Abstract
Background
The value of counting inflammatory cells and especially their counting ratio in predicting adverse clinical outcomes in patients with acute coronary syndrome (ACS) undergoing revascularization has been shown, but the results of studies have been very diverse and paradoxical. The aim of the current study was to systematically review the studies that investigated the role of increased neutrophil-to-lymphocyte ratio (NLR) in predicting long-term clinical outcomes in patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI).
Methods
Data abstraction was independently performed by both un-blinded reviewers on deeply assessing Medline, Web of Knowledge, Google Scholar, Scopus, and Cochrane Central Register of Controlled Trials and using the relevant keywords. The risk of bias for each study was assessed using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions and the QUADAS-2 tool. Statistical analysis was performed using the Stata software. Overall, 14 articles published between 2010 and 2021 were eligible for the final analysis.
Results
A total of 20,846 ACS patients undergoing PCI were included. Higher values of NLR were associated with higher numbers of involved coronaries (RR: 1.175, 95%CI 1.021–1.353, P = 0.024). Increasing the value of NLR was associated with a 3.4 times increase in long-term death (RR: 3.424, 95%CI 2.325–5.025, P = 0.001). Similarly, higher values of NLR were significantly associated with a higher likelihood of long-term MACE (RR: 2.604, 95%CI 1.736–3.906, P = 0.001).
Conclusions
NLR has a high value in predicting both the severity of coronary artery involvement and long-term adverse clinical outcomes following the PCI procedure.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
There are multiple risk factors that can make a person more susceptible to arterial atherosclerosis. Along with genetic factors, which have been proven to play a role in various cardiovascular disorders, environmental and metabolic factors also contribute to the development of vascular disorders. Diabetes mellitus, hyperlipidemia, smoking, hypertension, and metabolic syndrome are all potential triggers for atherosclerotic processes, often by activating inflammatory processes, endothelial dysfunction, and oxidative stress [1,2,3]. The connection between inflammation and atherosclerosis is well-established. Inflammatory cells in the bloodstream produce cytokines and metalloproteinases, which lead to the formation of atherosclerotic plaques. These plaques increase the risk of tissue ischemia, ultimately resulting in acute myocardial infarction [4, 5]. It seems that the activation and accumulation of inflammatory cells such as neutrophils and lymphocytes also play a pathogenic role in the instability of atherosclerotic plaque [6]. It has been demonstrated that neutrophils have been recognized as key players in the process of athero-inflammation [7]. The white blood cells known as neutrophils have the ability to produce and release various enzymes, including matrix metalloproteinases, as well as different types of cytokines such as interleukin-1β and interleukin-6. These substances are believed to be the primary agents responsible for causing damage to the arterial plaque and vascular endothelial dysfunction, which in turn increases the risk of ischemia [8, 9]. In other words, neutrophil granulocytes can induce platelet aggregation in the intravascular lumen which results in increasing the extent of myocardial infarction [10]. Besides, lymphocytes have been also shown to have some inflammation-suppressing properties and therefore lowering the levels of lymphocytes may be associated with the risk for cardiac adverse sequels [11]. An increase in neutrophil count and a decrease in lymphocyte count, along with a higher ratio of neutrophils to lymphocytes, may indicate the severity of coronary vascular involvement and its long-term consequences. These adverse events are more likely to occur in patients with a history of cardiac ischemia who are undergoing revascularization procedures [12]. In this study, we thoroughly evaluated and reviewed research on the impact of a higher neutrophil-to-lymphocyte ratio (NLR) on the long-term clinical outcomes of patients with acute coronary syndrome (ACS) who are undergoing a percutaneous coronary intervention (PCI) procedure.
Methods
Search strategy
We conducted a study in accordance with the PRISMA-P protocols to review and analyze eligible studies on the long-term outcomes of PCI procedures. Our search involved Medline, Web of Knowledge, Google Scholar, Scopus, and Cochrane Central Register of Controlled Trials (CENTRAL) using a predefined search strategy and with the relevant keywords of “neutrophil,” “lymphocyte,” “neutrophil-to-lymphocyte ratio,” “coronary,” “percutaneous coronary intervention,” and “acute coronary syndrome.” We only included studies in English that assessed long-term outcomes of the PCI procedure and used baseline NLR to predict adverse outcomes. We included both full-text reports and abstracts that provided sufficient information for the study. The exclusion criteria were studies lacking outcome data, those in non-English languages, case reports, case series, review papers, and studies that only evaluated short-term and hospital outcomes of the procedure.
Data abstraction and validity assessment
Both un-blinded reviewers performed data abstraction independently on structured forms. There were no differences in the data collection, but any disagreements were resolved through consensus. One of the review authors transferred the data into the Review Manager file. The data entry was double-checked by comparing it with the systematic review and extraction form. The second review author verified the accuracy of the analysis of study characteristics against the trial report. The following information was abstracted: demographic data, follow-up time, the severity of coronary valve involvement, and the number of procedural adverse events. These included long-term death and major cardiovascular adverse events (MACE), such as myocardial infarction, cerebrovascular events, renal insufficiency, thromboembolic events, or other clinical adverse events. Long-term outcomes were measured at least 12 months after PCI.
Statistical analysis
We evaluated the risk of bias for each study based on the Cochrane Handbook for Systematic Reviews of Interventions and the QUADAS-2 tool, resolving any disagreements through discussion. Our assessment included the domains of random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective outcome reporting, with each potential source of bias judged as high, low, or unclear. We provided quotes and justifications for our judgments in the 'Risk of bias' table and summarized the judgments for each domain across studies. We combined binary outcomes using the Mantel–Haenszel fixed effect or random-effect models. The odds ratios (ORs) and 95% confidence interval (CI) for OR were used as summary statistics for the comparison of dichotomous variables and for determining the likelihood of each adverse event after interventions. Cochrane’s Q test was used to determine the statistical heterogeneity of this study. This test was complemented with the I2 statistic, which quantifies the proportion of total variation across studies that is due to heterogeneity rather than chance. A value of I2 of 0–25% indicates insignificant heterogeneity, 26–50% low heterogeneity, 51–75% moderate heterogeneity, and 76–100% high heterogeneity. Publication bias was assessed by the rank correlation test and also confirmed by the funnel plot analysis. Reported values were two-tailed, and results were considered statistically significant at P = 0.05. Statistical analysis was performed using the Stata software (version 13.1, Stata Corp, College Station, TX, USA).
Results
Study selection and characteristics of the studies
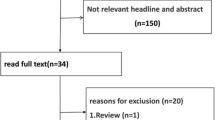
The flow diagram of the study selection is presented in Fig. 1. Initially, 62 articles were collected by database searches and review of the references. After removing 4 articles due to evidence of duplication, 58 records were primarily under-screened. Based on the titles and abstracts, 24 records were excluded and the remaining 34 citations were assessed for further eligibility. Of those, 20 were also excluded due to the incompleteness of the data and contents. In total, 14 articles published between 2010 and 2021 were eligible for the final analysis [13,14,15,16,17,18,19,20,21,22,23,24,25,26] (Table 1).
Methodological quality of the included studies
The studies included were assessed qualitatively by the QUADAS-2 tool. All 14 studies yielded good quality, and none of the citations was determined to have a high risk of bias (Fig. 2).
Overall study characteristics
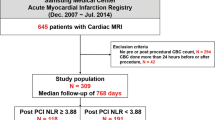
A total of 20,846 ACS patients undergoing PCI were included. Their mean age was 61.33 ± 4.39 years, range 49–69 years and 78.0% (ranged 59.6–89.7%) were male. The patients were followed up for 12–88 months for a mean follow-up time of 39 months (Table 1). With regard to coronary artery states, a wide range of multi-vessel involvement has been described in 14.4–78.8% of patients suffering from multi-vessel coronary disease (Table 2).
Outcome assessment
The two criteria were considered as the study end points including long-term death and long-term MACE. Regarding the death rate, the mean long-term mortality rate in the pointed population was estimated to be 8.2 ± 6.9% ranging from 1.4 to 35.0%. Furthermore, the long-term MACE rate was also shown to be 19.60 ± 11.52% ranged 3.7–50.0%.
The value of NLR to predict long-term outcome
It was first shown a significant association between NLR value and the number of involved coronary arteries that higher cutoff values of NLR were associated with higher numbers of involved coronaries (OR: 1.175, 95%CI 1.021–1.353, P = 0.024, Fig. 3). Besides, increasing the value of NLR (considering higher thresholds of this index) was associated with a 3.4 times increase in long-term death (OR: 3.424, 95%CI 2.325–5.025, P = 0.001), Fig. 4). Similarly, higher values of NLR were significantly associated with a higher likelihood of long-term MACE (OR: 2.604, 95%CI 1.736–3.906, P = 0.001). The heterogeneity among studies in reporting severity of coronary involvement (I2 = 62.723, P = 0.002), long-term death (I2 = 79.528, P = 0.001), and long-term MACE (I2 = 90.610, P = 0.001) remained significant. The publication bias is also significant for all study assessments assessed by the funnel plot with the p values ranging from 0.035 to 0.045 (Figs. 5, 6).
Discussion
It has been fully established that inflammatory cells play a significant role in the advancement of atherosclerotic plaque formation and injury. Research has been conducted to investigate the stimulatory role of some inflammatory factors in the destruction of atherosclerotic plaque and the reparative role of other factors. The development or inhibition of atherosclerosis is the outcome of the interaction between these two types of factors [27, 28]. Research has revealed that neutrophils' secretory activity, which involves producing and secreting certain cytokines and enzymes, can contribute to atherosclerotic plaque rupture, increased platelet aggregation, and the development of atherosclerosis [29]. Meanwhile, certain secretory compounds from lymphocytes can slow down this process. As a result, it is believed that keeping track of the number of these cells can forecast the immediate and prolonged clinical results of patients. According to existing research, the NLR is highly effective at predicting the occurrence of both short-term in-hospital events and long-term outcomes in patients with ACS [30]. Studies have demonstrated that the ability to predict outcomes for patients undergoing revascularization procedures varies greatly and is often conflicting. This can be attributed to several factors, including differences in follow-up duration, varying indicators used to select patients for the study, the severity of coronary artery involvement, underlying risk factors, and the design of the study. These factors have resulted in considerable heterogeneity in our study when determining the predictive value of the NLR index for patient mortality and long-term complications. Our findings indicate that the NLR index can play a dual role. Firstly, it can predict the severity of coronary artery involvement based on the number of affected arteries. Secondly, a higher NLR threshold level is associated with increased long-term mortality rates and a higher incidence of long-term complications or MACE after the PCI procedure. In other words, increasing the mentioned ratio can increase the mortality of patients more than 3.4 times and long-term MACE more than 2.6 times. Therefore, it seems that this parameter, along with other predictive clinical and laboratory factors, can be strongly used to predict the adverse events of the procedure.
Conclusions
It can be finally concluded that increasing NLR is associated with a higher likelihood of long-term outcomes including mortality and MACE following PCI procedure in ACS patients. Of course, the results of the studies were very heterogeneous, which could be due to the very different follow-up period as well as different definition criteria to define the long-term consequences of this procedure.
Availability of data and materials
All data generated or analyzed during this study are included in this published article, and further in detailed one are available from the corresponding author on reasonable request.
Abbreviations
- NLR:
-
Neutrophil-to-lymphocyte ratio
- ACS:
-
Acute coronary syndrome
- PCI:
-
Percutaneous coronary intervention
- RRs:
-
Risk ratios
- CI:
-
Confidence interval
References
Dawson LP, Layland J (2022) High-risk coronary plaque features: a narrative review. Cardiol Ther 11(3):319–335. https://doi.org/10.1007/s40119-022-00271-9
Demandt JPA, Zelis JM, Koks A, Smits GHJM, van der Harst P, Tonino PAL, Dekker LRC, van Het Veer M, Vlaar PJ (2022) Prehospital risk assessment in patients suspected of non-ST-segment elevation acute coronary syndrome: a systematic review and meta-analysis. BMJ Open 12(4):e057305
Bauer D, Toušek P (2021) Risk stratification of patients with acute coronary syndrome. J Clin Med 10(19):4574. https://doi.org/10.3390/jcm10194574
Olejarz W, Łacheta D, Kubiak-Tomaszewska G (2020) Matrix metalloproteinases as biomarkers of atherosclerotic plaque instability. Int J Mol Sci 21(11):3946. https://doi.org/10.3390/ijms21113946
Lahdentausta L, Leskelä J, Winkelmann A, Tervahartiala T, Sorsa T, Pesonen E, Pussinen PJ (2018) Serum MMP-9 diagnostics, prognostics, and activation in acute coronary syndrome and its recurrence. J Cardiovasc Transl Res 11(3):210–220. https://doi.org/10.1007/s12265-018-9789-x
Sim DS, Ahn Y (2013) Novel inflammatory biomarkers in acute coronary syndrome. Korean J Intern Med 28(2):156–158. https://doi.org/10.3904/kjim.2013.28.2.156
Shirakawa K, Sano M (2022) Neutrophils and neutrophil extracellular traps in cardiovascular disease: an overview and potential therapeutic approaches. Biomedicines 10(8):1850. https://doi.org/10.3390/biomedicines10081850
Maleki M, Tajlil A, Separham A, Sohrabi B, Pourafkari L, Roshanravan N, Aslanabadi N, Najjarian F, Mashayekhi S, Ghaffari S (2021) Association of neutrophil to lymphocyte ratio (NLR) with angiographic SYNTAX score in patients with non-ST-Segment elevation acute coronary syndrome (NSTE-ACS). J Cardiovasc Thorac Res 13(3):216–221
Paula da Silva MV, Villar-Delfino PH, Nogueira-Machado JA, Oliveira Volpe CM (2022) IL-6, IL-1β and MDA correlate with thrombolysis in myocardial infarction (TIMI) risk score in patients with acute coronary syndrome. Recent Adv Inflamm Allergy Drug Discov. https://doi.org/10.2174/2772270816666220211091231
Sridhar SK (2020) Significance of neutrophil-lymphocyte ratio as predictor of in-hospital morbidity and mortality in acute coronary syndrome. J Assoc Physicians India 68(1):56
Das D, Magoon R (2022) Letter to Editor: Predictive value of neutrophil to lymphocyte ratio on acute kidney injury after on-pump coronary artery bypass: a retrospective, single-center study. Gen Thorac Cardiovasc Surg 70(9):832–833
Shen XH, Chen Q, Shi Y, Li HW (2010) Association of neutrophil/lymphocyte ratio with long-term mortality after ST elevation myocardial infarction treated with primary percutaneous coronary intervention. Chin Med J 123:3438–3443
Han YC, Yang TH, Kim DI et al (2013) Neutrophil to lymphocyte ratio predicts long-term clinical outcomes in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Korean Circ J 43:93–99
Kaya MG, Akpek M, Lam YY et al (2013) Prognostic value of neutrophil/ lymphocyte ratio in patients with ST-elevated myocardial infarction undergoing primary coronary intervention: a prospective, multicenter study. Int J Cardiol 168:1154–1159
Sen N, Afsar B, Ozcan F et al (2013) The neutrophil to lymphocyte ratio was associated with impaired myocardial perfusion and long term adverse outcome in patients with ST-elevated myocardial infarction undergoing primary coronary intervention. Atherosclerosis 228:203–210
Arbel Y, Shacham Y, Ziv-Baran T et al (2014) Higher neutrophil/lymphocyte ratio is related to lower ejection fraction and higher long-term all-cause mortality in ST-elevation myocardial infarction patients. Can J Cardiol 30:1177–1182
Ergelen M, Uyarel H, Altay S et al (2014) Predictive value of elevated neutrophil to lymphocyte ratio in patients undergoing primary angioplasty for ST-segment elevation myocardial infarction. Clin Appl Thromb Hemost 20:427–432
Pan W, Zhao D, Zhang C et al (2015) Application of neutrophil/lymphocyte ratio in predicting coronary blood flow and mortality in patients with ST-elevation myocardial infarction undergoing percutaneous coronary intervention. J Cardiol 66:9–14
Zhou D, Wan Z, Fan Y, Zhou J, Yuan Z (2015) A combination of the neutrophil-to-lymphocyte ratio and the GRACE risk score better predicts PCI outcomes in Chinese Han patients with acute coronary syndrome. Anatol J Cardiol 15(12):995–1001. https://doi.org/10.5152/AnatolJCardiol.2015.6174
Wada H, Dohi T, Miyauchi K, Shitara J, Endo H, Doi S, Konishi H, Naito R, Tsuboi S, Ogita M, Kasai T, Hassan A, Okazaki S, Isoda K, Suwa S, Daida H (2017) Pre-procedural neutrophil-to-lymphocyte ratio and long-term cardiac outcomes after percutaneous coronary intervention for stable coronary artery disease. Atherosclerosis 265:35–40. https://doi.org/10.1016/j.atherosclerosis.2017.08.007
Zuin M, Rigatelli G, Picariello C, Dell’Avvocata F, Marcantoni L, Pastore G, Carraro M, Nanjundappa A, Faggian G, Roncon L (2017) Correlation and prognostic role of neutrophil to lymphocyte ratio and SYNTAX score in patients with acute myocardial infarction treated with percutaneous coronary intervention: a six-year experience. Cardiovasc Revasc Med 18(8):565–571. https://doi.org/10.1016/j.carrev.2017.05.007
Xu N, Tang XF, Xu JJ, Yao Y, Song Y, Liu R, Jiang L, Jiang P, Wang HH, Zhao XY, Chen J, Gao Z, Qiao SB, Yang YJ, Gao RL, Xu B, Yuan JQ (2019) Predictive value of neutrophil to lymphocyte ratio on long-term outcomes of acute myocardial infarction patients with multivessel disease. Zhonghua Xin Xue Guan Bing Za Zhi 47(1):42–48. https://doi.org/10.3760/cma.j.issn.0253-3758.2019.01.005
Choi DH, Kobayashi Y, Nishi T, Kim HK, Ki YJ, Kim SS, Park KH, Song H, Fearon WF (2019) Combination of mean platelet volume and neutrophil to lymphocyte ratio predicts long-term major adverse cardiovascular events after percutaneous coronary intervention. Angiology 70(4):345–351. https://doi.org/10.1177/0003319718768658
Fan W, Liu Y, Zhang Y, Gao X, Shi F, Liu J, Sun L (2022) Prognostic value of a novel dNLR-PNI score in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Perfusion 24:2676591221090620
Gu LF, Gu J, Wang SB, Wang H, Wang YX, Xue Y, Wei TW, Sun JT, Lian XQ, Liu JB, Jia EZ, Wang LS (2021) Combination of D-dimer level and neutrophil to lymphocyte ratio predicts long-term clinical outcomes in acute coronary syndrome after percutaneous coronary intervention. Cardiol J. https://doi.org/10.5603/CJ.a2021.0097
Wang H, Liu Z, Shao J, Lin L, Jiang M, Wang L, Lu X, Zhang H, Chen Y, Zhang R (2020) Immune and inflammation in acute coronary syndrome: molecular mechanisms and therapeutic implications. J Immunol Res 2020:4904217. https://doi.org/10.1155/2020/4904217
Centurión OA (2016) Serum biomarkers and source of inflammation in acute coronary syndromes and percutaneous coronary interventions. Cardiovasc Revasc Med 17(2):119–128
Kamińska J, Koper OM, Siedlecka-Czykier E, Matowicka-Karna J, Bychowski J, Kemona H (2018) The utility of inflammation and platelet biomarkers in patients with acute coronary syndromes. Saudi J Biol Sci 25(7):1263–1271. https://doi.org/10.1016/j.sjbs.2016.10.015
He J, Bian X, Song C, Zhang R, Yuan S, Yin D, Dou K (2022) High neutrophil to lymphocyte ratio with type 2 diabetes mellitus predicts poor prognosis in patients undergoing percutaneous coronary intervention: a large-scale cohort study. Cardiovasc Diabetol 21(1):156
Rostami A, Tajlil A, Separham A, Sohrabi B, Pourafkari L, Roshanravan N, Aslanabadi N, Ziaee M, Mashayekhi S, Ghaffari S (2021) Association between neutrophil-to-lymphocyte ratio and the systemic inflammatory immunologic index and the angiographic SYNTAX score and the TIMI flow grade in acute STEMI: a Cohort Study. J Tehran Heart Cent 16(4):147–155. https://doi.org/10.18502/jthc.v16i4.8600
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
FSH and SB analyzed and interpreted the data. NR and SA were major contributors in writing the manuscript. BR revised all the manuscript and supervised all the above from beginning to the end. All of the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shahsanaei, F., Abbaszadeh, S., Behrooj, S. et al. The value of neutrophil-to-lymphocyte ratio in predicting severity of coronary involvement and long-term outcome of percutaneous coronary intervention in patients with acute coronary syndrome: a systematic review and meta-analysis. Egypt Heart J 76, 39 (2024). https://doi.org/10.1186/s43044-024-00469-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-024-00469-3