Abstract
Sternal wound infection (SWI) is the most common complication of the median sternal incision. The treatment time is long, and the reconstruction is difficult, which causes challenges for surgeons. Plastic surgeons were often involved too late in such clinical scenarios when previous empirical treatments failed and the wound damage was relatively serious. Accurate diagnosis and risk factors against sternal wound infection need to be in focus. Classification of different types of sternotomy complications post-cardiac surgery is important for specific categorization and management. Not familiar with this kind of special and complex wound, objectively increasing the difficulty of wound reconstruction. The purpose of this comprehensive review is to review the literature, introduce various SWI risk factors related to wound nonunion, various classification characteristics, advantages and disadvantages of various wound reconstruction strategies, to help clinicians understand the pathophysiological characteristics of the disease and choose a better treatment method.
Similar content being viewed by others
Introduction
As early as 1957, the median sternal incision was first reported for open-heart surgery, which has become the standard surgical approach for thoracic and cardiac surgery [1]. As one of the common complications, SWI has been gradually taken seriously. It has been reported that the incidence rate of SWI is 1%~5%. Severe cases can lead to heart, lung, and kidney-related organ failure and even death. The mortality rate is 10%~30%2. In the United States, about 700,000 open heart operations are performed every year, and nearly 8300 patients develop sternal incision infections [3]. The long-term non-healing of the wound, repeated debridement, and failure of wound closure bring huge mental pressure to the patients, affect the quality of life, prolong the hospital stay, bring high costs, and increase the economic burden of the patients. There are many risk factors for sternotomy complications, including age, body mass index, smoking, and complications such as low immunity, diabetes, radiation, reoperation, and chronic lung and kidney diseases [4]. SWI can be classified as the surgical incision infection, mainly occurring within one month after cardiac surgery. It can be divided into two types according to the level and depth of the infection. Superficial sternal wound infection (SSWI) only accumulates on the skin, subcutaneous tissue, and deep fascia, while deep sternal wound infection (DSWI) can affect muscle tissue, sternum, sub sternum, and mediastinum. Other scholars believe that SSWI accumulates skin and subcutaneous tissue, and chest muscle tissue, while DSWI is mainly a mediastinal infection [5]. It should be noted that the mortality of mediastinal infection is very high, which still remains as high as 3% ~ 35%6. SSWI can be corrected by having debridement and direct closure of the wound edge. DSWI refers to the correction of complex defects, and there are various methods including greater omentum, tissue flap, platelet-rich plasma (PRP), and so on. There is no standard treatment method currently.
Diagnostic procedures
Diagnosis
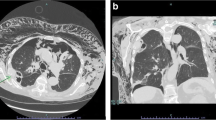
Sternal wound infection, also known as post-thoracotomy infection nonunion or median sternal incision infection, refers to the infection of soft tissue and/or sternum, ribs, costal cartilage, and mediastinum under the influence of local or systemic factors after median sternal incision. DSWI wounds are limited to the deep fascia and are easier to diagnose. Whereas DSWI, according to the Centers for Disease Control and Prevention (CDC), DSWI can be confirmed by the presence of skin redness and swelling, increased skin temperature, fever (> 38℃), pain, and other infectious symptoms accompanied by purulent secretions, supplemented by etiological and pathological evidence after the median thoracic incision in thoracic and cardiac surgery. According to the clinical manifestation, with X-ray, CT, and other medical film examinations, it is found that mediastinal widening, mediastinal gas-liquid level, mediastinal emphysema, pleural effusion, and wire displacement have value in early DSWI diagnosis, and CT shows a better effect [7,8,9,10,11].
Auxiliary diagnosis
In clinical practice, we found that chest X-ray films are not helpful for the diagnosis of mediastinitis. Because there are many metal internal fixators in the body of patients undergoing cardiac surgery, MRI, which has better imaging of soft tissue, cannot be used, after admission, each patient should preferably undergo a chest CT examination before debridement. Determine the “stability of the sternum” to facilitate more thorough debridement and prepare for subsequent wound closure treatment. However, a CT examination is also insufficient. It is reported that its ability to identify costochondritis is very limited. Cardiac surgery patients often have metal internal fixators, and MRI, which is better for soft tissue filming, cannot be used. But the studies have shown that the sensitivity and specificity of PET/CT were higher than that of CT. In the CT diagnosis of patients with costochondritis complicated by DSWI, the sensitivity and specificity of senior radiologists were 87.6% and 56.9%, which were far less than that of PET/CT. PET/CT can effectively reduce the dependence of clinicians on film readers and reduce the occurrence of missed diagnoses [12,13,14]. The bacterial culture of wound secretions is a necessary indicator for formulating anti-infection plans, wound classification, and formulating treatment plans, but there are occasional false negatives. Nick et al. using classical microbial culture, FISH combined with molecular nucleic acid amplification technology (FISHseq) to analyze specimens from 12 patients, found that microbial biofilms did not always exist in DSWI wounds, but the microorganisms were “plaque-like” in the tissue distributed Therefore, deep excision of the wound must be carried out to control the infection [15]. It is suggested that culture analysis should be carried out on at least two wound samples from different locations, and FISHseq should be used for additional molecular biological analysis when it is difficult to explain.
Risk factors
Risk factors for sternotomy wound complications include: patient-related risk factors were obesity, advanced age, active smoking, diabetes, coronary artery disease, low ejection fraction, steroid treatment, chronic infections, innutrition, kidney disease, and chronic lung disease. Procedure-related risk factors were inadequate skin preparation, use of bone wax, emergency operation, nonskeletonized (pedicled) or bilateral harvesting of the internal mammary artery (IMA), blood product infusion, prolonged operative time and perfusion time, sternal rewiring, postoperative bleeding, use of an intra-aortic balloon pump, extensive use of electrocautery, and antibiotic administration [8, 11]. Some risk factors can not only increase the SWI incidence but also lead to the wound that is hard to heal.
Old people are the main population of thoracotomy [16]. Age is an independent risk factor for surgical incision infection. The risk of wound infection is directly proportional to age. Affected by poor tissue regeneration ability and existing systemic diseases, the old people have poor wound healing and are more prone to infection [17, 18]. According to the range of body mass index specified by the World Health Organization (WHO), obesity refers to BMI > 30 kg / m2, and China’s standard for obesity is BMI > 28 kg / m2. Engelman et al. [19] reported that obese patient with BMI > 30 kg / m2 were more likely to develop sternal incision infection and great saphenous vein incision infection than those with BMI < 30 kg/m2. The mechanism is adipocyte hypertrophy, cellular hypoxia, dysfunction of adipocytokines, increased vascular permeability, promoting immune cell infiltration into adipose tissue, releasing more inflammatory factors, and forming a vicious circle of the inflammatory response, leading to the persistence of a chronic inflammatory state [20]. In addition, thicker subcutaneous fat, larger body surface area, higher skin tension, and poor subcutaneous blood supply and lymphatic function in obese patients will also seriously affect surgical wound healing [21].
Diabetes or long-term hyperglycemia can lead to a local high glucose environment, accumulation of advanced glycation end products, microcirculatory disturbance, insufficient tissue oxygen supply, increased repair cell apoptosis, and metabolic and immune system defense dysfunction, resulting in an increased risk of infection and delayed wound healing. The absolute or relative lack of insulin in the body will form a continuous hyperglycemia state. Animal experiments showed that the sugar content of the skin tissue in diabetic mice increased, and the blood sugar level was related to skin incision. Wound healing was delayed significantly. PGP9.5IR innervation was significantly reduced, the capillary network decreased and NGF receptor expression decreased. Molecular regulation of hypoxia-related genes (HIF1A, Flt1, and KDR) is impaired, while extracellular matrix coding genes (ITGB3, TIMP1, Fn1, COL4a1) are up-regulated due to hyperglycemia and lesions [22]. Viola et al. [23] reported that in obese and diabetic patients, the number of regulatory T lymphocytes and M2 macrophages with anti-inflammatory phenotype decreased, the production of inflammatory cytokines in adipose tissue decreased, and the normal inflammation / anti-inflammatory balance was destroyed, leading to chronic inflammation. In addition, smoking and lung disease are also independent risk factors of SWI. Long-term smoking will decrease the concentration of immunoglobulin, inhibit the activity of lysozyme, reduce the number of NK cells, CD3 +, CD4 +, CD8 +, T cells, reduce the immune function, and lead to respiratory edema, increase sputum production, pulmonary infections, and even COPD [24]. Smoking, pulmonary inflammation, and COPD can cause repeated coughing, resulting in repeated friction activities at the broken end of the sternum, increasing the contact force of the fixed steel wire, and increasing the probability of sternal cracking and steel wire fracture. This situation is conducive to bacterial colonization, causing sternal necrosis and infection in the operation area, significantly increasing the probability of non-healing, and seriously affecting the quality of recovery after wound closure after debridement. Immune dysfunction is an important cause of vasculitis. Inflammation of the vascular wall will cause inflammatory cell infiltration, thickening of the vascular wall, and destruction of the vascular inner layer, narrowing or even obstruction of the vascular cavity, affecting the microcirculation and blood supply of the wound, causing a series of skin problems and the delayed wound healing for a long time. Inhibins are often used to fight immune dysfunction. Statin drugs are often used to fight immune dysfunction. However, glucocorticoid is a “double-edged sword”. It has strong immunosuppressive effects, resulting in osteoporosis and fungal infection. Fungal infection is an important factor in causing mediastinal infection [4, 25]. Patients with renal insufficiency will aggravate tissue edema, accompanied by malnutrition, anemia, and decreased immunity, which will reduce the efficiency of wound healing and aggravate the possibility of infection. It also aggravates the burden on the heart, reduces the patient’s tolerance to the surgery, interferes with the doctor’s choice of surgical strategy, reduces the effect of the debridement, and objectively increases the number of debridements [26]. Malnutrition causes additional difficulties in the debridement and reconstruction of SWI. In patients with hypoproteinemia and anemia, insufficient protein synthesis, reduction in the number of red blood cells, and insufficient oxygen-carrying capacity lead to hypoxia, slow cell regeneration, a decline in the number and function of inflammatory cells and immune cells, cause tissue edema, obstruction of granulation tissue and collagen fiber formation, and finally delay wound healing and increase the risk of infection [27]. In addition, we found in clinical practice that coagulation status also plays an important role in the occurrence and repair of SWI, which needs further clinical research. To sum up, we believe that paying attention to the adverse effects of risk factors on wound healing in advance and taking corresponding measures to intervene is the key to increase the first-stage wound healing rate and improve the efficacy of wound reconstruction.
Clinical classification
At present, wound classification has been used to guide the treatment of SWI for a long time in clinical practice. After reviewing the literature, we found that the classification methods are various and cumbersome, and they are not uniform. This may be one of the important reasons for the current wound reconstruction methods are not uniform.
Early classification mostly used the time, depth of infection and its relationship with risk factors as the starting point to classify WSI. Early in 1984, PaiRoler et al. [28] divided SWI into three types according to the time of wound infection; Type I: incision rupture/cracking, serous exudation, sternal instability, no osteomyelitis/costochondritis within a few days (7 days) after the operation; Type II: purulent secretion with cellulitis, osteomyelitis, mediastinitis, exposed steel wire, and positive bacterial culture within a few weeks (2–6 weeks) after the operation; Type III: chronic sinus and chronic osteomyelitis are formed within months/years (6 weeks-6 years) after the operation, but mediastinitis is rare (Table 1). In order to further refine the diagnosis of DSWI and improve the treatment effect, El Oakley et al. [29] proposed a new classification and gave corresponding treatment suggestions in 1996. On the basis of the original DSWI classification, they were classified into four new subtypes based on the time of first presentation, the presence or absence of risk factors, and whether previous attempts at treating the condition have failed (Table 2). Mekontso et al. [6] divided DSWI into two types according to the onset time, Early-onset: the onset time is less than 14 days; Late-onset: more than 14 days. Gao et al. [30] In view of the complexity of SWI domestically and internationally, and no relevant reports of uninfected SWI were found, divided into three types according to whether it was infected or not, Type I: Unhealing Wound, no infection; Type IIA: Unhealing Wound, shallow infection (extraperiosteal); Type IIB: deep infection (mediastinal infection, osteomyelitis); Type III: deep sinus with localized osteomyelitis and mediastinal foreign body.
Jones et al. [31] reported the first classification based on the affected anatomical structure, superficial to deep, looking at sternal stability and the presence of septicemia, and advocated single-stage debridement and closure to reduce the number and time of treatment (Table 3). Greig et al. [32] recognized that when the wound extends below the attachment point of the lower edge of the pectoralis major muscle, it is more difficult to reconstruct the lower part. In order to facilitate the treatment and reconstruction of DSWI, according to the lower margin of the pectoralis major muscle and indicating the type of reconstruction necessary for the management of deep sternal infection and dehiscence (Table 4). Rupprecht and Schmid et al. [33] classified DSWI into 3 types according to the degree of infection and sternal damage, and recommend appropriate treatment options.(Table 5). Van Wingerden proposed a classification of post-sternotomy mediastinitis, looking mainly at sternal stability, sternal bone viability, and stock, including management for the first time [34]. Based on meta-analysis and evidence-based reconstructive procedures, the authors summarized different treatment proposals and divided them into different subtypes. For example, Type I supports wound treatment through the application of negative pressure wound treatment (NPWT). In Type II, IIa can directly seal the wound without conservative treatment; IIb requires delayed closure. IIIa uses steel wire or steel plate to seal the sternum and is supplemented by NPWT; IIIb needs to be covered with a tissue flap after sternal closure. IVa needs to be repaired with myocutaneous flap after debridement; IVb was mostly closed by greater omentum; IVb uses two methods at the same time (Table 6). Anger et al. [35] improved the previous typing method (Jones and Greig), Type I refers to skin and soft tissue infection, Type II refers to sternum and rib exposure, Type III refers to sternum and rib defect, and Type IV refers to mediastinum exposure, according to the lower edge of pectoralis major muscle as a reference, determine whether it is partial or complete relative to its vertical range, and finally determine whether its position is higher or lower (Table 7).
Plastic surgeons have referred to and summarized the original classification method and Schiraldi’s new treatment process, improved the existing classification method from the perspective of plastic surgeons, and proposed a treatment plan that is convenient for plastic surgeons to repair the closure [11]. (Table 8). In addition to the above-recognized classification methods, there are also various classification methods that are based on the material of coronary artery graft, sternal stability, prognosis, basic diseases, the morphology of bone nonunion, etc [36, 37]. To sum up, we can see that the early classification focuses on the time of infection and the influence of risk factors; the later classification focuses on the damage to anatomical structures but ignores the influence of risk factors on wound healing, and some classifications only focus on the classification of DSWI, while ignoring SSWI.
Management
At present, there is no standard scheme for the treatment of SWI. Clinicians can choose different treatment methods according to different classification methods, mainly including several major directions: infection control, general drainage, and wound reconstruction. Although it is impossible to unify the treatment plan for wound reconstruction, two basic principles must be followed, namely, the control of infection and the treatment of sternal instability/defect. New treatment methods have been proposed continuously, each has advantages and disadvantages.
Eliminate infection
Regardless of the classification of treatment, wound debridement and unobstructed drainage are the primary treatment for infection control [39]. If the necrotic tissue and foreign bodies in the wound were not completely removed, the forced closure of the wound would increase the chance of wound nonunion and recurrence. The long-term effect of this adverse result would result in larger wound defect and heavier infection, thus increasing the difficulty of wound reconstruction. Wound debridement only has a certain therapeutic effect on early low-grade wounds; however, the DSWI with complex wound situations has little effect and the drainage effect is not good [4]. According to El Oakley’s classification, thorough debridement and mediastinal lavage are recommended (Antibiotics + iodophor + saline) for Type I and II, and there was little difference between the wound closure effect and the treatment effect (hospital time, success rate) of the wound closure after debridement. The use of antibiotics (> 6 weeks) and thorough wound debridement according to drug susceptibility results are the keys to the treatment of DSWI [29].
One should mind that some patients have no obvious symptoms of infection. It has been reported that most DSWI patients with PaiRolero classification I-II have typical clinical manifestations such as fever, purulent exudation, and chest pain after admission. However, most of the type III patients do not have the above-mentioned typical clinical manifestations, and the indicators such as WBC and neutrophil percentage are not abnormal [40]. Therefore, we believe that multiple bacterial cultures of wound secretions, sputum, and blood should be performed in DSWI patients after admission, regardless of whether they have obvious symptoms of infection. In their study, Zhou Dan et al. [40] found that pathogenic bacteria could not be detected in about 1/2 of the 69 patients, which was considered to be related to the routine use of broad-spectrum antibiotics to prevent infection before cardiac surgery. Atypical pathogens such as bacteria and mycoplasma are also difficult to diagnose by in vitro culture. Therefore, we believe that the empirical use of antibiotics is also necessary before the results of drug susceptibility are available. The most common bacteria in SWI are gram-positive cocci, of which Staphylococcus aureus and Staphylococcus epidermidis account for more than 60%, gram-negative bacilli account for 5% ~ 22%, in addition, some are fungi, and about 25% of patients are infected by multiple pathogens [41].
Staphylococcus aureus is the most common gram-positive bacteria, while Pseudomonas aeruginosa and Acinetobacter Bauman are the most common gram-negative bacteria. Staphylococcus aureus and Staphylococcus epidermidis are highly resistant to penicillin G and sensitive to linezolid, tigecycline, ciprofloxacin, and vancomycin [40, 42]. It has been reported that linezolid is highly recommended, which has better tissue penetration, can form effective drug concentration under the sternum and mediastinum, conduct a more excellent antibacterial effect, and has an explicit clinical effect on Gram-positive bacteria in DSWI with osteomyelitis. Vancomycin has poor tissue penetration, obvious adverse effects of renal injury, and a poor antibacterial effect against methicillin-resistant Staphylococcus aureus. The drug resistance of Pseudomonas aeruginosa increased year by year, and the drug resistance of Acinetobacter baumannii increased more seriously. The former showed high resistance to imipenem, meropenem, cefuroxime, and ceftriaxone, and the drug resistance rate to common antibiotics of the latter exceeded 70% [44, 44].
In conclusion, the author believes that the wounds of those patients with DSWI mostly have residual necrotic tissue, pus, bone wax, loose steel wire, and other foreign bodies. Before the reconstruction operation, the foreign bodies need to be removed by multiple debridement operations, and the wounds need to be continuously rinsed and drained smoothly. Otherwise, even if the wound is forcibly closed, it will be difficult to heal or form a stealth sinus, which could be resulting in aggravation of infection. Clinicians must be highly skeptical about DSWI to avoid delaying the treatments for patients, although prophylactic antibiotics before cardiac surgery can improve the host’s natural defense function, it will prolong the incubation period, resulting in delayed onset of DSWI for several months after cardiac surgery, and plastic surgeons should pay close attention. After admission to the hospital, DSWI patients are recommended to perform a daily bacterial culture of secretions for three consecutive days and should be vigilant against false-negative results of bacterial culture. Even if the bacterial culture results are temporarily negative or the drug sensitivity results are delayed, antibiotics should be empirically used to prevent infection according to the local bacterial ecology and the antibiotic policy of the institution, and then the anti-infection strategy should be changed according to the drug sensitivity results.
Keep the drainage unobstructed
Whether it is based on the classification of infection or depth of anatomy, it is advocated that thorough debridement and irrigation drainage before wound reconstruction should be carried out [29]. Negative Pressure Wound Therapy (NPWT) has been widely used in the treatment of SWI. The material selection and operation are simple, which can effectively close the wound, promote the growth of granulation, have a high wound drainage effect, and speed up the closure of the cavity. It can be applied to sternal wound fat liquefaction and osteomyelitis wound. Compared with ordinary mediastinal tube drainage after debridement, NPWT can optimize the treatment efficiency, reduce patients’ pain and maintain a continuous “debridement-like” effect. NPWT can induce venous gradient hydrostatic pressure difference, promote blood flow, reduce local osmotic active molecules effectively, reduce tissue edema, reduce microcirculation damage, maintain the tissue blood supply, reduce residual flushing fluid and inflammatory exudation, and significantly reduce patients’ pain by stabilizing the sternum halves, shorten rehabilitation time [45,46,47]. The risk of secondary infection and the emergence of multidrug resistant microorganisms or the erosion of the exposed right ventricle, large blood vessels and bypass pipes resulting in fatal bleeding will seriously affect the late secondary healing effect of NPWT [11]. NPWT alone can significantly promote the healing of SSWI, but it is less effective for DSWI with osteomyelitis or mediastinal infection. NPWT combined with other treatments can achieve more satisfactory results. Hao et al. [41] retrospectively analyzed 62 cases of DSWI with sternal osteomyelitis, the sinus tract sealing time, wound healing time, compared with NPWT alone, PRP combined with NPWT has great curative effects on DSWI with sternal osteomyelitis and sinus tract, for it shortens sinus tract sealing time, wound healing time, and avoids the secondary repair surgery. There are also literature reports, PNWT only induces an inferior outcome in terms of fungal infections, treatment times, and the number of reoperations [48]. Xia et al. [49] evaluated the utility of antibiotic-loaded bone cement combined with vacuum sealing drainage on DSWI, all patients’ healing wounds were first-stage healing without complications and reoperation. Federico et al. [50] found that in a high-risk patient population, the incidence of adverse events in the treatment of DSWI with NPWT and pectoralis major muscle flap was lower than that in the treatment of skin flap reconstruction alone. And preoperative NPWT makes reconstructive surgery easier and faster [51].
Wound reconstruction
The optimal reconstruction method of DSWI is also controversial. It is difficult to unify the results of different classifications in order to obtain a recognized and unique optimal closure method. The choice of surgical strategy ultimately depends on the wound classification, risk factors, previous surgical history, potential donor sites, and the size and tissue characteristics of the residual defect area after debridement. For DSWI with mediastinal infection, sternal instability, and sternal defect necrosis, the strategy of greater omentum transplantation or myocutaneous flap closure is the majority. The Greater omentum is the peritoneum attached to the front of abdominal organs, which can limit inflammation and prevent infection. It is rich in epidermal growth factor (EGF), promotes epithelial synthesis protein, stimulates epithelial proliferation and migration, and is rich in vascular endothelial growth factor (VEGF) to promote the reconstruction of the blood supply in ischemic tissues. Compared with traditional debridement and closed drainage, muscle or omental flap reconstruction has a complication rate and mortality of 22% and 0% respectively, while the latter has a complication rate and mortality of 92% and 33% respectively [52]. As early as the 1990s, it was reported that the success rate of greater omentum transplantation was more than 95%, and the 5-year survival rate was 82%. It was easy to operate, effectively controlled the inflammation, promoted a healing effect, and shortened the hospital stay [53]. Several articles have shown that in the case of wound infection with drug-resistant bacteria, such as wounds infected with methicillin-resistant Staphylococcus aureus, the greater omentum transplantation is more recommended, which has more advantages than muscle flap [54,55,56]. The disadvantage of omental transplantation is that it may cause new invasive injury, which requires training in the use of special equipment such as laparoscopy or cooperation of professional teams, and may cause complications such as epigastric hernia, bleeding, necrosis, massive exudation, and peritoneal cavity pollution, and significantly reduce the patient’s vital capacity and exercise ability [54, 57]. The musculocutaneous flap is another option besides the omental flap, for example, the unilateral or bilateral pectoralis major myocutaneous flap is still the most common reconstruction method, which is because the muscle close to the wound, as well as the function of flip or push flap. Liu et al. [58] reported that the use of unilateral or bilateral pectoralis major flap can effectively fill the DSWI residual cavity, and believed that the development of the right pectoralis major muscle is better, the muscle fiber is fuller, the blood supply is richer, and the stage I healing rate is 91.3%. In Greig’s classification, more than 50% of the severe upper sternal defect (type I) with bone loss is recommended to be closed with pectoralis major myocutaneous flap; In the lower part of the sternum or the whole sternal space (type II ~ III), the space can be filled with pedicled rectus abdominis, latissimus dorsi or greater omentum. However, the rectus abdominisflap is close to the wound and is affected by inflammation for a long time, and the internal thoracic artery has been damaged during cardiac surgery, affecting the blood supply of the flap [32]. The Cologne merheim algorithm can select the coverage strategy based on the size and depth of the wound, which means, in patients with El Oakley type IV and V DSWI, small wounds less than 6 cm were covered with unilateral or bilateral pectoral myocutaneous flaps. Unilateral pedicled pectoralis major flap is suitable for medium wounds (7 ~ 12 cm), while for large wounds (> 13 cm), it is recommended to use the left latissimus dorsi flap [59]. However, compared with pectoralis major and rectus abdominis, the latissimus dorsi flap is far away from the infection, avoids local inflammatory invasion, has a rich blood supply, and has strong anti-infectivity [60]. A recent review article compared the greater omentum transplantation with muscle flap. The results showed that the mortality from using muscle flaps was slightly higher, and the relative risk was 1.29. The greater omentum transplantation and myocutaneous flap have their own advantages and disadvantages, which need to be further demonstrated. However, a full-time and highly professional team is needed to deal with sternal wound complications, select appropriate closure or coverage, and be familiar with various types of muscle flap collection and laparoscopic greater omentum transfer. (Table 9) (Fig. 1).
Wounds of any type and depth are necessary to expand debridement and to remove the infection, dead bone, and foreign bodies to the greatest extent, resulting in serious wound tissue defect and sternal instability. After the debridement, the loss of soft tissue and bone and the depth of the wound are the most important factors to determine whether to close the wound in one stage and how to choose the reconstruction scheme. ( Table 9) (Fig. 1).
New progress in treatment
Platelet-rich plasma (PRP) is an autologous plasma containing abnormal concentrations of platelets. The main component is concentrated platelets 3 ~ 10 times higher than the normal value, containing only a small amount or no white blood cells. In addition, it can also have an anti-infection ability by releasing some inflammatory inhibitory factors. It can also relieve surgical pain and neuropathic pain by regulating inflammatory response, promoting prominent regeneration, and restoring local tissue innervation [61,62,63,64,65]. In fact, the clinical medicine of PRP has decades of experience, widely covering orthopedics, stomatology, vascular surgery, oncology, plastic surgery and other disciplines. In recent years, it has been rapidly discovered in the field of skin and soft tissue repair and obtained good curative effect. PRP can run through the whole process of tissue repair, including hemostasis, inflammation, proliferation, and remodeling. Firstly, PRP is activated through endogenous and exogenous coagulation pathways, agglutinates into blocks, participates in the coagulation process and plays a role in hemostasis. Secondly, CXCR4 inhibits excessive inflammatory response, and bioactive proteins chemotactic mesenchymal stem cells, macrophages and fibroblasts promote inactivation, necrotic tissue clearance and tissue regeneration [66,67,68]. Again, platelets contain α Granules and high-density granules secrete a variety of bioactive proteins, regulate the migration and appreciation of keratinocytes, fibroblasts, and endothelial cells, promote angiogenesis, collagen synthesis, and epithelization, and then promote wound healing [69, 70]. Bielecki et al. [71] reported that PRP has an inhibitory effect on Staphylococcus aureus and Escherichia coli common in SWI. However, it was reported in the mate analysis of the effect of PRP on preventing sternal infection by Sun et al. [72], that compared with the control group, PRP can reduce the risk of postoperative nonunion of SWI by 74%, especially the therapeutic effect of SSWI, but the combined results of SWI and DSWI are heterogeneous. Hao et al. [41] found that in the treatment of sternal osteomyelitis and sinus after thoracotomy, PRP combined with NPWT can significantly improve the effect of stage I healing, reduce the number of stage II wound closure, and shorten the time of treatment and hospitalization. They also suggested that platelets should be controlled at (120 ~ 150) × 109 / L, only when the platelet count in PRP reaches 1000 × 109 / L or 4 ~ 7 times of whole blood platelets can achieve effective clinical results. Therefore, platelet condition is also an important factor affecting the reasonable choice of wound treatment. Antibiotic-loaded bone cement (ALBC) has a therapeutic effect on osteomyelitis. It was first reported by Klemm that bone cement cannot only conduct good mechanical support but also have a certain antibacterial effect. It has been widely used in the treatment of open fractures, osteomyelitis, and prosthesis / foreign body infection [73,74,75]. The advantages of ALBC in the treatment of refractory complex wounds are: ① ALBC can adjust the dosage and shape according to the size of the wound defects to better fill the residual cavity without leaving a dead cavity. The chest cavity is fixed after ALBC hardening. If necessary, it is convenient to take out and change the dressing, and the operation is simple; ② ALBC can be mixed with a variety of antibiotics according to bacterial culture and drug sensitivity results to provide mechanical support and local antibacterial. ③ Combined with NPWT, the treatment effect is obvious. However, there are relatively few public reports on ALBC for DSWI. Xia et al. [74] applied ALBC to the defect reconstruction of DSWI to solve the problem of DSWI and sternal instability and achieved a definite effect. However, it is not sure whether ALBC should be removed, or whether it will release cytotoxicity and inhibit local bone perfusion and bone remodeling, which needs further clinical research. In recent years, hyperbaric oxygen therapy (HBO2) has been gradually applied to the treatment of chronic and refractory wounds. It has the effects of local anti-inflammatory, down-regulating cell adhesion molecules, reducing the effect of leukocytes on endothelium, inhibiting the reproduction of anaerobic bacteria, stimulating angiogenesis, reducing edema and stimulating collagen production. Rados ł Aw et al. [76] evaluated the efficacy and effectiveness of HBO2 in DSWI patients. 11 DSWI patients were treated with HBO2 with an 80% success rate and no complications. It is considered as a valuable alternative to the treatment of recurrent refractory DSWI.
Regardless of the type and depth of the wound, expanded debridement is required to remove infection, sequestrum, and foreign bodies to the greatest extent possible, resulting in severe wound tissue defects and sternum instability. After debridement, the amount of soft tissue and bone loss and the depth of the wound are the most important factors in deciding whether to close the wound in one stage and how to choose the reconstruction plan. We refer to and summarize the new classification proposed by plastic surgery and the practical algorithm proposed by Schiraldi, and give corresponding treatment suggestions according to different characteristics of wounds. (Fig. 2)
Conclusion
DSWI is a potentially life-threatening complication of cardiac surgery. However, in recent years, more and more SWI patients come to the plastic surgery department for wound reconstruction. It is necessary for plastic surgeons to further understand the diagnosis, risk factors, and classification of SWI in order to select a more appropriate strategy for wound reconstruction. Accurate diagnosis is the main cornerstone in the management of this complication. Various risk factors of SWI must be taken into consideration before operating on those patients, especially the risk factors highly related to wound healing. Risk factors need to be considered together with classification to help surgeons choose more reasonable strategies for wound reconstruction. The reconstruction of complex DSWI requires the cooperation of cardiothoracic surgeons and plastic surgeons to learn from each other, so as to wait for better treatment effects.
Data Availability
The data analyzed in this manuscript are all from the literature consulted on PubMed and CNKI, which can be found according to the content of the article.
References
Yang JF, Yang K, Xia HN, et al. Clinical characteristics of deep sternal wound infections after cardiac surgery and etiological analysis. Chin J Nosocomiol. 2017;27(5):1145–8.
Kaye AE, Kaye AJ, Pahk B et al. Sternal wound reconstruction: management in different cardiac populations.Ann Plast Surg 2010May;64(5). PubMed PMID: 20395796. Epub 2010/03/02.
Vyas RM, Orgill DP. Reply: transdiaphragmatic omental harvest: a simple, efficient method for sternal wound coverage. Plast Reconstr Surg. 2013 Dec;132(6):1074. e. PubMed PMID: 24281620. Epub 2013/11/28.
Alebrahim K, Al-Ebrahim E, Prevention. Classification and Management Review of Deep Sternal Wound Infection. Heart Surg Forum. 2020 Sep 14;23(5):E652-E7. PubMed PMID: 32990568. Epub 2020/09/30.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting.Am J Infect Control. 2008Jun;36(5):309–32. PubMed PMID: 18538699. Epub 2008/06/10.
Mekontso Dessap A, Vivier E, Girou E, Brun-Buisson C, Kirsch M. Effect of time to onset on clinical features and prognosis of post-sternotomy mediastinitis. Clin Microbiol Infect. 2011 Feb;17(2):292–9. PubMed PMID: 20167008. Epub 2010/02/20.
Chung, Kevin C, Lizi, Waljee J, et al. The impact of Deep Sternal Wound infection on mortality and resource utilization: a Population-based study. J World Journal of Surgery: Official Journal of the Societe Internationale de Chirurgie Collegium Internationale Chirurgiae Digestivae of the International Association of Endocrine Surgeons. 2016;40(11):2673–80.
Schiraldi L, Jabbour G, Centofanti P, Giordano S, Abdelnour E, Gonzalez M et al. Deep sternal wound infections: Evidence for prevention, treatment, and reconstructive surgery.Arch Plast Surg. 2019Jul;46(4):291–302. PubMed PMID: 31336416. Pubmed Central PMCID: PMC6657195. Epub 2019/07/25.
Lazar HL, Salm TV, Engelman R, Orgill D, Gordon S. Prevention and management of sternal wound infections. J Thorac Cardiovasc Surg. 2016 Oct;152(4):962–72. PubMed PMID: 27555340. Epub 2016/08/25.
Zahiri HR, Lumpkins K, Kelishadi SS, Zhu Y, Medina D, Conde-Green A et al. Significant predictors of complications after sternal wound reconstruction: a 21-year experience.Ann Plast Surg. 2012Oct;69(4):439–41. PubMed PMID: 22214795. Epub 2012/01/05.
Alebrahim K, Al-Ebrahim E, Prevention. Classification and Management Review of Deep Sternal Wound Infection. Heart Surg Forum. 2020 Sep 14;23(5):E652-E657. PubMed PMID: 32990568. Epub 2023/01/09.
RF Z FZ, LN TH, WJ, QF. 18F-FDG PET/CT guided management of infective costal chondritis after cardiac surgery. Chin J Aesthetic Med. 2018;27(2):28.
Irmler IM, Opfermann T, Gebhardt P, Gajda M, Brauer R, Saluz HP, et al. In vivo molecular imaging of experimental joint inflammation by combined (18)F-FDG positron emission tomography and computed tomography. Arthritis Res Ther. 2010;12(6):R203. PubMed PMID: 21047399. Pubmed Central PMCID: PMC3046507. Epub 2010/11/05.
Gur E, Stern D, Weiss J, Herman O, Wertheym E, Cohen M, et al. Clinical-radiological evaluation of poststernotomy wound infection. Plast Reconstr Surg. 1998 Feb;101(2):348–55. PubMed PMID: 9462765. Epub 1998/02/14.
Spindler N, Moter A, Wiessner A, Gradistanac T, Borger M, Rodloff AC, et al. Fluorescence in situ hybridization (FISH) in the Microbiological Diagnostic of Deep Sternal Wound infection (DSWI). Infect Drug Resist. 2021;14:2309–19. PubMed PMID: 34188497. Pubmed Central PMCID: PMC8232876. Epub 2021/07/01.
Landes G, Harris PG, Sampalis JS, Brutus JP, Cordoba C, Ciaburro H, et al. Outcomes in the management of sternal dehiscence by plastic surgery: a ten-year review in one university center. Ann Plast Surg. 2007 Dec;59(6):659–66. PubMed PMID: 18046149. Epub 2007/11/30.
Kaye AE, Kaye AJ, Pahk B, McKenna ML, Low DW. Sternal wound reconstruction: management in different cardiac populations. Ann Plast Surg. 2010 May;64(5):658–66. PubMed PMID: 20395796. Epub 2010/04/17.
Wu YY, Liu Y, Dong WP, et al. Logistic regression analysis on surgical site infection safter open heart surger. Chin J Nosocomi. 2016;26(15):3487–91.
Chan PG, Sultan I, Gleason TG, Wang Y, Navid F, Thoma F et al. Contemporary outcomes of coronary artery bypass grafting in obese patients.J Card Surg. 2020Mar;35(3):549–56. PubMed PMID: 31945232. Epub 2020/01/17.
Engelman DT, Adams DH, Byrne JG, Aranki SF, Collins JJ Jr, Couper GS, et al. Impact of body mass index and albumin on morbidity and mortality after cardiac surgery. J Thorac Cardiovasc Surg. 1999 Nov;118(5):866–73. PubMed PMID: 10534692. Epub 1999/10/27.
Moussa M, Tkaczuk J, Ragab J, Garcia J, Abbal M, Ohayon E, et al. Relationship between the fatty acid composition of rat lymphocytes and immune functions. Br J Nutr. 2000 Mar;83(3):327–33. PubMed PMID: 10884721. Epub 2000/07/08.
Baldassarro VA, Lorenzini L, Giuliani A, Cescatti M, Alastra G, Pannella M et al. Molecular mechanisms of skin wound healing in non-diabetic and diabetic mice in excision and pressure experimental wounds.Cell Tissue Res. 2022Jun;388(3):595–613. PubMed PMID: 35386010. Pubmed Central PMCID: PMC9110453. Epub 2022/04/08.
Viola A, Munari F, Sanchez-Rodriguez R, Scolaro T, Castegna A. The Metabolic Signature of Macrophage Responses.Front Immunol. 2019;10:1462. PubMed PMID: 31333642. Pubmed Central PMCID: PMC6618143. Epub 2019/07/25.
Nikitina OV, Chainikova IN, Skachkova MA, Barsukova SV. [Features of immunity in tobacco smoking among adolescents].Gig Sanit. 2012 May-Jun(3):59–61. PubMed PMID: 23088131. Epub 2012/10/24.
Floyd L, Morris A, Joshi M, Dhaygude A. Glucocorticoid Therapy in ANCA Vasculitis: Using the Glucocorticoid Toxicity Index as an Outcome Measure. Kidney360. 2021 Jun 24;2(6):1002-10. PubMed PMID: 35373091. Pubmed Central PMCID: PMC8791372. Epub 2022/04/05.
Raanani E, Spiegelstein D, Sternik L, Preisman S, Moshkovitz Y, Smolinsky AK, et al. Quality of mitral valve repair: median sternotomy versus port-access approach. J Thorac Cardiovasc Surg. 2010 Jul;140(1):86–90. PubMed PMID: 19969315. Epub 2009/12/09.
Vitartaite M, Vaiciulyte D, Vencloviene J, Sirvinskas E, Bukauskiene R, Jakuska P et al. Risk Factors Associated with an Increased Risk of Deep Sternal Wound Infections in Patients After Coronary Artery Bypass Grafting and Heart Defect Surgery.Heart Surg Forum. 2021 Aug25;24(4):E741-E5. PubMed PMID: 34473026. Epub 2021/09/03.
Pairolero PC, Arnold PG. Management of recalcitrant median sternotomy wounds. J Thorac Cardiovasc Surg. 1984 Sep;88(3):357–64. PubMed PMID: 6471886. Epub 1984/09/01.
El Oakley RM, Wright JE. Postoperative mediastinitis: classification and management. Ann Thorac Surg. 1996 Mar;61(3):1030–6. PubMed PMID: 8619682. Epub 1996/03/01.
Gao Yongshun LY. Treatment of deep infection of sternal incision after cardiac surgery. J Clin Surg. 2017;25(5):17–9.
Jones G, Jurkiewicz MJ, Bostwick J, Wood R, Bried JT, Culbertson J, et al. Management of the infected median sternotomy wound with muscle flaps. The Emory 20-year experience. Ann Surg. 1997 Jun;225(6):766–76. discussion 76 – 8. PubMed PMID: 9230817. Pubmed Central PMCID: PMC1190886. Epub 1997/06/01.
Greig AV, Geh JL, Khanduja V, Shibu M. Choice of flap for the management of deep sternal wound infection–an anatomical classification. J Plast Reconstr Aesthet Surg. 2007;60(4):372–8. PubMed PMID: 17349591. Epub 2007/03/14.
Rupprecht L, Schmid C. Deep sternal wound complications: an overview of old and new therapeutic options. Open J Cardiovasc Surg. 2013;6:9–19. PubMed PMID: 25512698. Pubmed Central PMCID: PMC4222320. Epub 2013/01/01.
van Wingerden J, Ubbink D, van der Horst C, de Mol, BJJocs. Poststernotomy mediastinitis: a classification to initiate and evaluate reconstructive management based on evidence from a structured review. 2014;9:179. PubMed PMID: 25417190.
Anger J, Dantas DC, Arnoni RT, Farsky PS. A new classification of post-sternotomy dehiscence. Rev Bras Cir Cardiovasc. 2015 Jan-Mar;30(1):114–8. PubMed PMID: 25859875. Pubmed Central PMCID: PMC4389524. Epub 2015/04/11.
Nahai F, Rand RP, Hester TR, Bostwick J 3rd, Jurkiewicz MJ. Primary treatment of the infected sternotomy wound with muscle flaps: a review of 211 consecutive cases.Plast Reconstr Surg. 1989Sep;84(3):434–41. PubMed PMID: 2762402. Epub 1989/09/01.
Trouillet JL, Vuagnat A, Combes A, Bors V, Chastre J, Gandjbakhch I, et al. Acute poststernotomy mediastinitis managed with debridement and closed-drainage aspiration: factors associated with death in the intensive care unit. J Thorac Cardiovasc Surg. 2005 Mar;129(3):518–24. PubMed PMID: 15746733. Epub 2005/03/05.
van Wingerden JJ, Ubbink DT, van der Horst CM, de Mol BA. Poststernotomy mediastinitis: a classification to initiate and evaluate reconstructive management based on evidence from a structured review.J Cardiothorac Surg. 2014 Nov 23;9:179. PubMed PMID: 25417190. Pubmed Central PMCID: PMC4247689. Epub 2014/11/25.
Elassal AA, Al-Ebrahim KE, Al-Radi OO, Jabbad HH, Eldib OS. Sternal Wound Complications: Objective Reclassification and Surgical Reconsideration. Heart Surg Forum. 2020 Feb 27;23(1):E076-E80. PubMed PMID: 32118548. Epub 2020/03/03.
Zhou Dan TL. Chen Xufa,Zhou Hong,Yang Kai. Clinical characteristics of postoperative deep sternal wound infection in patients undergoing cardiacsurgery and distribution and drug resistanceofpathogens. Chin J Nosocomio. 2017;27(5):1117–20.
Hao D, Feng G, Li T, Chu W, Chen Z, Li S, et al. Curative effects of platelet-rich plasma combined with negative-pressure wound therapy on sternal osteomyelitis and sinus tract after thoracotomy. Zhonghua Shao Shang Za Zhi. 2016 Jun;32(6):331–5. PubMed PMID: 27321486. Epub 2016/06/21.
Magro PL, Sousa Uva M. Does routine topical antimicrobial administration prevent sternal wound infection after cardiac surgery? Interact Cardiovasc Thorac Surg. 2021 Apr 8;32(3):452-6. PubMed PMID: 33346346. Pubmed Central PMCID: PMC8691553. Epub 2020/12/22.
Ma JG, An JX. Deep sternal wound infection after cardiac surgery: a comparison of three different wound infection types and an analysis of antibiotic resistance.J Thorac Dis. 2018Jan;10(1):377–87. PubMed PMID: 29600070. Pubmed Central PMCID: PMC5863177. Epub 2018/03/31.
Reineke S, Carrel TP, Eigenmann V, Gahl B, Fuehrer U, Seidl C et al. Adding vancomycin to perioperative prophylaxis decreases deep sternal wound infections in high-risk cardiac surgery patients. Eur J Cardiothorac Surg. 2018 Feb 1;53(2):428 – 34. PubMed PMID: 29045740. Epub 2017/10/19.
Drossos G, Ampatzidou F, Baddour A, Madesis A, Karaiskos T. The impact of deep sternal wound infections treated by negative pressure on early, 1 year and late mortality: a longitudinal case-control study. J Card Surg. 2019 Dec;34(12):1550–5. PubMed PMID: 31654592. Epub 2019/10/28.
Gatti G, Benussi B, Brunetti D, Ceschia A, Porcari A, Biondi F et al. The fate of patients having deep sternal infection after bilateral internal thoracic artery grafting in the negative pressure wound therapy era.Int J Cardiol. 2018 Oct15;269:67–74. PubMed PMID: 30049494. Epub 2018/07/28.
Gatti G, Ledwon M, Gazdag L, Cuomo F, Pappalardo A, Fischlein T, et al. Management of closed sternal incision after bilateral internal thoracic artery grafting with a single-use negative pressure system. Updates Surg. 2018 Dec;70(4):545–52. PubMed PMID: 29460174. Epub 2018/02/21.
Hamalainen E, Laurikka J, Huhtala H, Jarvinen O. Vacuum assistance therapy as compared to early reconstructive treatment in deep sternal wound infection. Scand J Surg. 2021 Jun;110(2):248–53. PubMed PMID: 33327852. Pubmed Central PMCID: PMC8258712. Epub 2020/12/18.
Jiang X, Xu Y. Guoqing Jiao, The combined application of antibiotic- loaded bone cement and vacuum sealing drainage for sternal reconstruction in the treatment of deep sternal wound infection. J Cardiothorac Surg 2022 Aug 26;17(1) PubMed PMID: 36028875. Epub 2022/08/26.
Lo Torto F, Monfrecola A, Kaciulyte J, Ciudad P, Casella D, Ribuffo D, Carlesimo B. Preliminary result with incisional negative pressure wound therapy and pectoralis major muscle flap for median sternotomy wound infection in a high-risk patient population. Int Wound J. 2017 Dec;14(6):1335–39. PubMed PMID: 28901717. Epub 2017/09/13.
Barbera F, Lorenzetti F, Marsili R, Lisa A, Guido G, Pantaloni M. The Impact of Preoperative Negative-Pressure Wound Therapy on Pectoralis Major Muscle Flap Reconstruction for Deep Sternal Wound Infections.Ann Plast Surg 2019Aug;83(2):195–200. PubMed PMID:30882416. Epub 2019/08/02.
Brandt C, Alvarez JM. First-line treatment of deep sternal infection by a plastic surgical approach: superior results compared with conventional cardiac surgical orthodoxy. Plast Reconstr Surg. 2002 Jun;109(7):2231–7. PubMed PMID: 12045542 Epub 2001/10/09.
Belcher P, McLean N, Breach N, Paneth M. Omental transfer in acute and chronic sternotomy wound breakdown. Thorac Cardiovasc Surg. 1990 Jun;38(3):186–91. PubMed PMID: 2375036. Epub 1990/06/01.
Botianu PVH. Current indications for the intrathoracic transposition of the omentum. J Cardiothorac Surg. 2019 Jun 10;14(1):103. PubMed PMID: 31182112. Pubmed Central PMCID: PMC6558767. Epub 2019/06/12.
van Wingerden JJ, Lapid O, Boonstra PW, de Mol BA. Muscle flaps or omental flap in the management of deep sternal wound infection. Interact Cardiovasc Thorac Surg. 2011 Aug;13(2):179–87. PubMed PMID: 21543366. Epub 2011/05/06.
Danner BC, Zenker D, Didilis VN, Grossmann M, Stojanovic T, Seipelt R, et al. Transposition of greater omentum in deep sternal wound infection caused by methicillin-resistant Staphylococci, with differing clinical course for MRSA and MRSE. Thorac Cardiovasc Surg. 2011 Feb;59(1):21–4. PubMed PMID: 21243567. Epub 2011/01/19.
Tewarie L, Moza AK, Khattab MA, Autschbach R, Zayat R. Effective Combination of Different Surgical Strategies for Deep Sternal Wound Infection and Mediastinitis. Ann Thorac Cardiovasc Surg. 2019 Apr 20;25(2):102 – 10. PubMed PMID: 30404980. Pubmed Central PMCID: PMC6477456. Epub 2018/11/09.
Shuo LJGYLBXXH. New technique of pectoral muscle flap reconstruction for 23 patients with deep sernal wound infections. Chin J Clin Thorac Cardiovasc Surg. 2018;25(4):4.
Weinand C, Xu W, Perbix W, Theodorou P, Lefering R, Spilker G. Deep sternal osteomyelitis: an algorithm for reconstruction based on wound width. J Plast Surg Hand Surg. 2013 Oct;47(5):355–62. PubMed PMID: 23710791. Epub 2013/05/29.
Kuang Bin CY. Deng Guosan,Kuang Shifeng,Huang Guangxiang,Zhao Chengli,Deng Jian,Lian Jihong,Xie Wenbin. Application of latissimus dorsi myocutaneous flap in repair of sternal incision infection and rupture after coronary artery bypass grafting. Chin J Surg. 2005;43(3):195.
Sethi D, Martin KE, Shrotriya S, Brown BL. Systematic literature review evaluating evidence and mechanisms of action for platelet-rich plasma as an antibacterial agent. J Cardiothorac Surg. 2021 Sep 28;16(1):277. PubMed PMID: 34583720. Pubmed Central PMCID: PMC8480088. Epub 2021/09/30.
Serraino GF, Dominijanni A, Jiritano F, Rossi M, Cuda A, Caroleo S, et al. Platelet-rich plasma inside the sternotomy wound reduces the incidence of sternal wound infections. Int Wound J. 2015 Jun;12(3):260–4. PubMed PMID: 23692143. Pubmed Central PMCID: PMC7950781. Epub 2013/05/23.
Lutz C, Cheng J, Prysak M, Zukofsky T, Rothman R, Lutz G. Clinical outcomes following intradiscal injections of higher-concentration platelet-rich plasma in patients with chronic lumbar discogenic pain. Int Orthop. 2022 Jun;46(6):1381–5. PubMed PMID: 35344055. Pubmed Central PMCID: PMC9117340. Epub 2022/03/29.
Jiang YH, Jhang JF, Lin TY, Ho HC, Hsu YH, Kuo HC. Therapeutic efficacy of Intravesical platelet-rich plasma injections for interstitial Cystitis/Bladder Pain Syndrome-A comparative study of different injection number, additives and concentrations. Front Pharmacol. 2022;13:853776. PubMed PMID: 35392571. Pubmed Central PMCID: PMC8980355. Epub 2022/04/09.
Patel AN, Selzman CH, Kumpati GS, McKellar SH, Bull DA. Evaluation of autologous platelet rich plasma for cardiac surgery: outcome analysis of 2000 patients. J Cardiothorac Surg. 2016 Apr 12;11(1):62. PubMed PMID: 27068030. Pubmed Central PMCID: PMC4828785. Epub 2016/04/14.
Lusini M, Di Martino A, Spadaccio C, Rainer A, Chello M, Fabbrocini M et al. Resynthesis of sternal dehiscence with autologous bone graft and autologous platelet gel. 2012;21(2):74, 6–7. PubMed PMID: 22584526.
Pourkarim R, Farahpour MR, Rezaei SA. Comparison effects of platelet-rich plasma on healing of infected and non-infected excision wounds by the modulation of the expression of inflammatory mediators: experimental research. Eur J Trauma Emerg Surg. 2022 Aug;48(4):3339–47. PubMed PMID: 35149876. Epub 2022/02/13.
Giannini S, Cielo A, Bonanome L, Rastelli C, Derla C, Corpaci F, et al. Comparison between PRP, PRGF and PRF: lights and shadows in three similar but different protocols. Eur Rev Med Pharmacol Sci. 2015;19(6):927–30. PubMed PMID: 25855914. Epub 2015/04/10.
Mautner K, Malanga GA, Smith J, Shiple B, Ibrahim V, Sampson S, et al. A call for a standard classification system for future biologic research: the rationale for new PRP nomenclature. PM R. 2015 Apr;7(4 Suppl):53–S9. PubMed PMID: 25864661. Epub 2015/04/14.
Yao D, Feng G, Zhao F, Hao D. Effects of platelet-rich plasma on the healing of sternal wounds: A meta-analysis. Wound Repair Regen. 2021 Jan;29(1):153–67. PubMed PMID: 33128501. Epub 2020/11/01.
Bielecki TM, Gazdzik TS, Arendt J, Szczepanski T, Król W, Wielkoszynski T. Antibacterial effect of autologous platelet gel enriched with growth factors and other active substances. THE JOURNAL OF BONE AND JOINT SURGERY; 2007. 89-B(3).
Sun Bin FZ, Xu F, Meixian ZYanH, Qian Baohua. Efficacy and safety of the use of platelet-rich plasma for sternal wound infections: a meta-analysis. Chin J Blood Transfus. 2015;28(3):295–8.
Klemm KW. Gentamicin-PMMA chains (Septopal chains) for the local antibiotic treatment of chronic osteomyelitis. Reconstr Surg Traumatol. 1988;20:11–35. PubMed PMID: 3399737. Epub 1988/01/01.
Fevrier A, Boursot C, Tannugi KC. Osteomyelitis and Gentamicin-PMMA Chains. Clin Nucl Med. 2022 Nov 1;47(11):e708-e9. PubMed PMID: 35961640. Epub 2022/08/13.
Jiang X, Bu F, Xu Y, Jing Z, Jiao G, Li M et al. Antibiotic-loaded bone cement combined with vacuum sealing drainage to treat deep sternal wound infection following cardiac surgery: the first case report.J Cardiothorac Surg. 2021 Oct10;16(1):292. PubMed PMID: 34629078. Pubmed Central PMCID: PMC8504067. Epub 2021/10/12.
Litwinowicz R, Bryndza M, Chrapusta A, Kobielska E, Kapelak B, Grudzien G. Hyperbaric oxygen therapy as additional treatment in deep sternal wound infections – a single center’s experience. Kardiochir Torakochirurgia Pol. 2016 Sep;13(3):198–202. PubMed PMID: 27785131. Pubmed Central PMCID: PMC5071585. Epub 2016/10/28.
Funding
This study was supported from the Military Logistics Scientific Research Project Health Special Project (22BJZ35,21BJZ29), the Program of National Natural Science Foundation of China (82072169, 82272279), the Major Program of Military Logistics Research Plan (ALB18J001), and the Innovation Cultivation Fund(CXPY201732).
Author information
Authors and Affiliations
Contributions
Yaoyao Song and Wanli Chu mainly wrote the main manuscripts. Jiachen Sun, Hongjuan Zhu, Xinzhu Liu and Hongli Yu were responsible for drawing figures and collecting some documents, and Chuanan Shen conceived the framework of the manuscript. All the authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This manuscript is a review and is not subject to Ethical Approval.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Song, Y., Chu, W., Sun, J. et al. Review on risk factors, classification, and treatment of sternal wound infection. J Cardiothorac Surg 18, 184 (2023). https://doi.org/10.1186/s13019-023-02228-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-023-02228-y