petrillo A, Fusco R, Di Bernardo E, Petrosino T, Barretta ML, Porto A, Granata V, Di Bonito M, Fanizzi A, Massafra R, Petruzzellis N, Arezzo F, Boldrini L, La Forgia D. Prediction of Breast Cancer Histological Outcome by Radiomics and Artificial Intelligence Analysis in Contrast-Enhanced Mammography. Cancers (Basel). 2022 Apr 25;14(9):2132. doi: https://doi.org/10.3390/cancers14092132.
Granata V, Fusco R, De Muzio F, Cutolo C, Setola SV, Dell’Aversana F, Belli A, Romano C, Ottaiano A, Nasti G, Avallone A, Miele V, Tatangelo F, Petrillo A, Izzo F. Magnetic resonance features of liver mucinous colorectal metastases: what the Radiologist should know. J Clin Med. 2022 Apr;15(8):2221. https://doi.org/10.3390/jcm11082221.
Cutolo C, Dell’Aversana F, Fusco R, Grazzini G, Chiti G, Simonetti I, Bruno F, Palumbo P, Pierpaoli L, Valeri T, Izzo F, Giovagnoni A, Grassi R, Miele V, Barile A, Granata V. Combined Hepatocellular-Cholangiocarcinoma: What the Multidisciplinary Team Should Know. Diagnostics (Basel). 2022 Apr 2;12(4):890. doi: https://doi.org/10.3390/diagnostics12040890.
Committeri U, Fusco R, Di Bernardo E, Abbate V, Salzano G, Maglitto F, Dell’Aversana Orabona G, Piombino P, Bonavolontà P, Arena A, Perri F, Maglione MG, Setola SV, Granata V, Iaconetta G, Ionna F, Petrillo A, Califano L. Radiomics Metrics Combined with Clinical Data in the Surgical Management of Early-Stage (cT1-T2 N0) Tongue Squamous Cell Carcinomas: A Preliminary Study. Biology (Basel). 2022 Mar 18;11(3):468. doi: https://doi.org/10.3390/biology11030468.
Fusco R, Sansone M, Filice S, Granata V, Catalano O, Amato DM, Di Bonito M, D'Aiuto M, Capasso I, Rinaldo M, Petrillo A. Integration of DCE-MRI and DW-MRI Quantitative Parameters for Breast Lesion Classification. Biomed Res Int. 2015;2015:237863. https://doi.org/10.1155/2015/237863. Epub 2015 Aug 3. PMID: 26339597; PMCID: PMC4538369.
Giannini V, Pusceddu L, Defeudis A, Nicoletti G, Cappello G, Mazzetti S, Sartore-Bianchi A, Siena S, Vanzulli A, Rizzetto F, Fenocchio E, Lazzari L, Bardelli A, Marsoni S, Regge D. Delta-Radiomics Predicts Response to First-Line Oxaliplatin-Based Chemotherapy in Colorectal Cancer Patients with Liver Metastases. Cancers (Basel). 2022 Jan 4;14(1):241. doi: https://doi.org/10.3390/cancers14010241.
Wang Y, Ma LY, Yin XP, Gao BL. Radiomics and Radiogenomics in Evaluation of Colorectal Cancer Liver Metastasis.Front Oncol. 2022 Jan7;11:689509. doi: https://doi.org/10.3389/fonc.2021.689509.
Defeudis A, Cefaloni L, Giannetto G, Cappello G, Rizzetto F, Panic J, Barra D, Nicoletti G, Mazzetti S, Vanzulli A, Regge D, Giannini V. Comparison of radiomics approaches to predict resistance to 1st line chemotherapy in liver metastatic colorectal cancer. Annu Int Conf IEEE Eng Med Biol Soc. 2021 Nov;2021:3305–8. https://doi.org/10.1109/EMBC46164.2021.9630316.
Tharmaseelan H, Hertel A, Tollens F, Rink J, Woźnicki P, Haselmann V, Ayx I, Nörenberg D, Schoenberg SO, Froelich MF. Identification of CT Imaging Phenotypes of Colorectal Liver Metastases from Radiomics Signatures-Towards Assessment of Interlesional Tumor Heterogeneity. Cancers (Basel). 2022 Mar 24;14(7):1646. doi: https://doi.org/10.3390/cancers14071646.
Markich R, Palussière J, Catena V, Cazayus M, Fonck M, Bechade D, Buy X, Crombé A. Radiomics complements clinical, radiological, and technical features to assess local control of colorectal cancer lung metastases treated with radiofrequency ablation. Eur Radiol. 2021 Nov;31(11):8302–14. https://doi.org/10.1007/s00330-021-07998-4.
Wesdorp NJ, van Goor VJ, Kemna R, Jansma EP, van Waesberghe JHTM, Swijnenburg RJ, Punt CJA, Huiskens J, Kazemier G. Advanced image analytics predicting clinical outcomes in patients with colorectal liver metastases: a systematic review of the literature. Surg Oncol. 2021 Sep;38:101578. https://doi.org/10.1016/j.suronc.2021.101578.
Li M, Li X, Guo Y, Miao Z, Liu X, Guo S, Zhang H. Development and assessment of an individualized nomogram to predict colorectal cancer liver metastases. Quant Imaging Med Surg. 2020 Feb;10(2):397–414. https://doi.org/10.21037/qims.2019.12.16.
Costa G, Cavinato L, Masci C, Fiz F, Sollini M, Politi LS, Chiti A, Balzarini L, Aghemo A, di Tommaso L, Ieva F, Torzilli G, Viganò L. Virtual Biopsy for Diagnosis of Chemotherapy-Associated Liver Injuries and Steatohepatitis: A Combined Radiomic and Clinical Model in Patients with Colorectal Liver Metastases. Cancers (Basel). 2021 Jun 20;13(12):3077. doi: https://doi.org/10.3390/cancers13123077.
Jones RP, Brudvik KW, Franklin JM, Poston GJ. Precision surgery for colorectal liver metastases: Opportunities and challenges of omics-based decision making. Eur J Surg Oncol. 2017 May;43(5):875–83. https://doi.org/10.1016/j.ejso.2017.02.014.
Han Y, Chai F, Wei J, Yue Y, Cheng J, Gu D, Zhang Y, Tong T, Sheng W, Hong N, Ye Y, Wang Y, Tian J. Identification of predominant histopathological growth patterns of colorectal liver metastasis by Multi-Habitat and Multi-Sequence Based Radiomics Analysis. Front Oncol. 2020 Aug;14:10:1363. https://doi.org/10.3389/fonc.2020.01363.
Hu R, Chen I, Peoples J, Salameh JP, Gönen M, Romesser PB, Simpson AL, Reyngold M. Radiomics artificial intelligence modelling for prediction of local control for colorectal liver metastases treated with radiotherapy.Phys Imaging Radiat Oncol. 2022 Sep13;24:36–42. doi: https://doi.org/10.1016/j.phro.2022.09.004.
Cheng J, Wei J, Tong T, Sheng W, Zhang Y, Han Y, Gu D, Hong N, Ye Y, Tian J, Wang Y. Prediction of histopathologic growth patterns of Colorectal Liver Metastases with a noninvasive imaging method. Ann Surg Oncol. 2019 Dec;26(13):4587–98. https://doi.org/10.1245/s10434-019-07910-x.
Donato H, França M, Candelária I, Caseiro-Alves F, Liver MRI. From basic protocol to advanced techniques. Eur J Radiol. 2017 Aug;93:30–9. https://doi.org/10.1016/j.ejrad.2017.05.028.
Li S, Li Z, Huang X, Zhang P, Deng J, Liu X, Xue C, Zhang W, Zhou J. CT, MRI, and radiomics studies of liver metastasis histopathological growth patterns: an up-to-date review. Abdom Radiol (NY). 2022 Oct;47(10):3494–506. https://doi.org/10.1007/s00261-022-03616-z.
Bianchi A, Mazzoni LN, Busoni S, Pinna N, Albanesi M, Cavigli E, Cozzi D, Poggesi A, Miele V, Fainardi E, Gadda D. Assessment of cerebrovascular disease with computed tomography in COVID-19 patients: correlation of a novel specific visual score with increased mortality risk. Radiol Med. 2021 Apr;126(4):570–6. https://doi.org/10.1007/s11547-020-01313-9.
Cartocci G, Colaiacomo MC, Lanciotti S, Andreoli C, De Cicco ML, Brachetti G, Pugliese S, Capoccia L, Tortora A, Scala A, Valentini C, Almberger M, D’Aprile MR, Avventurieri G, Giura R, Kharrub Z, Leonardi A, Boccia M, Catalano C, Ricci P. Correction to: Chest CT for early detection and management of coronavirus disease (COVID-19): a report of 314 patients admitted to Emergency Department with suspected pneumonia. Radiol Med. 2021 Apr;126(4):642. doi: https://doi.org/10.1007/s11547-020-01292-x. Erratum for: Radiol Med. 2020 Oct;125(10):931–942.
Masci GM, Iafrate F, Ciccarelli F, Pambianchi G, Panebianco V, Pasculli P, Ciardi MR, Mastroianni CM, Ricci P, Catalano C, Francone M. Tocilizumab effects in COVID-19 pneumonia: role of CT texture analysis in quantitative assessment of response to therapy. Radiol Med. 2021 Sep;126(9):1170–80. https://doi.org/10.1007/s11547-021-01371-7.
Francolini G, Desideri I, Stocchi G, Ciccone LP, Salvestrini V, Garlatti P, Aquilano M, Greto D, Bonomo P, Meattini I, Scotti V, Scoccianti S, Simontacchi G, Livi L. Impact of COVID-19 on workload burden of a complex radiotherapy facility. Radiol Med. 2021 May;126(5):717–21. https://doi.org/10.1007/s11547-021-01338-8.
Ligero M, Jordi-Ollero O, Bernatowicz K, Garcia-Ruiz A, Delgado-Muñoz E, Leiva D, Mast R, Suarez C, Sala-Llonch R, Calvo N, Escobar M, Navarro-Martin A, Villacampa G, Dienstmann R, Perez-Lopez R. Minimizing acquisition-related radiomics variability by image resampling and batch effect correction to allow for large-scale data analysis. Eur Radiol. 2021 Mar;31(3):1460–70. https://doi.org/10.1007/s00330-020-07174-0.
Spinelli MS, Balbaa MF, Gallazzi MB, Eid ME, Kotb HT, Shafei ME, Ierardi AM, Daolio PA, Barile A, Carrafiello G. Role of percutaneous CT-guided radiofrequency ablation in treatment of intra-articular, in close contact with cartilage and extra-articular osteoid osteomas: comparative analysis and new classification system. Radiol Med. 2022 Oct;127(10):1142–50. https://doi.org/10.1007/s11547-022-01542-0.
Caruso D, Polici M, Rinzivillo M, Zerunian M, Nacci I, Marasco M, Magi L, Tarallo M, Gargiulo S, Iannicelli E, Annibale B, Laghi A, Panzuto F. CT-based radiomics for prediction of therapeutic response to Everolimus in metastatic neuroendocrine tumors. Radiol Med. 2022 Jul;127(7):691–701. https://doi.org/10.1007/s11547-022-01506-4.
Han D, Yu N, Yu Y, He T, Duan X. Performance of CT radiomics in predicting the overall survival of patients with stage III clear cell renal carcinoma after radical nephrectomy. Radiol Med. 2022 Aug;127(8):837–47. https://doi.org/10.1007/s11547-022-01526-0.
Donati OF, Hany TF, Reiner CS, von Schulthess GK, Marincek B, Seifert B, Weishaupt D. Value of retrospective fusion of PET and MR images in detection of hepatic metastases: comparison with 18F-FDG PET/CT and Gd-EOB-DTPA-enhanced MRI. J Nucl Med. 2010 May;51(5):692–9. https://doi.org/10.2967/jnumed.109.068510.
Masci GM, Ciccarelli F, Mattei FI, Grasso D, Accarpio F, Catalano C, Laghi A, Sammartino P, Iafrate F. Role of CT texture analysis for predicting peritoneal metastases in patients with gastric cancer. Radiol Med. 2022 Mar;127(3):251–8. https://doi.org/10.1007/s11547-021-01443-8.
Fusco R, Granata V, Mazzei MA, Meglio ND, Roscio DD, Moroni C, Monti R, Cappabianca C, Picone C, Neri E, Coppola F, Montanino A, Grassi R, Petrillo A, Miele V. Quantitative imaging decision support (QIDS™) tool consistency evaluation and radiomic analysis by means of 594 metrics in lung carcinoma on chest CT scan.Cancer Control. 2021 Jan-Dec;28:1073274820985786. doi: https://doi.org/10.1177/1073274820985786.
Zerunian M, Pucciarelli F, Caruso D, Polici M, Masci B, Guido G, De Santis D, Polverari D, Principessa D, Benvenga A, Iannicelli E, Laghi A. Artificial intelligence based image quality enhancement in liver MRI: a quantitative and qualitative evaluation. Radiol Med. 2022 Sep;7. https://doi.org/10.1007/s11547-022-01539-9.
Kang YJ, Cho JH, Hwang SH. Diagnostic value of various criteria for deep lobe involvement in radiologic studies with parotid mass: a systematic review and meta-analysis. Radiol Med. 2022 Aug;26. https://doi.org/10.1007/s11547-022-01540-2.
Borgheresi A, De Muzio F, Agostini A, Ottaviani L, Bruno A, Granata V, Fusco R, Danti G, Flammia F, Grassi R, Grassi F, Bruno F, Palumbo P, Barile A, Miele V, Giovagnoni A. Lymph nodes evaluation in rectal Cancer: where do we stand and future perspective. J Clin Med. 2022 May;5(9):2599. https://doi.org/10.3390/jcm11092599.
Tamburini E, Tassinari D, Ramundo M, De Stefano A, Viola MG, Romano C, Elia MT, Zanaletti N, Rudnas B, Casadei-Gardini A, Delrio P, Toma I, Granata V, Petrucelli L, Avallone A. Adjuvant chemotherapy after neoadjuvant chemo-radiotherapy and surgery in locally advanced rectal cancer. A systematic review of literature with a meta-analysis of randomized clinical trials. Crit Rev Oncol Hematol. 2022 Apr;172:103627. https://doi.org/10.1016/j.critrevonc.2022.103627.
Granata V, Grassi R, Fusco R, Belli A, Cutolo C, Pradella S, Grazzini G, La Porta M, Brunese MC, De Muzio F, Ottaiano A, Avallone A, Izzo F, Petrillo A. Diagnostic evaluation and ablation treatments assessment in hepatocellular carcinoma.Infect Agent Cancer. 2021 Jul19;16(1):53. doi: https://doi.org/10.1186/s13027-021-00393-0.
Granata V, Grassi R, Fusco R, Setola SV, Belli A, Piccirillo M, Pradella S, Giordano M, Cappabianca S, Brunese L, Grassi R, Petrillo A, Izzo F. Abbreviated MRI Protocol for the Assessment of Ablated Area in HCC Patients.Int J Environ Res Public Health. 2021 Mar30;18(7):3598. doi: https://doi.org/10.3390/ijerph18073598.
Petrillo A, Fusco R, Granata V, Filice S, Sansone M, Rega D, Delrio P, Bianco F, Romano GM, Tatangelo F, Avallone A, Pecori B. Assessing response to neo-adjuvant therapy in locally advanced rectal cancer using Intra-voxel Incoherent Motion modelling by DWI data and Standardized Index of Shape from DCE-MRI.Ther Adv Med Oncol. 2018 Nov16;10:1758835918809875. doi: https://doi.org/10.1177/1758835918809875.
Fusco R, Sansone M, Granata V, Grimm R, Pace U, Delrio P, Tatangelo F, Botti G, Avallone A, Pecori B, Petrillo A. Diffusion and perfusion MR parameters to assess preoperative short-course radiotherapy response in locally advanced rectal cancer: a comparative explorative study among Standardized Index of Shape by DCE-MRI, intravoxel incoherent motion- and diffusion kurtosis imaging-derived parameters. Abdom Radiol (NY). 2019 Nov;44(11):3683–3700. doi: https://doi.org/10.1007/s00261-018-1801-z.
Scola E, Desideri I, Bianchi A, Gadda D, Busto G, Fiorenza A, Amadori T, Mancini S, Miele V, Fainardi E. Assessment of brain tumors by magnetic resonance dynamic susceptibility contrast perfusion-weighted imaging and computed tomography perfusion: a comparison study. Radiol Med. 2022 Jun;127(6):664–72. https://doi.org/10.1007/s11547-022-01470-z.
Vicini S, Bortolotto C, Rengo M, Ballerini D, Bellini D, Carbone I, Preda L, Laghi A, Coppola F, Faggioni L. A narrative review on current imaging applications of artificial intelligence and radiomics in oncology: focus on the three most common cancers. Radiol Med. 2022 Aug;127(8):819–36. https://doi.org/10.1007/s11547-022-01512-6.
Petrillo A, Fusco R, Petrillo M, Granata V, Delrio P, Bianco F, Pecori B, Botti G, Tatangelo F, Caracò C, Aloj L, Avallone A, Lastoria S. Standardized Index of Shape (DCE-MRI) and Standardized Uptake Value (PET/CT): Two quantitative approaches to discriminate chemo-radiotherapy locally advanced rectal cancer responders under a functional profile.Oncotarget. 2017 Jan31;8(5):8143–8153. doi: https://doi.org/10.18632/oncotarget.14106.
Liu P, Zhu H, Zhu H, Zhang X, Feng A, Zhu X, Sun Y. Predicting Survival for Hepatic Arterial Infusion Chemotherapy of Unresectable Colorectal Liver Metastases: Radiomics Analysis of Pretreatment Computed Tomography. J Transl Int Med. 2022 Apr 2;10(1):56–64. doi: https://doi.org/10.2478/jtim-2022-0004.
Rahmim A, Bak-Fredslund KP, Ashrafinia S, Lu L, Schmidtlein CR, Subramaniam RM, Morsing A, Keiding S, Horsager J, Munk OL. Prognostic modeling for patients with colorectal liver metastases incorporating FDG PET radiomic features. Eur J Radiol. 2019 Apr;113:101–9. https://doi.org/10.1016/j.ejrad.2019.02.006.
De Robertis R, Geraci L, Tomaiuolo L, Bortoli L, Beleù A, Malleo G, D’Onofrio M. Liver metastases in pancreatic ductal adenocarcinoma: a predictive model based on CT texture analysis. Radiol Med. 2022 Sep;4. https://doi.org/10.1007/s11547-022-01548-8.
McHugh DJ, Porta N, Little RA, Cheung S, Watson Y, Parker GJM, Jayson GC, O’Connor JPB. Image Contrast, Image Pre-Processing, and T1 Mapping Affect MRI Radiomic Feature Repeatability in Patients with Colorectal Cancer Liver Metastases. Cancers (Basel). 2021 Jan 11;13(2):240. doi: https://doi.org/10.3390/cancers13020240.
Granata V, Grassi R, Fusco R, Setola SV, Palaia R, Belli A, Miele V, Brunese L, Grassi R, Petrillo A, Izzo F. Assessment of Ablation Therapy in Pancreatic Cancer: The Radiologist’s Challenge.Front Oncol. 2020 Nov27;10:560952. doi: https://doi.org/10.3389/fonc.2020.560952.
Chiti G, Grazzini G, Cozzi D, Danti G, Matteuzzi B, Granata V, Pradella S, Recchia L, Brunese L, Miele V. Imaging of Pancreatic Neuroendocrine Neoplasms.Int J Environ Res Public Health. 2021 Aug24;18(17):8895. doi: https://doi.org/10.3390/ijerph18178895.
Li Y, Gong J, Shen X, Li M, Zhang H, Feng F, Tong T. Assessment of Primary Colorectal Cancer CT Radiomics to Predict Metachronous Liver Metastasis.Front Oncol. 2022 Feb28;12:861892. doi: https://doi.org/10.3389/fonc.2022.861892.
Margonis GA, Vauthey JN. Precision surgery for colorectal liver metastases: Current knowledge and future perspectives.Ann Gastroenterol Surg. 2022 Jun27;6(5):606–615. doi: https://doi.org/10.1002/ags3.12591.
Vauthey JN, Zimmitti G, Kopetz SE, Shindoh J, Chen SS, Andreou A, et al. Ras mutation status predicts survival and patterns of recurrence in patients undergoing hepatectomy for colorectal liver metastases. Ann Surg. 2013;258(4):619–26. discussion 26 – 7.
Margonis GA, Sasaki K, Gholami S, Kim Y, Andreatos N, Rezaee N, et al. Genetic and morphological evaluation (game) score for patients with colorectal liver metastases. Br J Surg. 2018;105(9):1210–20.
Brudvik KW, Jones RP, Giuliante F, Shindoh J, Passot G, Chung MH, et al. Ras mutation clinical risk score to predict survival after resec- tion of colorectal liver metastases. Ann Surg. 2019;269(1):120–6.
Denbo JW, Yamashita S, Passot G, Egger M, Chun YS, Kopetz SE, et al. Ras mutation is associated with decreased survival in patients undergoing repeat hepatectomy for colorectal liver metastases. J Gastrointest Surg. 2017;21(1):68–77.
Douillard JY, Oliner KS, Siena S, Tabernero J, Burkes R, Barugel M, et al. Panitumumab-FOLFOX4 treatment and RAS mutations in Colorectal Cancer. N Engl J Med. 2013;369(11):1023–34. https://doi.org/10.1056/NEJMoa1305275.
Van Cutsem E, Lenz HJ, Kohne CH, Heinemann V, Tejpar S, Melezinek I, et al. Fluorouracil, Leucovorin, and Irinotecan Plus Cetuximab treatment and RAS mutations in Colorectal Cancer. J Clin Oncol. 2015;33(7):692–700. https://doi.org/10.1200/JCO.2014.59.4812.
Venook AP, Niedzwiecki D, Lenz HJ, Innocenti F, Fruth B, Meyerhardt JA, et al. Effect of First-Line Chemotherapy Combined with Cetuximab or Bevacizumab on overall survival in patients with KRAS Wild-Type Advanced or metastatic colorectal Cancer: a Randomized Clinical Trial. JAMA. 2017;317(23):2392–401. https://doi.org/10.1001/jama.2017.7105.
Lambin P, Rios-Velazquez E, Leijenaar R, Carv- alho S, van Stiphout RG, Granton P, Zegers CM, Gillies R, Boellard R, Dekker A, Aerts HJ. Radiomics: extracting more information from medical images using advanced feature analysis. Eur J Cancer. 2012;48:441–6.
Gebauer L, Moltz JH, Mühlberg A, Holch JW, Huber T, Enke J, Jäger N, Haas M, Kruger S, Boeck S, Sühling M, Katzmann A, Hahn H, Kunz WG, Heinemann V, Nörenberg D, Maurus S. Quantitative Imaging Biomarkers of the Whole Liver Tumor Burden Improve Survival Prediction in Metastatic Pancreatic Cancer. Cancers (Basel). 2021 Nov 16;13(22):5732. doi: https://doi.org/10.3390/cancers13225732.
Hesketh RL, Zhu AX, Oklu R. Radiomics and circulating tumor cells: personalized care in hepatocellular carcinoma? Diagn Interv Radiol. 2015 Jan-Feb;21(1):78–84. doi: https://doi.org/10.5152/dir.2014.14237.
Reimer RP, Reimer P, Mahnken AH. Assessment of Therapy Response to Transarterial Radioembolization for Liver Metastases by Means of Post-treatment MRI-Based Texture Analysis. Cardiovasc Intervent Radiol. 2018 Oct;41(10):1545–1556. doi: https://doi.org/10.1007/s00270-018-2004-2.
Rompianesi G, Pegoraro F, Ceresa CD, Montalti R, Troisi RI. Artificial intelligence in the diagnosis and management of colorectal cancer liver metastases. World J Gastroenterol. 2022 Jan;7(1):108–22. https://doi.org/10.3748/wjg.v28.i1.108.
Rabe E, Cioni D, Baglietto L, Fornili M, Gabelloni M, Neri E. Can the computed tomography texture analysis of colorectal liver metastases predict the response to first-line cytotoxic chemotherapy?World J Hepatol. 2022 Jan27;14(1):244–259. doi: https://doi.org/10.4254/wjh.v14.i1.244.
Euler A, Laqua FC, Cester D, Lohaus N, Sartoretti T, Pinto Dos Santos D, Alkadhi H, Baessler B. Virtual Monoenergetic Images of Dual-Energy CT-Impact on Repeatability, Reproducibility, and Classification in Radiomics. Cancers (Basel). 2021 Sep 20;13(18):4710. doi: https://doi.org/10.3390/cancers13184710.
Kim N, Lee ES, Won SE, Yang M, Lee AJ, Shin Y, Ko Y, Pyo J, Park HJ, Kim KW. Evolution of Radiological Treatment Response assessments for Cancer Immunotherapy: from iRECIST to Radiomics and Artificial Intelligence. Korean J Radiol. 2022 Sep;5. https://doi.org/10.3348/kjr.2022.0225.
Ter Maat LS, van Duin IAJ, Elias SG, van Diest PJ, Pluim JPW, Verhoeff JJC, de Jong PA, Leiner T, Veta M, Suijkerbuijk KPM. Imaging to predict checkpoint inhibitor outcomes in cancer. A systematic review.Eur J Cancer. 2022 Sep9;175:60–76. doi: https://doi.org/10.1016/j.ejca.2022.07.034.
Granata V, Petrillo M, Fusco R, Setola SV, de Lutio di Castelguidone E, Catalano O, Piccirillo M, Albino V, Izzo F, Petrillo A. Surveillance of HCC Patients after Liver RFA: Role of MRI with Hepatospecific Contrast versus Three-Phase CT Scan-Experience of High Volume Oncologic Institute. Gastroenterol Res Pract. 2013;2013:469097. doi: https://doi.org/10.1155/2013/469097. Epub 2013 Nov 12. PMID: 24324487; PMCID: PMC3845503.
Devoto L, Ganeshan B, Keller D, Groves A, Endozo R, Arulampalam T, Chand M. Using texture analysis in the development of a potential radiomic signature for early identification of hepatic metastasis in colorectal cancer.Eur J Radiol Open. 2022 Mar21;9:100415. doi: https://doi.org/10.1016/j.ejro.2022.100415.
Kelahan LC, Kim D, Soliman M, Avery RJ, Savas H, Agrawal R, Magnetta M, Liu BP, Velichko YS. Role of hepatic metastatic lesion size on inter-reader reproducibility of CT-based radiomics features. Eur Radiol. 2022 Jun;32(6):4025–33. https://doi.org/10.1007/s00330-021-08526-0.
Bracco S, Zanoni M, Casseri T, Castellano D, Cioni S, Vallone IM, Gennari P, Mazzei MA, Romano DG, Piano M, Comelli C, Tassi R, Ciceri EFM. Endovascular treatment of acute ischemic stroke due to tandem lesions of the anterior cerebral circulation: a multicentric italian observational study. Radiol Med. 2021 Jun;126(6):804–17. https://doi.org/10.1007/s11547-020-01331-7.
Gurgitano M, Angileri SA, Rodà GM, Liguori A, Pandolfi M, Ierardi AM, Wood BJ, Carrafiello G. Interventional Radiology ex-machina: impact of Artificial Intelligence on practice. Radiol Med. 2021 Jul;126(7):998–1006. https://doi.org/10.1007/s11547-021-01351-x.
Sudhir Pillai P, Hsieh S, Holmes D, Carter R, Fletcher JG, McCollough C. Individualized and Generalized Learner Models for Predicting Missed Hepatic Metastases.Proc SPIE Int Soc Opt Eng. 2022 Feb-Mar;12035:120350 C. doi: https://doi.org/10.1117/12.2612745.
Dohan A, Gallix B, Guiu B, Le Malicot K, Reinhold C, Soyer P, Bennouna J, Ghiringhelli F, Barbier E, Boige V, Taieb J, Bouché O, François E, Phelip JM, Borel C, Faroux R, Seitz JF, Jacquot S, Ben Abdelghani M, Khemissa-Akouz F, Genet D, Jouve JL, Rinaldi Y, Desseigne F, Texereau P, Suc E, Lepage C, Aparicio T, Hoeffel C. PRODIGE 9 investigators and PRODIGE 20 investigators. Early evaluation using a radiomic signature of unresectable hepatic metastases to predict outcome in patients with colorectal cancer treated with FOLFIRI and bevacizumab. Gut. 2020 Mar;69(3):531–9. https://doi.org/10.1136/gutjnl-2018-316407.
Giurazza F, Contegiacomo A, Calandri M, Mosconi C, Modestino F, Corvino F, Scrofani AR, Marra P, Coniglio G, Failla G, Lucarelli N, Femia M, Semeraro V, Ierardi AM. IVC filter retrieval: a multicenter proposal of two score systems to predict application of complex technique and procedural outcome. Radiol Med. 2021 Jul;126(7):1007–16. https://doi.org/10.1007/s11547-021-01356-6.
Nishino M, Hatabu H, Hodi FS. Imaging of Cancer Immunotherapy: current approaches and future directions. Radiology. 2019 Jan;290(1):9–22. https://doi.org/10.1148/radiol.2018181349.
Oyama A, Hiraoka Y, Obayashi I, Saikawa Y, Furui S, Shiraishi K, Kumagai S, Hayashi T, Kotoku J. Hepatic tumor classification using texture and topology analysis of non-contrast-enhanced three-dimensional T1-weighted MR images with a radiomics approach. Sci Rep. 2019 Jun 19;9(1):8764. doi: https://doi.org/10.1038/s41598-019-45283-z.
Zhao X, Liang P, Yong L, Jia Y, Gao J. Radiomics Study for Differentiating Focal Hepatic Lesions Based on Unenhanced CT Images.Front Oncol. 2022 Apr27;12:650797. doi: https://doi.org/10.3389/fonc.2022.650797.
Michallek F, Genske U, Niehues SM, Hamm B, Jahnke P. Deep learning reconstruction improves radiomics feature stability and discriminative power in abdominal CT imaging: a phantom study.Eur Radiol. 2022 Jul;32(7):4587–4595. doi: https://doi.org/10.1007/s00330-022-08592-y.
Min L, Hodi FS, Giobbie-Hurder A, et al. Systemic high-dose corticosteroid treatment does not improve the outcome of ipilimumab-related hypophysitis: a retrospective cohort study. Clin Cancer Res. 2015;21(4):749–55.
Barile A. Some thoughts and greetings from the new Editor-in-Chief. Radiol Med. 2021 Jan;126(1):3–4. doi: https://doi.org/10.1007/s11547-020-01324-6. Erratum in: Radiol Med. 2021 Oct;126(10):1377.
Cappabianca S, Granata V, Di Grezia G, Mandato Y, Reginelli A, Di Mizio V, Grassi R, Rotondo A. The role of nasoenteric intubation in the MR study of patients with Crohn’s disease: our experience and literature review. Radiol Med. 2011 Apr;116(3):389–406. https://doi.org/10.1007/s11547-010-0605-1. English, Italian.
De Filippo M, Puglisi S, D’Amuri F, Gentili F, Paladini I, Carrafiello G, Maestroni U, Del Rio P, Ziglioli F, Pagnini F. CT-guided percutaneous drainage of abdominopelvic collections: a pictorial essay. Radiol Med. 2021 Dec;126(12):1561–70. https://doi.org/10.1007/s11547-021-01406-z.
De Felice F, Boldrini L, Greco C, Nardone V, Salvestrini V, Desideri I. ESTRO vision 2030: the young Italian Association of Radiotherapy and Clinical Oncology (yAIRO) commitment statement. Radiol Med. 2021 Oct;126(10):1374–6. https://doi.org/10.1007/s11547-021-01398-w.
Pecoraro M, Cipollari S, Marchitelli L, Messina E, Del Monte M, Galea N, Ciardi MR, Francone M, Catalano C, Panebianco V. Cross-sectional analysis of follow-up chest MRI and chest CT scans in patients previously affected by COVID-19. Radiol Med. 2021 Oct;126(10):1273–81. https://doi.org/10.1007/s11547-021-01390-4.
Gabelloni M, Faggioni L, Cioni D, Mendola V, Falaschi Z, Coppola S, Corradi F, Isirdi A, Brandi N, Coppola F, et al. Extracorporeal membrane oxygenation (ECMO) in COVID-19 patients: a pocket guide for radiologists. Radiol Med. 2022;13:369–82.
Mayerhoefer ME, Materka A, Langs G, Häggström I, Szczypiński P, Gibbs P, Cook G. Introduction to Radiomics. J Nucl Med. 2020 Apr;61(4):488–95. https://doi.org/10.2967/jnumed.118.222893.
Petralia G, Zugni F, Summers PE, Colombo A, Pricolo P, Grazioli L, Colagrande S, Giovagnoni A, Padhani AR, Italian Working Group on Magnetic Resonance. Whole-body magnetic resonance imaging (WB-MRI) for cancer screening: recommendations for use. Radiol Med. 2021 Nov;126(11):1434–50. https://doi.org/10.1007/s11547-021-01392-2.
Assadsangabi R, Babaei R, Songco C, Ivanovic V, Bobinski M, Chen YJ, Nabavizadeh SA. Multimodality oncologic evaluation of superficial neck and facial lymph nodes. Radiol Med. 2021 Aug;126(8):1074–84. https://doi.org/10.1007/s11547-021-01367-3.
Scapicchio C, Gabelloni M, Barucci A, Cioni D, Saba L, Neri E. A deep look into radiomics. Radiol Med. 2021 Oct;126(10):1296–311. https://doi.org/10.1007/s11547-021-01389-x.
Morin O, Vallières M, Jochems A, Woodruff HC, Valdes G, Braunstein SE, Wildberger JE, Villanueva-Meyer JE, Kearney V, Yom SS, Solberg TD, Lambin P. A Deep Look Into the Future of Quantitative Imaging in Oncology: A Statement of Working Principles and Proposal for Change.Int J Radiat Oncol Biol Phys. 2018 Nov15;102(4):1074–1082. doi: https://doi.org/10.1016/j.ijrobp.2018.08.032.
Cellina M, Pirovano M, Ciocca M, Gibelli D, Floridi C, Oliva G. Radiomic analysis of the optic nerve at the first episode of acute optic neuritis: an indicator of optic nerve pathology and a predictor of visual recovery? Radiol Med. 2021 May;126(5):698–706. doi: https://doi.org/10.1007/s11547-020-01318-4.
Santone A, Brunese MC, Donnarumma F, Guerriero P, Mercaldo F, Reginelli A, Miele V, Giovagnoni A, Brunese L. Radiomic features for prostate cancer grade detection through formal verification. Radiol Med. 2021 May;126(5):688–97. https://doi.org/10.1007/s11547-020-01314-8.
Agazzi GM, Ravanelli M, Roca E, Medicina D, Balzarini P, Pessina C, Vermi W, Berruti A, Maroldi R, Farina D. CT texture analysis for prediction of EGFR mutational status and ALK rearrangement in patients with non-small cell lung cancer. Radiol Med. 2021 Jun;126(6):786–94. https://doi.org/10.1007/s11547-020-01323-7.
Benedetti G, Mori M, Panzeri MM, Barbera M, Palumbo D, Sini C, Muffatti F, Andreasi V, Steidler S, Doglioni C, Partelli S, Manzoni M, Falconi M, Fiorino C, De Cobelli F. CT-derived radiomic features to discriminate histologic characteristics of pancreatic neuroendocrine tumors. Radiol Med. 2021 Jun;126(6):745–60. https://doi.org/10.1007/s11547-021-01333-z.
Failla G, Libra F, Giurazza F, Lucarelli NM, Coniglio G, Vacirca F, Santonocito SM, Dell’Atti C, Camerano F, Palmucci S, Niola R, Basile A, Patanè D. Endovascular treatment of cesarean scar pregnancy: a retrospective multicentric study. Radiol Med. 2022 Sep;27. https://doi.org/10.1007/s11547-022-01536-y.
Kim SJ, Pak K, Kim K. Diagnostic perfor- mance of F-18 FDG PET/CT for prediction of KRAS mutation in colorectal cancer patients: a systematic review and meta-analysis. Abdom Radiol (NY). 2019;44:1703–11.
Lovinfosse P, Koopmansch B, Lambert F, Jodo- gne S, Kustermans G, Hatt M, Visvikis D, Seidel L, Polus M, Albert A, Delvenne P, Hustinx R. (18)F-FDG PET/CT imaging in rectal cancer: re- lationship with the RAS mutational status. Br J Radiol. 2016;89:20160212.
Zhang Z, Shen L, Wang Y, Wang J, Zhang H, Xia F, Wan J, Zhang Z. MRI Radiomics Signature as a Potential Biomarker for Predicting KRAS Status in Locally Advanced Rectal Cancer Patients.Front Oncol. 2021 May7;11:614052. doi: https://doi.org/10.3389/fonc.2021.614052.
Granata V, Fusco R, Risi C, Ottaiano A, Avallone A, De Stefano A, Grimm R, Grassi R, Brunese L, Izzo F, Petrillo A. Diffusion-Weighted MRI and Diffusion Kurtosis Imaging to Detect RAS Mutation in Colorectal Liver Metastasis. Cancers (Basel). 2020 Aug 26;12(9):2420. doi: https://doi.org/10.3390/cancers12092420.
Yang L, Dong D, Fang M, Zhu Y, Zang Y, Liu Z, et al. Can Ct-Based Radiomics signature predict Kras/Nras/Braf mutations in Colorectal Cancer? Eur Radiol. 2018;28:2058–67. https://doi.org/10.1007/s00330-017-5146-8.
Lubner MG, Stabo N, Lubner SJ, del Rio AM, Song C, Halberg RB, et al. Ct textural analysis of hepatic metastatic colorectal Cancer: Pre-Treatment Tumor Heterogeneity correlates with Pathology and Clinical Outcomes. Abdom Imaging. 2015;40:2331–7. https://doi.org/10.1007/s00261-015-0438-4.
Shi R, Chen W, Yang B, Qu J, Cheng Y, Zhu Z, Gao Y, Wang Q, Liu Y, Li Z, Qu X. Prediction of KRAS, NRAS and BRAF status in colorectal cancer patients with liver metastasis using a deep artificial neural network based on radiomics and semantic features. Am J Cancer Res. 2020 Dec 1;10(12):4513–4526.
Granata V, Fusco R, Avallone A, De Stefano A, Ottaiano A, Sbordone C, Brunese L, Izzo F, Petrillo A. Radiomics-Derived Data by Contrast Enhanced Magnetic Resonance in RAS Mutations Detection in Colorectal Liver Metastases. Cancers (Basel). 2021 Jan 25;13(3):453. doi: https://doi.org/10.3390/cancers13030453.
Liang M, Cai Z, Zhang H, Huang C, Meng Y, Zhao L, Li D, Ma X, Zhao X. Machine learning-based analysis of rectal Cancer MRI Radiomics for Prediction of Metachronous Liver Metastasis. Acad Radiol. 2019 Nov;26(11):1495–504. https://doi.org/10.1016/j.acra.2018.12.019.
Shur J, Orton M, Connor A, Fischer S, Moulton CA, Gallinger S, Koh DM, Jhaveri KS. A clinical-radiomic model for improved prognostication of surgical candidates with colorectal liver metastases. J Surg Oncol. 2019 Dec;3. https://doi.org/10.1002/jso.25783.
Li Wen Y, Leech M. Review of the Role of Radiomics in Tumour Risk Classification and Prognosis of Cancer.Anticancer Res. 2020Jul;40(7):3605–3618. doi: https://doi.org/10.21873/anticanres.14350.
D’Agostino V, Caranci F, Negro A, Piscitelli V, Tuccillo B, Fasano F. Sirabella,G.;Marano,I.;Granata,V.;Grassi,R.;etal.A Rare Case of cerebral venous thrombosis and disseminated intravascular coagulation temporally Associated to the COVID-19 Vaccine Administration. J Pers Med. 2021;11:285.
Agostini A, Borgheresi A, Carotti M, Ottaviani L, Badaloni M, Floridi C, Giovagnoni A. Third-generation iterative reconstruction on a dual-source, high-pitch, low-dose chest CT protocol with tin filter for spectral shaping at 100 kV: a study on a small series of COVID-19 patients. Radiol Med. 2021;126:388–98.
Palmisano A, Scotti GM, Ippolito D, Morelli MJ, Vignale D, Gandola D, Sironi S, De Cobelli F, Ferrante L, Spessot M, et al. Chest CT in the emergency department for suspected COVID-19 pneumonia. Radiol Med. 2021;126:498–502.
Lombardi AF, Afsahi AM, Gupta A, Gholamrezanezhad A. Severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), influenza, and COVID-19, beyond the lungs: a review article. Radiol Med. 2021;126:561–9.
Grassi R, Cappabianca S, Urraro F, Feragalli B, Montanelli A, Patelli G, Granata V, Giacobbe G, Russo GM, Grillo A, et al. Chest CT computerized aided quantification of PNEUMONIA lesions in COVID-19 infection: a comparison among three Commercial Software. Int J Environ Res Public Health. 2020;17:6914.
Fusco R, Grassi R, Granata V, Setola SV, Grassi F, Cozzi D, Pecori B, Izzo F, Petrillo A. Artificial Intelligence and COVID-19 using chest CT scan and chest X-ray images: machine learning and deep learning approaches for diagnosis and treatment. J Pers Med. 2021;11:993.
Özel M, Aslan A, Araç S. Use of the COVID-19 Reporting and Data System (CO-RADS) classification and chest computed tomography involvement score (CT-IS) in COVID-19 pneumonia. Radiol Med. 2021;126:679–87.
Ippolito D, Giandola T, Maino C, Pecorelli A, Capodaglio C, Ragusi M, Porta M, Gandola D, Masetto A, Drago S, et al. Acute pulmonary embolism in hospitalized patients with SARS-CoV-2-related pneumonia: multicentric experience from italian endemic area. Radiol Med. 2021;126:669–78.
Moroni C, Cozzi D, Albanesi M, Cavigli E, Bindi A, Luvarà S, Busoni S, Mazzoni LN, Grifoni S, Nazerian P, et al. Chest X-ray in the emergency department during COVID-19 pandemic descending phase in Italy: correlation with patients’ outcome. Radiol Med. 2021;126:661–8.
Cereser L, Girometti R, Da Re J, Marchesini F, Como G, Zuiani C. Inter-reader agreement of high-resolution computed tomography findings in patients with COVID-19 pneumonia: a multi-reader study. Radiol Med. 2021;126:577–84.
Rawashdeh MA, Saade C. Radiation dose reduction considerations and imaging patterns of ground glass opacities in coronavirus: risk of over exposure in computed tomography. Radiol Med. 2021;126:380–7.
Granata V, Ianniello S, Fusco R, Urraro F, Pupo D, Magliocchetti S, Albarello F, Campioni P, Cristofaro M, Di Stefano F, et al. Quantitative analysis of residual COVID-19 lung CT features: consistency among two Commercial Software. J Pers Med. 2021;11:1103.
Granata V, Fusco R, Bicchierai G, Cozzi D, Grazzini G, Danti G, De Muzio F, Maggialetti N, Smorchkova O, D’Elia M, et al. Diagnostic protocols in oncology: workup and treatment planning: part 1: the optimitation of CT protocol. Eur Rev Med Pharmacol Sci. 2021;25:6972–94.
Fusco R, Granata V, Petrillo A. Introduction to Special Issue of Radiology and Imaging of Cancer. Cancers (Basel). 2020 Sep 18;12(9):2665. doi: https://doi.org/10.3390/cancers12092665.
Cai D, Duan X, Wang W, Huang ZP, Zhu Q, Zhong ME, Lv MY, Li CH, Kou WB, Wu XJ, Gao F. A Metabolism-Related Radiomics Signature for Predicting the Prognosis of Colorectal Cancer.Front Mol Biosci. 2021 Jan7;7:613918. doi: https://doi.org/10.3389/fmolb.2020.613918.
Granata V, Grassi R, Fusco R, Galdiero R, Setola SV, Palaia R, Belli A, Silvestro L, Cozzi D, Brunese L, Petrillo A, Izzo F. Pancreatic cancer detection and characterization: state of the art and radiomics. Eur Rev Med Pharmacol Sci. 2021 May;25(10):3684–99. https://doi.org/10.26355/eurrev_202105_25935.
Nakamoto T, Haga A, Takahashi W. [An introduction to Radiomics: toward a new era of Precision Medicine]. Igaku Butsuri. 2018;38(3):129–34. https://doi.org/10.11323/jjmp.38.3_129. Japanese.
Vuong D, Tanadini-Lang S, Wu Z, Marks R, Unkelbach J, Hillinger S, Eboulet EI, Thierstein S, Peters S, Pless M, Guckenberger M, Bogowicz M. Radiomics Feature Activation Maps as a New Tool for Signature Interpretability.Front Oncol. 2020 Dec8;10:578895. doi: https://doi.org/10.3389/fonc.2020.578895.
Yip SS, Aerts HJ. Applications and limitations of radiomics. Phys Med Biol. 2016 Jul 7;61(13):R150-66. doi: https://doi.org/10.1088/0031-9155/61/13/R150.
Granata V, Bicchierai G, Fusco R, Cozzi D, Grazzini G, Danti G, De Muzio F, Maggialetti N, Smorchkova O, D’Elia M, Brunese MC, Grassi R, Giacobbe G, Bruno F, Palumbo P, Grassi F, Brunese L, Grassi R, Miele V, Barile A. Diagnostic protocols in oncology: workup and treatment planning. Part 2: abbreviated MR protocol. Eur Rev Med Pharmacol Sci. 2021 Nov;25(21):6499–528. https://doi.org/10.26355/eurrev_202111_27094.
Granata V, Fusco R, Catalano O, Setola SV, de Lutio di Castelguidone E, Piccirillo M, Palaia R, Grassi R, Granata F, Izzo F, Petrillo A. Multidetector computer tomography in the pancreatic adenocarcinoma assessment: an update.Infect Agent Cancer. 2016 Nov15;11:57.: 27891175; PMCID: PMC5111267.
Wilson R, Devaraj A. Radiomics of pulmonary nodules and lung cancer.Transl Lung Cancer Res. 2017Feb;6(1):86–91. doi: https://doi.org/10.21037/tlcr.2017.01.04.
Binczyk F, Prazuch W, Bozek P, Polanska J. Radiomics and artificial intelligence in lung cancer screening. Transl Lung Cancer Res. 2021 Feb;10(2):1186–99. https://doi.org/10.21037/tlcr-20-708.
Beig N, Bera K, Tiwari P. Introduction to radiomics and radiogenomics in neuro-oncology: implications and challenges. Neurooncol Adv. 2021 Jan 23;2(Suppl 4):iv3-iv14. doi: https://doi.org/10.1093/noajnl/vdaa148.
Salaffi F, Carotti M, Di Matteo A, Ceccarelli L, Farah S, Villota-Eraso C, Di Carlo M, Giovagnoni A. Ultrasound and magnetic resonance imaging as diagnostic tools for sarcopenia in immune-mediated rheumatic diseases (IMRDs). Radiol Med. 2022 Nov;127(11):1277–91. https://doi.org/10.1007/s11547-022-01560-y.
Stefanini M, Simonetti G, Interventional Magnetic Resonance Imaging Suite (IMRIS). How to build and how to use. Radiol Med. 2022 Oct;127(10):1063–7. https://doi.org/10.1007/s11547-022-01537-x.
Chen Q, Zhang L, Liu S, You J, Chen L, Jin Z, Zhang S, Zhang B. Radiomics in precision medicine for gastric cancer: opportunities and challenges.Eur Radiol. 2022Sep;32(9):5852–5868. doi: https://doi.org/10.1007/s00330-022-08704-8.
Shi Z, Traverso A, van Soest J, Dekker A, Wee L. Technical note: ontology-guided radiomics analysis workflow (O-RAW). Med Phys. 2019 Dec;46(12):5677–84. https://doi.org/10.1002/mp.13844.
Boland CR, Goel A. Microsatellite Instability in Colorectal Cancer. Gastroenterology (2010) 138:2073–2087 e2073. doi: https://doi.org/10.1053/j.gastro.2009.12.064 83.
Gupta R, Sinha S, Paul RN. The impact of microsatellite Stability Status in Colorectal Cancer. Curr Probl Cancer. 2018;42:548–59. 10.1016/ j.currproblcancer.2018.06.01084.
Cohen R, Pellat A, Boussion H, Svrcek M, Lopez-Trabada D, Trouilloud I, et al. Immunotherapy and metastatic colorectal cancers with microsatellite instability or Mismatch Repair Deficiency. Bull Cancer. 2019;106:137–42. https://doi.org/10.1016/j.bulcan.2018.09.004.
De’ Angelis GL, Bottarelli L, Azzoni C, De’ Angelis N, Leandro G, Di Mario F, Gaiani F, Negri F. Microsatellite instability in colorectal cancer.Acta Biomed. 2018 Dec17;89(9-S):97–101. doi: https://doi.org/10.23750/abm.v89i9-S.7960.
Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, Skora AD, Luber BS, Azad NS, Laheru D, Biedrzycki B, Donehower RC, Zaheer A, Fisher GA, Crocenzi TS, Lee JJ, Duffy SM, Goldberg RM, de la Chapelle A, Koshiji M, Bhaijee F, Huebner T, Hruban RH, Wood LD, Cuka N, Pardoll DM, Papadopoulos N, Kinzler KW, Zhou S, Cornish TC, Taube JM, Anders RA, Eshleman JR, Vogelstein B, Diaz LA Jr. PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. N Engl J Med. 2015 Jun 25;372(26):2509-20. doi: https://doi.org/10.1056/NEJMoa1500596.
Chianca V, Albano D, Messina C, Vincenzo G, Rizzo S, Del Grande F, Sconfienza LM. An update in musculoskeletal tumors: from quantitative imaging to radiomics. Radiol Med. 2021 Aug;126(8):1095–105. https://doi.org/10.1007/s11547-021-01368-2.
Halefoglu AM, Ozagari AA. Tumor grade estımatıon of clear cell and papıllary renal cell carcınomas usıng contrast-enhanced MDCT and FSE T2 weıghted MR ımagıng: radıology-pathology correlatıon. Radiol Med. 2021 Sep;126(9):1139–48. https://doi.org/10.1007/s11547-021-01350-y.
Granata V, Fusco R, Setola SV, Simonetti I, Cozzi D, Grazzini G, Grassi F, Belli A, Miele V, Izzo F, Petrillo A. An update on radiomics techniques in primary liver cancers.Infect Agent Cancer. 2022 Mar4;17(1):6. doi: https://doi.org/10.1186/s13027-022-00422-6.
Chen J, Zhang C, Traverso A, Zhovannik I, Dekker A, Wee L, Bermejo I. Generative models improve radiomics reproducibility in low dose CTs: a simulation study. Phys Med Biol. 2021 Aug 3;66(16). doi: https://doi.org/10.1088/1361-6560/ac16c0.
Shiri I, Rahmim A, Ghaffarian P, Geramifar P, Abdollahi H, Bitarafan-Rajabi A. The impact of image reconstruction settings on 18F-FDG PET radiomic features: multi-scanner phantom and patient studies.Eur Radiol. 2017Nov;27(11):4498–4509. doi: https://doi.org/10.1007/s00330-017-4859-z.
Granata V, Fusco R, Sansone M, Grassi R, Maio F, Palaia R, Tatangelo F, Botti G, Grimm R, Curley S, Avallone A, Izzo F, Petrillo A. Magnetic resonance imaging in the assessment of pancreatic cancer with quantitative parameter extraction by means of dynamic contrast-enhanced magnetic resonance imaging, diffusion kurtosis imaging and intravoxel incoherent motion diffusion-weighted imaging. Therap Adv Gastroenterol. 2020 May 21;13:1756284819885052. doi: https://doi.org/10.1177/1756284819885052.
Granata V, Fusco R, Setola SV, Picone C, Vallone P, Belli A, Incollingo P, Albino V, Tatangelo F, Izzo F, Petrillo A. Microvascular invasion and grading in hepatocellular carcinoma: correlation with major and ancillary features according to LIRADS. Abdom Radiol (NY). 2019 Aug;44(8):2788–2800. doi: https://doi.org/10.1007/s00261-019-02056-6.
Wu J, Zhang Q, Zhao Y, Liu Y, Chen A, Li X, et al. Radiomics Analysis of Iodine-Based material decomposition images with dual-energy computed Tomography Imaging for Preoperatively Predicting microsatellite instability status in Colorectal Cancer. Front Oncol. 2019;9:1250. 10.3389/ fonc.2019.01250.
Golia Pernicka JS, Gagniere J, Chakraborty J, Yamashita R, Nardo L, Creasy JM, et al. Radiomics-Based prediction of microsatellite instability in Colorectal Cancer at initial computed tomography evaluation. Abdom Radiol (NY). 2019;44:3755–63. https://doi.org/10.1007/s00261-019-02117-w.
Fan S, Li X, Cui X, Zheng L, Ren X, Ma W, et al. Computed tomography- based Radiomic features could potentially predict microsatellite instability status in stage II colorectal Cancer: a preliminary study. Acad Radiol. 2019;26:1633–40. https://doi.org/10.1016/j.acra.2019.02.009.
Wu J, Lv Y, Wang N, Zhao Y, Zhang P, Liu Y, Chen A, Li J, Li X, Guo Y, et al. The value of single-source dual-energy CT imaging for discriminating microsatellite instability from microsatellite stability human colorectal cancer. Eur Radiol. 2019;29:3782–90.
Damilakis E, Mavroudis D, Sfakianaki M, Souglakos J. Immunotherapy in Metastatic Colorectal Cancer: Could the Latest Developments Hold the Key to Improving Patient Survival? Cancers (Basel). 2020 Apr 6;12(4):889. doi: https://doi.org/10.3390/cancers12040889.
Neri E, Granata V, Montemezzi S, Belli P, Bernardi D, Brancato B, Caumo F, Calabrese M, Coppola F, Cossu E, Faggioni L, Frigerio A, Fusco R, Petrillo A, Girardi V, Iacconi C, Marini C, Marino MA, Martincich L, Nori J, Pediconi F, Saguatti G, Sansone M, Sardanelli F, Scaperrotta GP, Zuiani C, Ciaghi E, Montella M, Miele V, Grassi R. Structured reporting of x-ray mammography in the first diagnosis of breast cancer: a Delphi consensus proposal. Radiol Med. 2022 May;127(5):471–83. https://doi.org/10.1007/s11547-022-01478-5.
Sun J, Li H, Gao J, Li J, Li M, Zhou Z, Peng Y. Performance evaluation of a deep learning image reconstruction (DLIR) algorithm in “double low” chest CTA in children: a feasibility study. Radiol Med. 2021 Sep;126(9):1181–8. https://doi.org/10.1007/s11547-021-01384-2.
Granata V, Faggioni L, Grassi R, Fusco R, Reginelli A, Rega D, Maggialetti N, Buccicardi D, Frittoli B, Rengo M, Bortolotto C, Prost R, Lacasella GV, Montella M, Ciaghi E, Bellifemine F, De Muzio F, Grazzini G, De Filippo M, Cappabianca S, Laghi A, Grassi R, Brunese L, Neri E, Miele V, Coppola F. Structured reporting of computed tomography in the staging of colon cancer: a Delphi consensus proposal. Radiol Med. 2022 Jan;127(1):21–9. https://doi.org/10.1007/s11547-021-01418-9.
Reynolds IS, Furney SJ, Kay EW, McNamara DA, Prehn JHM, Burke JP. Meta-analysis of the molecular associations of mucinous colorectal cancer. Br J Surg. 2019;106:682–91.
Reynolds IS, O’Connell E, Fichtner M, McNamara DA, Kay EW, Prehn JHM, Furney SJ, Burke JP. Mucinous adenocarcinoma is a pharmacogenomically distinct subtype of colorectal cancer. Pharm J. 2020;20:524–32.
McCawley N, Clancy C, O’Neill BDP, Deasy J, McNamara DA, Burke JP. Mucinous rectal adenocarcinoma is Associated with a poor response to Neoadjuvant Chemoradiotherapy: a systematic review and Meta-analysis. Dis Colon Rectum. 2016;59:1200–8.
Granata V, Fusco R, Setola SV, De Muzio F, Dell’ Aversana F, Cutolo C, Faggioni L, Miele V, Izzo F, Petrillo A. CT-Based Radiomics Analysis to Predict Histopathological Outcomes Following Liver Resection in Colorectal Liver Metastases. Cancers (Basel). 2022 Mar 24;14(7):1648. doi: https://doi.org/10.3390/cancers14071648.
Granata V, Fusco R, De Muzio F, Cutolo C, Setola SV, Dell’Aversana F, Ottaiano A, Nasti G, Grassi R, Pilone V, Miele V, Brunese MC, Tatangelo F, Izzo F, Petrillo A. EOB-MR Based Radiomics Analysis to Assess Clinical Outcomes following Liver Resection in Colorectal Liver Metastases. Cancers (Basel). 2022 Feb 27;14(5):1239. doi: https://doi.org/10.3390/cancers14051239.
Granata V, Fusco R, De Muzio F, Cutolo C, Setola SV, Dell’ Aversana F, Ottaiano A, Avallone A, Nasti G, Grassi F, Pilone V, Miele V, Brunese L, Izzo F, Petrillo A. Contrast MR-Based Radiomics and Machine Learning Analysis to Assess Clinical Outcomes following Liver Resection in Colorectal Liver Metastases: A Preliminary Study. Cancers (Basel). 2022 Feb 22;14(5):1110. doi: https://doi.org/10.3390/cancers14051110.
van Dam PJ, van der Stok EP, Teuwen LA, Van den Eynden GG, Illemann M, Frentzas S, Majeed AW, Eefsen RL, van den Coebergh RRJ, Lazaris A, Fernandez MC, Galjart B, Laerum OD, Rayes R, Grünhagen DJ, Van de Paer M, Sucaet Y, Mudhar HS, Schvimer M, Nyström H, Kockx M, Bird NC, Vidal-Vanaclocha F, Metrakos P, Simoneau E, Verhoef C, Dirix LY, Van Laere S, Gao ZH, Brodt P, Reynolds AR, Vermeulen PB. International consensus guidelines for scoring the histopathological growth patterns of liver metastasis.Br J Cancer. 2017 Nov7;117(10):1427–1441. doi: https://doi.org/10.1038/bjc.2017.334.
Granata V, Fusco R, Avallone A, Filice F, Tatangelo F, Piccirillo M, Grassi R, Izzo F, Petrillo A. Critical analysis of the major and ancillary imaging features of LI-RADS on 127 proven HCCs evaluated with functional and morphological MRI: Lights and shadows. Oncotarget. 2017 Apr 19;8(31):51224–37. https://doi.org/10.18632/oncotarget.17227. PMID: 28881643; PMCID: PMC5584244.
Nielsen K, Rolff HC, Eefsen RL, Vainer B. The morphological growth patterns of colorectal liver metastases are prognostic for overall survival. Mod Pathol. 2014 Dec;27(12):1641–8. https://doi.org/10.1038/modpathol.2014.4.
Cheng J, Wei J, Tong T, Sheng W, Zhang Y, Han Y, Gu D, Hong N, Ye Y, Tian J, Wang Y. Prediction of histopathologic growth patterns of Colorectal Liver Metastases with a noninvasive imaging method. Ann Surg Oncol. 2019 Dec;26(13):4587–98. https://doi.org/10.1245/s10434-019-07910-x.
Fusco R, Sansone M, Granata V, Setola SV, Petrillo A. A systematic review on multiparametric MR imaging in prostate cancer detection. Infect Agent Cancer. 2017 Oct 30;12:57. https://doi.org/10.1186/s13027-017-0168-z. PMID: 29093748; PMCID: PMC5663098.
Qin H, Que Q, Lin P, Li X, Wang XR, He Y, Chen JQ, Yang H. Magnetic resonance imaging (MRI) radiomics of papillary thyroid cancer (PTC): a comparison of predictive performance of multiple classifiers modeling to identify cervical lymph node metastases before surgery. Radiol Med. 2021 Oct;126(10):1312–27. https://doi.org/10.1007/s11547-021-01393-1.
Fusco R, Di Bernardo E, Piccirillo A, Rubulotta MR, Petrosino T, Barretta ML, Mattace Raso M, Vallone P, Raiano C, Di Giacomo R, Siani C, Avino F, Scognamiglio G, Di Bonito M, Granata V, Petrillo A. Radiomic and Artificial Intelligence Analysis with Textural Metrics extracted by contrast-enhanced Mammography and Dynamic contrast magnetic resonance imaging to detect breast malignant lesions. Curr Oncol. 2022 Mar;13(3):1947–66. https://doi.org/10.3390/curroncol29030159.
Brunese L, Brunese MC, Carbone M, Ciccone V, Mercaldo F, Santone A. Automatic PI-RADS assignment by means of formal methods. Radiol Med. 2022 Jan;127(1):83–9. https://doi.org/10.1007/s11547-021-01431-y.
Bellardita L, Colciago RR, Frasca S, De Santis MC, Gay S, Palorini F, La Rocca E, Valdagni R, Rancati T, Lozza L. Breast cancer patient perspective on opportunities and challenges of a genetic test aimed to predict radio-induced side effects before treatment: analysis of the italian branch of the REQUITE project. Radiol Med. 2021 Oct;126(10):1366–73. https://doi.org/10.1007/s11547-021-01395-z.
Caruso D, Pucciarelli F, Zerunian M, Ganeshan B, De Santis D, Polici M, Rucci C, Polidori T, Guido G, Bracci B, Benvenga A, Barbato L, Laghi A. Chest CT texture-based radiomics analysis in differentiating COVID-19 from other interstitial pneumonia. Radiol Med. 2021 Nov;126(11):1415–24. https://doi.org/10.1007/s11547-021-01402-3.
Zhang L, Cai P, Hou J, Luo M, Li Y, Jiang X. Radiomics Model Based on Gadoxetic Acid Disodium-Enhanced MR Imaging to Predict Hepatocellular Carcinoma Recurrence After Curative Ablation.Cancer Manag Res. 2021 Mar25;13:2785–2796. doi: https://doi.org/10.2147/CMAR.S300627.
Wu M, Zhang Y, Zhang Y, Liu Y, Wu M, Ye Z. Imaging-based Biomarkers for Predicting and Evaluating Cancer Immunotherapy Response.Radiol Imaging Cancer. 2019 Nov29;1(2):e190031. doi: https://doi.org/10.1148/rycan.2019190031.
Sun R, Limkin EJ, Vakalopoulou M, et al. A radiomics approach to assess tumour-infiltrating CD8 cells and response to anti-PD-1 or anti-PD-L1 immunotherapy: an imaging biomarker, retrospective multicohort study. Lancet Oncol. 2018;19(9):1180–91.
Rega D, Pace U, Scala D, Chiodini P, Granata V, Fares Bucci A, Pecori B, Delrio P. Treatment of splenic flexure colon cancer: a comparison of three different surgical procedures: Experience of a high volume cancer center. Sci Rep. 2019 Jul 29;9(1):10953. https://doi.org/10.1038/s41598-019-47548-z. PMID: 31358904; PMCID: PMC6662908.
Tunali I, Tan Y, Gray JE, Katsoulakis E, Eschrich SA, Saller J, Aerts HJWL, Boyle T, Qi J, Guvenis A, Gillies RJ, Schabath MB. Hypoxia-Related Radiomics and Immunotherapy Response: A Multicohort Study of Non-Small Cell Lung Cancer. JNCI Cancer Spectr. 2021 May 13;5(4):pkab048. doi: https://doi.org/10.1093/jncics/pkab048.
Matsoukas S, Scaggiante J, Schuldt BR, Smith CJ, Chennareddy S, Kalagara R, Majidi S, Bederson JB, Fifi JT, Mocco J, Kellner CP. Accuracy of artificial intelligence for the detection of intracranial hemorrhage and chronic cerebral microbleeds: a systematic review and pooled analysis. Radiol Med. 2022 Aug;13. https://doi.org/10.1007/s11547-022-01530-4.
Karmazanovsky G, Gruzdev I, Tikhonova V, Kondratyev E, Revishvili A. Computed tomography-based radiomics approach in pancreatic tumors characterization. Radiol Med. 2021 Aug;12. https://doi.org/10.1007/s11547-021-01405-0.
Danti G, Flammia F, Matteuzzi B, Cozzi D, Berti V, Grazzini G, Pradella S, Recchia L, Brunese L, Miele V. Gastrointestinal neuroendocrine neoplasms (GI-NENs): hot topics in morphological, functional, and prognostic imaging. Radiol Med. 2021 Dec;126(12):1497–507. https://doi.org/10.1007/s11547-021-01408-x.
Satake H, Ishigaki S, Ito R, Naganawa S. Radiomics in breast MRI: current progress toward clinical application in the era of artificial intelligence. Radiol Med. 2022 Jan;127(1):39–56. https://doi.org/10.1007/s11547-021-01423-y.
Cozzi D, Bicci E, Cavigli E, Danti G, Bettarini S, Tortoli P, Mazzoni LN, Busoni S, Pradella S, Miele V. Radiomics in pulmonary neuroendocrine tumours (NETs). Radiol Med. 2022 Jun;127(6):609–15. https://doi.org/10.1007/s11547-022-01494-5.
Gregucci F, Fiorentino A, Mazzola R, Ricchetti F, Bonaparte I, Surgo A, Figlia V, Carbonara R, Caliandro M, Ciliberti MP, Ruggieri R, Alongi F. Radiomic analysis to predict local response in locally advanced pancreatic cancer treated with stereotactic body radiation therapy. Radiol Med. 2022 Jan;127(1):100–7. https://doi.org/10.1007/s11547-021-01422-z.
Granata V, Fusco R, De Muzio F, Cutolo C, Mattace Raso M, Gabelloni M, Avallone A, Ottaiano A, Tatangelo F, Brunese MC, Miele V, Izzo F, Petrillo A. Radiomics and Machine Learning Analysis Based on Magnetic Resonance Imaging in the Assessment of Colorectal Liver Metastases Growth Pattern. Diagnostics (Basel). 2022 Apr 29;12(5):1115. doi: https://doi.org/10.3390/diagnostics12051115.
Ji GW, Wang K, Xia YX, Li XC, Wang XH. [Application and challenge of radiomics technique in the era of precision medicine for hepatobiliary disease]. Zhonghua Wai Ke Za Zhi. 2020 Oct 1;58(10):749–753. Chinese. doi: https://doi.org/10.3760/cma.j.cn112139-20200605-00439.
Yip SS, Aerts HJ. Applications and limitations of radiomics. Phys Med Biol. 2016 Jul 7;61(13):R150-66. doi: https://doi.org/10.1088/0031-9155/61/13/R150.
Rizzo S, Botta F, Raimondi S, Origgi D, Fanciullo C, Morganti AG, Bellomi M. Radiomics: the facts and the challenges of image analysis.Eur Radiol Exp. 2018 Nov14;2(1):36. doi: https://doi.org/10.1186/s41747-018-0068-z.
Orlhac F, Nioche C, Klyuzhin I, Rahmim A, Buvat I. Radiomics in PET Imaging:: a practical guide for newcomers. PET Clin. 2021 Oct;16(4):597–612. https://doi.org/10.1016/j.cpet.2021.06.007.
Avanzo M, Stancanello J, El Naqa I. Beyond imaging: the promise of radiomics. Phys Med. 2017 Jun;38:122–39. https://doi.org/10.1016/j.ejmp.2017.05.071.
Da-Ano R, Visvikis D, Hatt M. Harmonization strategies for multicenter radiomics investigations. Phys Med Biol. 2020 Dec 17;65(24):24TR02. doi: https://doi.org/10.1088/1361-6560/aba798.
Bogowicz M, Vuong D, Huellner MW, Pavic M, Andratschke N, Gabrys HS, Guckenberger M, Tanadini-Lang S. CT radiomics and PET radiomics: ready for clinical implementation?Q J Nucl Med Mol Imaging. 2019Dec;63(4):355–370. doi: https://doi.org/10.23736/S1824-4785.19.03192-3.
Arimura H, Soufi M, Kamezawa H, Ninomiya K, Yamada M. Radiomics with artificial intelligence for precision medicine in radiation therapy. J Radiat Res. 2019 Jan 1;60(1):150–157. doi: https://doi.org/10.1093/jrr/rry077.
Neri E, Del Re M, Paiar F, Erba P, Cocuzza P, Regge D, Danesi R. Radiomics and liquid biopsy in oncology: the holons of systems medicine. Insights Imaging. 2018 Dec;9(6):915–24. https://doi.org/10.1007/s13244-018-0657-7.
Scheckenbach K, Radiomics. Big Data Instead of Biopsies in the Future? Laryngorhinootologie. 2018 Mar;97(S 01):S114-S141. doi: https://doi.org/10.1055/s-0043-121964.
Cascella M, Bimonte S, Barbieri A, Del Vecchio V, Caliendo D, Schiavone V, Fusco R, Granata V, Arra C, Cuomo A. Dissecting the mechanisms and molecules underlying the potential carcinogenicity of red and processed meat in colorectal cancer (CRC): an overview on the current state of knowledge. Infect Agent Cancer. 2018 Jan 15;13:3. https://doi.org/10.1186/s13027-018-0174-9. PMID: 29371880; PMCID: PMC5769331.
Lafata KJ, Wang Y, Konkel B, Yin FF, Bashir MR. Radiomics: a primer on high-throughput image phenotyping. Abdom Radiol (NY). 2022 Sep;47(9):2986–3002. https://doi.org/10.1007/s00261-021-03254-x.
Lenga L, Bernatz S, Martin SS, Booz C, Solbach C, Mulert-Ernst R, Vogl TJ, Leithner D. Iodine Map Radiomics in Breast Cancer: Prediction of Metastatic Status. Cancers (Basel). 2021 May 18;13(10):2431. doi: https://doi.org/10.3390/cancers13102431.
Granata V, Fusco R, Filice S, Catalano O, Piccirillo M, Palaia R, Izzo F, Petrillo A. The current role and future prospectives of functional parameters by diffusion weighted imaging in the assessment of histologic grade of HCC. Infect Agent Cancer. 2018 Jul 3;13:23. https://doi.org/10.1186/s13027-018-0194-5. PMID: 29988667; PMCID: PMC6029348.
Haarburger C, Müller-Franzes G, Weninger L, Kuhl C, Truhn D, Merhof D. Radiomics feature reproducibility under inter-rater variability in segmentations of CT images. Sci Rep. 2020 Jul 29;10(1):12688. doi: https://doi.org/10.1038/s41598-020-69534-6. Erratum in: Sci Rep. 2021 Nov 16;11(1):22670.
Fusco R, Granata V, Grazzini G, Pradella S, Borgheresi A, Bruno A, Palumbo P, Bruno F, Grassi R, Giovagnoni A, Grassi R, Miele V, Barile A. Radiomics in medical imaging: pitfalls and challenges in clinical management. Jpn J Radiol. 2022 Sep;40(9):919–29. https://doi.org/10.1007/s11604-022-01271-4.
Li Y, Eresen A, Lu Y, Yang J, Shangguan J, Velichko Y, Yaghmai V, Zhang Z. Radiomics signature for the preoperative assessment of stage in advanced colon cancer. Am J Cancer Res. 2019 Jul 1;9(7):1429–1438.
Cappabianca S, Reginelli A, Iacobellis F, Granata V, Urciuoli L, Alabiso ME, Di Grezia G, Marano I, Gatta G, Grassi R. Dynamic MRI defecography vs. entero-colpo-cysto-defecography in the evaluation of midline pelvic floor hernias in female pelvic floor disorders. Int J Colorectal Dis. 2011 Sep;26(9):1191–6. https://doi.org/10.1007/s00384-011-1218-4. Epub 2011 May 3. PMID: 21538053.
Gang GJ, Deshpande R, Stayman JW. Standardization of histogram- and GLCM-based radiomics in the presence of blur and noise.Phys Med Biol. 2021 Mar15:https://doi.org/10.1088/1361-6560/abeea5.
Granata V, Fusco R, De Muzio F, Cutolo C, Setola SV, Dell’Aversana F, Grassi F, Belli A, Silvestro L, Ottaiano A, et al. Radiomics and machine learning analysis based on magnetic resonance imaging in the assessment of liver mucinous colorectal metastases. Radiol Med. 2022;127:763–72. https://doi.org/10.1007/s11547-022-01501-9.
Gabelloni M, Faggioni L, Cioni D, Mendola V, Falaschi Z, Coppola S, Corradi F, Isirdi A, Brandi N, Coppola F, Granata V, Golfieri R, Grassi R, Neri E. Extracorporeal membrane oxygenation (ECMO) in COVID-19 patients: a pocket guide for radiologists. Radiol Med. 2022 Apr;127(4):369–82. https://doi.org/10.1007/s11547-022-01473-w.
Granata V, Fusco R, Cozzi D, Danti G, Faggioni L, Buccicardi D, Prost R, Ferrari R, Trinci M, Galluzzo M, et al. Structured reporting of computed tomography in the polytrauma patient assessment: a Delphi consensus proposal. Radiol Med. 2023;128(2):222–33. https://doi.org/10.1007/s11547-023-01596-8.
Available online. : https://www.aapm.org/org/policies/details.asp?id=468 (accessed on 30 November 2022).
Granata V, Fusco R, Catalano O, Piccirillo M, De Bellis M, Izzo F, Petrillo A. Percutaneous ablation therapy of hepatocellular carcinoma with irreversible electroporation: MRI findings. AJR Am J Roentgenol. 2015 May;204(5):1000–7. https://doi.org/10.2214/AJR.14.12509.
Bimonte S, Leongito M, Barbieri A, Del Vecchio V, Barbieri M, Albino V, Piccirillo M, Amore A, Di Giacomo R, Nasto A, Granata V, Petrillo A, Arra C, Izzo F. Inhibitory effect of (-)-epigallocatechin-3-gallate and bleomycin on human pancreatic cancer MiaPaca-2 cell growth.Infect Agent Cancer. 2015 Jul29;10:22. doi: https://doi.org/10.1186/s13027-015-0016-y.
Avallone A, Pecori B, Bianco F, Aloj L, Tatangelo F, Romano C, Granata V, Marone P, Leone A, Botti G, Petrillo A, Caracò C, Iaffaioli VR, Muto P, Romano G, Comella P, Budillon A, Delrio P. Critical role of bevacizumab scheduling in combination with pre-surgical chemo-radiotherapy in MRI-defined high-risk locally advanced rectal cancer: Results of the BRANCH trial. Oncotarget. 2015 Oct 6;6(30):30394-407. doi: https://doi.org/10.18632/oncotarget.4724.
Granata V, Fusco R, Avallone A, De Stefano A, Ottaiano A, Sbordone C, Brunese L, Izzo F, Petrillo A. Radiomics-Derived Data by Contrast Enhanced Magnetic Resonance in RAS Mutations Detection in Colorectal Liver Metastases. Cancers (Basel). 2021 Jan 25;13(3):453. doi: https://doi.org/10.3390/cancers13030453.
Acknowledgements
The authors are grateful to Alessandra Trocino, librarian at the National Cancer Institute of Naples, Italy.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
V.G. wrote the initial manuscript. All authors revised the manuscript for intellectual content and approved the final manuscript as submitted. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Institutional review board statement
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that there are no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
“The original version of this article was revised: the ‘Data availability’ statement was corrected.”
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Granata, V., Fusco, R., Setola, S.V. et al. Colorectal liver metastases patients prognostic assessment: prospects and limits of radiomics and radiogenomics. Infect Agents Cancer 18, 18 (2023). https://doi.org/10.1186/s13027-023-00495-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13027-023-00495-x