Abstract
Background
Oesophageal atresia is a congenital malformation of the oesophagus and a serious malformation of the digestive system, postoperative complications include acute respiratory failure, pneumonia, anastomotic fistula, anastomotic stenosis, tracheal stenosis, gastroesophageal reflux and eosinophilic oesophagitis, anastomotic fistula is one of the important causes of postoperative death. The objective of this study is to identify the risk factors for anastomotic complications after one-stage anastomosis for oesophageal atresia.
Methods
A retrospective analysis was performed on the clinical data of 107 children with congenital oesophageal atresia who underwent one-stage anastomosis in our hospital from January 2013 to December 2018. Single-factor and multivariate logistic regression analyses were performed to determine the risk factors for anastomotic fistula and anastomotic stenosis.
Results
A total of 107 children with oesophageal atresia underwent one-stage anastomosis, and the incidence of anastomotic fistula was 26.2%. The probability of anastomotic stenosis in the long term was 52.3%, and the incidence of refractory stenosis (dilation ≥5 times) was 13.1%. Analysis of the clinical count data in the anastomotic fistula group and non-anastomotic fistula group showed that preoperative albumin (F = 4.199, P = 0.043), low birth weight (F = 7.668, P = 0.007) and long gap defects (F = 6.107, P = 0.015) were risk factors for postoperative anastomotic fistula. Further multivariate logistic regression analysis showed that low birth weight (Wald2 = 4.499, P = 0.034, OR = 2.775) and long gap defects (Wald2 = 6.769, P = 0.009, OR = 4.939) were independent risk factors for postoperative anastomotic fistula. Premature delivery (F = 5.338, P = 0.023), anastomotic fistula (F = 11.381, P = 0.001), endoscopic surgery (F = 6.343, P = 0.013), preoperative neutrophil count (F = 8.602, P = 0.004), preoperative low albumin (F = 8.410, P = 0.005), and a preoperative prognostic nutritional index < 54 (F = 5.54, P = 0.02) were risk factors for refractory anastomotic stenosis in children. Further multivariate logistic regression analysis showed that postoperative anastomotic fistula (Wald2 = 11.417, P = 0.001, OR = 8.798), endoscopic surgery (Wald2 = 9.633, P = 0.002, OR = 4.808), and a prognostic nutritional index < 54 (Wald2 = 4.540, P = 0.002, OR = 2.3798) were independent risk factors for refractory anastomotic stenosis.
Conclusion
Low birth weight and long gap defects are important predictors of postoperative anastomotic fistula, and the possibility of refractory anastomotic stenosis should be considered. The long-term risk of anastomotic stenosis was increased in children undergoing endoscopic surgery and in those with a preoperative prognostic nutritional index < 54.
Similar content being viewed by others
Background
Oesophageal atresia (EA) is a congenital malformation of the oesophagus and a serious malformation of the digestive system. The global overall incidence is 2.4 cases per 100,000, and the incidence of congenital EA in China is 1/1250–1/4000 [1]. At present, this disease is believed to be due to the interruption of oesophageal continuity caused by abnormal development of the preembryonic intestinal area. Approximately 70–90% of children often have tracheal oesophageal fistula (TEF) [2], and 55% of children may have other systemic congenital malformations, especially severe heart malformations, which is an important factor for poor prognosis in children [3]. The treatment of EA has made great progress in the past 20 years, and the survival rate can reach more than 90%. With the development of endoscopic technology in recent years, video-assisted one-stage anastomosis has gradually become the main surgical method instead of open-chest operations.
Common EA postoperative complications include acute respiratory failure, pneumonia, anastomotic fistula, anastomotic stenosis, tracheal stenosis, gastroesophageal reflux and eosinophilic oesophagitis [4]. Anastomotic complications mainly include recent postoperative anastomotic fistula and refractory anastomotic stenosis, and anastomotic fistula is one of the important causes of postoperative death. Severe anastomotic fistula may increase the risk of refractory anastomotic stenosis [5]. This study attempts to explore the related risk factors for postoperative anastomotic complications in children with congenital EA through a retrospective study.
Methods
Excluded two infants with EA type Vogt II and another with IV, data from the 127 children born in or admitted to our hospital with EA type Vogt IIIb were collected and followed, with 14 of the parents of sick children refusing surgery. A total of 113 children received surgical treatment, and 6 died perioperatively; thus, 107 children were enrolled. The patients were divided into two groups according to the occurrence of anastomotic fistula.
General conditions
From January 2013 to December 2018, 107 children with EA underwent surgery in our hospital with complete clinical and pathological data; there were 74 male patients and 33 female patients. The data of sex, birth weight, gestational age, surgical method, defect length (intraoperative measurement), preoperative mechanical ventilation, and combined deformity were collected (Table 1).
Preoperative data
-
1)
Serological indicators: the preoperative neutrophil count, preoperative lymphocyte count, and neutrophil to lymphocyte ratio (NLR).
-
2)
Nutritional indicators: the preoperative albumin, prognostic nutritional index (PNI) and albumin to globulin ratio. PNI = 10ALB(dg/L) + 5*LYMPH#.
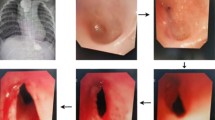
Key operative steps
Open surgery
Right posterolateral thoracotomy, extrapleural approach to the posteromedial mediastinum, to expose the TEF, and futher ligation is undertaken using Hem-o-Lok clips (Sinolinks clips; Sinolinks Medical Innovation,inc. Jiangsu, China). Following TEF ligation, upper pouch is dissected and incised in readiness for anastomosis. Oesophageal anastomosis with fine interrupted sutures begins with the back wall, following which a trans-anastomotic nasogastric tube is passed prior to completion of the anastomosis of the front wall.
Thoracoscopic surgery
The first step is to identify the TEF. The TEF is dissected and ligated using Hem-o-Lok clips. The upper pouch is identified and dissected with the aid of gentle pressure on the 10 Fr tube. The anastomosis is performed using interrupted sutures secured by intracorporeal ties. Once complete, a chest tube may be left through one of the port site incisions.
Postoperative data
Anastomotic fistula, anastomotic stenosis, pulmonary infection, oesophageal dilatation times and first dilatation time.
Inclusion criteria
Children born or admitted to our hospital with congenital EA and receiving stage I anastomosis with complete clinical data. The exclusion criteria were as follows: 1. parents refused the operation; 2. patients who could not undergo delayed anastomosis in the first stage of the operation; 3. patients who died in the perioperative period.
1.6 SPSS 22.0 software was used to analyse the data, and univariate and multivariate logistic regression analyses were performed for EA anastomotic fistula and anastomotic stenosis. The odds ratio (OR) and 95% confidence interval (95% CI) were used to indicate the correlation. T tests were used for the comparison of oesophageal dilatation analysis results, and P < 0.05 was considered statistically significant.
Results
Recent anastomotic complications: anastomotic fistula
Anastomotic fistula is a common and dangerous recent anastomotic complication of oesophageal reconstruction. In this study, the incidence of anastomotic fistula was 26.3%, which is slightly higher than the 20% reported in other studies [6]. The occurrence of anastomotic fistula after anastomosis in adults is mainly related to anastomotic tension and anastomotic blood supply [7]. It is difficult to quantitatively evaluate anastomotic tension and anastomotic blood supply during neonatal EA stage I anastomosis. In this study, clinical enumeration data were collected to seek objective clinical indicators to assess the risk of anastomotic complications. With the analysis of two groups of data, continuous variables using single-factor analysis of variance and classification variables using the chi-square test, the study found that preoperative albumin, birth weight and defect length were postoperative anastomotic fistula-related factors. The differences between groups were statistically significant, and the time, gestational age, sex, preoperative operation method of mechanical ventilation, neutrophil count, lymphocyte count, NLR, PNI, albumin, globulin, and merged heart deformities were not significantly different between these factors in the two groups. Further multivariate logistic regression analysis showed that a birth weight less than 2500 g and long gap defects larger than 3 cm were independent risk factors for postoperative anastomotic fistula in children. (Table 2 & Table 3).
Refractory anastomotic complications: anastomotic stenosis
Anastomotic stricture: symptoms of dysphagia and anastomotic stricture were confirmed by gastrointestinal radiography or endoscopy. This study found that the surgical method, gestational age, preoperative neutrophil count, PNI and anastomotic fistula may be related factors for the occurrence of anastomotic stenosis. Further multivariate logistic regression analysis found that open surgery, anastomotic fistula and low nutritional status (PNI ≤54) were high-risk factors for refractory anastomotic stenosis (Table 4 & Table 5).
Discussion
Risk factor analysis of recent anastomotic fistula
The occurrence of anastomotic fistula after first-stage oesophagostomy in children with congenital EA is still a serious complication that troubles surgeons and has an important influence on the prognosis and quality of life of children [8]. The occurrence of anastomotic fistula is mainly related to anastomotic blood supply, anastomotic tension and other factors [9, 10]. The incidence of anastomotic fistula after end-to-end oesophagostomy is reported to be approximately 8–12% in adults [11], and the incidence of anastomotic fistula after EA is approximately 20% [3]. This may be related to the large anastomotic tension and poor anastomotic blood supply caused by oesophageal defects. In this study, univariate analysis found that albumin, defect length and birth weight may be related to the occurrence of anastomotic fistula. Multivariate logistic regression analysis found that long gap defects and low birth weight were high risk factors for anastomotic fistula.
Preoperative low protein may lead to postoperative anastomotic oedema patients, which increases anastomotic tension and leads to poor local healing [12, 13]. However, in multiple factor analysis, albumin levels were not included in the regression equation. This may be because, in this study, the number of patients with low albumin (albumin < 28 g/L) was less relevant, further expanding the sample size to find the best values for a more suitable cut-off value to evaluate the relationship between albumin levels and anastomotic fistula.
The defect length is one of the important indexes for the preoperative evaluation of operation difficulty in children with EA [14]. In this study, the mean defect length was 1.53 ± 0.96 cm, 1.91 ± 1.01 cm in children with anastomotic fistula, and 1.39 ± 0.91 cm in children without anastomotic fistula, showing statistically significant differences. There were 14 patients with long gap EA, and the possibility of anastomotic fistula was 4.9 times that of non-long-gap EA. Long defects are an independent risk factor for anastomotic fistula. Children with an intraoperative defect length > 3 cm were more prone to anastomotic fistula 7 to 10 days after surgery. Four cases were excluded from this study due to intrathoracic extension and delayed anastomosis of long gap EAs. Fourteen cases of long gap EAs appeared among 8 cases of severe anastomotic fistula. We believe that the use of long gap defects to extend the anastomosis may be a better choice.
Birth weight reflects the developmental level of children in utero, and a low birth weight is often associated with a history of premature birth and foetal distress [15]. Children with a low birth weight may have more oesophageal defects due to the short duration of natural extension of the oesophagus in utero, and these defects may be accompanied by poorer peripheral circulation and lower cardiac output [16], which may lead to poor local blood supply at the anastomosis. The counting data showed that 8 of 32 children with a low birth weight had heart malformations, while only 6 of 75 children with a normal weight had heart malformations. This study found that the risk of anastomotic fistula was 2.7 times higher in children with a low birth weight than in children with a normal weight.
Risk factor analysis of refractory anastomotic stenosis
European Society of Gastrointestinal Endoscopy (ESGE) and European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) suggest the following definition of a benign refractory stricture in children: After 5 dilation sessions with maximal 4-week intervals, there is an inability to successfully remediate the anatomic problem to obtain age-appropriate feeding possibilities [17]. In this study, the probability of anastomotic stenosis was 52.3%, and the risk of anastomotic stenosis factors, including anastomotic fistula, long defects, severe gastroesophageal reflux and eosinophilic oesophagitis [18, 19], may cause inflammation of the anastomotic fistula after conservative treatment as well as related scar factors. Anastomotic fistula was one of the most relevant factors, OR = 7.506, but the length of the defect was not included in the regression equation. Univariate analysis revealed that the surgical method, gestational age, preoperative neutrophil count, and PNI may also be related factors. In multivariate analysis, thoracoscopic surgery, anastomotic fistula, and low nutritional status (PNI ≤54) were high risk factors for anastomotic stenosis. The incidence of anastomotic stenosis after thoracoscopic surgery was 32/49, which was significantly higher than that after open surgery (24/58). Open surgery may provide better oesophageal mucosal alignment and firmer end-to-end anastomosis. Thoracoscopic oesophageal anastomosis is still under development, and it is believed that the incidence of anastomotic stenosis in endoscopic surgery will decrease with the maturity of endoscopic technology in the future. According to the results of this study, thoracoscopic surgery is still considered to increase the risk of anastomotic stenosis.
Most anastomotic fistulas can be cured by conservative treatment, including total parenteral nutrition support or post-pyloric enteral nutrition support, pleural drainage and adequate antibiotic use [20, 21]. Some scholars advocate early operations to close the fistula in order to avoid severe pulmonary infection and empyema [22, 23]. Anastomotic fistula leads to severe anastomotic inflammation. Although conservative treatment is successful, it is still inevitable that the incidence of anastomotic stenosis will increase or even develop into refractory anastomotic stenosis due to scarring [24].
At present, there are few studies on nutritional assessment indicators for neonates, and the PNI is a commonly used nutritional assessment indicator for gastrointestinal tumours in adults [25]. Univariate analysis found that the preoperative difference in PNI values between the two groups was statistically significant. At present, there is no clear numerical classification of neonatal nutritional risk with the PNI. By calculating the Youden index, we obtained the optimal truncation value of the PNI value in this sample to be 54. Based on this, we conducted a multifactor analysis and found that the risk of anastomotic stenosis in children in the low PNI group (PNI ≤54) was 5.7 times higher than that in the high PNI group. For children with preoperative nutritional risk, perioperative nutritional support may help reduce the risk of refractory anastomotic stenosis, which needs to be further confirmed by future prospective studies.
Conclusion
Low birth weight and long gap defects are important predictors of postoperative anastomotic fistula, and the possibility of refractory anastomotic stenosis should be considered. The long-term risk of anastomotic stenosis was increased in children undergoing endoscopic surgery and in those with a preoperative prognostic nutritional index < 54.
Availability of data and materials
Written informed consent was obtained from the patients for publication of this article.
Abbreviations
- EA:
-
Oesophageal atresia
- TEF:
-
Tracheal oesophageal fistula
- NLR:
-
Neutrophil to lymphocyte ratio
- PNI:
-
Prognostic nutritional index
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- VATS:
-
Video-assisted thoracic surgery
- UPJO:
-
Uretero pelvic juriction obstruction
References
Pedersen RN, Calzolari E, Husby S, Garne E, EUROCAT Working group*. Oesophageal atresia: prevalence, prenatal diagnosis and associated anomalies in 23 European regions. Arch Dis Child. 2012;97(3):227–32. https://doi.org/10.1136/archdischild-2011-300597.
Thomas B, Nadine Z, Vera C, et al. Esophageal atresia with or without tracheoesophageal fistula (EA/TEF): Association of Different EA/TEF subtypes with specific co-occurring congenital anomalies and implications for diagnostic workup. Eur J Pediatr Surg. 2018;28:176–82.
van Lennep M, Singendonk MMJ, Dall'Oglio L, et al. Oesophageal atresia. Nat Rev Dis Primers. 2019;5(1):26. https://doi.org/10.1038/s41572-019-0077-0.
R Daum. Postoperative complications following operation for oesophageal atresia and tracheo-oesophageal fistula. Progress Pediatr Surg. 1970;1(1):209.
Robert B, Jean-Martin L, Dominique L. Anastomotic stricture after esophageal atresia repair: a critical review of recent literature. Eur J Pediatr Surg. 2013;23:204–13.
Helena R, Lucas M, Charlotte V, et al. Multicentre survey on the current surgical management of oesophageal atresia in Belgium and Luxembourg. J Pediatr Surg. 2017;52:239–46.
Korenaga D, Toh Y, Maekawa S, Ikeda T, Sugimachi K. Intra-operative measurement of the tissue blood flow for evaluating blood supply to the gastric tube for esophageal reconstruction. Hepatogastroenterology. 1998;45(24):2179–80.
Céline L, Laurent M, Julia S, et al. Long-term outcome of children with oesophageal atresia type III. Arch Dis Child. 2012;97:808–11.
Oscar Å, Dan F, Göran J, et al. Surface microdialysis detects ischemia after esophageal resection-an experimental animal study. J Surg Res. 2020;245:537–43.
Lyall P, Bao-Quan Q, Beasley S. The effect of neck flexion on oesophageal tension in the pig and its relevance to repaired oesophageal atresia. Pediatr Surg Int. 2001;17(2-3):193–5. https://doi.org/10.1007/s003830000457.
Turkyilmaz A, Eroglu A, Aydin Y, Tekinbas C, Muharrem Erol M, Karaoglanoglu N. The management of esophagogastric anastomotic leak after esophagectomy for esophageal carcinoma. Dis Esophagus. 2009;22(2):119–26. https://doi.org/10.1111/j.1442-2050.2008.00866.x.
Jinxi H, Yi Z, Wang C, et al. Logistic regression analysis of the risk factors of anastomotic fistula after radical resection of esophageal-cardiac cancer. Thorac Cancer. 2017;8:666–71.
Kudsk Kenneth A,Tolley Elizabeth A, De Witt R Chance, et al. Preoperative albumin and surgical site identify surgical risk for major postoperative complications. JPEN J Parenter Enteral Nutr, 2003, 27: 1–9, 1, DOI: https://doi.org/10.1177/014860710302700101.
Stadil T, Koivusalo A, Svensson JF, Jönsson L, Lilja HE, Thorup JM, et al. Surgical treatment and major complications within the first year of life in newborns with long gap esophageal atresia gross type a and B - a systematic review. J Pediatr Surg. 2019;54(11):2242–9. https://doi.org/10.1016/j.jpedsurg.2019.06.017.
Anil KC, Lal BP, Sarswoti S. Low birth weight and its associated risk factors: Health facility-based case-control study. PLoS ONE. 2020;15:e0234907.
Meredith K, Patrick HC, Anthony RC, et al. Perfusion index in the very preterm infant. Acta Paediatr. 2013;102:e398–401.
Tringali A, Thomson M, Dumonceau JM, Tavares M, Tabbers MM, Furlano R, et al. Pediatric gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy (ESGE) and European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) guideline executive summary. Endoscopy. 2017;49(1):83–91. https://doi.org/10.1055/s-0042-111002.
Yuichi O, Kosaku M, Yuko B, et al. Evaluation of the intraoperative risk factors for esophageal anastomotic complications after primary repair of esophageal atresia with tracheoesophageal fistula. Pediatr Surg Int. 2016;32:869–73.
Shah R, Varjavandi V, Krishnan U. Predictive factors for complications in children with esophageal atresia and tracheoesophageal fistula. Dis Esophagus. 2015;28(3):216–23. https://doi.org/10.1111/dote.12177.
Xu C, Yuanbin H, Liu C, et al. The Value of Thoracic Lavage in the Treatment of Anastomotic Leakage After Surgery for Type III Esophageal Atresia. Med Sci Monit. 2020;26:e919962.
D'Urzo C, et al., Major anastomotic dehiscence after repair of esophageal atresia: conservative management or reoperation? Dis Esophagus. 2005;18(2):120–3.
Godoy J, Ferraris T and Guelfand M. Early Management of Esophageal Leak in Esophageal Atresia: Changing Paradigms. J Laparoendosc Adv Surg Tech A. 2020;30(8):923–6.
Indalecio CN, Belén AC, Jorge GL, et al. Thoracoscopic approach for complications after esophageal atresia repair: initial experience. Asian J Endosc Surg. 2020;13:147–51.
Vergouwe Floor WT, John V, Hanneke IJ, et al. Risk factors for refractory anastomotic strictures after oesophageal atresia repair: a multicentre study. Arch Dis Child. 2019;104:152–7.
Kazuo O, Yoshifumi B, Taisuke Y, et al. Prognostic nutritional index, tumor-infiltrating lymphocytes, and prognosis in patients with esophageal Cancer. Ann Surg. 2020;271:693–700.
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Jin-Xi Huang participated in clinical practice, contributed to collection and analysis of data, drafting the manuscript, and revising it. Song-Ming Hong carried out data collection. Qiang Chen participated in clinical practice. Dian-Ming Wu and Jun-Jie Hong helped in design of study and drafting the manuscript. Chaoming Zhou carried out patient recruitment and clinical practice, contributed to conception, design, drafting the manuscript, and revising it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The hospital ethics committee approval was granted of this article. Consent for publication was obtained from the children’s parents.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, JX., Hong, SM., Chen, Q. et al. Risk factors for anastomotic complications after one-stage anastomosis for oesophageal atresia. J Cardiothorac Surg 16, 176 (2021). https://doi.org/10.1186/s13019-021-01557-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-021-01557-0