Abstract
Background
Conservative management is recommended as the first therapeutic step in chronic low back pain (LBP), but there is no available evidence regarding the possible effect of patients’ baseline characteristics on the therapeutic outcomes. A systematic review of the literature was performed to investigate this point.
Methods
In February 2024, all the level I studies investigating the role of pharmacological management for chronic LBP were accessed. Data concerning the patient demographic at baseline were collected: number of patients and related mean BMI and age, duration of the symptoms, duration of the follow-up, percentage of females, Numeric Rating Scale (NRS), the Roland Morris Disability Questionnaire (RMQ), Oswestry Disability Index (ODI). The outcomes at the last follow-up were evaluated through NRS, RMQ, and ODI. A multiple linear model regression diagnostic through the Pearson Product-Moment Correlation Coefficient (r) was used.
Results
Data from 47 articles (9007 patients) were obtained. The analysis yielded the following significant associations: age at baseline and NRS at follow-up (r = − 0.22; P = 0.04), NRS at baseline with NRS (r = 0.26; P = 0.03) and RMQ (r = − 0.58; P = 0.02) at follow-up, RMQ at baseline and the same at follow-up (r = 0.69; P = 0.0001).
Conclusion
Older age, higher BMI, presence of comorbidities, higher ODI and a long history of symptoms or surgical treatments do not reduce the efficacy of pharmacological management of chronic LBP. However, pharmacological therapy is not an effective option for patients with high baseline RMQ.
Level of evidence
I systematic review of RCTs.
Similar content being viewed by others
Introduction
Chronic low back pain (LBP) is one of the leading causes of disability worldwide [1, 2]. 40% of LBP is discogenic in nature [3], but in many patients a specific cause of pain cannot be identified [4]. Chronic LBP is increasingly prevalent and has an increasing socioeconomic impact. In the United States, over 80% of the population will experience one episode of chronic LBP during their lifetime [5]. While the majority of cases are self-limiting, 20–44% of the affected population will develop chronic symptoms [6]. The economic costs of LBP are estimated at between US$ 100–200 billion annually, mainly from loss in wages and productivity of the affected patients [7]. Conservative management of LBP, the first therapeutic step in international guidelines [8, 9], mainly consists of physical therapy and pharmacological management. Nonpharmacologic management is recommended as the first treatment option, but this can prove inadequate for some patients and, in this case, pharmacological therapy should be initiated [9]. Several therapeutic options are available and include non-steroidal anti-inflammatory drugs (NSAIDs), tricyclic antidepressants selective serotonin reuptake inhibitors (SSRIs), and opioids [9, 10]. A holistic approach to the management of patients with chronic LBP is required, and it includes the evaluation of social and psychological factors or expectations [8]. However, there is no available evidence regarding the possible effect of patients’ characteristics such as age, body mass index (BMI), gender, duration of symptoms and follow-up on the responsiveness to pharmacological therapy. The evaluation of a patient’s specific features and the identification of possible risk factors which may reduce the effectiveness of a given therapeutic approach is of paramount importance to tailor the management of the patient’s needs. Therefore, a systematic review of the literature was performed to investigate whether patients’ baseline characteristics influence the efficacy of pharmacological management in terms of pain and disability. In this way, it would be possible to highlight negative or positive prognostic factors to guide healthcare professionals in identifying the ideal candidate for pharmacological management of chronic LBP. A multiple linear model analysis was conducted to investigate the impact of duration of follow-up, age, gender, BMI, symptoms duration before treatment, previous surgery, comorbidities, pain and disability pre-treatment on pain and disability at the last available follow-up.
Methods
Eligibility criteria
All the randomised controlled trials (RCTs) investigating the role of pharmacological treatments for chronic LBP were accessed. Articles in English, German, Italian, French and Spanish, according to the authors language capabilities, were eligible. According to the Oxford Centre of Evidence-Based Medicine (OCEBM) [12], only level I of evidence were considered. Articles treating patients with diagnosed psychiatric disorders were included. Articles treating patients with any type or form of adjuvants were excluded. Studies reporting data on patients with neurological, mechanical or non-specific LBP were eligible. Studies reporting data on patients with acute LBP were excluded, along with those reporting data concerning the cervicothoracic or sacroiliac spine tracts. Reviews, letters, registers, case reports, editorials, and expert opinions were excluded. Animal, cadaveric and biomechanics studies were also excluded. Only articles reporting quantitative data on the patient-reported outcome measures (PROMs) at the last follow-up were eligible. Missing data under the outcomes of interest warranted the exclusion from this study.
Search strategy
The present study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement [11]. The search strategy was the following:
-
P (population): chronic low back pain;
-
I (intervention): medical treatments;
-
C (correlation): patient demographic, therapy protocol and clinical scores;
-
O (outcomes): Pain and disability.
Data source
In February 2024, the literature search was performed by two authors (A.B. & F.S.) independently. The following databases were accessed: PubMed, Google Scholar, Embase, and Scopus. The following keywords were used in combination: low, lumbar, spine, back, pain, disability, therapy, treatments, drugs, medication, medicine, conservative, tricyclic antidepressants, acetaminophen, amoxicillin, flupirtine, baclofen, atc, bupropion, ssri, topiramate, gabapentinoids, selective serotonin reuptake inhibitors, opioids, gabapentin, pregabalin, celecoxib, etoricoxib, valdecoxib, naproxen, diclofenac, nsaid, coxib, selective, non-selective, visual analogic scale, numeric rating scale, roland morris questionnaire, oswestry disability index. The same authors screened the resulting papers for inclusion. The article full-text was accessed for eligible articles. A cross reference of the bibliographies was even performed. The process of data source and extraction was supervised by a third senior author (N.M.).
Data extraction
Two authors (A.B. & F.S.) independently performed data extraction. Study generalities (author, year, journal, type of study) and data concerning the patient demographic were collected: number of patients and related mean BMI and age, duration of the symptoms and of the follow-up (months), women (%), previous surgery (n), and comborbiditites (n). Data on the following PROMs were retrieved at baseline and at the last follow-up: Numeric Rating Scale (NRS), the Roland Morris Disability Questionnaire (RMQ) [13], Oswestry Disability Index (ODI) [14]. Data on the following PROMs were retrieved at last follow-up: NRS, RMQ, ODI.
Methodology quality assessment
For the methodological quality assessment, the risk of bias summary graph of the Review Manager Software (The Nordic Cochrane Collaboration, Copenhagen) was performed by two authors (A.B. & F.S.) independently. The following risks of bias were evaluated for analysis: selection, detection, reporting, attrition, and other source of bias.
Statistical analysis
The statistical analyses were performed by one author (F.M.). The baseline was assessed through the IBM SPSS software version 25. To assess whether factors at baseline (length of the follow-up symptoms duration, age, BMI, sex, previous surgery, comorbidities, PROMs) exert an influence on pain and disability at the last follow-up, a multiple linear model regression diagnostic was conducted. The STATA/MP 16.1 (StataCorp, College Station, TX) software was used. For pairwise correlation, the Pearson Product-Moment Correlation Coefficient (r) was used. The final effect ranked between + 1 (positive linear correlation) and − 1 (negative linear correlation), according to the Cauchy–Schwarz inequality. Values of 0.1 <| r |< 0.3, 0.3 <|r|< 0.5, and |r|> 0.5 were considered to have small, moderate, and strong correlations, respectively. The test of overall significance was performed through the χ2 test, with values of P < 0.05 considered statistically significant.
Results
Search result
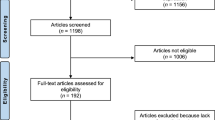
The literature search resulted in 2701 articles. Of them, 951 were RCTs, with 181 duplicates. A further 684 articles were not eligible: surgical waiting list articles (N = 2), not matching the topic (N = 231), major trauma, deformities, neurologic disorders, comorbidities or uncontrolled medical illness (N = 138), combined treatments (N = 112), spondylodiscitis or other infective illness (N = 37), language limitation (N = 45), acute onset LBP (N = 49), cervicothoracic or sacroiliac pain (N = 41), other (N = 29). Given the lack of data on the outcomes of interests, a further 39 RCTs were excluded. This left 47 articles for review. The literature search results are shown in Fig. 1.
Methodological quality assessment
The risk of selection bias was low, reflecting the selective inclusion of RCTs. Two-thirds of the included papers performed sample blinding, thus leading to a poor to moderate risk of detection bias. The overall good quality of the included studies results in a low risk of reporting, attrition and other biases. Concluding, the quality of the methodological assessment scored good. The Cochrane graph of the bias tool is shown in Fig. 2.
Patient demographics
Data from 9007 patients (mean age 52.6 ± 7.0 years; mean BMI: 28.3 ± 2.8 kg/m2; mean duration of symptoms before beginning treatment: 81.2 ± 46.2 months; mean follow-up: 3.2 ± 3.2 months) were obtained. At baseline, NRS scored 55.3 ± 19.5, RMQ 10.67 ± 2.6, and ODI 37.20 ± 11.1. Patient demographics are shown in Table 1.
Outcomes of interest
No evidence of a statistically significant association was observed between NRS, RMQ and ODI at the last follow-up and other parameters such as symptom duration before treatment, duration of the follow-up, gender, BMI, comorbidities and previous surgeries. Patients’ age at baseline showed evidence of a statistically significant negative association with the NRS (r = − 0.22; P = 0.04). The ODI at baseline also did not influence any of the outcomes at the last follow-up (P > 0.1). The NRS at baseline was associated proportionally with NRS (r = 0.26; P = 0.03) and RMQ (r = − 0.58; P = 0.02) at follow-up. The RMQ at baseline showed evidence of a statistically significant association with the RMQ at the last follow-up (r = 0.69; P = 0.0001). An overview of the main results is shown in Table 2.
Discussion
The main results of the present study were that in patients with chronic LBP, higher pain and disability levels at baseline showed evidence of a statistically significant association with poorer outcomes at the last follow-up, while a negative, albeit weak, association was observed between age and NRS. Other factors such as gender, BMI, comorbidities, duration of symptoms and previous surgeries did not have any influence on the effectiveness of the pharmacological therapy.
To our knowledge, this is the first study to assess the effects of patient baseline characteristics on the outcomes of the pharmacological management of chronic LBP. Given the availability of different treatment options for this condition, identifying the factors that, positively or negatively, are associated with the outcomes of a given therapy is paramount to offer patients the management with the highest likelihood of success based on their specific characteristics.
One previously published work highlighted numerous demographic, social and psychological factors associated with LBP [61]. Among these, older age and the consequent decline in mobility and cognitive function were reported to be possible risk factors for developing LBP [10]. Such features may suggest a worse prognosis for older patients, but this hypothesis was surprisingly not confirmed by the results of the present investigation. Even though the negative association between age and NRS was weak, and thus it may not be inferred that older patients show better outcomes than younger ones, it is safe to conclude that older age does not exert a negative impact on the effects of pharmacological management of LBP. Nonetheless, when planning pharmacological therapy for older individuals, it is of paramount importance to consider possible comorbidities and impairment of the renal and hepatic function to prevent potentially serious adverse events [10, 61].
Chronic LBP is reported to be more prevalent among women [1, 62, 63]. However, the available data show no association between gender and pain and disability levels after pharmacological therapy. While this management had the same effects on the male and female population, it is important to bear in mind the differences in the biomechanical and aetiologic backgrounds of LPB between the genders [64, 65], as these may be specifically targeted with additional physiotherapy or psychological support to tailor the therapy on the patients’ needs. Further research is required to investigate this topic.
One clinically relevant finding of the current study was that the duration of symptoms and previous spinal surgery did not exert a negative effect on the outcomes at the last follow-up after pharmacological therapy. This observation is relevant both for the treating physician, as a long course of unsatisfactory symptom control does not translate into a poorer prognosis, and for the patients. Pain-related fear and the perception of treatment failure contribute to a vicious cycle which potentially increases pain perception and disability [66, 67]. While specific psychological therapies can and should be employed to target this particular issue, an optimistic view, giving the message that previous treatment failure does not impact on the future outcome and prognosis, may represent a first step in reassuring the patients with a long history of spinal symptoms.
Notably, the RMQ at the last follow-up showed a strong association with the NRS and RMQ at baseline. This finding suggests that pharmacological management may not be sufficient to target the limitations that patients with chronic LBP encounter in their daily activities. Thus, in patients with consistent disability at baseline, a multimodal approach may be more successful [68]. Another interpretation of this finding is that the ODI offers a more nuanced scale (how much does an item apply to the patient) rather than a yes/no answer such as in the RMQ. Thus, after pharmacological management, a patient could be “less impaired” in the activities of daily living but still experience some limitations. While this can be highlighted with the use of the ODI, the results of the RMQ would likely be similar before and after treatment. Unfortunately, the literature regarding this aspect is still lacking, and the evidence concerning the most effective physiotherapeutic interventions is still low [69]. Further studies are required to investigate this point.
Many compounds are available for the pharmacological management of chronic LBP, including opioids, NSAIDs, and tricyclic antidepressants. Peck et al. [70] have published a comprehensive review of over-the-counter medication for the treatment of low back pain: all may be effective, but it is unclear whether one is more effective than the others. A recent systematic review observed that NSAIDs, duloxetine, baclofen and opiates are the most effective drugs in the setting of chronic LBP [10]. This highlights an area of future research, as different prognostic factors may be analysed concerning every specific treatment option. However, the available literature does not currently present sufficient data for this analysis, and thus represents a limitation of this work.
Another limitation of this study was that patients with neurological, mechanical and non-specific LBP were included. While a different aetiology may lead to a different response to the pharmacological management and thus to a different weight of prognostic factors on pain and disability, the available data did not allow a separate analysis for the different causes of LBP as the included investigations did not present separate outcomes for the different aetiologies included. Similarly, patients with concomitant psychological disorders were also included in the analysis: while this might represent a possible confounding factor, the authors opted to maintain these patients in the work to allow for sufficient numerosity. However, it is important to highlight that LBP is often managed by general practitioners and, upon successful initial treatment, a further investigation of the cause of LBP is not performed. Thus, despite possibly including a source of bias, the heterogeneity of the data reflects the clinical practice. Lastly, the available data were insufficient to perform a sub-analysis of possible differences among the predictive factors in the various considered pharmaceutic compounds. During the database search and data extraction, the inter-agreement rate was not evaluated.
Conclusion
Pharmacological management of LBP can yield good results also in older patients, in those with a higher BMI or other comorbidities, or patients with a long history of symptoms or previous surgical treatment. There are no differences between the genders in the effectiveness of pharmacological management. Patients who present with a high RMQ score are likely to maintain high RMQ values after treatment. A precise definition of the baseline traits influencing therapeutic outcomes in patients undergoing pharmacological therapy for chronic LBP is an essential step to tailor management to the specific needs and characteristics of the patient.
Availability of data and materials
The data underlying this article are available in the article and in its online supplementary material.
Abbreviations
- NRS:
-
Numeric Rating Scale
- RMQ:
-
The Roland Morris Disability Questionnaire
- ODI:
-
Oswestry Disability Index
- PROMs:
-
Patient-reported outcome measures
- RCT:
-
Randomised clinical trial
- BMI:
-
Body mass index
- NSAID:
-
Nonsteroidal anti-inflammatory drugs
- LBP:
-
Low back pain
References
Hayden JA, Wilson MN, Stewart S, Cartwright JL, Smith AO, Riley RD, van Tulder M, Bendix T, Cecchi F, Costa LOP, Dufour N, Ferreira ML, Foster NE, Gudavalli MR, Hartvigsen J, Helmhout P, Kool J, Koumantakis GA, Kovacs FM, Kuukkanen T, Long A, Macedo LG, Machado LAC, Maher CG, Mehling W, Morone G, Peterson T, Rasmussen-Barr E, Ryan CG, Sjogren T, Smeets R, Staal JB, Unsgaard-Tondel M, Wajswelner H, Yeung EW, Pain CLB, IPDM-AG. Exercise treatment effect modifiers in persistent low back pain: an individual participant data meta-analysis of 3514 participants from 27 randomised controlled trials. Br J Sports Med. 2020;54(21):1277–8. https://doi.org/10.1136/bjsports-2019-101205.
Fatoye F, Gebrye T, Odeyemi I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol Int. 2019;39(4):619–26. https://doi.org/10.1007/s00296-019-04273-0.
Migliore A, Sorbino A, Bacciu S, Bellelli A, Frediani B, Tormenta S, Pirri C, Foti C. The technique of intradiscal injection: a narrative review. Ther Clin Risk Manag. 2020;16:953–68. https://doi.org/10.2147/TCRM.S251495.
Bedaiwi MK, Sari I, Wallis D, O’Shea FD, Salonen D, Haroon N, Omar A, Inman RD. Clinical efficacy of celecoxib compared to acetaminophen in chronic nonspecific low back pain: results of a randomized controlled trial. Arthritis Care Res (Hoboken). 2016;68(6):845–52. https://doi.org/10.1002/acr.22753.
Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, Castel LD, Kalsbeek WD, Carey TS. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169(3):251–8. https://doi.org/10.1001/archinternmed.2008.543.
Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Jt Surg Am. 2006;88(Suppl 2):21–4. https://doi.org/10.2106/JBJS.E.01273.
van Tulder M, Koes B, Bombardier C. Low back pain. Best Pract Res Clin Rheumatol. 2002;16(5):761–75. https://doi.org/10.1053/berh.2002.0267.
Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, Mannion AF, Reis S, Staal JB, Ursin H, Zanoli G. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15(Suppl 2):S192–300. https://doi.org/10.1007/s00586-006-1072-1.
Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–30. https://doi.org/10.7326/M16-2367.
Migliorini F, Maffulli N, Eschweiler J, Betsch M, Catalano G, Driessen A, Tingart M, Baroncini A. The pharmacological management of chronic lower back pain. Expert Opin Pharmacother. 2020. https://doi.org/10.1080/14656566.2020.1817384.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. https://doi.org/10.1136/bmj.b2535.
Howick JCI, Glasziou P, Greenhalgh T, Carl Heneghan, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 Oxford CEBM levels of evidence. Oxford Centre for Evidence-Based Medicine. https://www.cebm.net/indexaspx?o=5653
Stevens ML, Lin CC, Maher CG. The Roland Morris disability questionnaire. J Physiother. 2016;62(2):116. https://doi.org/10.1016/j.jphys.2015.10.003.
Fairbank JC. Oswestry disability index. J Neurosurg Spine. 2014;20(2):239–41. https://doi.org/10.3171/2013.7.SPINE13288.
Allan L, Richarz U, Simpson K, Slappendel R. Transdermal fentanyl versus sustained release oral morphine in strong-opioid naive patients with chronic low back pain. Spine (Phila Pa 1976). 2005;30(22):2484–90. https://doi.org/10.1097/01.brs.0000186860.23078.a8.
Atkinson JH, Slater MA, Wahlgren DR, Williams RA, Zisook S, Pruitt SD, Epping-Jordan JE, Patterson TL, Grant I, Abramson I, Garfin SR. Effects of noradrenergic and serotonergic antidepressants on chronic low back pain intensity. Pain. 1999;83(2):137–45. https://doi.org/10.1016/s0304-3959(99)00082-2.
Atkinson JH, Slater MA, Capparelli EV, Patel SM, Wolfson T, Gamst A, Abramson IS, Wallace MS, Funk SD, Rutledge TR, Wetherell JL, Matthews SC, Zisook S, Garfin SR. A randomized controlled trial of gabapentin for chronic low back pain with and without a radiating component. Pain. 2016;157(7):1499–507. https://doi.org/10.1097/j.pain.0000000000000554.
Baron R, Martin-Mola E, Muller M, Dubois C, Falke D, Steigerwald I. Effectiveness and safety of tapentadol prolonged release (PR) versus a combination of tapentadol PR and pregabalin for the management of severe, chronic low back pain with a neuropathic component: a randomized, double-blind, phase 3b study. Pain Pract. 2015;15(5):455–70. https://doi.org/10.1111/papr.12200.
Birbara CA, Puopolo AD, Munoz DR, Sheldon EA, Mangione A, Bohidar NR, Geba GP, Etoricoxib Protocol 042 Study Group. Treatment of chronic low back pain with etoricoxib, a new cyclo-oxygenase-2 selective inhibitor: improvement in pain and disability: a randomized, placebo-controlled, 3-month trial. J Pain. 2003;4(6):307–15. https://doi.org/10.1016/s1526-5900(03)00633-3.
Braten LCH, Rolfsen MP, Espeland A, Wigemyr M, Assmus J, Froholdt A, Haugen AJ, Marchand GH, Kristoffersen PM, Lutro O, Randen S, Wilhelmsen M, Winsvold BS, Kadar TI, Holmgard TE, Vigeland MD, Vetti N, Nygaard OP, Lie BA, Hellum C, Anke A, Grotle M, Schistad EI, Skouen JS, Grovle L, Brox JI, Zwart JA, Storheim K, Group AIMs. Efficacy of antibiotic treatment in patients with chronic low back pain and Modic changes (the AIM study): double blind, randomised, placebo controlled, multicentre trial. BMJ. 2019;367:l5654. https://doi.org/10.1136/bmj.l5654.
Buynak R, Shapiro DY, Okamoto A, Van Hove I, Rauschkolb C, Steup A, Lange B, Lange C, Etropolski M. Efficacy and safety of tapentadol extended release for the management of chronic low back pain: results of a prospective, randomized, double-blind, placebo- and active-controlled phase III study. Expert Opin Pharmacother. 2010;11(11):1787–804. https://doi.org/10.1517/14656566.2010.497720.
Chu LF, D’Arcy N, Brady C, Zamora AK, Young CA, Kim JE, Clemenson AM, Angst MS, Clark JD. Analgesic tolerance without demonstrable opioid-induced hyperalgesia: a double-blinded, randomized, placebo-controlled trial of sustained-release morphine for treatment of chronic nonradicular low-back pain. Pain. 2012;153(8):1583–92. https://doi.org/10.1016/j.pain.2012.02.028.
Coats TL, Borenstein DG, Nangia NK, Brown MT. Effects of valdecoxib in the treatment of chronic low back pain: results of a randomized, placebo-controlled trial. Clin Ther. 2004;26(8):1249–60. https://doi.org/10.1016/S0149-2918(04)80081-X.
Gordon A, Callaghan D, Spink D, Cloutier C, Dzongowski P, O’Mahony W, Sinclair D, Rashiq S, Buckley N, Cohen G, Kim J, Boulanger A, Piraino PS, Eisenhoffer J, Harsanyi Z, Darke AC, Michalko KJ. Buprenorphine transdermal system in adults with chronic low back pain: a randomized, double-blind, placebo-controlled crossover study, followed by an open-label extension phase. Clin Ther. 2010;32(5):844–60. https://doi.org/10.1016/j.clinthera.2010.04.018.
Hale ME, Ahdieh H, Ma T, Rauck R, Oxymorphone ERSG. Efficacy and safety of OPANA ER (oxymorphone extended release) for relief of moderate to severe chronic low back pain in opioid-experienced patients: a 12-week, randomized, double-blind, placebo-controlled study. J Pain. 2007;8(2):175–84. https://doi.org/10.1016/j.jpain.2006.09.011.
Hwang CJ, Lee JH, Kim JH, Min SH, Park KW, Seo HY, Song KS. Gabapentin versus transdermal fentanyl matrix for the alleviation of chronic neuropathic pain of radicular origin: a randomized blind multicentered parallel-group noninferiority trial. Pain Res Manag. 2019;2019:4905013. https://doi.org/10.1155/2019/4905013.
Jamison RN, Raymond SA, Slawsby EA, Nedeljkovic SS, Katz NP. Opioid therapy for chronic noncancer back pain. A randomized prospective study. Spine (Phila Pa 1976). 1998;23(23):2591–600. https://doi.org/10.1097/00007632-199812010-00014.
Kalita J, Kohat AK, Misra UK, Bhoi SK. An open labeled randomized controlled trial of pregabalin versus amitriptyline in chronic low backache. J Neurol Sci. 2014;342(1–2):127–32. https://doi.org/10.1016/j.jns.2014.05.002.
Katz J, Pennella-Vaughan J, Hetzel RD, Kanazi GE, Dworkin RH. A randomized, placebo-controlled trial of bupropion sustained release in chronic low back pain. J Pain. 2005;6(10):656–61. https://doi.org/10.1016/j.jpain.2005.05.002.
Katz N, Rauck R, Ahdieh H, Ma T, Gerritsen van der Hoop R, Kerwin R, Podolsky G. A 12-week, randomized, placebo-controlled trial assessing the safety and efficacy of oxymorphone extended release for opioid-naive patients with chronic low back pain. Curr Med Res Opin. 2007;23(1):117–28. https://doi.org/10.1185/030079906x162692.
Khoromi S, Patsalides A, Parada S, Salehi V, Meegan JM, Max MB. Topiramate in chronic lumbar radicular pain. J Pain. 2005;6(12):829–36. https://doi.org/10.1016/j.jpain.2005.08.002.
Klinger R, Kothe R, Schmitz J, Kamping S, Flor H. Placebo effects of a sham opioid solution: a randomized controlled study in patients with chronic low back pain. Pain. 2017;158(10):1893–902. https://doi.org/10.1097/j.pain.0000000000000977.
Konno S, Oda N, Ochiai T, Alev L. Randomized, double-blind, placebo-controlled phase III trial of duloxetine monotherapy in Japanese patients with chronic low back pain. Spine (Phila Pa 1976). 2016;41(22):1709–17. https://doi.org/10.1097/BRS.0000000000001707.
Krebs EE, Gravely A, Nugent S, Jensen AC, DeRonne B, Goldsmith ES, Kroenke K, Bair MJ, Noorbaloochi S. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: the SPACE randomized clinical trial. JAMA. 2018;319(9):872–82. https://doi.org/10.1001/jama.2018.0899.
Markman JD, Frazer ME, Rast SA, McDermott MP, Gewandter JS, Chowdhry AK, Czerniecka K, Pilcher WH, Simon LS, Dworkin RH. Double-blind, randomized, controlled, crossover trial of pregabalin for neurogenic claudication. Neurology. 2015;84(3):265–72. https://doi.org/10.1212/WNL.0000000000001168.
Muehlbacher M, Nickel MK, Kettler C, Tritt K, Lahmann C, Leiberich PK, Nickel C, Krawczyk J, Mitterlehner FO, Rother WK, Loew TH, Kaplan P. Topiramate in treatment of patients with chronic low back pain: a randomized, double-blind, placebo-controlled study. Clin J Pain. 2006;22(6):526–31. https://doi.org/10.1097/.ajp.0000192516.58578.a4.
Perrot S, Krause D, Crozes P, Naim C, GZS Group. Efficacy and tolerability of paracetamol/tramadol (325 mg/37.5 mg) combination treatment compared with tramadol (50 mg) monotherapy in patients with subacute low back pain: a multicenter, randomized, double-blind, parallel-group, 10-day treatment study. Clin Ther. 2006;28(10):1592–606. https://doi.org/10.1016/j.clinthera.2006.10.001.
Pheasant H, Bursk A, Goldfarb J, Azen SP, Weiss JN, Borelli L. Amitriptyline and chronic low-back pain. A randomized double-blind crossover study. Spine (Phila Pa 1976). 1983;8(5):552–7. https://doi.org/10.1097/00007632-198307000-00012.
Pota V, Barbarisi M, Sansone P, Moraci M, Pace MC, Passavanti MB, Aurilio C. Combination therapy with transdermal buprenorphine and pregabalin for chronic low back pain. Pain Manag. 2012;2(1):23–31. https://doi.org/10.2217/pmt.11.71.
Robertson K, Marshman LAG, Plummer D, Downs E. Effect of gabapentin vs pregabalin on pain intensity in adults with chronic sciatica: a randomized clinical trial. JAMA Neurol. 2019;76(1):28–34. https://doi.org/10.1001/jamaneurol.2018.3077.
Romano CL, Romano D, Bonora C, Mineo G. Pregabalin, celecoxib, and their combination for treatment of chronic low-back pain. J Orthop Traumatol. 2009;10(4):185–91. https://doi.org/10.1007/s10195-009-0077-z.
Ruoff GE, Rosenthal N, Jordan D, Karim R, Kamin M, Protocol C-SG. Tramadol/acetaminophen combination tablets for the treatment of chronic lower back pain: a multicenter, randomized, double-blind, placebo-controlled outpatient study. Clin Ther. 2003;25(4):1123–41. https://doi.org/10.1016/s0149-2918(03)80071-1.
Sakai Y, Ito K, Hida T, Ito S, Harada A. Pharmacological management of chronic low back pain in older patients: a randomized controlled trial of the effect of pregabalin and opioid administration. Eur Spine J. 2015;24(6):1309–17. https://doi.org/10.1007/s00586-015-3812-6.
Schiphorst Preuper HR, Geertzen JH, van Wijhe M, Boonstra AM, Molmans BH, Dijkstra PU, Reneman MF. Do analgesics improve functioning in patients with chronic low back pain? An explorative triple-blinded RCT. Eur Spine J. 2014;23(4):800–6. https://doi.org/10.1007/s00586-014-3229-7.
Schliessbach J, Vuilleumier PH, Siegenthaler A, Butikofer L, Limacher A, Juni P, Zeilhofer HU, Arendt-Nielsen L, Curatolo M. Analgesic effect of clobazam in chronic low-back pain but not in experimentally induced pain. Eur J Pain. 2017;21(8):1336–45. https://doi.org/10.1002/ejp.1032.
Schliessbach J, Siegenthaler A, Butikofer L, Limacher A, Juni P, Vuilleumier PH, Stamer U, Arendt-Nielsen L, Curatolo M. Effect of single-dose imipramine on chronic low-back and experimental pain. A randomized controlled trial. PLoS ONE. 2018;13(5):e0195776. https://doi.org/10.1371/journal.pone.0195776.
Schliessbach J, Siegenthaler A, Butikofer L, Vuilleumier P, Juni P, Stamer U, Arendt-Nielsen L, Curatolo M. Predicting drug efficacy in chronic low back pain by quantitative sensory tests. Eur J Pain. 2018;22(5):973–88. https://doi.org/10.1002/ejp.1183.
Schukro RP, Oehmke MJ, Geroldinger A, Heinze G, Kress HG, Pramhas S. Efficacy of duloxetine in chronic low back pain with a neuropathic component: a randomized, double-blind, placebo-controlled crossover trial. Anesthesiology. 2016;124(1):150–8. https://doi.org/10.1097/ALN.0000000000000902.
Shell WE, Charuvastra EH, DeWood MA, May LA, Bullias DH, Silver DS. A double-blind controlled trial of a single dose naproxen and an amino acid medical food theramine for the treatment of low back pain. Am J Ther. 2012;19(2):108–14. https://doi.org/10.1097/MJT.0b013e3181f4b297.
Skljarevski V, Zhang S, Desaiah D, Alaka KJ, Palacios S, Miazgowski T, Patrick K. Duloxetine versus placebo in patients with chronic low back pain: a 12-week, fixed-dose, randomized, double-blind trial. J Pain. 2010;11(12):1282–90. https://doi.org/10.1016/j.jpain.2010.03.002.
Skljarevski V, Zhang S, Chappell AS, Walker DJ, Murray I, Backonja M. Maintenance of effect of duloxetine in patients with chronic low back pain: a 41-week uncontrolled, dose-blinded study. Pain Med. 2010;11(5):648–57. https://doi.org/10.1111/j.1526-4637.2010.00836.x.
Steiner DJ, Sitar S, Wen W, Sawyerr G, Munera C, Ripa SR, Landau C. Efficacy and safety of the seven-day buprenorphine transdermal system in opioid-naive patients with moderate to severe chronic low back pain: an enriched, randomized, double-blind, placebo-controlled study. J Pain Symptom Manag. 2011;42(6):903–17. https://doi.org/10.1016/j.jpainsymman.2011.04.006.
Takahashi N, Omata JI, Iwabuchi M, Fukuda H, Shirado O. Therapeutic efficacy of nonsteroidal anti-inflammatory drug therapy versus exercise therapy in patients with chronic nonspecific low back pain: a prospective study. Fukushima J Med Sci. 2017;63(1):8–15. https://doi.org/10.5387/fms.2016-12.
Tetsunaga T, Tetsunaga T, Tanaka M, Ozaki T. Efficacy of tramadol-acetaminophen tablets in low back pain patients with depression. J Orthop Sci. 2015;20(2):281–6. https://doi.org/10.1007/s00776-014-0674-4.
Uberall MA, Mueller-Schwefe GH, Terhaag B. Efficacy and safety of flupirtine modified release for the management of moderate to severe chronic low back pain: results of SUPREME, a prospective randomized, double-blind, placebo- and active-controlled parallel-group phase IV study. Curr Med Res Opin. 2012;28(10):1617–34. https://doi.org/10.1185/03007995.2012.726216.
Urquhart DM, Wluka AE, van Tulder M, Heritier S, Forbes A, Fong C, Wang Y, Sim MR, Gibson SJ, Arnold C, Cicuttini FM. Efficacy of low-dose amitriptyline for chronic low back pain: a randomized clinical trial. JAMA Intern Med. 2018;178(11):1474–81. https://doi.org/10.1001/jamainternmed.2018.4222.
Webster LR, Butera PG, Moran LV, Wu N, Burns LH, Friedmann N. Oxytrex minimizes physical dependence while providing effective analgesia: a randomized controlled trial in low back pain. J Pain. 2006;7(12):937–46. https://doi.org/10.1016/j.jpain.2006.05.005.
Yang JH, Suk KS, Lee BH, Jung WC, Kang YM, Kim JH, Kim HS, Lee HM, Moon SH. Efficacy and safety of different aceclofenac treatments for chronic lower back pain: prospective, randomized, single center, open-label clinical trials. Yonsei Med J. 2017;58(3):637–43. https://doi.org/10.3349/ymj.2017.58.3.637.
Zaringhalam J, Manaheji H, Rastqar A, Zaringhalam M. Reduction of chronic non-specific low back pain: a randomised controlled clinical trial on acupuncture and baclofen. Chin Med. 2010;5:15. https://doi.org/10.1186/1749-8546-5-15.
Zerbini C, Ozturk ZE, Grifka J, Maini M, Nilganuwong S, Morales R, Hupli M, Shivaprakash M, Giezek H, Etoricoxib CSG. Efficacy of etoricoxib 60 mg/day and diclofenac 150 mg/day in reduction of pain and disability in patients with chronic low back pain: results of a 4-week, multinational, randomized, double-blind study. Curr Med Res Opin. 2005;21(12):2037–49. https://doi.org/10.1185/030079905X75069.
Wong AY, Karppinen J, Samartzis D. Low back pain in older adults: risk factors, management options and future directions. Scoliosis Spinal Disord. 2017;12:14. https://doi.org/10.1186/s13013-017-0121-3.
Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, Woolf A, Vos T, Buchbinder R. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–37. https://doi.org/10.1002/art.34347.
Palacios-Cena D, Albaladejo-Vicente R, Hernandez-Barrera V, Lima-Florencio L, Fernandez-de-Las-Penas C, Jimenez-Garcia R, Lopez-de-Andres A, de Miguel-Diez J, Perez-Farinos N. Female gender is associated with a higher prevalence of chronic neck pain, chronic low back pain, and migraine: results of the Spanish National Health Survey, 2017. Pain Med. 2020. https://doi.org/10.1093/pm/pnaa368.
Bento TPF, Genebra C, Maciel NM, Cornelio GP, Simeao S, Vitta A. Low back pain and some associated factors: is there any difference between genders? Braz J Phys Ther. 2020;24(1):79–87. https://doi.org/10.1016/j.bjpt.2019.01.012.
Scholtes SA, Van Dillen LR. Gender-related differences in prevalence of lumbopelvic region movement impairments in people with low back pain. J Orthop Sports Phys Ther. 2007;37(12):744–53. https://doi.org/10.2519/jospt.2007.2610.
Bunzli S, Smith A, Schutze R, Lin I, O’Sullivan P. Making sense of low back pain and pain-related fear. J Orthop Sports Phys Ther. 2017;47(9):628–36. https://doi.org/10.2519/jospt.2017.7434.
O’Sullivan PB, Caneiro JP, O’Keeffe M, Smith A, Dankaerts W, Fersum K, O’Sullivan K. Cognitive functional therapy: an integrated behavioral approach for the targeted management of disabling low back pain. Phys Ther. 2018;98(5):408–23. https://doi.org/10.1093/ptj/pzy022.
Heinrich M, Monstadt D, Michel C. Psychological therapy as part of an interdisciplinary treatment of chronic back pain. Orthopade. 2009;38(10):937–42. https://doi.org/10.1007/s00132-009-1486-7.
Owen PJ, Miller CT, Mundell NL, Verswijveren S, Tagliaferri SD, Brisby H, Bowe SJ, Belavy DL. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. 2020;54(21):1279–87. https://doi.org/10.1136/bjsports-2019-100886.
Peck J, Urits I, Peoples S, Foster L, Malla A, Berger AA, Cornett EM, Kassem H, Herman J, Kaye AD, Viswanath O. A comprehensive review of over the counter treatment for chronic low back pain. Pain Ther. 2020. https://doi.org/10.1007/s40122-020-00209-w.
Acknowledgements
None.
Funding
No external source of funding was used.
Author information
Authors and Affiliations
Contributions
FM: conception and design, statistical analysis, drafting (original and revision); NM: supervision, drafting (revision); MM: drafting (original); AB: literature search, study selection and data extraction, risk of bias assessment; FS: literature search, study selection and data extraction, risk of bias assessment; RV: supervision, drafting (revision). All authors have agreed to the final version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Professor Nicola Maffulli is the Editor in Chief of the Journal of Orthopaedic Surgery and Research. The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Baroncini, A., Maffulli, N., Mian, M. et al. Predictors of success of pharmacological management in patients with chronic lower back pain: systematic review. J Orthop Surg Res 19, 248 (2024). https://doi.org/10.1186/s13018-024-04741-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04741-9