Abstract
Esophageal atresia with/without tracheoesophageal fistula (EA/TEF) is a congenital digestive tract anomaly that represents a major therapeutic challenge. Postoperative digestive morbidities such as gastroesophageal reflux disease (GERD) and esophageal stricture are common. The aim of this study was to identify the incidence of and potential risk factors for digestive morbidities after EA/TEF repair. We retrospectively reviewed all EA/TEF patients who underwent repair at a single institution between January 1999 and December 2018, excluding patients who died prior to discharge. Patient demographics, perioperative management, and postoperative GERD and esophageal stricture rates were collected. We performed univariate and multivariate analyses to examine risk factors associated with postoperative GERD and esophageal stricture. The study enrolled 58 infants (58.6% male, 17.2% with type A EA/TEF, 62.1% with associated anomalies). Postoperative GERD occurred in 67.2% of patients and was the most common digestive morbidity. Esophageal stricture occurred in 37.9% of patients after EA/TEF repair. Multivariate analysis showed that long-gap EA/TEF and postoperative GERD were independent risk factors for esophageal stricture after repair surgery.
Conclusion: The incidence of postoperative GERD and esophageal stricture was 67.2% and 37.9%, respectively. The risk factors for postoperative esophageal stricture were long-gap EA/TEF and postoperative GERD.
What is Known: • EA/TEF is a congenital digestive tract anomaly with a high postoperative survival rate but can be complicated by many long-term morbidities. | |
What is New: • Long-gap EA/TEF and postoperative GERD are risk factors of anastomotic stricture after repair. • Surgeons and pediatricians should be highly experienced in managing anastomotic tension and the GERD. |

Similar content being viewed by others
Abbreviations
- BW:
-
Birth weight
- CHD:
-
Congenital heart disease
- EA/TEF:
-
Esophageal atresia with/without tracheoesophageal fistula
- GERD:
-
Gastroesophageal reflux disease
- GA:
-
Gestational age
- MV:
-
Mechanical ventilation
- PDA:
-
Patent ductus arteriosus
- PFO:
-
Patent foramen ovale
References
Spitz L, Kiely E, Brereton RJ (1987) Esophageal atresia: five year experience with 148 cases. J Pediatr Surg 22(2):103–108. https://doi.org/10.1016/soo22-3468(87)80420-7
Pedersen RN, Calzolari E, Husby S, Garne E (2012) Oesophageal atresia: prevalence, prenatal diagnosis and associated anomalies in 23 European regions. Arch Dis Child 97(3):227–232. https://doi.org/10.1136/archdischild-2011-300597
Wang B, Tashiro J, Allan BJ, Sola JE, Parikh PP, Hogan AR, Neville HL, Perez EA (2014) A nationwide analysis of clinical outcomes among newborns with esophageal atresia and tracheoesophageal fistulas in the United States. J Surg Res 190(2):604–612. https://doi.org/10.1016/j.jss.2014.04.033
Sfeir R, Bonnard A, Khen-Dunlop N, Auber F, Gelas T, Michaud L, Podevin G, Breton A, Fouquet V, Piolat C, Lemelle JL, Petit T, Lavrand F, Becmeur F, Polimerol ML, Michel JL, Elbaz F, Habonimana E, Allal H, Lopez E, Lardy H, Morineau M, Pelatan C, Merrot T, Delagausie P, de Vries P, Levard G, Buisson P, Sapin E, Jaby O, Borderon C, Weil D, Gueiss S, Aubert D, Echaieb A, Fourcade L, Breaud J, Laplace C, Pouzac M, Duhamel A, Gottrand F (2013) Esophageal atresia: data from a national cohort. J Pediatr Surg 48(8):1664–1669. https://doi.org/10.1016/j.jpedsurg.2013.03.075
Sulkowski JP, Cooper JN, Lopez JJ, Jadcherla Y, Cuenot A, Mattei P, Deans KJ, Minneci PC (2014) Morbidity and mortality in patients with esophageal atresia. Surgery 156(2):483–491. https://doi.org/10.1016/j.surg.2014.03.016
Pini Prato A, Carlucci M, Bagolan P, Gamba PG, Bernardi M, Leva E, Paradies G, Manzoni C, Noccioli B, Tramontano A, Jasonni V, Vaccarella F, de Pascale S, Alberti D, Riccipetitoni G, Falchetti D, Caccia F, Pelizzo G, Schleef J, Lima M, Andriolo P, Franchella A, Cacciari A, Caravaggi F, Federici S, Andermarcher M, Perrino G, Codrich D, Camoglio FS, Chiarenza FS, Martino A, Appignani A, Briganti V, Caterino S, Cozzi D, Messina M, Rizzo A, Liotta L, Salerno D, Aceti MGR, Bartoli F, Romeo C, Esposito C, Lelli Chiesa PL, Clemente E, Mascia L, Cacciaguerra S, di Benedetto V, Licciardi S, de Grazia E, Ubertazzi M, Piazza G, Mattioli G, Rossi F, Nobili M (2015) A cross-sectional nationwide survey on esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 50(9):1441–1456. https://doi.org/10.1016/j.jpedsurg.2015.01.004
Koivusalo AI, Pakarinen MP, Rintala RJ (2013) Modern outcomes of oesophageal atresia: single centre experience over the last twenty years. J Pediatr Surg 48(2):297–303. https://doi.org/10.1016/j.jpedsurg.2012.11.007
Friedmacher F, Kroneis B, Huber-Zeyringer A, Schober P, Till H, Sauer H, Hollwarth ME (2017) Postoperative complications and functional outcome after esophageal atresia repair: results from longitudinal single-center follow-up. J Gastrointest Surg 21(6):927–935. https://doi.org/10.1007/s11605-017-3423-0
Acher CW, Ostlie DJ, Leys CM, Struckmeyer S, Parker M, Nichol PF (2016) Long-term outcomes of patients with tracheoesophageal fistula/esophageal atresia: survey results from tracheoesophageal fistula/esophageal atresia online communities. Eur J Pediatr Surg 26(6):476–480. https://doi.org/10.1055/s-0035-1570103
Menzies J, Hughes J, Leach S, Belessis Y, Krishnan U (2017) Prevalence of malnutrition and feeding difficulties in children with esophageal atresia. J Pediatr Gastroenterol Nutr 64(4):e100–e105. https://doi.org/10.1097/mpg.0000000000001436
Nomura A, Yamoto M, Fukumoto K, Takahashi T, Ohyama K, Sekioka A, Yamada Y, Urushihara N (2017) Evaluation of developmental prognosis for esophageal atresia with tracheoesophageal fistula. Pediatr Surg Int 33(10):1091–1095. https://doi.org/10.1007/s00383-017-4142-z
Patria MF, Ghislanzoni S, Macchini F, Lelii M, Mori A, Leva E, Principi N, Esposito S (2017) Respiratory morbidity in children with repaired congenital esophageal atresia with or without tracheoesophageal fistula. Int J Environ Res Public Health 14(10). https://doi.org/10.3390/ijerph14101136
Vergouwe FWT, Spoel M, van Beelen NWG, Gischler SJ, Wijnen RMH, van Rosmalen J, IJsselstijn H (2017) Longitudinal evaluation of growth in oesophageal atresia patients up to 12 years. Arch Dis Child Fetal Neonatal Ed 102(5):F417–f422. https://doi.org/10.1136/archdischild-2016-311598
Ev E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2007) Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335(7624):806–808. https://doi.org/10.1136/bmj.39335.541782.AD
Richardson DK, Corcoran JD, Escobar GJ, Lee SK (2001) SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J Pediatr 138(1):92–100. https://doi.org/10.1067/mpd.2001.109608
Stoll C, Alembik Y, Dott B, Roth MP (2017) Associated anomalies in cases with esophageal atresia. Am J Med Genet A 173(8):2139–2157. https://doi.org/10.1002/ajmg.a.38303
Rintala RJ, Pakarinen MP (2013) Long-term outcome of esophageal anastomosis. Eur J Pediatr Surg 23(3):219–225. https://doi.org/10.1055/s-0033-1347912
Tovar JA, Fragoso AC (2013) Gastroesophageal reflux after repair of esophageal atresia. Eur J Pediatr Surg 23(3):175–181. https://doi.org/10.1055/s-0033-1347911
Serhal L, Gottrand F, Sfeir R, Guimber D, Devos P, Bonnevalle M, Storme L, Turck D, Michaud L (2010) Anastomotic stricture after surgical repair of esophageal atresia: frequency, risk factors, and efficacy of esophageal bougie dilatations. J Pediatr Surg 45(7):1459–1462. https://doi.org/10.1016/j.jpedsurg.2009.11.002
Nice T, Tuanama Diaz B, Shroyer M, Rogers D, Chen M, Martin C, Beierle E, Chaignaud B, Anderson S, Russell R (2016) Risk factors for stricture formation after esophageal atresia repair. J Laparoendosc Adv Surg Tech A 26(5):393–398. https://doi.org/10.1089/lap.2015.0120
Okata Y, Maeda K, Bitoh Y, Mishima Y, Tamaki A, Morita K, Endo K, Hisamatsu C, Fukuzawa H, Yokoi A (2016) Evaluation of the intraoperative risk factors for esophageal anastomotic complications after primary repair of esophageal atresia with tracheoesophageal fistula. Pediatr Surg Int 32(9):869–873. https://doi.org/10.1007/s00383-016-3931-0
Donoso F, Lilja HE (2017) Risk factors for anastomotic strictures after esophageal atresia repair: prophylactic proton pump inhibitors do not reduce the incidence of strictures. Eur J Pediatr Surg 27(1):50–55. https://doi.org/10.1055/s-0036-1593607
Vergouwe FWT, Vlot J, IJsselstijn H, Spaander MCW, van Rosmalen J, Oomen MWN, Hulscher JBF, Dirix M, Bruno MJ, Schurink M, Wijnen RMH (2019) Risk factors for refractory anastomotic strictures after oesophageal atresia repair: a multicentre study. Arch Dis Child 104(2):152–157. https://doi.org/10.1136/archdischild-2017-314710
Campos J, Tan Tanny SP, Kuyruk S, Sekaran P, Hawley A, Brooks JA, Bekhit E, Hutson JM, Crameri J, McLeod E, Teague WJ, King SK (2020) The burden of esophageal dilatations following repair of esophageal atresia. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2020.02.018
Baird R, Lal DR, Ricca RL, Diefenbach KA, Downard CD, Shelton J, Somme S, Grabowski J, Oyetunji TA, Williams RF et al (2019) Management of long gap esophageal atresia: a systematic review and evidence-based guidelines from the APSA Outcomes and Evidence Based Practice Committee. J Pediatr Surg 54(4):675–687. https://doi.org/10.1016/j.jpedsurg.2018.12.019
Lopes MF, Botelho MF (2007) Midterm follow-up of esophageal anastomosis for esophageal atresia repair: long-gap versus non-long-gap. Dis Esophagus 20(5):428–435. https://doi.org/10.1111/j.1442-2050.2007.00691.x
Upadhyaya VD, Gangopadhyaya AN, Gupta DK, Sharma SP, Kumar V, Pandey A, Upadhyaya AD (2007) Prognosis of congenital tracheoesophageal fistula with esophageal atresia on the basis of gap length. Pediatr Surg Int 23(8):767–771. https://doi.org/10.1007/s00383-007-1964-0
Thakkar HS, Cooney J, Kumar N, Kiely E (2014) Measured gap length and outcomes in oesophageal atresia. J Pediatr Surg 49(9):1343–1346. https://doi.org/10.1016/j.jpedsurg.2014.03.021
Shah R, Varjavandi V, Krishnan U (2015) Predictive factors for complications in children with esophageal atresia and tracheoesophageal fistula. Dis Esophagus 28(3):216–223. https://doi.org/10.1111/dote.12177
Parolini F, Leva E, Morandi A, Macchini F, Gentilino V, Di Cesare A, Torricelli M (2013) Anastomotic strictures and endoscopic dilatations following esophageal atresia repair. Pediatr Surg Int 29(6):601–605. https://doi.org/10.1007/s00383-013-3298-4
Quiroz HJ, Turpin A, Willobee BA, Ferrantella A, Parreco J, Lasko D, Perez EA, Sola JE, Thorson CM (2020) Nationwide analysis of mortality and hospital readmissions in esophageal atresia. J Pediatr Surg 55:824–829. https://doi.org/10.1016/j.jpedsurg.2020.01.025
Castilloux J, Noble AJ, Faure C (2010) Risk factors for short- and long-term morbidity in children with esophageal atresia. J Pediatr 156(5):755–760. https://doi.org/10.1016/j.jpeds.2009.11.038
Acknowledgments
The statistical analysis was supported by National Taiwan University Hospital, Hsin-Chu Branch and Yu-Han, Chang, MPH from Clinical Trial Center, National Taiwan University Hospital and Chin-Hao, Chang, PhD, from Department of Medical Research, National Taiwan University Hospital. The supplementary online figure in our article was drafted by Chun-Min, Kang, MD.
Author information
Authors and Affiliations
Contributions
Hung-Chieh, Chou conceived the study. Po-Nien, Tsao, Ting-An Yen, and Chien-Yi, Chen designed the study. Yi-Hsuan, Lu collected and analyzed the data. The first draft of manuscript was written by Yi-Hsuan, Lu. All authors contributed to manuscript revisions and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
This research study was conducted retrospectively from data obtained for clinical purpose. The Institutional Review Board of the National Taiwan University Hospital approved this study (NTUH 201901076 RINC).
Additional information
Communicated by Daniele De Luca
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary online Fig. 1
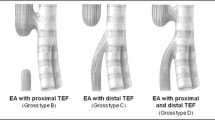
Types of esophageal atresia with/without tracheoesophageal fistula (EA/TEF) Listed to gross classification. Type A is isolated EA. Type B is EA with a proximal fistula connecting the upper pouch of the esophagus and the trachea. Type C is EA with a distal fistula connecting the lower pouch of the esophagus and the trachea. Type D involves both fistulae connecting the upper/lower pouch and the trachea. Type E or H TEF involves a fistula connecting the esophagus and the trachea without EA. (PNG 12327 kb)
Rights and permissions
About this article
Cite this article
Lu, YH., Yen, TA., Chen, CY. et al. Risk factors for digestive morbidities after esophageal atresia repair. Eur J Pediatr 180, 187–194 (2021). https://doi.org/10.1007/s00431-020-03733-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-020-03733-1