Abstract
Objective
Recent studies have reported that neutrophil-to-lymphocyte ratio (NLR) is associated with cardiovascular disease. The aim of the present study was to investigate the prognostic value of NLR in aortic disease.
Methods
We systematically searched electronic databases (Cochrane, PubMed, Elsevier, Medline, and Embase) from their inception to March 2020. Observational studies that evaluated the relationship between NLR and aortic disease were eligible for critical appraisal. Data were extracted from applicable articles, risk ratio (RR), weighted mean differences (MD) and 95% confidence intervals (CI) were calculated by RevMan 5.3, and statistical heterogeneity was assessed by the I2 statistic.
Results
Fourteen studies enrolling 4066 individuals were included in the meta-analysis. Compared with the control group, NLR was significantly higher in the aortic disease group (MD 3.44, 95%CI: 0.81–6.07, P = 0.01, I2 = 99%). The NLR was also significantly higher in non-survivors with aortic disease, compared to the survivors (MD 4.62, 95%CI: 2.75–6.50, P < 0.00001, I2 = 60%). Compared with the aortic disease patients with a low NLR, mortality was significantly higher in those with a high NLR (RR 2.63, 95%CI: 1.79–3.86, P < 0.00001, I2 = 67%).
Conclusion
Based on current evidence, an elevated NLR was associated with aortic disease and in-hospital mortality. Raised NLR also demonstrated a significantly increased the risk of mortality after surgical repair in aortic disease patients. NLR may be a good prognostic biomarker in aortic disease and deserve further research in this area.
Similar content being viewed by others
Introduction
Aortic disease is common and consists of pathologies that are both congenital and acquired. Aortic aneurysm and aortic dissection are the most frequent types of aortic disease which have high complication rates and carry a high risk of mortality [1, 2]. Literature has shown that inflammation of the aortic wall is considered to be the principal causes of aortic disease. It has been found that inflammatory biomarkers such as macrophages, C-reactive protein, neutrophils, lymphocytes are elevated in aortic disease [3,4,5].
Complete blood count parameters are widely known markers of systemic inflammation and have been associated with various cardiovascular diseases [6, 7]. Neutrophils secret various enzymes and mediators to participate in inflammation. High neutrophil counts are highly susceptible to inflammation not only in infective disease, but also in cardiovascular diseases. Low lymphocyte counts reflect the inflammation that is associated with adverse outcomes in patients with cardiovascular diseases [8]. Therefore, the neutrophil to lymphocyte ratio (NLR) is easy to obtain, inexpensive and widely available that has been suggested as a new indicator of inflammation and a predictor of clinical outcomes in cardiovascular disease, in addition to traditional markers [9, 10].
Recently, the relationship between NLR and aortic disease has been investigated by several studies [11, 12]. Authors focus on the NLR level in aortic aneurysm and aortic dissection patients, and the predictive value of high NLR in mortality and other clinical outcomes [13,14,15,16,17,18,19,20,21,22,23,24,25,26]. Therefore, the current meta-analysis was performed to clarify the relationship between NLR and aortic disease.
Methods
Search strategy
This study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA). We performed a literature search by a comprehensive computer search of electronic databases (Cochrane, PubMed, Medline, Elsevier, and Embase) from their inception to March 2020. Medical subject headings (MeSH) and free-text words were used in the meta-analysis. The following search terms were used: “Neutrophil lymphocyte ratio (MeSH)”, “NLR (MeSH)”, “aortic disease (MeSH)”, “aortic aneurysm (MeSH)”, “aortic dissection (MeSH)”. When appropriate, Boolean operators (NOT, AND, OR) were used to widen or narrow the search range. The references, reviews and editorials in the retrieved articles were manually searched for relevant articles.
Study selection
The inclusion criteria were listed as follows: (a) publications about observational studies focused on the relationship between NLR and aortic disease, (b) participants in the studies had aortic aneurysm or aortic dissection, (c) studies grouped with aortic disease and control, or high NLR and low NLR, and (d) The NLR in each group was presented as mean ± standard error (SD). Letters, reviews, case reports, animal studies, or non-English publications were excluded. All observational studies that met these requirements were considered eligible for the meta-analysis.
Data extraction
The literature search, study selection, and data extraction were done independently by 2 investigators (Y. Xu and H. Fang). Any discrepancies were resolved by the coauthors (Z. Qiu and X. Cheng). The following data were collected: first author name, publication year, country, journal, sources of controls, sample size, cutoff values for NLR, and outcomes.
Quality assessment
Newcastle-Ottawa scale (NOS) was used to assess the quality of the included studies by 2 investigators (Y. Xu and Z. Qiu) [27]. Studies included in the current meta-analysis was judged on three main dimensions: the selection of the study groups, the comparability of the study populations, and the determination of the exposure. The total score for a single study ranged from 0 to 9 stars. Studies whose scores less than 5 stars were categorized as low quality, scores 5–7 stars categorized as moderate quality, and scores more than 7 stars categorized as high quality. The mean score of studies in the meta-analysis was 7.8 stars. Another 11 items were used for assessing Kalkan ME’s study [26], which was a case-sectional study and recommend by AHRQ (Agency for Healthcare Research and Quality), the score is 10.
Data synthesis and meta-analysis
The meta-analysis and statistical analyses were performed by Review Manager (RevMan) version 5.3 (The Nordic Cochrane Centre, Rigshospitalet, Copenhagen, Denmark). Weighted mean differences (MD), 95% confidence intervals (CI), and risk ratio (RR) were used to evaluate the association between NLR and aortic disease. The Mantel-Haenszel method for fixed effects and the DerSimonian-Laird method for random effects were used to estimate MD, RR. The heterogeneity among studies was tested by Cochran’s Q statistic and I2 test. A P < 0.1 and I2 test value > 50% indicated substantial heterogeneity; in that case, the summary estimate was analyzed by the random effects model. Otherwise, the fixed effects model was used. Statistical significance was set at a P < 0.05 (two-tailed).
Results
General characteristic of studies included in the meta-analysis
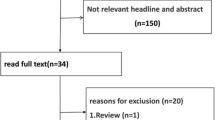
The initial search produced 98 results, of which 23 records met the general inclusion criteria and were reviewed for strict screening the titles and abstracts, the PRISMA study flowchart was shown in Fig. 1. After reviewing the full-text articles, the remaining 14 observational studies were included in current meta-analysis [13,14,15,16,17,18,19,20,21,22,23,24,25,26].
The patient demographics and basic characteristics of the included studies were shown in Table 1. Overall, these studies included 4066 patients. Four studies evaluated the NLR value in aortic disease (n = 868). Six studies investigated the NLR value in survivor and non-survivor patients with aortic disease (n = 600). Seven studies estimated the relationship between high or low NLR and mortality in aortic disease (n = 2963). The cutoff values of NLR for dichotomization ranged from 3.5 to 9.7024. The worse outcomes included in-hospital mortality and long-term mortality, follow-up period ranged from 30 days to 10 years. Among these 14 studies, 13 were cohort studies, and 1 was a case-sectional study.
The level of NLR in aortic disease
The relationship between the NLR value and aortic disease was reported in four studies that included 460 aortic disease patients and 408 controls [13, 15,16,17]. The patients with aortic aneurysm in two studies (n = 391), and with aortic dissection in other two studies (n = 477). Significant heterogeneity was found between the two groups (I2 = 99%) (Fig. 2). Analysis of the overall effect on NLR revealed a significant difference in NLR between individuals in the aortic disease and control group (MD 3.44, 95%CI: 0.81–6.07, P = 0.01). A subgroup analysis was conducted for patients from different aortic disease. The results showed NLR value was significantly higher in patients with aortic aneurysm and aortic dissection than individuals in the control group (MD 0.48, 95%CI: 0.19–0.76, P = 0.001, I2 = 0%; MD 6.45, 95%CI: 5.26–7.64, P < 0.00001, I2 = 64%). Compared with individuals in the control group, the NLR was significantly higher in aortic disease patients.
The relationship between NLR and mortality in aortic disease
Researches have shown NLR is a predictive marker of mortality in aortic disease. Six studies investigated the NLR level in survivor and non-survivor patients with aortic disease [14, 16,17,18,19,20]. One hundred sixty-sixdeceased patients, and 434 survived patients were included in meta-analysis. The patients with aortic aneurysm in one study, and with aortic dissection in other five studies. Analysis of the overall effect revealed NLR value was significantly higher in non-survivor patients with aortic disease (MD 4.62, 95%CI: 2.75–6.5, P < 0.00001, I2 = 60%) (Fig. 3). We also performed a subgroup analysis according to different aortic disease. The results showed NLR was significantly higher in non-survivor patients than those in survivor patients (MD 5.15, 95%CI: 2.94–7.35, P < 0.00001, I2 = 53%).
Prognostic value of high NLR for mortality in aortic disease
Seven studies also investigated the prognostic value of high NLR for mortality in aortic disease, the outcome was mortality [14, 21,22,23,24,25,26]. One thousand one hundred thirty-nine aortic disease patients in the high NLR group, and 1824 aortic disease patients in the low NLR group were included in meta-analysis (Fig. 4). The mortality rate in high NLR group of aortic disease patients was 17.91% (n = 204/1139), and in low NLR group was 9.1% (n = 166/1824). The patients with aortic aneurysm who underwent surgical repair in six studies, and with aortic dissection who underwent surgical repair in the other study. Analysis of the overall effect showed that the mortality in high NLR group of aortic disease patients was 2.63 times higher than that in low NLR group (RR 2.63, 95%CI: 1.79–3.86, P < 0.00001, I2 = 67%). Result of subgroup analysis also showed that NLR greater than the cutoff value was associated with higher mortality in aortic aneurysm patients (RR 2.60, 95%CI: 1.67–4.05, P < 0.0001, I2 = 72%). Overall, aortic disease patients with a high NLR had significantly higher mortality after surgical repair than those with a low NLR.
Sensitivity analysis and publication bias
The heterogeneity among studies reporting on the relationship between NLR and mortality changed to 34% after eliminating the study by Oz K et al. [16] (MD 3.52, 95%CI: 2.23–4.81, P < 0.00001) (Supplemental Fig. 1). The heterogeneity among studies reporting on prognostic value of high NLR for mortality changed to 0% after eliminating the study by Appleton ND et al. [21] (RR 3.06, 95%CI: 2.36–3.98, P < 0.00001) (Supplemental Fig. 2).
Funnel plot, Egger’s and Begg’s test are used to access publication bias in most meta-analysis. We did not assess publication bias in this meta-analysis, because the number of trials was low.
Discussion
Accumulated evidence has shown that NLR is a simple and reliable marker for predicting worse outcomes in systematic inflammatory disease [28, 29]. In this meta-analysis, we evaluated the prognostic role of NLR in aortic disease from 14 observational studies. The results showed aortic disease patients and these patients who died on hospitalization had higher NLR. Raised NLR also demonstrated a significantly increased the risk of mortality after surgical repair in 2963 patients with aortic disease. According to our literature screening, this is the first meta-analysis to evaluate the link between NLR and aortic disease.
Inflammation represents a main pathophysiological feature contributing to the development of aortic aneurysm and aortic dissection [30, 31]. It is plausible that the damaged aorta, due to the inflammatory process within the wall and intima, may enlarge more easily and may be more prone to re-dissection and rupture [32, 33]. Vrsalovic M et al. conducted a systematic review and found elevated admission C-reactive protein levels indicated increased in-hospital and medium-term mortality in aortic disease [34]. The high white blood cell count level on admission was related to high in-hospital mortality in patients with aortic dissection [35]. Elevated NLR correlated well with other markers of inflammation, such as C-reactive protein, interleukin-6, tumor necrosis factor-alpha [36, 37]. NLR was first described in 1967 as a novel inflammatory biomarker that recently been linked to cardiovascular disease, such as heart failure, coronary artery disease (CAD) [38]. In the present study, we demonstrated the association between the NLR and aortic disease, this result was similar with others [14, 15, 17].
Several factors have been suggested to be associated with poor outcomes in aortic disease patients, such as older age, the large diameter of the descending aorta, and shock [39, 40]. However, few effective biomarkers predicting the prognosis of patients with aortic disease are currently available [40]. In our meta-analysis, we found that elevated NLR predicted worse outcomes in patients with aortic aneurysm and aortic dissection. Tan TP et al. conducted a meta-analysis to investigate the prognostic value of NLR in cardiovascular surgery. They found that raised NLR appeared to be associated with increased mortality and morbidity after cardiac and vascular surgery [10]. Elevated NLR was also associated with increasingly severe symptoms of peripheral artery disease in a graded response from claudication to tissue loss, and was independently associated with preoperatively and postoperatively and complications after lower extremity procedures [41].
C-reactive protein has been widely used in the clinical setting to assess inflammatory disorders. However, Wada H et al. found NLR was strongly associated with poor clinical outcomes in CAD patients with low C-reactive protein levels [42]. In the Rotterdam study, even with the addition of C-reactive protein in the multivariate model, an elevated NLR remained an independent predictor of all-cause mortality and cardiovascular mortality [43]. De jager CP et al. [44] also found NLR predict bacteremia better than conventional infection markers like C-reactive protein, white blood cell count and neutrophil in emergency department admission. NLR was a better predictor of weaning failure than leukocyte levels and C-reactive protein in patients receiving invasive mechanical ventilation [45]. Previous studies have reported that NLR is associated with malignant diseases [46]. In included studies of the meta-analysis, patients with relatively high NLR were excluded active inflammatory disease and known malignancy. Overall, NLR is a simple, widely applied, and inexpensive and easily accessible inflammatory marker in various cardiac and vascular diseases.
In our meta-analysis, we found the NLR level was significantly higher in aortic aneurysm and aortic dissection patients compared with controls, and there was a great disparity between the aortic aneurysm subgroup (MD 0.48) and the aortic dissection subgroup (MD 6.45). The patients with aortic aneurysm included in our meta-analysis were non-ruptured aortic aneurysm patients, the inflammatory response occurred in these patients was chronic and low-grade. However, the patients with aortic dissection patients were acute aortic dissection patients. Acute aortic dissection and ruptured aortic aneurysm were emergency and life-threatening diseases associated with severe mortality, a strong inflammatory response occurred in acute and ruptured status. The level of NLR was significantly higher in patients with ruptured aortic aneurysm compared with those with non-ruptured [15, 18]. The subgroup analysis results showed patients with aortic aneurysm and aortic dissection had higher NLR than the controls with moderate heterogeneity (I2 = 0%, I2 = 64%), but a significant heterogeneity was detected when the data were combined and analysed (I2 = 99%), the great disparity between two subgroups may be the sources of heterogeneity.
Our meta-analysis has several limitations. First, marked heterogeneity among studies was observed, the source of heterogeneity need to be explored. Second, NLR has been reported in a variety of different ways, and there has not been an established method for reporting NLR. Third, the cutoff value of NLR in included studies are different. The most of patients were men. Finally, all studies in the meta-analysis were observational. Large- scale RCT trials are necessary to further validate the current results.
Conclusions
In conclusion, this meta-analysis showed that an elevated NLR was associated with aortic disease and in-hospital mortality. Raised NLR also demonstrated a significantly increased the risk of mortality after surgical repair in aortic disease patients. NLR may be a good prognostic biomarker in aortic disease and deserve further research in this area.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- NLR:
-
Neutrophil-to-lymphocyte ratio
- RevMan:
-
Review Manager
- RR:
-
Risk ratio
- MD:
-
Weighted mean differences
- CI:
-
Confidence intervals
- SD:
-
Standard error
- NOS:
-
Newcastle-Ottawa scale
- AHRQ:
-
Agency for Healthcare Research and Quality
- CAD:
-
Coronary artery disease
References
Lu N, Hu P, Wang J, Yan W, He Z, Xu T, et al. Simple renal cysts are associated with 24-month prognosis of patients with type B aortic dissection and hypertension. Can J Cardiol. 2019;35(11):1499–504.
Kochanek KD, Murphy SL, Xu J, Tejada-Vera B. Deaths: final data for 2014. Natl Vital Stat Rep. 2016;65(4):1–122.
Eliason JL, Hannawa KK, Ailawadi G, Sinha I, Ford JW, Deogracias MP, et al. Neutrophil depletion inhibits experimental abdominal aortic aneurysm formation. Circulation. 2005;112(2):232–40.
He R, Guo DC, Estrera AL, Safi HJ, Huynh TT, Yin Z, et al. Characterization of the inflammatory and apoptotic cells in the aortas of patients with ascending thoracic aortic aneurysms and dissections. J Thorac Cardiovasc Surg. 2006;131(3):671–8.
Sakakura K, Kubo N, Ako J, Wada H, Fujiwara N, Funayama H, et al. Peak C-reactive protein level predicts long-term outcomes in type B acute aortic dissection. Hypertension. 2010;55(2):422–9.
Kristono GA, Holley AS, Harding SA, Larsen PD. White blood cell subtypes as predictors of adverse cardiac events. Coron Artery Dis. 2020;31(5):446-50.
Cho JH, Cho HJ, Lee HY, Ki YJ, Jeon ES, Hwang KK, et al. Neutrophil-lymphocyte ratio in patients with acute heart failure predicts in-hospital and long-term mortality. J Clin Med. 2020;9(2):E557.
Núñez J, Sanchis J, Bodí V, Núñez E, Heatta AM, Miñana G, et al. Therapeutic implications of low lymphocyte count in non-ST segment elevation acute coronary syndromes. Eur J Intern Med. 2009;20(8):768–74.
Boralkar KA, Kobayashi Y, Amsallem M, Ataam JA, Moneghetti KJ, Cauwenberghs N, et al. Value of neutrophil to lymphocyte ratio and its trajectory in patients hospitalized with acute heart failure and preserved ejection fraction. Am J Cardiol. 2020;125(2):229–35.
Tan TP, Arekapudi A, Metha J, Prasad A, Venkatraghavan L. Neutrophil-lymphocyte ratio as predictor of mortality and morbidity in cardiovascular surgery: a systematic review. ANZ J Surg. 2015;85(6):414–9.
Balta S, Alemdar R, Yildirim AO, Erdogan S, Ozturk C, Celik T. The relationship between neutrophil-lymphocyte ratio and acute aortic dissection. Perfusion. 2017;32(4):336–7.
Sbarouni E, Georgiadou P, Kosmas E, Analitis A, Voudris V. Platelet to lymphocyte ratio in acute aortic dissection. J Clin Lab Anal. 2018;32(7):e22447.
Ikenaga H, Kurisu S, Watanabe N, Shimonaga T, Higaki T, Iwasaki T, et al. Predictive value of neutrophil to lymphocyte ratio for the presence of coronary artery ectasia in patients with aortic aneurysms. Int J Cardiol Heart Vessel. 2014;4:30–4.
King AH, Schmaier AH, Harth KC, Kumins NH, Wong VL, Zidar DA, et al. Elevated neutrophil-lymphocyte ratio predicts mortality following elective endovascular aneurysm repair. J Vasc Surg. 2020;S0741–5214(19):32550–9.
Vuruşkan E, Saraçoğlu E, Düzen İV. Serum bilirubin levels and the Presenc and progression of abdominal aortic aneurysms. Angiology. 2017;68(5):428–32.
Oz K, Iyigun T, Karaman Z, Çelik Ö, Akbay E, Akınc O, et al. Prognostic value of neutrophil to lymphocyte ratio and risk factors for mortality in patients with Stanford type a aortic dissection. Heart Surg Forum. 2017;20(3):E119–23.
Onuk T, Güngör B, Karataş B, Ipek G, Akyüz S, Ozcan KS, et al. Increased neutrophil to lymphocyte ratio is associated with in-hospital mortality in patients with aortic dissection. Clin Lab. 2015;61(9):1275–82.
Bedel C, Selvi F. Association of Platelet to lymphocyte and neutrophil to lymphocyte ratios with in-hospital mortality in patients with type a acute aortic dissection. Braz J Cardiovasc Surg. 2020;34(6):694–8.
Karakoyun S, Gürsoy MO, Akgün T, Öcal L, Kalçık M, Yesin M, et al. Neutrophil-lymphocyte ratio may predict in-hospital mortality in patients with acute type a aortic dissection. Herz. 2015;40(4):716–21.
Lafçi G, Ciçek ÖF, Uzun HA, Yalçinkaya A, Diken Aİ, Turak O, et al. Relationship of admission neutrophil-to-lymphocyte ratio with in-hospital mortality in patients with acute type I aortic dissection. Turk J Med Sci. 2014;44(2):186–92.
Appleton ND, Bailey DM, Morris-Stiff G, Lewis MH. Neutrophil to lymphocyte ratio predicts perioperative mortality following open elective repair of abdominal aortic aneurysms. Vasc Endovascular Surg. 2014;48(4):311–6.
Aurelian SV, Adrian M, Andercou O, Bruno S, Alexandru O, Catalin T, et al. Neutrophil-to-lymphocyte ratio (NLR): a comparative study of rupture to non-ruptured infra-renal abdominal aortic aneurysm. Ann Vasc Surg. 2019;58:270-5.
Bath J, Smith JB, Kruse RL, Vogel TR. Association of neutrophil-to-lymphocyte ratio with outcomes after elective abdominal aortic aneurysm repair. J Vasc Nurs. 2019;37(3):213–20.
Kordzadeh A, Malietzis G, Browne T, Prionidis I, Panayiotopoulos YP. Neutrophil to lymphocyte ratio (NLR) of five predicts 30-day morbidity in ruptured abdominal aortic aneurysms (rAAA): a retrospective cohort study. Int J Surg. 2015;15:45–8.
Lareyre F, Raffort J, Le D, Chan HL, Houerou TL, Cochennec F, et al. High neutrophil to lymphocyte ratio is associated with symptomatic and ruptured thoracic aortic aneurysm. Angiology. 2018;69(8):686–91.
Kalkan ME, Kalkan AK, Gündeş A, Yanartaş M, Oztürk S, Gurbuz AS, et al. Neutrophil to lymphocyte ratio: a novel marker for predicting hospital mortality of patients with acute type a aortic dissection. Perfusion. 2017;32(4):321–7.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The new-castle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses; 2000. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Clarke SJ, Burge M, Feeney K, Gibbs P, Jones K, Marx G, et al. The prognostic role of inflammatory markers in patients with metastatic colorectal cancer treated with bevacizumab: a translational study [ASCENT]. PLoS One. 2020;15(3):e0229900.
Maestrini I, Tagzirt M, Gautier S, Dupont A, Mendyk AM, Susen S, et al. MPO is partially associated with neutrophil deleterious effect in acute cerebral ischemia. Neurology. 2020;10:1212.
Nordon IM, Hinchliffe RJ, Loftus IM, Thompson MM. Pathophysiology and epidemiology of abdominal aortic aneurysms. Nat Rev Cardiol. 2011;8(2):92–102.
del Porto F, Proietta M, Tritapepe L, Miraldi F, Koverech A, Cardelli P, et al. Inflammation and immune response in acute aortic dissection. Ann Med. 2010;42(8):622–9.
Wu D, Choi JC, Sameri A, Minard CG, Coselli JS, Shen YH, et al. Inflammatory cell infiltrates in acute and chronic thoracic aortic dissection. Aorta (Stamford). 2013;1(6):259–67.
Jia LX, Zhang WM, Zhang HJ, Li TT, Wang YL, Qin YW, et al. Mechanical stretch-induced endoplasmic reticulum stress, apoptosis and inflammation contribute to thoracic aortic aneurysm and dissection. J Pathol. 2015;236(3):373–83.
Vrsalović M, Vrsalović PA. Admission C-reactive protein and outcomes in acute aortic dissection: a systematic review. Croat Med J. 2019;60(4):309–15.
Ma M, Shi J, Feng X, Wang J, Liu L, Wei X. The elevated admission white blood cell count relates to adverse surgical outcome of acute Stanford type a aortic dissection. J Cardiothorac Surg. 2020;15(1):48.
Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol. 2008;102(6):653–7.
Kantola T, Klintrup K, Väyrynen JP, Vornanen J, Bloigu R, Karhu T, et al. Stage-dependent alterations of the serum cytokine pattern in colorectal carcinoma. Br J Cancer. 2012;107(10):1729–36.
Afari ME, Bhat T. Neutrophil to lymphocyte ratio (NLR) and cardiovascular diseases: an update. Expert Rev Cardiovasc Ther. 2016;14(5):573–7.
Tolenaar JL, Froehlich W, Jonker FH, Upchurch GR Jr, Rampoldi V, Tsai TT, et al. Predicting in-hospital mortality in acute type B aortic dissection: evidence from international registry of acute aortic dissection. Circulation. 2014;130(11 Suppl 1):S45–50.
Ueki C, Sakaguchi G, Shimamoto T, Komiya T. Prognostic factors in patients with uncomplicated acute type B aortic dissection. Ann Thorac Surg. 2014;97(3):767–73.
Bath J, Smith JB, Kruse RL, Vogel TR. Neutrophil-lymphocyte ratio predicts disease severity and outcome after lower extremity procedures. J Vasc Surg. 2019;S0741–5214(19):32648–5.
Wada H, Dohi T, Miyauchi K, Nishio R, Takeuchi M, Takahashi N, et al. Neutrophil to lymphocyte ratio and long-term cardiovascular outcomes in coronary artery disease patients with low high-sensitivity C-reactive protein level. Int Heart J. 2020;61(3):447–53.
Fest J, Ruiter TR, Groot Koerkamp B, Rizopoulos D, Ikram MA, van Eijck CHJ, et al. The neutrophil-to-lymphocyte ratio is associated with mortality in the general population: the Rotterdam study. Eur J Epidemiol. 2019;34(5):463–70.
de Jager CP, van Wijk PT, Mathoera RB, de Jongh-Leuvenink J, van der Poll T, Wever PC. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit Care. 2010;14(5):R192.
Luo Z, Zheng Y, Yang L, Liu S, Zhu J, Zhao N, et al. Neutrophil/lymphocyte ratio is helpful for predicting weaning failure: a prospective, observational cohort study. J Thorac Dis. 2018;10(9):5232–45.
Templeton AJ, McNamara MG, Šeruga B, Vera-Badillo FE, Aneja P, Ocaña A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):dju124.
Acknowledgements
Not applicable.
Declaration of conflicting interests
None.
Funding
Study design, data collection, data management and synthesis, paper retouching, and paper proofreading were support by the National Natural Science Foundation of China (81760086).
Author information
Authors and Affiliations
Contributions
Yan Xu, Haiyang Fang collected the data and drafted the manuscript. Yan Xu, Zhiqiang Qiu and Xiaoshu Cheng edited the manuscript, participated in the study design and coordination, and helped to draft the manuscript. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Supplementary information
Additional file 1.
Supplemental Figure 1 The sensitive analysis for the relationship between NLR and mortality.
Additional file 2.
Supplemental Figure 2 The sensitive analysis for prognostic value of high NLR for mortality.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, Y., Fang, H., Qiu, Z. et al. Prognostic role of neutrophil-to-lymphocyte ratio in aortic disease: a meta-analysis of observational studies. J Cardiothorac Surg 15, 215 (2020). https://doi.org/10.1186/s13019-020-01263-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-020-01263-3