Abstract
Background
The treatment of symptomatic severe aortic stenosis (AS) has rapidly evolved over the past decade, in both transcatheter (TAVR) and surgical aortic valve replacement (SAVR), resulting in reported improved clinical outcomes. Operator experience and technical improvements have improved outcomes especially for patients undergoing TAVR. We sought to determine and compare 1-year outcomes using a contemporary meta-analysis.
Method
We searched the Medline (MESH), Cochrane and Google scholar databases using keywords “AS”, “atrial fibrillation” (AFib) and “stroke”. We performed a meta-analysis to compare TAVR with SAVR populations for post-procedural stroke, all-cause and cardiovascular mortality at 1-year.
Results
A total of 23 studies met criteria for analysis with total population of 66,857 patients, of which 61,913 had TAVR and 4944 had SAVR. Temporal trends demonstrated overall improvement in outcome for both, TAVR and SAVR groups through the decade. Outcomes, in terms of stroke (3.1% vs. 5%), all-cause (12.4% vs. 10.3%) and cardiovascular mortality (7.2% vs. 6.2%) were similar at 1-year, in TAVR versus SAVR, respectively.
Conclusion
Despite overall gradual improvement in both TAVR and SAVR outcomes over the decade, there is a statistical overlap in confidence intervals for all-cause, cardiovascular mortality and postprocedural stroke at 1-year. While 23 individual studies demonstrate considerable advantages of each technique in certain cohorts, integrating over 65,000 pts with our stratified surgical analysis suggests that TAVR is comparable to SAVR for low and intermediate risk population while superior to SAVR only in the highest-risk population for short and intermediate term outcomes. This has substantial socio-economic implications as we contemplate expanding our TAVR indications to low/intermediate risk populations.
Similar content being viewed by others
Introduction
Aortic stenosis (AS) is a progressive debilitating valvular heart disease with rapid development of clinical heart failure and high risk of mortality once patients become symptomatic. Aortic valve replacement is the standard of care for severe symptomatic AS patients and is associated with significant improvement in symptoms, quality of life and survival [1]. Transcatheter aortic valve replacement (TAVR) was introduced in 2002 and, although initially considered as a salvage procedure for patients who are prohibitive surgical risk for surgical aortic valve replacement (SAVR), emerging literature continues to reveal constant progressive technical advancements with improved valve systems, matched with improved implantation hardware and techniques making it an attractive alternative, not only for high-risk but also for selected intermediate and low risk patients [2,3,4]. Given the significant accumulation of data from trials and cohort studies, we conducted a meta-analysis to determine any clinical differences in adverse clinical outcomes and identify temporal changes between patients undergoing TAVR and SAVR over nearly two decades.
Materials and methods
Study design
The study was designed according to the PRISMA (Preferred Reported Items for Systematic Reviews and Meta-analyses) guidelines (Fig. 1) [5]. We carried out an extensive literature search through Medline (MESH), Cochrane and Google scholar databases using the keywords “AS”, “atrial fibrillation” (AFib) and “stroke”, and reviewed TAVR and SAVR studies from January 2005 to November 2018. Two independent investigators assessed the eligibility of the studies for inclusion and divergence was resolved by 3rd reviewer. The risk of bias was evaluated by all authors based on Cochrane collaboration methods for Randomized clinical trials (RCT) and Risk Of Bias In Non-randomized Studies of Interventions (ROBIN-I) for observational studies.
Inclusion criteria
The included studies were restricted to RCTs, prospective and retrospective studies. Case reports and small case series were not included in our analysis. Overlap of included patients was strictly avoided and duplicate studies were excluded. We included both the Society of Thoracic Surgeons (STS) and the Logistic European System for Cardiac Operative Risk Evaluation (EuroSCORE) system for risk stratification of both groups (TAVR and SAVR) into low, intermediate or high risk for mortality. The adverse clinical outcomes of our study (primary endpoints) included (1) Post-procedural stroke (2) All-cause mortality and (3) Cardiovascular mortality at 1-year. Studies not reporting data on AFib were excluded considering stroke was one of our primary endpoints.
Statistical analysis
The relative risk (RR) was calculated for grouped results of each outcome. Statistical significance of the differences between TAVR and SAVR groups was performed using meta-analysis (Mantel–Haenszel) with a random-effect model. Heterogeneity of the studies was assessed using Cochran's Q test to calculate I2 and Z test was used to assess the significance of the effect size. The differences between the results in the TAVR and SAVR groups were considered significant if p < 0.05. The statistical analyses were performed using the R program meta [6, 7] and SPSS for Windows v 18, IBM Inc. In order to represent the heterogeneity of the studies, we constructed forest plots of the risk ratio. A visual assessment of publication bias was assessed by inspection of funnel plots. Weighting for publication ‘n’ was performed but in the R program meta, additional strengthening of statistical observations was accomplished through accounting for homogeneity, variability and bias.
TAVR and SAVR patient populations were organized as three 4-year groups to analyze the temporal trend and organized by surgical risk to assess variation with risk level. The rate over time and between groups was assessed using Chi-square, with p < 0.05 considered statistically significant.
Results
Out of 540 studies, 23 studies met our eligibility criteria with the majority excluded due to specific reasons (Fig. 1). Eight studies were RCTs, and the remaining were prospective and retrospective studies (Table 1). Overall, we included 66,857 patients from January 2005 to November 2018, among which 61,913 underwent TAVR and 4944 SAVR.
In our forest plot meta-analysis, overall, post-procedural stroke at 1-year was 3.1% in TAVR versus 5% in SAVR patients (RR, 0.81; 95% CI, 0.31–2.13; p = 67). All-cause mortality at 1-year was 12.4% in the TAVR versus 10.3% in SAVR group (RR, 087; 95% CI, 0.53–1.43; p = 0.58), whereas CV mortality at 1-year was 7.2% in the TAVR versus 6.2% in the SAVR group (RR, 1.05; 95% CI, 0.79–1.4; p = 74) (Figs. 2, 3).
To study temporal changes between the two groups, we divided our total patient population in three 4-year subcategories. There was a significant temporal decline in all-cause and cardiovascular mortality at 1-year in both groups (TAVR all-cause mortality trend—17 to 12 to 6%; SAVR all-cause mortality trend—25 to 9 to 8%; TAVR cardiovascular mortality trend—11.6 to 7 to 4.6%; SAVR cardiovascular mortality trend—11 to 5.6 to 5.7%; p < 0.05 for changes over time for all) (Fig. 5A, C). On the other hand, even though the changes over time were significant (p < 0.05) for post-procedural stroke at 1 year for both groups, there was no significant temporal change for TAVR but had progressively higher reported post-procedural stroke for SAVR group (TAVR trend—7 to 3 to 7%; SAVR Stroke/TIA trend 3.7 to 8.2 to 8.7%; p < 0.05 only for SAVR) (Fig. 5E).
Overall, preexisting AFib was more common in TAVR compared to SAVR patients (38% vs. 25%, p < 0.0001). Although there was no temporal decline noted in post-procedural stroke at 1-year in either group, there was a decline over time noted in the rates of preexisting AFib in both populations (38 to 24% for SAVR; 42 to 25% for TAVR; p < 0.05 for changes over time) (Figs. 5E, 6A). New onset AFib post valve replacement, was progressively higher in the SAVR group compared to the TAVR group (2005–2008 group to 2009–2012 group; 10 to 8% for TAVR, p = NS; 17 to 29% for SAVR, p < 0.05) and did not change significantly over time in TAVR but did for SAVR (Fig. 6B). In relation to this, we found that the incidence of stroke/TIA at 1-year was higher in SAVR population in 2009–2012 group compared to 2005–2008 group (8.2 to 3.7%; p < 0.05) (Fig. 5E). There were no studies reporting data on new onset AFib for our last 4 years of study (2013–2016 group).
A Temporal decline in preexisting AFib over the decade. The changes overtime is statistically significant (p < 0.05). B Higher risk of new onset AFib with SAVR compared to SAVR and temporal increase in new onset AFib in early decade. The changes overtime is statistically significant for SAVR but not TAVR (p < 0.05). C Increased rehospitalization with increased surgical risk. The changes between the surgical risks are statistically significant (p < 0.05) for figure C
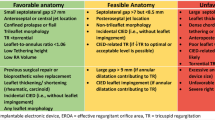
When stratified according to the pre-procedural surgical risk, there was a progressive increase in stroke, all-cause and cardiovascular mortality at 1-year with increasing surgical risk in both populations (Figs. 4, 5B, D, F). For low surgical risk, there was no statistically significant difference in all-cause mortality and stroke at 1-year between the two groups though cardiovascular mortality at 1-year was significantly lower in TAVR compared to SAVR (1.6% vs. 2.8%, p < 0.05) (Figs. 4, 5B, D, F). For intermediate surgical risk, there was no statistically significant difference in all-cause and cardiovascular mortality at 1-year, however stroke was significantly lower in TAVR compared to SAVR patients (2.7% vs. 9.5%, p < 0.05) (Figs. 4, 5B, D, F). For high surgical risk, there was no statistically significant difference in all-cause mortality at 1-year though cardiovascular mortality and stroke at 1-year were significantly lower in TAVR patients (9.5% vs. 11.8%; p < 0.05 and 4.9% vs. 8.4%; p < 0.05, respectively) (Figs. 4, 5B, D, F). Repeat hospitalizations at 1-year were progressively higher with increasing surgical risk in both groups. Rehospitalization after valve replacement was significantly higher for low (4.8% vs. 8.1%; p < 0.05) and intermediate surgical risk (8.4% vs. 11%; p < 0.05) patients undergoing SAVR compared to TAVR but there was no difference between groups in high surgical risk patients (Figs. 4, 6C).
Discussion
Since the advent of TAVR in the early 2000s, there has been a tremendous amount of research and evolution in the field of aortic valve replacement. This led to considerable improvements in patient identification, along with procedural and technical improvements especially for patients undergoing TAVR but also for SAVR given the contemporary mini-thoracotomy approach utilized in many patients. Subsequently, there has been a vast amount of data from both large, randomized trials and smaller cohort studies that have evaluated the outcomes of these patients. Some level of clinical equipoise has been noted between these two techniques and cardiovascular societies have been engaged in improving the adverse clinical outcomes of TAVR and SAVR including reduction in post-procedural stroke, cardiovascular and all-cause mortality. TAVR being a minimally invasive technique, appears to be an attractive alternative and is now considered the treatment of choice for patients with prohibitive surgical risk, and an equivalent option for high surgical risk. TAVR is also considered an alternative option for intermediate surgical risk patients and recently approved for selected low surgical risk patients from the U.S Food and Drug Administration (FDA) as well [8, 9]. The threshold of performing TAVR is gradually declining with ongoing advancement in operator experience, technique and valvular specifications. Cost effective analysis also supports TAVR in selected patient population as demonstrated by Weintraub et al. TAVR is comparable to medical therapy (PARTNER B sub study) and comparable to SAVR if trans-femoral approach is considered (PARTNER A sub study) [10].
Periprocedural stroke remains a dreaded complication for both procedures and, the literature demonstrates conflicting evidence for this adverse outcome. Unfortunately, over nearly two decades, we were not able to appreciate any temporal decline in postprocedural stroke at 1-year despite lower rates of preexisting AFib in more recent studies. Although the incidence of stroke/TIA at 1-year was higher in TAVR in first tertile of our study period, incidence of stroke/TIA at 1 year in TAVR was lower compared to SAVR population in the latter tertiles (Fig. 4). Given the fact that despite progressively less preexisting AFib in SAVR population, there is more incidence of post-procedural strokes indicating, in aggregate, increased risk with this procedure. In clinical practice, anticoagulation for peri-operative AFib post-SAVR is often neglected due to the misconception that AFib is incidental and purely catecholamine induced, although recurrent AFib is common and could be responsible for these events [11,12,13,14]. Chakravarty et al. described the effect of short term (up to 1 year) anticoagulation post-SAVR population with decreased risk of stroke post-procedure [15]. Given this data, it is important to note that peri-operative AFib needs to be considered as a potential driver of these findings.
On the contrary, structural valve degeneration (SVD) remains an area of concern after TAVR and the longevity of these prosthetic valves needs to be considered in the decision making especially in patients with a life expectancy of more than 5 years. A recent study from the UK assessed the durability of TAVR up to 10 years in 241 patients and found > 90% to remain free of SVD and < 1% to suffer from severe SVD [16]. Another study evaluating high surgical risk patients undergoing TAVR from the FRANCE-2 registry found the rate of severe SVD and moderate to severe SVD at 5 year to be 2.5% and 13.3% respectively [17]. Five-year outcomes from high-risk patients enrolled in PARTNER 1 trial showed no SVD requiring surgical valve replacement in both TAVR and SAVR population, however, moderate-to-severe aortic regurgitation rate was higher in TAVR compared to SAVR (14% vs. 1%) and, when present, associated with worse mortality [18]. Five-year outcome from PARTNER 2 demonstrated that more patients in TAVR group had at least mild paravalvular aortic regurgitation (33.3% vs. 6.3%), as were aortic-valve reinterventions at 5 years, there was no significant difference in the incidence of death from any cause or disabling stroke between the TAVR group and the surgery group (47.9% and 43.4%) [19]. On the contrary, in the low surgical risk NOTION trial, at 6 year follow up, moderate-to-severe SVD was higher in SAVR population compared to TAVR population (24% vs. 4.8%) [20]. Moreover, emerging data on newer generation valves is revealing very low incidence of SVD up to at least 5 years following the intervention [21]. This evidence does support the efficacy of TAVR for the intermediate term, but more studies are required to validate these findings and to determine the long-term durability of TAVR compared to SAVR.
Accordingly, our meta-analysis provides the conceptualized framework for temporal changes in hard outcomes over the previous 15–20 years due to the constant evolution of technological advances. It represents the paradigm shift of post procedural stroke at 1 year over the decade favoring TAVR over SAVR populations. It also provides the framework for evidence to support the current practice for giving preference to TAVR for prohibitive and high surgical risk patients, while validating its applicability in intermediate and selected low surgical risk populations due to comparable all-cause and cardiovascular mortality with SAVR population.
Importantly, rehospitalization rates were higher in the SAVR compared to TAVR population and one needs to consider the potential increase burden in healthcare utilization from this aspect. The economic evaluation of medical technologies is usually performed by cost-effectiveness analysis. Quality adjusted life years (QALYs) and incremental cost effectiveness ratio (ICER) are two valuable parameters used for this purpose as described by Baron et al. [22]. The American Heart Association and American College of Cardiology have created a general guideline in which an ICER < $50,000/QALY gained is considered to be of a high economic value, $50,000 to $150,000/QALY is considered to be of an intermediate value and an ICER > $150,000/QALY is considered to be of a low valve in US healthcare system [23]. As demonstrated by Baron et al., TAVR was cost-effective in prohibitive and high-risk populations, and cost-saving in intermediate risk population, despite high procedural cost of TAVR compared to SAVR [22]. Meduri et al. exhibited a similar analysis that when taking all costs into account; overall there are comparable expenditures in both TAVR and SAVR groups. Similarly, Baron et al. demonstrated that TAVR is estimated to be beneficial in providing grater quality adjusted life expectancy along with lower long-term cost for the US healthcare system [24].
Limitations
Our study has certain limitations. We could not control the inherent variations among the included studies including baseline characteristics, different vascular access, type of the implanted valves and different expertise of centers where these procedures were performed. Similarly, temporal trend analyses always have limitations. However, in order to incorporate the inherent limitations utilizing a meta-analysis, a far more sophisticated computation approach using ‘R program meta’ was herein utilized with the guidance of two mathematicians/ statisticians (GR and MD). We note that there is always a chance of publication bias in meta-analysis. Here, Abramowitz et al. contributed a larger number of patients even though that was not clearly seen on our funnel plot analysis [25]. Another inherent limitation of our meta-analysis is that we were not able to incorporate data at the individual patient level, but in study groups based on the published studies, thus possibly underestimating the temporal changes between these procedures. This is a well understood limitation not unique to our analysis. Also, very few studies had reported comparison between TAVR and SAVR data hence certain statistics could not be applied for entire population. The cohorts were not stratified by risk and year combined as we did not have enough patient population to perform accurate analysis. We did not include other adverse clinical outcomes such as paravalvular leak, concomitant (other than SAVR) cardiothoracic intervention, permanent pacemaker implantation or vascular complications which may play a role in the surgical decision over either of these modalities. Also, data on new onset AFib post procedural were not reported in all the studies. Although our study provides considerable of insightful information for early to intermediate outcomes, we are unable to comment on the long-term outcomes for valve durability and degeneration.
Conclusion
While there is a trend for overall improvement over nearly 2 decades in both TAVR and SAVR outcomes, our integration of over 65,000 patients incorporating 23 studies, in aggregate, failed to robustly demonstrate that either outperforms the other when it comes to hard short-term outcomes, supporting no distinct separation in all-cause mortality and adjudicated cardiovascular mortality at 1-year between groups except for the highest surgical risk population who shared lower post procedural stroke, cardiovascular and all-cause mortality at 1-year. We propose that this has substantial socio-economic implications as we contemplate further expansion of our TAVR indications to low/intermediate risk populations.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AS:
-
Aortic stenosis
- TAVR:
-
Transcatheter aortic valve replacement
- SAVR:
-
Surgical aortic valve replacement
- AFib:
-
Atrial fibrillation
- PRISMA:
-
Preferred Reported Items for Systematic Reviews and Meta-analyses
- RCT:
-
Randomized clinical trial
- ROBIN-I:
-
Risk Of Bias In Non-Randomized Studies of Interventions
- STS:
-
Society of Thoracic Surgeons
- EuroSCORE:
-
European System for Cardiac Operative Risk Evaluation
- RR:
-
Relative risk
- FDA:
-
Food and Drug Administration
- SVD:
-
Structural valve degeneration
- QALYs:
-
Quality adjusted life years
- ICER:
-
Incremental cost effectiveness ratio
References
Bonow RO, Brown AS, Gillam LD, Kapadia SR, Kavinsky CJ, Lindman BR, et al. ACC/AATS/AHA/ASE/EACTS/HVS/SCA/SCAI/SCCT/SCMR/STS 2017 appropriate use criteria for the treatment of patients with severe aortic stenosis. A report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, European Association for Cardio-Thoracic Surgery, Heart Valve Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. Eur J Cardio Thorac Surg. 2017;70(20):2566–98.
Adams DH, Popma JJ, Reardon MJ, Yakubov SJ, Coselli JS, Deeb GM, et al. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med. 2014;370(19):1790–8.
Kodali SK, Williams MR, Smith CR, Svensson LG, Webb JG, Makkar RR, et al. Two-year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med. 2012;366(18):1686–95.
Popma JJ, Adams DH, Reardon MJ, Yakubov SJ, Kleiman NS, Heimansohn D, et al. Transcatheter aortic valve replacement using a self-expanding bioprosthesis in patients with severe aortic stenosis at extreme risk for surgery. J Am Coll Cardiol. 2014;63(19):1972–81.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2013.
Balduzzi SRG, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22:153–60.
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Fleisher LA, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25):e1159–95.
Coylewright M, Forrest JK, McCabe JM, Nazif TM. TAVR in low-risk patients: FDA approval, the new NCD, and shared decision-making. J Am Coll Cardiol. 2020;75(10):1208–11.
Eze-Nliam CM, Zhang Z, Weiss SA, Weintraub WS. Cost-effectiveness assessment of cardiac interventions: determining a socially acceptable cost threshold. Interv Cardiol (London). 2014;6(1):45–55.
Filardo G, Hamilton C, Hamman B, Hebeler RF Jr, Adams J, Grayburn P. New-onset postoperative atrial fibrillation and long-term survival after aortic valve replacement surgery. Ann Thorac Surg. 2010;90(2):474–9.
Carter-Storch R, Dahl JS, Christensen NL, Pecini R, Sondergard EV, Ovrehus KA, et al. Postoperative atrial fibrillation after aortic valve replacement is a risk factor for long-term atrial fibrillation. Interact Cardiovasc Thorac Surg. 2019;29(3):378–85.
Park-Hansen J, Greve AM, Clausen J, Holme SJ, Carranza CL, Irmukhamedov A, et al. New-onset of postoperative atrial fibrillation is likely to recur in the absence of other triggers. Ther Clin Risk Manag. 2018;14:1641–7.
Lin MH, Kamel H, Singer DE, Wu YL, Lee M, Ovbiagele B. Perioperative/postoperative atrial fibrillation and risk of subsequent stroke and/or mortality. Stroke. 2019;50(6):1364–71.
Chakravarty T, Patel A, Kapadia S, Raschpichler M, Smalling RW, Szeto WY, et al. Anticoagulation after surgical or transcatheter bioprosthetic aortic valve replacement. J Am Coll Cardiol. 2019;74(9):1190–200.
Blackman DJ, Saraf S, MacCarthy PA, Myat A, Anderson SG, Malkin CJ, et al. Long-term durability of transcatheter aortic valve prostheses. J Am Coll Cardiol. 2019;73(5):537–45.
Didier R, Eltchaninoff H, Donzeau-Gouge P, Chevreul K, Fajadet J, Leprince P, et al. Five-year clinical outcome and valve durability after transcatheter aortic valve replacement in high-risk patients. Circulation. 2018;138(23):2597–607.
Mack MJ, Leon MB, Smith CR, Miller DC, Moses JW, Tuzcu EM, et al. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet. 2015;385(9986):2477–84.
Makkar RR, Thourani VH, Mack MJ, Kodali SK, Kapadia S, Webb JG, et al. Five-year outcomes of transcatheter or surgical aortic-valve replacement. N Engl J Med. 2020;382(9):799–809.
Sondergaard L, Ihlemann N, Capodanno D, Jorgensen TH, Nissen H, Kjeldsen BJ, et al. Durability of transcatheter and surgical bioprosthetic aortic valves in patients at lower surgical risk. J Am Coll Cardiol. 2019;73(5):546–53.
Abdel-Wahab M, Landt M, Neumann F-J, Massberg S, Frerker C, Kurz T, et al. 5-year outcomes after tavr with balloon-expandable versus self-expanding valves. Results From the CHOICE Randomized Clinical Trial. 2020;13(9):1071–82.
Baron S, Cohen DJ. Economic considerations for TAVR versus SAVR: historical perspective and future predictions. Expert analysis. Am Coll Cardiol. 2019. https://www.acc.org/latest-in-cardiology/articles/2019/06/18/07/43/economic-considerations-for-tavr-vs-savr.
Anderson JL, Heidenreich PA, Barnett PG, Creager MA, Fonarow GC, Gibbons RJ, et al. ACC/AHA statement on cost/value methodology in clinical practice guidelines and performance measures: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(21):2304–22.
Baron SJ, Wang K, House JA, Magnuson EA, Reynolds MR, Makkar R, et al. Cost-effectiveness of transcatheter versus surgical aortic valve replacement in patients with severe aortic stenosis at intermediate risk. Circulation. 2019;139(7):877–88.
Abramowitz Y, Vemulapalli S, Chakravarty T, Li Z, Kapadia S, Holmes D, et al. Clinical impact of diabetes mellitus on outcomes after transcatheter aortic valve replacement: insights from the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. Circ Cardiovasc Interv. 2017;10(11):e005417.
Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364(23):2187–98.
Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016;374(17):1609–20.
Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 2019;380(18):1695–705.
Thyregod HG, Steinbruchel DA, Ihlemann N, Nissen H, Kjeldsen BJ, Petursson P, et al. Transcatheter versus surgical aortic valve replacement in patients with severe aortic valve stenosis: 1-year results from the all-comers NOTION randomized clinical trial. J Am Coll Cardiol. 2015;65(20):2184–94.
Reardon MJ, Van Mieghem NM, Popma JJ, Kleiman NS, Sondergaard L, Mumtaz M, et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017;376(14):1321–31.
Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O’Hair D, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. 2019;380(18):1706–15.
Waksman R, Rogers T, Torguson R, Gordon P, Ehsan A, Wilson SR, et al. Transcatheter aortic valve replacement in low-risk patients with symptomatic severe aortic stenosis. J Am Coll Cardiol. 2018;72(18):2095–105.
Castrodeza J, Amat-Santos IJ, Blanco M, Cortes C, Tobar J, Martin-Morquecho I, et al. Propensity score matched comparison of transcatheter aortic valve implantation versus conventional surgery in intermediate and low risk aortic stenosis patients: a hint of real-world. Cardiol J. 2016;23(5):541–51.
Chopard R, Teiger E, Meneveau N, Chocron S, Gilard M, Laskar M, et al. Baseline characteristics and prognostic implications of pre-existing and new-onset atrial fibrillation after transcatheter aortic valve implantation: results From the FRANCE-2 Registry. JACC Cardiovasc Interv. 2015;8(10):1346–55.
Tarantini G, Mojoli M, Windecker S, Wendler O, Lefevre T, Saia F, et al. Prevalence and impact of atrial fibrillation in patients with severe aortic stenosis undergoing transcatheter aortic valve replacement: an analysis from the SOURCE XT Prospective Multicenter Registry. JACC Cardiovasc Interv. 2016;9(9):937–46.
Yankelson L, Steinvil A, Gershovitz L, Leshem-Rubinow E, Furer A, Viskin S, et al. Atrial fibrillation, stroke, and mortality rates after transcatheter aortic valve implantation. Am J Cardiol. 2014;114(12):1861–6.
Sannino A, Stoler RC, Lima B, Szerlip M, Henry AC, Vallabhan R, et al. Frequency of and prognostic significance of atrial fibrillation in patients undergoing transcatheter aortic valve implantation. Am J Cardiol. 2016;118(10):1527–32.
Nombela-Franco L, Webb JG, de Jaegere PP, Toggweiler S, Nuis RJ, Dager AE, et al. Timing, predictive factors, and prognostic value of cerebrovascular events in a large cohort of patients undergoing transcatheter aortic valve implantation. Circulation. 2012;126(25):3041–53.
Tay EL, Gurvitch R, Wijesinghe N, Nietlispach F, Wood D, Cheung A, et al. A high-risk period for cerebrovascular events exists after transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2011;4(12):1290–7.
Stortecky S, Buellesfeld L, Wenaweser P, Heg D, Pilgrim T, Khattab AA, et al. Atrial fibrillation and aortic stenosis: impact on clinical outcomes among patients undergoing transcatheter aortic valve implantation. Circ Cardiovasc Interv. 2013;6(1):77–84.
Muneretto C, Bisleri G, Moggi A, Di Bacco L, Tespili M, Repossini A, et al. Treating the patients in the “grey-zone” with aortic valve disease: a comparison among conventional surgery, sutureless valves and transcatheter aortic valve replacement. Interact Cardiovasc Thorac Surg. 2015;20(1):90–5.
Barbash IM, Minha S, Ben-Dor I, Dvir D, Torguson R, Aly M, et al. Predictors and clinical implications of atrial fibrillation in patients with severe aortic stenosis undergoing transcatheter aortic valve implantation. Catheter Cardiovasc Interv. 2015;85(3):468–77.
Maan A, Heist EK, Passeri J, Inglessis I, Baker J, Ptaszek L, et al. Impact of atrial fibrillation on outcomes in patients who underwent transcatheter aortic valve replacement. Am J Cardiol. 2015;115(2):220–6.
Yoon YH, Ahn JM, Kang DY, Ko E, Lee PH, Lee SW, et al. Incidence, predictors, management, and clinical significance of new-onset atrial fibrillation after transcatheter aortic valve implantation. Am J Cardiol. 2019;123(7):1127–33.
Abdelgawad AME, Hussein MA, Naeim H, Abuelatta R, Alghamdy S. A comparative study of TAVR versus SAVR in moderate and high-risk surgical patients: hospital outcome and midterm results. Heart Surg Forum. 2019;22(5):E331–9.
Zweiker D, Froschl M, Tiede S, Weidinger P, Schmid J, Manninger M, et al. Atrial fibrillation in transcatheter aortic valve implantation patients: Incidence, outcome and predictors of new onset. J Electrocardiol. 2017;50(4):402–9.
Acknowledgements
None.
Author information
Authors and Affiliations
Contributions
AP: Conceptualization; data curation; writing—original draft; writing—review and editing. AK: Supervision; validation; writing—review and editing. GR: Formal analysis; methodology. MD: Formal analysis; methodology; writing—review and editing. RWWB: Conceptualization; investigation; supervision; validation; writing—review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Panchal, A., Kyvernitakis, A., Rayarao, G. et al. Propitious temporal changes in clinical outcomes after transcatheter compared to surgical aortic valve replacement; a meta-analysis of over 65,000 patients. J Cardiothorac Surg 16, 312 (2021). https://doi.org/10.1186/s13019-021-01689-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-021-01689-3