Abstract
Background
Childhood dementias are a group of rare and ultra-rare paediatric conditions clinically characterised by enduring global decline in central nervous system function, associated with a progressive loss of developmentally acquired skills, quality of life and shortened life expectancy. Traditional research, service development and advocacy efforts have been fragmented due to a focus on individual disorders, or groups classified by specific mechanisms or molecular pathogenesis. There are significant knowledge and clinician skill gaps regarding the shared psychosocial impacts of childhood dementia conditions. This systematic review integrates the existing international evidence of the collective psychosocial experiences of parents of children living with dementia.
Methods
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We systematically searched four databases to identify original, peer-reviewed research reporting on the psychosocial impacts of childhood dementia, from the parent perspective. We synthesised the data into three thematic categories: parents’ healthcare experiences, psychosocial impacts, and information and support needs.
Results
Nineteen articles met review criteria, representing 1856 parents. Parents highlighted extensive difficulties connecting with an engaged clinical team and navigating their child’s rare, life-limiting, and progressive condition. Psychosocial challenges were manifold and encompassed physical, economic, social, emotional and psychological implications. Access to coordinated healthcare and community-based psychosocial supports was associated with improved parent coping, psychological resilience and reduced psychological isolation. Analysis identified a critical need to prioritize access to integrated family-centred psychosocial supports throughout distinct stages of their child’s condition trajectory.
Conclusion
This review will encourage and guide the development of evidence-based and integrated psychosocial resources to optimise quality of life outcomes for of children with dementia and their families.
Key points
-
A synthesis of the shared psychosocial experiences and impacts of conditions causing childhood dementia is warranted.
-
Parents share a tranche of overlapping challenges owing to limited access to psychosocial resources for their child’s dementia condition.
-
Severe neurocognitive decline is associated with higher parent psychological distress and isolation.
-
Coordinated psychosocial interventions are required to improve outcomes for the family unit.
-
Growing childhood dementia public awareness may activate earlier access to coordinated, sustainable and integrated supports.
Similar content being viewed by others
Introduction
Childhood dementia comprises a group of devastating, predominantly neurodegenerative conditions, characterised by global and progressive neurocognitive decline, relative loss of developmental skills, as well as a shortened life expectancy in infants, children, and adolescents [1]. Whilst individually rare, surveillance studies have reported incidence rates between 10 and 60 per 100,000 births [2,3,4] which is on par with other well-recognised conditions such as cystic fibrosis (1 in 3139 births) [5, 6]. Noting that there are differences in population, terminology, definition and grouping of disorders in these studies. Examples of conditions that consistently fit the definition of childhood dementia include Batten disease, Sanfilippo syndrome, Niemann–Pick disease types A and C, Tay-Sachs disease, metachromatic leukodystrophy, and some mitochondrial disorders, amongst others [7,8,9,10]. While global neurocognitive decline is a core deficit, each individual childhood dementia-causing disorder is clinically heterogeneous, with variable patterns of disease progression that affects every aspect of adaptive function [9,10,11]. Pathways to identify causes for this clinically severe group of conditions are complex [12]. Treatment options are limited for this group of rare diseases resulting in a severely shortened life expectancy ranging from infancy (e.g. Gaucher disease type 2 and nonketotic hyperglycinemia glycine encephalopathy) [13, 14], to ~ 50 years of age (e.g. Rett syndrome)[15]. It has been estimated that 75% of children with dementia die before the age of 18 [16]. While extensive progress has been made in understanding the underlying pathophysiology for individually rare childhood dementia conditions, with a growing number of genetic causes still being discovered, scientific advancements have yet to translate into accessible healthcare services and psychosocial supports for affected families [11, 17, 18].
Often, children will demonstrate typical development, then decelerate their progress, with substantial regression and global deterioration [19]. In other cases, syndromes can be so severe that the impact on neurodevelopment and associated neurocognitive decline begins from a low baseline of development, resulting in the prevention of the attainment of developmental skills [20,21,22]. Although symptomatology can vary across disorder groups, children commonly develop a spectrum of co-existing and progressive symptoms related to the primary disease mechanism that impact cognitive, behavioral, and physical domains, including organ systems associated with their dementia condition [11, 23]. Childhood dementia shares several hallmark features akin to adult dementia, including: decline in cognitive ability, memory loss, wandering and restlessness, emotional difficulties (e.g. anxiety, fear, panic attacks), personality and behavioral changes (e.g. aggression, irritability, hyperactivity)[19]. Moreover, children with childhood dementias suffer severe sleep disturbances, movement disorders (e.g. muscle spasms, tremors), deterioration of communication skills, loss of vision and hearing, mood disorders, psychosis (including hallucinations and delusions) and incontinence [11]. Childhood dementia conditions are also severely life-limiting and life-threatening; causes of death include respiratory complications (e.g. pneumonia), neurological complications (e.g. intractable epilepsy), or cardiac events [16]. Throughout the course of the illness acute global brain dysfunction including delirium, encephalopathy are common and towards the end of life prolonged periods of stupor and coma [1, 7, 24].
Given the non-specific initial presenting symptoms, the rarity of the individual conditions, and associated limited natural history data, diagnosis of a childhood dementia condition is typically delayed, sometimes for years after the first symptoms appear [12, 25]. Children are commonly misdiagnosed with autism, developmental or intellectual delay [25] and families can face a ‘diagnostic odyssey’ in the search for a diagnosis for their child. Research in other rare disease groups has demonstrated that delayed and prolonged diagnoses, lack of treatment options and chronically unmet needs negatively impact parents’ physical and psychological wellbeing [26,27,28,29,30]. There has been an increasing focus on interdisciplinary collaboration and cross-pollination of knowledge to enhance healthcare services, including diagnostics and therapeutic advancements for individuals living with rare diseases [18, 31]. Emerging from this climate, the Childhood Dementia Initiative was launched in Australia in 2020 with the purpose to transform research, care and quality of life for children with dementia by: bringing together the many individual ‘siloed’ conditions; focusing on the commonalities of childhood dementia; fostering diverse but complementary approaches; driving collective progress.
Psychosocial research specifically considering the collective healthcare experiences and psychosocial impacts of childhood dementia conditions on parents is currently lacking. This lack of evidence represents a significant obstacle for clinicians, patients, and their families and has delayed the development of a multidisciplinary healthcare approach and evidence-based psychosocial supports [32, 33]. Psychosocial research is important to facilitate better understanding of the unique caregiving demands placed on parents and to explore how parents respond to and cope with the challenges of their child’s rare disease. This review will contribute to the knowledge base to inform coordinated healthcare and community supports and the development of evidence-based psychosocial resources to address the unmet needs of parents.
Our review focused on three research questions:
-
1.
What are parents’ experiences of navigating their child’s healthcare?
-
2.
What is the current evidence regarding the psychosocial impacts of childhood dementia, as reported from the parent perspective?
-
3.
What are parents’ information and support needs?
Method
We structured the review using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [34]. We searched the PROSPERO database [35] prior to commencing this review and published a protocol for this review (CRD42021291858).
Search strategy
We conducted the search and article selection process between February and April 2022, identifying original studies by searching four electronic databases including PubMed, PsycINFO, Embase, and the Cumulative Index to Nursing and Allied Health Literature (CINAHL). We applied a detailed and extensive review of indexing terms used in a set of articles that met the search inclusion criteria to identify suitable search terms. We then consulted clinical subject matter experts (KE and MF) to refine the set of search terms and to ensure the relevance and clinical applicability of our search. In addition, we consulted with an independent research librarian to assess our search strategy completeness. We modified individual search strategies according to the database MeSH/subject headings and employed database searching conventions for identifying the use of single and plural terms, as well as to account for different spellings of search terms to create a comprehensive search (see Additional file 1: Table S1).
We employed the following search strategy (parents OR caregiver OR family OR child) AND (childhood dementia OR mental deterioration OR progressive cognitive decline OR cognitive decline) AND (psychosocial OR quality of life OR health service needs and demands OR mental health OR coping). We also conducted a search on Google Scholar and reviewed the reference lists of included studies.
Eligibility criteria
We determined the article eligibility criteria using the PICOS characteristics [36] (i.e., characteristics describing the study population (P), illness/condition (I), comparison condition (C), outcome (O) and study design (S)). We included original, peer-reviewed articles published in English addressing the parent-reported psychosocial impacts of caring for a child with a childhood dementia. To surmount the heterogeneity between childhood dementia conditions, we adopted the clinical criteria proposed in Box 1, adapted from published case definitions [11]. When studies included sub-groups of parents of healthy children, general population norms, or parents of children with chronic diseases, we included these sub-groups as comparisons. Qualitative, quantitative and mixed-methods studies were included if 1) they assessed the parent-reported psychosocial impacts of caring for a child with a dementia (< 18 years); and 2) > 50% of the sample were parents of children with a childhood dementia (that met the criteria according to the below text description). The inclusion criteria for childhood dementia included any child (under 18 years of age at symptom onset) with any illness that fulfilled all the following criteria:
*A note on terminology
The term childhood dementia is not ubiquitously employed as standard throughout the medical literature. Conditions that cause progressive cognitive decline in childhood have been grouped as 'progressive intellectual and neurological deterioration' (PIND) in children [7], progressive childhood encephalopathy ([8, 9] and childhood dementia [1], albeit with slightly different definitions. At present, Human Phenotype Ontology (HPO) and Online Mendelian Inheritance in Man (OMIM) do not catalogue search terms to identify childhood dementia conditions. Mental retardation and dementia are terms that are far broader than childhood dementia. 'Mental retardation' includes conditions where IQ is low, but IQ does not necessarily decline as it does in childhood dementia. 'Dementia' includes adult-onset conditions such as Alzheimer's disease. This inconsistency of both language and definition is hampering efforts to understand this group of diseases and very little is known about the shared needs of families. This was our reasoning to conduct this systematic review, to provide the evidence needed to advocate for improved care and treatment of this group of patients. Concomitant interdisciplinary research and advocacy efforts are currently underway to improve consistency of definition, terminology and coding for this group of diseases [40].
We excluded: case studies, unpublished dissertations, clinical intervention trials, validation studies of quality of life instruments, and studies that did not directly report on parents’ self-reported psychosocial impacts of caregiving. We also excluded articles which reported on the aggregate findings of different disease groups, wherein the specific impact of childhood dementia conditions on parents could not be ascertained.
Selection criteria
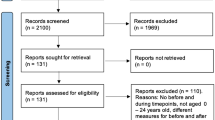
We exported all citations from our individual database searches using Endnote X7 (Thomas Reuters) and removed duplicates. We imported and merged all articles in RAYYAN, which is a specialized software program for conducting systematic reviews [41]. SMN and BM independently screened the titles and abstracts of the studies which were potentially eligible for inclusion using RAYYAN QCRI, to identify citations that related to the psychosocial experiences of parents and families of children with childhood dementia. To ensure agreement and equal understanding of the eligibility criteria between the two reviewers, a pre-test of the criteria was conducted, with each reviewer screening 100 abstracts and comparing their decisions before they continued the screening. SMN and BM independently reviewed all full texts, noting their decisions for including or excluding articles in the RAYYAN system. Wherever uncertainty regarding clinical diagnostic criteria for childhood dementia was arose, SMN consulted a clinical expert in childhood dementia (KE) to make a final decision. Figure 1 shows the PRISMA flow diagram of the identified and selected citations [42].
Data extraction
SMN lead the data extraction for all 19 studies and BM independently extracted data for 20% of studies (randomly selected) to monitor accuracy of the process. Information extracted included [1] study characteristics (author, year and country of publication, study design); [2] parent characteristics (gender, age range) and patient characteristics (childhood dementia diagnosis, gender, age range of child); [3] recruitment methods and outcome assessment methods (questionnaire, interview, focus group); [4] relevant thematic findings (healthcare experiences, psychosocial impacts, information and support needs). Summary and evidence tables were created for this purpose.
Quality analysis
We used the QualSyst tool [43] to assess the research methodology quality and risk of bias of included studies. SMN and BM rated the studies according to either qualitative or quantitative criteria. To ensure fairness in ratings, if the studies included both qualitative and quantitative elements but were not explicitly stated to be mixed methods, then SMN and BM evaluated the primary research design described in the methods. SMN and BM rated the studies independently, compared assessments, and resolved any discrepancies through discussion until they reached consensus.
Methodological Rigour
The QualSyst scoring system contains 14 items to assess quantitative studies, with each item scored as 0 (no), 1 (partial), 2 (yes), or ‘not applicable’. The same ranking process is used to assess qualitative studies that are rated on a scale containing 10 items. Total summary scores were obtained for each study (see Additional file 1: Tables S2 and S3) and converted to a quality index score, ranging 0–1. To be included in the review, studies required a quality index score of 0.5 or above [43]. This threshold was chosen following consideration of the quality score distribution and the relatively small number of articles that met our review inclusion criteria (Additional file 1: Tables S2 and S3). To account for the heterogeneity of included articles and outcomes reported, we performed a content analysis [44] and narrative synthesis of the results to characterize the impact of childhood dementia conditions on parents’ healthcare experiences and psychosocial outcomes [45]. This included exploring and comparing patterns of thematic findings highlighting the effects parents’ healthcare experiences and factors shaping parents’ psychosocial impacts across the included studies [46]. We also considered the quality of the methodologies, to guide clinical practice recommendations and future research directions.
Results
We identified 19 eligible articles, including 7 qualitative [47,48,49,50,51,52,53] and 12 quantitative studies [54,55,56,57,58,59,60,61,62,63,64,65] representing the perspectives of 1856 parents of children across 21 different dementia-causing conditions. The mean quality score for the quantitative studies was 0.91 and the mean quality core of the qualitative studies was 0.94 (see Additional file 1: Table S1). We excluded one article that did not provide sufficient detail of the study methodological rigour to be included in this review. These studies stemmed from 11 countries: the USA [48, 50, 52, 55, 61, 63, 64], Canada [47, 57], Germany [58, 62], Australia [65], Ireland [49], Japan [60], Poland [54], Spain [53], Sweden [51], the Netherlands [59], and the United Kingdom [56]. Several studies ascertained data from international populations using online platforms (e.g. rare disease advocacy websites) to maximise recruitment. Of the 19 studies, 15 were cross-sectional [47, 48, 50,51,52, 54,55,56,57,58,59,60,61,62, 64], 3 were longitudinal [49, 63, 65], and one study comprised a multi-perspective cohort [53]. Table 1 lists the dementia causing conditions examined in each included study. Sixteen studies examined the perspectives of both mothers and fathers [47, 48, 50,51,52,53, 56,57,58,59,60, 62,63,64,65,66], three studies did not specify parents’ gender [49, 54, 55] and one study included only mothers [61]. There was large variance in sample size within the included studies ranging from N = 8 [51] to N = 727 participants [63]. Twelve included more than 20 participants [48, 50, 52,53,54, 56,57,58,59,60,61,62], while four studies included more than 50 participants [55, 63,64,65]. In line with our review questions, we extracted the results from the articles into three thematic categories focusing on [1] parents’ healthcare experiences; [2] psychosocial impacts; and [3] information and support needs (Fig. 2). A summary of the results of each study can be found in Tables 1 and 2.
Parents' experiences searching for a diagnosis and navigating health and social care systems
Battling for a diagnosis
Parents spent an extended length of time and energy visiting numerous clinicians and undergoing multiple diagnostic tests after the birth of their child in the hope of obtaining a diagnosis which was highly emotionally and physically taxing [50, 51]. Extensive challenges connecting with specialist clinical teams who could engage empathetically and listen to parents’ concerns regarding their child’s developmental and behavioral features, that medical teams have not previously considered as part of the diagnostic formulation were identified in several studies [51, 53, 56, 62]. The prolonged delay in achieving a diagnosis incurred substantial delays in accessing timely therapies and was a source of heightened chronic stress which parents reported was like ‘watching a ticking time bomb’ [49]. As their child’s condition progressed, acute-onset and non-specific disease-related symptomatology, such as severe seizures had a significant traumatic impact on parents’ emotional wellbeing [26, 49, 53, 59, 67, 68] leading to a state of prolonged state of alertness in parents [53].
Perpetuating obstacles to management and supports for progressive symptomology
Beyond the diagnostic period, parents experienced ongoing decisional uncertainty and limited access to information about how to manage the range of their child’s non-specific and uncertain neurocognitive and behavioral disease symptoms, which “arose at irregular intervals” [50, 52, 53, 65]. Parents reported perpetuating obstacles managing their child’s daily care, without access to first-line non-pharmacological and behavioral therapies (e.g. speech therapy, physiotherapy) to reduce the acceleration of their child’s developmental impairments and cognitive decline [47, 53, 54, 58, 63]. In several studies, parents emphasized that the prolonged delays they experienced in accessing healthcare services combined with the perceived amplification of their child’s progressive physical symptoms and neurocognitive regression compounded the intensity of their distress [47, 51]. Parents experienced frustration, and despair, “battling” beurocracy [49] for basic healthcare supports including a medical card or a wheelchair for their child [49, 51, 52, 65]. Profound developmental regression, life-threatening seizures, respiratory complications, motor impairment, sleep disturbances, and associated psychotic manifestations were repeatedly identified as conferring a high physical burden on parents [47, 50, 53, 55, 58, 63]. In addition, uncooperative behaviors including aggression, hyperactivity, agitation, orality, and a loss of communication skills were emotionally distressing for parents, who frequently reported a deficit of available guidance and support to manage and cope with their child’s challenging behaviors [58].
Parents emphasized that healthcare and social insurance systems did not cater for a rare disease where life-threatening symptoms could suddenly develop and progressively cause loss of function [48, 51, 53]. The perceived manageability of their child’s comorbidities and physical disabilities became more difficult with their child’s increasing age [52, 55] and parents described feeling powerless, watching their child being “eaten away” by disease [49]. Although some parents had a team of engaged clinicians to provide holistic support for their child in the paediatric healthcare system [51, 62], transitioning to the adult healthcare setting, where clinicians lacked knowledge about their child’s condition and treated co-occurring developmental and behavioral features in isolation caused parents significant additional anguish [48, 51]. For example, parents described experiencing feeling “trapped in a box” [49] without support when they no longer belonged in the paediatric healthcare system and had not completed passage to the adult healthcare system [49].
The advanced disease stage had a significant negative impact on parents’ quality of life due to the high level of impairment their child was suffering, the physicality of heavy caregiving demands, coupled with minimal feedback from their child [62]. Challenging symptoms in the advanced stages included blindness, complete loss of mobility, communication and basic sensorimotor function, and independent eating capacity or the requirement for a percutaneous endoscopic gastrostomy tube [62]. Complete dependence on parents, coupled with severe emotional and behavioral impairments including psychotic symptoms brought additional loss and resignation towards the end stage of the disease [48]. While some parents preferred the option to care for their child in the comfort of their own home (e.g. rather than a hospital setting) [49], longitudinal studies indicated parent quality of life improved when the child was living in out-of-home care and when parents were allocated time to cater for their own needs [51, 55, 65].
The psychosocial impacts of childhood dementia throughout the child’s life and ongoing grief
Multiple layers of recurring losses
Parents described an all-consuming experience of chronic sorrow associated with their child’s deteriorating function and progressive clinical features which commonly began after the birth of their child [53], and continued throughout the disease course [51]. As their child matured, physical disabilities including loss of function and mobility had profound “destroying impact on the child’s body” and caused their child significant frustration [49]. Parents in turn experienced reciprocal distress, anticipatory grief and intense prolonged emotional heartache watching their child feel anxious, unhappy, and in pain [49, 50, 52]. Further, their child’s marked loss of communication skills impaired parents’ capacity to understand their child’s verbal/non-verbal messages and was perceived as losing a crucial aspect of the parent–child relationship [52]. For example, parents reported their child’s loss of communication skills hindered primary parenting goals and caused parents to question their self-efficacy to meet their child’s evolving healthcare needs [49, 52]. Parents reported a perceived pressure to protect both their child and family from the stigmatization of a “cruel society”[49], particularly when their child’s uncooperative behavior (e.g. aggression, irritability, hyperactivity) was negatively misinterpreted by others [51, 58].
Parents described feeling that their life was “on pause”, with reduced capacity for social activities outside the family home, whilst they simultaneously grieved the losses of their relationship with their child and their relationships with people who used to be close [50, 51]. Parents also reported intense fear and chronic traumatic distress experiencing their child “slowly deteriorate and die” [50] and coinciding communication difficulties with clinical teams who often could not offer appropriate emotional counselling support [51]. Notably, the family and clinical team seeing the disease as a common enemy helped parents to cope with the grief of their child’s diagnosis [51]. The relief from care assistants and a short-term stay at a care centre where families of children with disabilities meet were described as a salvation which provided a source of recovery for parents [51]. Furthermore, parents who accessed psychosocial supports and shared responsibilities with other family members reported enhanced self-efficacy and more effective family functioning [48, 49, 54, 62,63,64,65]. On the other hand, the lack of psychosocial supports contributed to resentment and anger [48] especially among parents of children approaching end of life [49]. Parents whose child had died reported experiencing a loss not only related to their child’s death but also a loss of identity [51].
Personal costs and sacrifices
Parents reported challenges meeting their physical, social and psychological needs due to the significant demands of their child’s extensive healthcare needs and complex care and management requirements [48, 51, 52]. Parents frequently reported interruption to their professional career to be able to take care of their child, resulting in decreased economic income for the family [53, 62]. The intensity of caregiving demands was illuminated in a study indicating that mothers spent, on average, 88 h per week caring for their child and managing their child’s high-risk behaviors [62]. Additionally, the high direct economic costs of therapies that were indispensable for their child’s care and the indirect costs associated with frequent hospital appointments and work readjustments reinforced economic struggles for parents [53]. Multivariate analyses indicated that having two or more siblings, or being a single parent was associated with poor family functioning and poor physical wellbeing among parents over time [65]. In several studies, parents also reported guilt and tension regarding not being present for the healthy siblings of their ill child [49,50,51, 65].
Quality of life and mental health impacts
Six studies investigated the relationship between a spectrum of disease-specific factors, including the severity of the child’s physical, behavioral and neurocognitive functioning [57,58,59, 63, 65, 69] with parent quality of life outcomes [57, 59, 69]. Although the heterogeneity of individual dementia phenotypes in the included studies varied both within and across patient conditions, overall, the severity of the child’s diagnostic presentation appeared to have consistent, adverse impacts on parents’ quality of life and mental health outcomes. Poorer quality of life and mental health outcomes were highlighted in studies which compared parents of children with a dementia with other illness conditions (e.g. parents of oncology patients) [56], reference group populations (e.g., healthy controls or norm values) [57, 59], as well as those that investigated subgroups of parents of children with mild and severe forms of the same diagnosis (e.g. Mucopolysaccharidosis II; MPS II)[55, 58]. The severity of the child’s clinical presentation (e.g., degree of developmental regression) was associated with greater adverse impacts on parent quality of life outcomes (e.g., physical health component scores and mental health component scores) [63, 65], lower scores on psychological examinations [60, 61] and lower family functioning [52, 55, 62, 64, 65]. For example, a more severe presentation of MPS II was correlated with lower parent health-related quality of life and lower family functioning in terms of family relationships, communication, stress, decision-making, psychosocial functioning, and psychological status [55].
Several studies indicated clinically-relevant levels of parent stress [57], depression [50, 60], anxiety [56] and post-traumatic stress disorder [56, 59], particularly among younger mothers of recently diagnosed children [60, 61]. Conversely, greater time period beyond their child’s age of regression was associated with improved parent psychological wellbeing [63]. Sleep and mood disturbances contributed heightened emotional and behavioral challenges in children and were associated with poorer parent psychological wellbeing and poorer parent physical wellbeing over time [65]. For example, sleep disturbances and behavioral difficulties translated to exacerbated parent distress, anxiety, sleep quality and subsequent capacity to care for their child’s healthcare needs [51,52,53, 58, 65]. Additionally, the relationship between the severity of the child’s clinical presentation and parent psychological status [57, 59] was examined in quantitative and qualitative studies which indicated significantly higher stress among parents of children with severe behavioral comorbidities, including aggression and feeding difficulties [54, 58]. Affirming this, qualitative interviews investigating parent psychosocial functioning indicated that the severity and chronicity of their child’s symptom progression conferred high psychological distress [50], and adversely impacted on parents’ health related quality of life [62].
Expressions of resilience
Interestingly, although disease severity was shown to predict parents’ psychological status [55], coping and stress reduction strategies, including accessing psychological counselling and social support networks served to alleviate parents’ levels of stress and improved family functioning, regardless of the severity of their child’s condition [49, 51, 52, 58, 64]. In these studies, parents shared that their experience with their child’s condition encouraged them to see life from a new perspective and to adopt new beliefs about what was meaningful in life [51, 52]. To maintain a positive outlook, parents prioritized social connectedness and accessible community supports to facilitate shared learning and emotional support amidst the ongoing challenges [51, 58, 60]. In addition, parents reported that spending time without the affected child was important to maintain balance in the family and to support relationship dynamics between parents and healthy siblings, as well as the couple's relationship [51]. Additionally, quantitative studies investigating family functioning found better quality of life outcomes, including improved psychological wellbeing, among family members who allocated time spent without their affected child to fulfil their personal and family’s needs [63, 65]. Likewise, factors related to family functioning and parent adaptation to their child’s diagnosis found more effective family functioning was associated with greater parent self-efficacy, and enhanced problem and emotion-focused coping [64]. In this study, family functioning was a significant partial mediator of the relationships between adaptation, parent self-efficacy and coping [64].
Parents’ information and support needs
Proactive communication and collective learning
Insufficient information to navigate the slow and arduous diagnostic process was a prevailing theme [49, 50, 58, 62]. Parents advocated for proactive explanations about what tests their child was undergoing and honest discussions to help parents to set realistic expectations regarding what to expect following diagnostic investigations [48]. Accordingly, when honest and comprehensible conversations about their child’s anticipated disease severity were initiated early, this had a significant positive impact on parents’ psychological wellbeing [49, 62] and their capacity to emotionally prepare to care for their child [51]. As with the information gap, parents widely reported a perceived lack of knowledge and openness to learning among clinicians with respect to their child’s condition and subsequent challenges accessing coordinated therapeutic supports for their child’s progressive disease symptomology [53]. Parents emphasized the importance of having clinicians listen to their concerns about the onset of developmental and behavioral symptoms in their child, which clinicians may not have encountered before [62]. Parents underscored that collaborative communication and collective learning between multidisciplinary and sub-specialist clinicians and families was crucial to expediate delayed wait times and barriers to access to therapeutic interventions to halt the acceleration of their child’s cognitive regression, and progressive comorbidities [48, 51, 58, 62].
Intense need for urgent therapeutic development
Parents prioritized the urgent need for therapeutic interventions that target their child’s cognitive regression, and behavioral and psychiatric comorbidities as their primary goal for new treatments [50, 52]. For example, parents reported that therapeutic interventions that reduce the pace of their child’s global regression including slowing the rate of decline in cognition, communication and mobility, as conferring the greatest benefit in terms of their quality of life outcomes [50, 52]. Worthwhile approaches to manage challenging behavior included play and distraction techniques, environmental changes and repeated specific reassurance, rather than traditional operant conditioning [58]. To accelerate therapeutic developments, parents emphasized the need for faster pathways to a diagnosis, as well as broader access to clinical trials and approved therapies [52]. To better meet the needs of families, parents advocated for clinical trials to incorporate measures that holistically quantify the impact of their child’s progressive clinical phenotype (e.g., improvements in mobility or treatments for pain management would be meaningful, even in the absence of evidence for improvement in cognition) [51, 52, 66]. Parents of children who were older or had further progressed in their disease course expressed disappointment in the age limitations for past and ongoing clinical trials [52]. Parents proposed that a dedicated space, such as a centre of expertise for rare disease, would optimize clinical practice as it would expand clinician knowledge and facilitate collaboration between clinicians, healthcare providers, patients, and families, [49, 52].
Advocacy for meaningful resources and services
To achieve equitable healthcare services to address their child’s basic needs, parents underscored a pressing need for collective advocacy to generate awareness and recognition for the psychosocial support needs of children with dementia, and their parents in hospital and community settings [47, 48, 54, 60, 62]. Parents considered that stage-specific psychoeducational resources and support during different stages of their child’s condition trajectory was critical to support emotional adaption to their child’s progressive condition [51, 56, 57, 60]. For example, parents advocated for tailored psychoeducation about how to identify and manage complex psychiatric and behavioral symptoms that their child could develop, and how to integrate their child’s “ever-changing” and progressive care requirements into daily life and family routine [53]. Parents strongly recommended family counselling in a private space to provide an opportunity to collectively learn about their child’s condition [51, 62] and to help strengthen interfamilial functioning surrounding the diagnostic period [48, 58]. Studies demonstrated psychological counselling was especially important for younger mothers with few years since the child’s diagnosis [60]. Similarly, parents shared that opportunities to emotionally connect with others who understood their circumstances and did not hold disparaging views of their child’s uncooperative behaviors was necessary to provide parents with emotional support and reassurance that they were advocating appropriately for their child [51,52,53]. In terms of additional psychosocial resources, parents considered that in-home nursing and respite care, flexible supports in the workplace, and accessible community resources were necessary to reduce and treat parent psychological sequelae [47, 48, 54, 55, 60, 62].
Discussion
Despite emerging knowledge of individually rare childhood dementia conditions, the collective psychosocial impacts of childhood dementias remain under-explored. This is the first systematic review to comprehensively integrate current international evidence documenting the healthcare experiences, psychosocial impacts and unmet information and support needs shared by parents of children with dementia. We identified 3 key overarching themes from 19 studies (Fig. 2). Firstly, parents experience a range of challenges navigating quality health and social care for their child owing to the rare, life-limiting, and progressive nature of their child’s dementia condition [49, 52, 58]. Difficulties accessing clinical teams equipped to provide early and coordinated care for their child’s complex progressive condition, compounded by a deficit of condition-specific information, impart a high physical and mental toll on parents [53, 56]. Secondly, psychosocial challenges are manifold and encompass physical, economic, social, emotional and psychological implications, which frequently precipitate prolonged grief and impaired quality of life among parents [54, 62, 63, 65]. Thirdly, our review identified priority areas that can be targeted with future interventions to protect and promote parents’ psychosocial wellbeing during key stages along the trajectory of their child’s condition (Fig. 3). These priority areas include providing additional evidence-based and integrated psychosocial support to parents during; (1) their child’s diagnostic phase; (2) periods of transition between different healthcare or community care settings; and (3) the advanced stages of the disease, when children lose key skills, such as language or mobility [56, 67].
Our first objective was to investigate parents’ healthcare experiences managing their child’s condition. The most prevalent obstacle that presented across the studies was achieving a diagnosis for their child and connecting with clinical teams who could provide honest and comprehensive information and counselling support about the uncertainty and potential severity of their child’s condition [62]. Persistent barriers accessing information and therapeutic interventions to reduce the acceleration of their child’s progressive neurocognitive decline and deteriorating function cultivated significant grief and frustration among parents, who felt powerless without a clinical team to support them [49]. Our findings extend on emerging rare disease research highlighting that early engagement with coordinated healthcare teams that are equipped to communicate appropriately with families during the “diagnostic odyssey” and to advocate for the child’s progressive healthcare needs, may have a substantial positive impact on parents’ psychosocial wellbeing, and their capacity to care for their child [49, 51, 62, 70]. Importantly, our review identified that the cumulative uncertainties and chronic traumatic stress endured by parents are exacerbated by concurrent progressive global deteriorating function [49, 51, 52] and the fear of their child’s imminent death [48, 51, 55]. Global clinical guidelines highlight the importance of adopting a trauma-informed approaches to care and support families affected by progressive and severely life-limiting disease, including providing timely referrals to paediatric palliative care services [71, 72]. Earlier access to paediatric palliative care services with can improve a child and family’s quality of life through the provision of holistic care and gently introducing conversations about end of life throughout the various phases of a child’s condition [73, 74]. Our findings support that providing early and appropriate integrated care, considering the specific needs of the families and involving both generalist and subspecialist paediatric palliative care teams may improve parents’ preparedness for end of life [51, 53, 56, 58].
A second key finding was that complex childhood dementia phenotypes had wide-ranging psychosocial impacts on parents’ physical, emotional, social, psychological and economic wellbeing [51,52,53,54, 60]. Analysis revealed multiple domains of unmet need that impact child and parent quality of life, including neurocognitive regression, loss of communication skills, downstream cognitive-behavioral challenges, sleep disturbances, uncooperative behaviors, as well as progressive physical impairments including pain and mobility [52]. Our findings extend on global research demonstrating that rare diseases and childhood dementias impose significant economic costs far surpassing some of the costliest chronic diseases, to individual households and the broader health systems [75, 76]. Regarding psychological impacts, often, the early age of onset, and the rate of insidious decline in their child’s neurocognitive capacity hastens the demand on parent emotional and psychological adaption, resulting in intensifying psychological isolation and sequalae [77, 78]. Interestingly, although disease severity was shown to predict parents’ psychological wellbeing [55], expressions of parent resilience associated with adaptive coping strategies were highlighted across several studies, [49, 51, 58], regardless of the severity of their child’s condition [52, 64]. Our findings draw parallels with burgeoning research emphasizing the importance of accessible psychosocial resources to promote coping as more reliable predictors for parent quality of life than disease-specific factors [79, 80]. Additionally, our results lend support to national guidelines recommending the application of individually tailored applied behavioural analysis therapy as an intervention to support managing the neurobehavioral aspects of certain childhood dementia conditions [72]. Our finding that parents' psychosocial needs progress during distinct stages of their child’s condition trajectory align with broader conceptual frameworks, which attest that early and integrated healthcare and psychosocial supports are required to support parents’ evolving needs throughout the child’s lifetime [81]. Given the extensive and wide-ranging demands associated with parenting a child with dementia elicited through this research synthesis, integrated family-centred and trauma-informed psychosocial resources tailored to leverage parents’ adaptive coping skills are likely to be important empowerment tools for parents to alleviate psychological and social isolation [78, 82].
Importantly, while unprecedented progress has been achieved in understanding the cellular pathogenesis of many individually rare childhood dementia causing conditions, efficacious treatments are unavailable for the majority [83]. Currently, there are over 70 genetic disorders known to cause childhood dementia [16] and many of these conditions are detected late, adding to the high level of suffering endured by patients and their families [62]. For parents of children with rare diseases, clinical trials are often their only hope to benefit from the pipeline of therapeutic developments [84] and our review emphasized parents’ pressing desire for as broad as possible access to clinical trials and to subsequently approved therapies [52]. Further, our results highlight paediatric clinical trials targeting reduction in the rate of decline of clinical features (e.g. deteriorating motor function and mobility) offers a source of intervention that can complement pharmaceutical approaches and improve parent quality of life outcomes [52]. Collaboration and knowledge sharing achieved through rare disease initiatives has been shown to improve the quality of patient care and is of benefit to researchers, clinicians, and families alike, in considering appropriate referral pathways for available clinical trials and therapeutic interventions [85, 86]. Establishing an integrated and interdisciplinary center of expertise with a wide periphery of clinician involvement may be a strategic approach to assist parents and clinicians in several ways. First, it would facilitate information flow to circumvent the obstacles parents and clinicians face in accessing information, and clinical trials [87]. Secondly, the center could prove advantageous for connecting families to appropriate community-based services, to alleviate social and psychological isolation and to empower families to cope with the uncertainty of their child’s rare and progressive condition [48]. Thirdly, a centralized and interdisciplinary center of expertise engaging informed decision-makers, parents, and clinician researchers would provide a sustainable platform that is conductive to social influence to drive awareness and advocacy to address the shared unmet needs of children and families [88, 89].
Strengths and limitations
While the findings of this review provide valuable information to accelerate the development of enhanced healthcare and psychosocial resources for families, there are limitations. First, the review contained only articles published in English and hence, additional studies might have been overlooked. Although the review included studies from multiple countries, the experiences and needs of parents in low- and middle-income countries; and those from remote regions, lower socioeconomic and culturally and linguistically diverse populations were underrepresented [90]. Research to understand how we can develop and provide healthcare services for families in low- and middle-income countries is crucial to develop culturally appropriate resources which are aligned to their specific needs [91]. Equally, other priority populations include those from remote regions, lower socioeconomic background and that are Indigenous or otherwise culturally and linguistically diverse [92].
This research was carried out by a cross-disciplinary team whose members contributed a broad and diverse knowledge base. A potential limitation of the current systematic search related to the variable and inconsistent use of terminology to define different conditions that are identified as childhood dementias. While the criteria for defining the childhood dementia diagnoses was not always clearly delineated in specific studies, the authors agreed on set inclusion criteria, as delineated in published literature prior to the data extraction process [1, 11]. Four authors engaged in decisions about inclusion/exclusion in the review, and articles were critically appraised by two authors to ensure methodological rigour and to avoid risk of bias. Additionally, the wide range of study quality and the use of different instruments to assess quality of life outcomes in the individual studies should be considered when interpreting the quantitative results. Two studies directly compared the quality of life of parents of children with a dementia with another illness conditions [56, 62] and two studies relied on population-based norms to describe parent quality of life and psychological wellbeing [57, 59]. Thirdly, few studies explicitly linked their research to a theoretical framework and only two studies reported sample size estimations and power analyses [55, 57]. Importantly, the use of validated instruments within a theory-driven framework may be a useful future approach to facilitate the development of psychosocial resources for parents that will be applicable across their child’s lifespan [93].
Future directions
As scientific understanding of childhood dementia continues to evolve, an increasing number of families will receive this diagnosis for their child. With this knowledge, streamlined access to multidisciplinary and interdisciplinary healthcare teams, including subspeciality paediatric palliative care teams should be prioritised to provide holistic healthcare and psychosocial support for children and their families [94]. While our review focussed on the impact of caring for a child with dementia from the perspective of parents, several studies acknowledged that unaffected siblings may be adversely impacted by the increased time and energy required to care for the sick child [48,49,50,51, 55]. Future research expanding on the present research is necessary to investigate the psychosocial impacts of childhood dementia conditions on siblings and to improve the depth of understanding regarding what psychosocial resources may be required to support other family members in the community [55]. This is particularly important given that siblings are often tasked with caring for their brother or sister from a young age and the physical and emotional responsibilities can become more prevalent over time as the parents age and are less able to undertake all the necessary caring responsibilities [95, 96].
Secondly, we acknowledge that clinicians can also be impacted by the professional and emotional demands of caring for children with severe and rare neurodegenerative conditions and their families [97,98,99,100]. Clinicians experience a protracted clinical care remit, navigating pervasive clinical uncertainty associated with genetic discovery and prognostication challenges, in the face of limited natural history data, and limited hopes for targeted therapeutics across time [101]. The increased complexity of health care delivery for this group of severe and complex neurodevelopmental and neurodegenerative conditions has elevated the importance of understanding the clinician experience, and for continued research to understand the natural history of childhood dementia disorders to enable clinicians to better support families [12]. Engagement with paediatric palliative care services specialised in caring for children with life-limiting conditions and their families ensures a layer of holistic consultancy support [102, 103]. Our results highlight that the need for clinician education and training in compassionate communication models about the progression of childhood dementia, as well as guidance about navigating appropriate psychosocial supports for families. Future research assessing the perceptions and psychosocial support needs of clinicians and parents collectively may help to map out what resources can be co-developed to empower clinicians to optimally care for patients and their families [104].
Conclusion
Parents’ health and social care experiences are characterised their child’s rare, life-limiting and progressively impairing childhood dementia specific complexities. Our review demonstrated that parents share a tranche of overlapping challenges, especially related to the psychiatric and behavioral impacts of their child’s cognitive regression and the perpetuating psychosocial challenges that result. Nonetheless, many parents employed adaptive coping strategies and demonstrated significant resilience. Findings highlight the need for early access to coordinated healthcare services and trauma-informed integrated psychosocial supports to alleviate parent psychological distress. The unifying focus on the collective lived experiences of parents underscores the urgent need to increase awareness of the impact of childhood dementias among all stakeholders, to drive investment, integrated services, and interventional research.
Availability of data and materials
The author confirms that all data analysed and generated during this study are included in this published article. Furthermore, the secondary sources and data supporting the findings of this study were all publicly available at the time of submission. One can obtain the relevant materials from the references below.
References
Nunn K, Williams K, Ouvrier R. The australian childhood dementia study. Eur Child Adolesc Psychiatry. 2002;11(2):63–70.
Chin SJ, Fuller M. Prevalence of lysosomal storage disorders in Australia from 2009 to 2020. The Lancet Regional Health–Western Pacific. 2022;19.
El-Beshlawy A, Tylki-Szymanska A, Vellodi A, Belmatoug N, Grabowski GA, Kolodny EH, et al. Long-term hematological, visceral, and growth outcomes in children with Gaucher disease type 3 treated with imiglucerase in the International Collaborative Gaucher Group Gaucher Registry. Mol Genet Metab. 2017;120(1–2):47–56.
Stirnemann J, Vigan M, Hamroun D, Heraoui D, Rossi-Semerano L, Berger MG, et al. The French Gaucher’s disease registry: clinical characteristics, complications and treatment of 562 patients. Orphanet J Rare Dis. 2012;7:1–13.
Ahern S, Sims G, Earnest A, Scott C. Optimism, opportunities, outcomes: the Australian Cystic Fibrosis Data Registry. Intern Med J. 2018;48(6):721–3.
Massie RJH, Curnow L, Glazner J, Armstrong DS, Francis I. Lessons learned from 20 years of newborn screening for cystic fibrosis. Med J Aust. 2012;196(1):67–70.
Verity C, Baker E, Maunder P, Pal S, Winstone AM. Differential diagnosis of progressive intellectual and neurological deterioration in children. Dev Med Child Neurol. 2021;63(3):287–94.
Stromme P, Kanavin OJ, Abdelnoor M, Woldseth B, Rootwelt T, Diderichsen J, et al. Incidence rates of progressive childhood encephalopathy in Oslo, Norway: a population based study. BMC Pediatr. 2007;7(1):1–8.
Uvebrant P, Lanneskog K, Hagberg B. The epidemiology of progressive encephalopathies in childhood I. Live birth prevalence in West Sweden. Neuropediatrics. 1992;23(04):209–11.
Warmerdam HA, Termeulen-Ferreira EA, Tseng LA, Lee JY, van Eeghen AM, Ferreira CR, et al. A scoping review of inborn errors of metabolism causing progressive intellectual and neurologic deterioration (PIND). Front Neurol. 2020;10:1369.
Djafar JV, Johnson AM, Elvidge KL, Farrar MA. Childhood Dementia: a collective clinical approach to advance therapeutic development and care. Pediatr Neurol. 2022;139:76–85.
Garbade SF, Zielonka M, Komatsuzaki S, Kölker S, Hoffmann GF, Hinderhofer K, et al. Quantitative retrospective natural history modeling for orphan drug development. J Inherit Metab Dis. 2021;44(1):99–109.
Hoover-Fong J, Shah S, Van Hove J, Applegarth D, Toone J, Hamosh A. Natural history of nonketotic hyperglycinemia in 65 patients. Neurology. 2004;63(10):1847–53.
Mignot C, Doummar D, Maire I, De Villemeur TB, Group FTGDS. Type 2 Gaucher disease: 15 new cases and review of the literature. Brain and Development. 2006;28(1):39–48.
Anderson A, Wong K, Jacoby P, Downs J, Leonard H. Twenty years of surveillance in Rett syndrome: What does this tell us? Orphanet J Rare Dis. 2014;9:1–9.
Childhood Dementia In Australia: Quantifying The Burden On Patients, Carers, The Healthcare System And Our Society. [Internet]. THEMA Consulting Report. 2020. (accessed June 2022). Available from: https://www.childhooddementia.org/burdenstudy.
Smits RM, Vissers E, Te Pas R, Roebbers N, Feitz WF, van Rooij IA, et al. Common needs in uncommon conditions: a qualitative study to explore the need for care in pediatric patients with rare diseases. Orphanet J Rare Dis. 2022;17(1):1–9.
Monaco L, Zanello G, Baynam G, Jonker AH, Julkowska D, Hartman AL, et al. Research on rare diseases: ten years of progress and challenges at IRDiRC. Nat Rev Drug Discovery. 2022;21(5):319–20.
Haugen P, von Tetzchner S, Oxley J, Elmerskog B. Dementia in Adulthood and Childhood. In: von Tetzchner S, Elmerskog B, Tøssebro A-G, Rokne S, editors. Juvenile Neuronal Ceroid Lipofuscinosis, Childhood Dementia and Education: Intervention, education and learning strategies in a lifetime perspective Norway: Snøfugl: Forlag; 2019. p. 76.
Bose M, Yergeau C, D’souza Y, Cuthbertson DD, Lopez MJ, Smolen AK, et al. Characterization of severity in Zellweger spectrum disorder by clinical findings: a scoping review, meta-analysis and medical chart review. Cells. 2022;11(12):1891.
Lang FM, Korner P, Harnett M, Karunakara A, Tifft CJ. The natural history of Type 1 infantile GM1 gangliosidosis: a literature-based meta-analysis. Mol Genet Metab. 2020;129(3):228–35.
Lal TR, Seehra GK, Steward AM, Poffenberger CN, Ryan E, Tayebi N, et al. The natural history of type 2 Gaucher disease in the 21st century: a retrospective study. Neurology. 2020;95(15):e2119–30.
Platt FM, d’Azzo A, Davidson BL, Neufeld EF, Tifft CJ. Lysosomal storage diseases. Nat Rev Dis Primers. 2018;4(1):27.
Dyken P, Krawiecki N. Neurodegenerative diseases of infancy and childhood. Annals Neurology Offl J Am Neurol Assoc Child Neurol Soc. 1983;13(4):351–64.
Nunn K, Williams K, Ouvrier R. The Australian childhood dementia study. J Eur Child Adolesc Psychiatry. 2002;11(2):63–70.
Shapiro E, Lourenco CM, Mungan NO, Muschol N, O’Neill C, Vijayaraghavan S. Analysis of the caregiver burden associated with Sanfilippo syndrome type B: panel recommendations based on qualitative and quantitative data. Orphanet J Rare Dis. 2019;14(1):168.
Palacios-Ceña D, Famoso-Pérez P, Salom-Moreno J, Carrasco-Garrido P, Pérez-Corrales J, Paras-Bravo P, et al. “Living an obstacle course”: a qualitative study examining the experiences of caregivers of children with Rett syndrome. Int J Environ Res Public Health. 2019;16(1):41.
Wu Y, Al-Janabi H, Mallett A, Quinlan C, Scheffer IE, Howell KB, et al. Parental health spillover effects of paediatric rare genetic conditions. Qual Life Res. 2020;29(9):2445–54.
Nevin SM, McLoone J, Wakefield CE, Kennedy SE, McCarthy HJ. Genetic testing in the pediatric nephrology clinic: understanding families’ experiences. J Pediatr Genet. 2020;11:117–25.
Nevin SM, Wakefield CE, Schilstra CE, McGill BC, Bye A, Palmer EE. The information needs of parents of children with early-onset epilepsy: a systematic review. Epilepsy Behav. 2020;112:107382.
EURORDIS survey results voice concerns over the subpar healthcare experience of people living with a rare disease [press release]. 03/02/2021 2021.
Wiegand-Grefe S, Liedtke A, Morgenstern L, Hoff A, Csengoe-Norris A, Johannsen J, et al. Health-Related Quality of Life and mental health of families with children and adolescents affected by rare diseases and high disease burden: the perspective of affected children and their siblings. BMC Pediatr. 2022;22(1):1–9.
Boettcher J, Boettcher M, Wiegand-Grefe S, Zapf H. Being the pillar for children with rare diseases-a systematic review on parental quality of life. Int J Environ Res Public Health. 2021;18(9):4993.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
PROSPERO International Prospective Register of Systematic Reviews. Available at: https://www.crd.york.ac.uk/prospero/. Accessed July 2022.
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014;14(1):1–10.
Guerrini R. Epilepsy in children. Lancet. 2006;367(9509):499–524.
Ono T, Galanopoulou AS. Epilepsy and epileptic syndrome. In: Neurodegenerative diseases. New York: Springer; 2012. p. 99–113.
Bernasconi N. Is epilepsy a curable neurodegenerative disease? Brain. 2016;139(9):2336–7.
Childhood Dementia Initiative. Childhood Dementia: The case for urgent action (white paper). Sydney: Childhood Dementia Initiative; 2020.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Moher D, Altman DG, Liberati A, Tetzlaff J. PRISMA statement. Epidemiology. 2011;22(1):128.
Kmet LM, Cook LS, Lee RC. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. 2004.
Elo S, Kyngas H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15.
Munn Z, Stern C, Aromataris E, Lockwood C, Jordan Z. What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med Res Methodol. 2018;18(1):1–9.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S. Guidance on the conduct of narrative synthesis in systematic reviews. Prod ESRC Methods Prog Version. 2006;1(1):b92.
Amir Yazdani P, St-Jean ML, Matovic S, Spahr A, Tran LT, Boucher RM, et al. Experience of Parents of Children with Genetically Determined Leukoencephalopathies Regarding the Adapted Health Care Services During the COVID-19 Pandemic. Journal of Child Neurology. 2022;37:237–45.
Bose M, Mahadevan M, Schules DR, Coleman RK, Gawron KM, Gamble MB, et al. Emotional experience in parents of children with Zellweger spectrum disorders: a qualitative study. Mol Genet Metab Rep. 2019;19:100459.
Somanadhan S, Larkin PJ. Parents’ experiences of living with, and caring for children, adolescents and young adults with Mucopolysaccharidosis (MPS). Orphanet J Rare Dis. 2016;11(1):138.
Eichler FS, Cox TM, Crombez E, Dali CI, Kohlschutter A. Metachromatic leukodystrophy: an assessment of disease burden. J Child Neurol. 2016;31(13):1457–63.
Krantz M, Malm E, Darin N, Sofou K, Savvidou A, Reilly C, et al. Parental experiences of having a child with CLN3 disease (juvenile Batten disease) and how these experiences relate to family resilience. Child Care Hlth Dev. 2022;48:842–51.
Porter KA, O’Neill C, Drake E, Parker S, Escolar ML, Montgomery S, et al. Parent experiences of sanfilippo syndrome impact and unmet treatment needs: a qualitative assessment. Neurol Ther. 2021;10(1):197–212.
Palacios-Cena D, Famoso-Perez P, Salom-Moreno J, Carrasco-Garrido P, Perez-Corrales J, Paras-Bravo P, et al. “Living an Obstacle Course”: a qualitative study examining the experiences of caregivers of children with rett syndrome. Int J Environ Res Public Health. 2019;16(1):41.
Rozensztrauch A, Sebzda A, Smigiel R. Clinical presentation of Rett syndrome in relation to quality of life and family functioning. J Int Med Res. 2021;49(4):3000605211007714.
Needham M, Packman W, Rappoport M, Quinn N, Cordova M, Macias S, et al. MPS II: adaptive behavior of patients and impact on the family system. J Genet Couns. 2014;23(3):330–8.
Grant S, Cross E, Wraith JE, Jones S, Mahon L, Lomax M, et al. Parental social support, coping strategies, resilience factors, stress, anxiety and depression levels in parents of children with MPS III (Sanfilippo syndrome) or children with intellectual disabilities (ID). J Inherit Metab Dis. 2013;36(2):281–91.
Dermer E, Spahr A, Tran LT, Mirchi A, Pelletier F, Guerrero K, et al. Stress in parents of children with genetically determined leukoencephalopathies: a pilot study. J Child Neurol. 2020;35(13):901–7.
Hoffmann F, Hoffmann S, Kunzmann K, Ries M. Challenging behavior in mucopolysaccharidoses types I-III and day-to-day coping strategies: a cross sectional explorative study. Orphanet J Rare Dis. 2020;15(1):275.
Conijn T, Nijmeijer SC, van Oers HA, Wijburg FA, Haverman L. Psychosocial functioning in parents of MPS III patients. In: JIMD Reports, Volume 44. Berlin: Springer; 2018. p. 33–41.
Kuratsubo I, Suzuki Y, Shimozawa N, Kondo N. Parents of childhood X-linked adrenoleukodystrophy: high risk for depression and neurosis. Brain Dev. 2008;30(7):477–82.
Varvogli L, Waisbren SE. Personality profiles of mothers of children with mitochondrial disorders. J Inherit Metab Dis. 1999;22(5):615–22.
Ammann-Schnell L, Groeschel S, Kehrer C, Frolich S, Krageloh-Mann I. The impact of severe rare chronic neurological disease in childhood on the quality of life of families-a study on MLD and PCH2. Orphanet J Rare Dis. 2021;16(1):211.
Killian JT Jr, Lane JB, Lee HS, Pelham JH, Skinner SA, Kaufmann WE, et al. Caretaker quality of life in Rett syndrome: disorder features and psychological predictors. Pediatr Neurol. 2016;58:67–74.
Lamb AE, Biesecker BB, Umstead KL, Muratori M, Biesecker LG, Erby LH. Family functioning mediates adaptation in caregivers of individuals with Rett syndrome. Patient Educ Couns. 2016;99(11):1873–9.
Mori Y, Downs J, Wong K, Leonard H. Longitudinal effects of caregiving on parental well-being: the example of Rett syndrome, a severe neurological disorder. Eur Child Adolesc Psychiatry. 2019;28(4):505–20.
Eisengart JB, King KE, Shapiro EG, Whitley CB, Muenzer J. The nature and impact of neurobehavioral symptoms in neuronopathic Hunter syndrome. Mol Genet Metab Rep. 2020;22:100549.
Malcolm C, Hain R, Gibson F, Adams S, Anderson G, Forbat L. Challenging symptoms in children with rare life-limiting conditions: findings from a prospective diary and interview study with families. Acta Paediatr. 2012;101(9):985–92.
Senger BA, Ward LD, Barbosa-Leiker C, Bindler RC. The parent experience of caring for a child with mitochondrial disease. J Pediatr Nurs. 2016;31(1):32–41.
Mirchi A, Pelletier F, Tran LT, Keller S, Braverman N, Tonduti D, et al. Health-related quality of life for patients with genetically determined leukoencephalopathy. Pediatr Neurol. 2018;84:21–6.
Scharpen AL, Stille CJ. From strangers in a foreign land to active, engaged citizens. Pediatrics. 2018;141(2):e20171845.
Ekberg S, Bowers A, Bradford N, Ekberg K, Rolfe M, Howard C, et al. Paediatric Palliative Care National Action Plan Project: Background Literature Review. 2021.
Muschol N, Giugliani R, Jones SA, Muenzer J, Smith NJ, Whitley CB, et al. Sanfilippo syndrome: consensus guidelines for clinical care. Orphanet J Rare Dis. 2022;17(1):1–23.
Burns KH, Casey PH, Lyle RE, Bird TM, Fussell JJ, Robbins JM. Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126(4):638–46.
Bradford N, Herbert A, Mott C, Armfield N, Young J, Smith A. Components and principles of a pediatric palliative care consultation: results of a Delphi study. J Palliat Med. 2014;17(11):1206–13.
Yang G, Cintina I, Pariser A, Oehrlein E, Sullivan J, Kennedy A. The national economic burden of rare disease in the United States in 2019. Orphanet J Rare Dis. 2022;17(1):1–11.
Wu Y, Al-Janabi H, Mallett A, Quinlan C, Scheffer IE, Howell KB, et al. Parental health spillover effects of paediatric rare genetic conditions. Qual Life Res. 2020;29(9):2445–54.
Wong MG, Heriot SA. Vicarious futurity in autism and childhood dementia. J Autism Dev Disord. 2007;37(10):1833–41.
Carmassi C, Dell’Oste V, Foghi C, Bertelloni CA, Conti E, Calderoni S, et al. Post-traumatic stress reactions in caregivers of children and adolescents/young adults with severe diseases: a systematic review of risk and protective factors. Int J Environ Res Public Health. 2021;18(1):189.
Bryson BA, Bogart KR. Social support, stress, and life satisfaction among adults with rare diseases. Health Psychol. 2020;39(10):912–20.
Ernst MM, Marino BS, Cassedy A, Piazza-Waggoner C, Franklin RC, Brown K, et al. Biopsychosocial predictors of quality of life outcomes in pediatric congenital heart disease. Pediatr Cardiol. 2018;39(1):79–88.
Nevin SM, Wakefield CE, Barlow-Stewart K, Mcgill BC, Bye A, Palmer EE, et al. Psychosocial impact of genetic testing on parents of children with developmental and epileptic encephalopathy. Dev Med Child Neurol. 2022;64(1):95–104.
Cousineau TM, Hobbs LM, Arthur KC. The role of compassion and mindfulness in building parental resilience when caring for children with chronic conditions: a conceptual model. Front Psychol. 2019;10:1602.
Kaufmann P, Pariser AR, Austin C. From scientific discovery to treatments for rare diseases–the view from the National Center for Advancing Translational Sciences-Office of Rare Diseases Research. Orphanet J Rare Dis. 2018;13(1):1–8.
Wright CF, FitzPatrick DR, Firth HV. Paediatric genomics: diagnosing rare disease in children. Nat Rev Genet. 2018;19(5):253.
Crocker JC, Ricci-Cabello I, Parker A, Hirst JA, Chant A, Petit-Zeman S, et al. Impact of patient and public involvement on enrolment and retention in clinical trials: systematic review and meta-analysis. BMJ. 2018;363:k4738.
Black AP, Baker M. The impact of parent advocacy groups, the Internet, and social networking on rare diseases: the IDEA League and IDEA League United Kingdom example. Epilepsia. 2011;52(Suppl 2):102–4.
Forman J, Taruscio D, Llera VA, Barrera LA, Coté TR, Edfjäll C, et al. The need for worldwide policy and action plans for rare diseases. Acta Paediatr. 2012;101(8):805–7.
Juando-Prats C, James E, Bilder DA, McNair L, Kenneally N, Helfer J, et al. DRAVET ENGAGE. Parent caregivers of children with Dravet syndrome: Perspectives, needs, and opportunities for clinical research. Epilepsy Behav. 2021;122:108198.
Radu R, Hernandez-Ortega S, Borrega O, Palmeri A, Athanasiou D, Brooke N, et al. Global collaborative social network (Share4Rare) to promote citizen science in rare disease research: platform development study. JMIR Form Res. 2021;5(3):e22695.
Organization WH. Optimizing brain health across the life course: WHO position paper. 2022.
Stoner CR, Lakshminarayanan M, Durgante H, Spector A. Psychosocial interventions for dementia in low-and middle-income countries (LMICs): a systematic review of effectiveness and implementation readiness. Aging Ment Health. 2021;25(3):408–19.
D’Angelo CS, Hermes A, McMaster CR, Prichep E, Richer É, Van der Westhuizen FH, et al. Barriers and considerations for diagnosing rare diseases in Indigenous populations. Front Pediatr. 2020;8:579924.
Richardson A, Pedley G, Pelone F, Akhtar F, Chang J, Muleya W, et al. Psychosocial interventions for people with young onset dementia and their carers: a systematic review. Int Psychogeriatr. 2016;28(9):1441–54.
Bhattacharya K, Millis N, Jaffe A, Zurynski Y. Rare diseases research and policy in Australia: on the journey to equitable care. J Paediatr Child Health. 2021;57(6):778–81.
Ce L, Burke MM. Caregiving roles of siblings of adults with intellectual and developmental disabilities: a systematic review. J Policy Pract Intell Disabil. 2018;15(3):237–46.
Kelada L, Wakefield CE, Drew D, Ooi CY, Palmer EE, Bye A, et al. Siblings of young people with chronic illness: caring responsibilities and psychosocial functioning. J Child Health Care. 2022;26(4):581–96.
Skirrow P, Hatton C. “Burnout” amongst direct care workers in services for adults with intellectual disabilities: a systematic review of research findings and initial normative data. J Appl Res Intellect Disabil. 2007;20(2):131–44.
Rousseau MC, Baumstarck K, Leroy T, Khaldi-Cherif C, Brisse C, Boyer L, et al. Impact of caring for patients with severe and complex disabilities on health care workers’ quality of life: determinants and specificities. Dev Med Child Neurol. 2017;59(7):732–7.
Yates M, Samuel V. Burnout in oncologists and associated factors: a systematic literature review and meta-analysis. Eur J Cancer Care. 2019;28(3):e13094.
Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of burnout among physicians a systematic review. Jama-J Am Med Assoc. 2018;320(11):1131–50.
Elliott EJ, Zurynski YA. Rare diseases are a “common” problem for clinicians. Aust Fam Physician. 2015;44(9):630–3.
Van der Steen JT, Onwuteaka-Philipsen BD, Knol DL, Ribbe MW, Deliens L. Caregivers’ understanding of dementia predicts patients’ comfort at death: a prospective observational study. BMC Med. 2013;11(1):1–12.
Chan D, Livingston G, Jones L, Sampson EL. Grief reactions in dementia carers: a systematic review. Int J Geriatr Psychiatry. 2013;28(1):1–17.
Jaffe A, Zurynski Y, Beville L, Elliott E. Call for a national plan for rare diseases. J Paediatr Child Health. 2010;46(1–2):2–4.
Acknowledgements
Not applicable for this section.
Funding
This study was funded by the Childhood Dementia Initiative. Prof Wakefield is supported by the National Health and Medical Research Council of Australia (APP2008300). Dr Kelada is supported by the Golda Meir Post-Doctoral Fellowship Fund. M Farrar is supported by the National Health and Medical Research Council of Australia (APP1194940). Dr Signorelli is supported by a Cancer Institute NSW Early Career Fellowship (2020/ECF1144).
Author information
Authors and Affiliations
Contributions
SMN, CW, LK, KN, KE, MM, GH developed the study concept and initiated the project. SMN, BM, KE, MF, CW contributed to the design and development of the protocol. SMN, BM, KE, MF, LK completed the data screening and article selection process. SMN was responsible for the writing this manuscript. BM, LK, GH, MM, KE, MF, GB, NK, LD, SG, CS, KB, KN, CW were responsible for reviewing the manuscript and providing feedback. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable for this study.
Consent for publication
All authors have approved the final manuscript and provided consent for publication.
Competing interests
Gail Hilton is the Head of Programs at the Childhood Dementia Initiative Foundation. Megan Maack is the Chief Executive Officer at the Childhood Dementia Initiative Foundation. Kris Elvidge is the Head of Research at the Childhood Dementia Initiative Foundation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1 Database search terms. Tables S2 and S3 Quality analysis summary scores for qualitative articles.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nevin, S.M., McGill, B.C., Kelada, L. et al. The psychosocial impact of childhood dementia on children and their parents: a systematic review. Orphanet J Rare Dis 18, 277 (2023). https://doi.org/10.1186/s13023-023-02859-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-023-02859-3